Abstract
Objectives
Evaluating the outcomes of enhanced case management (ECM) for patients with tuberculosis (TB) in the North Central London TB Service (NCLTBS).
Design
Retrospective cohort study.
Setting
The NCLTBS provides care for persons diagnosed with TB across north and central London. Management involves both medical and psychosocial support, leading to the implementation ECM to provide additional non-clinical assistance to patients at risk of treatment non-completion. However, there has been limited evaluation of its outcomes.
Participants
All adults with TB notified to NCLTBS between January 2013 and June 2021.
Main outcome measures
Descriptive socio-economic and clinical characteristics grouped by binary ECM status (yes/no) and level (0–3). Clinical outcomes at 12 months (completed treatment, death, lost-to-follow-up, continuing on treatment) were compared using multivariable logistic regression.
Results
Totally, 2437 patients were included (57.2% male, 79.1% born outside the UK). Overall, 82.3% completed treatment and 4.1% died. Factors associated with mortality included older age (over 70 years odds ratio (OR) 3.3), inpatient diagnosis (OR 4.4), and mental health issues (OR 2.2). 52.8% received ECM, with the proportion increasing over time, and 76% of this group successfully competed treatment.
Conclusions
This comprehensive evaluation of ECM in a diverse London population indicates high treatment completion rates even among those with multiple social risk factors. However, ECM needs of patients has increased over time, with a particular rise in patients requiring the highest support level. Given the small difference between standard care and ECM categories 1 and 2, there may be scope to simplify the system.
Keywords: tuberculosis, respiratory medicine, infectious diseases, effectiveness of care, evidence-based practice
Despite a general reduction in the amount of tuberculosis disease (TB) in the UK since 2011, TB remains a significant clinical and public health issue, with 4425 cases notified in 2021, and an increased incidence recorded between 2022 and 2023. 1 The UK Health Security Agency (UKHSA) collects data on social factors associated with a greater risk of treatment non-completion, namely: harmful alcohol use, drug misuse, homelessness and history of imprisonment; and considers two additional risks (mental health and asylum seeker status). The proportion of people diagnosed with TB with social risk factors has increased from 8.9% in 2011 to 12.7% in 2020. 2 Improving treatment and outcomes of patients with social risk factors is a core element of the TB Action Plan for England (2021–2026). 3
The North Central London TB Service (NCLTBS) is a network of clinics responsible for investigation and management of TB across a large urban area of North London. The network cares for around 200–250 persons diagnosed with TB each year. In 2010 the service implemented a system of cohort review, comprising a quarterly appraisal of key clinical outcomes designed to improve service delivery, patient management and public health practice. This was derived from a similar system recommended by the US Centers for Disease Control and Prevention.4,5 In 2013 cohort review was supplemented by implementation of the UK Royal College of Nursing (RCN) individual case management system, where, on notification, patients undergo a holistic appraisal of their clinical and social circumstances and are assessed as requiring either standard case management (SCM), that is, are able to independently take their anti-TB medication and attend for routine follow-up, or enhanced case management (ECM), where they require a higher level of clinical, psychological and social support, as shown in Table 1. 6 This type of person-centred intervention is important as an increasing proportion of new diagnoses are culture positive, creating a risk of onward transmission or development of drug resistance if inadequately treated. 7
Table 1.
Standard and enhanced case management levels with indication of additional support offered.
| Enhanced case management level | Example risk factors | Interventions |
|---|---|---|
| Standard Case Management | No risk factors identified for poor treatment outcomes | Standard management: including case manager appointments or phone contacts at weeks 1 and 2, and months 1, 3, 4 and 5, in addition to doctor appointments at diagnosis, 2 and 6 months. |
| ECM 1 | Single risk factors identified, for example, older age, socially vulnerable, anxiety diagnosis, previous TB diagnosis, language barrier. | Increase nurse-led follow-up frequency, which may include additional nurse-led appointments and home visits. |
| ECM 2 | Significant risk factors identified, for example, previous non-compliance with TB treatment, single drug resistance, disease transmission within contacts. | Increased nurse led follow up, possibly necessitating involvement of additional services, such a social care involvement |
| ECM 3 | Multiple risk factors identified, for example, complex social/medical and/or mental health issues, for example persons with mental health and substance misuse problems living in temporary or insecure accommodation who rarely attend booked appointments, or with multi-drug resistant TB. | Likely to require multiple additional services, such as regular home support, including case manager, nurse and social care visits, and directly or video observed therapy |
ECM is provided to the most complex patients, including those with issues around drug and alcohol use, mental health concerns, or who are homeless. It offers a range of measures including referral to other health and social services, as well as increased frequency of home visits. Features of ECM are presented in Table 1. Patients identified as requiring ECM receive support from clinical and social service agencies to provide ongoing assistance throughout the treatment period. 6
In 2019, due to the number of patients requiring ECM, and based on further guidance from the Royal College of Nursing, a holistic, qualitative assessment of patient needs was used to identify which of three levels of ECM was required for each patient. 6 The aim was to improve the flexibility of the ECM system, identify those most at risk of poor outcomes, and provide appropriate levels of support to mitigate these. However, it is resource intensive and requires significant input from nurses, allied staff in the TB service and external agencies, in during the ECM assessment, triage and subsequent long-term follow-up.
