Abstract
The presence of patients who leave without being seen (LWBS) by a physician in the emergency department (ED) is an essential indicator of the accessibility and quality of healthcare delivery. A high LWBS rate implies low patient satisfaction. This study aims to analyze the prevalence and characteristics of LWBS patients in Türkiye and their ED readmission rate within 3 days. This retrospective, single-center, observational study was conducted in the ED of a Turkish tertiary university hospital. It looked at patients who left without being evaluated by a physician admitted to the ED between June 01, 2021, and June 01, 2023. Data on age, gender, residential area, health insurance status, ED readmission within 3 days, complaints, and hospitalization were obtained through the hospital’s electronic record system. The prevalence of LWBS patients was 0.43%. Only 0.6% (n = 5) of LWBS patients had no health insurance. About 12.8% (n = 99) of them were 65 years and older. About 10.2% (n = 79) of LWBS patients were readmitted to the ED within 72 hours. The most common reason for readmission was musculoskeletal system complaints. Statistically, ED readmission was significantly more common in older adults (P = .05). Older LWBS patients are more likely hospitalized upon return visits to the ED (P = .014). LWBS patients are both a result and a consequence of ED crowding. A zero LWBS rate is crucial for older adults’ health as they may fall victim to an invisible accident while avoiding ED traffic. Prioritizing older adults and reorganizing waiting areas can reduce ED crowding and cost burden due to delayed treatments.
Keywords: emergency department, health insurance, leave without being seen, older adults
1. Introduction
In the increasingly busy emergency department (ED) environment, addressing the issue of patients who leave without being seen (LWBS) by a doctor is crucial. LWBS rates are a data showing the accessibility of emergency services and the quality of the service provided. High LWBS rates indicate low patient satisfaction.[1,2] ED crowding and prolonged waiting durations are the most critical factors that may cause people to leave early. Uncomfortable waiting areas, worsening of the patient’s complaints during the waiting process to the extent that they can no longer wait, or getting better to the extent that they no longer want to stay are also seen as a reason for patients to LWBS.[3,4] A study with 8 years of patient data reported that LWBS rates increased yearly.[5]
When patients LWBS, the diagnosis of possible disorders are delayed, treatment becomes more challenging due to this delay, and the risk of mortality and morbidity increases. Delays in diagnosis and treatment will increase the cost to the patient’s healthcare system in terms of the money spent and the labor force used. One study showed that 11% of LWBS patients needed inpatient treatment within 1 week, and some of these patients were operated on.[6]
Patients admitted to the ED with lower severity symptoms may not suffer from delayed diagnosis or treatment when they LWBS, but these patients cause ED crowding and prolonged waiting times for other patients with repeated ED visits due to the same complaint.[1] High LWBS rates are both the cause and the consequence of ED crowding.
Although there are many studies on discharge against medical advice in the literature,[7,8] studies on the characteristics of LWBS patients and their adverse effects on ED functionality have remained limited. To our knowledge, studies have yet to be conducted on patients who left without being seen by a doctor in Türkiye.
Our study aimed to explore the prevalence of patients who leave the ED without being seen, understand their characteristics, and evaluate whether they revisited the ED within 3 days, which could indicate a need for improved care or follow-up.
2. Methods
2.1. Study setting and design
This study is retrospective, single-center, and observational. It was conducted in the ED of a tertiary university hospital in Turkiye, with approximately 100,000 admissions per year. After local ethics committee approval (Düzce University Non-Invasive Health Research Ethics Committee, approval id 2023/95, dated July 10, 2023) was obtained, all patients aged 18 and over who visited the ED between June 01, 2021, and June 01, 2023 but left the ED without being evaluated by a physician after their urgency was determined in the triage area were identified and included in the study.
In the ED where the study was conducted, at least 4 emergency medicine assistants and 1 emergency medicine specialist work together continuously in each shift, and a 3-color triage scale is applied for patients. Patients are given the appropriate triage code, which is green (nonurgent), yellow (urgent), or red (emergent). Triage is performed by a nurse trained in triage management, and those coded as yellow/red are immediately taken to the relevant area accompanied by paramedics. Patients with a green triage code are given documents with their vital signs, complaints, and short medical history and directed to the waiting room. The patients’ data are recorded into the computer system by the physician during the examination.
