Abstract
Background
Precise knowledge of the apical construction, which determines the end of the area for canal preparation and filling, is essential for the success of root canal treatment and the management of postoperative pain. For this purpose, devices based on various methods that determine the working length (WL) are used. However, it is still controversial which method provides the most accurate measurements.
Aim
To investigate the compatibility of the electronic apex locator (EWL) and simultaneous working length determination (SWL) methods in single-root teeth in comparison with the radiographic working length determination (RWL) method and to determine which one produced more effective results in terms of postoperative pain.
Materials & methods
One hundred patients scheduled for root canal treatment (RCT) were randomly assigned to one of the three groups according to the working length measurement method (EWL, SWL or RWL). After WL determination with assigned method, root canals were prepared and then obturated. Age, gender, simplified oral hygiene index (OHI-S), oral and dental examinations and Visual Analogue Scale (VAS) results of all participants were recorded. The incidence and intensity of postoperative pain were rated on a Visual Analogue Scale (VAS) by patients 6, 12, 24, 48 h and 7 days after RCT. The number of analgesic tablets (400 mg Ibuprofen) taken by patients was also recorded. Data were analyzed using the chi-square, One- way ANOVA and Kruskal-Wallis tests. Bland-Altman and Passing-Bablock regression analysis were used as method comparison techniques.
Results
It was determined that the number of patients receiving analgesia and the total number of analgesia doses were higher in EWL and RWL groups compared to SWL group (p < 0.0001). When the WL values at which the treatment was applied were compared in the patient groups; WL values of EWL group were statistically lower than SWL group (p < 0.01). While there was no difference between the preoperative VAS scores of the groups (p = 0.7590), the postoperative 6th and 12th hour VAS scores of SWL group were lower than those of EWL and RWL groups (p = 0.005 and p = 0.0002, respectively). Again, the VAS scores of SWL group at the 24th and 48th postoperative hours were lower than those of RWL group (p < 0.05). According to the Bland-Altman and Passing-Bablock regression analysis results, although there was no statistically significant difference between the EWL and SWL methods (p = 0.471), the bias value of -0.1190 was well below the acceptable total error (0.1648). Additionally, a strong relationship was found between EWL and SWL methods (r = 0.9698, r2 = 0.9406, p < 0.001). Therefore, statistically these two methods were considered compatible with each other. It was determined that there was a statistically significant bias (0.340, p < 0.0001) between the RWL and SWL methods, exceeding the total error.
Conclusions
As a result, it was determined that the SWL method, which is used to determine working length for the success of endodontic treatment, can be used as an alternative to the EWL method thus producing more effective results in the management of postoperative pain. However, in addition to the method used, the technology of the device developed for this method should not be ignored.
Clinical relevance
Precise knowledge of the apical construction, which determines the end of the area for canal preparation and filling, is essential for the success of root canal treatment and the management of postoperative pain. For this purpose, devices based on various methods that determine the working length are used. However, it is still controversial which method provides the most accurate measurements. This study found that the simultaneous working length determination method can be used as an alternative to the electronic working length determination method and produces more effective results in the management of postoperative pain. Another important outcome of this study is that the Total Allowable Error (TEa) for the electronic apex locator method, which is accepted as the reference, has been calculated for the first time. Other methods have been evaluated according to this reference method. This is a first in literature.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-05200-x.
Keywords: Irreversible pulpitis, Root canal treatment, Simultaneous working length determination, Electronic apex locator, Postoperative pain
Introduction
Root canal treatment (RCT) procedures should be confined within the root canal system. The working length (WL) is defined as the distance between a coronal reference point and the apical construction ([AC] or in other words, minor apical foramen). AC represents the histologic point of transition between the pulpal and the periodontal tissue at the cementodentinal junction, and is accepted as the physiological apical limit for ending endodontic instrumentation and obturation [1]. The location of the apical constriction is 0.5 to 1.0 mm short of the radiographic apex [1]. Exceeding the tolerance of 0.5–1.0 mm from the AC and making the root canal filling shorter or longer will either cause the infected and necrotic tissue not to be completely cleaned or the periapical area where healthy vessels and nerves are located will be damaged [2]. However, there are limitations in relying solely on radiographs to determine the working length because of variation in the distance and location of the apical constriction relative to the anatomical and radiographic apex, root curvature, and superimposition of the zygomatic arch in maxillary molars [2]. Therefore, the digital radiograph method, which previously used the radiological working length (RWL) technique, has been replaced by the working length determination with electronic apex locator (EWL) method, which is more widely used today [3]. Devices that apply various methods to determine the root canal working length have been developed. The simultaneous working length (SWL) determination is a newer development that allows clinicians to clean and shape root canals while monitoring the file’s position inside the canal using dynamic feedback from EAL. In this method, an endodontic motor with a built-in EAL provides continuous feedback during root canal instrumentation allowing clinicians to make real-time adjustments to the WL. Thus, it provides continuous feedback, which allows the clinician to make real-time adjustments. The motor of devices using this method has automatic apical reverse and automatic apical stop operation. In this way, when the tip of the file reaches the apical foramen, the file safely reverses and stops rotating. Thereby, SWL method reduces the risk of over- instrumentation [4]. In the light of the above information, the null hypothesis tested in this study is that there is no significant difference between the SWL, the EWL and RWL methods, these methods are equally effective in postoperative pain management.
Materials and methods
Design of working groups
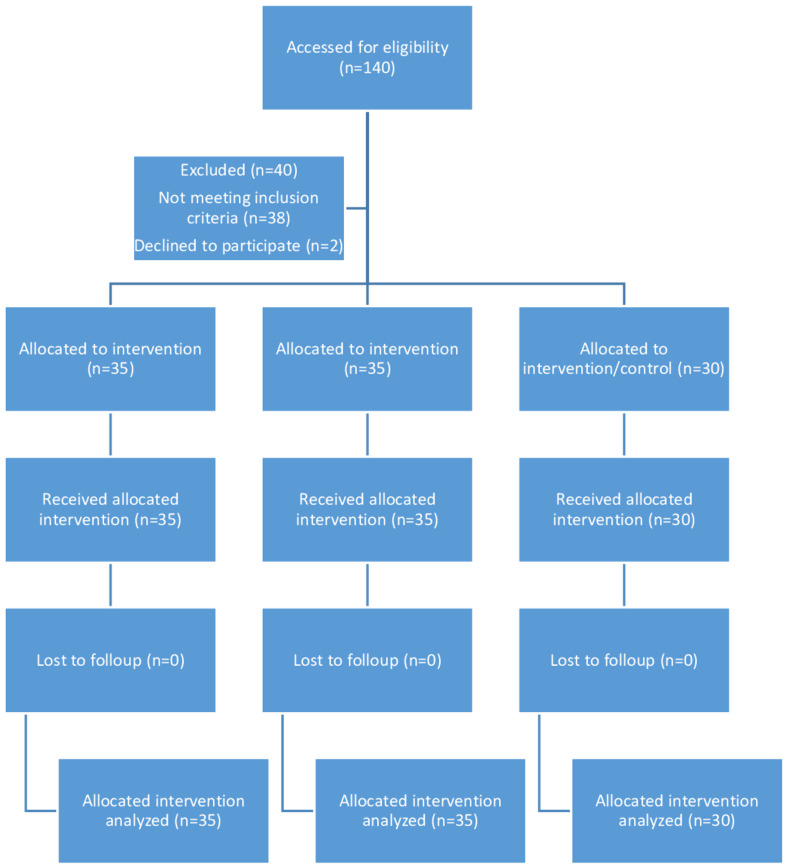
The prospective study included 100 patients aged 18–59 years who applied to the Department of Endodontics of Istanbul Medipol University between June 2022 and January 2023 due to irreversible pulpitis (IP). The study was approved by the Institutional Ethical Committee (E-10840098-202.3.02-3130, 25/05/2022), and written consent was obtained from all participants.
