Abstract
Background
With an increasing demand for critical care expertise and limitations in intensivist availability, innovative staffing models, such as the utilization of advanced practice providers (APPs), have emerged.
Objectives
The purpose of the study was to compare patient outcomes between APP and housestaff teams in the cardiac intensive care unit (CICU).
Methods
This retrospective study, spanning March 2022 to July 2023, compares patient characteristics and outcomes between two CICU teams embedded in the same CICU at a large urban academic hospital: one staffed by housestaff and the other by APPs (80% physician assistants, 20% nurse practitioners) who each had approximately 1 to 2 years of experience in the CICU. The primary outcome was CICU mortality. Multivariable Cox regression analyses and Kaplan-Meier curves were used to assess the primary outcome.
Results
A total of 1,620 admissions were analyzed: 1,013 patients on the housestaff service and 607 patients on the APP service. There were no significant differences in patient demographics, admitting diagnoses, use of vasoactive medications, inotropes, or mechanical circulatory support. There was no difference in CICU mortality (8.4% vs 8.2%, adjusted hazard ratio 0.73; 95% CI: 0.51-1.05; P = 0.10), in-hospital mortality (13.5% vs 13.8%, aHR 0.82; 95% CI: 0.62-1.08; P = 0.17), or in-hospital length of stay between the housestaff and APP teams. Patients managed by the housestaff team had a lower CICU length of stay (2 days IQR: 1-4 days] vs 3 days [IQR: 1-5 days], P = 0.047). Fellowship rotation scores (based on surveys completed by the cardiology fellows) of the CICU also improved after the implementation of the APP-based team (3.87 ± 0.14 before vs 4.61 ± 0.06 after, P < 0.0001).
Conclusions
Our moderately sized study demonstrated no difference in CICU or in-hospital mortality between patients managed by a housestaff team versus those managed by an APP team.
Key words: advanced, housestaff, intensive care unit, provider
Central Illustration
The cardiac intensive care unit (CICU) has undergone a substantial transformation since the first coronary care unit was created by Desmond Julian in the 1960s.1 Initially designed to monitor patients exclusively after myocardial infarction, the contemporary CICU now manages critically ill cardiac patients with a spectrum of conditions, ranging from complex cardiovascular disease to respiratory failure, renal failure, sepsis, multiorgan dysfunction, and end-of-life issues.1, 2, 3 Such diagnoses have increased in parallel with the use of critical care therapies and procedures, including bronchoscopy, invasive hemodynamic monitoring, renal replacement therapy, and mechanical circulatory support.2, 3, 4, 5, 6 This increasing complexity and acuity has prompted the development of critical care cardiology as a rapidly evolving specialty to provide optimal care to these patients.7
Globally, institutions and professional societies have responded to the emerging field of critical care cardiology by developing formal training programs and educational pathways to prepare practitioners for roles in CICUs.8, 9, 10 Still, many institutions face a supply-demand mismatch as growing CICU patient volume and complexity outpace the supply of clinicians with the necessary expertise to practice effectively in the CICU setting, resulting in staffing shortages.11, 12, 13 In academic centers, the rotation of trainees through CICUs provides valuable learning opportunities while supporting CICU staffing, but is limited by challenges such as the fixed complements of residents and fellows in accredited programs, work hour regulations, and varying levels of experience and scope of practice.14 These “growing pains” have forced the development of novel staffing models, including the integration of APPs, including nurse practitioners and physician assistants, into routine CICU operations.1,15
The integration of APPs in the intensive care setting has proven instrumental in addressing staffing demands while varying widely in operational approaches. Although APPs have been part of the health care workforce since the 1960s, their utilization as primary providers in the intensive care unit (ICU) is a relatively recent development that has rapidly expanded.16 However, despite the increasing integration of APPs into the critical care workforce, this has been predominantly in general ICUs. Studies examining outcomes in CICUs staffed by APPs have been sparse, with prior publications focusing largely on the medical intensive care unit (MICU).16,17 Therefore, our study aims to assess the implementation of the APP-staffing model by comparing patient outcomes between the traditional housestaff-based model and the newly implemented APP-based CICU team in an American Heart Association Level 1 CICU.2
Methods
Study Design and Setting
We conducted a retrospective analysis using data collected from consecutive patients admitted to the Bellevue Hospital CICU, a Level 1 CICU within our tertiary care academic medical center. Bellevue Hospital serves as the safety-net hospital for advanced cardiovascular care in New York City's Health and Hospitals system, the largest public hospital network in the United States. In response to the growing patient acuity, complexity, and census, our institution implemented a second CICU team staffed with APPs, in addition to the original CICU team comprising of housestaff. Data were collected after the implementation of the APP-based team from March 2022 to July 2023. Although the inception of the APP team was in January 2022, we intentionally did not examine the first 2 months of data to allow for an operational adjustment period. This study was approved by the Institutional Review Board of NYU Langone Health. The data that support the findings of this study are available on reasonable request from the corresponding author.
