Abstract
Objective
To investigate the efficacy of Endobutton plate combined with high-strength suture Nice knot fixation in the treatment of distal clavicular fractures with coracoclavicular ligament injuries.
Methods
A retrospective analysis was performed on 43 patients who sustained distal clavicular fractures along with injuries to the coracoclavicular ligament. These patients were treated between January 2017 and December 2023. The fractures were classified according to the fixation method: high-strength Nice knot suture fixation (experimental group, n = 23) and acromioclavicular Kirschner wire fixation (control group, n = 20). The basic information of the two groups of patients, including age, gender, cause of injury, fracture classification, hospitalization duration, fracture healing time and complications, was collected and analyzed. The increase rate of coracoclavicular space on the affected side was collected and analyzed. The pain level of the affected shoulder was assessed using the visual analog scale (VAS). The shoulder joint function was assessed using the American Shoulder and Elbow Surgeons (ASES) scores and Constant-Murley scores before and after surgery.
Results
No significant differences were observed in the general demographic data, including age, gender, injury etiology, Craig classification, and hospitalization duration between the two groups (p > 0.05). Both groups were followed for a period ranging from 12 to 33 months, with an average follow-up of 20.53 ± 5.16 months. The bone healing time in the experimental group was significantly shorter than in the control group (12.82 ± 1.12 weeks vs. 17.25 ± 1.71 weeks, p < 0.05). At the final follow-up, The increase rate of coracoclavicular space was (9.25 ± 2.53) % in the experimental group and (8.10 ± 2.53) % in the control group, which was not significantly different (p > 0.05). Both groups demonstrated significant improvements in VAS scores, Constant-Murley scores, and ASES scores post-operatively compared to pre-operative values (p < 0.05). One month after surgery, the Constant-Murley and ASES scores were significantly superior in the experimental group compared to the control group (p < 0.05). However, no statistical difference was observed three months post-surgery or during the final follow-up (p > 0.05). The control group reported one case of infection related to the Kirschner wire and one case of Kirschner wire displacement postoperatively. Conversely, no significant complications were reported in the experimental group.
Conclusion
In the management of distal clavicle fractures accompanied by coracoclavicular ligament injuries, particularly oblique fractures or those with butterfly-shaped fragments, the application of a high-strength Nice knot suture in conjunction with Endobutton plate fixation can effectively stabilize the fracture site. This approach not only mitigates complications associated with Kirschner wire fixation but also enhances fracture healing, leading to favorable postoperative outcomes.
Keywords: Distal clavicle fracture, Endobutton plate, Coracoclavicular fixation, Kirschner wire, Nice knot
Introduction
In clinical practice, clavicle fractures are typically categorized into proximal, mid-shaft, and distal types. Notably, distal clavicle fractures frequently necessitate surgical intervention. These fractures occur in the outer third of the clavicle and are often associated with damage to the coracoclavicular ligament, leading to pronounced displacement and elevated nonunion rates [1]. While numerous fixation techniques exist, each exhibits certain limitations, and a universally accepted gold standard for treatment remains elusive [3]. Most distal clavicle fractures result from injury to the coracoclavicular ligament, which is why coracoclavicular ligament reconstruction has been gaining popularity. Additionally, coracoclavicular fixation has good biomechanical qualities [5] and the coracoid process is stronger than the distal clavicle [7]. As a result, in recent years, coracoclavicular suspension fixation has been suggested as a therapy approach [8].
A popular fixation technique for the coracoclavicular joint is the Endobutton plate [9]. However, it only offers vertical stability to the fracture site, making it challenging to manage horizontal displacement. This can lead to delayed or nonunion of the fracture and internal fixation failure [2]. Some studies have suggested combining coracoclavicular fixation with percutaneous Kirschner wire fixation of the fracture site. However, this approach can irritate the surrounding skin and presents risks of infection and Kirschner wire displacement [12], hindering early functional shoulder joint exercise. Suture ligation can be used for the reduction and fixation of fractures and small bone fragments. The Nice knot, a high-tension sliding knot with a double-wire structure, can achieve maximum suture tension.Therefore, Nice knot ligation could potentially enhance Endobutton plate coracoclavicular fixation. We conducted a retrospective analysis of the clinical data of patients who sustained distal clavicle fractures along with coracoclavicular ligament injuries and who underwent coracoclavicular fixation with an Endobutton plate between January 2017 and December 2023. This study compared the clinical efficacy of different fixation methods (percutaneous Kirschner wire fixation or high-strength suture Nice knot fixation). Also, it explored the feasibility and advantages of assisting high-strength suture Nice knot fixation of fracture sites based on coracoclavicular elastic fixation.
