Abstract
Objective
The most effective methods and entry sites for laparoscopic surgery remain a subject of ongoing investigation and discussion. The purpose of the study was to analyze and compare three umbilical entry sites for intraperitoneal access using the direct trocar insertion technique.
Material and Methods
A randomized pilot study was conducted between March 2021 and January 2023, involving women eligible for laparoscopic gynecological surgery. The women were allocated to one of three equally sized groups based on trocar entry points: subumbilical, supraumbilical, or umbilical. Success and failure rates of trocar entry, factors influencing success or failure, and early and late complications were systematically evaluated and compared across groups.
Results
A total of 243 patients, with a mean age of 32.93±8.33 years, were included in three groups of 81 each. Trocar entry success rates were 97.5%, 89.2%, and 89.5% in the supraumbilical, umbilical, and subumbilical groups, respectively (p>0.05). Failed trocar entry was significantly associated with age, gravidity, body mass index (BMI), waist circumference, hip circumference, and abdominal subcutaneous fat thickness (p<0.001). Regression analysis revealed that, in the subumbilical group, higher gravidity [odds ratios (OR): 0.390, 95% confidence interval (CI): 0.174-0.872, p=0.022) and greater abdominal subcutaneous fat thickness (OR: 0.090, 95% CI: 0.019-0.431, p=0.03) were associated with lower odds of successful trocar entry. In contrast, in the umbilical group, a higher waist circumference was associated with lower odds of successful trocar entry (OR: 0.673, 95% CI: 0.494-0.918, p=0.012). None of the covariates were significant in the supraumbilical group.
Conclusion
The study highlighted the importance of selecting the appropriate trocar entry site in laparoscopic gynecological surgery. Surgeons should consider factors such as age, gravidity, BMI, waist circumference, hip circumference, and abdominal subcutaneous fat thickness, as these factors significantly influence the success of trocar entry.
Keywords: Trocar insertion, laparoscopic surgery, complications, gynecologic surgery
Introduction
Laparoscopy, a versatile diagnostic and surgical procedure employed in a variety of surgical specialties, has numerous advantages for patients, healthcare systems, and society at large. The recent years have witnessed a significant enhancement in the proficiency of gynecologists in conducting both fundamental and sophisticated endoscopic procedures (1). An extensive meta-analysis incorporating findings from 27 randomized controlled trials comparing laparoscopy and laparotomy for benign gynecological procedures reported a notable 40% reduction in the risk of minor complications associated with laparoscopy. However, the risk of major complications remains comparable between the two surgical approaches (2). Significantly, trocar insertion, serving as the primary entry point in laparoscopic procedures, continues to present substantial risks, contributing to 40% of laparoscopic complications and the majority of fatalities associated with this surgical approach (3, 4). Life-threatening complications, including bowel and abdominal vessel perforations, underscore the critical nature of trocar insertion; 81% of trocar-related deaths are attributed to vascular injuries and 19% to intestinal injuries (5). Besides, minor complications, such as extraperitoneal insufflation, postoperative infection, subcutaneous emphysema, and trocar site hernia are also associated with laparoscopic entry (6, 7). Despite the existence of various laparoscopic entry methods, including the Veress needle (VER), direct trocar insertion (DIR), and open (OP) techniques, there is no clear consensus regarding the optimal method (8, 9, 10). Indeed, each technique possesses its own set of advantages and disadvantages, and the choice of the entry method frequently depends on the surgeon’s experience, training, and preference (3, 8, 9, 11).
Clinicians do not concur about the optimal method of entering the peritoneal cavity (12, 13). The ongoing debate about the methods and sites of initial entry underscores the need for further research in this field (14). The aim of the present study was to compare three umbilical entry sites, subumbilical, supraumbilical, and umbilical, for intraperitoneal access using the DIR technique.
Material and Methods
Study design and participants
This randomized pilot study was conducted at Afzalipour Hospital, affiliated with Kerman University of Medical Sciences, Kerman, Iran, from March 2021 and January 2023. Three umbilical entry sites (subumbilical, supraumbilical, umbilical) for intraperitoneal access in the DIR technique were compared. Women who could undergo gynecological laparoscopy, without a history of abdominal surgery, scars, contraindications for laparoscopic surgery, umbilical hernia, burns in the umbilical region, underlying heart or lung disease, gynecological malignancy, or the use of anticoagulant medication, were considered eligible. Women who were willing to participate in the study were included. Those requiring conversion to laparotomy, diagnosed with malignancy, transferred to an intensive care unit, or refusing further participation were excluded. The CONSORT flow diagram is shown in Figure 1.
