Abstract
Background
Pain from rib fractures often requires inpatient management with opioid medication. The need for ongoing opioid prescriptions following hospital discharge is poorly understood. Harms associated with long-term opioid use are generally accepted. However, a deeper understanding of current prescribing patterns in this population at-risk is required.
Methods
A retrospective cohort of adult patients hospitalised in Queensland, Australia between 2014 and 2015 with rib fractures (ICD-10-AM: S22.3, S22.4, S22.5), was obtained from the Community Opioid Dispensing after Injury (CODI) study, which includes person-linked hospitalisation, mortality and community opioid dispensing data. Data were extracted 90-days prior to the index-hospitalisation and 720-days after discharge. Factors associated with long-duration (>90 days cumulatively) and increased end-dose were examined using multivariable logistic regressions, odds ratios (OR), and 95% confidence intervals (95% CI).
Results
In total, 4306 patients met the inclusion criteria, and 58.8% had opioids dispensed in the community within 30 days of hospital discharge. 23.6% had long-duration dispensing and 13.7% increased opioid end-doses. Pre-injury opioid use was most associated with long-duration (OR = 12.00, 95% CI 8.99–16.01) and increased end-dose (OR = 9.00, 95% CI 6.75–12.00). Females and older persons had higher odds of long-duration dispensing (Females OR = 1.75, 95% CI 1.38–2.22; Age 65+ OR = 1.86, 95% CI 1.32–2.61). Injury severity and presence of concurrent injuries were not statistically significantly associated with duration or dose (p > .05). Subsequent hospitalisations and death during the follow-up period had statistically significant associations with long-duration and increased end-dose (p < .001).
Conclusion
Opiate prescribing following rib fractures is prolonged in older, and female patients, beyond the traditionally reported recovery time frames requiring analgesia. Previous opioid use (without dependence) is associated with long-duration opioid use and increased end-dose in rib fracture patients. These results support the need for a collaborative health system approach and individualised strategies for high-risk patients with rib fractures to reduce long-term opiate use.
Level of Evidence
Level III, Prognostic/Epidemiological.
Keywords: Blunt chest trauma, cohort study, data linkage, opioids, rib fractures
Background
Rib fractures are common injuries and are recognised to cause considerable pain both acutely and longer-term. 1 The provision of analgesia for the management of pain associated with rib fractures may reduce potential complications, chronic pain and mortality. This concept is supported by extensive literature from the acute hospitalisation phase reporting reduced length of stay and reduced complications when multimodal analgesic regimes are adopted.2–4 Recognising the importance of appropriate analgesia, studies have attempted to describe the relationship between rib fracture severity, pain level, and other patient factors to explain escalating analgesia requirements in the acute setting. 4
Analgesia requirements for rib fracture pain after discharge from hospital have been associated with similar factors: in-hospital analgesia use, the severity of rib fractures and premorbid conditions. 5 The recovery timeframe from rib fractures is often presumed to be short. However, observational studies have demonstrated prolonged pain and disability lasting beyond 6 months, for both single and complex rib fracture patterns.6–9 This discrepancy may influence patient expectations, analgesia prescribing and overall care of these patients beyond the hospitalisation phase.
Many countries, including the USA, have reported high rates of opioid use and misuse after trauma, with concern that opioid prescribing in the acute setting contributes to these outcomes. 2 Understandably, apprehension regarding the direct impact of prescribing habits on opioid-related deaths has led to renewed interest in acute pain management utilising opioid sparing strategies including adjunct analgesia and local anaesthetic techniques. 2 These strategies decrease rib fracture pain and improve function and may then result in reduced discharge and community prescribing. 4 Currently, there is a lack of information examining the direct relationship between rib fracture-related pain and opioid use beyond acute hospitalisation.10,11
A new integration of statewide hospitalisation and scheduled drug monitoring databases in Queensland 12 offers a novel, quantitative and efficient means for examining opioid dispensing in the community, within the context of individual clinical characteristics and ongoing health service use. The aim of this paper, therefore, is to describe community opioid dispensing patterns and factors associated with long-dispensing durations and increasing opioid end-doses, after hospitalisation for rib fractures.
