Abstract
Introduction:
Eating disorders (EDs) are debilitating mental illnesses that can lead to significant medical complications from malnutrition. Eating disorders are on the rise in Asia and the prevalence is expected to increase. The aim of this study was to understand the characteristics of local patients and evaluate our current inpatient nutritional rehabilitation protocol for anorexia nervosa (AN).
Methods:
Retrospective descriptive data were gathered from 47 patients diagnosed with AN. Patients with admissions were further stratified according to their nutritional management based on whether they were on the AN protocol or standard hospital care. Data on their rate of weight gain, length of stay and calorie prescription were collected.
Results:
Similar to previous studies, the majority of AN patients were female (96.7%). However, the age at presentation of AN in this study, as compared with previous local studies, had decreased (14 vs. 16 years). We also found that patients on the AN protocol were prescribed a higher amount of calories than those given standard care (2,700 vs. 2,317 calories). Patients on the AN protocol achieved a higher rate of weight gain per week (1.15 vs. 0.29 kg) and had a shorter length of hospital stay (23 vs. 36 days).
Conclusion:
Patients with AN appear to be presenting at a younger age. Medical stabilisation of AN patients can be achieved more quickly through a higher calorie inpatient AN treatment protocol. Future local studies examining actual calorie consumption, its effect on weight gain trajectory, severity of refeeding syndrome and time to remission will be beneficial.
Keywords: Anorexia, eating disorders, malnutrition
INTRODUCTION
Eating disorders (EDs) are debilitating mental illnesses that have consequent deleterious effects on physical health as a result of improper, imbalanced and inadequate nutrition. It has been established that EDs are on the rise in Asia, and the prevalence of EDs is expected to climb further, with several studies showing increasing body dissatisfaction among some segments of the population, particularly university students and Singaporean Chinese schoolgirls.[1,2] A study showed that the prevalence of young Singaporean females at risk of developing EDs was 7.4%, and this figure is similar to that in the West.[3] What is more, there is a cultural preference for thinness, especially among Chinese Singaporean female youths, and it is concerning that dieting and the desire to be thinner were present even among girls who were already underweight.[4]
A follow-up descriptive study of anorexia nervosa (AN) patients in acute Singapore hospital between 2003 and 2010 showed that the presentation of the disease had become more severe over the years.[5] Also, existing local literature on patients with AN who received medical nutritional therapy (MNT) from qualified dietitians is scarce. The latest such research included patients suffering from AN who were seen by dietitians between 1992 and 2004.[6] This highlights the need to improve our understanding of recent patient populations to facilitate more effective therapy and enhance patient outcomes.
Nutritional rehabilitation is fundamental in the treatment of AN. An essential component of nutritional rehabilitation involves weight restoration to prevent serious physical complications and to correct both the biological and psychological effects of malnutrition.[7,8,9] Weight restoration is also imperative in improving cognitive function to render psychological interventions effective.[8,9] Weight restoration in AN patients is achieved through consumption of adequate calories and nutrients under the guidance of their professional treatment team. However, there is limited data that address the optimum calories required for weight restoration.[8] The majority of local studies conducted so far focused on the types of treatment (inpatient/outpatient/day treatment, etc.) and psychotherapy.[2,6,10,11] Local data comparing calorie prescription to patient outcome have not been presented so far.
In this study, we aimed to (a) understand the characteristics of the local patients we see; (b) evaluate our current inpatient treatment protocol for underweight AN patients and correlate calorie prescription with patient outcomes; and (c) review the current literature on nutritional rehabilitation in patients with AN. This knowledge can guide us in improving clinical practice guidelines for managing underweight AN patients who require weight restoration in our setting.
METHODS
This is an observational, retrospective, cross-sectional study. Figure 1 depicts the study process. The electronic records of patients with EDs who had their first dietetic consultation at the National University Hospital (NUH) between 1 June 2015 and 31 December 2016 were accessed and reviewed retrospectively. Ethics approval was obtained to read and analyse these patient records. Waiver of informed consent was granted, as this was a retrospective review of patients’ medical records. Altogether, 62 patient records were available for analysis. All patients were included in this study, regardless of their age.