Figure 1.
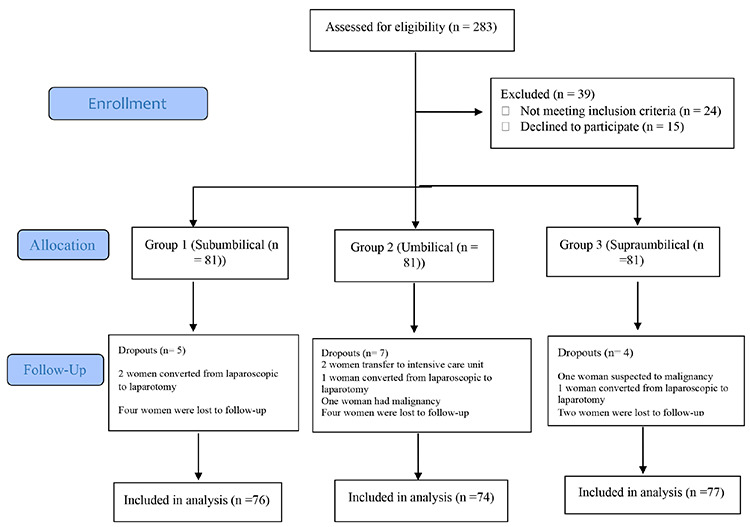
Diagram of the study
Intervention and randomization of study participants
Prior to the intervention, the objectives of the study were explained to the patients in detail. They were also informed of the confidentiality of information and the voluntary nature of their participation. Informed consent was obtained from each participant. A total of 243 patients were randomly assigned to one of three equally sized groups: subumbilical (n=81), umbilical (n=81), or supraumbilical (n=81). Randomization was performed using a computer-generated random table block of size 6 (e.g., ABCABC, AABBCC, and all other possible restricted permutations).
Coded envelopes were created by a nurse who was not involved in the research project. The envelopes were prepared using sequential numbers, and patients were then allocated to one of the three groups, based on the assignment in the coded envelopes. All laparoscopic surgeries were performed by the primary gynecologic surgeon (Gh.M.) under general anesthesia using Storz endoscopic tools (Karl Storz). All patients were placed in the supine position, and a vertical or transverse incision was appropriately widened (1.0-1.5 cm) to allow for trocar insertion. Access to the abdominal cavity was achieved using a direct trocar in all patients. For initial intraperitoneal access, incisions were made either subumbilically (1-2 cm below the lower transverse fold of the navel), at the umbilicus, or supraumbilically (1-2 cm above the upper transverse fold of the navel). The trocar entry sites for intraperitoneal access were randomized. A 10 mm trocar was inserted, and a pneumoperitoneum was achieved by carbon dioxide insufflation to a pressure of 12-14 mmHg. The surgical procedures were conducted using conventional laparoscopic instruments under vision with a rigid 0-degree, 10 mm telescope (Karl Storz Company, Germany). The success of trocar insertion was established with a telescope. The fascia was repaired using Vicryl 1 thread and skin closure performed using 0.3 nylon.
Outcomes, measurements, and follow-up
In each group success and failure rates of trocar entry, factors influencing success or failure, and early and late complications were systematically evaluated. Successful trocar entry was defined as the trocar entering the abdominal cavity after one or two attempts. More than two attempts or the need to switch to another entry technique was considered a failed entry.
Factors contributing to success or failure included gravidity, body mass index (BMI) in kg/m2, waist and hip circumferences, and abdominal subcutaneous fat thickness. Postoperative complications were categorized as early (including damage to vessels and viscera, ileus, postoperative fever, and bleeding/hematoma) and late (including hernia, wound infection, hematoma, and pain at the operative site).
All outcomes were compared among groups, and baseline parameters such as age, gravidity, weight, height, BMI, waist and hip circumferences, and abdominal subcutaneous fat thickness were recorded prior to the intervention. Waist circumference was measured using a flexible non-elastic measuring tape, midway between the lowest costal margin and the anterior superior iliac spine at the end of normal expiration, while hip circumference was measured at the widest part of the hip in a standing position. Abdominal subcutaneous fat thickness was measured using a caliper (Holtain, Dyfed, UK) with 0.2 mm accuracy, following a standardized protocol (15). Abdominal subcutaneous fat thickness was measured on the right side of the body with the patient standing upright. The exact measuring sites were selected and found according to Eston and Reilly (16), with the horizontal fold raised 3 cm lateral and 1 cm inferior to the umbilicus.