This study has a randomized, single-blind design. Patients participating in the study did not know which method was used. However, the blinding of the endodontist was not possible due to the use of different WL methods.
According to the methods used to determine the WL, 35 patients in whom EWL method was used with the electronic apex locator (Root ZX mini, J. Morita Corp., Tokyo, Japan) were included in EWL group; 35 patients in whom the simultaneous working length (SWL) method (Woodpecker Ai Endo Motor With Apex Locator, Guilin Woodpecker Medical Instrument Co., China) were used were included in SWL group; 30 patients in whom the radiologic working length (RWL) method was used were included in RWL group. The patient groups included in the study groups were randomly selected from people similar in terms of age and gender characteristics.
Demographic characteristics of all participants [age, gender, simplified oral hygiene index-score (OHI-S)], oral and dental examinations [(number of root canal treated teeth (RCT), number of crowns, number of composite/amalgam fillings (DDS), tooth types (maxillary anterior, mandibular anterior or mandibular premolars) and number of missing teeth (NMT) etc.] and Visual Analog Scale (VAS) results were recorded. Similarly, the number of patients using analgesics (NPA) and the total number of analgesic doses administered (TAD) per week were also recorded. Preoperative digital radiographs were taken using paralleling technique under standard exposure conditions. Periapical index (PAI) score was calculated from the radiological images of the patients [5].
Inclusion criteria
Patients between the ages of 18–59.
Patients without systemic disease.
Single-rooted teeth having one canal.
Those with an irreversible pulpitis diagnosis.
Teeth having mature apexes with no radiographic sign of root resorption.
Those with a root canal without severe curvature (< 30°).
Patients who signed an informed consent form were included in the study.
Patients forming all study groups were selected from those with PAI scores of 1–2.
Exclusion criteria
Maxillary premolar teeth.
Mandibular premolars and incisors with two root canals.
Patients who were pregnant, lactating, morbidly obese, had acute or chronic inflammatory disease (large local or generalized infection, cancer, cardiovascular disease and advanced diabetes mellitus) were excluded from the study.
Those who could not show the necessary compliance and were not able to remain inactive for the treatment to be carried out properly, those with mental retardation, advanced age and cooperation disorders were excluded from the study.
In addition, patients with calcified root canals, root resorption, periodontal problems (probing depth > 4 mm), incomplete root development, history of previous endodontic treatment, severely curved roots or excessive coronal destruction on the diagnostic radiograph taken before the procedure were not included.
Patients with radiographically confirmed periapical lesions.
Clinical procedures
The principal investigator (E.G.) performed the entire endodontic procedure on all the patients using a standardized protocol. Rubber dam isolation was used in all the cases, and local anaesthesia (Articaine 4% with 1:200,000 epinephrine, Ultracaine DS Fort, Hoechst-Marion Roussel, Frankfurt, Germany) was administered. A standard access cavity was prepared using sterile diamond and carbide burs. The incisal or occlusal edges were ground lightly to create stable reference points for the rubber stops on the root canal files. Canals were shaped using the ProTaper Universal SX shaper file system (ProTaper Universal; Dentsply Maillefer, Ballaigues, Switzerland), and then irrigated with 2.5% NaOCl solution. Then, patients were randomly assigned into 3 groups according to the WL determination methods: The EWL, SWL and RWL groups.
In the EWL group, the Root ZX mini Electronic Apex Locator (EAL, J Morita Corp, Tokyo, Japan) was used. After coronal flaring, a size #15 K-file attached to the EAL was inserted into the root canal. When the ‘‘APEX’’ was reached, the file was withdrawn until the ‘‘0.5 mm’’ mark. The file was removed from the root canal and the WL was determined. The rubber stop on the file shaft was positioned on the reference point after determining the apical limit. The distance between the instrument’s tip and the rubber stop was measured with a caliper to the nearest 0.01 mm. This procedure was repeated thrice, and the mean of these measurements was considered as the EWL [3]. After the WL was measured with EAL in EWL group, this length was also measured with SWL and RWL methods. However, in the EWL group, root canal preparation was performed based on the length measured according to EAL.
In the SWL group, the working length was determined by using the Ai Motor (WOODPECKER, Guilin, China), according to the manufacturer’s instructions. The file was advanced within the root canal to a point just beyond the major foramen, as indicated by the flashing ‘‘APEX’’ bar on the liquid crystal display. The file was then withdrawn until the liquid crystal display showed a flashing bar ‘‘0.5 mm’’ mark from the apex. Measurements were recorded in the same manner as in the EWL method. After the WL measurement in SWL group, this length was also measured with EWL and RWL methods. However, in the SWL group, root canal preparation was performed based using dynamic feedback from the device.
Radiographic determination was done by measuring the length of the root on radiograph and then subtracting millimeters from this estimate [6]. With a #15 K-file inserted into the canal, a periapical radiograph was taken with a parallel technique (Carestream RVG 5200; Carestream Health Inc, Atlanta, CA, USA). The measurement from the tip of the apex is added to the known length of the file that was in the canal, then another radiograph was taken again to confirm that the end of the file was placed 1 mm short of radiographic apex. This was accepted as RWL. After the WL measurement in RWL group, this length was also measured with EWL and SWL methods. However, in the RWL group, root canal preparation was performed based on the length measured according to RWL.
