Abstract
Background:
The aim of this study was to retrospectively investigate the effect of Crinone vaginal gel on pregnancy outcomes in women undergoing natural cycle (NC) frozen embryo transfer (FET) and to obtain the most suitable population for its routine application.
Methods:
The 1613 women who underwent FET in the NC regimen [including the controlled ovulation stimulation protocol for the natural cycle, or the controlled ovulation stimulation protocol for the natural cycle (NC-COS)] from 2017 to 2021 were included. All patients were divided into 2 groups including Control group and Crinone group, which administered with or without Crinone vaginal gel. The key clinical information and between the 2 groups was recorded in detail.
Results:
The results indicated that there were no statistical differences in blood β human chorionic gonadotropin (HCG) positive rate, clinical pregnancy, live birth, abortion (spontaneous and induced) and stillbirth between Control group and Crinone group. Moreover, Crinone could prevent spontaneous abortion. The spontaneous abortion rate in the Crinone group was 5.93% while this in control group was 8.32%. In the cohort exposed to Femoston, the preventive result was more significant (0/32 vs 5/15, P = .001). Furthermore, Crinone exhibited a significant protective effect on spontaneous abortion in 1520 patients who received no human menopausal gonadotropin (HMG) treatment.
Conclusion:
This study demonstrated that the Crinone could protect women against spontaneous abortion, especially in patients who do not need HMG or in combination with Femoston.
Keywords: Crinone, Femoston, frozen embryo transfer, natural cycle, spontaneous abortion
1. Introduction
It has been reported that up to 1 in 6 couples may experience fertility issues.[1,2] The use of assisted reproductive technology by couples seeking a healthy live birth is becoming increasingly common. Treatment cycles involving frozen (thawed) embryo transfer (FET) have been demonstrated to enhance cumulative pregnancy rates, reduce costs, and are relatively straightforward to perform.[3,4] Assisted reproduction has extensively utilized FET. It is primarily employed in cases where women do not conceive following fresh embryo transfer cycles, where the endometrium is unsuitable for fresh embryo transfer, or when there is a high risk of ovarian hyperstimulation syndrome. Typically, FET is conducted using various cycle regimens: spontaneous ovulatory cycles (natural cycle, NC); hormone therapy FET cycles, where the endometrium is artificially prepared using estrogen and progesterone; and cycles where ovulation is induced by medication (ovulation induction FET cycles).
FET success is influenced by the embryo, endometrial preparation, and luteal support. Both the oocyte/embryo and the maternal endometrium are crucial for achieving a successful birth. Since ovulation does not occur in the FET cycle, endogenous formation of the corpus luteum is absent. Thus, secretory transformation of the endometrium prior to embryo transfer and maintenance of normal embryonic development afterward relies entirely on exogenous progesterone supplementation. Progesterone is essential for establishing and maintaining early pregnancy until the luteal-placental transfer, offering numerous benefits to FET outcomes.[3,5,6] Even, live birth rates are not negatively impacted by the premature initiation of luteal phase progesterone support in natural FET cycles.[7] Overall, enhancing endometrial tolerance is positively affected by exogenous progesterone support, making it a recommended strategy. The most common routes for luteal phase support are via vaginal capsule (the most convenient administration), gel, or tablet. A steady endometrial concentration can be achieved by vaginal progesterone administration, while a low serum level of progesterone is caused, potentially avoiding systemic adverse effects.
One of the most widely used vaginal progesterone medications in assisted reproductive technology programs is Crinone vaginal gel (8%).[8] Studies on the efficacy and safety of Crinone in FET, as well as the most suitable population, are found to be inadequate.[9] Currently, there is less consensus on whether the administration of progesterone support affects the clinical outcome of FET cycles.[10,11] The benefits and risks associated with the routine use of Crinone vaginal gel in FET have yet to be supported by sufficient data, as conflicting findings regarding its effect on pregnancy outcomes compared to intramuscular progesterone exist.