Figure 1.
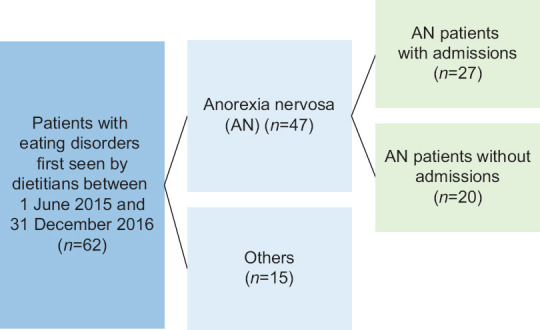
Flowchart of the study process.
We included only 47 patients who had been diagnosed with AN by attending psychiatrists or physicians based on the latest American Psychiatric Association’s (APA) criteria, Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), which was published in 2013. Based on DSM-5, the diagnostic criteria for AN are as follows:[12]
Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than that minimally expected.
Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight.
Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation or persistent lack of recognition of the seriousness of the current low body weight.
In addition to these, we also included patients with atypical AN defined by DSM-V as follows: All of the criteria for AN are met, except that despite significant weight loss, the individual’s weight is within or above the normal range.[12]
Clinical events of patients, such as admissions, were tracked for up to a 2-year period from their first dietetic consultation. The information collected included: type of EDs, gender, onset and duration of illness before the first presentation (i.e. when the patient was first seen by a dietitian), treatment setting, anthropometric data trend (i.e. weight, height and body mass index [BMI]) from initial diagnosis through treatment, diet history at the first presentation, and medical and psychiatric comorbidities. If patients were admitted for nutritional rehabilitation, we also collected additional information, including calories provided during admission, rate of weight gain per week, length of stay and whether the patient was treated using the hospital AN protocol.
All patients were provided with specialised dietetics care based on evidence-based clinical practice guidelines that were developed by the dietetics department of NUH. These included comprehensive MNT and counselling by specialist dietitians. Dietitians worked closely with the multidisciplinary team consisting of physicians, psychologists, art therapists and psychiatrists (if needed) to ensure that behavioural management strategies and advice were consistent in the treatment team. Dietetics care was also tailored to suit the individual needs of each patient depending on their age, treatment setting and stage of treatment. Nutritional intervention included extensive psychoeducation about the illness and individualised counselling for nutritional restoration (i.e. correction of suboptimal BMI, nutrient deficiencies and perception on healthy eating). Dietitians also identified foods that patients avoided due to AN and worked with each individual to gradually reintroduce these foods into their diets. Specialist dietitians incorporated motivational interviewing techniques to engage both patients and their caregivers.
At the first consultation, dietitians conducted a detailed history to understand the patients’ eating habits and attitudes towards eating. Where possible and required, the history taken was corroborated with their caregivers. As part of nutritional assessment, total daily calorie intake was estimated from the diet history taken and compared to estimated energy requirements. Estimated energy requirements were calculated using standard Schofield equations.
Weight and height were taken using calibrated hospital stadiometers and weighing scales at patient visits to the hospital. The BMI and rate of weight gain were calculated to track patients’ progress and as markers to determine overall average improvement. Local percentile charts were used to plot height-for-age, weight-for-height and BMI-for-age for those under 18 years of age.
Underweight AN inpatients who were admitted solely for the purpose of medical stabilisation and nutritional rehabilitation were put on a default AN protocol. The default AN protocol was started from day 1 of admission and provided 2,700 calories from a total of three meals (1,600 calories), three snacks (300 calories) and three oral nutritional supplements (800 calories). Patients were given 45 min to consume their main meals and 30 min to consume their snacks. The consumption of all food items and supplements was done under strict supervision by the nursing staff. If meals were unfinished, patients had to consume a ‘top-up’ of another oral nutritional supplement. If they were unable to complete the top-up supplement, a nasogastric tube was inserted to ensure that the patient achieved the prescribed calories. As part of the protocol, all patients were closely monitored for refeeding syndrome (RFS) and provided with thiamine (Vitamin B1) supplementation. Other multivitamins and minerals were recommended by the treating team and provided on an as-needed basis.