The canals were shaped at the working length determined for the group to which it was assigned in each group. Root canals were prepared by using the ProTaper Next files (Dentsply-Sirona, Ballaigues, Switzerland). These files were used with a preprogramed endomotor (Xsmart Plus; Dentsply Maillefer, Ballaigues, Switzerland) in EWL and RWL groups. However, the preparation in the SWL group was done using Ai Motor endomotor (WOODPECKER, Guilin, China), which has a built-in apex locator. The mode was set as an auto-apical stop to ensure that there was no over-preparation during instrumentation. Simultaneous length control was provided with SWL method. The canals were apically enlarged to size 40 (X4) at the working length (SX, X1, X2, X3, and X4, respectively). Between each instrument change, the root canal was irrigated with 5 ml of 2.5% NaOCl solution with a 30-gauge side-vented irrigation needle. Hence, a total of 25 ml of the irrigating solution was used. After instrumentation was completed, the smear layer was removed with 2 ml 17% EDTA, which was left in the canal for 3 min. Saline solution was used after to flash the root canals to eliminate the effect of EDTA. The canals were obturated using epoxy resin sealer (AH Plus, Dentsply DeTrey GmbH, Konstanz, Germany) and cold lateral compaction of gutta-percha. Ibuprofen 400 mg was prescribed to the patients, with instructions to use it as a rescue analgesic only in the event of unbearable pain.
Application of visual analog scale for pain
Visual Analogue Scale (VAS) is a valid, subjective measure of acute and chronic pain. It is based on determining the pain level on a numerical line. The basic principle is used to convert some qualitative values that cannot be measured numerically into numerical data. Scores from one end of a line to the other are recorded by making a handwritten mark on a 10 cm line representing the continuum between “no pain” and “worst pain” [7]. In this study, patients were informed about this scale before making the evaluation. It was announced that a VAS would be used to assess pain severity. Patients were asked to describe their pain condition by drawing a line or pointing where it fit on this line. Later, the distance from where there was no pain to where the marking was made was measured. This distance was recorded as the numerical value of the patient’s pain. All participants were asked to repeat the same procedure preoperatively and postoperatively at 6 h, 12 h, 24 h, 48 h and 7 days after RCT.
Statistical analysis
Statistical evaluation of the data obtained from the research was made using SPSS Statistic-Software (IBM Corp., Version 25, Chicago, USA) and MedCalc® Statistical-Software (MedCalc Software Ltd., Version 22.016, Ostend, Belgium) programs. Chi-square (χ2) test was used to examine whether the categorical data of this study were independent in affecting the test statistics. Before further statistical analysis, the Kolmogorov-Smirnov normality test, which tests the assumption of normality, was applied to determine how the data were distributed. In the analysis of parametric and nonparametric data of this study consisting of three groups, One- way ANOVA and Kruskal-Wallis tests were applied. To test whether there was a relationship between the independent variables of the study, Pearson and Spearman correlation tests were used for parametric and nonparametric data, respectively. Bland-Altman and Passing-Bablock regression analysis were used as method comparison techniques to evaluate whether the EWL, SWL and RWL methods used to determine the root canal working length of all participants produced compatible results.
Bland-Altman analysis
It is a statistical technique frequently used to compare two medical methods. With this analysis, it was evaluated how compatible the results of two methods are. By comparing the means of the differences between the measurements of the methods, it was examined whether these differences were within the 95% agreement range. On the graph, the differences were placed on the Y axis and the means of the two methods were placed on the X axis. The fact that the differences were randomly distributed around zero and the mean of the differences was within the range of ± 1.96 standard deviation (s) was accepted as evidence of agreement between the methods [8, 9]. In this study, the agreement of a new method was evaluated by taking the EWL method as a reference.
Total allowable error (TeaTEa) calculation for working length
In terms of patient safety, it is recommended that the total error of the measurement should not exceed the total allowable error (TeTEaa). The total error is the sum of systematic and random errors made during measurement. Below is the Westgard formula for calculating TEa [10]. The value of Ƶ is 1.65 with a 95% probability (one-sided).
 |
To determine the bias%, the EWL method was chosen as the standard method in endodontic treatment today, and the average WL value of group 1 patients was determined as the target value. The mean WL value of group 2 patients with the new method (SWL) was subtracted from the mean WL value of group 1 patients (measured by the EWL method), which represents the target value, and divided by the target value [bias% = 100 × (20.7–22.3) / 20.7)]. As a result, bias% was found to be 7.7%.
To determine the coefficients of variation (CV)%, WL values of the same patient were measured using the EWL method at 20 different times during the day. The mean (Mean) and standard deviation (SD) of these 20 WL values were calculated (19.87 ± 1.0574). The following formula was used for CV%.
 |
 |
Power analysis and randomization
To determine the minimum number of subjects, in the priori-power analysis (G*Power-Version 3.1, Düsseldorf, Germany) based on the data of a study [11] comparing the pain levels of patients undergoing root canal retreatment, at least 15 subjects were included for each patient group of this study (subjects) was calculated as required (effect size d = 1.11, α = 0.05, power = 0.90). However, in order to reach a stronger prediction and since the minimum number of samples should be ≥ 30 in parametric statistical analyses, it was planned to consist of 30 cases for the control and 35 cases for the experimental groups of this independent study.
The randomization process of the patients participating in the study into groups was carried out by two endodontists (M.U. and S.E.) working in the unit where the research was conducted. Patients who met the inclusion criteria were randomly assigned to one of 3 groups. Additionally, patients requiring RCT for more than one tooth were randomly assigned to groups to ensure objectivity and maintain equal sample size.
Results
Comparison of demographic and clinical characteristics
Demographic data of the study groups are shown in Table 1. The mean ages of patients were 35.3 ± 9.8 (18–53), 35.8 ± 11.9 (18–53) and 35.8 ± 10.9 (18–56) years, respectively for EWL (M/F: 15/20), SWL (M/F: 16/19), and RWL (M/F: 16/14) groups. The mean body mass index (BMI) values were 26.7 ± 3.8 (21–35), 27.1 ± 3.8 (20–34) and 26.3 ± 4.7 (19–36) kg/m2, respectively for EWL, SWL and RWL groups. There were no differences between groups in terms of gender, age and BMI (p = 0.6880, p = 0.9747 and p = 0.7586, respectively). Therefore, the differences detected between the groups in terms of the variables investigated were considered to be independent of these demographic characteristics.
Table 1.
Comparison of data on demographic characteristics of study groups
| EWL | SWL | RWL | p value | |
|---|---|---|---|---|
| n, | 35 | 35 | 30 | - |
| Gender, Male (%) | 15(43%) | 16(46%) | 16(53%) | C 0.6880 |
| Age, year | 35.3 ± 9.8 | 35.8 ± 11.9 | 35.8 ± 10.9 | B 0.9747 |
| BMI, kg/m2 | 26.7 ± 3.8 | 27.1 ± 3.8 | 26.3 ± 4.7 | B 0.7586 |
B One-way ANOVA with post-test (Tukey Kramer Multiple-Comparisons Test), C Pearson Chi-Square test. Statistical significance level = p < 0.05. Parametric data are given as mean ± standard deviation. EWL: working length determination with EAL method, SWL: Simultaneous working length determination, RWL: Radiographic working length, BMI: Body mass index
Comparison of clinical and examination findings
The clinical and examination findings of the study groups are given in Table 2. There was no statistically significant difference between groups in terms of PAI and tooth type (p > 0.05). Similarly, there was no statistically significant difference between the groups in terms of OHI-S score, tooth types, number of crowns, number of root canal treated teeth, number of filled teeth and number of missing teeth (p > 0.05). Therefore, it shows that the groups are homogeneous in terms of OHI-S, PAI, tooth type, number of crowned teeth, filled teeth, root canal treated teeth and missing teeth. This indicates that pain-related evaluations between groups will be independent of the influence of these variables.