2.2. Selection of participants and study protocol
Data regarding the patient’s age, gender, ED admission day, admission time, province of residence, health insurance status, and whether or not they were admitted to the ED within 3 days were obtained through the hospital’s electronic patient record system and ED archive records. Information regarding their revisits was also noted among the patients who left the hospital without being evaluated by a physician and returned to the ED within 3 days.
After finding the total number of ED visits that resulted in LWBS (n = 806), it was determined how many different patients had these visits (n = 772). Descriptive statistical characteristics of LWBS patients were revealed. The patients were divided into 2 groups: those readmitted to the ED within 3 days and those not. The patient groups were compared regarding the characteristics screened in the study. Patients were divided into 3 shift groups according to their admission time: 00.01 to 08.00 was called shift1, 08.01 to 16.00 was called shift2, and 16.01–00.00 was called shift3.
2.3. Statistical analysis
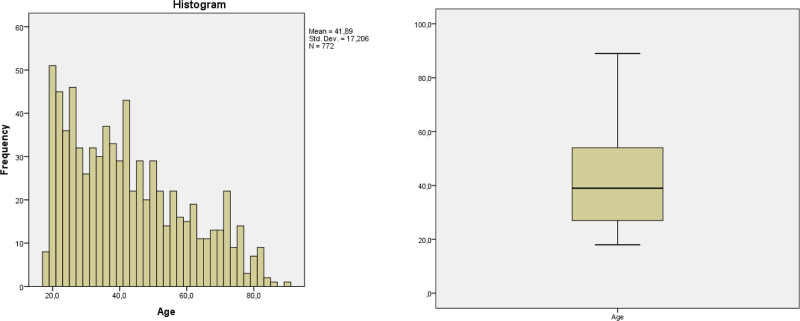
Continuous variables were summarized as median, 25th, and 75th percentile, and categorical variables were summarized as frequency and percentage. Conformity to normal distribution was evaluated by the Shapiro–Wilk test and histogram. Logarithmic transformation was applied in order to apply parametric tests with age data that did not conform to normal distribution. Since the data obtained as a result of logarithmic transformation did not conform to normal distribution, age, which is a continuous data in the study, was evaluated with nonparametric tests (Mann–Whitney U test). Pearson chi-square test or Fisher exact test analyzed the relationship between 2 categorical variables. Statistical software SPSS version 23 (SPSS Inc., Armonk, NY) was used for these analyses. The significance level was determined as P < .05. Bonferroni correction was applied to the P-value in comparative statistical tests performed with more than 2 groups.
3. Results
During the 2 years of the study, 188,313 patients aged 18 years and older visited the ED, and 806 of these visits resulted in LWBS (0.43% of total ED visits). It was determined that 772 different people made these 806 visits. The median (25% to 75%) age of the patients was 39 years (27–54), and 54.1% (n = 418) were female. 12.8% (n = 99) of the patients were 65 years and older. Distrubution of age values are shown at Figure 1. It was observed that 10.2% (n = 79) of the patients were readmitted to the ED within 72 hours after LWBS. During the 2 years, 1 patient had LWBS 6 times, 1 patient had LWBS 3 times, and 27 patients had LWBS 2 times, but none of the patients with recurrent LWBS presented to the ED within 72 hours. The first admissions of patients with multiple LWBS admissions were included in the study.
Figure 1.
Histogram and box-blot analyzes of age data.
We observed that 76.3% of the patients presented to the ED on weekdays. 5.8% (n = 45) of LWBS patients admitted during shift1, 36.1% (n = 279) during shift2 and 58% (n = 448) during shift3. We noticed that 76% (n = 587) of the LWBS patients lived in the centrum, where the study was conducted, and the other patients were from other cities. Among the LWBS patients, 47.4% (n = 366) lived in cities, 20.1% (n = 155) in districts, and 32.5% (n = 251) in villages. 89.4% (n = 694) of the patients had health insurance covered by the National Social Security Institution (SSI), 9.5% (n = 73) had general health insurance (GHI) organized by the state or private health insurance provided by insurance companies, and 0.6% (n = 5) had no health insurance (Table 1).