Other AN patients who were admitted for stabilisation of urgent mental health issues such as attempted suicide or overdose were not put on the default AN protocol. Those not on the AN protocol were provided standard hospital meals of 1,800 calories from a total of three meals (1,600 calories) and one snack (200 calories). No time limit was imposed on finishing the meals or snack. Nurses monitored these patients’ intake as per standard care and continued to encourage them to finish their food. Oral caloric nutritional supplements were prescribed by dietitians on an as-needed basis. If meals were unfinished, oral nutritional supplements were recommended for top-up, although patients could refuse, with no further action taken. In some patients, additional oral nutritional supplements were also recommended outside of mealtimes to enhance calorie intake, especially if they were not eating well. Monitoring for RFS was dependent on recommendations by the treating team. Multivitamins and minerals were recommended and provided on an as-needed basis.
Data analysis was carried out using IBM SPSS Statistics version 23.0 (IBM Corp, Armonk, NY, USA). Due to the small sample size, the Shapiro–Wilk test was performed to check for normality. As the data were not normally distributed, descriptive data were presented as median and range. Mann–Whitney U test was performed to compare the differences between the medians of variables for those on the AN protocol versus those not on the protocol. Statistical significance was set at P < 0.05.
RESULTS
Patient profile and characteristics
Patient characteristics such as age, duration of illness, weight and BMI, and the estimated calorie intake before the first dietetics session are presented in Table 1. Out of the 47 AN patients seen by dietitians, 45 (96.7%) were females and the rest were males. The median age was 14 (range 11–38) years. The median duration from first diagnosis of AN to the first presentation to the dietitian was 9.5 (range 1–108) months. The median weight at the first diagnosis of AN was 39.52 kg with a median BMI of 16.05 kg/m2, and the median weight at the first dietitian consult was 39.30 kg with a median BMI of 15.70 kg/m2. The median estimated reported calorie intake of the 47 AN patients before seeing the dietitian was 17.6 (range 3.4–42.2) calories/kg weight. Of the 47 AN patients seen by dietitians, six (12.8%) were seen solely in the inpatient setting, 20 (42.6%) were seen solely in the outpatient setting and 21 (44.7%) were seen in both inpatient and outpatient settings.
Table 1.
Characteristics of patients with anorexia nervosa (N=47).
| Variable | Median (range) |
|---|---|
| Age at first presentation (yr) | 14 (11–38) |
|
| |
| Duration of illness before first presentation (mth) | 9.5 (1–108) |
|
| |
| Estimated reported calorie intake before first dietetics session (kcal/kg) | 17.6 (3.4–42.2) |
|
| |
| Weight (kg) | |
|
| |
| At onset of illness | 39.52 (30.20–61.90) |
|
| |
| At first dietetics presentation | 39.30 (27.60–64.25) |
|
| |
| Body mass index (kg/m2) | |
|
| |
| At onset of illness | 16.05 (12.60–21.84) |
|
| |
| At first dietetics presentation | 15.70 (11.00–21.67) |
Inpatient nutrition rehabilitation for underweight patients with AN
Of the 47 AN patients, 27 (57%) patients had hospital admission. Five of these 27 patients were readmitted for a second time and another two were readmitted for a third time over a 2-year period. Data from the first admissions of 22 underweight patients were analysed. The remaining five patients were excluded, as their data were incomplete (i.e. two patients were discharged at their own risk and did not complete the inpatient treatment, while three patients did not have their weight trend taken through the course of admission). Food and supplements prescribed to all 22 patients were consumed via the oral route. None of the patients on the AN protocol required insertion of a nasogastric tube.
