Abstract
Oral cancer is the second most prevalent cancer in India and 5% of all cancers in women is contributed by oral cancer. In spite of being a part of national programme, the screening coverage rates remain low. Studies have indicated that the societal status of women and their empowerment plays a role in screening coverage for cancer. The objective of the current study is to estimate the coverage of oral cancer screening among Indian women within reproductive age-group across Indian states and union territories (UTs), to explore the relationship of socioeconomic status (SES) and women empower status (WES) with oral cancer screening coverage across Indian states and union territories (UT). Data from the fifth round of the nationally representative cross-sectional survey (National Family Health Survey, NFHS-2019–2021) was used in the present study with 3,48,882 individuals being included in the final analysis. We have cross-tabulated SES and WES composite scores with the Dimension Index (DI) of screening and categorised states and UTs into low, middle and high. We have represented these values over the Indian map. The interaction among these was graphically represented by a bubble plot. Further, we estimated the association of each indicator of SES and WES with screening coverage using multivariable logistic regression. The national coverage of oral cancer screening among women of reproductive age was 0.77% with Andhra Pradesh (7%) and Andaman and Nicobar Islands (10%) recording the highest screening coverage. Despite having high SES and WES scores, Madhya Pradesh and Uttar Pradesh, the screening (DI) was low. States with both high women empowerment status and high socioeconomic status showed high oral cancer screening uptake but the trend was not universal. Still, there were variations in the association among the states. The increased screening was significantly associated with higher access to improved sanitary facility (76%) and clean fuel for cooking (44%). Socio-economic status is an important precursor for better oral cancer screening coverage but women empowerment status did not always translate into good cancer screening uptake. Deep-rooted socio-cultural constructs and stigma associated with cancer and its implications may play a role. Implementation research for better uptake of oral cancer screening coverage is required.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-80346-w.
Keywords: Oral cancer screening, Oral cancer, Cancer screening, Women of reproductive age group, Women, NFHS 5, India
Subject terms: Cancer, Health care
Introduction
Oral cancer is one of the most common type of cancers in India accounting for one third of the global burden1. It is the second most prevalent cancer in India with the second highest incidence and mortality of all cancers, affecting both men and women2. Epidemiological studies have established the role of tobacco in the causation of oral cancer3. 5% of all cancers in women is contributed by oral cancer. There has also been a rising trend of tobacco use among women in India. The prevalence of current tobacco use among women in India is 14.2%4. The World Health Organization- Framework Convention on Tobacco Control (WHO-FCTC) Guiding Principles highlighted the importance of tobacco control efforts. It also pointed out the probable gender disparity as the intended targets for such control efforts. It emphasized the “need for taking measures to address gender-specific risks when developing tobacco control strategies”5.
In such a scenario, it becomes imperative to expand cancer screening services so as to facilitate early detection and treatment of cancers. The National Programme for Non-Communicable Diseases6has recommended population based screening in adults aged more than 30 years as a strategy for detection and treatment of cancer cases in the community. Screening for oral cancer is recommended for both men and women and additionally women are also screened for breast cancer and cervical cancer. However, the current screening coverage, as per the National Family Health Survey7, is very low at 0.8% for women and 1.3% for men. Studies have indicated that the societal status of women and their empowerment plays a role in screening coverage for cancer8. It has been historically seen that systemic gender inequities, and conflicting family responsibilities negatively impact women’s participation in preventive healthcare or screening programs9. This social disadvantage, coupled with the stigma about cancer and oral cancer in particular, puts the oral cancer screening numbers precariously low in females10. Established societal norms11and taboo about the lifestyle factors12associated with oral cancer make women reluctant to undergo screening. Previous studies have also indicated that women educational and thus their empowerment status plays a role in cancer screening uptake13.
The objective of the current study is to estimate the coverage of oral cancer screening among Indian women within reproductive age-group across Indian states and union territories (UT), to explore the relationship of socioeconomic and women empower factors with oral cancer screening coverage across Indian states and union territories (UT) and to identify various demographic, socioeconomic, women empowerment, health related and behavioural determinants associated with oral cancer screening.
