Abstract
Background
Non-suicidal self-injury (NSSI) is a serious mental health problem among adolescents and young adults. Childhood trauma is a distal factor for NSSI and can also lead to cognitive abnormalities and maladaptive emotion regulation during the growth and development of individuals. However, it is unclear how childhood trauma and cognitive-emotional factors interact with NSSI.
Objective
This study investigated the roles of childhood trauma and cognitive-emotional factors in NSSI among Chinese college students using network analysis.
Methods
A total of 999 students from a university in central China were included in this study. Network analysis was used to examine the interrelationships between the frequency of NSSI thoughts and behaviors, childhood trauma subtypes (measured using the Childhood Trauma Questionnaire-Short Form), and cognitive-emotional factors such as early maladaptive schemas (EMSs) (measured using the Young Schema Questionnaire-Short Form), core self-evaluation (measured using the Core Self-Evaluations Scale), and emotion regulation (ER) strategies (measured using the Emotion Regulation Questionnaire). Structural equation modeling was used to further explore the role of the nodes most closely related to NSSI in the network analysis.
Results
Emotional abuse and disconnection/rejection EMS are found to be directly related to NSSI thoughts (edge weight = 0.16 and 0.08, respectively). Disconnection/rejection EMS partially mediated (28.64%) the relationship between emotional abuse and NSSI thoughts, with a higher level of expression suppression corresponding to a greater positive relationship between emotional abuse and the disconnection/rejection EMS (p < 0.01).
Conclusion
Our findings were in line with the cognitive-emotional model of NSSI, highlighting the importance of NSSI prevention in identifying risk groups who experienced emotional abuse in childhood and tended to use expressive suppression as an ER strategy.
Keywords: childhood trauma, early maladaptive schema, emotion regulation strategy, non-suicidal self-injury, network analysis
Introduction
Non-suicidal self-injury (NSSI) is defined as repeated (occurring more than 5 days in a year), intentional, and direct injury to one’s body (eg, cutting, plucking, or scratching) in a non-socially sanctioned manner, without suicidal intent.1 NSSI is one of the leading causes of death among young people globally,2 with some self-injurers dying as a result of unexpected consequences of high-risk but low suicidal intentions behaviors.3 Although NSSI mainly occurs in early adolescence,4 it is also common in early adulthood, especially among college students. Due to the sudden changes in lifestyle and the pressure of competition,5–7 the prevalence of NSSI among college students has reached 20.2% worldwide.8 Regarding the strong association of NSSI with emotional problems, suicide attempts, and other risky behaviors,9 people at risk of self-injury should be identified and provided with appropriate intervention as early as possible; thus, a better understanding of the reason why some people are more likely to engage in NSSI is crucial.10 According to the cognitive-emotional model of NSSI, when confronted with emotionally volatile situations, individuals with intense emotional reactions, maladaptive emotion regulation strategies, negative self-schemas, beliefs of incapability of resisting NSSI, and beliefs that desired outcomes (eg, reducing negative emotions) can be achieved by NSSI may be at a significantly increased risk of engaging in NSSI.11,12 Based on this model, the present study looks to identify both cognitive and emotional risk factors for NSSI and to further explore how each dimension of these factors affects NSSI, so as to provide more specific targets for the identification and intervention of NSSI. The present study may also enrich the existing model by including childhood trauma, which may affect the cognitive and emotional factors of NSSI.
Childhood trauma is defined as physical or emotional abuse, neglect or negligent treatment, sexual abuse, or other exploitations from parents or other caregivers before the age of 18 years.13 It is generally classified into five subtypes, ie, emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect.14 Childhood trauma is a distal risk factor for NSSI in early adulthood.15 Distal risk factors are events or factors independent of one’s behavior, whereas proximal risk factors are the characteristics of one’s own; it has been found that distal risk factors indirectly contribute to mental disorders mainly through the mediating effect of proximal risk factors.16 A study by Wan et al found that all subtypes of childhood trauma were significantly correlated with NSSI and that there might be a strong graded relationship between the frequency of childhood traumatic experiences and NSSI.17 Childhood trauma may cause maladaptive emotion regulation and cognitive biases (eg, early maladaptive schemas and lower core self-evaluations) during one’s growth and development;18,19 thus, these emotional and cognitive problems are proximal risk factors of NSSI based on the cognitive-emotional model of NSSI.11
Maladaptive emotion regulation (ER) strategies can increase the risk of NSSI.20,21 Generally, emotion regulation strategies are categorized into two main dimensions: cognitive reappraisal, which refers to the use of positive views of the situation or the adjustment of one’s understanding of the situation, and expressive suppression, which refers to the inhibition of emotion expression that is occurring or about to occur.22 As cognitive reappraisal reduces the negative emotional experience triggered by stressful situations,23 it is considered adaptive and more effective than expressive suppression in reducing the risk and severity of NSSI.24,25 Long-term suppression of emotional expression gradually depletes one’s self-control resources, which can lead to difficulties in emotion regulation.26 Due to the lack of alternative strategies, individuals are likely to adopt NSSI as an approach to regulating their emotions. Thus, if strong emotional stimuli cannot be avoided, the lack of appropriate emotion regulation strategies becomes the most important factor in increasing the risk of NSSI.20
Individuals’ negative perceptions and evaluations of themselves may also lead to self-depreciation and feelings of disgust; to avoid or escape these experiences, low self-evaluation may develop into self-punishing behaviors such as NSSI.27 It has been demonstrated that individuals with low core self-evaluation have low self-esteem, are more skeptical of their abilities, have less control over their emotions, and are more likely to use NSSI as a coping strategy.28–30 Moreover, people with a history of NSSI usually report negative self-schemas.30 Experiences of childhood abuse, such as emotional abuse and physical abuse, are a major source of early maladaptive schemas (EMSs).31 Previous research has revealed that experiences of emotional abuse and neglect could lead to maladaptive schemas such as low self-efficacy, interpersonal sensitivity, and feelings of abandonment among college students,32 and these maladaptive schemas played a mediating role in the relationship between early traumatic experiences and later emotional disorders.33 On this basis, the present study included core self-evaluation and EMS as potential risk factors for the cognitive aspects of NSSI.
Although current evidence suggests that childhood trauma, emotional factors, and cognitive factors are strongly associated with NSSI, how these factors interact with each other and directly or indirectly influence the thoughts and behaviors of NSSI is still unclear. Studies have suggested that psychiatric symptoms are more likely to be the result of interactions between various factors rather than the combination of these factors;34 thus, network analysis may be the best approach to exploring the complex interactions between factors and identifying key nodes in the network.35–37 This approach has been used in many studies examining the interrelationships between the risk factors for NSSI among children, adolescents, and college students,38,39 but few studies have analyzed the cognitive and emotional risk networks for NSSI based on the cognitive-emotional model.
The present study aims to establish a relationship network consisting of childhood trauma, related cognitive and emotional factors, and NSSI thoughts and behaviors among Chinese college students based on the cognitive-emotional model. On this basis, the dimensions with a significant effect on NSSI were selected to construct a more specific structural equation model, in order to explore the occurrence mechanism of NSSI in cognitive and emotional aspects and provide a reference to the formulation of risk assessment and intervention strategies for NSSI. In addition, as the emotional and cognitive factors selected in this study are modifiable, interventions targeting the most important dimensions of these factors can be more effective in reducing and preventing the occurrence of NSSI.