The aim of this study was to retrospectively investigate the effect of Crinone vaginal gel on pregnancy outcomes in women undergoing natural cycle (NC) frozen embryo transfer (FET) and to obtain the most suitable population for its routine application. The results were hoped to provide some references of the application of comprehensive utilization in clinical selection of luteal support regimens.
2. Methods
2.1. Study design and participants
The whole experiment was approved by Wuxi Maternal and Child Health Hospital Ethics Committee (No. 2024-06-0515-17). The files of medical ethics approval, medical ethics review and patient informed consent were attached in the submission files.
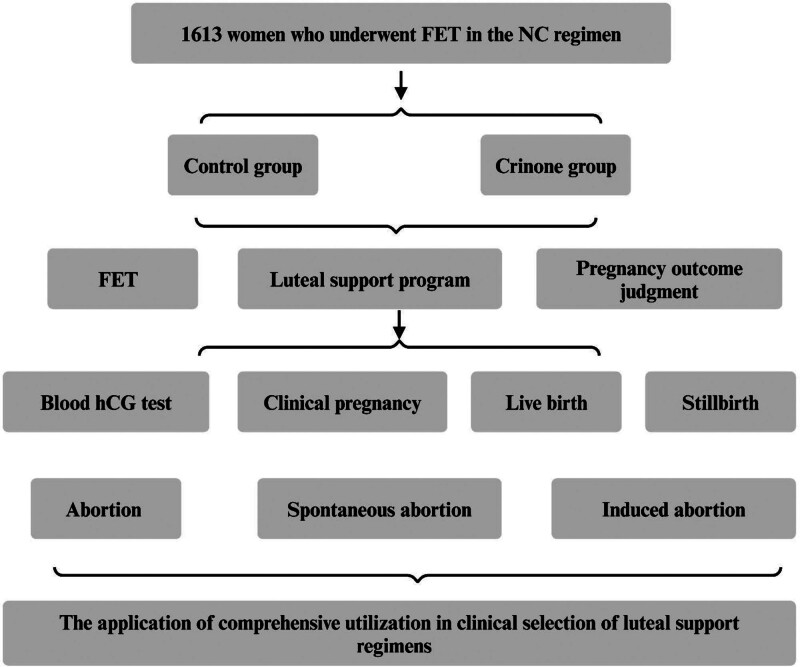
All 1613 women who underwent frozen embryo transfer (FET) for pregnancy in our Reproductive Center from 2017 to 2021 in the natural cycle (NC) regimen (including the controlled ovulation stimulation protocol for the natural cycle, or NC-COS) were retrospectively analyzed. The inclusion criteria were: patients aged between 20 and 48, and day 3 to 6 frozen embryos were used. Based on our purpose, all the enrolled patients were divided into 2 groups: the control group and the Crinone group. The Crinone group was administered to Crinone vaginal gel (Merck Serono, Switzerland, 90 mg/d), while the control group had not. The whole study was shown in Figure 1.
Figure 1.
The brief experimental plan. FET = frozen embryo transfer, HCG = human chorionic gonadotropin, NC = natural cycle.
2.2. FET study
Embryos were frozen and thawed by vitrification according to the routine procedures of the center. Embryo evaluation was performed according to the literature criteria. Follicle growth was monitored by transvaginal ultrasound from the 10th to 12th day of menstruation. If the dominant follicle diameter was ≥ 14 mm and endometrial thickness ≤ 6 mm, Fenmortone (2 mg/d, Abbott, Netherlands) was added, vaginal medication was used, and the endometrial thickness reached 8 mm or the endometrial transformation day was changed to oral administration. If the dominant follicle diameter is ≥ 16 mm, luteinizing hormone (LH), estradiol (E2) and progesterone (P) levels are measured and LH support is given from the day of ovulation or 24 hours after the LH peak (labeled as ovulation day) until 14 days after embryo transfer. Under the guidance of abdominal ultrasound, the embryo at the cleavage stage was transferred on day 3 after ovulation, and the blastocyst on day 5 after ovulation.