Methods
Study design
Data from the fifth round of the nationally representative cross-sectional survey (National Family Health Survey, NFHS-2019–2021) was a used in the present research7. This extensive survey is carried out using a multi-phase, stratified cluster sampling methodology. Because the NFHS survey primarily focuses on women of reproductive age and children under five, it has an uneven proportion of women and men. Consequently, more women than men were covered by the state module. Data on emerging family and health-related issues are gathered for the survey from the NFHS rounds that follow. It provides solid evidence to support, monitor and evaluate ongoing national programmes and opens new avenues for finding unmet needs in the population. Four different questionnaire types—the Household, Woman’s, Man’s, and Biomarker—were used to gather the data, and computer-assisted personal interviewing (CAPI) was used to translate the results into the local languages. All regular household members and guests who spent the night before were asked to fill out a Household Schedule. Other details included socioeconomic status, health insurance status, land ownership, water, sanitation, and hygiene practices, the number of deaths in the household in the three years prior to the survey, and the use and ownership of mosquito nets. The Woman’s Schedule addressed a broad range of subjects, such as the attributes of women, marriage, fertility, contraception, children’s healthcare and vaccinations, nutrition, sexual behaviour, HIV/AIDS, women’s empowerment, and domestic abuse. The Man’s Schedule addressed the man’s attributes, including his marital status, the number of children he had, his choice for contraception, nutrition, sexual behaviour, health problems, views on gender roles, and HIV/AIDS. The Biomarker Questionnaire included measures of children’s height, weight, and haemoglobin; for women aged 15–49 and males aged 15–54, measurements of height, weight, waist, hip circumference haemoglobin, blood pressure, and random blood glucose were included7.
Missing value analysis and data pertaining to present study
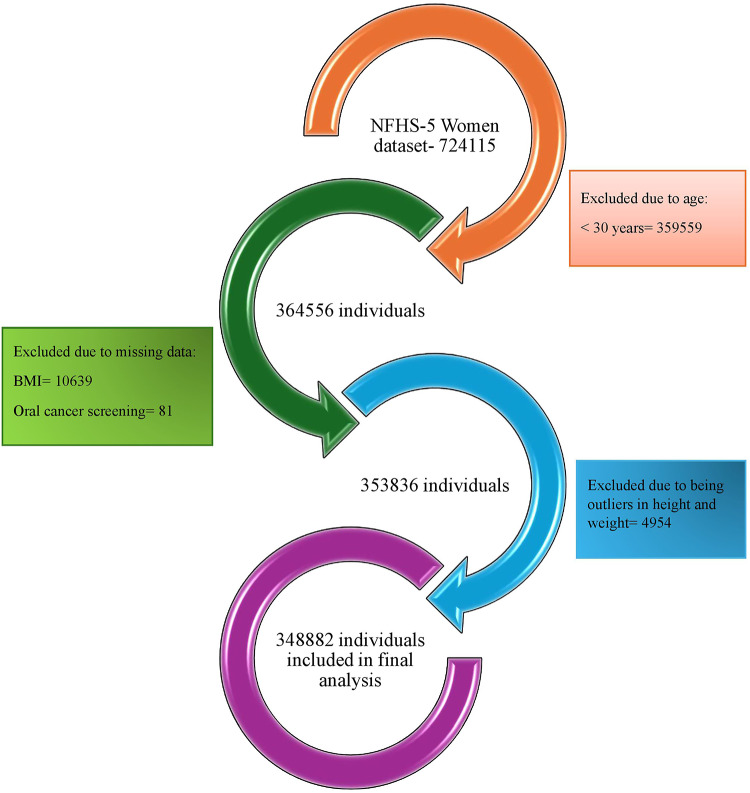
A total of 636,699 households were included in NFHS-5, comprising 724,115 women (15 to 49 years) and 101,839 men (15 to 54 years). As a part of population-based screening (PBS) directed by Ministry of Health & Family Welfare, Government of India (MoHFW), women aged ≥30 years are recommended to undergo regular oral cancer screening6. Thus, only included women in the aforementioned age category were included in the study. After adjusting missing variables and outliers by complete case analysis (row wise complete deletion) the final sample size came out to be 348,882. (Fig. 1)
Fig. 1.
Study flow diagram- selection of the participants for analysis.
Outcome variable
The outcome variable was self-reported oral cancer screening. The participants were asked if they had ever undergone a screening test for oral cancer and the answers were recorded in a dichotomous format as “yes” or “no”.