Methods
Participants
Ethical approval for this study was obtained from Shanghai Changning Mental Health Center (M202151), in accordance with the Declaration of Helsinki. The questionnaire was randomly distributed to 1132 college students (non-psychology majors) at a university in mainland China by professionally trained graduate students majoring in psychology. Before the start of the survey, all participants were informed of the purpose of the study, the confidentiality of personal information, the voluntariness of participation, and the right to withdraw at any time; written informed consent was obtained from all participants or the parents of participants younger than 18 years of age. After excluding responses with excessive missing data, a total of 999 (88.25%) valid responses were analyzed in this study. The valid sample consisted of 330 males (33.03%) and 669 females (66.97%), with an age of 16–23 years (M = 18.10, SD = 0.70).
Measure
Childhood Trauma Questionnaire-Short Form (CTQ-SF)
The Chinese version of CTQ-SF consists of 28 items on five dimensions: emotional abuse, emotional neglect, sexual abuse, physical abuse, and physical neglect.40,41 All items are rated on a 5-point Likert scale (1 = never true to 5 = very often true), with a higher score indicating more severe childhood trauma. The Cronbach’s alpha coefficients for all subscales ranged from 0.72 to 0.80 in this study.
Emotion Regulation Questionnaire (ERQ)
The Chinese version of ERQ was used to assess the emotion regulation strategies habitually used by participants.42 The scale consists of 10 items on two dimensions: cognitive reappraisal and expressive suppression. All items are rated on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree), with a higher score indicating a greater tendency to use the emotion regulation strategy. In this study, the Cronbach’s alpha coefficients were 0.82 for the cognitive reappraisal dimension and 0.72 for the expressive suppression dimension.
Young Schema Questionnaire-Short Form (YSQ-SF)
The Chinese version of YSQ-SF was used to measure the level of early maladaptive schemas of participants.43 The scale consists of 64 items covering 14 schemas, which are divided into three schema domains, namely disconnection/rejection (including 5 schemas, ie, emotional deprivation, mistrust/abuse, social isolation/alienation, defectiveness/shame, and emotional inhibition), impaired autonomy and performance (including 6 schemas, ie, abandonment/instability, dependence/incompetence, vulnerability to harm or illness, failure to achieve, enmeshment/undeveloped self, and insufficient self-control/self-discipline), and hyperactivity (including 3 schemas, ie, entitlement/grandiosity, self-sacrifice, unrelenting standards). All items in this questionnaire are rated on a 6-point Likert scale (1 = completely untrue for me to 6 = describes me perfectly), with a higher score indicating a more severe early maladaptive schema. In this study, the Cronbach’s alpha coefficients for the subscales of disconnection/rejection, impaired autonomy and performance, and hyperactivity were 0.95, 0.92, and 0.86, respectively.
Core Self-Evaluations Scale (CSES)
The Chinese version of CSES was used to assess the self-evaluation of participants.44 The scale consists of 10 items with a single dimension; all items were rated on a 5-point Likert scale (1 = completely disagree to 5 = completely agree), with a higher score indicating a higher level of core self-evaluation. The Cronbach’s alpha coefficient was 0.87 in this study.
NSSI Thoughts and Behaviors
The frequency subscale of The Ottawa Self-Injury Inventory (Chinese Revision) was used to assess the self-reported frequency of NSSI thoughts and behaviors in the past 1, 6, and 12 months.45 In the present study, only the frequency of NSSI thoughts and behaviors in the past 12 months was used for data analysis, with this factor rated on a 5-point Likert scale (0 = never, 1 = 1–5 times, 2 = once a month, 3 = once a week, and 4 = every day).
Statistical Analysis
Descriptive statistics and correlation analysis were performed using SPSS 27.0. The network analysis, with five subtypes of childhood trauma, three dimensions of EMSs, two dimensions of ER strategies, core self-evaluation, and the frequency of NSSI thoughts and behaviors being nodes, was conducted using R 4.2.1. First, the network structure was constructed using the graphical least absolute shrinkage and selection operator (LASSO)46 in the qgraph toolbox; then, the strength closeness, betweenness, and expected influence index of the node centrality were calculated to quantify the importance of each node in the network structure; finally, the bootnet package was used to test the invariance of nodes on the centrality metrics by reducing the sample size in the network structure (bootnet sample size = 5000). According to Epskamp et al, a CS coefficient of 0.70 indicates the maximum acceptable sample reduction, a CS coefficient above 0.50 is acceptable, and the coefficient should not be lower than 0.25.47 The structural equation model was constructed based on the network analysis and tested using SPSS 27.0 with PROCESS 4.1.
Results
Descriptive Data
Based on the 999 valid samples used in the analysis, 244 participants (24.4%) reported having experienced NSSI thoughts, and 114 (11.4%) reported having engaged in NSSI behaviors. The sample characteristics and the mean scores of all variables are presented in Table 1.
Table 1.
Sample Characteristics and Mean Scores of Each Variable
| Variables | Total (n = 999) |
|---|---|
| Age, M(S.D.) | 18.23(4.86) |
| Gender | |
| Male, n (%) | 330(33.0) |
| Female, n (%) | 669(67.0) |
| Urban-rural residence place | |
| Urban, n (%) | 464(46.4) |
| Rural, n (%) | 528(52.9) |
| NSSI thoughts | |
| 1 month, n (%) | 121(12.1) |
| 6 month, n (%) | 180(18.0) |
| 12 month, n (%) | 229(22.9) |
| NSSI behaviors | |
| 1 month, n (%) | 38(3.8) |
| 6 month, n (%) | 87(8.7) |
| 12 month, n (%) | 107(10.8) |
| CTQ-SF | |
| Emotional abuse, M (S.D.) | 7.14(2.57) |
| Physical abuse, M (S.D.) | 5.81(1.73) |
| Sexual abuse, M (S.D.) | 5.33(1.11) |
| Emotional neglect, M (S.D.) | 8.54(3.88) |
| Physical neglect, M (S.D.) | 6.27(2.03) |
| YSQ-SF | |
| Disconnection/Rejection, M (S.D.) | 48.99(19.79) |
| Impaired autonomy and performance, M (S.D.) | 52.27(17.87) |
| Hyperactivity, M (S.D.) | 37.76(11.49) |
| ERQ | |
| Cognitive reappraisal, M (S.D.) | 30.48(5.94) |
| Expressive suppression, M (S.D.) | 14.07(4.70) |
| CSES, M (S.D.) | 35.16(6.70) |
Abbreviations: NSSI, Non-suicidal self-injury; CTQ-SF, Childhood Trauma Questionnaire Short Form; YSQ-SF, Young Schema Questionnaire Short Form; ERQ, Emotion Regulation Questionnaire; CSES, Core Self-Evaluations Scale.