Methods
Study design
This is a subgroup analysis from the Community Opioid Dispensing after Injury (CODI) study, which is a population-based retrospective cohort study, using linked administrative health data. CODI includes hospitalisation data for all adults aged 18 years or older, admitted to any hospital in Queensland, Australia after sustaining an injury, with hospitalisation records linked to community opioid dispensing and mortality data collections. The study protocol and full population cohort characteristics have been published elsewhere.12,13 The STROBE cohort guideline was used to ensure proper reporting of methods, results, and discussion.
Ethics
Ethics approval with a waiver of consent was obtained from the Royal Brisbane and Women’s Hospital Human Research Ethics Committee (HREC/2018/QRBW/48236). Additional approval was obtained for the release of confidential information for the purposes of research under the provision of Section 280 of Public Health Act (PHA) 2005, Queensland (QCOS/033343/RD007954).
Data sources
CODI included three data sources, (1) Queensland Hospital Admitted Patient Data Collection (QHAPDC), 14 (2) Registry of Births, Deaths and Marriages (BDM) 15 and (3) Monitoring of Drugs of Dependence System (MODDS) 16 with these sources person-linked using deterministic and probabilistic methods by the Statistics and Linkage Unit at Queensland Health. 17
Data obtained from QHAPDC included patient demographics, diagnostic and procedural information, hospital type (public or private), admission dates, intensive care unit admission (ICU), length of stay (LOS) and separation destination, including hospital transfers and inpatient deaths. Mortality data from BDM included dates and International Classification of Diseases, 10th Revision (ICD-10) coded causes of death. Data on all prescribed opioids dispensed at community pharmacies across Queensland were, at the time of the study, included in MODDS. MODDS contains dispensing information for all Schedule eight drugs, including opioids.18,19 Data obtained from MODDS included the prescribed drug name, formulation, quantity and dispensing dates. MODDS also contains a classification code that identifies if a person has ever been medically diagnosed as drug dependent, or registered on a formal Opioid Treatment Program (OTP). 20 Inpatient opioid dispensing data are not captured in MODDS.
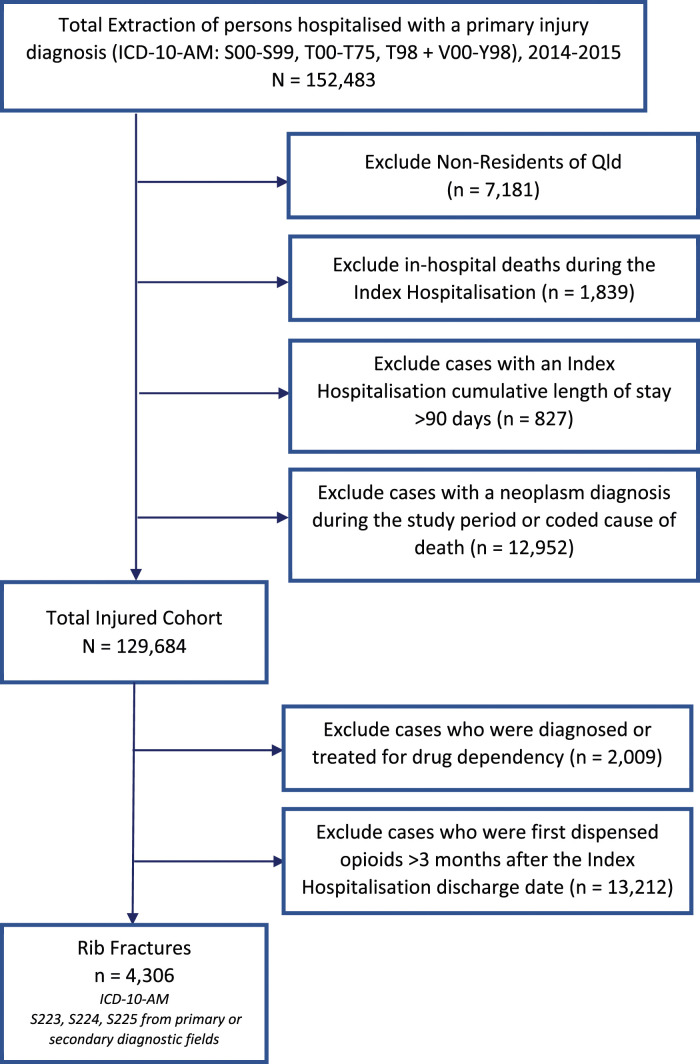
Cohort inclusion and exclusion
The full CODI cohort included all hospitalised adults with any injury-related principal diagnosis (International Classification of Diseases, 10th Revision, Australian Modification (ICD-10-AM: S00-S99, T00-T75, T98 + V00-Y98), with their acute care hospital episode ending between 1 January 2014 and 31 December 2015. All public and private hospitalisations were included. Related, contiguous episodes of care were grouped to form a hospital encounter with a cumulative LOS. 21 The first encounter was called the index-hospitalisation. Patients were excluded if their place of residence was outside Queensland, they died during their index-hospitalisation, the LOS for their index-hospitalisation was greater than 90 days, they had a neoplasm diagnosis code at any time during the total study period, or the cause of death code was a neoplasm (ICD-10: C00-D48).12,13