Explanatory variables
The explanatory variables were socioeconomic status (SES), women empowerment status (WES), socio-demographic, health related and behavioural factors. As per the national and state wise report of NFHS-5, SES and WES were obtained from household profile and women empowerment indicators14. The components of SES and WES are provided in Supplementary Table S1. Under socio-demographic factors, age-group in years (30–34, 35–39, 40–44 and 45–49), religion (Hindu, Muslim, Christian and Others), caste (schedules caste, scheduled tribe, OBC/ other backward caste and others), wealth quintile (poorest, poorer, middle, richer and richest), education (illiterate, primary secondary and higher secondary), gender of head of household (Male, female), marital status (married, others), health insurance (no, yes) and region (north, central, east, northeast, west and south) were included. Categorisation of states and union territories (UT) into regions were shown in Table 1. Under health-related factors, Body Mass Index/ BMI (Underweight (< 18.5), Normal (18.5–22.9), Overweight (23.0–24.9) and Obesity (≥25.0)), diabetes (no, yes and don’t know) and hypertension (no, yes and don’t know) were included. Under behavioural factors, frequency of fruits intake (never, daily, weekly and occasionally), fried food intake (never, daily, weekly and occasionally), chewing tobacco (no, yes), smoking (no, yes), alcohol consumption (no, yes) and exposure to media i.e. television or radio or phone (no, yes) were included7.
Table 1.
State-wise ranking of composite scores for SES, WES, oral cancer screening coverage and dimension index (DI) for women aged between 30 and 49 years of age.
| States/ Union Territories | SES | WES | Coverage (%) | DI |
|---|---|---|---|---|
| North | ||||
| Chandigarh | 4.05 | 2.99 | 0.00 | 0.00 |
| Delhi | 4.08 | 2.68 | 1.14 | 0.11 |
| Haryana | 3.59 | 2.51 | 0.28 | 0.03 |
| Himachal Pradesh | 3.31 | 2.87 | 0.30 | 0.03 |
| Jammu & Kashmir | 3.67 | 2.74 | 0.90 | 0.09 |
| Ladakh | 3.24 | 2.84 | 0.22 | 0.02 |
| Punjab | 3.67 | 2.97 | 0.20 | 0.02 |
| Rajasthan | 3.44 | 2.39 | 0.10 | 0.01 |
| Uttarakhand | 3.45 | 2.69 | 0.49 | 0.05 |
| Central | ||||
| Chhattisgarh | 3.11 | 2.68 | 0.15 | 0.01 |
| Madhya Pradesh | 3.06 | 2.37 | 0.53 | 0.05 |
| Uttar Pradesh | 2.87 | 2.56 | 0.50 | 0.05 |
| East | ||||
| Bihar | 2.68 | 2.68 | 0.25 | 0.02 |
| Jharkhand | 2.82 | 2.65 | 0.15 | 0.01 |
| Odisha | 2.66 | 2.69 | 0.28 | 0.03 |
| West Bengal | 2.97 | 2.37 | 0.11 | 0.01 |
| North-east | ||||
| Arunachal Pradesh | 3.53 | 2.96 | 0.46 | 0.04 |
| Assam | 2.62 | 2.65 | 0.17 | 0.02 |
| Manipur | 3.54 | 3.00 | 0.32 | 0.03 |
| Meghalaya | 3.10 | 3.21 | 0.45 | 0.04 |
| Mizoram | 3.81 | 2.78 | 0.26 | 0.03 |
| Nagaland | 3.40 | 2.76 | 0.28 | 0.03 |
| Sikkim | 3.74 | 2.98 | 0.41 | 0.04 |
| Tripura | 2.96 | 2.52 | 0.46 | 0.04 |
| West | ||||
|
Dadra & Nagar Haveli and Daman & Diu |
3.71 | 3.10 | 0.00 | 0.00 |
| Goa | 3.93 | 3.07 | 0.22 | 0.02 |
| Gujarat | 3.56 | 2.59 | 0.19 | 0.02 |
| Maharashtra | 3.54 | 2.56 | 0.92 | 0.09 |
| South | ||||
|
Andaman & Nicobar Islands |
3.83 | 2.91 | 10.32 | 1.00 |
| Andhra Pradesh | 3.91 | 2.91 | 7.02 | 0.68 |
| Karnataka | 3.71 | 3.11 | 0.40 | 0.04 |
| Kerala | 3.55 | 3.02 | 0.52 | 0.05 |
| Lakshadweep | 3.51 | 2.81 | 0.00 | 0.00 |
| Puducherry | 3.87 | 3.34 | 0.41 | 0.04 |
| Tamil Nadu | 3.65 | 3.34 | 1.01 | 0.10 |
| Telangana | 4.12 | 3.27 | 2.11 | 0.20 |
| India | 3.24 | 2.71 | 0.77 | 0.07 |
Data analysis
Data was analysed using Microsoft Excel 2024 and STATA v17 (StataCorp LLC, College Station, TX). A suitable map and pictorial representation of data using the aforementioned software was created15. Appropriate survey weights were applied during analysis. Dimension Index by Iyengar and Sudarshan (DI) is an estimate of the development of the area of interest. From the NFHS-5 state summary report the DI of each state/ UT was calculated. The range of DI varies from 0 to 1, higher value indicating better performance16.
 |
Composite scores- SES and WES composite scores were determined by summing the DI values of their respective component indicators. The 33rd and 66th percentile marks in the range of index values were used to rank the coverage, DI values of oral cancer screening, SES and WES composite scores as low, middle, and high level. The states and UTs were categorised into these categories as per coverage of screening (Supplementary Table S2). They were further categorised by cross tabulating DI categories with each of SES and WES categories (Supplementary Table S3).