Team Composition and Staffing Structure
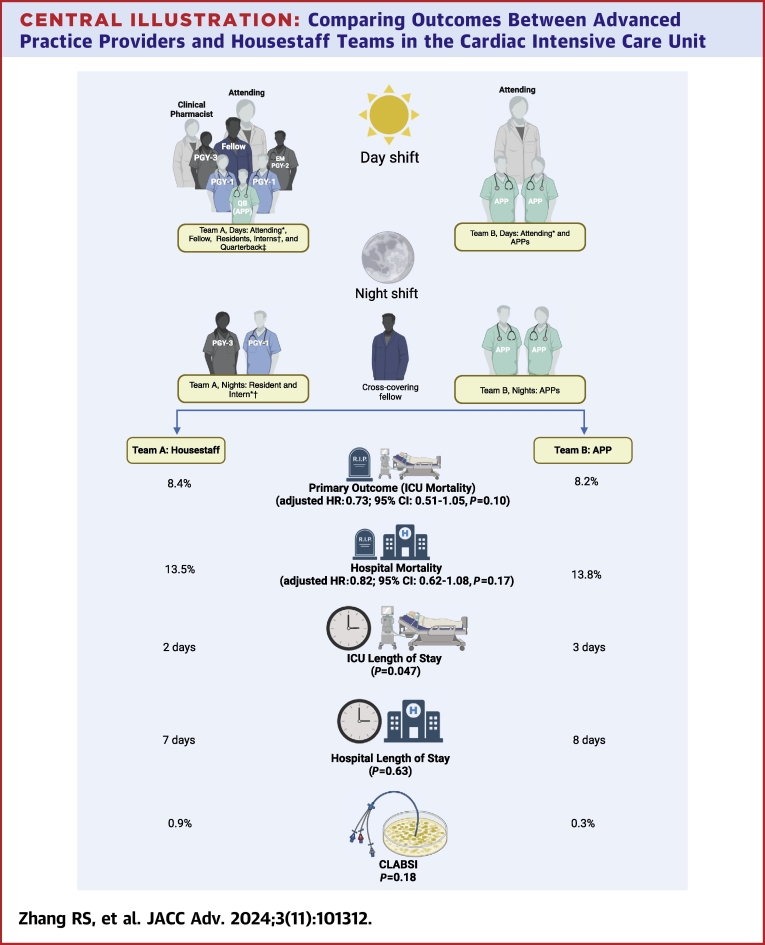
During the daytime, the housestaff team comprised 2 interns, 1 to 2 internal medicine residents (postgraduate year 3 [PGY-3]), one emergency medicine resident (PGY-2), a cardiology fellow (rotating every 2-4 weeks), and a cardiology attending (Central Illustration). The interns included a combination of categorical and preliminary internal medicine trainees. A clinical pharmacist actively participated in daily rounds with the housestaff team on weekdays and provided guidance on pharmacy-related matters for both teams. Additionally, a designated APP, known as the “quarterback,” was assigned to the housestaff team to orient trainees, assist in the daily workflow and allocation of new admissions to either team, as well as facilitate transfers into and out of the CICU, working closely with nursing and the admitting office. The role of the “quarterback” existed prior to the study period. The housestaff typically rotated through the CICU in 2 to 4-week periods. Nighttime coverage on the housestaff service included one internal medicine resident (PGY-3) and one intern (PGY-1) with an in-house cardiology fellow with coverage duties across 2 hospitals. In our model, the CICU-attending physician took an overnight call from home without in-house cardiology attending coverage overnight.
Central Illustration.
Comparing Outcomes Between Advanced Practice Providers and Housestaff Teams in the Cardiac Intensive Care Unit
Illustration of team dynamics within the cardiac intensive care unit, highlighting the distinctive compositions of housestaff and advanced practice provider (APP) services, and showcasing the associated outcomes for each team. ∗At least one attending is a dual-certified Critical Care Cardiologist. †Includes categorical and preliminary interns. ‡APP on the housestaff team who allocated new admissions and facilitated bed transfers. CLASBI = central line-associated bloodstream infection; ICU = intensive care unit. Created with BioRender.com.
The APP team was staffed by 2 APPs for both day and night shifts and a supervising cardiology attending who was not in-house at night but available by phone. The APPs consulted the cardiology fellow at any time for emergencies, including activation of the cardiac catheterization laboratory, urgent echocardiography, device interrogations, etc.
The majority of the APPs were hired immediately following graduation or with minimal previous experience (<18 months). Most APPs had accrued 1 to 2 years of CICU experience within the same unit by the time 2 distinct teams were implemented, and 80% of the APPs were physician assistants and the remaining 20% were nurse practitioners. All APPs participated in an on-boarding program upon commencing their roles in our CICU, which consisted of a 10- to 12-week program of formal CICU training with 2 to 3 senior APPs as preceptors. Continuing education and professional development consist of daily academic rounds with the board-certified cardiologist on-service, hands-on simulation training, and monthly APP-led lectures.
On any given rotation, each team had a separate cardiology attending. One of the 2 CICU attendings was a critical care cardiologist with dual training and board certification in cardiology and critical care medicine. This specialist played a crucial role in managing critical care conditions, including airway issues and mechanical ventilation (MV), as well as addressing multisystem organ dysfunction, across both teams. The rounding structures were similar between the 2 teams, with the exception of the aforementioned personnel differences. The standard nurse-to-patient ratio was 2 patients per nurse.
Decisions regarding patient triage to specific teams were made by consensus between the cardiology fellow and the quarterback APP. Notably, there were no formal guidelines for triaging patients, and decisions were generally based on team availability and an equitable distribution of acuity. Both teams could accept admissions 24 hours a day with no changes in the distribution of admissions on the weekends. During triaging of admissions, the APP quarterback took into consideration a cap of a maximum of 15 patients for the housestaff team census according to regulations established by the CICU, as well as the by the internal medicine and cardiovascular medicine training program leadership. The APP-based team had a soft census cap of 8, with a census that generally varied between 6 and 8 patients. Patients admitted to a particular team and subsequently transferred between units (eg, inpatient floor, MICU) were categorized according to their initial admission team, and their outcomes were analyzed based on an intention-to-treat approach according to the initial team. In our institution, extracorporeal membrane oxygenation (ECMO) patients are managed by a dedicated APP in conjunction with one of the CICU teams, and thus were excluded from the analysis.