For the current analysis of patients hospitalised with rib fractures, additional exclusions were applied. Patients were excluded if they had been previously diagnosed or formally treated for a drug dependency or were first dispensed opioids greater than 3 months after they were discharged from their index-hospitalisation (as likely to be unrelated to their initial injury). Rib fracture patients were selected from the full CODI cohort if they had a principal or other diagnosis code for rib fractures or flail injury (ICD-10-AM: S22.3, S22.4, and S22.5).
Follow-up data
Opioid dispensing data was extracted for 90 days before the index-hospitalisation, through to 720 days following discharge. Details of any subsequent hospitalisation, for any cause, were also extracted for 720 days following discharge. Death data were extracted for the complete follow-up period, which ended on 31 December 2017. The study covers a maximum calendar period from 1 October 2013 to 31 December 2017.
Data management and classifications
Hospitalisation data
Rib fractures were classified as (1) single rib fracture (2) multiple rib fractures and (3) flail injuries. All other injuries were subclassified as concurrent injuries if not superficial. All demographic and injury data were recorded at the time of the index-hospitalisation. Age was categorised as 18–44, 45–64, and 65+ years. Mechanism (cause) of injury ICD-10-AM codes were aggregated to three categories (1) falls (W00-W19, X80, Y01, Y30), (2) transport-related (V00-V99, X82, Y03, Y32, Y361) and (3) other cause (all remaining cause codes). Surgical procedures requiring a general anaesthetic, based on Australian Classification of Health Interventions (ACHI) codes, 22 were identified. The total LOS was dichotomised as ≤21 days and >21 days. The number of hospital encounters for each patient, for any cause, was summed across the entire follow-up period and categorised as 0, 1, 2–4, and 5+.
ICD-based Injury Severity Score
The severity of injury, based on ICD-10-AM injury-related diagnoses, was estimated using the ICD-based Injury Severity Score (ICISS).23,24 The ICISS was dichotomised to low threat to life (>0.941) and high threat to life (≤0.941). 25
Accessibility/Remoteness Index of Australia
Geographic remoteness using the Accessibility/Remoteness Index of Australia (ARIA) was assigned to each person in QHAPDC, based on area of residence. 26 ARIA was then categorised as Urban (Major Cities), Rural (Inner Regional, Outer Regional) and Remote (Remote and Very Remote).