Table 1.
Characteristics of left without being seen patients.
| Features | 100% (n = 772) |
|---|---|
| Age, yr | 39 (27.0, 27–54) (18–89) |
| Age group | |
| ≥65 yrs | 12.8% (n = 99) |
| <65 yrs | 87.2% (n = 673) |
| Gender | |
| Female | 54.1% (n = 418) |
| Male | 45.9% (n = 354) |
| Admission day | |
| Weekday | 76.3% (n = 589) |
| Weekend | 23.7% (n = 183) |
| Admission shift | |
| Shift1 (00.01–08.00) | 5.8% (n = 45) |
| Shift2 (08.01–16.00) | 36.1% (n = 279) |
| Shift3 (16.01–00.00) | 58% (n = 448) |
| Readmission in 72 h | |
| No | 89.8% (n = 693) |
| Yes | 10.2% (n = 79) |
| City of residence | |
| In-province | 76% (n = 587) |
| Another province | 24% (n = 185) |
| Residential unit | |
| Town center | 47.4% (n = 366) |
| District | 20.1% (n = 155) |
| Villiage | 32.5% (n = 251) |
| Health insurance | |
| National Social Security Institution | 89.4% (n = 694) |
| Other | 9.5% (n = 73) |
| No | 0.6% (n = 5) |
Values presented as % (n) or median (interquartile range, 25th–75th) [min–max].
The most common reason for admission of LWBS patients to the ED within 3 days was musculoskeletal system complaints, with 20.3% (n = 16). Respiratory system complaints, with 17.7% (n = 14), and cardiovascular system complaints, with 15.2%, were the other common reasons for admission (Table 2).
Table 2.
Complaints of patients returning to the emergency department within 72 h.
| Reason of Admission | 100% (n = 79) |
|---|---|
| Musculoskeletal System Complaints | 20.3% (n = 16) |
| Respiratory System Complaints | 17.7% (n = 14) |
| Cardiovascular System Complaints | 15.2% (n = 12) |
| Gastrointestinal System Complaints | 12.7% (n = 10) |
| Complaints caused by infection | 8.9% (n = 7) |
| Urinary System Complaints | 7.6% (n = 6) |
| Gynaecological and Obstetric Complaints | 7.6% (n = 6) |
| Complaints Related to Malignancies | 6.3% (n = 5) |
| Central Nervous System Complaints | 2.5% (n = 2) |
| Psychiatric Complaints | 1.3% (n = 1) |
LWBS patients were divided into 2 groups according to their readmission to the ED within 3 days. Patients aged 65 years and older were statistically significantly more in the group with readmission (P = .05). No statistically significant difference was found between the groups regarding other parameters (Table 3).
Table 3.
Comparing patients’ characteristics who returned to the ED within 72 hours to those who did not.