The distribution of oral cancer screening coverage across states and UTs was visualised using maps. The DI values of each state/ UT with respect to SES and WES composite scores was used to create a bubble plot. Furthermore, the association of oral cancer screening with socioeconomic status (SES), women empowerment status (WES), socio-demographic, health related and behavioural factors was reported using multivariable logistic regression. P-value < 0.05 was considered as statistically significant.
Results
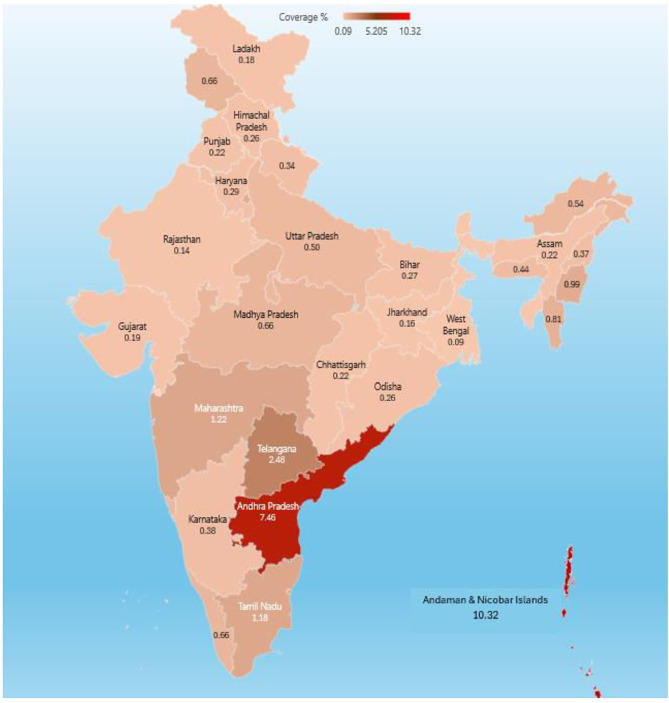
It was found that the national coverage of oral cancer screening among women aged 30 to 49 years was 0.77% with Andhra Pradesh and Andaman and Nicobar Islands being the state and Union Territory with the highest proportion of oral cancer screening among women at 7.02% and 10.32% respectively. The Dimension Index (DI) for India was 0.07 and was the highest for Andhra Pradesh and Andaman and Nicobar Islands. The states and UT included in the Southern geographical divisions were found to show the highest coverage of oral cancer screening (Table 1).
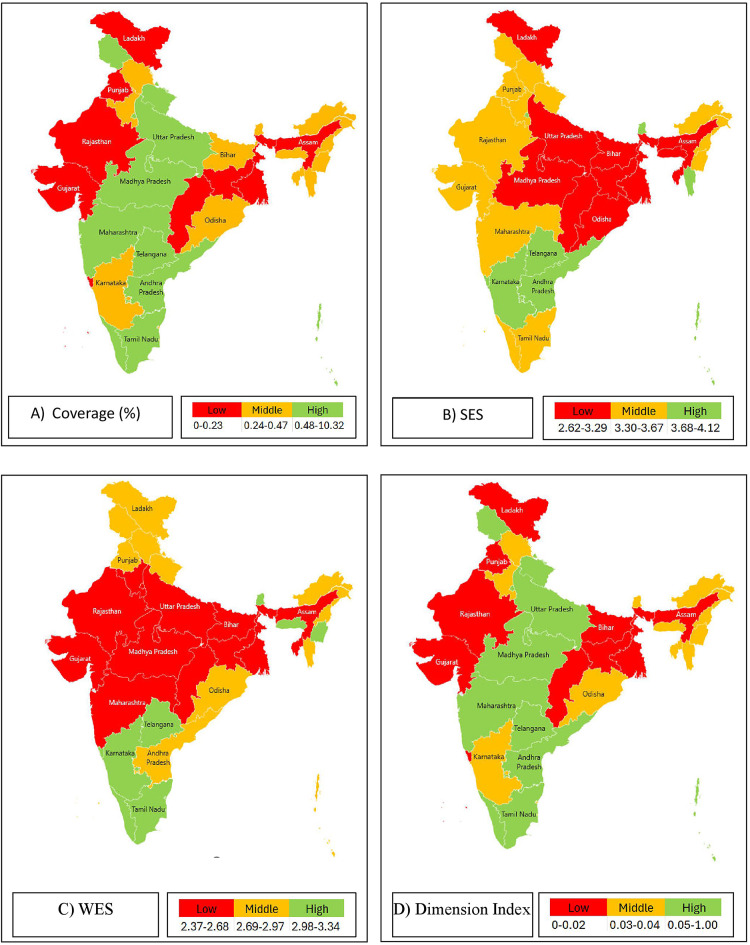
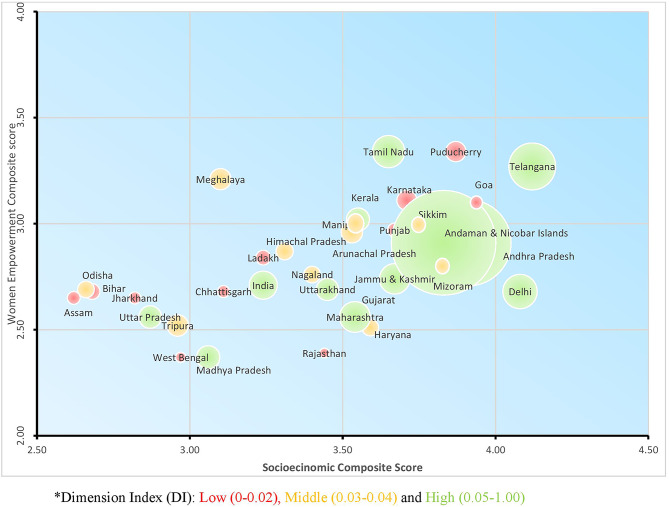
The heat map (Fig. 2) also shows that Andhra Pradesh, Andaman and Nicobar Islands and Telangana showed relatively higher coverage of screening. The socioeconomic status (SES) score, women empowerment status (WES) score, oral cancer screening coverage and the composite score was classified into low, middle and high so as to divide