Oral morphine equivalents and opioid duration estimation
The amount of opioid prescribed, and considering its formulation (e.g. tablet, patch, liquid), was converted to the equivalent amount of oral morphine, expressed as oral morphine equivalents (OME), using conversion factors recommended for research. 27 Given individual dosing information (e.g. prescribed number of tablets per day) is not recorded in MODDS, estimates were required for how long the prescription was intended to last (i.e. duration of use, e.g. 14 days), and for daily OME. The estimation of prescription duration followed a structured approach, prioritising the time between subsequent scripts for the same drug type to indicate prescription duration. For patients with no repeat scripts, or scripts dispensed intermittently, dispensing durations were estimated based on prescribing guidelines and clinician input. The calculated total OME was divided by the estimated duration (in days) to determine the daily OME for each prescription, with extreme values refined. Daily OMEs from concurrent prescriptions were combined. Detailed information on the duration estimation steps has been previously published. 13 Based on literature and the clinical guidelines in place during the timeframe of this study, cumulative durations greater than 90 days were considered long-term or chronic use.28–30
Analysis
Initial data management and final analysis were conducted using SAS 9.4 (SAS Institute, Cary NC), with duration and daily OME calculated using Stata v16.1 (StataCorp, College Station TX). Descriptive statistics (frequencies, percentages, medians and interquartile ranges) were used to describe the rib-fractured cohort in terms of demographics, injury factors (rib fracture type and mechanism of injury) and index-hospitalisation characteristics (ICU admission, LOS, surgery performed). Associations were measured using Chi-squared and Kruskal–Wallis non-parametric tests, depending on the data type and distribution.
For visual descriptive purposes, daily OMEs were averaged for each 30-day interval before and after the index-hospitalisation. In addition, an OME ‘end-dose’ was calculated by summing the OMEs for all opioids dispensed before the last opioid dispensing date (considering the duration of the last prescription) and averaged using the cumulative days duration in those 90 days. Similar methods were used to calculate an OME ‘start-dose’ based on the average dose in the 90 days before the index-hospitalisation, or the average dose after the index-hospitalisation (if no opioids were dispensed in the 90 days prior). Proportions of the cohort having opioids dispensed, cumulative duration of dispensing across the study period, and averaged daily OMEs for the follow-up period were compared, stratified by rib fracture group. Due to the skewed distribution of the data, medians are presented. Factors associated with long-duration dispensing (>90 cumulative days v ≤ 90 cumulative days) and increased dose (comparing OME start-dose and end-dose; increase v no increase) were examined in two separate models using multivariable logistic regression including all factors described above, with statistical significance set at 0.05. Both logistic regression models were specified with a time offset, which accounts for the number of days an individual was alive and not readmitted to hospital during the follow-up period.
Results
Cohort characteristics
After exclusions, 4306 patients were identified with rib fractures in the index-hospitalisation (Figure 1). Most of the cohorts were male (69.7%), aged below 65 years (63.0%) and resided in urban areas (59.5%), with 10.4% dispensed opioids in the 90 days before hospitalisation (Table 1). Two-thirds of patients had multiple rib fractures (66.9%), the primary mechanisms of injury were falls (44.0%) and transport-related (43.3%), and more than one-third of patients had injuries classified as a high threat to life, based on their ICISS (35.4%). Rib fractures occurred in isolation (i.e. no other thoracic injuries or injuries to other body regions) for 36.3% of patients with single rib fractures and 25.9% with multiple-rib fractures. However, for those with flail injuries, 95.3% had other concurrent injuries.
Figure 1.
Flow chart for [BLINDED] rib fracture case extraction and exclusions.
Table 1.