Despite the significant resources required to deliver these services there has been little assessment of the ECM system since 2017, and no validation of the levels in the triage system. Here we present the results of a retrospective observational cohort study to describe and evaluate the use of ECM in TB patients notified to NCLTBS between 2013 and 2021, comparing the outcomes of those who did and did not receive ECM, and investigate the factors associated with additional risk of poor outcomes.
Methods
Records that were notified to the NCLTBS between 01/01/2013 and 30/06/2021 were extracted, duplicates were removed, with first episodes included where multiple episodes per patient were identified. Cases that had been de-notified and cases where notified after death were removed. Patient outcomes were updated to December 2023.
Local ECM status was added to each record. Ethnicity codes and self-reported ethnicity were aggregated into ethnic group categories (see Supplementary Table S1). Records for children under the age of 18 were excluded. The total adult cohort was analysed using a binary ECM status (yes or no) and compared to socio-economic risk factors. A secondary analysis was then undertaken with those notified between 01/01/2013 and 31/03/2019, where ECM status was a binary outcome (yes or no); and between 01/04/2019 and 30/06/2021 where ECM was categorised as levels 1, 2 and 3. Descriptive statistics were calculated for the whole cohort, age groups, and ECM status sub-groups.
Six outcome measures were considered, which were derived from the treatment outcome recorded in the database 12 months after notification: completed treatment, died, continuing on treatment at 12 months (CoT), lost-to-follow-up (LTF), transferred out (TO) to another TB service, and treatment stopped (TS). Records with no outcome recorded (database not completed or updated with12-month outcome by December 2023) were excluded. Associations between binary outcomes were undertaken with multivariate logistic regression using a stochastic average gradient method with Gaussian prior regularisation. Variables with collinearity correlations of >0.7 were not considered independent. Chi-squared testing was performed with Yates’ correction. All analysis was conducted in KNIME Analytics (v5.2.0, Zurich, Switzerland). As this was a service evaluation of routinely collected anonymised healthcare data, individual patient consent was not required. The study was registered as a Quality Improvement Project at the Royal Free Hospital NHS Foundation Trust.
Results
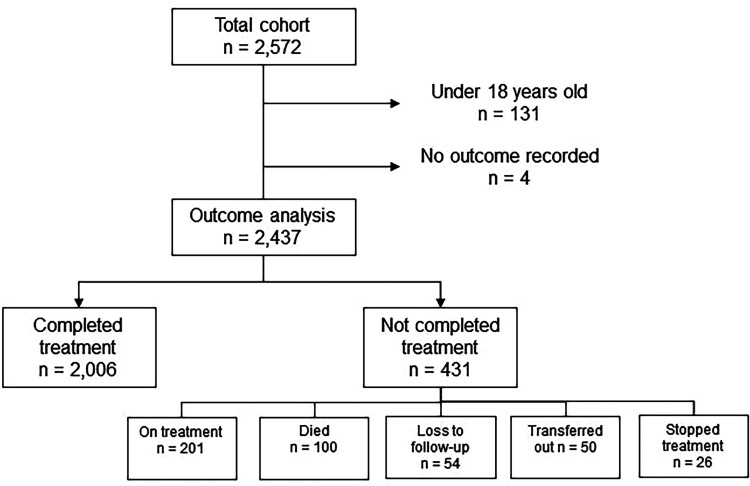
The total number of notifications recorded was 2889, of which 125 were duplicate entries for the same notification, 11 were later de-notified, and 3 were post-mortem diagnoses. A further 178 were secondary notifications for persons with multiple notifications, where the first instance of notification was included. Of the remaining 2572 individual patients, those under 18-years old (n = 131), and those with no 12-month outcome recorded (n = 4) were excluded and 2437 entered the outcomes analysis (Supplementary Table S2). Patient flow through the analysis is presented in Figure 1.