Network results
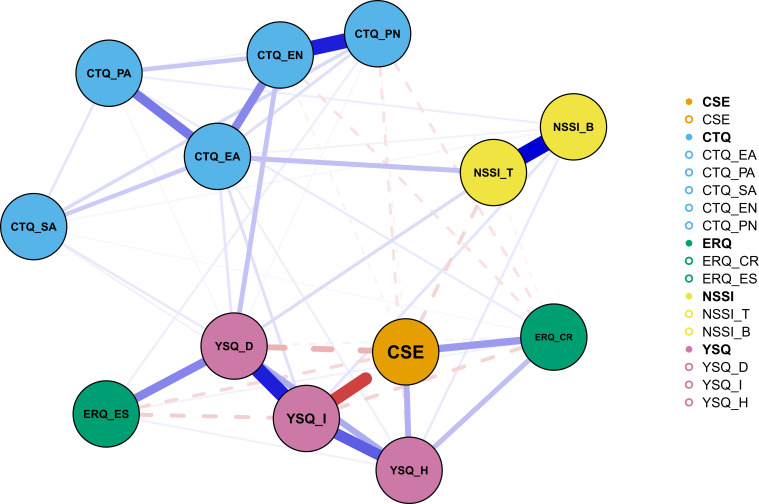
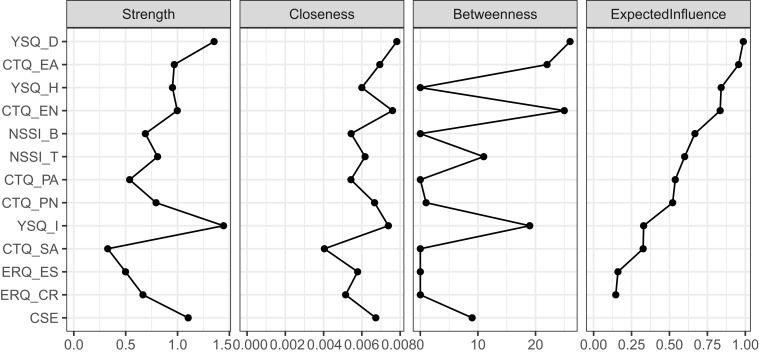
A regularized network of 13 nodes of NSSI thoughts and behaviors with their potential correlates is shown in Figure 1. A strong positive correlation was found between NSSI thoughts and behaviors (edge weight = 0.51). Both core self-evaluation and cognitive reappraisal were found to be weakly and negatively correlated with NSSI thoughts (edge weight = −0.08 and −0.02, respectively). Emotional abuse and the disconnection/rejection EMS were directly and positively associated with NSSI thoughts (edge weight = 0.12 and 0.07, respectively), and there was also a correlation between emotional abuse and the disconnection/rejection EMS (edge weight = 0.05). Emotional abuse, physical abuse, sexual abuse, the impaired autonomy and performance EMS, and the hyperactivity EMS were found to be directly and positively correlated with NSSI behaviors (edge weight = 0.03, 0.03, 0.02, 0.05, and 0.04, respectively). The disconnection/rejection EMS was found to be positively correlated with emotional neglect and expressive suppression (edge weight = 0.12 and 0.24, respectively). On the contrary, the disconnection/rejection EMS was found to be negatively correlated with core self-evaluation (edge weight = −0.15). Among all other nodes, expressive suppression had the strongest connection with the disconnection/rejection EMS. With regard to node centrality estimates, the disconnection/rejection EMS and emotional abuse were relatively important nodes four indices of strength, closeness, betweenness, and expected influence (Figure 2). The CS coefficient was satisfactory for strength (0.75), closeness (0.67), betweenness (0.75), and expected influence (0.75), suggesting the high accuracy and stability of the order of centrality indices.
Figure 1.
Regularized network consisting of 13 nodes for non-suicidal self-injury (NSSI) and its correlates (n = 999).
Notes: Blue solid edges represent positive associations between two nodes, while red dashed edges represent negative associations. The thickness of lines indicates the weights of edges.
Abbreviations: CSE, Core self-evaluation; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; CTQ_PA, Physical abuse in Childhood Trauma Questionnaire; CTQ_SA, Sexual abuse in Childhood Trauma Questionnaire; CTQ_EN, Emotional neglect in Childhood Trauma Questionnaire; CTQ_PN, Physical neglect in Childhood Trauma Questionnaire; ERQ-CR, Cognitive reappraisal in Emotion Regulation Questionnaire; ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire; NSSI_T, Non-suicidal self-injury thoughts; NSSI_B, Non-suicidal self-injury behaviors; YSQ_D, Disconnection/rejection in Young Schema Questionnaire; YSQ_I, Impaired autonomy and performance in Young Schema Questionnaire; YSQ_H, Hyperactivity in Young Schema Questionnaire.
Figure 2.
Centrality estimates of strength, closeness, betweenness and expected influence of the 13 nodes in the network model.
Abbreviations: CSE, Core self-evaluation; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; CTQ_PA, Physical abuse in Childhood Trauma Questionnaire; CTQ_SA, Sexual abuse in Childhood Trauma Questionnaire; CTQ_EN, Emotional neglect in Childhood Trauma Questionnaire; CTQ_PN, Physical neglect in Childhood Trauma Questionnaire; ERQ-CR, Cognitive reappraisal in Emotion Regulation Questionnaire; ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire; NSSI_T, Non-suicidal self-injury thoughts; NSSI_B, Non-suicidal self-injury behaviors; YSQ_D, Disconnection/rejection in Young Schema Questionnaire; YSQ_I, Impaired autonomy and performance in Young Schema Questionnaire; YSQ_H, Hyperactivity in Young Schema Questionnaire.
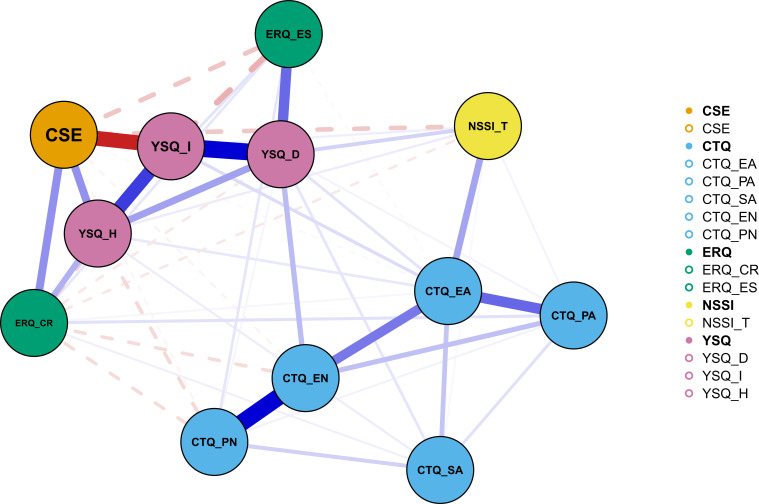
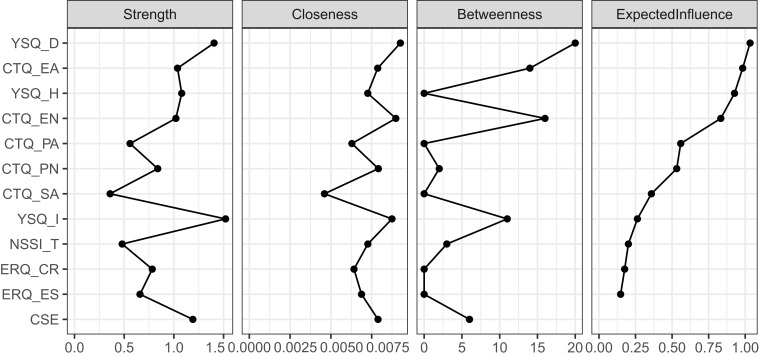
Due to the high correlation between NSSI thoughts and behaviors, the interrelationships between these two nodes and other nodes in the network analysis might be obscured. As NSSI thoughts precede NSSI behaviors in general, we removed the NSSI behaviors and ran the network analysis again for the remaining 12 nodes (Figure 3). After removal of NSSI behaviors, the node closeness of this network model became higher than that of the network consisting of all 13 nodes (Figures 2 and 4). More significant negative associations were found of core self-evaluation and cognitive reappraisal with NSSI thoughts (edge weight = −0.10 and −0.04, respectively). The correlation between emotional abuse and the disconnection/rejection EMS, as well as the direct positive correlation between both of these two nodes and NSSI thoughts also became more apparent (edge weight = 0.05, 0.16, and 0.08, respectively). Physical abuse, sexual abuse, the impaired autonomy and performance EMS, and the hyperactivity EMS were weakly and positively correlated with NSSI thoughts (edge weight = 0.02, 0.02, 0.03, and 0.03, respectively). Moreover, other nodes in the network model were found to have indirectly influenced NSSI thoughts through the bridging effects of emotional abuse and the disconnection/rejection EMS. Expressive suppression still had the strongest association with the disconnection/rejection EMS (edge weight = 0.27). As indicated by the node centrality estimates, the disconnection/rejection EMS and emotional abuse were relatively important nodes based on various indices (Figure 4). The CS coefficient was satisfactory for strength (0.75), closeness (0.75), betweenness (0.75), and expected influence (0.75), suggesting the high accuracy and stability of the order of centrality indices.