Demographic and injury characteristics, follow-up hospitalisations and mortality for (1) the total rib fracture cohort, (2) patients with no opioids dispensed, and (3) patients with opioids dispensed, during the 2-year follow-up period (N = 4306).
| No opioids dispensed during follow-up | Opioids dispensed during follow-up | Chi-square test | |
|---|---|---|---|
| N (row %) | N (row %) | p-value | |
| Total (N = 4306) | 1676 (38.9) | 2630 (61.1) | |
| Demographic characteristics | |||
| Sex | |||
| Female (n = 1306) | 533 (40.8) | 773 (59.2) | 0.09 |
| Male (n = 3000) | 1143 (38.1) | 1857 (61.9) | |
| Age groups | |||
| 18–44 (n = 1180) | 445 (37.7) | 735 (62.3) | <0.0001 |
| 45–64 (n = 1533) | 528 (34.4) | 1005 (65.6) | |
| 65+ (n = 1593) | 703 (44.1) | 890 (55.9) | |
| Place of residence (ARIA) a | |||
| Urban (n = 2561) | 977 (38.1) | 1584 (61.9) | <0.0001 |
| Rural (n = 1600) | 608 (38.0) | 992 (62.0) | |
| Remote (n = 145) | 91 (62.8) | 54 (37.2) | |
| Pre-injury opioid dispensing | |||
| No (n = 3858) | 1609 (41.7) | 2249 (58.3) | <0.0001 |
| Yes (n = 488) | 67 (15.0) | 381 (85.0) | |
| Injury characteristics | |||
| Rib fracture group | |||
| Single rib (n = 1145) | 554 (48.4) | 591 (51.6) | <0.0001 |
| Multiple ribs (n = 2882) | 1034 (35.9) | 1848 (64.1) | |
| Flail (n = 279) | 88 (31.5) | 191 (68.5) | |
| Concurrent injuries | |||
| Isolated (n = 1175) | 478 (40.7) | 697 (59.3) | 0.147 |
| Other injuries (n = 3131) | 1198 (38.3) | 1933 (61.7) | |
| Mechanism of injury | |||
| Fall (n = 1895) | 749 (39.5) | 1146 (60.5) | <0.0001 |
| Transport related (n = 1864) | 661 (35.5) | 1203 (64.5) | |
| Other (n = 547) | 266 (48.6) | 281 (51.4) | |
| Injury severity (ICISS) | |||
| Low threat to life (SRR >0.941) (n = 2780) | 1123 (40.4) | 1657 (59.6) | 0.007 |
| High threat to life (SRR ≤0.941) (n = 1526) | 553 (36.2) | 973 (63.8) | |
| Index hospitalisation characteristics | |||
| Length of stay (LOS) in days | |||
| ≤21 days (n = 3822) | 1443 (37.8) | 2379 (62.2) | <0.0001 |
| >21 days (n = 484) | 233 (48.1) | 251 (51.9) | |
| Surgery performed | |||
| No (n = 3576) | 1404 (39.3) | 2172 (60.7) | 0.31 |
| Yes (n = 730) | 272 (37.3) | 458 (62.7) | |
| ICU Admission | |||
| No (n = 3925) | 1530 (39.0) | 2395 (61.0) | 0.80 |
| Yes (n = 381) | 146 (38.3) | 235 (61.7) | |
| Follow-up period characteristics | |||
| Number of hospitalisations (all cause) | |||
| 0 (n = 1926) | 830 (43.1) | 1096 (56.9) | <0.0001 |
| 1 (n = 1005) | 375 (37.3) | 630 (62.7) | |
| 2-4 (n = 948) | 325 (34.3) | 623 (65.7) | |
| 5+ (n = 427) | 146 (34.2) | 281 (65.8) | |
| Died (all cause) | |||
| No (n = 4009) | 1560 (38.9) | 2449 (61.1) | 0.96 |
| Yes (n = 297) | 116 (39.1) | 181 (60.9) | |
ARIA - Accessibility/Remoteness Index of Australia.