Figure 1.
Inclusions, exclusions, and 12-month outcomes of patients in the analysis.
Of this group, 82.3% completed treatment (n = 2006), 4.1% died (100), 2.2% were LTF (54), 8.2% were continuing on treatment (201), and 3.2% (76) had other outcomes (31). 57.2% were male, 47.5% were aged between 18 and 39 years and a further 33.2% between 40 and 59 years. 79.1% were not born in the UK and thus the cohort was ethnically diverse with 32.0% black, 26.6% white and 24.3% from Asian (Indian, Pakistani, Bangladeshi) backgrounds. Most lived in relatively deprived areas (27.9% in the two most deprived deciles 1 and 2, and 35.8% in deciles 3 and 4). Of recorded social risk factors 5.5% reported a history of drug use, 3.8% problematic alcohol use, 7.1% homelessness, 8.8% of a mental health condition and 4.1% had a prison history.
Enhanced case management
During the study period 1287 (52.8%) were triaged by the nursing team to require ECM. Of those who completed treatment 48.8% received ECM, compared to 79.6%, 67.0% and 64.8% and of those who were continuing treatment, died and LTF, respectively (Supplementary Table S2).
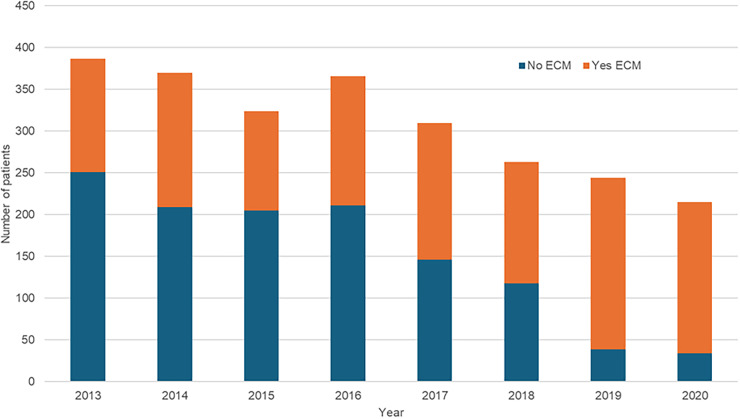
The annual proportion of patients assessed as requiring ECM is shown in Figure 2 and the proportion with assessed ECM levels in Figure 3. Although total numbers of notifications decreased since 2013 from 387 to 215, the proportion of those patients triaged to receive ECM increased from 35% to 84%, with a minority (16%) of patients treated without ECM.
Figure 2.
Notifications to the NCLTBS categorised as not requiring ECM (blue) or needing ECM (orange) between 2013 and 2020.
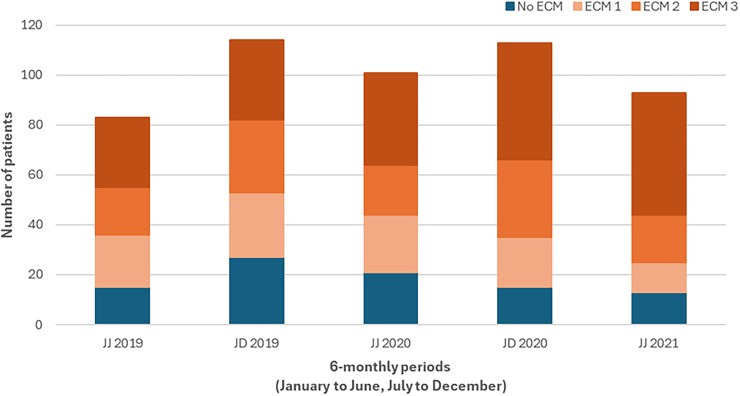
Figure 3.
Notifications to the NCLTBS categorised as not requiring ECM (blue) or needing ECM (orange shading) at levels 1, 2 or 3, between January 2019 and June 2021. JJ = January to June, JD = July to December. Note: Not all patients notified in JJ 2019 were triaged, as this is when 3-level ECM commenced.