Figure 3.
Regularized network consisting of 12 nodes for non-suicidal self-injury (NSSI) and its correlates (n = 999).
Notes: Blue solid edges represent positive associations between two nodes, while red dashed edges represent negative associations. The thickness of the lines indicates the weights of the edges.
Abbreviations: CSE, Core self-evaluation; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; CTQ_PA, Physical abuse in Childhood Trauma Questionnaire; CTQ_SA, Sexual abuse in Childhood Trauma Questionnaire; CTQ_EN, Emotional neglect in Childhood Trauma Questionnaire; CTQ_PN, Physical neglect in Childhood Trauma Questionnaire; ERQ-CR, Cognitive reappraisal in Emotion Regulation Questionnaire; ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire; NSSI_T, Non-suicidal self-injury thoughts; YSQ_D, Disconnection/rejection in Young Schema Questionnaire; YSQ_I, Impaired autonomy and performance in Young Schema Questionnaire; YSQ_H, Hyperactivity in Young Schema Questionnaire.
Figure 4.
Centrality estimates of strength, closeness, betweenness and expected influence of the 12 nodes in the network model.
Abbreviations: CSE, Core self-evaluations; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; CTQ_PA, Physical abuse in Childhood Trauma Questionnaire; CTQ_SA, Sexual abuse in Childhood Trauma Questionnaire; CTQ_EN, Emotional neglect in Childhood Trauma Questionnaire; CTQ_PN, Physical neglect in Childhood Trauma Questionnaire; ERQ-CR, Cognitive reappraisal in Emotion Regulation Questionnaire; ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire; NSSI_T, Non-suicidal self-injury thoughts; YSQ_D, Disconnection/rejection in Young Schema Questionnaire; YSQ_I, Impaired autonomy and performance in Young Schema Questionnaire; YSQ_H, Hyperactivity in Young Schema Questionnaire.
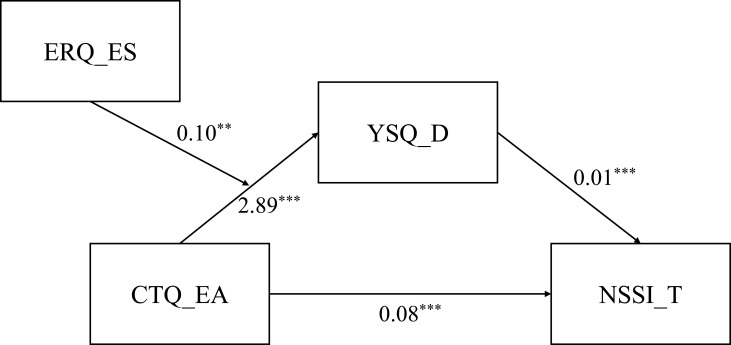
Structural Equation Modeling Results
Based on the results of the network analysis and the cognitive-emotional model, we included some of the important nodes in the structural equation modeling. First, both emotional abuse and the disconnection/rejection EMS, which are relatively important nodes, were found to be directly related to NSSI thoughts. As emotional abuse is theoretically a distal risk factor of NSSI and disconnection/rejection is a cognitive influencing factor of NSSI in the cognitive-emotional model, we conducted a mediation analysis with emotional abuse as the independent variable, NSSI thoughts as the dependent variable, and the disconnection/rejection EMS as the mediating variable. In addition, as an influencing factor of NSSI in the cognitive-emotional model, expressive suppression was found to be strongly correlated with the disconnection/rejection EMS in the network model. Moreover, maladaptive emotion regulation strategies might also aggravate the adverse consequences caused by childhood trauma. Therefore, it is also necessary to incorporate expressive suppression as a moderating variable in the moderated mediation analysis.
The results of PROCESS Model 4 indicated that the disconnection/rejection EMS partially mediated the effect of emotional abuse on NSSI thoughts (Table 2). The overall effect of emotional abuse on NSSI thoughts was significant (p < 0.001); with the addition of the disconnection/rejection EMS as a mediating variable, the direct effect of emotional abuse on NSSI thoughts was still significant (p < 0.001). In addition, the upper and lower limits of the confidence intervals for direct and indirect effects did not contain 0, indicating that emotional abuse could affect NSSI thoughts directly and through the mediation of the disconnection/rejection EMS. The direct and indirect effects of emotional abuse accounted for 71.36% and 28.64% of the total effect, respectively.
Table 2.
Results of the Mediation Effect Analysis of Disconnection/Rejection
| path | Effect | S.E. | t | P | LLCI | ULCI | Percentage |
|---|---|---|---|---|---|---|---|
| CTQ_EA→NSSI_T (Total effect) |
0.11 | 0.01 | 14.90 | 0.00 | 0.09 | 0.12 | / |
| CTQ_EA→NSSI_T (Direct effect) |
0.08 | 0.01 | 10.11 | 0.00 | 0.06 | 0.09 | 71.36% |
| CTQ_EA→YSQ_D→NSSI_T (Indirect effect) |
0.03 | 0.01 | / | / | 0.02 | 0.04 | 28.64% |
Abbreviations: CTQ_EA, Emotional abuse of Childhood Trauma Questionnaire; NSSI_T, Non-suicidal self-injury thoughts; YSQ_D, Disconnection/Rejection of Young Schema Questionnaire.