2.3. Luteal support program
From the day of ovulation, the control group was given progesterone injection 60 mg/d intramuscular injection, the seronotone group was given progesterone sustained-release gel 90 mg/d, vaginal medication combined with dydrogesterone tablet 20 mg/d orally, serum β-HCG was detected 12 to 14 days after transplantation, and the drug was stopped if there was no pregnancy, and continued to be used if pregnancy continued until 10 weeks of pregnancy. Discontinue medication if there are indications that pregnancy cannot continue.
2.4. Pregnancy outcome judgment
Serum β-HCG was measured 12 to 14 days after embryo transfer, and if β-HCG < 5 U/L was defined as no pregnancy; β-HCG ≥ 5 U/L was defined as HCG positive, and vaginal ultrasound was performed 25 to 30 days after transplantation. The pregnancy was biochemical if β-HCG was positive in blood or urine and there was no echo of pregnancy sac under vaginal ultrasound. Intrauterine pregnancy sac or fluid product and extrauterine tissue villi were clinically pregnant. If the gestational age is <28 weeks and the pregnancy is terminated, it is an abortion (including natural abortion and artificial abortion); Gestational age ≥ 28 weeks delivered with heartbeat, breathing is a live birth, vice versa for stillbirth.
The detailed arrangement between Control group and Crinone group was as follows: patient age, the husband’s age, NC regimen (NC or NC-COS), medications used in addition to Crinone (including Progynova, Femoston, progesterone injection, dydrogesterone, HCG and HMG), the FET date, endometrial thickness, endometrial type, and the embryo grade. The following outcome indicators were used to analyze the differences between groups: biochemical pregnancy indicated by the blood HCG test result on day 12 post FET, clinical pregnancy (the vaginal ultrasound examination revealed a fetal sac in the uterus with a germ and primitive heartbeat) or not, live birth or not, abortion (including spontaneous abortion and induced abortion during the late pregnancy), and stillbirth or not.
2.5. Data measurement
The main outcome measures observed are blood HCG test, clinical pregnancy, live birth, abortion, spontaneous abortion, induced abortion and stillbirth.
Blood HCG test = number of HCG positive cycles/total number of transfer cycles × 100%
Clinical pregnancy = clinical pregnancy cycle/total number of transfer cycles × 100%
Abortion = number of abortion cycles within 28 weeks of pregnancy/total clinical pregnancy cycles × 100%
Spontaneous abortion = spontaneous abortion cycles/number of clinical pregnancy cycles × 100%
Stillbirth = stillbirth cycles/number of live birth cycles × 100%
2.6. Statistical methods
The data were analyzed by SPSS (version 25). Categorical data were described by percentages and compared by χ2 test (double checked by Fisher’s exact test when necessary); numeric variables were expressed as mean ± standard deviation (SD) and compared by t test (between 2 groups). A P value <.05 was regarded as statistically significant.
3. Results
3.1. General information of enrolled subjects
Together, this retrospective study analyzed the records of 1613 cases, including 685 ones in the control group and 928 ones in the Crinone group (Table 1). Between 2 groups, there were no differences in the age of the patient, the age of the husband, the pregnancy protocol, the endometrial thickness, and endometrial type. The average ages were both around 32 in 2 groups. In the control group, 5.98% cases received the NC-COS protocol, and 4.85% received the NC-COS protocol in the Crinone group (P > .05). The endometrial thickness was about 10 mm in both groups. Additionally, 93.4% (640/685) had the B type endometrium in the control group, and this ratio was 92.8% (861/928; P > .05).
Table 1.