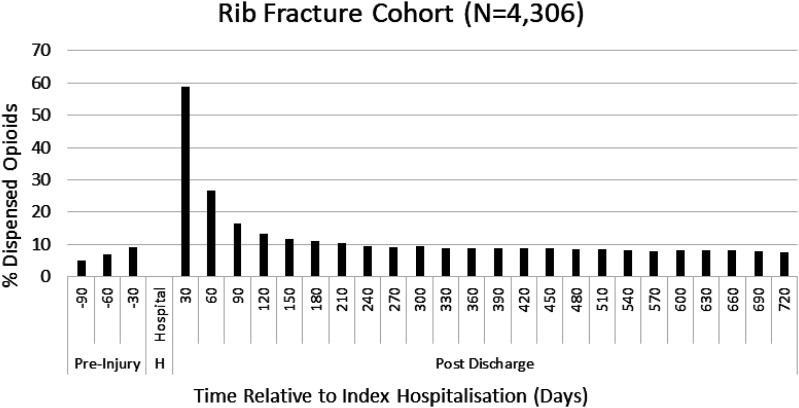
Cohort opioid dispensing
In the first 30 days immediately after hospitalisation, 58.8% of patients had opioids dispensed (Figure 2), and in total, 61.1% of the cohort had opioids dispensed at least once over the 2-year follow-up period (Table 1). The proportion of people having opioids dispensed rapidly decreased in the first 90 days after hospitalisation but remained at approximately 8% of the cohort for the entire 2 years post-hospitalisation (Figure 2).
Figure 2.
Proportion of persons in the rib fracture cohort having opioids dispensed for each 30-day interval, from 90 days prior to the index injury hospitalisation and from day of hospital discharge up to 720 days after.
There was no gender difference in the proportion of patients dispensed opioids post-hospitalisation (females 59.2% v males 61.9%, p = .09) (Table 1). Patients from urban (61.9%) and rural areas (62.0%) had higher proportions of patients dispensed opioids when compared to patients who resided in remote areas (37.2%, p < .0001). A higher proportion of patients dispensed opioids pre-injury had opioids dispensed post-hospitalisation when compared to patients not dispensed opioids pre-injury (85.0% v 58.3%, p < .0001). A higher percentage of patients with multiple rib fractures (64.1%) and flail injury (68.5%) had opioids dispensed post-hospitalisation, compared to patients with single rib fractures (51.6%, p < .0001).
Opioid dispensing patterns by rib fracture group
For patients who had opioids dispensed post-hospitalisation (n = 2630), the single rib fracture group had a higher representation of females, persons aged 65+ and fall-related injuries compared to the other rib fracture groups (Table 2). Conversely, males, persons aged 45–64 years, and transport-related injuries were more prevalent for flail injuries. Pre-injury opioid dispensing was more prevalent in patients with single rib fractures (18.8%) and multiple rib fractures (13.9%), compared to flail injuries (6.8%).
Table 2.
Opioid dispensing durations and oral morphine equivalent (OME) end doses ^ during the 2-year follow-up period for patients who had opioids dispensed during follow-up, and by rib fracture group (N = 2630).