We compared the effect of the AN protocol on the total calories prescribed to patients, the rate of weight gain per week and length of stay of patients [Table 2] was higher than that for those not on the AN protocol (median 2,700 vs. 2,317 kcal). Results from Mann–Whitney U test indicated a statistically significant difference between the two groups (U = 2.0, z = −2.92, P = 0.001). Likewise, the rate of weight gain per week for those on the AN protocol was higher than that for those not on the AN protocol (median 1.15 vs. 0.29 kg), and this was also statistically significant (U = 7.0, z = −2.47, P = 0.010). The length of stay for those on the AN protocol was shorter than that for those not on the AN protocol (median 23 vs. 36 days), although this was not statistically significant (U = 31.0, z = −0.43, P = 0.712).
Table 2.
Comparison of underweight patients on the AN protocol versus those not on the AN protocol.
| Variable | Median (range) | P* | |
|---|---|---|---|
|
| |||
| AN protocol (n=18) | Non-AN protocol (n=4) | ||
| Daily calories prescribed (kcal) | 2,700 (2,380–3,167) | 2,317 (2,150–2,400) | 0.001† |
|
| |||
| Rate of weight gain per week (kg) | 1.15 (0.23–3.54) | 0.29 (0.12–0.81) | 0.010† |
|
| |||
| Length of stay (day) | 23 (14–76) | 36 (11–51) | 0.712 |
*Mann–Whitney U test. †Statistically significant. AN: anorexia nervosa
DISCUSSION
The majority of patients with AN in our study were females, similar to the reports in the literature[13,14] and those from Singapore.[5,6,10] One study found that females were twice as likely to post pictures of people and food on their social media; this suggests that females tend to have a greater focus on appearance and food than males, which makes them more likely to be at high risk for AN[15] Other studies also found that compared to males, females reported significantly higher levels of body dissatisfaction and disordered eating.[16,17] Ata et al.[17] reported that females had lower self-esteem and faced significantly higher pressure from friends and family to lose weight, while males felt more pressure to gain muscles. Their study also found that adolescents who perceived pressures to lose weight reported negative eating patterns and perceived that their actual body differed from their ideal figure; also those with lower self-esteem may interpret comments from people close to them as inducing pressure, and therefore be more vulnerable to pressures to be thin.[17]
Interestingly, the age at first presentation of AN seems to have decreased compared to that reported by earlier studies. In our study, the median age at first presentation of AN was 14 years compared to 16 years reported by Lim et al. in 2007.[6] This decrease in age of onset of AN coincides with increasing availability of personal computers (69.7%–77% in 2003–2008 vs. 81.4% in 2018).[18] The study by Wilksch et al. (2020) also noted that those with no social media accounts had significantly lower Eating Disorder Examination-Questionnaire (EDE-Q) global scores than those with social media accounts, and strongly suggests that increased social media exposure is associated with higher risk of disordered eating.[15] A Dutch study also found that social media use in high school males and females predicted elevated body dissatisfaction 18 months later, while elevated body dissatisfaction at baseline did not predict social media use 18 months later.[19] This suggests that social media use leads to elevated body dissatisfaction, but body dissatisfaction does not necessarily lead to a greater need for use of social media.[19] Therefore, it may be important for parents to control the time their child spends on social media, especially during the preadolescent period, when parents still have more influence over their child’s behaviour than in the later years. Parental control over the time preadolescents spend on social media has been shown to be associated with greater preadolescent life satisfaction in part because parents may be more involved in the child’s life or the child may be more open to parental direction.[20] However, further studies are still needed to determine this relationship.