Clinical characteristics of included women.
| Variables | Control group | Crinone group | P | |
|---|---|---|---|---|
| Number | 685 | 928 | ||
| Age | 32.16 ± 4.708 | 31.96 ± 4.308 | .383 | |
| Age of husband | 33.45 ± 5.331 | 33.36 ± 5.369 | .741 | |
| Pregnancy regimen | NC | 644 (94.0%) | 883 (95.2%) | .315 |
| NC-COS | 41 (6.0%) | 45 (4.8%) | ||
| Endometrial thickness (mm) | 10.117 ± 1.8089 | 10.000 ± 1.6571 | .181 | |
| Endometrial type | A | 45 (6.6%) | 67 (7.2%) | .611 |
| B | 640 (93.4%) | 861 (92.8%) |
NC = natural cycle, NC-COS = the controlled ovulation stimulation protocol for the natural cycle.
3.2. Effect of Crinone on pregnancy outcomes
Overall, no statistical differences were observed between 2 groups in the blood HCG test, clinical pregnancy, live birth, abortion (spontaneous abortion and induced abortion), and stillbirth (Table 2). However, Crinone could prevent spontaneous abortion, that the spontaneous abortion percentage in the Crinone group was 5.93% in comparison with 8.32% in the control group (P = .061 by χ2 test, and P = .039 by Fisher’s exact test).
Table 2.
Pregnancy outcomes of 2 groups.
| Outcomes | Control group | Crinone group | P | |||
|---|---|---|---|---|---|---|
| Blood HCG test | Negative | 236 | 35.2% | 330 | 36.1% | .706 |
| Positive | 434 | 64.8% | 583 | 63.9% | ||
| Clinical pregnancy | Fail | 338 | 49.3% | 454 | 48.9% | .867 |
| Success | 347 | 50.7% | 474 | 51.1% | ||
| Live birth | No | 405 | 59.1% | 525 | 56.6% | .305 |
| Yes | 280 | 40.9% | 403 | 43.4% | ||
| Abortion | No | 626 | 91.4% | 868 | 93.5% | .103 |
| Yes | 59 | 8.6% | 60 | 6.5% | ||
| Spontaneous abortion | No | 628 | 91.7% | 873 | 94.1% | .061* |
| Yes | 57 | 8.3% | 55 | 5.9% | ||
| Induced abortion | No | 683 | 99.7% | 923 | 99.5% | .456 |
| Yes | 2 | 0.3% | 5 | 0.5% | ||
| Stillbirth | No | 683 | 99.7% | 927 | 99.9% | .396 |
| Yes | 2 | 0.3% | 1 | 0.1% | ||
HCG = human chorionic gonadotophin.
In Fisher’s exact test, P = .039.
Moreover, the subgroups in the patients under NC and NC-COS regimens, respectively were analyzed. In the NC regimen (Table 3), the preventive effect of Crinone on spontaneous abortion was statistically significant (P = .045 by χ2 test, and P = .0329 by Fisher’s exact test), and no impacts on other outcomes were found. And this influence was not observed in patients under the NC-COS protocol (Table 4, P > .05 in all outcomes).
Table 3.
Pregnancy outcomes of 2 groups in the NC regimen.
| Outcomes | Control group | Crinone group | P | |||
|---|---|---|---|---|---|---|
| Blood HCG test | Negative | 225 | 35.7% | 314 | 36.2% | .854 |
| Positive | 405 | 64.3% | 554 | 63.8% | ||
| Clinical pregnancy | Fail | 317 | 49.2% | 434 | 49.2% | .978 |
| Success | 327 | 50.8% | 449 | 50.8% | ||
| Live birth | No | 382 | 59.3% | 502 | 56.9% | .335 |
| Yes | 262 | 40.7% | 381 | 43.1% | ||
| Abortion | No | 587 | 91.1% | 826 | 93.5% | .079 |
| Yes | 57 | 8.9% | 57 | 6.5% | ||
| Spontaneous abortion | No | 589 | 91.5% | 831 | 94.1% | .045* |
| Yes | 55 | 8.5% | 52 | 5.9% | ||
| Induced abortion | No | 642 | 99.7% | 878 | 99.4% | .465 |
| Yes | 2 | 0.3% | 5 | 0.6% | ||
| Stillbirth | No | 642 | 99.7% | 882 | 99.9% | .390 |
| Yes | 2 | 0.3% | 1 | 0.1% | ||
NC = natural cycle.