| All patients | Single rib | Multiple ribs | Flail | |||||
|---|---|---|---|---|---|---|---|---|
| N (col %) | [Median duration; median end OME] ^ | N (col %) | [Median duration; median end OME] ^ | N (col %) | [Median duration; median end OME] ^ | N (col %) | [Median duration; median end OME] ^ | |
| 2630 | [Days: 29; OME: 20] | 591 | [Days: 28; OME: 16] | 1848 | [Days: 29; OME: 21] | 191 | [Days: 40; OME: 26] | |
| Demographic characteristics | ||||||||
| Sex | ||||||||
| Female | 773 (29.4) | [Days: 43; OME: 19] | 217 (36.7) | [Days: 42; OME: 16] | 516 (27.9) | [Days: 45; OME: 20] | 40 (20.9) | [Days: 40; OME: 15] |
| Male | 1857 (70.6) | [Days: 24; OME: 21] | 374 (63.3) | [Days: 19; OME: 15] | 1332 (72.1) | [Days: 25; OME: 22] | 151 (79.1) | [Days: 41; OME: 28] |
| Age groups | ||||||||
| 18–44 | 735 (27.9) | [Days: 19; OME: 19] | 169 (28.6) | [Days:15; OME: 10] | 513 (27.8) | [Days: 20; OME: 22] | 53 (27.8) | [Days: 38; OME: 28] |
| 45–64 | 1005 (38.2) | [Days: 25; OME: 20] | 210 (35.5) | [Days: 20; OME: 19] | 704 (38.1) | [Days: 24; OME: 20] | 91 (47.6) | [Days: 40; OME: 28] |
| 65+ | 890 (33.8) | [Days: 50; OME: 21] | 212 (35.9) | [Days: 63; OME: 17] | 631 (34.1) | [Days: 48; OME: 22] | 47 (24.6) | [Days: 44; OME: 15] |
| Place of residence (ARIA) a | ||||||||
| Urban (MC) | 1584 (60.2) | [Days: 29; OME: 19] | 363 (61.4) | [Days: 30; OME: 14] | 1111 (60.1) | [Days: 28; OME: 21] | 110 (57.6) | [Days: 40; OME: 24] |
| Rural (OR, IR) | 992 (37.7) | [Days: 29; OME: 22] | 219 (37.1) | [Days: 22; OME: 20] | 696 (37.7) | [Days: 30; OME: 22] | 77 (40.3) | [Days: 40; OME: 33] |
| Remote (R, VR) | 54 (2.1) | [Days: 27; OME: 18] | ## | ## | 41 (2.2) | [Days: 25; OME: 20] | ## | ## |
| Pre-injury opioid dispensing | ||||||||
| No | 2249 (85.5) | [Days: 23; OME: 19] | 480 (81.2) | [Days: 19; OME: 14] | 1591 (86.1) | [Days: 22; OME: 20] | 178 (93.2) | [Days: 38; OME: 28] |
| Yes | 381 (14.5) | [Days: 335; OME: 30] | 111 (18.8) | [Days: 290; OME: 29] | 257 (13.9) | [Days: 342; OME: 32] | 13 (6.8) | [Days: 127; OME: 14] |
| Injury characteristics | ||||||||
| Concurrent injuries | ||||||||
| Isolated | 697 (26.5) | [Days: 26; OME: 17] | 222 (37.6) | [Days: 27; OME: 15] | 467 (25.3) | [Days: 26; OME: 20] | ## | ## |
| Other injuries | 1933 (73.5) | [Days: 30; OME: 21] | 369 (62.4) | [Days: 28; OME: 16] | 1381 (74.7) | [Days: 29; OME: 22] | 183 (95.8) | [Days: 40; OME: 28] |
| Injury mechanism | ||||||||
| Falls | 1146 (43.6) | [Days: 36; OME: 20] | 303 (51.3) | [Days: 38; OME: 16] | 787 (42.6) | [Days: 35; OME: 22] | 56 (29.3) | [Days: 39; OME: 24] |
| Transport | 1203 (45.7) | [Days: 25; OME: 21] | 192 (32.5) | [Days: 17; OME: 14] | 890 (48.2) | [Days: 24; OME: 21] | 121 (63.4) | [Days: 41; OME: 28] |