the states into three groups equally. The states in South and Central India were found to show relatively higher coverage off oral cancer screening among women. The oral cancer screening corresponded with the Dimension Index (DI) of the states. (Fig. 3) On plotting the women empowerment composite score and the composite score for the socio-economic status, it was seen that states with both high women empowerment status and high socioeconomic status showed high oral cancer screening uptake but the trend was not universal. States with low women empowerment composite score almost always had low oral cancer screening coverage. (Fig. 4)
Fig. 2.
Coverage of oral cancer screening among Indian women within reproductive age-group.
Fig. 3.
Categorisation of states and union territories by oral cancer screening among Indian women within reproductive age- group: (A) Coverage, (B) SES, (C) WES, (D) Dimension Index.
Fig. 4.
State-wise uptake of screening (DI) and socioeconomic status (SES) and women empowerment status (WES).
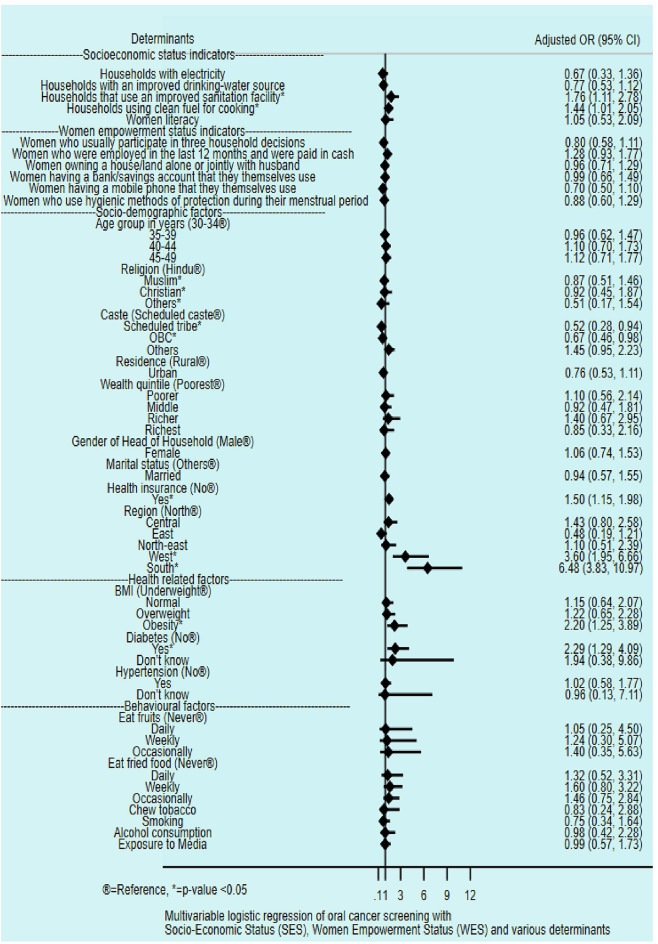
Multivariable logistic regression of oral cancer screening coverage with various factors showed that a higher screening coverage was found in areas with households with improved sanitation facility (aOR = 1.76 (1.11, 2.78, p < 0.05) and using clean fuel for cooking (aOR = 1.44 (1.01–2.05), p < 0.05). Thus, the increased screening was significantly associated with higher access to improved sanitary facility (76%) and clean fuel for cooking (44%).