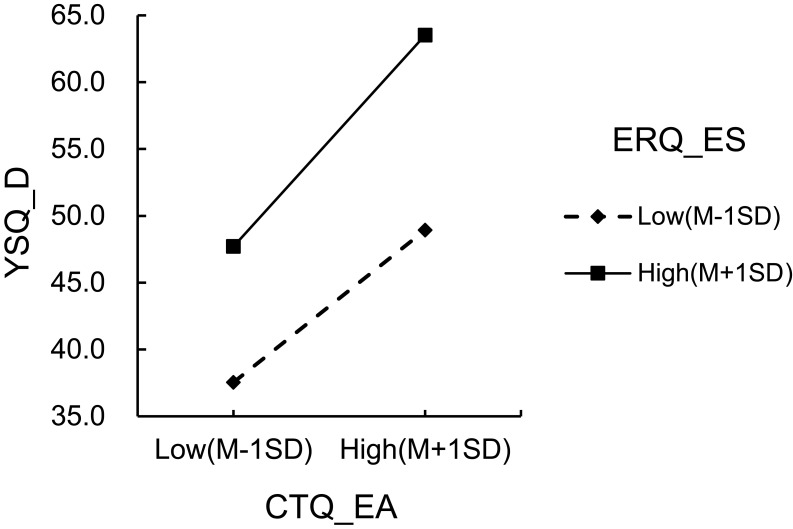
The results of PROCESS Model 7 (Figure 5) indicated that expressive suppression moderated the effect of emotional abuse on the disconnection/rejection EMS as well as the mediating effect of disconnection/rejection in a positive manner (Tables 3 and 4). All three paths, ie, emotional abuse in Childhood Trauma Questionnaire (CTQ_EA)→disconnection/rejection in Young Schema Questionnaire (YSQ_D), and expressive suppression in Emotion Regulation Questionnaire (ERQ_ES)→YSQ_D, and the interaction between CTQ_EA and ERQ_ES (INT)→YSQ_D, were significant (p < 0.01) (Table 3). Notably, the coefficient of INT→YSQ_D was 0.10 with p = 0.007 (< 0.01), indicating that ERQ_ES plays a significant positive moderating role in the effect of CTQ_EA on YSQ_D; as the level of expression suppression increased, the positive relationship between emotional abuse and disconnection/rejection became stronger. The simple slopes graph is shown in Figure 6. Furthermore, the conditional indirect effect values also exhibited a gradual upward trend with the increase in ERQ_ES score from M-SD to M+SD (Table 4). With the decrease of ERQ_ES score from M+SD to M-SD, the subtraction between conditional indirect effect values was 0.009, with the upper and lower limits of the confidence intervals (0.001, 0.017) for pairwise contrast not containing 0, indicating that ERQ_ES had a significant moderating effect on the mediating effect.
Figure 5.
Structure and path coefficients of the moderated mediation model.
Notes: ** P < 0.01; *** P < 0.001.
Abbreviations: ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; YSQ_D, Disconnection/rejection in Young Schema Questionnaire; NSSI_T, Non-suicidal self-injury thoughts.
Table 3.
Results of the Moderation Effect Analysis of Expressive Suppression on the Effect of Emotional Abuse on Disconnection/Rejection
| path | coeff | S.E. | t | P | LLCI | ULCI |
|---|---|---|---|---|---|---|
| CTQ_EA→YSQ_D | 2.89 | 0.21 | 13.70 | 0.00 | 2.47 | 3.30 |
| ERQ_ES→YSQ_D | 1.29 | 0.11 | 11.36 | 0.00 | 1.07 | 1.52 |
| INT→YSQ_D | 0.10 | 0.04 | 2.71 | 0.01 | 0.03 | 0.17 |
Abbreviations: CTQ_EA, Emotional abuse of Childhood Trauma Questionnaire; YSQ_D, Disconnection/Rejection of Young Schema Questionnaire; ERQ-ES, Expressive suppression of Emotion Regulation Questionnaire; INT, the interaction of CTQ_EA and ERQ_ES.
Table 4.
Results of the Moderated Mediation Analysis of Expressive Suppression on Conditional Indirect Effect of Disconnection/Rejection
| ERQ_ES | Effect | BootSE | BootLLCI | BootULCI |
|---|---|---|---|---|
| −4.710(−1SD) | 0.022 | 0.004 | 0.015 | 0.032 |
| 0.000 | 0.027 | 0.005 | 0.018 | 0.036 |
| 4.710 (1SD) | 0.031 | 0.006 | 0.021 | 0.042 |
Abbreviations: ERQ-ES, Expressive suppression of Emotion Regulation Questionnaire.
Figure 6.
Simple slopes graph of the conditional relationship.
Abbreviations: YSQ_D, Disconnection/rejection in Young Schema Questionnaire; CTQ_EA, Emotional abuse in Childhood Trauma Questionnaire; ERQ-ES, Expressive suppression in Emotion Regulation Questionnaire.
Discussion
The present study established an NSSI network model for Chinese college students, with childhood trauma as a distal factor and the inclusion of cognitive-emotional factors such as EMSs, core self-evaluations, and ER strategies based on the cognitive-emotional model.
Nearly a quarter (24.4%) of the participants in this study reported having NSSI thoughts, and nearly half of them (11.4%) reported having engaged in NSSI behaviors. The incidence of NSSI behaviors in this study is close to the results of previous studies on college students in Belgium (10.3%) and Brazil (17.8%),48,49 suggesting that college students may be a high-risk group for NSSI regardless of cultural background, and highlighting the importance of investigating the occurrence mechanisms and intervention priorities of NSSI in college students.
Compared to the 13-node network model that included NSSI behaviors, the relationships among nodes in the 12-node network model (with NSSI behaviors removed) were clearer, with connections between NSSI thoughts and its related nodes being enhanced. This difference may also be explained by the influence of cognitive-emotional factors on NSSI primarily at the cognitive and motivational level, with the influence of NSSI thoughts being direct and on NSSI behaviors being indirect (ie, through the effect of NSSI thoughts).
Our network analysis, especially the 12-node network analysis with NSSI behaviors removed, found significant negative relationships between core self-evaluation and NSSI thoughts and between cognitive reappraisal and NSSI thoughts as well as a significant positive relationship between the disconnection/rejection EMS and NSSI thoughts. These results supported the cognitive-emotional model of NSSI,11 and were in line with the findings of previous studies. For example, a cross-lagged study reported that core self-evaluation was a stable predictor of NSSI.50 Individuals’ negative perceptions and evaluations of themselves may lead to self-depreciation and feelings of disgust; to avoid or escape such experiences, they may engage in self-punishing behaviors such as NSSI.27 Among the EMSs involved in the present study, dissociation/rejection has been identified as the most damaging and pervasive schema domain on NSSI.51 The defectiveness/shame and abandonment/instability schemas in the dissociation/rejection schema domain can lead to feelings of isolation from others, which are often accompanied by intense loneliness, shame, or anger.52–54
Regarding ER strategies, numerous studies have suggested that expressive suppression is positively associated with NSSI,55,56 and that cognitive reappraisal is negatively associated with NSSI.57 Specifically, inhibiting the external expression of internal pain may increase stress responses,58 and will not be helpful in alleviating negative emotions, thus potentially keeping unresolved emotional issues to accumulate,59 eventually individuals might become overwhelmed and will tend to adopt NSSI as a resolution. In contrast, the use of cognitive reappraisal as an emotion regulation strategy helps to alter one’s perceptions of events, which contributes to the reconstruction of stressful situations, relieves negative emotions,60 and improves one’s decision-making ability.61 Therefore, the maladaptive ER strategy of expressive suppression increases the risk of NSSI, whereas cognitive reappraisal decreases the risk of NSSI.
In addition to core self-evaluation and disconnection/rejection, emotional abuse was also significantly linked to NSSI thoughts. Emotional abuse is an important distal factor of NSSI. Childhood emotional abuse refers to a series of behaviors such as blaming, threatening, and humiliating towards the child.62 Nock et al suggests that the experience of emotional abuse may hinder the development of the ability to regulate strong negative emotions such as sadness and anger, leading to the adoption of NSSI to manage these emotions.63 Compared to other trauma subtypes, emotional abuse is the most severe and long-lasting type with the greatest impact on NSSI,64,65 which is in line with a meta-analysis revealing the highest effect size of emotional abuse on NSSI among all childhood trauma subtypes.66 In addition to being predictive of NSSI, emotional abuse is also highly correlated with depression and suicide later in life.67,68 In the network model, other nodes were able to indirectly influence NSSI thoughts through the bridging effects of emotional abuse and Disconnection/Rejection EMS. These findings indicated that emotional abuse and disconnection/rejection EMS might be important pathways for the interaction between NSSI and other nodes in the network.