Study Outcomes
Data encompassing patient characteristics, such as age, sex, race, CICU admitting diagnosis, vasoactive medication requirement, MV, pulmonary artery catheter, mechanical circulatory support (MCS), as well as in-hospital and CICU mortality, were compared between groups. The primary outcome was all-cause mortality in the CICU. Secondary outcomes included all-cause in-hospital mortality, CICU length of stay (LOS), in-hospital LOS, and health care-associated infections, including central line-associated blood stream infection and catheter-associated urinary tract infection. Data abstractors were blinded to the study hypothesis to reduce ascertainment bias. We also examined the effect of adding a second CICU team on trainee satisfaction and educational experience. This was done by comparing anonymous rotation evaluation scores across five domains, which cardiology fellows ranked on a scale of 1 to 5 (1 = very dissatisfied, 5 = very satisfied), both before and after the study period.
Statistical Analyses
Continuous variables are presented as mean ± SD or median IQR for skewed data, while categorical data are expressed as frequency and proportions. Student’s t-test was utilized to compare paired continuous variables when assumptions were met for normal distribution, and the Wilcoxon signed-rank test was used when normal distributions were not present. Categorical variables were compared using chi-square test or Fisher exact test.
To examine the relationship between the 2 teams and CICU all-cause mortality, a Kaplan-Meier curve was constructed for the 2 groups. The log rank test was used to compare survival between the 2 groups. The relationship between the 2 teams and CICU all-cause mortality at follow-up was assessed using a Cox proportional hazards model and adjusted for covariates based off of clinical rationale and prior studies,3 and included age, sex, race, ejection fraction (at presentation), admitting diagnosis of cardiogenic shock or ST-segment elevation myocardial infarction, and needing mechanical circulatory support (percutaneous left ventricular assist device or intra-aortic balloon pump) or renal replacement therapy within 48 hours of admission to the CICU. Schoenfeld residuals were employed to test the proportional hazard assumption of the Cox model. Similar models were developed to examine the relationship between the 2 teams and in-hospital all-cause mortality. All tests were considered significant at a 2-sided alpha level <0.05. All analyses were performed using Stata software (StataCorp 18 LP).
Results
There were a total of 1,639 CICU admissions recorded between March 2022 and July 2023. Nineteen patients who were on ECMO were excluded from the analysis, resulting in a final sample size of 1,620 patients. Of these, 1,013 were admitted to the housestaff team, and 607 patients were admitted to the APP team. There was no difference between the housestaff vs APP teams with regard to patient demographic and clinical characteristics, including age (62.9 ± 15.3 years vs 63.8 ± 14.9 years, P = 0.24), male (62.8% vs 67.4%, P = 0.061), race, body mass index (26.9 ± 6.9 kg/m2 vs 27.3 ± 7.3 kg/m2, P = 0.22), and ejection fraction (44.2% ± 19.9% vs 44.2% ± 19.9%, P = 0.96) (Table 1). In addition, there were no differences in the use of MV, pulmonary artery catheter, percutaneous left ventricular assist device, dialysis, cardiac arrest, targeted temperature management, presence of any shock on arrival, and use of inotropes and vasopressors (Table 1).
Table 1.
Baseline Characteristics
| House Staff (n = 1,013) | Advanced Practice Provider (n = 607) | P Value | |
|---|---|---|---|
| Age, y | 62.9 ± 15.3 | 63.8 ± 14.9 | 0.24 |
| Male | 636 (62.8%) | 409 (67.4%) | 0.061 |
| Race | 0.68 | ||
| Black | 434 (42.8%) | 258 (42.5%) | |
| White | 114 (11.3%) | 67 (11.0%) | |
| Hispanic or Latino | 265 (26.2%) | 166 (27.3%) | |
| Asian | 75 (7.4%) | 33 (5.4%) | |
| Other | 98 (9.7%) | 63 (10.4%) | |
| Unknown | 27 (2.7%) | 20 (3.3%) | |
| BMI, kg/m2 | 26.9 ± 6.9 | 27.3 ± 7.3 | 0.22 |
| Ejection fraction, % | 44.2 ± 19.9 | 44.2 ± 19.9 | 0.96 |
| Mechanical ventilation | 211 (20.8%) | 120 (19.8%) | 0.61 |
| Invasive PA catheter | 167 (16.5%) | 107 (17.6%) | 0.55 |
| Impella | 14 (1.4%) | 6 (1.0%) | 0.49 |
| IABP | 47 (4.6%) | 30 (4.9%) | 0.78 |
| Dialysis | 91 (9.0%) | 61 (10.0%) | 0.48 |
| Cardiac arrest | 94 (9.3%) | 52 (8.6%) | 0.63 |
| Targeted temperature management | 46 (4.5%) | 25 (4.1%) | 0.69 |
| Shock | 220 (21.7%) | 145 (23.9%) | 0.31 |
| Pressor or Inotrope | 293 (28.9%) | 170 (28.0%) | 0.69 |
| Norepinephrine | 256 (25.3%) | 144 (23.7%) | 0.48 |
| Vasopressin | 150 (14.8%) | 89 (14.7%) | 0.94 |
| Dobutamine | 172 (17.0%) | 103 (17.0%) | 1.00 |
| Milrinone | 44 (4.3%) | 19 (3.1%) | 0.22 |
Values are mean ± SD or n (%).
BMI = body mass index; IABP = intra-aortic balloon pump; LVAD = left ventricular assist device; PA = pulmonary artery.
There was no difference in the admitting diagnoses for patients managed by the housestaff team vs APP teams, including ST-segment elevation myocardial infarction (14.6% vs 15%, P = 0.83), cardiogenic shock (11% vs 10.9%, P = 0.88), cardiac arrest (5.5% vs 5.1%, P = 0.78), ventricular arrythmias (3.3% vs 2.5%, P = 0.31), and others (Table 2).
Table 2.
