Abstract
Lemierre's syndrome is a fatal condition characterized by septic thrombophlebitis of the internal jugular vein (IJV). Early diagnosis of Lemierre's syndrome in primary care remains challenging because of its rarity and common initial symptoms like fever and sore throat. The COVID‐19 pandemic has increased the difficulty of diagnosis, along with many diagnostic delays. Herein, we report a case in which an IJV thrombus was detected using point‐of‐care ultrasound (POCUS), leading to the diagnosis of Lemierre's syndrome. During the COVID‐19 pandemic, POCUS was a simple and noninvasive technique for screening Lemierre's syndrome without radiation and low droplet exposure.
Keywords: COVID‐19, internal jugular vein thrombus, Lemierre's syndrome, pandemic, point‐of‐care ultrasound
We report a case in which an internal jugular vein thrombus was detected using point‐of‐care ultrasonography (POCUS), leading to the diagnosis of Lemierre's syndrome. During the COVID‐19 pandemic, POCUS was a simple and non‐invasive technique for screening Lemierre's syndrome without radiation and low droplet exposure.
1. BACKGROUND
Lemierre's syndrome is a rare but fatal condition commonly caused by Fusobacterium necrophorum and characterized by septic thrombophlebitis of the internal jugular vein (IJV) with pharyngotonsillitis, septic emboli, and metastatic abscesses. Early diagnosis in primary care remains challenging because initial symptoms like fever and sore throats are common and occur frequently in young, healthy individuals. 1
Furthermore, the COVID‐19 pandemic caused a dramatic increase in the number of patients with common cold symptoms. Even during a pandemic, Lemierre's syndrome should not be overlooked; however, no efficient screening tools have been established. Here, we report a case in which point‐of‐care ultrasound (POCUS) was used to identify an IJV thrombus in a patient with Lemierre's syndrome.
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
2. CASE PRESENTATION
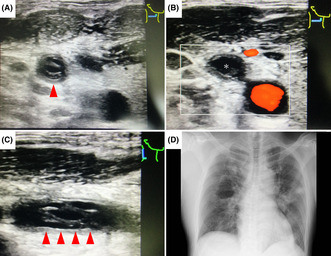
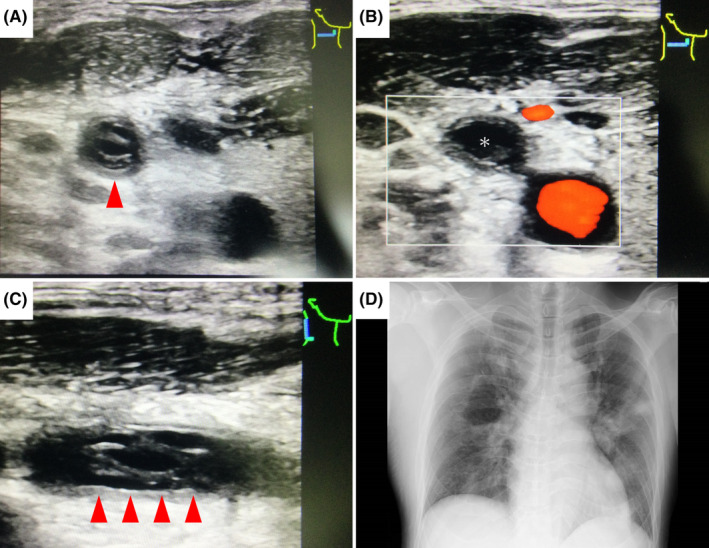
A man in his 40s with recurrent tonsillitis had developed a sore throat and fever a week before the presentation, followed by pain in his right shoulder. He visited his primary care physician four times and underwent four tests (polymerase chain reaction and antigen tests) for suspected COVID‐19, all of which were negative. Eventually, the patient developed respiratory distress and was referred to our hospital. The patient's blood pressure was 136/95 mmHg, pulse rate was 100 bpm, respiratory rate was 22 breaths/min, oxygen saturation was 96% at 5 L/min, and body temperature was 38.4°C. A physical examination revealed swelling and tenderness of the right neck and shoulder. The right tonsil showed traces of tonsillitis. POCUS of neck, performed by placing a high‐frequency (4.2–13 MHz) linear probe, revealed a thrombus in the right IJV (Figure 1A–C). Chest X‐ray showed multiple consolidations in both lungs (Figure 1D). Laboratory workup revealed an increased number of white blood cells (13,200 cells/μL), elevated C‐reactive protein (26.2 mg/L) and D‐dimer (7.6 μg/mL), and thrombocytopenia (18,000 cells/μL). Computed tomography (CT) revealed a thrombus in the right IJV and multiple systemic abscesses (Figure 2). We tentatively diagnosed the patient with Lemierre's syndrome and performed drainage surgery for shoulder joint abscesses. On day 5, F. necrophorum was detected in the blood culture, confirming the diagnosis of Lemierre's. The patient was discharged on day 91 after four drainage surgeries.
FIGURE 1.