The structural equation model indicated that the disconnection/rejection EMS partially mediated the effect of emotional abuse on NSSI thoughts, and that maladaptive ER strategies (eg, expressive suppression) aggravated the impact of emotional abuse on the disconnection/rejection EMS. Previous studies have found that experiences of emotional abuse and neglect may lead to maladaptive schemas such as low self-efficacy, interpersonal sensitivity, and feelings of abandonment among college students, and the reason might be that emotional abuse can be internalized in the form of overall negative beliefs about oneself, which in turn have long-term negative impacts.32 Schemas lead to automatic thinking and are persistent across time and situations.51 Young et al hypothesized that individuals with maladaptive schemas might come from cold, lonely, unpredictable, and often abusive families,31 which is supported by the results of the present study. Maladaptive schemas mediate the association between negative experiences and NSSI,69 which may lead to habitual blame on oneself for negative experiences and the adoption of NSSI as self-punishment. A previous study also showed that EMS mediated the relationship between stressful life events and NSSI.70 EMSs, as a mode of information processing, can influence one’s emotional response when they experience life events,71 and when negative emotional responses are so intense that they are hard to regulate effectively, individuals will engage in NSSI. The moderating effect of expressive suppression indicated that suppression of the expression of negative emotions might exacerbate the impact of childhood emotional abuse on the development of schemas, especially those in the domain of disconnection/rejection. From another perspective, expression of negative emotions may help individuals resolve their emotions through catharsis and seeking social support,72 making them less likely to develop the maladaptive schema of dissociation/rejection after the experience of emotional abuse. This result also supports the hypothesis that maladaptive ER strategies increase the risk of NSSI.11
Notably, in the network model of the present study, expressive suppression was not directly related to the thoughts and behaviors of NSSI but rather acted indirectly on NSSI through the bridging effect of other nodes such as the disconnection/rejection EMS and core self-evaluation. The reason might be that long-term repression of emotional expression exacerbates one’s internalization of negative beliefs about themselves, reduces the likelihood of receiving external attention and intervention, and depletes self-control resources, thereby leading to difficulties in emotion regulation;59,73 with the lack of effective emotion regulation strategies, individuals are more likely to engage in NSSIs as a way to mitigate their negative emotions.
The results of this study are also implicated in practical prevention and intervention efforts for NSSI. For instance, the NSSI risk screening for college students needs to focus on those who have experienced emotional abuse have low self-evaluation and are used to adopting expressive suppression as an emotion regulation strategy. In the intervention work of cognitive–behavioral therapy, the dissociation/rejection dimension of EMSs should be the focus of the cognitive aspect, and in the behavioral aspect of the intervention, by training cognitive reappraisal skills to increase the ability and frequency of using cognitive reappraisal strategies and to reduce the use of expressive suppression strategies, thereby reducing the incidence of NSSI.
Limitation
The present study has several limitations. Firstly, only a limited number of the cognitive and emotional factors were included in the present study, which may be more closely related to NSSI thoughts. Future research may include more factors closely related to NSSI behaviors, such as emotional response, impulsivity, and reward processing. Secondly, this study only focused on the five subtypes of childhood trauma without taking the time of occurrence, chronicity, and severity into account; other forms of early adversity, such as witnessing domestic violence, low family economic status, and peer bullying, which may also be risk factors for NSSI, were not included. Moreover, in addition to the frequency of NSSI thoughts and behaviors, the motivation, function, and severity of NSSI are also important aspects, which may be examined in future studies. Finally, due to the cross-sectional design, causality or temporal relationship involving the studied factors could not be established; thus, the findings of this study may serve as a basis for future research rather than for clinical judgment. Future studies should longitudinally assess both the distal and proximal factors of NSSI from a cognitive-emotional perspective.
Conclusion
The present study is one of the few studies using network analyses to explore the interrelationships between childhood trauma, cognitive and emotional risk factors, and NSSI among college students based on the cognitive-emotional model. Our findings emphasize the roles of childhood emotional abuse, low core self-evaluation, and expressive suppression as an emotion regulation strategy in the assessment of NSSI risk among college students and may provide guidance for the screening and intervention of high-risk populations.
Acknowledgments
We thank all the participants for completing the questionnaire.
Funding Statement
This study was funded by the Shanghai Changning District Medical Health Research Project (CNKW2022Y39), Changzhou City Application and Basic Research Project (CJ20230050), Jiangsu Province Preventive Medicine Research Project (Yl2023011), and the Educational Science Planning Project of Hunan Province (XJK22BXL002). The funders held no role in the development of this manuscript.
Disclosure
All authors declare no conflict of interest.
References
- 1.Nock MK. Self-injury. Ann rev clin psychol. 2010;6(1):339–363. doi: 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- 2.WHO. Suicide Worldwide in 2019: Global Health Estimates; 2021. [Google Scholar]
- 3.Plener PL, Brunner R, Fegert JM, et al. Treating nonsuicidal self-injury (NSSI) in adolescents: consensus based German guidelines. Child Adoles Psych Mental Health. 2016;10(1):46. doi: 10.1186/s13034-016-0134-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plener PL, Schumacher TS, Munz LM, Groschwitz RC. The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personality Disorder Emotion Dysreg. 2015;2(1):2. doi: 10.1186/s40479-014-0024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gandhi A, Luyckx K, Baetens I, et al. Age of onset of non-suicidal self-injury in Dutch-speaking adolescents and emerging adults: an event history analysis of pooled data. Comprehensive Psychiatry. 2018;80:170–178. doi: 10.1016/j.comppsych.2017.10.007 [DOI] [PubMed] [Google Scholar]
- 6.Mortier P, Cuijpers P, Kiekens G, et al. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol med. 2018;48(4):554–565. doi: 10.1017/s0033291717002215 [DOI] [PubMed] [Google Scholar]