| Characteristics | Return-visiting patients (n = 693) | Patients who did not revisit (n = 79) | P |
|---|---|---|---|
| Age, yr | 39 (26.0, 27–53) [18–89] | 41 (28.0, 28–56) [19–82] | .44 |
| Gender | |||
| Female | 54.7% (n = 379) | 49.4% (n = 36) | .36 |
| Male | 45.3% (n = 314) | 50.6% (n = 43) | |
| Age group | |||
| ≥65 years | 12% (n = 83) | 20.3% (n = 16) | .03 |
| <65 years | 88% (n = 610) | 79.7% (n = 63) | |
| Admission day | |||
| Weekday | 76.3% (n = 529) | 75.9% (n = 60) | .91 |
| Weekend | 23.7% (n = 164) | 24.1% (n = 19) | |
| Admission shift | |||
| Shift1 (00.01–08.00) | 5.9% (n = 41) | 5.1% (n = 4) | .93 |
| Shift2 (08.01–16.00) | 36.2% (n = 251) | 35.4% (n = 28) | |
| Shift3 (16.01–00.00) | 57.9% (n = 401) | 59.5% (n47) | |
| City of residence | |||
| Within the province | 76.5% (n = 524) | 79.7% (n = 63) | .41 |
| Another province | 24.4% (n = 169) | 20.3% (n = 16) | |
| Residential unit | |||
| Town center | 48.3% (n = 335) | 39.2% (n = 31) | .10 |
| District | 20.3% (n = 141) | 17.7% (n = 14) | |
| Villiage | 31.3% (n = 217) | 43.1% (n = 34) | |
| Health insurance | |||
| National Social Security Intuition | 89.3% (n = 619) | 94.9% (n = 75) | .27 |
| Other | 10% (n = 69) | 5.1% (n = 4) | |
| No | 0.7% (n = 5) | 0% (n = 0) | |
Values presented as % (n) or median (interquartile range, 25th-75th) [min-max]. Bold values indicate statistically significant results having P < .05.
It was found that 88.6% (n = 70) of the patients who were returned to the ED within 3 days after LWBS were discharged with recommendations after the examination in the ED, and 11.4% (n = 9) were hospitalized in the wards. None of the readmissions resulted in surgery, intensive care hospitalization, or death. Older patients (above 65 years of age) were significantly more likely to be readmitted as inpatients than as discharged patients (P = .014).
LWBS patients were divided into 3 shift groups according to the time of admission. Statistically significant differences between the shift groups and age groups were found. Patients admitted in shift 1 were statistically significantly younger than the other 2 groups (P = .016). The proportion of patients who were 65 or older was statistically significantly higher in shift 2 compared to the other 2 groups (P = .016) (Table 4).
Table 4.
Comparison of the LWBS patients’ characteristics by emergency visit hours.
| Characteristics | Shift 1 (n = 45) to 08.00 |
Shift 2 (n = 279) 08.01 to 16.00 |
Shift 3 (n = 448) 16.01 to 00.00 |
P |
|---|---|---|---|---|
| Age, yr | 33 (20.0, 25–45) [18–79]* | 42 (29.0, 31–60) [18–89]** | 38 (26.0, 26–52) [18–83]** | .001 |
| Gender | ||||
| Female | 46.7% (n = 21) | 53.4% (n = 149) | 55.4% (n = 248) | .51 |
| Male | 53.3% (n = 24) | 46.6% (n = 130) | 44.6% (n = 200) | |
| Age group | ||||
| ≥65 yrs | 6.7% (n = 3)* | 17.9% (n = 50)** | 10.3% (n = 46)* | .005 |
| <65 yrs | 93.3% (n = 42) | 82.1% (n = 229) | 89.7% (n = 402) | |
| Admission day | ||||
| Weekday | 75.6% (n = 34) | 78.5% (n = 219) | 75.0% (n = 336) | .55 |
| Weekend | 24.4% (n = 11) | 21.5% (n = 60) | 25.0% (n = 112) | |
| City of residence | ||||
| In-province | 82.2% (n = 37) | 78.1% (n = 218) | 74.1% (n = 332) | .28 |
| Another province | 17.8% (n = 8) | 21.9% (n = 61) | 25.9% (n = 116) | |
| Residential unit | ||||
| Town center | 37.8% (n = 17) | 48.4% (n = 135) | 47.8% (n = 214) | .69 |
| District | 22.2% (n = 10) | 20.8% (n = 58) | 19.4% (n = 87) | |
| Villiage | 40% (n = 18) | 30.8% (n = 86) | 32.8% (n = 147) | |
| Health insurance | ||||
| National Social Security Institution | 91.1% (n = 41) | 91.0% (n = 254) | 89.1% (n = 399) | .61 |
| Other | 8.9% (n = 4) | 7.9% (n = 22) | 10.5% (n = 47) | |
| No | 0.0% (n = 0) | 1.1% (n = 3) | 0.4% (n = 2) | |
Values presented as % (n) or median (interquartile range, 25th-75th) [min-max].