Measurements were conducted by an experienced and trained nurse. The duration of laparoscopic surgery and indications were recorded at the end of the surgery. All participants were followed up for 6-8 weeks, and any complications were documented in the patients’ files.
Ethical considerations
In all steps carried out in this study, the principles of the Declaration of Helsinki (ethical principles for medical research involving human subjects) and the Ethics Committee of Kerman University of Medical Sciences were followed. The study was approved by the ethics committee of the Afzalipour Hospital-Kerman University of Medical Sciences (approval number: IR.KMU.AH.REC.1400.168, date: 25.10.2021), and registered at the Iranian Registry of Clinical Trials (no: IRCT20230307057644N1). The objectives of the trial were explained to women enrolling in the trial, and their written informed consent was obtained. The subjects were free to discontinue their participation at any time. All personal data were treated confidentially and only reported in collective form.
Statistical analysis
The statistical software program IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA), was used for data analysis. Quantitative variables were described using means (standard deviation), and qualitative variables were described using frequencies (percentage). The chi-square test was employed for qualitative variables. Normal distribution of quantitative data was assessed using the one-sample Kolmogorov-Smirnov test. Student’s t-test and ANOVA were used to examine intragroup differences. Logistic regression models utilizing the backward (Wald) method were employed to assess the association between successful trocar entry and entry site. Estimates were adjusted for age, gravidity, BMI, waist and hip circumferences, and abdominal subcutaneous fat thickness. Dependent variables were categorized as successful (1) or failed (0) trocar entry. Estimated logits and odds ratios (OR) with corresponding 95% confidence intervals (CI) 95% were reported, and the level of significance was set to 0.05.
Results
Of 283 eligible patients, 243 were included in the study (81 cases in each group). Five, seven, and four cases were excluded from the first, second, and third groups, respectively (Figure 1). The mean age of the patients was 32.93±8.3 years, with no significant differences in demographic or clinical characteristics between the three groups prior to the intervention (Table 1). Indications for surgery included hysterectomy, cystectomy, myomectomy, infertility, ectopic pregnancy, and diagnostic laparoscopy. Differences in the indications for surgery and the duration of surgery did not differ significantly between groups.
Table 1. Comparison of demographic and clinical characteristics between groups prior to intervention.
|
Variable |
Subumbilical, (n=76) |
Umbilical, (n=74) |
Supraumbilical, (n=77) |
p* |
|
|
Age, years |
Min.-max. |
18-51 |
18-57 |
19-57 |
0.65 |
|
Mean ± SD |
32.8±7.87 |
33.6±8.6 |
32.4±8.5 |
||
|
Gravidity, (n) |
Min.-max. |
0-5 |
0-5 |
0-5 |
0.25 |
|
Mean ± SD |
2.01±1.5 |
1.9±1.4 |
1.6±1.3 |
||
|
BMI, kg/m2 |
Min.-max. |
18.2-43.7 |
17.5-47 |
18-47.5 |
0.3 |
|
Mean ± SD |
31.2±6.03 |
32.7±6.9 |
31.3±7.3 |
||
|
Waist circumstance, cm |
Min.-max. |
69-130 |
68-128 |
67-130 |
0.5 |
|
Mean ± SD |
91.6±12.3 |
94±13.3 |
93.28±15.8 |
||
|
Hip circumstance, cm |
Min.-max. |
85-142 |
85-149 |
82-150 |
0.3 |
|
Mean ± SD |
108.3±12.06 |
111.5±12.8 |
109.7±15.49 |
||
|
Abdominal subcutaneous fat thickness, cm |
Min.-max. |
0.5-6.5 |
0.5-6 |
0.5-6.5 |
0.43 |
|
Mean ± SD |
3.25±1.34 |
3.55±1.38 |
3.47±1.57 |
||
*Comparison of three groups prior to intervention by ANOVA, SD: Standard deviation, min.: Minimum, max.: Maximum, BMI: Body mass index
Failure and success rates of trocar entry into the abdomen in the three groups are presented in Table 2. As shown in Table 2, the overall success rate of entry was 92.9% while the success rates in the subumbilical, umbilical and supraumbilical groups were 89.5% (68/76), 89.2% (66/74), and 97.5% (75/77), respectively. The successful entry rate was higher in the supraumbilical group than in the umbilical and subumbilical groups, but the difference was not significant.