- 7.O’Neill S, McLafferty M, Ennis E, et al. Socio-demographic, mental health and childhood adversity risk factors for self-harm and suicidal behaviour in College students in Northern Ireland. J Affective Disorders. 2018;239:58–65. doi: 10.1016/j.jad.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 8.Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self‐injury in nonclinical samples: systematic review, meta‐analysis and meta‐regression. Suicide Life-Threatening Behav. 2014;44(3):273–303. doi: 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- 9.Voss C, Hoyer J, Venz J, Pieper L, Beesdo-Baum K. Non-suicidal self-injury and its co-occurrence with suicidal behavior: an epidemiological-study among adolescents and young adults. Acta Psychiatrica Scandinavica. 2020;142(6):496–508. doi: 10.1111/acps.13237 [DOI] [PubMed] [Google Scholar]
- 10.Duncan-Plummer T, Hasking P, Tonta K, Boyes M. Cognitive-emotional networks in students with and without a history of non-suicidal self-injury. J Affective Disorders. 2023;329:394–403. doi: 10.1016/j.jad.2023.02.054 [DOI] [PubMed] [Google Scholar]
- 11.Hasking P, Whitlock J, Voon D, Rose A. A cognitive-emotional model of NSSI: using emotion regulation and cognitive processes to explain why people self-injure. Cognition Emotion. 2017;31(8):1543–1556. doi: 10.1080/02699931.2016.1241219 [DOI] [PubMed] [Google Scholar]
- 12.Dawkins JC, Hasking PA, Boyes ME, Greene D, Passchier C. Applying a cognitive‐emotional model to nonsuicidal self‐injury. Stress Health. 2019;35: 39–48. [DOI] [PubMed] [Google Scholar]
- 13.Zhou Q, Liu S, Chen J, et al. The role of sleep quality and anxiety symptoms in the association between childhood trauma and self-harm attempt: a chain-mediated analysis in the UK Biobank. J Affective Disorders. 2024;362:569–577. doi: 10.1016/j.jad.2024.07.041 [DOI] [PubMed] [Google Scholar]
- 14.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- 15.Sahle BW, Reavley NJ, Li W, et al. The association between adverse childhood experiences and common mental disorders and suicidality: an umbrella review of systematic reviews and meta-analyses. Eur Child Adolesc Psychiatry. 2021;2021:1–11. [DOI] [PubMed] [Google Scholar]
- 16.Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspectives Psychol Sci. 2011;6(6):589–609. doi: 10.1177/1745691611419672 [DOI] [PubMed] [Google Scholar]
- 17.Wan Y, Chen J, Sun Y, Tao F. Impact of childhood abuse on the risk of non-suicidal self-injury in mainland Chinese adolescents. PLoS One. 2015;10(6):e0131239. doi: 10.1371/journal.pone.0131239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. J Child Psychol Psychiatry. 2010;51(6):706–716. doi: 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gawęda Ł, Pionke R, Krężołek M, Frydecka D, Nelson B, Cechnicki A. The interplay between childhood trauma, cognitive biases, psychotic-like experiences and depression and their additive impact on predicting lifetime suicidal behavior in young adults. Psychol med. 2020;50(1):116–124. doi: 10.1017/S0033291718004026 [DOI] [PubMed] [Google Scholar]
- 20.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behavl Assess. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- 21.McKenzie KC, Gross JJ. Nonsuicidal self-injury: an emotion regulation perspective. Psychopathology. 2014;47(4):207–219. doi: 10.1159/000358097 [DOI] [PubMed] [Google Scholar]
- 22.Gross JJ. Antecedent-and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Personality Soc Psychol. 1998;74(1):224. doi: 10.1037/0022-3514.74.1.224 [DOI] [PubMed] [Google Scholar]
- 23.John OP, Gross JJ. Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J Personal. 2004;72(6):1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x [DOI] [PubMed] [Google Scholar]
- 24.Voon D, Hasking P, Martin G. The roles of emotion regulation and ruminative thoughts in non‐suicidal self‐injury. Br J Clin Psychol. 2014;53(1):95–113. doi: 10.1111/bjc.12030 [DOI] [PubMed] [Google Scholar]
- 25.Voon D, Hasking P, Martin G. Change in emotion regulation strategy use and its impact on adolescent nonsuicidal self-injury: a three-year longitudinal analysis using latent growth modeling. J Abnormal Psychol. 2014;123(3):487. doi: 10.1037/a0037024 [DOI] [PubMed] [Google Scholar]
- 26.Chen C, Chen F, Wang L, Wu M, Yang Z, F YU. A chain mediating model of emotion dysregulation and trait anger in the relationship between childhood abuse and aggressive behavior within the undergraduate students. Chinese J Behav Med Brain Sci. 2021;30(7):621–626. doi: 10.3760/cma.j.cn371468-20210127-00058 [DOI] [Google Scholar]
- 27.Barrocas AL, Jenness JL, Davis TS, et al. Developmental perspectives on vulnerability to nonsuicidal self-injury in youth. Advn Child Dev Behav. 2011;40:301–336. [DOI] [PubMed] [Google Scholar]
- 28.Dunkel-Schetter C. Differentiating the cognitive and behavioral aspects of social support. Soc Support. 1990;1990:267–296. [Google Scholar]
- 29.Hodgson S. Cutting through the silence: a sociological construction of self‐injury. Sociol Inquiry. 2004;74(2):162–179. doi: 10.1111/j.1475-682X.2004.00085.x [DOI] [Google Scholar]
- 30.Forrester RL, Slater H, Jomar K, Mitzman S, Taylor PJ. Self-esteem and non-suicidal self-injury in adulthood: a systematic review. J Affective Disorders. 2017;221:172–183. doi: 10.1016/j.jad.2017.06.027 [DOI] [PubMed] [Google Scholar]
- 31.Young JE, Klosko JS, Weishaar ME. Schema therapy: a practitioner’s guide. New York: Guilford Press; 2003. [Google Scholar]
- 32.Wright MOD, Crawford E, Del Castillo D. Childhood emotional maltreatment and later psychological distress among college students: the mediating role of maladaptive schemas. Child Abuse Negl. 2009;33(1):59–68. doi: 10.1016/j.chiabu.2008.12.007 [DOI] [PubMed] [Google Scholar]
- 33.Gong J, Chan RC. Early maladaptive schemas as mediators between childhood maltreatment and later psychological distress among Chinese college students. Psychiatry Res. 2018;259:493–500. doi: 10.1016/j.psychres.2017.11.019 [DOI] [PubMed] [Google Scholar]
- 34.Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Ann rev clin psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 36.Barrat A, Barthelemy M, Pastor-Satorras R, Vespignani A. The architecture of complex weighted networks. Proc Natl Acad Sci. 2004;101(11):3747–3752. doi: 10.1073/pnas.0400087101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhong B-L, Yuan M-D, Li F, Sun P. The psychological network of loneliness symptoms among Chinese residents during the COVID-19 outbreak. Psychol res behav manag. 2023;16:3767–3776. doi: 10.2147/PRBM.S424565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hinze V, Ford T, Evans R, Gjelsvik B, Crane C. Exploring the relationship between pain and self-harm thoughts and behaviours in young people using network analysis. Psychol med. 2022;52(15):3560–3569. doi: 10.1017/S0033291721000295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou H-Y, Luo Y-H, Shi L-J, Gong J. Exploring psychological and psychosocial correlates of non-suicidal self-injury and suicide in college students using network analysis. J Affective Disorders. 2023;336:120–125. doi: 10.1016/j.jad.2023.05.089 [DOI] [PubMed] [Google Scholar]
- 40.Zhao X, Zhang Y, Li L, Zhou Y. Evaluation on reliability and validity of Chinese version of childhood trauma questionnaire. Chin J Clin Rehabil. 2005;2005(16):209–211. [Google Scholar]