In Fisher’s exact test, P = .029.
Table 4.
Pregnancy outcomes of 2 groups in the NC-COS protocol.
| Outcomes | Control group | Crinone group | P | |||
|---|---|---|---|---|---|---|
| Blood HCG test | Negative | 11 | 27.5% | 16 | 35.6% | .426 |
| Positive | 29 | 72.5% | 29 | 64.4% | ||
| Clinical pregnancy | Fail | 21 | 51.2% | 20 | 44.4% | .530 |
| Success | 20 | 48.8% | 25 | 55.6% | ||
| Live birth | No | 23 | 56.1% | 23 | 51.1% | .643 |
| Yes | 18 | 43.9% | 22 | 48.9% | ||
| Abortion | No | 39 | 95.1% | 42 | 93.3% | .723 |
| Yes | 2 | 4.9% | 3 | 6.7% | ||
| Spontaneous abortion | No | 39 | 95.1% | 42 | 93.3% | .723 |
| Yes | 2 | 4.9% | 3 | 6.7% | ||
| Induced abortion | No | 41 | 100% | 45 | 100% | – |
| Yes | 0 | 0 | 0 | 0 | ||
| Stillbirth | No | 41 | 100% | 45 | 100% | – |
| Yes | 0 | 0 | 0 | 0 | ||
HCG = human chorionic gonadotophin, NC-COS = the controlled ovulation stimulation protocol for the natural cycle.
Further, whether Crinone still palyed a role in preventing spontaneous abortion in each treatment subgroup were analyzed. Patients were stratified according to different drugs and different embryonic grades, and no differences were detected in most stratification. However, in the cohort with Femoston treatment (Table 5), a dramatically strong effect was found (0/32 vs 5/15, P = .001). Moreover, 1520 patients among the 1613 cases had not received HMG treatment. In these patients, the protective effect of Crinone on spontaneous abortion was able to manifest (P = .040, Table 5).
Table 5.
Crinone prevents spontaneous abortion for women with Femoston treatment and those without progesterone injection.
| Cohort | Control group | Crinone group | P | |
|---|---|---|---|---|
| Femoston treatment | No Spontaneous abortion | 12 (70.6%) | 32 (100%) | .001 |
| Spontaneous abortion | 5 (29.4%) | 0 (0%) | ||
| Without HMG | No Spontaneous abortion | 583 (91.4%) | 830 (94.1%) | .040 |
| Spontaneous abortion | 55 (8.6%) | 52 (5.9%) |
HMG = human menopausal gonadotropin.