Women belonging to the Scheduled Tribes (aOR = 0.52 (0.28–0.94), p < 0.05) or Other Backward Classes (aOR = 0.67 (0.468–0.94), p < 0.05) had lesser chances of being screened for oral cancer compared to women belonging to the Scheduled Castes. Compared to the North Indian states, women belonging to the South Indian (aOR = 6.48 (3.83–10.97), p < 0.05) or West Indian states (aOR = 3.60 (1.95–6.66), p < 0.05) had a higher chance of being screened for oral cancer. Compared to underweight women, obese women (aOR = 2.20 (1.25–3.89), p < 0.05) had a higher chance of being screened for oral cancer. Women who were diabetic (aOR = 2.29 (1.29–4.09), p < 0.05) had a higher chance of being screened for cancer compared to the women who were not diabetic. (Fig. 5)
Fig. 5.
Association of oral cancer screening coverage with SES, WES and various determinants.
Discussion
The current study assessed the role of socio-economic status and the women empowerment status in the oral cancer screening coverage rates in India. The national oral cancer screening coverage among women was found to be 0.77%. The expected oral cancer screening coverage among men and aged 30 to 65 years, as per the programmatic guidelines, is 50% with a projected 15% increase in coverage every year6. The causes for low oral cancer screening coverage has been proposed to be socio-cultural factors and the stigma associated with cancer8. Women, especially, face a stigma related to cancer diagnosis which stems from fear of contagion, a belief in personal responsibility for cancer and a lack of knowledge about the risk factors which led to the cancer17,18. It was seen that the southern states of India have reported higher cancer screening coverage rates. The Southern parts of India have reported the highest incidence of oral cancer among women in India as well as worldwide1. The high incidence may have contributed to better awareness and higher numbers presenting and allowing oral examination. Ramped-up population based screening efforts by the government in the areas may have also contributed to better numbers. Comparison with male statistics showed that men (1.06%) reported a higher rate of screening compared to women (0.77%)19. Established societal roles and norms, the site of the cancer and the prevalent belief about the causes for oral cancer may have led to stigma about the cancer diagnosis. The same may have been reflected in low screening numbers.
It was seen that states with women with higher educational status, belonging to higher castes, empowerment status and better socio-economic status reported higher cancer screening uptake. Possible causes for the same include ability to make decisions about their health20, monetary independence to independently ask for the screening service. However, this trend was not uniform. States like Daman & Diu, Dadra and Nagar Haveli, Goa and Chandigarh were the exceptions with low oral cancer screening coverage. Specific lack of knowledge and awareness about the importance of cancer screening and the importance of detecting pre-cancerous lesions may have contributed to the low figures. Fear of disfigurement, feelings of inevitability of death after cancer diagnosis20may have contributed to the low numbers21. Women who were already in contact with the health system for some other comorbidity had higher chances of being screened for oral cancer for the same reason.
Oral cancer screening uptake is significantly more in obese and diabetic women. As a part of PBS diabetes is also screened along with oral cancer among women aged 30 years and above. Due to various shared risk factors like sedentary lifestyle, obesity etc. these might coexist. Due to higher public health awareness and health consciousness in obese and diabetic participants continuing regular health monitoring might lead to higher screening22.