Figure 3 shows the proportion of patients triaged to ECM levels since 2019. The proportion triaged to ECM 3 increased over this time from 28% to 53%, with the proportion not triaged to receive ECM falling from 24% to 14%.
Table 2 shows the demographic, clinical and outcome characteristics of those who were assessed as requiring ECM and those who were not. Compared to patients who completed treatment without ECM, a higher proportion of those receiving ECM died (2.9% vs 5.2%, p ≤ 0.001), were LTF (1.7% vs 2.7%, p = 0.02), and continued treatment at 12 months (3.6% vs 12.4%, p ≤ 0.001). This suggests that despite ECM, there is some residual risk in these groups of patients.
Table 2.
Socio-demographic characteristics and outcomes of patients who did and did not receive enhanced case management.
| Category | Variable | ECM | NO ECM | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | Female | 543 | 42.2 | 500 | 43.5 |
| Male | 744 | 57.8 | 650 | 56.5 | |
| Age group | 18–29 | 306 | 23.8 | 327 | 28.4 |
| 30–39 | 250 | 19.4 | 275 | 23.9 | |
| 40–49 | 243 | 18.9 | 217 | 18.9 | |
| 50–59 | 202 | 15.7 | 147 | 12.8 | |
| 60–69 | 124 | 9.6 | 106 | 9.2 | |
| 70+ | 162 | 12.6 | 78 | 6.8 | |
| IMD Quintile | 1 Least deprived | 389 | 30.2 | 292 | 25.4 |
| 2 | 466 | 36.2 | 407 | 35.4 | |
| 3 | 224 | 17.4 | 246 | 21.4 | |
| 4 | 153 | 11.9 | 145 | 12.6 | |
| 5 most deprived | 55 | 4.3 | 60 | 5.2 | |
| Ethnic group | White | 372 | 28.9 | 277 | 24.1 |
| Unknown | 5 | 0.4 | 10 | 0.9 | |
| Black | 457 | 35.5 | 324 | 28.2 | |
| Asian (IPB) | 250 | 19.4 | 343 | 29.8 | |
| Asian (East) | 68 | 5.3 | 71 | 6.2 | |
| Mixed | 15 | 1.2 | 10 | 0.9 | |
| MENA | 66 | 5.1 | 57 | 5.0 | |
| Latin American | 11 | 0.9 | 10 | 0.9 | |
| Other | 43 | 3.3 | 48 | 4.2 | |
| Born UK | No | 987 | 76.7 | 941 | 81.8 |
| Drug use | Yes | 128 | 9.9 | 7 | 0.6 |
| Homelessness | Yes | 167 | 13.0 | 5 | 0.4 |
| Prison | Yes | 96 | 7.5 | 5 | 0.4 |
| Alcohol | Yes | 91 | 7.1 | 2 | 0.2 |
| Mental health | Yes | 196 | 15.2 | 19 | 1.7 |
| Previous TB | Yes | 65 | 5.1 | 39 | 3.4 |
| DOT | Yes | 415 | 32.2 | 12 | 1.0 |
| Inpatient | Yes | 523 | 40.6 | 251 | 21.8 |
| Isoniazid | Resistant | 133 | 10.5 | 34 | 2.9 |
| Rifampicin | Resistant | 31 | 2.4 | 2 | 0.2 |
| Treatment | Completed | 979 | 76.1 | 1027 | 89.3 |
| Died | 67 | 5.2 # | 33 | 2.9 # | |
| LTF | 35 | 2.7* | 19 | 1.7* | |
| CoT | 160 | 12.4 # | 41 | 3.6 # | |
| TO | 27 | 2.1 | 23 | 2.0 | |
| TS | 19 | 1.5 | 7 | 0.6 | |
Asian (IPB): Indian, Pakistani, Bangladeshi; CoT: continuing on treatment at 12 months; DOT: directly observed therapy; ECM: enhanced case management; IMD: index of multiple deprivation; LTF: lost to follow-up; MENA: middle-eastern and north African; TO: transferred out of the TB service; TS: treatment stopped.
* X2 testing: p = 0.02.
X2 testing: p ≤ 0.001.