The duration of illness before the first presentation to dietetics ranged from 1 to 108 months, resulting in a drop in median BMI from 16.05 to 15.07 kg/m2. It is important for AN to be treated early before it becomes chronic. Chronic AN places tremendous strain on the caregivers, as AN patients require a lot of care and attention, which can negatively impact the relationship between caregivers and patients.[21] It is, therefore, important to reduce the time to seek dietetics intervention to prevent the worsening of AN. There are many factors that can affect an individual’s decision to seek medical treatment, such as financial cost of treatment, health insurance concerns, availability of treatment, lack of health literacy, (i.e. not perceiving ED as an illness), lack of social support, social pressure and public stigma about mental illness.[22,23,24,25] Furthermore, those with AN are often in denial and therefore not likely to seek treatment.[12,26] Vandereycken[26] describes two types of denial: unintentional denial, which refers to failure of oneself to realise the disorder as a result of biological and/or psychological reasons, and intentional denial as a result of reluctance to accept medical treatment, a fear of stigmatisation and even a loss of autonomy. One strategy to help AN patients who are in denial or increase the health literacy of caregivers is through the development of public health awareness and community interventions, which have been found to be effective in decreasing stigmatising attitudes and changing knowledge and beliefs about effective treatments.[27] Various reliable and valid screening tools such as the Eating Disorder Examination[28] and the Eating Disorder Quality of Life Scale[29] can be used by health professionals. It has been found that malnutrition and AN can affect brain function and are associated with grey and white matter reduction.[30,31] Early detection and treatment of AN is crucial for reducing the duration of AN and may even reverse brain abnormalities in individuals with AN after long-term recovery.[32,33]
Calorie restriction of differing severities is a hallmark of AN. It is associated with weight loss and can result in a low fat and fat-free mass. Patients with AN are classified by the Global Leadership Initiative on Malnutrition as having disease-related malnutrition without inflammation.[34] This indicates that starvation is the causative factor of malnutrition arising from AN.[35,36] Starvation can have many debilitating biological and psychological consequences on a patient with AN. If left untreated, it can even lead to death. As such, reversing the effects of starvation via refeeding to achieve weight restoration is a fundamental component in the treatment of underweight AN patients.[7,8,9] Apart from improvements in physical health, weight gain in malnourished AN patients is also necessary to improve cognitive function to render the psychological interventions effective.[8,9,35] Weight recovery can improve the cognitive and behavioural changes associated with the disease, such as food anxiety, depression, obsessions and apathy.[35] To achieve optimal weight gain, both the quantity (i.e. adequate calorie provision) and quality of nutrition are important factors. While refeeding the AN patient is the main way of achieving weight restoration and medical stability, the process can be tricky because AN is driven by an intense fear of weight gain.[35] Although treatment in the outpatient setting is recommended as the first-line option, the decision to admit a patient for inpatient treatment is necessitated for specific reasons, including acute medical stabilisation to reverse or manage the complications associated with emaciation or suicidality.[37,38]
The recommended rate of weight gain per week in the inpatient setting varies internationally, with the majority of guidelines suggesting a minimum of 0.5 kg per week and a maximum of 1–1.5 kg per week.[38] However, there are disparities in the current recommendations for calorie provision to facilitate such weight gain.[38] Our patients on the inpatient AN protocol were prescribed and provided with a higher amount of calories upon admission and throughout the course of their stay. This allowed patients on the protocol to meet the recommended guidelines for weight gain. Furthermore, patients who were on the AN protocol had a clinically significant reduction in their hospital length of stay, which shows that medical stabilisation was achieved more quickly through a higher calorie protocolised treatment regimen. By international standards, the initial calories provided by the default AN protocol on admission is high (i.e. 2,700 calories). Although this was the case, it is possible that patients did not consume all the prescribed calories initially but gradually increased their intake to meet the higher calorie prescription over the course of their stay. Strict supervision is also another factor that could have conferred higher compliance to calorie intake. Patients not on the AN protocol were not strictly supervised by healthcare professionals, and may have had less compliance to the meal intake, which resulted in less weight gain. There could be an increase in purging or compensatory behaviours (such as hiding or discarding food) with less supervision from healthcare professionals.