Table 2.
Comparison of clinical and dental examination data of study groups
| EWL | SWL | RWL | p value | |
|---|---|---|---|---|
| n, | 35 | 35 | 30 | - |
| OHI-S |
3.2 ± 1.8 2.8(0.8–6.3) |
3.2 ± 1.6 3.5(0.8-6.0) |
3.2 ± 1.5 2.9(0.8–6.9) |
a 0.9676 |
| PAI |
2 ± 1 2(1–2) |
2 ± 1 2(1–2) |
1 ± 1 1(1–2) |
c 0.6880 |
| MaxA/ManA/ManPre, n | 9/16/10 | 17/7/11 | 11/7/12 | C 0.1060 |
| Number of dental crown, n |
1.8 ± 2.0 1.0(0.0–7.0) |
2.4 ± 4.6 0.0(0.0–16.0) |
2.1 ± 2.6 1.5(0.0–12.0) |
A 0.3130 |
| RCF, n |
1.8 ± 2.0 1.0(0.0–9.0) |
4.1 ± 3.1 4.0(0.0–11.0) |
4.2 ± 3.7 3.0(0.0–17.0) |
B 0.8559 |
| NF, n |
2.7 ± 2.1 2.0(0.0–7.0) |
2.6 ± 1.6 3.0(0.0–6.0) |
2.7 ± 1.8 3.0(0.0–8.0) |
B 0.9760 |
| MT, n |
6 ± 6 4(0–15) |
6 ± 6 4(0–20) |
4 ± 4 3(0–13) |
B 0.1957 |
| PRA, n(%) | 29(83%) | 17(49%) | 29(%97%) | A<0.0001 |
| Intergroup p | < 0.01, > 0.05, < 0.001 | |||
| TADS, week |
1.1 ± 0.7 0(2 − 1) |
0.5 ± 0.7 0(3 − 0) |
1.4 ± 0.6 0(2 − 1) |
A<0.0001 |
| Intergroup p | < 0.01, > 0.05, 0.001 | |||
| Working length, mm | 20.7 ± 1.7 | 22.3 ± 2.5 | 21.2 ± 2.5 | B 0.0095 |
| Intergroup p | < 0.01, > 0.05, > 0.05 | |||
A Kruskal-Wallis Test (Nonparametric ANOVA) with post-test (Dunn’s Multiple-Comparisons Test), B One-way ANOVA with post-test (Tukey Kramer Multiple-Comparisons Test), C Pearson Chi-Square test. Statistical significance level = p < 0.05. When p values obtained by ANOVA tests are < 0.05, p values are determined by making comparisons between groups (Group 1–2, Group 1–3 and Group 2–3, respectively). Parametric data are given as mean ± standard deviation. MaxA/ManA/ManPre: Maxillary anterior /mandibular anterior / Mandibular premolars, EWL: working length determination with EAL method, SWL: Simultaneous working length determination, RWL: Radiographic working length, OHI-S: Simplified oral hygiene index, PAI: Periapical index score, RCT: Root canal treatment, NF: Number of filling, MT: Missing teeth, PRA: Number of patients receiving analgesia, TADS: Total number of analgesics dose per week
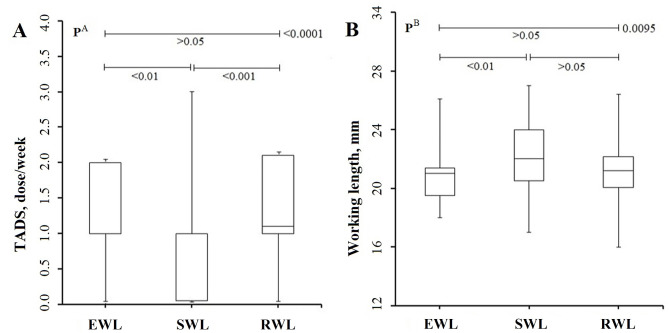
The number of patients receiving analgesia in the study groups and the working length values measured by three different methods are given in Table 2. It was determined that the number of patients receiving analgesia was statistically higher in EWL and RWL groups compared to SWL group (p < 0.0001). The total number of analgesic doses (TADS) administered to EWL and RWL groups’ patients was also higher compared to SWL group (p < 0.0001) (Fig. 1a). When the WL values of the patient groups created according to the WL methods in which endodontic treatment is applied are examined; While the WL values of RWL group were not statistically different from the WL values of both EWL and SWL groups (p > 0.05), the WL values of EWL group were statistically lower than those of SWL group (p < 0.01) (Fig. 1b).
Fig. 1.
Boxplot showing (A) total number of analgesia doses administered (TADS) and (B) working length (WL) data of the study groups according to the method in which endodontic treatment was applied. It appears that the total number of analgesia doses administered to EWL and RWL patients was higher compared to SWL. While there is no difference between the other groups, the WL values of EWL are statistically lower than group 2. A Kruskal-Wallis Test (Nonparametric ANOVA), B One-way ANOVA Test
Comparison of SWL method with EWL and RWL methods
When the measurements of all patients taken with all three methods were examined, there was no statistical difference between the EWL, SWL and RWL methods in terms of WL values (p = 0.3386) (Table 3).
Table 3.
Comparison of WL values of all patients measured according to working length (WL) determination methods
| EWL | SWL | RWL | p value | |
|---|---|---|---|---|
| n, | 100 | 100 | 100 | - |
| Working length, mm |
21.3 ± 2.3 21.0(16.0–27.0) |
21.5 ± 2.3 21.3(15.0–27.0) |
21.8 ± 2.3 21.6(16.0–27.0) |
B 0.3386 |
B One-way ANOVA. Data are presented as mean ± standard deviation and median (min-max). EWL: working length determination with EAL method, SWL: Simultaneous working length determination, RWL: Radiographic working length
There was no statistical difference between the WL values determined by EWL and SWL methods (mean difference = 0.1190, 95% CI = -0.5207 and 0.7587, p = 0.7141), and a strong relationship was found between the two methods (Correlation coefficient (r) = 0.9698, r2 = 0.9406).