Bold values indicate statistically significant results having P < .016 when comparing triple groups with double groups.
Different numbers of asterisks indicate statistically significant difference.
4. Discussion
Previous studies on LWBS patients showed that the population was relatively young, predominantly female, had a low triage grade, and was mainly admitted in the evening or at night.[1,2,5,9,10] The patients in our study have a similar profile. This may be because young people usually visit EDs with complaints of lower severity that can be postponed. When the literature is analyzed, ED crowding and prolonged waiting times are the most common causes of LWBS. In our study, the median (25% to 75%) age of the LWBS population was 39 (27–54) years, the age range in which the general population is employed in the daytime and tired in the evening and night hours. Studies conducted in Türkiye have reported that the highest number of patient admissions to EDs is between 16.00 and 00.00 hours.[11–13] Our study observed that most of the patients’ LWBS in shift 3, i.e., between 16.01 and 00.00, It can be said that frequent visits cause ED crowding, ED crowding causes prolonged waiting times, and long waiting times cause young adults who are tired of labor to postpone the complaints that lead them to admit to ED.
Patients in shift group 1 (00.01–08.00) were younger, while shift group 2 (08.00–16.00) had a higher rate of patients over 65. The fact that the transportation options to the hospital change according to the hours, that older adults cannot drive, and that the public transport vehicles to be used for returning to their homes, especially for patients coming from districts and villages, are at certain hours, cause older adults to be unable to wait until late hours. The higher rate of patients with LWBS in shift 2 being over 65 compared to other groups may be due to the patient’s efforts to return home on time. The fact that those who applied in the Shift1 group and subsequently LWBS were younger than the other 2 groups can be explained by the fact that ED admissions for reasons such as alcohol or substance use, fighting, and psychiatric problems are generally made at night and by young people. Low-severity complaints usually cause these admissions and may result in LWBS.
Türkiye, the country where the study was conducted, is a social state. With the ongoing state policies, it is desired that all people living in the country benefit from health services equally. Everyone who is employed in Türkiye is obliged to have health insurance. SSI is the state institution that provides most health and pension insurance in the country. Employees are insured by their employers with 1 of the systems called SSK, Bağ-kur, and Emekli Sandiği according to the work and institution of employment. Although there are some technical differences between them, each person in all 3 of these systems benefits from the health services provided by the state free of charge and is granted a pension when they complete the required prepayment period. Individuals can also optionally purchase insurance from private companies. The GHI system, which provides coverage of health expenses in case of need by paying 3% of the minimum wage in force monthly, is available for everyone living in the country and is compulsory for Turkish citizens. In our study, it was observed that only 0.6% (n = 5) of LWBS patients did not have any health insurance. People with health insurance are not charged additional fees for any emergency health service. It can be easily said that for Türkiye, the rate of LWBS is not related to health insurance, thanks to the compulsory GSS for the country’s citizens, the low number of people without health insurance, and the social state facilities. In studies conducted in the United States of America (USA), a country that is not governed by social state principles, it has been seen that people with health insurance with low payment coverage have LWBS more frequently.[2,5,14]
In studies in the literature, LWBS rates are shown to range between 0.85% and 15%.[15–17] Our study is the first on LWBS patients in Türkiye, and the LWBS rate was found to be 0.43%. This rate is below the values shown in the literature. A low LWBS rate is a positive indicator of the quality and inclusiveness of the health system. The existing health insurance systems also contribute to this ratio. In 2021, the number of visits to EDs in the USA was 139.8 million, and the admission rate per patient was 0.46. In 2017, Türkiye’s annual ED admissions per patient was 1.31.[18–20] It is also an important indicator that the rate of LWBS is much lower in Türkiye, even though the annual ED admission rate per capita in Türkiye is 3 times higher than in the USA.