Materials and methods
Inclusion criteria
1.Acute closed distal clavicle fracture (fracture within three weeks) combined with coracoclavicular ligament injury or avulsion fracture of the coracoclavicular ligament insertio; 2. The fracture line was an oblique or butterfly-shaped fragment in the fracture area; 3. Normal shoulder joint function before injury.4. Craig’s classification type IIB and type V.
Exclusion criteria
(1) Old distal clavicle fracture; (2) Fracture end morphology was a transverse fracture that could not be fixed by wire tying; (3) Ipsilateral mid-clavicular or proximal fracture, scapular fracture, coracoid fracture; (4) Follow-up time of less than one year; (5) Craig’s classification type I, type IIA, type III, and type IV; (6) Pathologic fracture and contralateral clavicle fracture.
Patients
From January 2017 to December 2023, a total of 43 patients met the selection criteria and were included in this study. The study employed a stratified random allocation method. First, the patients were divided into four age groups, including the under-20 group, the 20–40 group, the 40–60 group, and the over-60 group. Then, within each stratum, patients were randomly assigned to the experimental group or the control group using coin flips. These patients were categorized into two groups: the high-strength suture Nice knot fixation group (experimental group, n = 23) and the acromioclavicular Kirschner wire fixation group (control group, n = 20).
The experimental group: The patients consisted of 7 males and 16 females. There were 10 cases on the left side and 13 cases on the right side. The cause of injury included 8 traffic accidents, 13 falls, and 2 sports injuries. There were 2 cases with rib fractures.
The control group: The patients consisted of 5 males and 15 females. There were 8 cases on the left side and 12 cases on the right side. The cause of injury included 9 traffic accidents and 11 falls.
Pre-surgery, both groups of patients underwent bilateral clavicular X-ray imaging and CT three-dimensional reconstruction of the affected shoulder. There were no significant differences in age, gender, cause of injury, Craig classification, comorbidities, length of stay, presurgical visual analog scale (VAS), American Shoulder and Elbow Surgeons (ASES) scores, and Constant-Murley scores between the two groups before the surgery (Tables 1, 2 and 3) (Figs. 1 and 2).
Table 1.
Baseline characteristics ( ±SD) in both groups
±SD) in both groups
| Total (n = 43) | A(n = 23) | B(n = 20) | P | |
|---|---|---|---|---|
| Age (years) | 46.28 ± 13.69 | 47.08 ± 12.89 | 45.8 ± 14.52 | 0.76 |
| Gender (female/male) | 31/12 | 16/7 | 15/5 | 0.69 |
| BMI(Kg/m2) | 24.87 ± 3.64 | 25.19 ± 3.80 | 24.49 ± 3.50 | 0.53 |
| LOS(length of stay) | 7.69 ± 1.67 | 7.82 ± 1.72 | 7.55 ± 1.64 | 0.59 |
| Bone healing time | 14.88 ± 2.61 | 12.82 ± 1.12 | 17.25 ± 1.71 | 0.003 |
| Drinking history | 16(37%) | 8(35%) | 8(40%) | 0.72 |
| Smoking history | 18(42%) | 10(44%) | 8(40%) | 0.053 |
| Hypertension | 16(37%) | 8(35%) | 8(40%) | 0.13 |
| Diabetes mellitus | 8(19%) | 3(13%) | 5(25%) | 1.01 |
| Craig’s classification | ||||
| IIB | 26(60%) | 14(60%) | 12(60%) | 0.95 |
| V | 17(40%) | 9(40%) | 8(40%) |
A: the experimental group; B: the control group; LOS: length of stay in hospital
Table 2.
Coracoclavicular space ( ±SD %)
±SD %)
| Group | Pre-op. | 1month | 3months | LFU | p(pre-op.vs.1 m) | p(1 m vs. 3 m) | p(3 m vs. LFU) |
|---|---|---|---|---|---|---|---|
| A | 62.76 ± 28.74 | 9.37 ± 3.46 | 9.66 ± 2.95 | 9.25 ± 2.53 | 0.0001 | 0.77 | 0.62 |
| B | 68.36 ± 30.59 | 7.49 ± 3.41 | 8.23 ± 2.60 | 8.10 ± 2.53 | 0.0001 | 0.46 | 0.88 |
| p(A vs. B) | 0.54 | 0.08 | 0.10 | 0.16 |
A: the experimental group; B: the control group;1month: 1month post-operation; 3 months: 3 months post-operation; LFU: last follow-up
Table 3.