- 41.Jiang W-J, Zhong B-L, Liu L-Z, Zhou Y-J, Hu X-H, Li Y. Reliability and validity of the Chinese version of the Childhood Trauma Questionnaire-Short Form for inpatients with schizophrenia. PLoS One. 2018;13(12):e0208779. doi: 10.1371/journal.pone.0208779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen W, Zhang G, Tian X, Luo J, Gao R, Yang T. Test of the emotion regulation questionnaire in the middle school students. Chin Mental Health J. 2020;34(03):206–211. [Google Scholar]
- 43.Cui L, Lin W, Oei TP. Factor structure and psychometric properties of the young schema questionnaire (short form) in Chinese undergraduate students. Int J Ment Health Addict. 2011;9:645–655. doi: 10.1007/s11469-010-9283-4 [DOI] [Google Scholar]
- 44.Du J, Zhang X, Zhao Y. Reliability, validation and construct confirmatory of core self-evaluations scale. Psychol Res. 2012;5(03):54–60. [Google Scholar]
- 45.Chen H, Pan B, Zhang C, Guo Y, Zhou J, Wang X. Revision of the non-suicidal self-injury behavior scale for adolescents with mental disorder. J Central South Univ. 2022;47(03):301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tibshirani R. Regression shrinkage and selection via the lasso. J Royal Statl Soc Series B. 1996;58(1):267–288. doi: 10.1111/j.2517-6161.1996.tb02080.x [DOI] [Google Scholar]
- 47.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Meth. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kiekens G, Hasking P, Claes L, et al. Predicting the incidence of non-suicidal self-injury in college students. Eur Psychiatry. 2019;59:44–51. doi: 10.1016/j.eurpsy.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 49.da Silva Bandeira BE, Dos Santos Júnior A, Dalgalarrondo P, de Azevedo RCS, Celeri EHVR. Nonsuicidal self-injury in undergraduate students: a cross-sectional study and association with suicidal behavior. Psychiatry Res. 2022;318:114917. doi: 10.1016/j.psychres.2022.114917 [DOI] [PubMed] [Google Scholar]
- 50.Wang S, Ding W, Song S, et al. The relationship between adolescent victimization, nonsuicidal self-injury, and core self-evaluation: a cross-lagged study. Curr Psychol. 2023;43:1–11. [Google Scholar]
- 51.Nicol A, Mak AS, Murray K, Kavanagh PS. Early maladaptive schemas in young people who self‐injure. J Clin Psychol. 2021;77(7):1745–1762. doi: 10.1002/jclp.23172 [DOI] [PubMed] [Google Scholar]
- 52.Calvete E, Orue I, Hankin BL. A longitudinal test of the vulnerability-stress model with early maladaptive schemas for depressive and social anxiety symptoms in adolescents. J Psychopathol Behav Assess. 2015;37:85–99. doi: 10.1007/s10862-014-9438-x [DOI] [Google Scholar]
- 53.Sigre‐Leirós VL, Carvalho J, Nobre P. Early maladaptive schemas and aggressive sexual behavior: a preliminary study with male college students. j Sex Med. 2013;10(7):1764–1772. doi: 10.1111/j.1743-6109.2012.02875.x [DOI] [PubMed] [Google Scholar]
- 54.Specht MW, Chapman A, Cellucci T. Schemas and borderline personality disorder symptoms in incarcerated women. J Behav Ther Exp Psych. 2009;40(2):256–264. doi: 10.1016/j.jbtep.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 55.Richmond S, Hasking P, Meaney R. Psychological distress and non-suicidal self-injury: the mediating roles of rumination, cognitive reappraisal, and expressive suppression. Arch Suicide Res. 2017;21(1):62–72. doi: 10.1080/13811118.2015.1008160 [DOI] [PubMed] [Google Scholar]
- 56.Hasking PA, Coric SJ, Swannell S, Martin G, Thompson HK, Frost AD. Brief report: emotion regulation and coping as moderators in the relationship between personality and self-injury. J Adolescence. 2010;33(5):767–773. doi: 10.1016/j.adolescence.2009.12.006 [DOI] [PubMed] [Google Scholar]
- 57.Zhao T, Zhong Y, Wei Y, SU Y, Dang Y, Wu X. Emotion regulation strategies and family function in non-suicidal self-injury adolescents. Chinese J Child Health Care. 2021;29(09):946–950. [Google Scholar]
- 58.Gross JJ. The emerging field of emotion regulation: an integrative review. Rev General Psychol. 1998;2(3):271–299. doi: 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- 59.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Personality Soc Psychol. 2003;85(2):348. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- 60.Joormann J, Gotlib IH. Emotion regulation in depression: relation to cognitive inhibition. Cognition Emotion. 2010;24(2):281–298. doi: 10.1080/02699930903407948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Heilman RM, Crişan LG, Houser D, Miclea M, Miu AC. Emotion regulation and decision making under risk and uncertainty. Emotion. 2010;10(2):257. doi: 10.1037/a0018489 [DOI] [PubMed] [Google Scholar]
- 62.Gu H, Ma P, Xia T. Childhood emotional abuse and adolescent nonsuicidal self-injury: the mediating role of identity confusion and moderating role of rumination. Child Abuse Negl. 2020;106:104474. doi: 10.1016/j.chiabu.2020.104474 [DOI] [PubMed] [Google Scholar]
- 63.Nock MK. Why do people hurt themselves? New insights into the nature and functions of self-injury. Current Dir Psychol Sci. 2009;18(2):78–83. doi: 10.1111/j.1467-8721.2009.01613.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Croyle KL, Waltz J. Subclinical self-harm: range of behaviors, extent, and associated characteristics. Am J Orthopsych. 2007;77(2):332–342. doi: 10.1037/0002-9432.77.2.332 [DOI] [PubMed] [Google Scholar]
- 65.Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behav Res Ther. 2007;45(10):2483–2490. doi: 10.1016/j.brat.2007.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry. 2018;5(1):51–64. doi: 10.1016/S2215-0366(17)30469-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brown GW, Craig TKJ, Harris TO, Handley RV, Harvey AL. Development of a retrospective interview measure of parental maltreatment using the childhood experience of care and abuse (CECA) instrument — a life-course study of adult chronic depression — 1. J Affective Disorders. 2007;103(1):205–215. doi: 10.1016/j.jad.2007.05.022 [DOI] [PubMed] [Google Scholar]
- 68.Blaauw E, Arensman E, Kraaij V, Winkel FW, Bout R. Traumatic life events and suicide risk among jail inmates: the influence of types of events, time period and significant others. J Traumatic Stress. 2002;15(1):9–16. doi: 10.1023/A:1014323009493 [DOI] [PubMed] [Google Scholar]
- 69.Faura-Garcia J, Orue I, Calvete E. Cyberbullying victimization and nonsuicidal self-injury in adolescents: the role of maladaptive schemas and dispositional mindfulness. Child Abuse Negl. 2021;118:105135. doi: 10.1016/j.chiabu.2021.105135 [DOI] [PubMed] [Google Scholar]
- 70.Liu J, Wang Y, Liu X, Li J, Xing S. Experiencing stress impact on adolescent repetitive nonsuicidal self-injury: the mediating role of emotion dysregulation and maladaptive cognitive schemas. J Affective Disorders. 2023;339:392–399. doi: 10.1016/j.jad.2023.07.074 [DOI] [PubMed] [Google Scholar]
- 71.Dozois D, Martin R, Bieling P. Early maladaptive schemas and adaptive/maladaptive styles of humor. Cognitive Ther Res. 2008;33:585–596. doi: 10.1007/s10608-008-9223-9 [DOI] [Google Scholar]
- 72.Lee S, Kim B. Cognitive and emotional processes and life satisfaction of Korean adults with childhood abuse experience according to the level of emotional expressiveness. Psychol Rep. 2022;125(4):1957–1976. doi: 10.1177/00332941211012622 [DOI] [PubMed] [Google Scholar]
- 73.Cutuli D. Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Fronti sys neurosci. 2014;8:175. doi: 10.3389/fnsys.2014.00175 [DOI] [PMC free article] [PubMed] [Google Scholar]