LWBS patients will likely readmit to the ED because of their ongoing complaints. A study showed that 24.4% of LWBS patients were readmitted to the ED within 72 hours.[1] In various studies in the literature, it has been shown that the rate of readmission to the ED within 48 hours in LWBS patients is higher than in non-LWBS patients.[21–24] In our study, 10.2% (n = 79) of LWBS patients admitted to the ED again within 72 hours. Previous studies showed that LWBS patients mostly admitted with musculoskeletal and gastrointestinal system complaints.[2,4,6,11] Since patients with green triage codes, who were given triage documents and directed to the waiting room, took their documents with them when they LWBS, there is no information about the complaints of LWBS patients in our study. Within 72 hours, musculoskeletal complaints were the most common reason for readmission to the ED. In another study in which the admitting complaints of LWBS patients who were readmitted to the ED within 72 hours were analyzed, the most common reasons for readmission were gastrointestinal complaints and pain due to trauma.[1] Readmissions within 72 hours are likely to be related to the reason for the previous admission. It is conceivable that patients admitted with relatively postponable complaints such as musculoskeletal system pain may leave the ED despite these complaints as a result of prolonged waiting times or various other reasons. Frequent reasons for readmission in the literature are gastrointestinal complaints and pain, which are also partially postponable complaints. The fact that readmissions are usually made with complaints of low severity indicates that the rate of LWBS may be lower in patients with severe complaints.
Older adults who returned within 72 hours after leaving without being seen had a significantly higher readmission rate than those who didn’t. Patients aged 65 years and older are more likely to admit to the ED with critical medical conditions requiring treatment compared to younger patients. If elderly and sick people spend long periods in uncomfortable ED waiting rooms, they are likely to feel worse than they did at the time of admission. Even if older patients leave the ED because of fatigue or deterioration in their current condition, they are likely to admit again with the same medical condition. The medical condition not intervened at the first admission will worsen in time, the treatment will become more complex, and the cost of treatment will increase. In our study, the rate of being over 65 years of age those who were readmitted and hospitalized within 72 hours was statistically significantly higher than those who were discharged. Factors that cause older people to become LWBS need to be investigated. The measures to be taken should aim to prevent this vulnerable group from leaving the hospital without treatment. Delayed treatment will lead to possible poor outcomes, prolonged treatment times and increased burden on the health system.
The first limitation of our study is that it is retrospective. Due to the retrospective design of the study, patients could not be asked valuable questions that could be used in the study and the data to be obtained could not be used in the study. However, in the light of the data that could be obtained, a window was opened to LWBS, a subject that had not been examined before in Türkiye. Prospective studies should be conducted on LWBS, patients should be asked with which complaint they came with, how long they waited, for which reason they left the hospital and what their requirements were during the waiting process. Studies to be conducted with these data obtained from patients in real time will provide a better understanding of the problem of LWBS. The second limitation is that it is a single-center study, which limits the generalizability of the results. Our study is the first study on LWBS in Türkiye and our findings give an idea about the situation in the country. Türkiye is a socio-economically heterogeneous country with significant differences in terms of development between eastern and western cities. It may not be correct to generalize the findings of our study conducted in a single hospital in a single city to the whole country. In order to better understand the LWBS issue in Türkiye and to reach more accurate results, multicentre studies should be conducted with hospitals in cities with different socioeconomic levels. The third limitation is that although the study population was large, the rate of LWBS was low. This may affect the reliability of statistical tests. As the fourth limitation, since patient complaints were written on the triage form rather than on the computer by the nurse during the triage phase and the patients left without handing these forms to the doctor, the complaints of LWBS patients could not be reached. The fifth limitation of the study is that the reason for the patients leaving the hospital without being seen by the physician could not be included in the study. Since most of the patients in the study had an outdated admission time and the patients or their relatives thought that they would not remember the reason for leaving, the reason for LWBS was not enquired by telephone. Prospective design of future studies on LWBS will prevent these problems. As the sixth limitation, mean or standard deviation values could not be obtained because the continuous data obtained in the study did not fit the normal distribution. The only continuous data in our study was patient age. Shapiro–Wilk test and histogram evaluation of the age data showed that they did not conform to normal distribution. In order to perform parametric tests, logarithmic equivalents of the age values were found and Shapiro–Wilk test and histogram evaluation were performed again with these values. Since normal distribution was not found in this evaluation, the study was continued with non parametric tests. The seventh limitation is that the study did not include information such as socioeconomic status, special medical needs and waiting times of the patients. These data are also among those that were intended to be used in the study but could not be accessed. The cause of LWBS varies from person to person. Different people will react differently to the same problem. The time that passes after LWBS may cause patients to think differently about the issue that forced them to leave the hospital. LWBS, which is largely caused by negative personal experiences, will be better understood with prospective studies to be conducted by real-time communication with patients.