Functional results ( ±SD)
±SD)
| Group | Pre-op. | 1month | 3months | LFU | p(pre-op.vs.1 m) | p(1 m vs. 3 m) | p(3 m vs. LFU) |
|---|---|---|---|---|---|---|---|
| VAS | |||||||
| A | 7.47 ± 1.01 | 2.52 ± 0.65 | 2.26 ± 0.94 | 1.83 ± 0.86 | 0.0001 | 0.29 | 0.12 |
| B | 7.55 ± 1.02 | 4.05 ± 0.80 | 2.25 ± 1.09 | 1.80 ± 0.67 | 0.0001 | 0.003 | 0.13 |
| p(A vs. B) | 0.82 | < 0.05 | 0.97 | 0.91 | |||
| CS | |||||||
| A | 43.86 ± 8.87 | 88.95 ± 1.82 | 90.52 ± 3.89 | 91.26 ± 3.21 | 0.0001 | 0.09 | 0.48 |
| B | 40.95 ± 9.31 | 67.95 ± 5.95 | 90.65 ± 3.64 | 91.15 ± 2.70 | 0.0002 | 0.002 | 0.59 |
| p(A vs. B) | 0.29 | < 0.05 | 0.91 | 0.90 | |||
| ASES | |||||||
| A | 41.45 ± 7.81 | 88.54 ± 1.97 | 89.86 ± 3.42 | 91.22 ± 2.73 | 0.0001 | 0.13 | 0.14 |
| B | 41.42 ± 9.78 | 67.63 ± 6.05 | 91.05 ± 3.06 | 90.78 ± 2.95 | 0.0001 | 0.002 | 0.91 |
| p(A vs. B) | 0.99 | 0.0003 | 0.26 | 0.71 | |||
A: the experimental group; B the control group;1 month: 1month post-operation; 3 months: 3 months post-operation; LFU: last follow-up; CS: Constant-Murley Score; ASES: American Shoulder and Elbow Surgeons Score
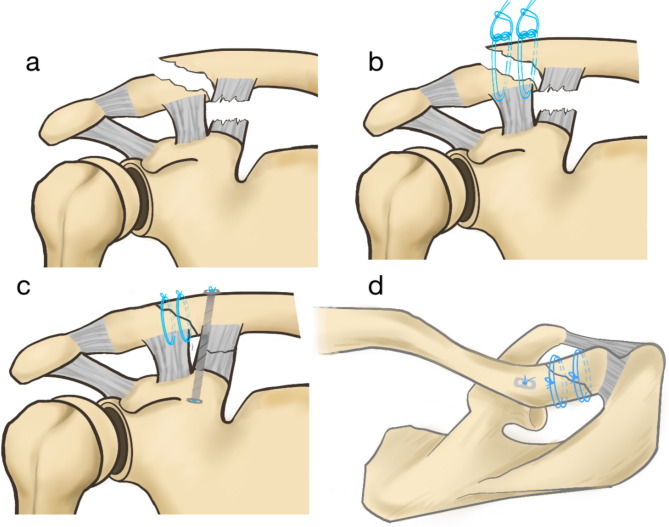
Fig. 1.
Schematic diagram of the surgical procedure. a The fracture shape is long oblique, and the coracoclavicular ligament is ruptured. b Nice knot fixation. c and d The Endobutton plate combined with high-strength suture Nice knot fixation. Both the coracoclavicular space and fracture reduction are well restored in the coronal and axial positions
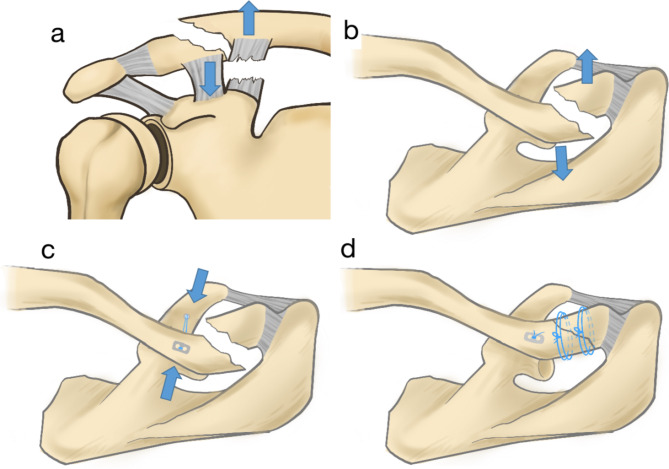
Fig. 2.