Table 2. Failure and success rates of trocar entry in the studied groups.
|
Subumbilical, (n=76) |
Umbilical, (n=74) |
Supraumbilical, (n=77) |
Total |
p* |
|||
|
Number (%) |
|||||||
|
Success and failure in trocar entry |
Failed |
8 (10.5) |
8 (10.8) |
2 (2.6) |
18 (7.9) |
0.1 |
|
|
Successful |
First entry |
52 (68.4) |
45 (60.8) |
61 (79.2) |
158 (69.6) |
||
|
Second entry |
16 (21.1) |
21(28.4) |
14 (18.2) |
51 (22.5) |
|||
*Chi-square (χ2)
Age, gravidity, BMI, waist circumference, hip circumference, and abdominal subcutaneous fat thickness were systematically compared between successful and failed trocar entries in each of the three groups. As detailed in Table 3, patients with failed trocar entry across all groups exhibited a significantly older age, and higher gravidity, BMI, waist circumference, hip circumference, and abdominal subcutaneous fat thickness compared to those with successful trocar entry (p<0.001).
Table 3. Success and failure of trocar insertion according to the studied variables in the three groups.
|
Subumbilical, (n=76) |
p† |
Umbilical, (n=74) |
p† |
Supraumbilical, (n=77) |
p† |
||||
|
Successful, (n=68) |
Failed, (n=8) |
Successful, (n=66) |
Failed, (n=8) |
Successful, (n=75) |
Failed, (n=2) |
||||
|
Mean ± SD | |||||||||
|
Age, y |
32.5±7.9 |
35.38±7.34 |
0.001 |
33.08±8.8 |
38.13±4.6 |
0.001 |
32.11±8.5 |
42.5±6.3 |
0.001 |
|
Gravidity, (n) |
1.91±1.5 |
2.87±1.4 |
0.001 |
1.8±1.39 |
2.75±1.28 |
0.001 |
1.62±1.4 |
2±0 |
0.001 |
|
BMI, kg/m2 |
30.31±5.5 |
38.87±4 |
0.001 |
31.64±6.38 |
42.01±3.37 |
0.001 |
31.09±7.3 |
40.35±0.91 |
0.001 |
|
Waist circumstance, cm |
89.61±10.91 |
108.75±11.28 |
0.001 |
91.43±11.63 |
115.12±6.49 |
0.001 |
92.61±15.31 |
118.5±4.9 |
0.001 |
|
Hip circumstance, cm |
106.5±11.11 |
123.37±9.42 |
0.001 |
109.25±11.28 |
130.87±7.73 |
0.001 |
109.1±15.21 |
132.5±6.36 |
0.001 |
|
Abdominal subcutaneous fat thickness, cm |
3.03±1.2 |
5.11±0.9 |
0.001 |
3.3±1.26 |
5.5±0.34 |
0.001 |
3.4±1.5 |
5.95±0.35 |
0.001 |
†Success and failure in each group compared by Student’s t-test, BMI: Body mass index, MD: Mean differences, SD: Standard deviation
Logistic regression was used to analyze successful trocar entry, adjusting for age, gravidity, BMI, waist circumference, hip circumference, and abdominal subcutaneous fat thickness. In the subumbilical group, the regression results demonstrated that the odds of success entry decreased with higher gravidity (OR: 0.390, 95% CI: 0.174-0.872, p=0.022) and abdominal subcutaneous fat thickness (OR: 0.090, 95% CI: 0.019-0.431, p=0.03). The remaining covariates (age, BMI, waist circumference, and hip circumference) were not statistically significant. In the umbilical group, a greater waist circumference was associated with decreased odds of successful entry (OR: 0.673, 95% CI: 0.494-0.918, p=0.012). In the supraumbilical group, none of the covariates reached statistical significance. The results of the multiple logistic regression analysis of successful trocar entry are summarized in Table 4.
Table 4. Binary logistic regression of the effects of variables on successful or failed entry.