5. Conclusion
LWBS patients are both the result and the cause of ED crowding. In the study, the LWBS prevalence was 0.43%. Older LWBS patients have higher probabilities of 3-day ED readmission than younger patients. In the age group of 65 years and older, the hospitalization rate at readmissions is higher.
Author contributions
Conceptualization: Erdinç Şengüldür, Mehmet Cihat Demir.
Data curation: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki, Emre Erdem, Hatice Güldal.
Formal analysis: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Investigation: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki, Emre Erdem, Hatice Güldal.
Methodology: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Project administration: Mehmet Cihat Demir.
Resources: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Software: Erdinç Şengüldür, Kudret Selki.
Supervision: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Visualization: Erdinç Şengüldür.
Writing – original draft: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Writing – review & editing: Erdinç Şengüldür, Mehmet Cihat Demir, Kudret Selki.
Abbreviations:
- ED
- emergency department
- GHI
- general health insurance
- LWBS
- leave without being seen
- SSI
- National Social Security Institution
- USA
- United States of America
The authors have no funding and conflicts of interest to disclose.
After obtaining ethical approval, the data were collected retrospectively by examining the Hospital Data Processing System and Archive records. The need for signed informed consent was waived due to the retrospective design of the study.
This study was initiated in the emergency department of a university hospital following the ethics committee approval (Düzce University Non-Invasive Health Research Ethics Committee’s approval with decision number 2023/95, July 10, 2023). The address of the institution where the study was performed: Düzce University, School of Medicine, Düzce, Türkiye.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
How to cite this article: Şengüldür E, Demir MC, Selki K, Erdem E, Güldal H. Characteristics of patients leaving the emergency department without being seen by a doctor: The first report from Türkiye. Medicine 2024;103:46(e40543).
No human rights were violated during this study and the study was in accordance with the Declaration of Helsinki.
References
- [1].Roby N, Smith H, Hurdelbrink J, et al. Characteristics and retention of emergency department patients who left without being seen (LWBS). Intern Emerg Med. 2022;17:551–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Pham JC, Ho GK, Hill PM, McCarthy ML, Pronovost PJ. National study of patient, visit, and hospital characteristics associated with leaving an emergency department without being seen: predicting LWBS. Acad Emerg Med. 2009;16:949–55. [DOI] [PubMed] [Google Scholar]
- [3].Rowe BH, Channan P, Bullard M, et al. Characteristics of patients who leave emergency departments without being seen. Acad Emerg Med. 2006;13:848–52. [DOI] [PubMed] [Google Scholar]
- [4].Weiss SJ, Ernst AA, Derlet R, King R, Bair A, Nick TG. Relationship between the National ED Overcrowding Scale and the number of patients who leave without being seen in an academic ED. Am J Emerg Med. 2005;23:288–94. [DOI] [PubMed] [Google Scholar]
- [5].Sun BC, Binstadt ES, Pelletier A, Camargo CA. Characteristics and temporal trends of “left before being seen” visits in US emergency departments, 1995-2002. J Emerg Med. 2007;32:211–5. [DOI] [PubMed] [Google Scholar]
- [6].Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician. Causes and consequences. JAMA. 1991;266:1085–90. [PubMed] [Google Scholar]
- [7].Demir MC, Ağaçkiran I, Özdamar Y, Boğan M. The pandemic’s effect on discharge against medical advice from the emergency department. J Surg Med. 2021;5:433–8. [Google Scholar]