Another important consideration in the weight restoration process is the risk of developing RFS and how to prevent and/or manage it. Refeeding syndrome refers to the potentially lethal shifts in fluid and electrolytes associated with metabolic and hormonal abnormalities, which can occur following the commencement of nutritional repletion (via oral/parenteral/enteral route) in malnourished or starved individuals.[36,39,40] When improperly managed, RFS can lead to multiorgan failure, even death.[36,39,40] It is widely accepted that RFS can be prevented through a cautious approach, where nutrition is reintroduced slowly and gradually increased until the nutritional needs are met (i.e. start low, go slow), so that significant electrolyte shifts are avoided.[36] This approach, along with close monitoring of electrolytes, electrolyte replacement if necessitated and thiamine supplementation, is supported by consensus guidelines.[36]
Among the pool of AN patients, there is debate between the cautious method of refeeding versus the more aggressive approach where higher amount of calories is started and advanced faster.[35,36] There is increasing evidence that there are benefits to the latter method of refeeding in AN patients, such as quicker weight gain, reduced length of hospital stay and remission at the end of treatment.[11,35,36,41,42] Studies showed that the more aggressive refeeding approach is safe as long as it is part of a protocol and the patients are closely supervised and monitored.[35] It is important to note that studies investigating the cautious approach of RFS are conducted mostly on critically ill patients with other medical comorbidities, while AN patients have isolated starvation without inflammation.[35,36] The difference in the manifestation of RFS may be explained by this reason.[36] A multicentre randomised controlled trial also found that the lowest point in post-refeeding phosphate concentration of AN patients was significantly related to percentage median BMI at the start of refeeding and baseline white blood cell count, rather than baseline energy intake.[43] This finding changes what we know about the stratification of RFS risk in this subgroup of malnourished patients.
Due to the limitation of the study design being retrospective in nature, we were unable to obtain all the information necessary to assess actual calories consumed per day and correlate it with weight gain trajectory. We were also unable to obtain information pertinent to the development of RFS or the time to remission. We acknowledge that this study is small, which may affect the validity of the study. Future studies could be done on a bigger scale and with a prospective design to further validate our findings. Further attention can be given to establish meaningful correlations between the actual calorie intake, its impact on the rate of weight gain, the progression and severity of RFS, and the time taken to remission.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pike KM, Dunne PE. The rise of eating disorders in Asia: A review. J Eat Disord. 2015;3:33. doi: 10.1186/s40337-015-0070-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ung EK. Eating disorders in Singapore: Coming of age. Singapore Med J. 2005;46:254–6. [PubMed] [Google Scholar]
- 3.Ho TF, Tai BC, Lee EL, Cheng S, Liow PH. Prevalence and profile of females at risk of eating disorders in Singapore. Singapore Med J. 2006;47:499–503. [PubMed] [Google Scholar]
- 4.Wang MC, Ho TF, Anderson JN, Sabry ZI. Preference for thinness in Singapore--A newly industrialised society. Singapore Med J. 1999;40:502–7. [PubMed] [Google Scholar]
- 5.Kuek A, Utpala R, Lee HY. The clinical profile of patients with anorexia nervosa in Singapore: A follow-up descriptive study. Singapore Med J. 2015;56:324–8. doi: 10.11622/smedj.2015090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim SL, Sinaram S, Ung EK, Kua EH. The pursuit of thinness: An outcome study of anorexia nervosa. Singapore Med J. 2007;48:222–6. [PubMed] [Google Scholar]