4. Discussion
The use of Crinone vaginal gel for luteal support has been reported by scholars. Comparative studies used following controls: without usage, Utrogestan capsules, aqueous subcutaneous progesterone (Prolutex), or intramuscular progesterone injection.[12–17] Our results are similar to majority of conclusions, that Crinone gel results in comparable pregnant outcomes vs controls, such as biochemical pregnancy,[13] clinical pregnancy,[15,18] live birth,[13] spontaneous abortion, implantation, and miscarriage rates.[14] When acknowledging that Crinone vaginal gel is equally effective to intramuscular progesterone, some studies also implied that it is better tolerated for luteal phase support.[19] However, there are some studies that suggest its safety risks. A study has investigated Crinone vaginal gel for luteal phase support for day 3 cryopreserved embryo transfer, and they reported that women supplemented with Crinone had significantly lower rates of clinical pregnancy (36.9% vs 51.1%) and live birth (24.4% vs 39.1%) compared with those on intramuscular progesterone.[20] In comparison with Prolutex, Crinone has fewer side effects, that patients receiving Prolutex complained of more local pain at the injection sites.[17]
Our study shows that Crinone has no effect on biochemical and clinical pregnancies, but slightly reduces the rate of spontaneous abortions, especially in the NC regimen, in patients who do not require HMG or in combination with Femoston. However, unlike previous studies, oral Utrogest capsules or intramuscular progesterone injection were not compared, but the use of vaginal gel with or without. Notably, Crinone also had no effect on pregnancy outcome in both subgroups that received progesterone injections and those that did not. This suggests that, although generally it is safe and perhaps available as a routine protocol, the additional administration of a vaginal gel does not provide more benefits from progesterone. Nevertheless, in Table 5, it was observed that Crinone prevents spontaneous abortion for women with Femoston treatment and those without HMG injection. These 2 populations may be the key contributors to the overall significant differences. Femoston is a hormone replacement therapy (HRT) preparation. Generally, it is used to relieve symptoms of the menopause, and it is the second-line option for preventing osteoporosis in postmenopausal women who are at high risk of fractures and cannot take other medicines licensed for preventing osteoporosis. Here, it is used in assisted reproduction for the preparation of the endometrium for FET and also for the prevention of early-pregnancy and preterm abortion. It is routinely administered orally but also can be used as a vaginal plug for endometrial preparation, which effectively increases the local estrogen level. A Chinese study showed that, for patients with thin endometrium, Femoston may be added vaginally if ideal endometrial thickness or E2 level is not achieved by Progynova alone.[21] In patients receiving Femoston treatment, Crinone exerted a highly significant protective effect against spontaneous abortion, which suggests that Crinone may act synergistically with Femoston locally and improve the endometrial receptivity. However, the above hypothesis has to be confirmed by further data accumulation. Besides, the protective role of Crinone is significant in patients without HMG treatment, and this effect was nor detected in the patients receiving HMG treatment. HMG (human menopausal gonadotropin) is a urinary sex hormone with components containing follicle-stimulating hormone and luteinizing hormone. Injection of HMG is aimed at the development of follicles and induction of secreting estrogen which drives the endometrial proliferation. HMG can promote the simultaneous development and maturation of follicles, which can result in a higher number of good quality eggs for embryos, therefore, it is commonly used by women with underdeveloped follicles.[22–24] In the late follicular phase, using HMG alone may be a feasible alternative for normal-ovulatory women undergoing FET.[25] The protective effect of Crinone against spontaneous abortion is more sufficient for patients without HMG treatment, and this finding suggests that in patients with normal follicular maturation function, improving the environment of the endometrium with Crinone can indeed bring benefits in assisted reproduction. In summary, on account of its mild protective effect against spontaneous abortion, as well as a high safety, Crinone may be a promising routine drug in FET, especially in patients who do not require HMG or in combination with Femoston.
Our study still has the following shortcomings. Firstly, as a retrospective study, its reliability remains to be verified by prospective experiments. Secondly, some positive statistical findings were on the margin of significance, and they were also validated post hoc by logistic regression, but the efficacy was found to be weak. Therefore, the previous consensus that the protective effect of Crinone was considered very limited remained unchallenged by the above findings.
5. Conclusions
Overall, Crinone showed good effect on pregnancy outcomes. But it protected woman from spontaneous abortion, especially in patients who did not require HMG or in combination with Femoston.
Acknowledgments
This study is based on data from the Clinical Practice Research Datalink obtained under license from the Wuxi Maternity and Child Health Care Hospital. However, the interpretation and conclusions contained in this study are those of the authors alone. This data reused with the permission of the Wuxi Maternity and Child Health Care Hospital. All rights reserved.
Author contributions
Conceptualization: Meiling Weng.
Data curation: Fang Xiong, Jie Chen.
Formal analysis: Meiling Weng.
Investigation: Lishuang Xu, Fang Xiong, Jie Chen.
Methodology: Lishuang Xu.