|
Groups |
Predictors |
B |
S.E. |
OR |
95% CI |
Wald |
p |
|
Model | |||||||
|
Subumbilical |
Age |
-0.089 |
0.081 |
0.915 |
0.780-1.073 |
1.200 |
0.273 |
|
Gravidity |
-0.942 |
0.411 |
0.390 |
0.174-0.872 |
5.261 |
0.022 |
|
|
BMI |
-0.072 |
0.220 |
0.931 |
0.605-1.431 |
0.107 |
0.743 |
|
|
Waist circumstance |
0.063 |
0.189 |
1.066 |
0.735-1.54 |
0.113 |
0.737 |
|
|
Hip circumstance |
-0.132 |
0.130 |
0.876 |
0.679-1.130 |
1.039 |
0.308 |
|
|
Abdominal subcutaneous fat thickness |
-2.409 |
0.799 |
0.090 |
0.019-0.431 |
9.082 |
0.003 |
|
|
Umbilical |
Age |
-0.214 |
0.113 |
0.808 |
0.647-1.008 |
3.565 |
0.059 |
|
Gravidity |
0.194 |
0.869 |
1.215 |
0.221-6.665 |
0.05 |
0.823 |
|
|
BMI |
-0.169 |
0.32 |
0.845 |
0.451-1.582 |
0.279 |
0.598 |
|
|
Waist circumstance |
-0.396 |
0.158 |
0.673 |
0.494-0.918 |
6.267 |
0.012 |
|
|
Hip circumstance |
0.325 |
0.343 |
1.384 |
0.706-2.713 |
0.894 |
0.344 |
|
|
Abdominal subcutaneous fat thickness |
-3.005 |
2.668 |
0.05 |
0-9.242 |
1.269 |
0.26 |
|
|
Supraumbilical |
Age |
-0.124 |
0.079 |
0.884 |
0.757-1.032 |
2.451 |
0.117 |
|
Gravidity |
1.899 |
1.754 |
6.679 |
0.215-207.92 |
1.172 |
0.279 |
|
|
BMI |
-11.011 |
334.183 |
0 |
0-4.73 |
0.001 |
0.974 |
|
|
Waist circumstance |
-0.14 |
0.081 |
0.869 |
0.742-1.018 |
3.013 |
0.083 |
|
|
Hip circumstance |
0.534 |
0.54 |
1.706 |
0.593-4.91 |
0.98 |
0.322 |
|
|
Abdominal subcutaneous fat thickness |
-191.306 |
4581.642 |
0 |
0-8.08 |
0.002 |
0.967 |
|
BMI: Body mass index, OR: Odds ratio, CI: Confidence interval
Complications included fever, bruising at the operation site, chronic pain, hematoma, and surgical site infection. As shown in Table 5, both early and late complications related to trocar entry tended to be lower in the supraumbilical and subumbilical groups than in the umbilical group. However, once again the differences were not statistically significant. A comparison of early and late complications of trocar entry into the abdomen among the three groups is provided in Table 5.
Table 5. Early and late complications of trocar entry into the abdomen in the three groups.
|
Subumbilical, (n=76) |
Umbilical, (n=74) |
Supraumbilical, (n=77) |
p* |
||
|
Number (%) |
|||||
|
Early postoperative complications |
Fever |
3 (3.94) |
10 (13.51) |
2 (2.59) |
0.099 |
|
Bruising at the operation site |
5 (6.57) |
6 (8.1) |
7 (9.09) |
||
|
Late postoperative complications |
Chronic pain |
3 (3.94) |
4 (5.4) |
6 (7.8) |
|
|
Hematoma |
0 |
1 (1.35) |
1 (1.29 |
||
|
Surgical site infection |
5 (6.57) |
4 (5.4) |
4 (5.19) |
||
|
Total |
16 (21.05) |
24 (32.43) |
20 (25.97) |
||
*Chi-square (χ2)
Discussion
The advancement of laparoscopic surgical techniques in recent decades has notably improved patient safety and reduced complications. In view of the fact that a significant number of laparoscopic complications occur during abdominal entry, the method of accessing the abdomen is of importance (13). The umbilicus is commonly selected as the site for primary trocar insertion because it offers the shortest distance between the skin and the anterior peritoneum, is cosmetically appealing, and its anatomic relation to vital retroperitoneal structures is well understood. The specific site of trocar entry has not been extensively evaluated (17), although a number of authors have analyzed and compared the outcomes of different entry techniques (14). To fill this gap, we undertook a comparison of three umbilical entry sites for intraperitoneal access using the DIR technique in laparoscopic gynecological surgery. Our findings revealed an overall failed trocar entry rate of 7.9%, which is consistent with previously reported rates of 7.8% to 35% (18, 19). While we registered a higher success rate in the supraumbilical group than in the umbilical or subumbilical groups, the difference was not significant. Although we were unable to compare our findings with others due to the absence of specific studies on the optimal trocar entry site for laparoscopic gynecological surgery, Stanhiser et al. (17) reported theoretic modelling and suggested that supraumbilical primary port placement is superior to umbilical entry in laparoscopy. This is because supraumbilical entry provides a greater distance to retroperitoneal vessels compared to umbilical entry, potentially reducing the risk of vascular injury (17).