Table 3 shows the number and proportion of patients with each treatment outcome for each individual risk factor, as well as the total number of risk factors per patient, classified by ECM status. Overall, 363 (14.9%) had at least 1 risk factor recorded. Most patients in each category required ECM (67–79%), with lowest completion rates in those with mental health concerns (67.4%). Two patients with mental health concerns died without receiving ECM and of those with alcohol use issues, 1 died without receiving ECM. In addition, 2 patients with mental health concerns did not receive ECM and were LTF. Eighty-eight percent (217) of 247 patients with 1 social risk factor required ECM and 10% (25) did not. Three from the latter group died (and all were early-on during their first inpatient admission), and 2 were LTF. Only 3 patients with 2 or more risk factors did not require ECM, and all completed treatment. Overall, the majority of patients who needed ECM support received ECM and the great majority successfully completed treatment.
Table 3.
Type and number of social risk factors and outcomes of patients by enhanced case management status.
| Risk factor | ECM status | Completed | Died | LTF | CoT | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Drug use | No | 7 | 5.2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 98 | 72.6 | 3 | 2.2 | 7 | 5.2 | 18 | 13.3 | |
| Homelessness | No | 5 | 2.9 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 136 | 79.1 | 4 | 2.3 | 5 | 2.9 | 18 | 10.5 | |
| Prison | No | 5 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 79 | 78.2 | 1 | 1.0 | 5 | 5.0 | 10 | 9.9 | |
| Alcohol use | No | 1 | 1.1 | 1 | 1.1 | 0 | 0 | 0 | 0 |
| Yes | 72 | 77.4 | 6 | 6.5 | 2 | 2.2 | 11 | 11.8 | |
| Mental health | No | 14 | 6.5 | 2 | 0.9 | 2 | 0.9 | 0 | 0 |
| Yes | 145 | 67.4 | 15 | 7.0 | 5 | 2.3 | 27 | 12.6 | |
| Social risk factors (n) | |||||||||
| 1 | No | 25 | 8.3 | 3 | 1.0 | 2 | 0.7 | 0 | 0 |
| Yes | 217 | 72.3 | 14 | 4.7 | 6 | 2.0 | 25 | 8.3 | |
| 2–3 | No | 3 | 2.3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 98 | 73.7 | 7 | 5.3 | 6 | 4.5 | 17 | 12.8 | |
| 4+ | No | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 20 | 76.9 | 0 | 0 | 1 | 3.8 | 5 | 19.2 | |
CoT: continuing on treatment at 12 months; LTF: lost to follow-up.
The demographic and social characteristics of patients by ECM Categories (no ECM, Categories 1 and 2 combined and Category 3) are shown in Supplementary Table S3. There was little difference between no ECM and ECM 1 and 2, but higher proportions of social risk factors in ECM 3. This also indicates that mortality was concentrated in the ECM 3 group (7.5%, vs 0% for no ECM and 1.9% for ECM 1 and 2 combined), though treatment completion remained high at 73.4%.
Treatment outcomes
Within the whole cohort, we compared factors in patients who completed treatment to those who died, were lost to follow up, and continued treatment past 12 months. Univariate comparisons are presented Supplementary Table S4 and the results of multivariate logistic regression are presented below. Evaluation for collinearity for variables identified none with a correlation factor of >0.7 (although drug use and prison history, and homelessness and prison history were closely associated at 0.67 with mortality as the outcome).
Factors independently associated with a higher risk of death were age over 60 (60–69 years OR 1.9, 95% confidence intervals 1.1–2.8), and 70, OR 3.3 (1.9–4.6), those who were inpatients when diagnosed with TB, OR 4.4 (2.7–6.0), and people with mental health concerns affecting treatment, OR 2.2 (1.0–3.4). People of black ethnicity were less likely to die when compared to people in the white ethnic group, OR 0.6 (0.4–0.9), whereas no association was observed for other ethnic groups. Other socio-economic factors were not identified as having a significant association with mortality.
No factors were identified as having a significant association with being LTF, which is likely to result from the small numbers in this group (n = 54).