Admitting Diagnosis to the Cardiac Intensive Care Unit
| House Staff (n = 1,013) | Advanced Practice Provider (n = 607) | P Value | |
|---|---|---|---|
| STEMI | 148 (14.6%) | 91 (15.0%) | 0.83 |
| NSTEMI/UA | 211 (20.8%) | 142 (23.4%) | 0.21 |
| Cardiogenic shock | 111 (11.0%) | 66 (10.9%) | 0.88 |
| Hypertensive emergency | 22 (2.2%) | 16 (2.6%) | 0.30 |
| Decompensated heart failure | 108 (10.7%) | 72 (11.9%) | 0.49 |
| Cardiac arrest | 56 (5.5%) | 31 (5.1%) | 0.78 |
| Tamponade/pericardial effusion | 53 (5.2%) | 25 (4.1%) | 0.48 |
| Mixed/undifferentiated shock | 4 (0.4%) | 3 (0.5%) | 0.63 |
| Septic shock | 3 (0.3%) | 1 (0.2%) | 0.68 |
| Ventricular arrhythmias | 33 (3.3%) | 15 (2.5%) | 0.31 |
| Atrial arrhythmias | 40 (3.9%) | 30 (4.9%) | 0.69 |
| Bradyarrhythmia | 78 (7.7%) | 46 (7.6%) | 0.48 |
| Postprocedure monitoring/complication | 69 (6.8%) | 33 (5.4%) | 0.94 |
| Endocarditis | 37 (3.7%) | 17 (2.8%) | 0.22 |
| Pulmonary embolism | 5 (0.5%) | 5 (0.8%) | 0.96 |
| Acute aortopathy | 4 (0.4%) | 4 (0.7%) | 0.61 |
| Miscellaneous | 31 (3.1%) | 10 (1.6%) | 0.08 |
Values are n (%).
NSTEMI = non-ST-segment elevation myocardial infarction; STEMI = ST-elevation myocardial infarction; UA = unstable angina.
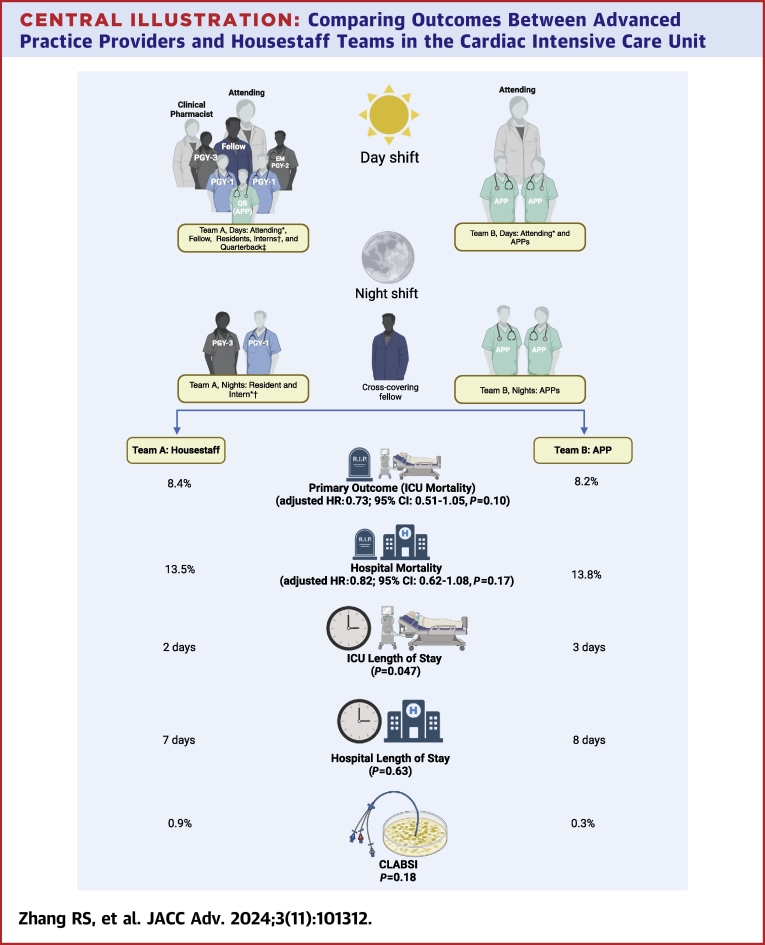
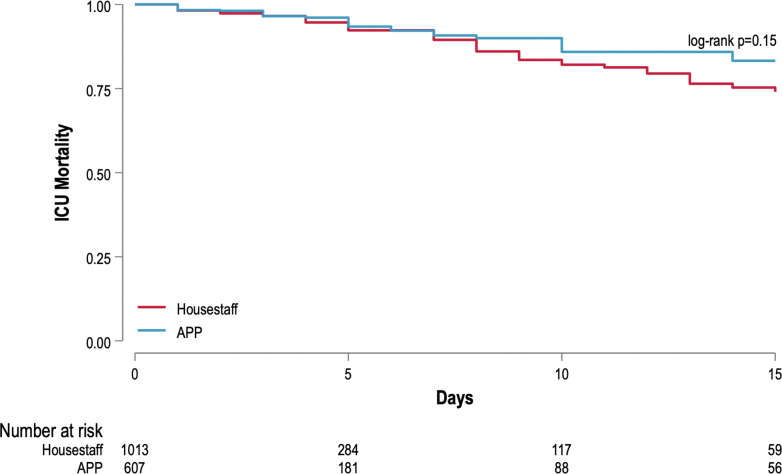
Of the 1,620 patients admitted to the CICU, there were a total of 135 (8.3%) deaths in the CICU and an additional 221 (13.6%) deaths in the hospital after transfer from the CICU. There was no difference in primary outcome of CICU mortality between the housestaff and APP teams (8.4% vs 8.2%, log-rank P = 0.15; adjusted HR: 0.73; 95% CI: 0.51-1.05; P = 0.10) (Figure 1, Table 3). There was also no difference in in-hospital mortality between the 2 teams (13.5% vs 13.8%, log-rank P = 0.62; adjusted HR: 0.82; 95% CI: 0.62-1.08; P = 0.17) (Figure 2). After adjusting for covariates, variables associated with CICU mortality were age (adjusted HR: 1.02; 95% CI: 1.01-1.03; P = 0.001) and need for renal replacement therapy (adjusted HR: 1.51; 95% CI: 1.02-2.26; P = 0.039) (Table 4). Variables associated with in-hospital mortality were age (adjusted HR: 1.02; 95% CI: 1.01-1.03; P < 0.001), need for mechanical circulatory support (adjusted HR: 1.74; 95% CI: 1.17-2.60; P = 0.006), need for renal replacement therapy (adjusted HR: 1.69; 95% CI: 1.24-2.31; P = 0.001), and admitting diagnosis of cardiogenic shock (adjusted HR: 1.49; 95% CI: 1.05-2.01; P = 0.025) (Table 5).