Compeau et al. (20) reviewed general surgical practices in Canada regarding laparoscopic entry, including 248 of 1000 members of the Canadian Association of General Surgeons. The findings showed that, in a virgin abdomen, the umbilical region was the primary port site, with 51.5% of surgeons favoring infraumbilical entry and 35.7% preferring supraumbilical entry. In addition, when peritoneal adhesions were known or suspected, the umbilical site remained the most popular choice for entry location (20). Şentürk et al. (21) evaluated the cosmetic outcomes of infraumbilical, supraumbilical, and transumbilical entry routes in laparoscopic surgery in 2018, and found no statistically significant differences in cosmetic results between the three groups.
We focused on the site of trocar entry and assessed success based on various factors: patients with failed trocar entry tended to be older, had higher gravidity, were more obese, and possessed a greater waist and hip circumference, as well as increased abdominal subcutaneous fat thickness. In the study of Warchałowski et al. (22), factors such as age, gender, neurological disease, and diabetes were predictor variables of laparoscopic surgery success and failure. In contrast, Tam et al. (23) found no statistically significant difference in patient characteristics (age and BMI) and the success of the surgery.
Subgroup analysis further identified associations between specific factors and trocar entry success or failure within each entry site group. In the subumbilical trocar entry group, higher gravidity and abdominal subcutaneous fat thickness were associated with failed trocar entry. In the umbilical group, a greater waist circumference was a significant predictor of failed entry. However, in the supraumbilical group, none of the covariates achieved statistical significance. This finding is consistent with the published literature, which supports different trocar insertion locations based on various factors (17, 24). In gynecological surgery, when dealing with cases involving large uteri or pelvic masses, the use of a primary umbilical port is severely limited due to its close proximity to the uterus or pelvic mass. This limitation reduces operative exposure and significantly complicates instrument manipulation as well as the overall surgical procedures (17). In cases of large fibroid uteri during myomectomy or hysterectomy (25), adnexal masses requiring cystectomy or oophorectomy (26), and surgery in pregnant patients, the use of a supraumbilical port has proven beneficial (27, 28). These ports provide better exposure and easier instrument manipulation, thereby facilitating minimally invasive procedures and avoiding injury to the pregnant uterus (17). In addition, Hurd et al. (24) found that the position of the umbilicus relative to major vessels varied significantly with BMI. In women of normal weight the umbilicus was 0.4 cm caudal to the aortic bifurcation, while in overweight and obese women it was 2.4 and 2.9 cm caudal, respectively (24). These anatomical differences highlight the need for alternative entry locations and techniques in obese patients in order to reduce surgical risks.
An inherent challenge in trocar entry is the possibility of delayed recognition of injury, potentially necessitating abdominal repair (29). We registered postoperative complications such as fever, bruising at the operation site, chronic pain, hematoma, and surgical site infection. Notably, complications associated with trocar entry tended to be less frequent in the supraumbilical and subumbilical groups compared to the umbilical group, but the differences were not significant. In line with our findings, a study conducted by Jategaonkar et al. (30) involving 2,300 patients suggests that trocar entry through the umbilicus is safe due to the thinness of the umbilicus. Conversely, Stanhiser et al. (17) reported that primary supraumbilical port placement is safer than entry through the umbilicus in laparoscopy, probably because the distance to retroperitoneal vessels was greater when the supraumbilical entry site was used.
Study limitations
The principal strength of the present study is its randomized clinical design to evaluate factors influencing the success and complications of trocar entry sites in laparoscopic gynecological surgery. The study effectively mitigated confounding variables, ensuring comparability between the three groups and enhancing the validity of the results. Despite the valuable insights provided by the investigation, its inherent limitations are worthy of mention. Prime among these is the relatively small sample size. Future studies should prioritize the design and execution of high-quality, long-term clinical studies featuring larger sample sizes. This approach will be essential for a comprehensive exploration of life-threatening issues, thereby substantiating and extending the findings of the current study.
Conclusion
The present investigation is a significant contribution to laparoscopic gynecological surgery in that it provides a comprehensive evaluation of the impact of trocar entry site on surgical success rates and postoperative complications. Our findings emphasize the importance of tailoring entry site selection based on patient-specific factors, such as gravidity, abdominal subcutaneous fat thickness, and waist circumference, for the purpose of optimizing surgical outcomes. Patients with higher gravidity and abdominal subcutaneous fat thickness exhibited increased odds of failed trocar entry, particularly in the subumbilical entry group. A greater waist circumference was also associated with a greater likelihood of failed entry in the umbilical group. These insights underscore the need for surgeons to carefully consider patient characteristics when determining the most suitable trocar entry site. While our study sheds light on the impact of the trocar entry site, further research will be needed to refine entry techniques and assess their impact on surgical outcomes. Continued investigation in this field will contribute to the ongoing enhancement of laparoscopic gynecological surgery, ultimately leading to better patient care and improved outcomes.