Project administration: Meiling Weng.
Resources: Xin Jin, Huiming Zeng.
Software: Lishuang Xu.
Supervision: Meiling Weng.
Validation: Meiling Weng.
Writing – original draft: Xin Jin, Huiming Zeng.
Abbreviations:
- FET
- frozen embryo transfer
- HCG
- human chorionic gonadotropin
- HMG
- human menopausal gonadotropin
- LH
- luteinizing hormone
- NC
- natural cycle
- NC-COS
- the controlled ovulation stimulation protocol for the natural cycle.
Financial support for this research was provided by National Natural Science Foundation of China (No. 82271686).
The informed consent was signed by each enrolled patient.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Xu L, Xiong F, Chen J, Jin X, Zeng H, Weng M. Clinical efficacy of Crinone on pregnancy outcomes in frozen embryo transfer: A retrospective study in the Chinese population. Medicine 2024;103:46(e40453).
LX and FX contributed to this article equally.
Contributor Information
Lishuang Xu, Email: 18762461524@163.com.
Fang Xiong, Email: xiongfang58@163.com.
Jie Chen, Email: swcjza@163.com.
Xin Jin, Email: Aganjin@163.com.
Huiming Zeng, Email: zhmkillern520@163.com.
References
- [1].Farquhar C, Marjoribanks J. Assisted reproductive technology: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2018;8:CD010537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. International Committee for Monitoring Assisted Reproductive Technology. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–4. [DOI] [PubMed] [Google Scholar]
- [3].Devine K, Richter KS, Jahandideh S, Widra EA, McKeeby JL. Intramuscular progesterone optimizes live birth from programmed frozen embryo transfer: a randomized clinical trial. Fertil Steril. 2021;116:633–43. [DOI] [PubMed] [Google Scholar]
- [4].Casper RF, Yanushpolsky EH. Optimal endometrial preparation for frozen embryo transfer cycles: window of implantation and progesterone support. Fertil Steril. 2016;105:867–72. [DOI] [PubMed] [Google Scholar]
- [5].Rahmani E, Rahsepar M, Eftekhar M. Effect of progesterone supplementation on natural frozen-thawed embryo transfer cycles: a randomized controlled trial. Int J Fertil Steril. 2013;7:13–20. [PMC free article] [PubMed] [Google Scholar]
- [6].Nasser LF, Sa Filho MF, Reis EL, et al. Exogenous progesterone enhances ova and embryo quality following superstimulation of the first follicular wave in Nelore (Bos indicus) donors. Theriogenology. 2011;76:320–7. [DOI] [PubMed] [Google Scholar]
- [7].Jiang WJ, Sun ZG, Song JY. Premature timing of progesterone luteal phase support initiation did not negatively impact live birth rates in modified natural frozen thawed embryo transfer cycles. Heliyon. 2023;9:e13218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chantilis SJ, Zeitoun KM, Patel SI, Johns DA, Mcintire DD. Use of Crinone vaginal progesterone gel for luteal support in in vitro fertilization cycles. Fertil Steril. 1999;72:823–9. [DOI] [PubMed] [Google Scholar]
- [9].Gleicher N, Wang Y, He Y, et al. Crinone gel for luteal phase support in frozen-thawed embryo transfer cycles: a prospective randomized clinical trial in the chinese population. PLoS One. 2015;10:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Liu Y, Wu Y. Progesterone intramuscularly or vaginally administration may not change live birth rate or neonatal outcomes in artificial frozen-thawed embryo transfer cycles. Front Endocrinol. 2020;11:539427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shiba R, Kinutani M, Okano SH, et al. Serum progesterone levels with the use of four different types of vaginal progesterone in frozen-thawed embryo transfer cycles and related pregnancy outcomes. Int J Fertil Steril. 2021;15:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chang SP. Comparison of Crinone 8% intravaginal gel and intramuscular progesterone for luteal support in in vitro fertilization. J Chin Med Assoc. 2008;71:381–5. [DOI] [PubMed] [Google Scholar]