Figure 1.
Mortality in the Cardiac Intensive Care Unit: A Comparison Between Housestaff and Advanced Practice Provider Teams
ICU = intensive care unit; APP = advanced practice provider.
Table 3.
Hospital Outcomes
| House Staff | Advanced Practice Provider | P Value | |
|---|---|---|---|
| Hospital LOS, d | 7 (3–16) | 8 (3–17) | 0.63 |
| In-Hospital mortality | 137 (13.5%) | 84 (13.8%) | 0.62a |
| ICU LOS, d | 2 (1–4) | 3 (1–5) | 0.047 |
| ICU mortality | 85 (8.4%) | 50 (8.2%) | 0.15a |
Values are median (IQR) or n (%).
ICU = intensive care unit; LOS = length of stay.
P values derived from log-rank test.
Figure 2.
In-Hospital Mortality: A Comparison Between Housestaff and Advanced Practice Provider Cardiac Intensive Care Unit Teams
APP = advanced practice provider.
Table 4.
Association Between CICU Mortality and Clinical Variables
| Univariable Analysis |
Multivariable Analysis |
|||
|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Age, y | 1.01 (1.01–1.03) | 0.003 | 1.02 (1.01–1.03) | 0.002 |
| Male | 1.14 (0.47–1.64) | 0.48 | 1.26 (0.85–1.85) | 0.23 |
| Race | 1.10 (0.98–1.23) | 0.09 | 1.10 (0.98–1.24) | 0.10 |
| BMI, kg/m2 | 0.99 (0.97–1.02) | 0.92 | ||
| Ejection fraction, % | 0.99 (0.98–1.00) | 0.33 | 0.99 (0.98–1.00) | 0.64 |
| MCS | 1.62 (1.05–2.50) | 0.029 | 1.27 (0.79–2.04) | 0.54 |
| Dialysis | 1.50 (1.03–2.20) | 0.03 | 1.51 (1.02–2.26) | 0.039 |
| Cardiogenic shock | 1.02 (0.69–1.51) | 0.90 | 1.05 (0.68–1.61) | 0.81 |
| STEMI | 1.67 (1.02–2.73) | 0.041 | 1.42 (0.83–2.43) | 0.19 |
| APP team | 0.77 (0.54–1.1) | 0.16 | 0.73 (0.51–1.05) | 0.10 |
APP = advanced practice provider; BMI = body mass index; CICU = cardiac intensive care unit; MCS = mechanical circulatory support; STEMI = ST-segment elevation myocardial infarction.
Table 5.
Association Between In-Hospital Mortality and Clinical Variables
| Univariable Analysis |
Multivariable Analysis |
|||
|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Age, y | 1.01 (1.01–1.03) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
| Male | 1.21 (0.91–1.61) | 0.17 | 1.33 (0.98–1.81) | 0.063 |
| Race | 1.05 (0.96–1.14) | 0.25 | 1.54 (0.97–1.16) | 0.15 |
| BMI, kg/m2 | 1.00 (0.97–1.02) | 0.63 | ||
| Ejection fraction, % | 0.99 (0.98–1.00) | 0.33 | 1.00 (0.99–1.00) | 1.00 |
| MCS | 2.31 (1.60–3.303) | <0.001 | 1.74 (1.17–2.60) | 0.006 |
| Dialysis | 1.74 (1.29–2.35) | <0.001 | 1.69 (1.24–2.31) | 0.001 |
| Cardiogenic shock | 1.74 (1.28–2.35) | <0.001 | 1.49 (1.05–2.01) | 0.025 |
| STEMI | 1.23 (0.79–1.89) | 0.35 | 1.48 (0.84–2.60) | 0.17 |
| APP team | 0.93 (0.71–1.23) | 0.64 | 0.82 (0.62–1.08) | 0.17 |
APP = advanced practice provider; BMI = body mass index; MCS = mechanical circulatory support; STEMI = ST-segment elevation myocardial infarction.
The median CICU LOS was lower on the housestaff team when compared to the APP team (2 days [IQR: 1-4 days] vs 3 days [IQR: 1-5 days], P = 0.047). There was, however, no difference in hospital LOS between the 2 teams (7 days [IQR: 3-16 days] vs 8 days [IQR: 3-17 days], P = 0.63). The rates of central line-associated blood stream infections and catheter-associated urinary tract infections between the housestaff and APP teams were 0.9% vs 0.3% (P = 0.18) and 0.6% vs 0.2% (P = 0.20), respectively.