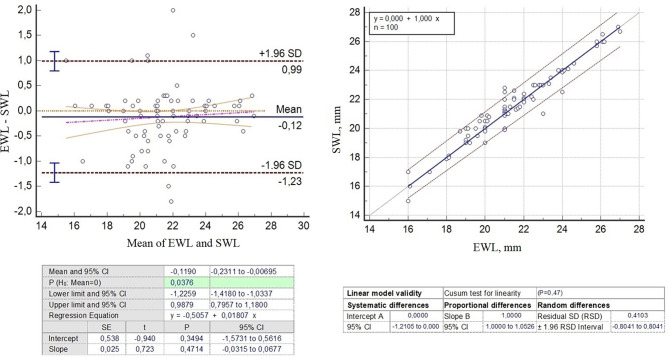
According to the Bland-Altman graph and Passing-Bablock regression analysis results of the EWL and SWL methods, although the model comparing these two methods was not found to be statistically different (the methods were found to be compatible) (p = 0.471), a bias (systematic or proportional) was found to be -0.1190 [95% CI: (-0.2311) - (-0.0069)] value was found to be statistically significant compared to 0 value (p = 0.0376) (Fig. 2). However, since the acceptable total error value (TEa = 0.1648) was taken as the tolerance value, the bias value found was smaller than TEa. Therefore, these two methods were found to be statistically compatible with each other.
Fig. 2.
Bland-Altman and passing-bablock regression plot showing WL data of EWL and SWL groups. Although there was no statistically significant difference between the two methods, the bias value of -0.1190 was statistically significant (p = 0.0376). However, this value was smaller than the acceptable total error value (TEa = 0.1648). Therefore, these two methods were found to be statistically compatible with each other
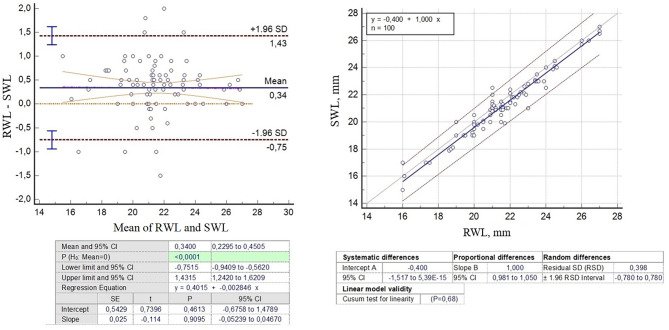
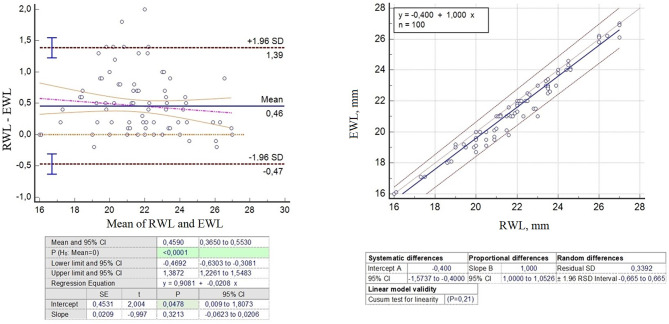
According to the Bland-Altman and Passing-Bablock regression analysis results of the RWL and SWL methods, although the model comparing the two methods was not statistically different (p = 0.681), the bias was found [0.340 (95% CI: 0.2295–0.4505), p < 0.0001] statistically significant and greater than TEa (Fig. 3). Similarly, according to the analysis results of the RWL and EWL methods, the model comparing the two methods was not found to be statistically different (p = 0.210), the bias was found to be statistically significant [0.459 (95% CI: 0.3650–0.5530), p < 0. 0001] and this bias value was above TEa (Fig. 4). Therefore, the RWL method was not fully compatible with both the EWL and SWL methods.
Fig. 3.
Bland-Altman and passing regression graph showing WL data of RWL and SWL groups. Although there was no statistically significant difference between the two methods, the bias value of 0.340 was statistically significant (p < 0.0001) and this value was larger than the acceptable total error value (TEa = 0.1648). Therefore, these two methods were not statistically compatible with each other
Fig. 4.
Bland-Altman and passing regression plot showing WL data of groups of EWL and RWL groups. Although there was no statistically significant difference between the two methods, the bias value of 0.4590 was statistically significant (p < 0.0001) and this value was larger than the acceptable total error value (TEa = 0.1648). Therefore, these two methods were not statistically compatible with each other
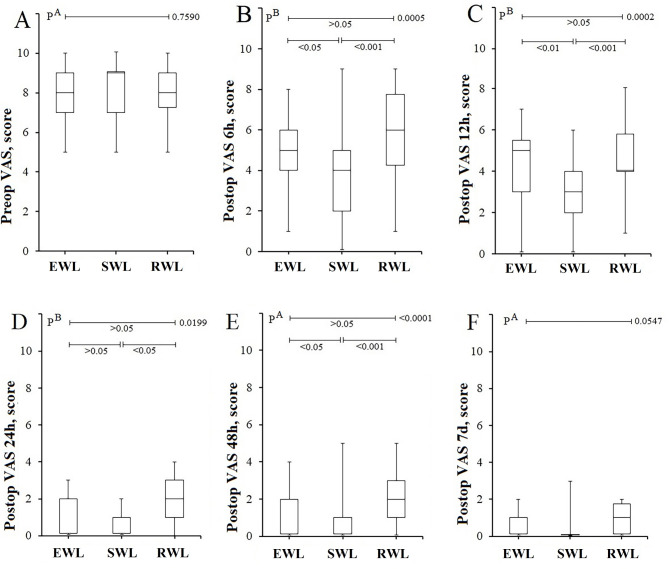
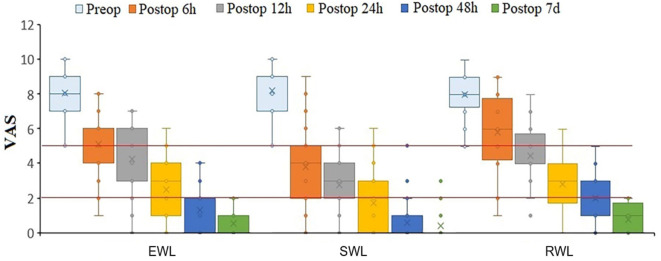
VAS scores of the groups are given in Table 4. There was no statistical difference between the VAS scores of the groups in the preoperative period (p = 0.7598). When the VAS scores of the groups at the 6th and 12th hours postoperatively were examined; while there was no statistical difference between EWL and RWL groups (p > 0.05), the VAS scores of SWL group were found to be lower than EWL and RWL groups (p < 0.05 and p < 0.05, respectively) (Fig. 5A-C). At the 24th postoperative hour, the VAS scores showed no difference between the groups. However, the VAS scores of SWL group were lower than the VAS scores of RWL group (p < 0.05) (Fig. 5D). Similarly, at the 48th postoperative hour, SWL exhibited lower VAS scores compared to both EWL and RWL groups (p < 0.05 and p < 0.001, respectively) (Fig. 5E). On the postoperative day 7, no significant difference was observed between the groups (p = 0.0547) (Fig. 5F). Over time, a more rapid decrease in VAS values was observed in EWL group (Fig. 6).