Factors associated with increased risk of continuing treatment at 12 months were:
Being an inpatient at diagnosis, OR 2.7 (1.9–3.4)
Isoniazid resistance, OR 3.3 (2.2–4.8)
Rifampicin resistance, OR 1.9 (1.0–3.0)
DOT treatment, OR 1.7 (1.1–2.3)
Extrapulmonary TB as site of disease, OR 1.4 (1.0–1.8)
These factors largely indicate disease severity (inpatient status, complex extra-pulmonary site such as intracranial TB) or resistance (including the provision of DOT for all multi-drug resistant isolates), where longer treatment courses are recommended, and thus duration in this group would not be modified by the provision of ECM. Rifampicin resistance is used here as a proxy for multidrug resistance, as the additional treatment duration is required in rifampicin mono-resistance and is highly correlated with multi-drug resistance. 8 In addition, male patients had a slightly lower risk of longer treatment durations, OR 0.7 (0.5–0.9).
Discussion
This study presents the most comprehensive evaluation of ECM since its implementation in 2013. The total number of patients notified to NCLTBS has decreased over time following the implementation of enhanced screening for persons migrating to the UK, requiring treatment for TB in their country of origin. 9 However, the proportion requiring ECM has climbed, with half of patients assessed as needing additional support. Since ECM was sub-categorised in 2019 into 3 Levels the proportion of people requiring the highest level (ECM 3) has also risen. Currently, only a minority of patients do not receive ECM. The reasons for this are multifactorial and are likely associated with increasing socio-economic risk for non-adherence or poor outcome. However, we cannot discount the effect of the TB nursing team being more aware of the availability of interventions that are associated with ECM status. Future work should explore which supportive interventions are most beneficial (and hence ought to be available) for the majority of patients.
Compared to national data, the total proportion of persons in our cohort was higher for those with at least 1 social risk factor (14.9% vs 12.7%), drug use history (5.5% vs 4.4%) and homelessness (7.1% vs 4.3%). Proportions were similar for harmful alcohol use (3.8% vs 4.5%) and previous imprisonment (4.1% vs 4.0%). 2 There was also a high proportion with mental health issues affecting treatment (8.8%), which was not reported in the national data until 2022. Of TB patients in the highest risk groups only 2 did not receive ECM, both of whom had good TB treatment outcomes, suggesting that patients were being appropriately assessed and triaged. Compared to the overall completion rate (82.3%), those with social risk factors had slightly lower completion rates, but these were similar irrespective of whether they had 1, 2–3, or 4 or more risk factors (72.3%, 73.7% and 76.9%, respectively). However, only small numbers of patients with social risk factors did not receive any ECM interventions, and a very small number did not receive ECM and had a negative outcome: 3 deaths, with death occurring as inpatients shortly after diagnosis), whilst 2 were LTF.
We identified age as a significant factor in poor outcomes. Within the cohort, 1 in 5 patients were aged over 60, however, two-thirds of the deaths were in this group. Of patients 60–70+, 184 did not receive any ECM support, suggesting there may be a role for increasing support to older age groups. The reason that people from black ethnic groups had lower may be because patients from white ethnic backgrounds present later, which may contribute to disease severity. 10 Or it could be related to the higher incidence of new HIV diagnoses in people from black ethnic backgrounds and thus may be screened through HIV services with TB diagnosed early. 11 However, further work is required to further unpick this association.
With the implementation of the 3 tiers of ECM support, a large proportion of patients fall into ECM level 3. Despite this, there remains residual risk of negative outcomes in this group. Given the relatively small difference in care provided between standard care and ECM levels 1 and 2, the current three-tier ECM could be streamlined into a smaller number of categories, allowing TB services to focus on those requiring the highest level of support.
Despite an overall reduction in case numbers, the increasing complexity and higher requirements of ECM have significant resource implications for the TB service. The RCN recommends 1 case manager per 40 notifications requiring SCM, but 1 per 20 patients requiring ECM. 6 However, this does not take into consideration the additional support from administrative staff and allied health professionals. Further work is required to identify the required skill mix to best support the complexity of patients in TB services.
Overall TB outcomes in this cohort were good, with most patients successfully completing therapy. Mortality was 4.1%, compared to 4.9% nationally. 2 Despite the prevalence and impact of social risk factors, none were associated with mortality when comparing patients who completed treatment to those who died in this cohort. Although it is not possible to determine whether this was a result of the additional support provided through the ECM system, or the proportion of deaths attributable to TB in people with and without ECM, it is reassuring data, given the historical evidence of negative outcomes associated with these social risk factors.