- [8].Tuffuor K, Su H, Meng L, et al. Inequities among patient placement in emergency department hallway treatment spaces. Am J Emerg Med. 2023;76:70–4. [DOI] [PubMed] [Google Scholar]
- [9].Chiu DT, Stenson BA, Alghamdi M, Antkowiak PS, Sanchez LD. The association between day of arrival, time of arrival, daily volume and the rate of patients that “left without being seen”. Am J Emerg Med. 2023;67:24–8. [DOI] [PubMed] [Google Scholar]
- [10].Rathlev NK, Visintainer P, Schmidt J, Hettler J, Albert V, Li H. Patient characteristics and clinical process predictors of patients leaving without being seen from the emergency department. West J Emerg Med. 2020;21:1218–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Liu S, Nie H, Huang W, et al. Characteristics of patients who leave the emergency department without being seen: the first report in China. Emerg Med Australas. 2014;26:243–8. [DOI] [PubMed] [Google Scholar]
- [12].Sert ET, Mutlu H, Yeşildağ K, et al. 5-year analysis of patients admitted to our emergency department. Med J Mugla Sitki Kocman Univ. 2021;8:1–4. [Google Scholar]
- [13].Serinken M, Türkcüer I, Özen M, Uyanik E, Elicabuk H, Karsli E. A retrospective analysis of patients who visited the emergency department and left by their own choice in a university hospital. J Acad Emerg Med. 2013;12:126–9. [Google Scholar]
- [14].Sheraton M, Gooch C, Kashyap R. Patients leaving without being seen from the emergency department: a prediction model using machine learning on a nationwide database. J Am Coll Emerg Physicians Open. 2020;1:1684–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Clarey AJ, Cooke MW. Patients who leave emergency departments without being seen: literature review and English data analysis. Emerg Med J. 2012;29:617–21. [DOI] [PubMed] [Google Scholar]
- [16].Arendt KW, Sadosty AT, Weaver AL, Brent CR, Boie ET. The left-without-being-seen patients: what would keep them from leaving? Ann Emerg Med. 2003;42:317–23. [DOI] [PubMed] [Google Scholar]
- [17].Kelen GD, Scheulen JJ, Hill PM. Effect of an emergency department (ED) managed acute care unit on ED overcrowding and emergency medical services diversion. Acad Emerg Med. 2001;8:1095–100. [DOI] [PubMed] [Google Scholar]
- [18].Dundar C, Yaylaoglu SD. Non-emergent care visits in a Turkish tertiary care emergency department after 2008 health policy changes: review and analysis. Arch Public Health. 2022;80:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2021 Emergency Department Summary Tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2021-nhamcs-ed-web-tables-508.pdf.
- [20].Şengüldür E, Selki K, Tuncer C, Demir MC. Emergency department neurosurgical consultations in a tertiary care hospital. Konuralp Tip Dergisi. 2023;15:412–6. [Google Scholar]
- [21].Kennedy M, MacBean CE, Brand C, Sundararajan V, McD Taylor D. Review article: leaving the emergency department without being seen. Emerg Med Australas. 2008;20:306–13. [DOI] [PubMed] [Google Scholar]
- [22].Hitti E, Hadid D, Tamim H, Al Hariri M, El Sayed M. Left without being seen in a hybrid point of service collection model emergency department. Am J Emerg Med. 2020;38:497–502. [DOI] [PubMed] [Google Scholar]
- [23].Fraser J, Atkinson P, Gedmintas A, Howlett M, McCloskey R, French J. A comparative study of patient characteristics, opinions, and outcomes, for patients who leave the emergency department before medical assessment. CJEM. 2017;19:347–54. [DOI] [PubMed] [Google Scholar]
- [24].Tropea J, Sundararajan V, Gorelik A, Kennedy M, Cameron P, Brand CA. Patients who leave without being seen in emergency departments: an analysis of predictive factors and outcomes. Acad Emerg Med. 2012;19:439–47. [DOI] [PubMed] [Google Scholar]