In a supplementary Bayesian Cox proportional hazards model analysis to address the limited statistical power, we found that there is a 99.8% probability that the relative hazard rate for death in the CICU with admission to the APP team vs the housestaff team is no greater than 5% higher. This suggests that the APP team's performance is comparable to the housestaff team in terms of mortality risk in the CICU, with a high degree of confidence.
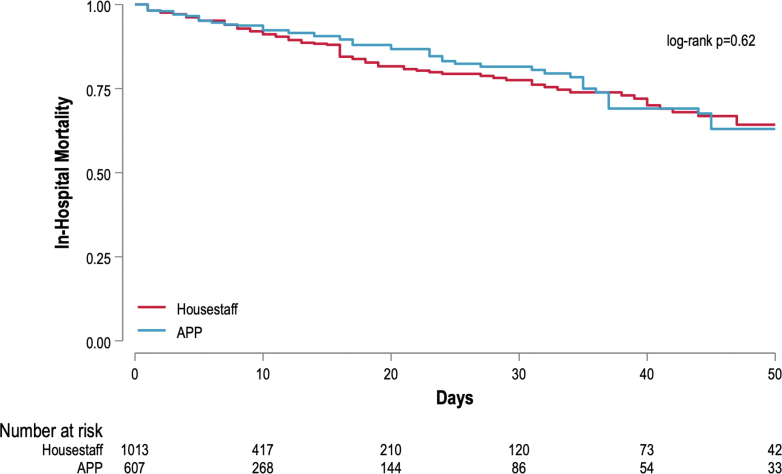
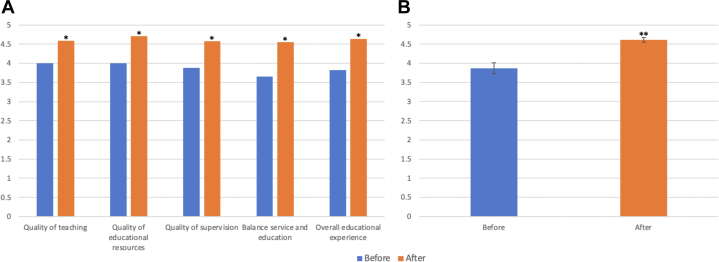
Lastly, the addition of a second CICU team had a positive impact on the perceived educational experience of cardiology fellows, as evidenced by an improvement in the rotation evaluation, both by individual domains and the average rotation scores (3.87 ± 0.14 before vs 4.61 ± 0.06 after, P < 0.0001) (Figure 3).
Figure 3.
Fellowship Rotation Evaluations
(A) Fellowship evaluation of coronary care unit rotation before and after implementation of a second team (APP-based) categorized by each domain. Overall fellowship educational experience before and after implementation of a second team (APP-based). (B) Bar graph displays the average scores for the overall educational experience as evaluated by fellows before (blue bar) and after (orange bar) the implementation of an APP-based second team. ∗P < 0.05; ∗∗P < 0.001. APP = advanced practice provider.
Discussion
The optimal staffing model for the delivery of cardiac critical care in the contemporary CICU remains a rapidly evolving issue as demand to treat critically ill cardiac patients continues to grow. In the present study, we demonstrate that implementation of an APP-based, housestaff-free team in a Level 1 CICU at a large safety-net university hospital allowed us to provide high-quality patient care while effectively managing the demands associated with a dynamic and busy clinical service. The addition of an APP-based, housestaff-free team also had a positive impact in the educational experience of rotating cardiology fellows.
To our knowledge, this is the first study to compare patient outcomes between housestaff-based and APP-based teams in the CICU. The primary findings of our study demonstrate no differences in CICU or in-hospital mortality between the teams with equivalent distribution of patients in terms of baseline characteristics, admitting diagnosis, disease severity, and need for critical care therapies, such as MV, MCS, invasive hemodynamics, and vasoactive medications. Importantly, our results demonstrate that an APP-led, housestaff-free team represents a potentially sustainable, safe, and effective staffing model for the CICU. These outcomes align with previously published results in other critical care populations that have demonstrated that ICU teams staffed by APPs offer safe care delivery models and serve as reasonable staffing alternatives to traditional physician-only models.16, 17, 18
In our study, we found that patients admitted to the APP-CICU team in our hospital experienced a longer CICU LOS compared to those under the care of medical residents. This finding is also similar to those from prior studies; however, prior studies have attributed this to differences in the patient population (older, more chronically ill).17,19 In our cohort, any difference in CICU LOS is less likely due to differences in the patient population, as we found no differences in patient characteristics between the 2 groups. Such LOS differences may be indicative of variations in clinical practices between APPs and trainees. An alternative explanation could be related to the unique structure of our APP CICU team. Unlike prior studies focusing on housestaff vs APP ICU teams in the MICU, our hospital's APP CICU team does not have a dedicated cardiology fellow, which may result in delays in a proactive approach for triage decision-making such as downgrading of patients to non-ICU settings. Moreover, unmeasured confounders and unforeseeable factors related to bed throughput according to census and capacity in the receiving inpatient units (eg, telemetry, step-down units) could have influenced the timing of bed allocation, potentially causing delays in transfer times out of the CICU. These factors include isolation status for infection control measures, bed availability in other units (eg, bed matching patient’s sex), and internal triaging needs.
Despite sharing many similarities with previous studies on APPs in the general ICU population, our study stands out in several important aspects. First, ours is the only study to compare outcomes between APP and housestaff teams among patients admitted to the same CICU. Secondly, our APP team is staffed by APPs during both day and night shifts, whereas earlier studies described residents or critical care fellows for nightshift coverage on the APP team, thus introducing challenges in isolating the direct effects of APP-based staffing in these models.18,19 Third, unlike prior studies comparing outcomes between the 2 teams, our APP CICU team does not include a dedicated fellow during the day, while prior studies included a dedicated critical care fellow on both housestaff and APP teams.17, 18, 19, 20 Similarly, this is the first study to evaluate the impact of adding a second APP-based team in the educational experience of cardiology trainees, highlighting another domain of relevance in cardiovascular medicine in addition to assisting with staffing crises and standardizing quality of care.