Schematic diagram of the fracture displacement direction. a and b Coronal and axial positions show the proximal fracture shifted upward and backward, while the distal fracture shifted downward and forward. c and d The Endobutton plate is fixed in the direction from anterior-inferior to posterior-superior, which is the same as the direction of fracture displacement. The fixation method conforms to the biomechanical characteristics of the patient, and ultimately, the fracture site is well reduced
Surgical technique
Upon administering general anesthesia, the patient was positioned in a beach chair with their upper torso elevated between 30° and 50°. The affected shoulder was cushioned, and the head and neck were gently extended backward and turned toward the unaffected side. A 4–5 cm transverse incision was made along the clavicle’s long axis above the fracture site. This allowed for layer-by-layer dissection of the skin and subcutaneous tissues to expose the fracture site, while also clearing any hematoma and soft tissue in the vicinity. Furthermore, a second incision of 2–3 cm was made on the coracoid process’s surface. Blunt separation of the muscle tissue revealed the base of the coracoid process. For fracture reduction under direct vision, two 2.0 mm K-wires were used in the control group to fix the fracture site percutaneously from the acromion. In the experimental group, non-absorbable sutures (Johnson & Johnson, USA) were used to tie a Nice knot to the fracture site for pre-reduction (note that the bone fragments torn off the insertion points of the trapezius or pyramidal ligaments should be tied to the shaft); temporary fixation with K-wires could be added depending on the stability of the fracture. With the assistance of the shoulder-lock joint guide (Arthrex, USA), a 1.5 mm K-wire was used as a guide pin to establish a bone tunnel from the clavicle to the base of the coracoid process. A 3.2 mm hollow drill was used to drill through the bone tunnel along the guide pin direction. A self-developed guide (Fig. 3; patent ID ZL 2022 2 2614319.6) was used to introduce a traction wire from the clavicle through the bone tunnel to the coracoid process. The Endobutton (Arthrex, USA) with high-strength sutures was introduced from the bone tunnel on the clavicle. The Endobutton plate was placed at the base of the coracoid process, and another Endobutton plate was placed on the clavicle. The Nice knot was tightened, and after confirming the satisfactory reduction of the fracture, it was tied up. In the experimental group, the Nice knot could be tied at the fracture end with complete final fixation with 3–5 single knots. The control group retained the Kirschner wire. After confirming the fracture’s accurate reduction and good position of the plate with a C-arm X-ray machine, the incision was closed with layered sutures (Figs. 4 and 5).
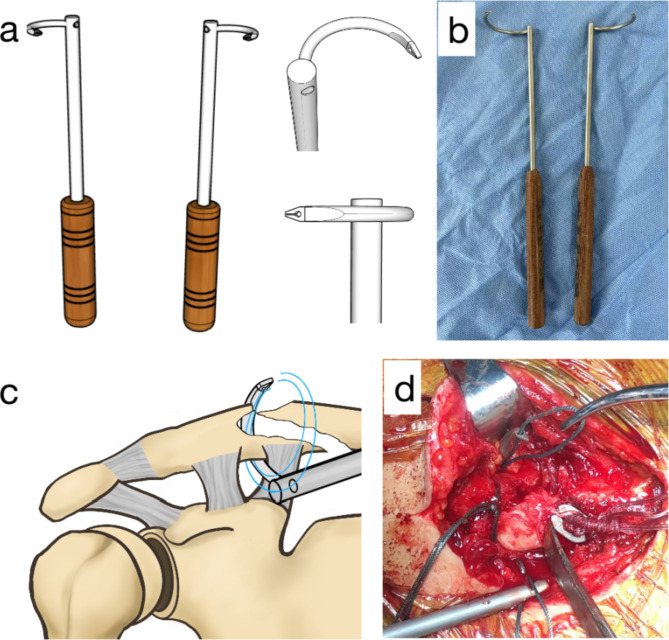
Fig. 3.
A self-developed guide. a and b The top end of the tool is designed in two models, one pointing to the left and the other to the right, suitable for left and right clavicle fractures, respectively. c and d The surgery is demonstrated in a schematic diagram and actual photograph. The tool can easily pass under the clavicle without causing damage to blood vessels or lungs
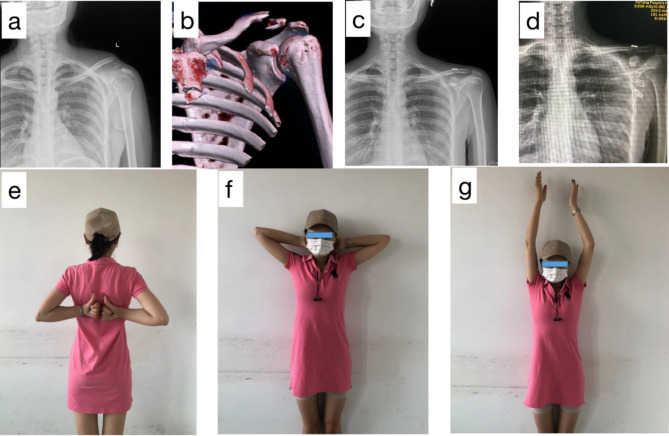
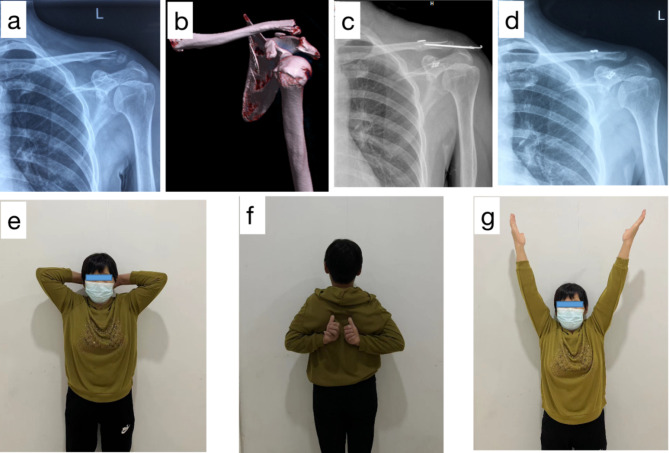
Fig. 4.