In this context, it becomes important to note the contribution of the health system in improving uptake rates. With a multitude of National Health Programmes running in an integrated manner, it becomes necessary to prioritise the resources. With India languishing under the “ Triple Burden”23high burden diseases like tuberculosis, vector-borne diseases, hypertension, diabetes and maternal and child health and nutrition have taken top priority and focus24. In such a case, adequate logistics and tracking of the screening numbers may not have been possible. Surveys have reported the additional burden on health personnel with high case- load and time constraints25. Cancer screening also requires trained dedicated personnel with proper tools. A strong referral system for diagnosis confirmation and fast-tracking the start of treatment is also necessary. With India undergoing “Epidemiological Transition”, there is increased focus on cancers and their screening26. Population-based screening has been adopted in the current National Programme guidelines. Studies have shown the opportunistic screening for oral cancer in women is a feasible option provided it is backed up with a robust referral system27.
Studies have recommended oral cancer screening among the population aged more than 30 years (both male and female) to be the most cost-effective approach to reducing the medical and the economic burden of oral cancer in India28. A proper screening programme necessitates adequate attendance rates, good calibration of screeners through training, quality control of the applied test and availability of a referral pathway for detected cases to receive adequate treatment. There must also be a provision for quality control, monitoring of the process, and evaluation of outcomes.
Strengths of the study include usage of data from a large-scale nationally representative survey7. This study explores the role of gender inequality and the social constructs involved in oral cancer screening. Study limitations included limited data on the comprehensive status of oral cancer screening. A single screening episode does not provide the correct picture. Longitudinal information about each successive screening visit, gap between two successive visits and the outcome of screening is necessary. Varied sample sizes from different states may have also affected the estimates to some extent, especially states with too few samples selected. Being a cross-sectional study design, temporality cannot be established. Due to self-reporting patterns of questionnaire, recall bias and social desirability bias could not be ignored. The MOHFW launched screening programmes simultaneously in every state, although differentiating rollouts and the participation of some large-scale, state-specific programmes could have increased screening adoption in some states. These impacts were too great for this study to measure.
Conclusion
Socio-economic status is an important precursor for better oral cancer screening coverage but women empowerment status did not always translate into good cancer screening uptake. Deep-rooted socio-cultural constructs and stigma associated with cancer and its implications may play a role. Implementation research for better uptake of oral cancer screening coverage is required for early detection and treatment of oral cancer. It may be done through improving awareness among the population and strengthening the health system so as to adequately carry out screening, referral, diagnostic, follow-up and maintain the continuum of care for oral cancer.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We want to express our sincere gratitude to the participants and the International Institute for Population Sciences (IIPS).
Author contributions
PH- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, SD - Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, GJ - Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, SS- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision. AD- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision. AS- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision. SR- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision.
Data availability
The study utilizes data of published summary of the fifth wave of National Family Health Survey, which is publicly accessible and can be obtained by registering at https://dhsprogram.com/Countries/CountryMain.cfm? ctry_id=57&c=India. The corresponding author (Dr. Pritam Halder) can provide the processed data upon reasonable requests.
Declarations
Competing interests
The authors declare no competing interests.
Ethics
The NFHS-5 received ethical approval from the International Institute for Population Sciences (IIPS), Mumbai (2019–21) as per Helsinki declaration. It was also reviewed by the International Review Board (IRB), which approved it ethically. After receiving complete information about the goal and methodology of the survey, the respondents signed to confirm their agreement. Interviews were conducted only after receiving each participant’s informed consent. Being an anonymous dataset it is publicly available on the Demographic and Health Surveys (DHS) Programme website that cannot be used to identify survey respondents. The current study was a secondary data analysis from the available records.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Borse, V., Konwar, A. N. & Buragohain, P. Oral cancer diagnosis and perspectives in India. Sens. Int.1, 100046 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cancer (ed) (IARC) TIA for R on. Global Cancer Observatory [Internet]. [cited 2024 Aug 1]. https://gco.iarc.fr/