Table 4.
Comparison of the number of patients receiving analgesia and working length (WL) values measured by three different methods in the study groups
| EWL | SWL | RWL | p value | |
|---|---|---|---|---|
| n, | 35 | 35 | 30 | - |
| Preop VAS, score |
8.1 ± 1.3 8(5–10) |
8.2 ± 1.4 9(5–10) |
8.0 ± 1.2 8(5–10) |
A 0.7598 |
| Postop VAS 6 h, score |
5.1 ± 1.6 5(1–8) |
3.8 ± 2.4 4(0–9) |
5.8 ± 2.1 6(1–9) |
B 0.0005 |
| Intergroup p | < 0.05, > 0.05, < 0.001 | |||
| Postop VAS 12 h, score |
4.3 ± 1.8 5(0–7) |
2.8 ± 1.7 3(0–6) |
4.5 ± 1.8 4(1–8) |
B 0.0002 |
| Intergroup p | < 0.01, > 0.05, < 0.001 | |||
| Postop VAS 24 h, score |
2.5 ± 1.7 3(0–6) |
1.7 ± 1.6 2(0–6) |
2.8 ± 1.6 3(0–6) |
B 0.0199 |
| > 0.05, > 0.05, < 0.05 | ||||
| Postop VAS 48 h, score |
1.3 ± 1.2 2(0–4) |
0.6 ± 1.1 0(0–5) |
2.0 ± 1.2 0(5 − 2) |
A <0.0001 |
| Intergroup p | < 0.05, > 0.05, < 0.001 | |||
| Postop VAS 7 day, score |
0.5 ± 0.7 0(0–2) |
0.4 ± 0.8 0(0–3) |
0.8 ± 0.8 1(0–2) |
A 0.0547 |
A Kruskal-Wallis Test (Nonparametric ANOVA) with post-test (Dunn’s Multiple-Comparisons Test), B One-way ANOVA with post-test (Tukey Kramer Multiple-Comparisons Test), C Pearson Chi-Square test. Statistical significance level = p < 0.05. When p values obtained by ANOVA tests are < 0.05, p values are determined by making comparisons between groups (Group 1–2, Group 1–3 and Group 2–3, respectively). Parametric data are given as mean ± standard deviation. VAS scores are given as mean ± standard deviation and median (min-max). EWL: working length determination with EAL method, SWL: Simultaneous working length determination, RWL: Radiographic working length
Fig. 5.
Boxplot plot showing the VAS score values of the study groups (A) preop, (B) postop 6th hour, (C) postop 12th hour, (D) postop 24th hour, (E) postop 48th hour and (F) postop 7th day. When the VAS scores of the groups are examined at the 6th and 12th hours postoperatively, it is seen that there is no statistical difference between EWL and RWL, while the VAS scores of SWL are lower than those of EWL and RWL. It is seen that the VAS scores of SWL are lower than RWL at the 24th postoperative hour. It is seen that the VAS score of SWL is lower than both EWL and RWL at the 48th postoperative hour. A Kruskal-Wallis Test (Nonparametric ANOVA), B One-way ANOVA Test
Fig. 6.
When the VAS scores of the groups are examined over time, it is observed that the VAS values of SWL show a faster decrease
According to the correlation analysis results, there was no statistically significant correlation between WL values and preoperative VAS score and OHI-S score (r < 0.200 and p > 0.05). Similarly, there was no significant correlation between postoperative VAS scores and WL and OHI-S values (r < 0.200 and p > 0.05).
Discussion
The correct determination of the WL is a key factor for successful RCT, because it reduces the possibility of insufficient debridement of the canal or damage to the periapical tissues due to over-instrumentation [12]. Due to the pivotal role of WL determination in root canal therapy, several methods have been used as follows tactile sensation, radiography, EAL, the simultaneous working length control [13]. Although there are many studies in the literature on the factors affecting the success of endodontic treatments and WL measurement techniques and current devices, there is still a need for studies that accurately analyze WL methods and reveal alternative techniques today [3, 14–17]. In this study, we discussed alternative methods that provide the most effective WL measurement, which is critical to the success of root canal treatment, and the importance of WL in postoperative pain management.
In the present study, WL was measured by three different methods, namely EWL, SWL and RWL, and the effect of these systems on the postoperative pain level was evaluated clinically. Since pain is a subjective concept encountered by every individual, the most important problem in studies on this subject is to convert and evaluate quantitative data due to the qualitative feature of pain. Various scales are employed in the assessment of pain, including verbal rating scale, visual analog scale (VAS), numerical rating scales, facial expression scale [17]. In the context of our study, the VAS descriptive scale was selected due to its ease of application and its ability to provide a visual indicator. This scale was utilized for the measurement and ongoing monitoring of pain intensity. In our data set consisting of three groups, there was no difference between the groups in terms of VAS scores in the preoperative period, which created a good basis for testing the effectiveness of the WL method used in the endodontic treatment approach. Preoperative pain levels were similar in all three methods. In the postoperative period, differences in pain management were observed according to the effectiveness of the method. In general, there was a decrease in pain levels in the postoperative period compared to the preoperative period. The most significant reduction in pain at the 6th and 12th hours after RCT was observed in SWL patients compared to the other groups. A similar picture was also seen at 24 and 48 h after RCT. This shows that the SWL method is more successful than others in pain management in the short and medium term. The homogeneity of all groups in terms of demographic and clinical characteristics defined in the Materials and methods section shows that the effect of SWL application on pain management is independent of other factors. Moreover, the fact that fewer patients SWL group required analgesia and received lower doses of analgesia supported this finding. Similarly, in a randomized controlled study conducted by Arslan et al. [18], they reported that the SWL technique during root canal preparation, as a non-pharmacological strategy to reduce postoperative pain, is useful in preventing postoperative pain, which is parallel to our study. Superiority of SWL method in postoperative pain management can be explained by use of electronic apex integrated endodontic motor, which allows simultaneous length control during instrumentation. An interesting property of this motor is that when an instrument reaches the working length, the motor automatically stops the instrumentation. Thus, it can be concluded that automatically stopping instrumentation when the instrument reaches the working length would decrease postoperative pain compared with manually controlling the working length by using stoppers during instrumentation (separate length determination and root canal preparation) [18].
The SX file used in this study was preferred for widening the coronal part and optimizing the root canal entrance during root canal shaping. This file is used especially for widening the coronal third and providing easier access to the apical part of the root canal. In addition, this widening process facilitates accurate measurement of the working length, ensuring complete cleaning and shaping of the root canal during treatment [19]. Standardization was achieved by using the SX file in all study groups.