- 7.Yager J, Devlin MJ, Halmi KA, Herzog DB, Mitchell JE, III, Powers P, et al. American Psychiatric Association: Practice guidelines for the treatment of patients with eating disorders third edition. Am J Psychiatry. 2006;163((7 Suppl)):4–54. [PubMed] [Google Scholar]
- 8.Marzola E, Nasser JA, Hashim SA, Shih PB, Kaye WH. Nutritional rehabilitation in anorexia nervosa: Review of the literature and implications for treatment. BMC Psychiatry. 2013;13:290. doi: 10.1186/1471-244X-13-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence. Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa, and Related Eating Disorders (National Clinical Practice Guideline Number CG9) Leicester: The British Psychological Society and Gaskell; 2004. [PubMed] [Google Scholar]
- 10.Lee HY, Lee EL, Pathy P, Chan YH. Anorexia nervosa in Singapore: An eight-year retrospective study. Singapore Med J. 2005;46:275–81. [PubMed] [Google Scholar]
- 11.Wong L, Goh LG, Ramachandran R. Family-based therapy for anorexia nervosa: Results from a 7-year longitudinal Singapore study. Eat Weight Disord. 2019;24:1215–9. doi: 10.1007/s40519-019-00654-3. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: APA; 2013. Feeding and eating disorders. [Google Scholar]
- 13.Petkova H, Simic M, Nicholls D, Ford T, Prina AM, Stuart R, et al. Incidence of anorexia nervosa in young people in the UK and Ireland: A national surveillance study. BMJ Open. 2019;9:e027339. doi: 10.1136/bmjopen-2018-027339. doi:10.1136/bmjopen-2018-027339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steinhausen HS, Jensen CM. Time trends in lifetime incidence rates of first-time diagnosed anorexia nervosa and bulimia nervosa across 16 years in a Danish nationwide psychiatric registry study. Int J Eat Disord. 2015;48:845–50. doi: 10.1002/eat.22402. [DOI] [PubMed] [Google Scholar]
- 15.Wilksch SM, O’Shea A, Ho P, Byrne S, Wade TC. The relationship between social media use and disordered eating in young adolescents. Int J Eat Disord. 2020;53:96–106. doi: 10.1002/eat.23198. [DOI] [PubMed] [Google Scholar]
- 16.Chng SC, Fassnacht DB. Parental comments: Relationship with gender, body dissatisfaction, and disordered eating in Asian young adults. Body Image. 2016;16:93–9. doi: 10.1016/j.bodyim.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Ata RN, Ludden AB, Lally MM. The effects of gender and family, and media influences on eating behaviours and body image during adolescence. J Youth Adolesc. 2007;36:1024–37. [Google Scholar]
- 18.Ministry of Trade and Industry-Department of Statistics. Availability of Selected Consumer Durables/Quinquennial. [[Last accessed on 2021 Apr 08]]. Available from: https://data.gov.sg .
- 19.de Vries DA, Peter J, de Graaf H, Nikken P. Adolescents'social network site use, peer appearance-related feedback, and body dissatisfaction: Testing a mediation model. J Youth Adolesc. 2016;45:211–24. doi: 10.1007/s10964-015-0266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fardouly J, Magson NR, Johnco CJ, Oar EL, Rapee RM. Parental control of the time preadolescents spend on social media: Links with preadolescents'social media appearance comparisons and mental health. J Youth Adolesc. 2018;47:1456–68. doi: 10.1007/s10964-018-0870-1. [DOI] [PubMed] [Google Scholar]
- 21.De La Rie SM, Van Furth EF, De Koning A, Noordenbos G, Donker MC. The quality of life of family caregivers of eating disorder patients. J Treat Prev. 2005;13:345–51. doi: 10.1080/10640260591005236. [DOI] [PubMed] [Google Scholar]
- 22.Furnham A, Manning R. Young people's theories of anorexia nervosa and obesity. Couns Psychol Q. 1997;10:389–414. [Google Scholar]
- 23.Geerling DM, Saunders SM. College students'perceptions of individuals with anorexia nervosa: Irritation and admiration. J Ment Health. 2015;24:83–7. doi: 10.3109/09638237.2014.998807. [DOI] [PubMed] [Google Scholar]
- 24.Cachelin FM, Striegel-Moore RH. Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. Int J Eat Disord. 2006;39:154–61. doi: 10.1002/eat.20213. [DOI] [PubMed] [Google Scholar]