(with written informed consent provided). A 30-year-old female patient who suffered distal clavicle fractures with coracoclavicular ligament injuries was treated with an Endobutton plate combined with high-strength suture Nice knot. a and b Preoperative X-ray and CT scans showing the distal clavicle fractures, with the proximal fracture shifted backwards and upwards and the distal fracture shifted forward and downward. c and d Immediate postoperative X-ray showed satisfactory fracture reduction. The final follow-up X-ray demonstrated satisfactory fracture healing and satisfactory coracoclavicular space. e, f and g The patient’s shoulder joint recovered satisfactorily after surgery
Fig. 5.
(with written informed consent provided). A 65-year-old female patient who suffered distal clavicle fractures with coracoclavicular ligament injuries was treated with an Endobutton plate combined with acromioclavicular Kirschner wire fixation. a and b Preoperative X-ray and CT scans showing the distal clavicle fractures, with the proximal fracture shifted backwards and upward and the distal fracture shifted forwards and downward. c An immediate postoperative X-ray showing satisfactory fracture reduction. d This patient developed an infection around the Kirschner wire two weeks after surgery and was hospitalized again for removal of the Kirschner wire. At the final follow-up, satisfactory fracture healing and coracoclavicular space were observed. e, f and g The patient’s shoulder joint healed satisfactorily after surgery
Postoperative treatment
Postoperatively, antibiotics were administered routinely for either one or two days. Within the first week following surgery, the affected shoulder joint was immobilized while the remaining joints of the limb could be exercised through flexion and extension movements. After a week, pendulum exercises for the shoulder joint were initiated. For the experimental group, activities involving shoulder joint elevation commenced four weeks after the surgery. In contrast, for the control group, these activities were permitted only after removing the Kirschner wires, which occurred six weeks after surgery.
Efficacy assessments
All surgeries were performed by two experienced orthopedic surgeons. The data were collected and analyzed by two orthopedic surgeons. The healing of the fracture was assessed by two experienced orthopedic surgeons and radiologists independently. The healing criteria were as follows: (1) The fracture site was pain-free and without deformity, and clinical symptoms had disappeared. (2) Physical examination revealed no abnormalities, with no local tenderness or abnormal mobility at the fracture site. (3) X-ray or CT scans showed the disappearance of the fracture line. Based on these criteria, the fracture healing time was calculated.Potential complications, including infection, coracoid fracture, displacement of the Kirschner wire, and local skin irritation, were documented. The distance between the affected and healthy sides of the coracoid process was measured on the X-ray images. The coracoclavicular distance in Type V: the vertical distance between the inferior cortical bone of the main fracture fragment of the clavicle and the upper border of the coracoid process.The increase rate of coracoclavicular space was determined using the following formula: (value of the affected side – value of the healthy side) / value of the healthy side × 100%. The VAS, ASES scores, and Constant-Murley scores were assessed preoperatively, at one month and three months post-surgery, and at the final follow-up.
Statistical analysis
SPSS 26.0 (version 26.0; IBM, Armonk, NY, USA) was used for statistical analysis. The measurement data were in normal distribution and are expressed as the mean ± standard deviation. Independent sample T-tests were used for comparisons between the two groups, and repeated measures analysis of variance was used for comparing VAS, ASES scores, and Constant-Murley scores between the two groups. Comparisons between different time points in the same group were performed using the Bonferroni method, and comparisons between different groups at the same time point were performed using multi-factor analysis of variance. Fisher’s exact probability method was used to compare count data between the groups. A p-value < 0.05 was considered statistically significant.