- 3.Gupta, P. C., Murti, P. R., Bhonsle, R. B., Mehta, F. S. & Pindborg, J. J. Effect of cessation of tobacco use on the incidence of oral mucosal lesions in a 10-yr follow-up study of 12,212 users. Oral Dis.1(1), 54–58 (1995). [DOI] [PubMed] [Google Scholar]
- 4.Global Adult Tobacco Survey [Internet]. [cited 2024 Aug 1]. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-adult-tobacco-survey
- 5.Gender women, and the tobacco epidemic [Internet]. [cited 2024 Aug 1]. https://www.who.int/publications/i/item/9789240004849
- 6.National Programme for prevention & Control of Cancer. Diabetes, Cardiovascular Diseases & stroke (NPCDCS):: National Health Mission [Internet]. [cited 2024 Jul 31]. https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604
- 7.National Family Health Survey [Internet]. [cited 2023 Aug 12]. http://rchiips.org/nfhs/
- 8.Patil, P. et al. Does women’s empowerment and their socioeconomic condition affect the uptake of breast cancer screening? Findings from NFHS-5, India. BMC Women’s Health. 23(1), 7 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jolidon, V. Gender inequality and mammography screening: does living with a partner improve women’s mammography uptake? Soc. Sci. Med.298, 114875 (2022). [DOI] [PubMed] [Google Scholar]
- 10.Sahoo, S. S., Sahu, D. P., Verma, M., Parija, P. P. & Panda, U. K. Cancer and Stigma: Present Situation and challenges in India. Oncol. J. India. 3(3), 51 (2019). [Google Scholar]
- 11.Wilding, S., O’Connor, D. B. & Conner, M. Social norms in Cervical Cancer Screening. Psychol. Rep.332941231219943. (2023). [DOI] [PubMed]
- 12.Kumar, M., Nanavati, R., Modi, T. G. & Dobariya, C. Oral cancer: etiology and risk factors: a review. J. Cancer Res. Ther.12(2), 458 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Donnelly, T. T. et al. Do socioeconomic factors influence breast cancer screening practices among arab women in Qatar? BMJ Open.5(1), e005596 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guide to DHS Statistics. (English) [Internet]. [cited 2024 Jul 31]. https://dhsprogram.com/publications/publication-dhsg1-dhs-questionnaires-and-manuals.cfm
- 15.Statistical software for. data science | Stata [Internet]. [cited 2024 May 25]. https://www.stata.com/
- 16.Iyengar, N. S. & Sudarshan, P. A method of classifying regions from Multivariate Data. Economic Political Wkly.17(51), 2047–2052 (1982). [Google Scholar]
- 17.Nyblade, L., Stockton, M., Travasso, S. & Krishnan, S. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Women’s Health. 17(1), 58 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Squiers, L. et al. Perceived, Experienced, and Internalized Cancer Stigma: Perspectives of Cancer Patients and Caregivers in India [Internet]. Research Triangle Park (NC): RTI Press; [cited 2024 Aug 29]. (RTI Press Research Report Series). (2021). http://www.ncbi.nlm.nih.gov/books/NBK577066/ [PubMed]
- 19.Roy, S., Girotra, S., Radhakrishnan, A. & Basu, S. Prevalence and determinants of tobacco consumption and oral cancer screening among men in India: evidence from a nationally representative cross-sectional Survey. J Public Health (Berl) [Internet]. 2023 Dec 18 [cited 2024 Aug 1]; 10.1007/s10389-023-02161-3
- 20.Tripathi, N., Kadam, Y. R., Dhobale, R. V. & Gore, A. D. Barriers for early detection of cancer amongst Indian rural women. South. Asian J. Cancer. 3(2), 122–127 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahalakshmi, S. & Suresh, S. Barriers to Cancer Screening Uptake in women: a qualitative study from Tamil Nadu, India. Asian Pac. J. Cancer Prev.21(4), 1081–1087 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.AshaRani, P. V. et al. Factors influencing uptake of diabetes health screening: a mixed methods study in Asian population. BMC Public. Health. 22(1), 1511 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Narain, J. P. Public Health Challenges in India: seizing the opportunities. Indian J. Community Med.41(2), 85–88 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dandona, R. Public health priorities for India. Lancet Public. Health. 7(2), e102–e103 (2022). [DOI] [PubMed] [Google Scholar]
- 25.Kedar, A., Kannan, R., Mehrotra, R. & Hariprasad, R. Implementation of Population-based Cancer Screening Program in a pilot study from India: views from Health personnel. Indian J. Community Med.44(1), 68–70 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krenz, A. & Strulik, H. Physiological aging in India: the role of the epidemiological transition. PLoS One. 18(7), e0287259 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaur, R., Kant, S., Mathur, V. P. & Lohia, A. Feasibility of opportunistic screening for oral cancers in a dental outpatient department of a secondary care hospital in Northern India. J. Family Med. Prim. Care. 9(2), 909–914 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dwivedi, P. et al. Cost-effectiveness of population-based screening for oral cancer in India: an economic modelling study. The Lancet Regional Health - Southeast Asia [Internet]. 2023 Sep 1 [cited 2024 Aug 1];16. https://www.thelancet.com/journals/lansea/article/PIIS2772-3682(23)00084-7/fulltext [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study utilizes data of published summary of the fifth wave of National Family Health Survey, which is publicly accessible and can be obtained by registering at https://dhsprogram.com/Countries/CountryMain.cfm? ctry_id=57&c=India. The corresponding author (Dr. Pritam Halder) can provide the processed data upon reasonable requests.