Our results are in line with previous research which demonstrated considerable need for ECM. Although there may be differences in categorisation, data published from another regional TB service in England, found 64% patients required ECM with 14% in the ECM3 group. 12 This study also noted there to be a useful discrimination between the three ECM categories, suggesting either differences in the underlying risk factors between different areas of England, or differences in using the ECM categories. However, outcomes were progressively worse with increasing ECM tier, despite the additional support provided. This suggests that the ECM categorisation does not fully mitigate the risks of negative outcome. Work is underway to identify what further interventions may help here. 13
Case management has been widely implemented in TB services, including those in London, and provision of ECM is recommended by the National Institute of Health and Care Excellence and the RCN.6,14 Due to the diffuse and variable nature of this type of intervention there is little evidence showing the benefit of its use. However there is evidence of ECM contributing to reduced LTF rates and improved outcomes in people experiencing homelessness and increased adherence in people who use drugs in low-incidence settings, which is consistent with our findings. 15 As an approach to inclusion health, ECM can provide essential co-ordination across multiple health and social care services for the most marginalised patients. 16 Increasing complexity of individual patients’ circumstances is associated with increased resources required to meet these needs. 17 The trade-off with the risk of poor health outcomes with un- or under-treated TB and further disease spread is important to consider and may support cost-effectiveness, although evidence is lacking. 15 Further research and evaluation are required to determine the most efficient way of providing ECM support.
Limitations
This study is retrospective in design and does not contain a comparison group not receiving ECM for a given set of risk factors. Therefore, it is not possible to determine the true benefit of ECM. Other risk factors may be important for TB outcomes, such as co-morbidities, smoking status, HIV co-infection and under-nutrition, and these were not included in this analysis.
Conclusions
Despite decreasing numbers of notifications to the NCLTBS in recent years, the proportion of patients triaged to receive ECM has increased to 85%. Very few people with social risk factors did not receive ECM support. The increasing level of ECM support required has significant resource implications and should be considered in future TB service planning and funding. Our data suggest that one approach might be to simplify the current 3-tier ECM categorisation.
Supplemental Material
Supplemental material, sj-docx-1-shr-10.1177_20542704241290486 for Providing personalised care for people with tuberculosis: an evaluation of enhanced case management in a UK TB Network 2013 to 2021 by Tim Crocker-Buque, Harry Hayden, Jacqui White, Jennifer Dekoningh, Moerida Belton, Narinder Boparai, James Brown, Mike Brown, Danielle Hawley, Stefan Lozewicz, Rob Miller, Rachel Moores, Karyn Moshal, Jessica Potter, Marc Lipman and in JRSM Open
Acknowledgements
Members of the North Central London Tuberculosis Service, including Ana Garcia Mingo, Anna Turkova, Santino Capocci, Dean Creer, Sarah Eisen, Hanif Esmail, Jacquie Flynn, Philip Gothard, Louis Grandjean, Mike Greenberg, Simon Lee, Ian Moonsie, Dave Moore, Ian Cropley, Stephen Morris-Jones, Mahdad Noursadeghi, Linda Walker, David Dicolen, Melody Eddy, Adriana Fiedler, Grace Parry, Emma Hamilton, Nicola Howell, Shakib Hussein, Jason Walmsley, Jenske Kamarudin, Lusha Kellgren, Peter Mackenzie, Yemi Martins, Meena Middleton, Siji Midhun, Lise Ridge, Ataulhaq San Sanaie, Rebecca Smith Bramley, Trevor Hart, Jacqueline Barrett, Stephen Mepham.
Declarations
Competing interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: This is a retrospective evaluation of routinely collected health services data registered as a quality improvement project at The Royal Free Hospital NHS Foundation Trust, thus ethical approval and individual patient consent was not required nor sought.
Guarantor: Marc Lipman.
Contributorship: Conception and design was done by TCB, ML, JW; data collection was done by TCB, JD; data analysis was done by TCB, ML; analysis and insight generation were done by TCB, ML, JW, JD, HH; drafting and review of the manuscript was done by TCB, HH, JW, JD, ML, MB1, NB, JB, MB2, DH, SL, RM1, RM2, KM, JP.
Provenance: Not commissioned, peer reviewed by Justin Denholm.
odds ratioconfidence intervalD iD: Tim Crocker-Buque https://orcid.org/0000-0003-0059-7735
Supplemental material: Supplemental material for this article is available online.