Results
Both patient groups underwent surgery without any severe complications, including vascular and nerve injury and coracoid process fracture. Postoperatively, one case in the control group experienced infection related to the Kirschner wire, which improved after cleaning and changing the dressing. No complications, such as skin necrosis or deep infections, were observed. Kirschner wire displacement occurred in one case and was removed by incision six weeks post-surgery. The experimental group did not experience any significant complications. Both groups were followed for a period ranging from 12 to 33 months, with an average of 20.53 ± 5.16 months. The fracture healing times in the experimental and control groups were 12.82 ± 1.12 weeks and 17.25 ± 1.71 weeks, respectively, which was statistically significantly different (p < 0.05, Table 1). At the last follow-up, the increase rate of the coracoclavicular space in the experimental and control groups were (9.25 ± 2.53) % and (8.12 ± 2.53) % ,respectively, with no statistically significant difference (p > 0.05, Table 2). The VAS, ASES scores, and Constant-Murley scores of both groups showed significant (p < 0.05) improvement one month after surgery compared to pre-surgery (Table 3). One month after surgery, the experimental group’s ASES and Constant-Murley scores were significantly better than the control group (p < 0.05, Table 3). However, there was no statistically significant difference in ASES and Constant-Murley scores at three months post-surgery and during the final follow-up (p > 0.05, Table 3).
Discusssion
The coracoclavicular ligament plays a crucial role in maintaining the vertical stability of the distal clavicle. Fractures involving this structure, particularly those with associated ligament injuries, often exhibit poor stability and typically necessitate surgical intervention. Present fixation techniques primarily encompass rigid fixation via the fracture or acromion, flexible fixation through the coracoid process, and a combination of both methods. Rigid fixation predominantly involves the use of a clavicle hook plate and anatomical locking plate fixation. While the clavicle hook plate provides firm fixation, it restricts shoulder joint movement and is associated with numerous complications [13]. Conversely, the anatomical locking plate eliminates the need for trans-articular fixation and preserves the range of motion of the acromioclavicular joint. However, for extremely distal fractures, comminuted fractures, or osteoporotic fractures, its screws may not effectively stabilize the distal bone fragment. Therefore, rigid fixation without coracoclavicular ligament reconstruction carries a long-term risk of increasing the coracoclavicular distance [16].
Endobutton plates are prevalent flexible fixation techniques that indirectly stabilize and repair fractures by reconstructing the coracoclavicular ligament. Unlike traditional methods, they do not necessitate consideration of the size and shape of distal bone fragments, making them suitable for fracture types that are challenging to secure effectively with locking plates. While Endobutton plates efficiently maintain vertical fracture stability, they can potentially cause horizontal displacement, leading to a ‘wipers’ effect. This effect heightens the risk of nonunion and internal fixation failure [7]. The Nice knot, a high-tension self-locking sliding knot, has shown promise in fracture reduction, fixation, and ligament repair [17]. However, its application in distal clavicle fracture fixation remains limited.
This study examined 43 patients with distal clavicle fractures characterized by an oblique fracture line or a butterfly-shaped bone fragment at the fracture site. We fixed the fractures with an Endobutton plate and high-strength suture Nice knot, achieving good clinical results. Specifically, No. 5 Ethibond non-absorbable suture was employed for the fixation of the fracture ends via loop ligation. This suture is renowned for its superior strength and resistance to breakage, making it a preferred choice for tendon and ligament repairs and fracture fragment fixation.The Nice knot, a high-tension self-locking sliding knot, features a two-wire structure that tightens and slides under pressure, analogous to the function of a strapping belt. This design ensures stability and prevents the knot from slipping. Furthermore, not only is the knot easy to loosen, but it is also user-friendly and can be reapplied multiple times. During surgical procedures, the knot’s quick adjustment between loosening and tightening facilitates minor modifications and temporary fixation during fracture reduction [12].
The experimental group in this study had a better average fracture healing time than the control group, and there were no cases of nonunion or delayed union. The average fracture healing time was much shorter than in earlier trials when clavicle fractures were fixed rigidly [17]. This is because the Nice knot gets tighter, reducing the fracture’s displacement and separation distance while increasing the fracture site’s contact area.Furthermore, it has to do with the reduction and fixation of the fragments of the mall fracture, which serve as the ligaments’ attachment points. Two patients in the control group in this trial had complications. Specifically, one patient developed an infection associated with the Kirschner wire, manifested by local redness, swelling, and minor exudation, which resulted in shoulder pain and discomfort. Another patient suffered from Kirschner wire displacement and underwent surgical removal six weeks after the initial surgery. In the control group, patients were required to wait six weeks to have the externally placed Kirschner wires removed, leading to early postoperative limitations in shoulder joint function. However, following the removal of these wires, the patients’ shoulder joint function demonstrated significant recovery and was effectively sustained at three months. post-surgery and during the final follow-up. Conversely, patients in the experimental group opted for a superior treatment method involving the use of an Endobutton plate combined with high-strength suture Nice knot fixation.