Lastly, while our study was a nonrandomized retrospective analysis, the allocation of patients based on bed availability, attempted equitable distribution of acuity between the 2 teams, mitigated differences in admitting diagnoses and crucial patient characteristics, including disease severity and risk profile. In contrast, numerous previous studies lacked the sequential allocation of patients to different ICU teams, resulting in significant differences in baseline characteristics between patients assigned to APP and housestaff teams. For instance, some institutions have diverse admission triage models and criteria where APP-based teams admit patients on either side of the spectrum of severity, where the highest-acuity patients (eg, ECMO, MCS) or the more stable patients (eg, postprocedural monitoring) go to APP-based teams. Although prior studies employed regression and propensity score analyses in an attempt to adjust for confounders, the possibility of overlooking important residual unmeasured confounders in those studies remains.18,20 In our study, the deliberate allocation of admissions to either team in a balanced manner played a pivotal role in mitigating potential confounders and selection biases. This strategic approach significantly enhances the reliability of our findings and provides a more meaningful interpretation and applicability of the study outcomes.
Our study's findings carry significant implications, particularly in highlighting the capability of APPs to provide care for patients in the CICU with similar risk profiles and conditions as those managed by housestaff teams, resulting in nearly indistinguishable outcomes, as well as in improving team workflow to allow for a better educational experience for trainees rotating in academic CICUs.
Study limitations
This study is subject to some limitations. First, this is a single-center study conducted at a Level 1 CICU within a large urban safety-net academic hospital with continuous (around the clock) presence of an in-house cardiology fellow. This level of supervision may not be available in many centers. The APPs in our study also underwent comprehensive training and onboarding, which may not be the case in other centers. Therefore, our findings may not be generalizable to other centers lacking similar levels of support and resources but may be applicable to Level 1 CICU with similar structure, patient profiles, and staffing needs. Second, given the retrospective nature of the study, despite large number of variables evaluated, it is not possible to completely control for baseline differences in the patient populations admitted to the 2 CICU teams. For example, although the covariates are well matched between the 2 groups, there remains a possibility that triage to the 2 teams was influenced by the severity of illness, which is not accounted for as a confounder. The absence of severity measures such as M-CARS (Modified Cardiac Arrest Risk Stratification) or APACHE II (Acute Physiology and Chronic Health Evaluation) may limit our ability to fully assess the impact of illness severity on outcomes. Third, changes in institutional protocols, nursing staffing, and practice patterns over the study period are not measured in this study and may have influenced our outcomes. Nevertheless, comparative analysis of data from 2 teams within the same institution offers a degree of standardization for many potential confounders that would affect both teams equally. Forth, we do not have data regarding the frequency and reasons for patient transfers between the APP and housestaff teams. However, such occurrences were rare. Fifth, our dataset did not include information on the timing of admissions, specifically day vs night and weekday vs weekend. This information could potentially impact the outcomes observed, as admission timing may influence patient care and resource availability. Future studies should consider including these variables to provide a more comprehensive analysis of their effects. Sixth, the difference in average census on teams may have impacted observed outcomes. Seventh, our study was limited by the statistical power available given our sample size. Therefore, our findings may be subject to type II errors, where potentially important differences could not be identified due to insufficient sample size. However, we have included a supplementary Bayesian analysis to support our findings. Eighth, secondary outcomes were not adjusted for multiplicity and thus should be interpreted with caution.
Finally, while our study provides valuable insights into the outcomes of patients managed by housestaff and APP teams in the CICU, there are several areas that were not addressed and warrant further investigation. Specifically, we did not collect data on the types of procedures performed (such as central lines, arterial lines, and intubations) or their associated complications for each team. Additionally, information on the health care resource utilization (such as frequency and types of testing, imaging, and consultations on other services) was not included in our analysis. Another important aspect that remains unexplored is the financial impact of using housestaff teams vs APP teams, as well as their effects on patient satisfaction. These areas represent critical gaps in our understanding and should be the focus of future research. Examining such data would provide a more comprehensive evaluation of the 2 staffing models and their implications for patient care, resource utilization, and cost-effectiveness in the CICU setting.
Conclusions
Our study is the first to compare outcomes between a housestaff and an APP team in the same CICU setting, providing a unique contribution to the existing literature. Our findings reveal no significant differences in ICU or in-hospital mortality rates between the 2 teams. Our study sheds light on the clinical utilization of APPs in CICU settings and provides valuable insight into the ongoing effort to define optimal staffing models in the ever-evolving field of critical care within the CICU.
PERSPECTIVES.
COMPETENCY IN SYSTEMS-BASED PRACTICE: Clinicians reading this study have an opportunity to enhance their competency in systems-based practice by critically assessing how the study's findings may translate into action plans within their own health care contexts in the contemporary and ever-evolving CICU. This may involve adapting to variations in staffing models, recognizing the impact of specialist involvement (such as critical care cardiology), and discerning the broader systemic factors that influence patient care. The study serves as a valuable resource for clinicians seeking to improve their ability to navigate and contribute effectively within the complex health care systems in which they operate. Similarly, our findings can assist clinicians in leadership positions as well as hospital administrators to support the use of an APP-based model to navigate staffing challenges and meet the demands of their CICUs.
TRANSLATIONAL OUTLOOK: This study, conducted within a specific Level 1 CICU setting, offers a valuable starting point for understanding the role of APPs in the CICU. However, recognizing the limitations such as the single-center focus at an academic teaching hospital, future research toward multicenter studies that encompass diverse health care settings are needed to shed light on the generalizability of our findings and contribute to establishing best practices in APP-led staffing models in the CICU.