Footnotes
Ethics Committee Approval: The study was approved by the Ethics Committee of the Afzalipour Hospital-Kerman University of Medical Sciences (approval number: IR.KMU.AH.REC.1400.168, date: 25.10.2021).
Informed Consent: Informed consent was obtained from each participant.
Author Contributions: Surgical and Medical Practices: G.M.; Concept: G.M., A.N.; Design: G.M., A.N.; Data Collection or Processing: G.M., A.N., F.K.R.; Analysis or Interpretation: H.S., L.A., I.A.; Literature Search: G.M., H.S., L.A.; Writing: G.M., F.K.R., H.S., L.A., I.A.
Conflict of Interest: No conflict of interest is declared by the authors.
Financial Disclosure: This study was funded by Kerman University of Medical Sciences (grant code: 400000399).
Contributor Information
Afsaneh Nikseresht, Email: Nikseresht@yahoo.com.
Leila Allahqoli, Email: lallahqoli@gmail.com.
References
- 1.Pascual-Pedreño A, Perez-Medina T, Brouard Urkiaga I, Fernández-Parra J, Sobreviela-Laserrada M. Practice of endoscopic gynecologic surgery: a survey of Spanish gynecologists. Eur J Obstet Gynecol Reprod Biol. 2013;169(1):64–8. doi: 10.1016/j.ejogrb.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Chapron C, Fauconnier A, Goffinet F, Bréart G, Dubuisson JB. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a meta-analysis. Hum Reprod. 2002;17:1334–42. doi: 10.1093/humrep/17.5.1334. [DOI] [PubMed] [Google Scholar]
- 3.Fuller J, Ashar BS, Carey-Corrado J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12(4):302–7. doi: 10.1016/j.jmig.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Shirk GJ, Johns A, Redwine DB. Complications of laparoscopic surgery: How to avoid them and how to repair them. J Minim Invasive Gynecol. 2006;13(4):352–9. doi: 10.1016/j.jmig.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192(6):677–83. doi: 10.1016/s1072-7515(01)00913-9. [DOI] [PubMed] [Google Scholar]
- 6.Magrina JF. Complications of laparoscopic surgery. Clin Obstet Gynecol. 2002;45(2):469–80. doi: 10.1097/00003081-200206000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Swank HA, Mulder IM, la Chapelle CF, Reitsma JB, Lange JF, Bemelman WA. Systematic review of trocar-site hernia. Br J Surg. 2012;99(3):315–23. doi: 10.1002/bjs.7836. [DOI] [PubMed] [Google Scholar]
- 8.Ahmad G, Baker J, Finnerty J, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2019;1(1):CD006583. doi: 10.1002/14651858.CD006583.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vilos GA, Ternamian A, Dempster J, Laberge PY. J Obstet Gynaecol Can. 2007;29(7):433–47. doi: 10.1016/j.jogc.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 10.Krishnakumar S, Tambe P. Entry complications in laparoscopic surgery. J Gynecol Endosc Surg. 2009;1(1):4–11. doi: 10.4103/0974-1216.51902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fader AN, Cohen S, Escobar PF, Gunderson C. Laparoendoscopic single-site surgery in gynecology. Curr Opin Obstet Gynecol. 2010;22(4):331–8. doi: 10.1097/GCO.0b013e32833be979. [DOI] [PubMed] [Google Scholar]
- 12.Merlin TL, Hiller JE, Maddern GJ, Jamieson GG, Brown AR, Kolbe A. Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg. 2003;90(6):668–79. doi: 10.1002/bjs.4203. [DOI] [PubMed] [Google Scholar]
- 13.Molloy D, Kaloo PD, Cooper M, Nguyen TV. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42(3):246–54. doi: 10.1111/j.0004-8666.2002.00246.x. [DOI] [PubMed] [Google Scholar]
- 14.Angioli R, Terranova C, De Cicco Nardone C, Cafà EV, Damiani P, Portuesi R. A comparison of three different entry techniques in gynecological laparoscopic surgery: a randomized prospective trial. Eur J Obstet Gynecol Reprod Biol. 2013;171:339–42. doi: 10.1016/j.ejogrb.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Hume P, Marfell-Jones M. The importance of accurate site location for skinfold measurement. J Sports Sci. 2008;26(12):1333–40. doi: 10.1080/02640410802165707. [DOI] [PubMed] [Google Scholar]