The primary advantage of this method is the rapid closure of the surgical wound, obviating the need for Kirschner wires to remain externally and eliminating the necessity for a second surgery to remove these wires.Consequently, patients in the experimental group were able to commence functional exercises early in the postoperative period. One month after the procedure, their shoulder joint function was significantly superior to that of the control group. As the follow-up period extended, these patients’ shoulder joint function continued to improve and remained in a good state for an extended period. This treatment approach expedites patient recovery and contributes to the long-term maintenance of optimal shoulder joint function.
Attention must be given when tying the Nice knot to ensure it is not tightened too early, which could lead to loosening. It is recommended that the Nice knot be retightened after the final fixation of the Endobutton plate. This step effectively ensures the stability of the Nice knot. When the ends of the sutures are tightened, if necessary, a needle holder can be used to gently push and compact the knot to make it more secure. When the sutures are under high tension, multiple square knots should be tied with both ends to achieve a firm final lock, which not only improves surgical results but also effectively reduces the risk of knot loosening. During the fracture reduction process, the periosteum should not be completely stripped, and it is important to preserve as much of the ligament tissue surrounding the fracture as possible. These soft tissues can increase the friction of the Nice knot, thereby providing a certain preventive effect against its sliding.The Nice knot uses a double-line structure, and guiding the folded line loop is an important step [18]. The traditional device needs a guide to draw out a single line first and then uses this single line to fix and draw out the folded line loop, which is cumbersome and time-consuming. To simplify the surgery, we designed a ring-structured wire loop guide [20]. This innovative design allows for close adhesion to the clavicle and facilitates smooth circular guidance of the wire. The unique structure streamlines the surgical procedure, significantly boosting its efficiency. The guide can steer the folded line loop in a single step, thereby optimizing the surgical process considerably. This cutting-edge technology has been successfully implemented in our research to date.
Patients with distal clavicle fractures in this study showed a particular pattern of fracture line displacement: the distal end changed forward and downward, while the proximal fracture line tended to migrate backward and upward. The anterior and middle bundles of the deltoid muscle and the trapezius muscle’s connection to the distal clavicle are the main causes of this pattern. A distal clavicle fracture is commonly caused by a direct, severe collision to the shoulder. The proximal clavicle fracture line is immediately pulled by the trapezius muscle, which extends from the back up to the front down, shifting it upward and backward. The distal fracture end is simultaneously pulled by the deltoid muscle, causing a displacement both forward and downward. It is important to recognize the unique anatomical relationship between the coracoid process and the distal clavicle. In the sagittal plane, the coracoid process precedes the distal clavicle, while in the coronal plane, it lies beneath it. This spatial orientation enables the Endobutton plate’s bone tunnel to be oriented from front to back, paralleling the direction of fracture displacement. Such alignment confers a distinct advantage to the Endobutton plate in terms of reduction and fixation. It can align with the natural trajectory of fracture displacement, ensuring stable support and fixation, thereby facilitating expedited fracture healing and recovery. In essence, the Endobutton plate’s alignment with the fracture displacement direction offers a distinctive benefit in the reduction and fixation of distal clavicle fractures.
In conclusion, Nice knots can effectively supplement Endobutton plates for oblique fractures or distal clavicle fractures with butterfly bone fragments. Combining Nice knots and Endobutton plates can significantly improve the stability of the fracture, promote fracture healing, and allow patients to perform early functional rehabilitation. In addition, it can reduce complications caused by percutaneous Kirschner wire fixation. However, this study is a retrospective case analysis, lacking a prospective design. It has limitations such as selection bias and recall error. It also has a small sample size and short follow-up duration, which might not be long enough to assess long-term outcomes, such as Endobutton plate failure, joint degeneration, and post-traumatic arthritis. Therefore, further large-scale, multi-center, long-term follow-up studies are needed to validate the results of this study.
Acknowledgements
I want to thank everyone who has supported me while I’ve been writing this paper. I sincerely thank Haiyang Yu and my supervisor, Professor Jishi Jiang, for their assistance. Throughout the composition of this report, I really appreciate their expert guidance, support, and patience.
Author contributions
Liu bin is the first author and major contributor in writing manuscript and interpreting the data. Shi lei is the co-first author. Ma huifang performed the collection and follow-up investigation. Jiang jishi and Yu haiyang contributed to the procedure and design of the study and critically revised the manuscript and contributed the intellectual content. All authors read and approved the integrity and accuracy of the final manuscript.
Funding
This research was conducted with the financial support of the Fuyang Health and Wellness Scientific Research Project (grant number FY2023-114 and FY2021-017).
Data availability
According to reasonable requirements, the corresponding authors will provide original data to support the conclusions of this paper.
Declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Fuyang people’s Hospital. Written informed consent is obtained from legal guardian of participants.
Consent for publication
All participants gave written informed consent for their personal and clinical details along with any identifying images to be published in this study.