- 25.Hart LM, Granillo MT, Jorm AF, Paxton SJ. Unmet need for treatment in the eating disorders: A systematic review of eating disorder specific treatment seeking among community cases. Clin Psychol Rev. 2011;31:727–35. doi: 10.1016/j.cpr.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Vandereycken W. Denial of illness in anorexia nervosa—A conceptual review: Part 2 different forms and meanings. Eur Eat Disord Rev. 2006;14:352–68. [Google Scholar]
- 27.Kitchener BA, Jorm AF. Mental health first aid training: Review of evaluation studies. Aust N Z J Psychiatry. 2006;40:6–8. doi: 10.1080/j.1440-1614.2006.01735.x. [DOI] [PubMed] [Google Scholar]
- 28.Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord. 1987;6:1–8. [Google Scholar]
- 29.Adair CE, Marcous GC, Cram BS, Ewashen CJ, Chafe J, Cassin SE, et al. Development and multi-site validation of a new condition-specific quality of life measure for eating disorders. Health Qual Life Outcomes. 2007;5:23. doi: 10.1186/1477-7525-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Treasure J, Russell G. The case for early intervention in anorexia nervosa: Theoretical exploration of maintaining factors. Br J Psychiatry. 2011;199:5–7. doi: 10.1192/bjp.bp.110.087585. [DOI] [PubMed] [Google Scholar]
- 31.Scharner S, Stengel A. Alterations of brain structure and functions in anorexia nervosa. Clin Nutr Exp. 2019;28:22–32. [Google Scholar]
- 32.Von HA, Pinheiro AP, Thornton LM, Klump KL, Berrettini WH, Brandt H, et al. Temporal patterns of recovery across eating disorder subtypes. Aust NZ J Psychiatry. 2008;42:108–17. doi: 10.1080/00048670701787610. [DOI] [PubMed] [Google Scholar]
- 33.Wagner A, Greer P, Bailer UK, Frank GK, Henry SE, Putnam K, et al. Normal brain tissue volumes after long-term recovery in anorexia and bulimia nervosa. Biol Psychiatry. 2006;59:291–3. doi: 10.1016/j.biopsych.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 34.Cederholm T, Jensen G, Correia M, Gonzalez M, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition –A consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9. doi: 10.1016/j.clnu.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 35.Cuerda C, Vasiloglou M, Arhip L. Nutritional management and outcomes in malnourished medical inpatients: Anorexia nervosa. J Clin Med. 2019;8:1042. doi: 10.3390/jcm8071042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.da Silva J, Seres D, Sabino K, Adams S, Berdahl G, Citty S, et al. ASPEN consensus recommendations for refeeding syndrome. Nutr Clin Pract. 2020;35:178–95. doi: 10.1002/ncp.10474. [DOI] [PubMed] [Google Scholar]
- 37.Watson HJ, Bulik CM. Update on the treatment of anorexia nervosa: Review of clinical trials, practice guidelines and emerging interventions. Psychol Med. 2012;43:2477–500. doi: 10.1017/S0033291712002620. [DOI] [PubMed] [Google Scholar]
- 38.Hilbert A, Hoek WH, Schmidt R. Evidence-based clinical guidelines for eating disorders: International comparison. Curr Opin Psychiatry. 2017;30:423–37. doi: 10.1097/YCO.0000000000000360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan LU, Ahmed J, Khan S, MacFie J. Refeeding syndrome: A literature review. Gastroenterol Res Pract. 2011;2011:410971. doi: 10.1155/2011/410971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehanna H, Moledina J, Travis J. Refeeding syndrome: What it is, and how to prevent and treat it. BMJ. 2008;336:1495–8. doi: 10.1136/bmj.a301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haynos A, Snipes C, Guarda A, Mayer L, Attia E. Comparison of standardized versus individualized caloric prescriptions in the nutritional rehabilitation of inpatients with anorexia nervosa. Int J Eat Disord. 2016;49:50–8. doi: 10.1002/eat.22469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Le Grange D, Accurso EC, Lock J, Agras S, Bryson SW. Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. Int J Eat Disord. 2014;47:124–9. doi: 10.1002/eat.22221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Connor G, Nicholls D, Hudson L, Singhal A. Refeeding low weight hospitalized adolescents with anorexia nervosa. Nutr Clin Pract. 2016;31:681–9. doi: 10.1177/0884533615627267. [DOI] [PubMed] [Google Scholar]