Funding support and author disclosures
Dr Bangalore serves on the advisory board of Abbott Vascular, Boston Scientific, Biotronik, Amgen, Pfizer, Merck, REATA, Inari, and Truvic. Dr Alviar serves as a consultant at Zoll Inc, Abbott, and Abiomed and receives research grants from Baxter Medical. Dr Katz has received research support (modest) from Abbott Corporation, Speaker Honoraria of Zoll Inc, and the member of the Data Safety & Monitoring Board of Abiomed Inc. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors extend our sincere gratitude to the nurses, housestaff, advanced practice providers, and cardiology attendings for their time and commitment dedicated to providing care for all the patients in the cardiac intensive care unit (CICU). Similarly, they thank Rebecca Fisher, CFO, and the leadership of Bellevue Hospital for their support in implementing this second CICU team. Their invaluable contributions have been instrumental, and without their unwavering dedication, this work would not have been possible.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Julian D.G. The evolution of the coronary care unit. Cardiovasc Res. 2001;51(4):621–624. doi: 10.1016/s0008-6363(01)00365-0. [DOI] [PubMed] [Google Scholar]
- 2.Morrow D.A., Fang J.C., Fintel D.J., et al. Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126(11):1408–1428. doi: 10.1161/CIR.0b013e31826890b0. [DOI] [PubMed] [Google Scholar]
- 3.Bohula E.A., Katz J.N., van Diepen S., et al. Demographics, care patterns, and outcomes of patients admitted to cardiac intensive care units: the critical care cardiology trials network prospective north American multicenter registry of cardiac critical illness. JAMA Cardiology. 2019;4(9):928–935. doi: 10.1001/jamacardio.2019.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinha S.S., Sjoding M.W., Sukul D., et al. Changes in primary noncardiac diagnoses over time among elderly cardiac intensive care unit patients in the United States. Circ Cardiovasc Qual Outcomes. 2017;10(8) doi: 10.1161/circoutcomes.117.003616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz J.N., Shah B.R., Volz E.M., et al. Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. 2010;38(2):375–381. doi: 10.1097/CCM.0b013e3181cb0a63. [DOI] [PubMed] [Google Scholar]
- 6.Metkus T.S., Miller P.E., Alviar C.L., et al. Advanced respiratory support in the contemporary cardiac ICU. Crit Care Explor. 2020;2(9) doi: 10.1097/cce.0000000000000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katz J.N., Minder M., Olenchock B., et al. The genesis, maturation, and future of critical care cardiology. J Am Coll Cardiol. 2016;68(1):67–79. doi: 10.1016/j.jacc.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 8.O'Gara P.T., Adams J.E., 3rd, Drazner M.H., et al. COCATS 4 task force 13: training in critical care cardiology. J Am Coll Cardiol. 2015;65(17):1877–1886. doi: 10.1016/j.jacc.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Miller P.E., Kenigsberg B.B., Wiley B.M. Cardiac critical care: training pathways and transition to early career. J Am Coll Cardiol. 2019;73(13):1726–1730. doi: 10.1016/j.jacc.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Geller B.J., Fleitman J., Sinha S.S. Critical care cardiology: implementing a training paradigm. J Am Coll Cardiol. 2018;72(10):1171–1175. doi: 10.1016/j.jacc.2018.07.024. [DOI] [PubMed] [Google Scholar]
- 11.Halpern N.A., Pastores S.M. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38(1):65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 12.Angus D.C., Kelley M.A., Schmitz R.J., White A., Popovich J., Jr. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 13.Katz J.N., Turer A.T., Becker R.C. Cardiology and the critical care crisis: a perspective. J Am Coll Cardiol. 2007;49(12):1279–1282. doi: 10.1016/j.jacc.2006.11.036. [DOI] [PubMed] [Google Scholar]
- 14.Prasad M., Iwashyna T.J., Christie J.D., et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9):2564–2569. doi: 10.1097/CCM.0b013e3181a93468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tennyson C.D., Bowers M.T., Dimsdale A.W., et al. Role of advanced practice providers in the cardiac intensive care unit team. J Am Coll Cardiol. 2023;82(24):2338–2342. doi: 10.1016/j.jacc.2023.08.061. [DOI] [PubMed] [Google Scholar]
- 16.Kleinpell R.M., Ely E.W., Grabenkort R. Nurse practitioners and physician assistants in the intensive care unit: an evidence-based review. Crit Care Med. 2008;36(10):2888–2897. doi: 10.1097/CCM.0b013e318186ba8c. [DOI] [PubMed] [Google Scholar]
- 17.Scherzer R., Dennis M.P., Swan B.A., Kavuru M.S., Oxman D.A. A Comparison of usage and outcomes between nurse practitioner and resident-staffed medical ICUs. Crit Care Med. 2017;45(2):e132–e137. doi: 10.1097/ccm.0000000000002055. [DOI] [PubMed] [Google Scholar]
- 18.Kawar E., DiGiovine B. MICU care delivered by PAs versus residents: do PAs measure up? JAAPA. 2011;24(1):36–41. doi: 10.1097/01720610-201101000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Gershengorn H.B., Wunsch H., Wahab R., et al. Impact of nonphysician staffing on outcomes in a medical ICU. Chest. 2011;139(6):1347–1353. doi: 10.1378/chest.10-2648. [DOI] [PubMed] [Google Scholar]
- 20.Landsperger J.S., Semler M.W., Wang L., Byrne D.W., Wheeler A.P. Outcomes of nurse practitioner-delivered critical care: a prospective cohort study. Chest. 2016;149(5):1146–1154. doi: 10.1016/j.chest.2015.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]