- [13].Bakkensen JB, Racowsky C, Thomas AM, Lanes A, Hornstein MD. Intramuscular progesterone versus 8% Crinone vaginal gel for luteal phase support following blastocyst cryopreserved single embryo transfer: a retrospective cohort study. Fertil Res Pract. 2020;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jobanputra K, Toner J, Denoncourt R, Gibbons W. Crinone 8% (90 mg) given once daily for progesterone replacement therapy in donor egg cycles. Fertil Steril. 1999;72:980–4. [DOI] [PubMed] [Google Scholar]
- [15].Ludwig M, Schwartz P, Babahan B, Katalinic A, Diedrich K. Luteal phase support using either Crinone 8% or Utrogest: results of a prospective, randomized study. Eur J Obstet Gynecol Reproduct Biol. 2002;103:48–52. [DOI] [PubMed] [Google Scholar]
- [16].Simunic V, Tomic V, Tomic J, Nizic D. Comparative study of the efficacy and tolerability of two vaginal progesterone formulations, Crinone 8% gel and Utrogestan capsules, used for luteal support. Fertil Steril. 2007;87:83–7. [DOI] [PubMed] [Google Scholar]
- [17].Kao T-C, Tu Y-A, Yang P-K, et al. Clinical use of aqueous subcutaneous progesterone compared with vaginal progesterone as luteal support in in vitro fertilization: a randomized controlled study in Taiwan. Taiwan J Obstet Gynecol. 2022;61:863–7. [DOI] [PubMed] [Google Scholar]
- [18].Child T, Leonard SA, Evans JS, Lass A. Systematic review of the clinical efficacy of vaginal progesterone for luteal phase support in assisted reproductive technology cycles. Reprod Biomed Online. 2018;36:630–45. [DOI] [PubMed] [Google Scholar]
- [19].Yanushpolsky E, Hurwitz S, Greenberg L, Racowsky C, Hornstein M. Crinone vaginal gel is equally effective and better tolerated than intramuscular progesterone for luteal phase support in in vitro fertilization–embryo transfer cycles: a prospective randomized study. Fertil Steril. 2010;94:2596–9. [DOI] [PubMed] [Google Scholar]
- [20].Kaser DJ, Ginsburg ES, Missmer SA, Correia KF, Racowsky C. Intramuscular progesterone versus 8% Crinone vaginal gel for luteal phase support for day 3 cryopreserved embryo transfer. Fertil Steril. 2012;98:1464–9. [DOI] [PubMed] [Google Scholar]
- [21].Xu W, Zhou F, Li C, Jin XY, Zhang SY. Application of Femoston in hormone replacement treatment-frozen embryo transfer and its clinical outcomes. Zhonghua yi xue za zhi. 2013;93:3766. [PubMed] [Google Scholar]
- [22].Ghobara T, Gelbaya TA, Ayeleke RO. Cycle regimens for frozen-thawed embryo transfer. Cochrane Database Syst Rev. 2017;7:CD003414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Barriere P, Procu-Buisson G, Avril C, Hamamah S; AME study group. Added value of anti-Mullerian hormone serum concentration in assisted reproduction clinical practice using highly purified human menopausal gonadotropin (HP-hMG). J Gynecol Obstet Human Reprod. 2022;51:102289. [DOI] [PubMed] [Google Scholar]
- [24].Zhu X, Ye J, Fu Y, Ai A, Kuang Y. The effect of human chorionic gonadotrophin contained in human menopausal gonadotropin on the clinical outcomes during progestin-primed ovarian stimulation. Oncotarget. 2017;8:87340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Zhu X, Fu Y. Evaluation of ovarian stimulation initiated from the late follicular phase using human menopausal gonadotropin alone in normal-ovulatory women for treatment of infertility: a retrospective cohort study. Front Endocrinol. 2019;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]