- 16.Eston RG, Reilly T. Kinanthropometry and Exercise Physiology Laboratory Manual. Routledge London; 2001. [Google Scholar]
- 17.Stanhiser J, Goodman L, Soto E, Al-Aref I, Wu J, Gojayev A. Supraumbilical primary trocar insertion for laparoscopic access: the relationship between points of entry and retroperitoneal vital vasculature by imaging. Am J Obstet Gynecol. 2015;213:506. doi: 10.1016/j.ajog.2015.05.060. [DOI] [PubMed] [Google Scholar]
- 18.Borgatta L, Gruss L, Barad D, Kaali SG. Direct trocar insertion vs. Verres needle use for laparoscopic sterilization. J Reprod Med. 1990;35(9):891–4. [PubMed] [Google Scholar]
- 19.Ertugrul I, Kayaalp C, Yagci MA, Sumer F, Karagul S, Tolan K. Comparison of Direct Trocar Entry and Veress Needle Entry in Laparoscopic Bariatric Surgery: Randomized Controlled Trial. J Laparoendosc Adv Surg Tech A. 2015;25(11):875–9. doi: 10.1089/lap.2015.0317. [DOI] [PubMed] [Google Scholar]
- 20.Compeau C, McLeod NT, Ternamian A. Laparoscopic entry: a review of Canadian general surgical practice. Can J Surg. 2011;54(5):315–20. doi: 10.1503/cjs.011210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Şentürk MB, Doğan O, Polat M, Kılıçcı Ç, Pulatoğlu Ç, Tayyar AT. Cosmetic outcomes of infraumbilical, supraumbilical, and transumbilical entry routes in laparoscopic surgery. Turk J Surg. 2018;34(4):290–4. doi: 10.5152/turkjsurg.2018.4025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Warchałowski Ł, Łuszczki E, Bartosiewicz A, Dereń K, Warchałowska M, Oleksy Ł. The Analysis of Risk Factors in the Conversion from Laparoscopic to Open Cholecystectomy. Int J Environ Res Public Health. 2020;17(20):7571. doi: 10.3390/ijerph17207571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tam T, Harkins G, Wegrzyniak L, Ehrgood S, Kunselman A, Davies M. Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol. 2014;21(6):1015–21. doi: 10.1016/j.jmig.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Hurd WW, Bude RO, DeLancey JO, Pearl ML. The relationship of the umbilicus to the aortic bifurcation: implications for laparoscopic technique. Obstet Gynecol. 1992;80:48–51. [PubMed] [Google Scholar]
- 25.Choi JS, Kyung YS, Kim KH, Lee KW, Han JS. The four-trocar method for performing laparoscopically-assisted vaginal hysterectomy on large uteri. J Minim Invasive Gynecol. 2006;13(4):276–80. doi: 10.1016/j.jmig.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Macciò A, Madeddu C, Kotsonis P, Pietrangeli M, Paoletti AM. Large twisted ovarian fibroma associated with Meigs’ syndrome, abdominal pain and severe anemia treated by laparoscopic surgery. BMC Surg. 2014;14:38. doi: 10.1186/1471-2482-14-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yuen PM, Ng PS, Leung PL, Rogers MS. Outcome in laparoscopic management of persistent adnexal mass during the second trimester of pregnancy. Surg Endosc. 2004;18(9):1354–7. doi: 10.1007/s00464-003-8283-x. [DOI] [PubMed] [Google Scholar]
- 28.Tazuke SI, Nezhat FR, Nezhat CH, Seidman DS, Phillips DR, Nezhat CR. Laparoscopic management of pelvic pathology during pregnancy. J Am Assoc Gynecol Laparosc. 1997;4(5):605–8. doi: 10.1016/s1074-3804(05)80097-0. [DOI] [PubMed] [Google Scholar]
- 29.Alkatout I. Complications of Laparoscopy in Connection with Entry Techniques. J Gynecol Surg. 2017;33(3):81–91. doi: 10.1089/gyn.2016.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jategaonkar PA, Jategaonkar SP, Yadav SP. A simple and safe method for creating closed pneumoperitoneum in slim patients with firm abdominal skin. Ann R Coll Surg Engl. 2016;98(3):228. doi: 10.1308/rcsann.2016.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]