Informed consent
Written informed consent is obtained from legal guardian of participants. Written informed consent is obtained from adult participants as well.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86(4):778–82. 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Kim DW, Kim DH, Kim BS, Cho CH. Current concepts for classification and treatment of distal clavicle fractures. Clin Orthop Surg. 2020;12(2):135–44. 10.4055/cios20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boonard M, Sumanont S, Arirachakaran A, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(6):1065–78. 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]
- 4.Allahabadi S, Janghala A, Kandemir U. Suture button placed beneath plate fixation for complex distal clavicle fractures and acromioclavicular joint injuries: a technical note. Eur J Orthop Surg Traumatol. 2023;33(7):3175–80. 10.1007/s00590-023-03533-x. [DOI] [PubMed] [Google Scholar]
- 5.Sharma V, Modi A, Armstrong A, Pandey R, Sharma D, Singh H. The management of distal clavicle fractures - a Survey of UK Shoulder and Elbow surgeons. Cureus. 2021;13(8):e17305. 10.7759/cureus.17305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yagnik GP, Brady PC, Zimmerman JP, Jordan CJ, Porter DA. A biomechanical comparison of new techniques for distal clavicular fracture repair versus locked plating. J Shoulder Elb Surg. 2019;28(5):982–8. 10.1016/j.jse.2018.11.041. [DOI] [PubMed] [Google Scholar]
- 7.Hislop P, Sakata K, Ackland DC, Gotmaker R, Evans MC. Acromioclavicular Joint stabilization: a Biomechanical Study of Bidirectional Stability and Strength. Orthop J Sports Med. 2019;7(4):2325967119836751. 10.1177/2325967119836751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu Y, Guo X, Peng H, Dai H, Huang Z, Zhao J. Different internal fixation methods for unstable distal clavicle fractures in adults: a systematic review and network meta-analysis. J Orthop Surg Res. 2022;17(1):43. 10.1186/s13018-021-02904-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapicioglu M, Erden T, Bilgin E, Bilsel K. All arthroscopic coracoclavicular button fixation is efficient for Neer type II distal clavicle fractures. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2064–9. 10.1007/s00167-020-06048-8. [DOI] [PubMed] [Google Scholar]
- 10.Erden T, Kapicioglu M, Ersen A, Toker B, Sahin K, Bilsel K. Arthroscopic coracoclavicular button fixation versus anatomic locking plate fixation for unstable distal clavicular fractures. JSES Int. 2021;5(5):835–9. 10.1016/j.jseint.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vannabouathong C, Chiu J, Patel R, et al. An evaluation of treatment options for medial, midshaft, and distal clavicle fractures: a systematic review and meta-analysis. JSES Int. 2020;4(2):256–71. 10.1016/j.jseint.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyons FA, Rockwood CA. Migration of pins used in operations on the shoulder. J Bone Joint Surg Am. 1990;72(8):1262–7. [PubMed] [Google Scholar]
- 13.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat R. 1987;(214):160–4. [PubMed]
- 14.Gordon JE, Kelly-Hahn J, Carpenter CJ, Schoenecker PL. Pin site care during external fixation in children: results of a nihilistic approach. J Pediatr Orthop. 2000;20(2):163–5. [PubMed] [Google Scholar]
- 15.Asadollahi S, Bucknill A. Hook plate fixation for Acute unstable distal clavicle fracture: a systematic review and Meta-analysis. J Orthop Trauma. 2019;33(8):417–22. 10.1097/BOT.0000000000001481. [DOI] [PubMed] [Google Scholar]
- 16.Furuhata R, Matsumura N, Udagawa K, Oki S, Morioka H. Residual coracoclavicular separation after plate fixation for distal clavicle fractures: comparison between fracture patterns. JSES Int. 2021;5(5):840–5. 10.1016/j.jseint.2021.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee HJ, Kim BK, Ryu HS, Dan J. Vertical Interfragmentary doubled suture for displaced Patella fractures: sequential compressive tightening with nice knot. Clin Orthop Surg. 2020;12(3):413–6. 10.4055/cios20018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fogagnolo F, Salim R, Kfuri M. A simple technique to prevent early or late EndoButton Deployment in Anterior Cruciate Ligament reconstructions: a technical note. J Knee Surg. 2018;31(1):75–7. 10.1055/s-0037-1600090. [DOI] [PubMed] [Google Scholar]
- 19.Fan XL, Wang J, Zhang DH, Mao F, Liao Y. The Use of Nice knots Cerclage to Aid reduction and fixation of Metacarpal fractures. Plast Reconstr Surg. 2021;148(2):e338–9. 10.1097/PRS.00000000000008182. [DOI] [PubMed] [Google Scholar]
- 20.Jiang Jishi. An orthopedic guide capable of using multiple leads:CN202222614319.6[P]. 2023-08-22.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to reasonable requirements, the corresponding authors will provide original data to support the conclusions of this paper.