Today, determining the working length in endodontic treatment with correct techniques is seen as the key element in the success of the treatment and new methods are being developed for this purpose [20]. Investigating the incidence of endodontic flare up and related factors in root canal treatment cases, Iqbal et al. [21] reported that incorrect WL detection may lead to flare up and secondary root canal treatment. A longer WL may cause unpredictable periapical instrumentation and debris being pushed into the periapical tissues, resulting in recurrent and exacerbated infections [21, 22]. For this reason, the WL must be determined with correct techniques. Although various methods have been developed today to determine WL, the real question here is which method, and which technological device is more suitable. This is a critical decision point for us endodontists. Therefore, current methods measuring WL should be known and the most appropriate method should be decided by evaluating these methods by applying correct analytical processes and test statistics. Method comparison analyzes used in this study, which we conducted to find an answer to this problem, showed that EWL and SWL methods can be alternatives to each other within acceptable error limits. However, the SWL technique was found to be more successful in pain management. For this reason, we recommend using the SWL technique as the first option. In addition, in this study, based on EWL data, TEa% (16.48%) was determined for the first time to be used in the evaluation of devices and methods to be used in determining working length. This is an important contribution to literature.
According to the Bland-Altman and Passing-Bablock regression analysis results of this study, the model comparing the EWL and SWL methods was found to be statistically compatible, and the bias (systematic or proportional) detected between the measurements made with these two methods remained within the allowable total error limit. It was evaluated as evidence that they made equivalent measurements and could be used as alternatives instead of each other. However, since the high bias values detected between the RWL method and the EWL and SWL methods, respectively, were above the acceptable total error. It was decided that the RWL method could not be used as an alternative to the other two methods. The minor apical foramen is the border line between the dental pulp and the periodontal area, approximately 0.5–1 mm from the anatomical apex [23]. For this reason, some sources accept a 0.5 mm error in finding the apex within the tolerance limit [24, 25]. Therefore, there is a possibility that the RWL technique, especially measured by radiological method, may exceed the tolerance limits. This can be explained by the variations in root canal anatomy and the consequential high variance of average values that are used to define the distance between anatomical apex and apical constriction [26]. The frequency of laterally located foramina can lead to misinterpretation of radiographic working length and result in unintentional overinstrumentation [27]. A further disadvantage of radiographs is their two-dimensionality. Superimposition of anatomical structures can require retakes of endodontic radiographs [27].
Correlation is often incorrectly used in method studies as part of the evaluation of whether two measurements agree. Because if one of the methods incorrectly overestimates all measurements by a certain amount, the correlation coefficient may indicate a strong relationship without detecting this consistent disagreement. In this case, it is not correct to say that the two measurements agree well [9, 10]. However, regression is closely linked to correlation and provides complementary information. In addition to the strength of the relationship (Pearson correlation coefficient (r) and r2 are calculated), it also gives the a and b values that provide the best bisector approximation of the relationship between Y and X. In this study, we used Bland-Altman and Passing-Bablock regression analyzes to make an accurate evaluation in method comparison.
Sharma and Arora [28] reported that the electronic method was a more accurate method than the radiographic method in determining the working length of the root canal finding significant differences between the radiographic method and the electronic apex locator method, which coincided with the incompatibility and high bias we detected between the EWL and the RWL methods. Therefore, these researchers confirm our conclusion that these two methods are not compatible with each other and cannot be used as alternatives to each other. The difference of our study is that in method comparisons, bias is compared with the total allowable error and creates a definitive judgment.
Endodontic treatment results attract great attention in dentistry. The aim of evaluating these results is to acquire the right skills and improve judgment ability. The main rule in the correct evaluation of endodontic success is the correct selection of the criteria that form the basis of success. Differences in postoperative pain levels in endodontic research are attributed to researchers using different criteria and making different radiographic and clinical evaluations [17, 24]. Therefore, in this study, in order to evaluate the postoperative pain after endodontic treatment depending on the working length in patients with irreversible pulpitis, sampling was made as appropriate as possible and basic criteria were determined at the beginning. Thus, factors that would affect the study were determined and blinding was ensured. As a matter of fact, the consistency between the groups’ results regarding VAS, analgesia application and working length was the best reflection of this.
Since pulp tissue located in the pulp chamber is inflamed due to caries, trauma or other reasons in irreversible pulpitis, severe spontaneous pain and clear pain reaction to warmth and cold stimuli, often, sharp to dull throbbing pain signs are usually present [29, 30]. If left untreated, an apical periodontitis may form in the tooth, periapical tissues may be damaged, or tooth loss may result. For this reason, studies that describe possible complications, focus on new endodontic developments regarding canal preparation, and determine the factors affecting treatment success have begun to increase. For a successful root canal treatment, it is necessary to know the root canal structure and morphology accurately [31]. This obligation requires the correct determination of the working length. To meet this requirement, in our study, in addition to the WL determined by the selected method as the basis for treatment in randomly formed groups, the WL values of all patients were measured with other methods. These values created an important data pool to be used in method comparison. Therefore, the results obtained provided strong analytical support for method comparisons.
Limitations of the study
First of all, since this research is an analytical prospective study, although the cause-effect relationship is stronger compared to other studies, the study findings can be supported with a larger sample size (Fig. 7). Even though no statistical difference was detected between the patient group and the control group in terms of age and gender, different biological and metabolic effects may have an impact on the pain stimulus and pain perception. Due to financial limitations, inflammatory and anti-inflammatory biomarkers such as prostaglandin E2, TNF-α, IL-6 and IL-10, which may be related to the severity of pain and pulpitis, were not evaluated.
Fig. 7.
Consort flow chart
Conclusions
As a result, it was determined that the SWL technique, which is used to determine working length for the success of endodontic treatment, can be used as an alternative to the EWL method and produces more effective results in the management of postoperative pain. However, in addition to the method used, the technology of the device developed for this method should not be ignored.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- EAL
Electronic apex locator
- RCT
Root canal treatment
- WL
Working length
- AC
Apical construction
- RWL
Radiological working length
- EWL
Working length determination with electronic apex locator
- SWL
Simultaneous working length determination
- OHI-S
Simplified oral hygiene index
- VAS
Visual Analogue Scale
- DDS
Number of composite/amalgam fillings
- NMT
Number of missing teeth
- BMI
Body mass index
- PRA
Number of patients receiving analgesia
- TAD
Total number of analgesics dose per week
- PAI
Periapical index score
- TEa
Total Allowable Error
- CV
Coefficients of variation
- r
Pearson correlation coefficient
Author contributions
EG, SE, MU: Conception, design, acquisition, analysis and interpretation of the data, write the manuscript. EG, SE, FO, MU: Design, revised the manuscript. MU, MG: Conception, design. MU, MG: Interpretation of the data, revision. EG, SE, MU: Data collection. FO: Analysis of the data.
Funding
Self-funded.
Data availability
All data generated or analyzed during this study are specific to this study and were not obtained from any other study.Code availability: All data generated or analyzed during this study are specific to this study and were not obtained from any other study.This data will be shared upon a reasonable request from corresponding author.
Declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of Istanbul Medipol University (with a serial number of E-10840098-202.3.02-3130, 25/05/2022 dated). This trial was retrospectively registered in www.clinicaltrials.gov and the registration number is NCT06507982 (18/07/2024). All patients were informed about the study and written consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mancini M, Felici R, Conte G, Costantini M, Cianconi L. Accuracy of three electronic apex locators in anterior and posterior teeth: an ex vivo study. J Endod. 2011;37:684–87. [DOI] [PubMed] [Google Scholar]
- 2.Gordon M, Chandler N. Electronic apex locators. Int Endod J. 2004;37:425–37. [DOI] [PubMed] [Google Scholar]
- 3.Kara Tuncer A, Gerek M. Effect of working length measurement by electronic apex locator or digital radiography on postoperative pain: a randomized clinical trial. J Endod. 2014;40(1):38–41. [DOI] [PubMed] [Google Scholar]
- 4.Klemz AA, Cruz ATG, Piasecki L, Carneiro E, Westphalen VPD, da Silva Neto UX. Accuracy of electronic apical functions of a new integrated motor compared to the visual control of the working length—an ex vivo study. Clin Oral Investig. 2021;25:231–6. [DOI] [PubMed] [Google Scholar]
- 5.Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20–34. [DOI] [PubMed] [Google Scholar]
- 6.Ingle JI, Bakland LK, Endodontics. 5th ed. Hamilton, Ontario, Canada: B. C. Decker Elsevier; 2002.
- 7.Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, et al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2(3):e088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hollis S. Analysis of method comparison studies. Ann Clin Biochem. 1996;33:1–4. [DOI] [PubMed] [Google Scholar]
- 9.Mansournia MA, Waters R, Nazemipour M, Bland M, Altman DG. Bland-Altman methods for comparing methods of measurement and response to criticisms. Glob Epidemiol. 2020;3:100045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Westgard JO, Carey RN, Wold S. Criteria for judging precision and accuracy in method development and evaluation. Clin Chem. 1974;20:825–33. [PubMed] [Google Scholar]
- 11.Cimilli H, Karacaylı U, Şişman N, Kartal N, Mumcu G. Comparison of the oral health-related quality of life and dental pain in symptomatic irreversible pulpitis and pericoronitis. J Dent Sci. 2012;7:250–60. [Google Scholar]
- 12.Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature: part 2—influence of clinical factors. Int Endod J. 2008;41:6–31. [DOI] [PubMed] [Google Scholar]
- 13.Shanmugaraj M, Nivedha R, Mathan R, Balagopal S. Evaluation of working length determination methods: an in vivo / ex vivo study. Indian J Dent Res. 2007;18:60–2. [DOI] [PubMed] [Google Scholar]
- 14.Kim E, Marmo M, Lee C-Y, Oh N-S, Kim I-K. An in vivo comparison of working length. determination by only. root-ZX apex locator versus combining root-ZX apex locator with radiographs using a new impression technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:79–83. [DOI] [PubMed]
- 15.Ravanshad S, Adl A, Anvar J. Effect of working length measurement by electronic apex locator or radiography on the adequacy of final working length: a randomized clinical trial. J Endod. 2010;11:1753–6. [DOI] [PubMed] [Google Scholar]
- 16.ElAyouti A, Dima E, Ohmer J, Sperl K, von Ohle C. Consistency of apex locator function: a clinical study. J Endod. 2009;35:179–81. [DOI] [PubMed] [Google Scholar]
- 17.Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125:143–57. [DOI] [PubMed] [Google Scholar]
- 18.Arslan H, Güven Y, Karataş E, Doğanay E. Effect of the simultaneous working length control during root canal preparation on postoperative pain. J Endod. 2017;43(9):1422–7. [DOI] [PubMed] [Google Scholar]
- 19.Morgental RD, Vier-Pelisser FV, Luisi SB, Cogo DM, Kopper PMP. Preflaring effects on the accuracy of three electronic apex locators. Revista Odonto Ciencia. 2011;26:331–5. [Google Scholar]
- 20.Jeger FB, Janner SF, Bornstein MM, Lussi A. Endodontic working length measurement with preexisting cone-beam computed tomography scanning: a prospective, controlled clinical study. J Endod. 2012;38(7):884–8. [DOI] [PubMed] [Google Scholar]
- 21.Iqbal M, Kurtz E, Kohli M. Incidence and factors related to flare-ups in a graduate endodontic programme. Int Endod J. 2009;42:99–104. [DOI] [PubMed] [Google Scholar]
- 22.Siqueira JF, Barnett F. Interappointment pain: mechanisms, diagnosis, and treatment. Endod Top. 2004;7:93–109. [Google Scholar]
- 23.Mancini M, Felici R, Conte G, Costantini M, Cianconi L. Accuracy of three electronic apex locators in anterior and posterior teeth: an ex vivo study. J Endod. 2011;37:684–7. [DOI] [PubMed] [Google Scholar]
- 24.Saha B, Alam S, Lyngdoh D, Mishra SK. Comparative evaluation of digital radiography, electronic apex locator and simultaneous working length determination on postoperative pain after root canal treatment: a randomized clinical trial. Eur Oral Res. 2024;58(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Unsal Peker B, Erdem Hepşenoğlu Y, Ersahan S, Eyüboğlu TF. Accuracy of working length measurement by Raypex 6: electronic apex locator versus actual measurements under stereomicroscope. Balk J Dent Med. 2022;26:15–21. [Google Scholar]
- 26.Dummer PM, McGinn JH, Rees DG. The position and topography of the apical canal constriction and apical foramen. Int Endod J. 1984;17:192–8. [DOI] [PubMed] [Google Scholar]
- 27.ElAyouti A, Weiger R, Löst C. Frequency of overinstrumentation with an acceptable radiographic working length. J Endod. 2001;27:49–52. [DOI] [PubMed] [Google Scholar]
- 28.Sharma MC, Arora V. Determination of working length of root canal. Med J Armed Forces India. 2010;66(3):231–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolters WJ, Duncan HF, Tomson PL, Karim IE, McKenna G, Dorri M, et al. Minimally invasive endodontics: a new diagnostic system for assessing pulpitis and subsequent treatment needs. Int Endod J. 2017;50:825–9. [DOI] [PubMed] [Google Scholar]
- 30.Duncan HF. Present status and future directions—vital pulp treatment and pulp preservation strategies. Int Endod J. 2022;55:497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fleming CH, Litaker MS, Alley LW, Eleazer PD. Comparison of classic endodontic techniques versus contemporary techniques on endodontic treatment success. J Endod. 2010;36:414–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are specific to this study and were not obtained from any other study.Code availability: All data generated or analyzed during this study are specific to this study and were not obtained from any other study.This data will be shared upon a reasonable request from corresponding author.