References
- 1.UK Health Security Agency. Tuberculosis in England: national quarterly reports, https://www.gov.uk/government/statistics/tuberculosis-in-england-national-quarterly-reports (2023, accessed 19 March 2024).
- 2.UK Health Security Agency. Tuberculosis in England, 2022 report (data up to end of 2021), https://www.gov.uk/government/publications/tuberculosis-in-england-2022-report-data-up-to-end-of-2021 (2023, accessed 19 March 2024).
- 3.UK Health Security Agency. Tuberculosis (TB): action plan for England, 2021 to 2026, https://www.gov.uk/government/publications/tuberculosis-tb-action-plan-for-england/tuberculosis-tb-action-plan-for-england-2021-to-2026 (2020, accessed 19 March 2024).
- 4.Anderson C, White J, Abubakar I, et al. Raising standards in UK TB control: introducing cohort review. Thorax 2014;69(2):187–189. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Understanding the TB Cohort Review Process. Division of Tuberculosis Elimination, https://www.cdc.gov/tb/publications/guidestoolkits/cohort/cohort.pdf (2006, accessed 19 March 2024).
- 6.Royal College of Nursing. A case management tool for TB prevention, care and control in the UK. London, UK: Royal College of Nursing, 2022. [Google Scholar]
- 7.McNally G, Solomon D, Morris-Jones S, et al. Does use of a diagnostic certainty score at TB cohort review improve culture confirmation of active tuberculosis? Thorax 2023;78(Suppl 4):A194–A195. [Google Scholar]
- 8.World Health Organisation. Meeting report of the WHO expert consultation on drug-resistant tuberculosis treatment outcome definitions, https://www.who.int/publications-detail-redirect/9789240022195 (2020, accessed 14 March 2024).
- 9.Aldridge RW, Zenner D, White PJ, et al. Tuberculosis in migrants moving from high-incidence to low-incidence countries: a population-based cohort study of 519 955 migrants screened before entry to England, Wales, and Northern Ireland. Lancet 2016;388(10059):2510–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodger A, Jaffar S, Paynter S, Hayward A, Carless J, Maguire H. Delay in the diagnosis of pulmonary tuberculosis, London, 1998-2000: analysis of surveillance data. Br Med J 2003;326(7395):909–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UK Health Security Agency. HIV testing, PrEP, new HIV diagnoses and care outcomes for people accessing HIV services: 2023 report, https://www.gov.uk/government/statistics/hiv-annual-data-tables/hiv-testing-prep-new-hiv-diagnoses-and-care-outcomes-for-people-accessing-hiv-services-2023-report (2024, accessed 24 March 2024).
- 12.Tucker A, Mithoo J, Cleary P, et al. Quantifying the need for enhanced case management for TB patients as part of TB cohort audit in the North West of England: a descriptive study. BMC Public Health 2017;17(1):881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stagg HR, Abubakar I, Campbell CN, et al. IMPACT Study on intervening with a manualised package to achieve treatment adherence in people with tuberculosis: protocol paper for a mixed-methods study, including a pilot randomised controlled trial. BMJ Open 2019;9(12):e032760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute for Health and Care Excellence. Tuberculosis guidance, https://www.nice.org.uk/guidance/ng33/chapter/recommendations#enhanced-case-management (2016, accessed 24 March 2024).
- 15.Heuvelings CC, de Vries SG, Greve PF, et al. Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis 2017;17(5):e144–e158. [DOI] [PubMed] [Google Scholar]
- 16.Luchenski S, Maguire N, Aldridge RW, et al. What works in inclusion health: overview of effective interventions for marginalised and excluded populations. Lancet 2018;391(10117):266–280. [DOI] [PubMed] [Google Scholar]
- 17.Rubado DJ, Choi D, Becker T, Winthrop K, Schafer S. Determining the cost of tuberculosis case management in a low-incidence state. Int J Tuberc Lung Dis 2008;12(3):301–307. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-shr-10.1177_20542704241290486 for Providing personalised care for people with tuberculosis: an evaluation of enhanced case management in a UK TB Network 2013 to 2021 by Tim Crocker-Buque, Harry Hayden, Jacqui White, Jennifer Dekoningh, Moerida Belton, Narinder Boparai, James Brown, Mike Brown, Danielle Hawley, Stefan Lozewicz, Rob Miller, Rachel Moores, Karyn Moshal, Jessica Potter, Marc Lipman and in JRSM Open