(A–C) Ultrasound image shows a hyperechoic thrombus in the right internal jugular vein (red arrowhead), and color Doppler ultrasound image demonstrates absence of flow (*). (D) Chest X‐ray shows multiple consolidations in both lungs.
FIGURE 2.
Computed tomography reveals (A) a thrombus of the right internal jugular vein (red arrow), (B) septic pulmonary embolisms, and (C, D) abscesses around the right shoulder and left psoas major muscle (red arrowhead).
3. DISCUSSION
Patients with pharyngitis, prolonged and severe symptoms, infections at secondary sites, and neck symptoms should be evaluated for Lemierre's syndrome. 1 During the COVID‐19 pandemic, delayed diagnosis and misdiagnosis were reported. 2 , 3 , 4 , 5 In addition to the increased number of patients with common cold symptoms, anchoring bias (focusing on a particular facet), premature closure (closing of the diagnostic process before all information is obtained), 2 , 3 avoidance of physical contact and aerosol‐generating examinations, 2 , 4 an insufficient emergency medical system, and a stay at home 5 have been identified as contributing factors.
Contrast‐enhanced CT is the most common imaging modality for diagnosing Lemierre's syndrome. 1 CT can identify disseminated lesions and IJV thrombi; however, it is time‐consuming and exposes the patient to radiation. CT is not a screening tool. Therefore, a new procedure is needed to avoid missing Lemierre's syndrome.
POCUS can rapidly screen for IJV without radiation and low droplet exposure. Many physicians are familiar with IJV screening because of the central venous catheter insertion. Several reports have shown the ultrasonography in detecting IJV thrombi for diagnosing Lemierre's syndrome. 6 , 7 , 8 Castro‐Marín and Kendall reported a case in which bedside IJV ultrasonography led to a rapid diagnosis. 6 However, no cases have been reported in which POCUS has been performed in the early stages during the pandemic. This indicates that the utility of POCUS is not widely known, and its importance needs to be recognized.
Two points should be noted when screening for POCUS. One is that ultrasound imaging is limited to regions deep in the clavicle and mandible, and less sensitive than CT. 1 The other is that early thrombus may not be echogenic. 1 , 6 This can be resolved by checking for the inability to compress the vessel and a lack of color Doppler flow and pulsation. 1 , 6 , 7 , 8
4. CONCLUSION
POCUS may be a valuable adjunct to customary procedures for detecting Lemierre's syndrome during the COVID‐19 pandemic. Ultrasound is a noninvasive technique that can immediately identify an IJV thrombus without radiation and low droplet exposure.
FUNDING INFORMATION
This study did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENTS
Ethics approval statement: None.
Patient consent statement: Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. Copies of the written consent are available for review by the Editor‐in‐Chief of this journal.
Clinical trial registration: None.
Kawai Y, Nishiyama K. Point‐of‐care ultrasound for Lemierre's syndrome during the COVID‐19 pandemic: A case report. J Gen Fam Med. 2024;25:274–276. 10.1002/jgf2.708
REFERENCES
- 1. Carius BM, Koyfman A, Long B. High risk and low prevalence diseases: Lemierre's syndrome. Am J Emerg Med. 2022;61:98–104. [DOI] [PubMed] [Google Scholar]
- 2. Soares C, Blackwood K, Vecchio M, Francis ER, Zhu S, Johnson J. Diagnosing Lemierre's syndrome as the cause of multifocal pneumonia during the COVID‐19 pandemic. R I Med J. 2021;104:46–49. [PubMed] [Google Scholar]
- 3. Repper DC, Arrieta AC, Cook JE, Renella P. A case of Lemierre syndrome in the era of COVID‐19: all that glitters is not gold. Pediatr Infect Dis J. 2020;39:e445. [DOI] [PubMed] [Google Scholar]
- 4. Miura T, Fukuda H, Kawada H, Kaga T, Matsuo M, Sakai T, et al. Delayed diagnosis of Lemierre's syndrome in a patient with severe coronavirus disease 2019: the importance of comprehensive oral and neck examination—a case report. BMC Infect Dis. 2023;23:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Howley F, O'Doherty L, McEniff N, O'Riordan R. Late presentation of ‘Lemierre's syndrome’: how a delay in seeking healthcare and reduced access to routine services resulted in widely disseminated Fusobacterium necrophorum infection during the global COVID‐19 pandemic. BMJ Case Rep. 2020;13:e239269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Castro‐Marín F, Kendall JL. Diagnosis of Lemierre syndrome by bedside emergency department ultrasound. J Emerg Med. 2010;39:436–439. [DOI] [PubMed] [Google Scholar]
- 7. Azzopardi C, Grech R, Mizzi A. Lemierre syndrome: more than just a sore throat. BMJ Case Rep. 2013;2013:bcr2013201868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davies O, Than M. Lemierre's syndrome: diagnosis in the emergency department. Emerg Med Australas. 2012;24:673–676. [DOI] [PubMed] [Google Scholar]