| Other | 281 (10.7) | [Days: 26; OME: 19] | 96 (16.2) | [Days: 27; OME: 17] | 171 (9.2) | [Days: 22; OME: 19] | 14 (7.3) | [Days: 41; OME: 13] |
| Injury severity (ICISS) | ||||||||
| Low threat to life (SRR >0.941) | 1657 (63.0) | [Days: 26; OME: 19] | 494 (83.6) | [Days: 28; OME: 15] | 1108 (60.0) | [Days: 25; OME: 20] | 55 (28.8) | [Days: 25; OME: 28] |
| High threat to life (SRR ≤0.941) | 973 (37.0) | [Days: 34; OME: 23] | 97 (16.4) | [Days: 27; OME: 23] | 740 (40.0) | [Days: 32; OME: 23] | 136 (71.2) | [Days: 43; OME: 26] |
| Index hospitalisation characteristics | ||||||||
| Length of stay (LOS) | ||||||||
| ≤21 days | 2379 (90.5) | [Days: 26; OME: 20] | 550 (93.1) | [Days: 24; OME: 15] | 1678 (90.8) | [Days: 25; OME: 21] | 151 (79.1) | [Days: 36; OME: 26] |
| >21 days | 251 (9.5) | [Days: 100; OME: 22] | 41 (6.9) | [Days: 69; OME: 16] | 170 (9.2) | [Days: 109; OME: 23] | 40 (20.9) | [Days: 146; OME: 27] |
| Surgery performed | ||||||||
| No | 2172 (82.6) | [Days: 26; OME: 20] | 506 (85.6) | [Days: 26; OME: 15] | 1536 (83.1) | [Days: 25; OME: 21] | 130 (68.1) | [Days: 36; OME: 26] |
| Yes | 458 (17.4) | [Days: 44; OME: 22] | 85 (14.4) | [Days: 33; OME: 20] | 312 (16.9) | [Days: 47; OME: 21] | 61 (31.9) | [Days: 53; OME: 32] |
| ICU Admission | ||||||||
| No | 2395 (91.1) | [Days: 27; OME: 20] | 568 (96.1) | [Days: 26; OME: 15] | 1697 (91.8) | [Days: 27; OME: 21] | 130 (68.1) | [Days: 30; OME: 26] |
| Yes | 235 (8.9) | [Days: 56; OME: 21] | 23 (3.9) | [Days: 65; OME: 23] | 151 (8.2) | [Days: 56; OME: 20] | 61 (31.9) | [Days: 53; OME: 28] |
| Follow-up period characteristics | ||||||||
| Number of hospitalisations (all cause) | ||||||||
| 0 | 1096 (41.7) | [Days: 15; OME: 20] | 240 (40.6) | [Days: 15; OME: 14] | 777 (42.1) | [Days: 15; OME: 21] | 79 (41.4) | [Days: 27; OME: 28] |
| 1 | 630 (24.0) | [Days: 30; OME: 21] | 145 (24.5) | [Days: 27; OME: 17] | 432 (23.4) | [Days: 30; OME: 22] | 53 (27.7) | [Days: 30; OME: 26] |
| 2–4 | 623 (23.7) | [Days: 54; OME: 20] | 135 (22.9) | [Days: 46; OME: 16] | 444 (24.0) | [Days: 53; OME: 21] | 44 (23.0) | [Days: 96; OME: 26] |
| 5+ | 281 (10.7) | [Days: 124; OME: 21] | 71 (12.0) | [Days: 142; OME: 16] | 195 (10.5) | [Days: 108; OME: 24] | 15 (7.9) | [Days: 215; OME: 15] |
| Died (all cause) | ||||||||
| No | 2449 (93.1) | [Days: 28; OME: 20] | 538 (91.0) | [Days: 25; OME: 14] | 1724 (93.3) | [Days: 27; OME: 21] | 187 (97.9) | [Days: 40; OME: 28] |
| Yes | 181 (6.9) | [Days: 70; OME: 32] | 53 (9.0) | [Days: 62; OME: 32] | 124 (6.7) | [Days: 73; OME: 32] | ## | ## |
| Cumulative opioid dispensing duration | ||||||||
| ≤90 days | 2010 (76.4) | [Days: 16; OME: 19] | 454 (76.8) | [Days: 15; OME: 13] | 1420 (76.8) | [Days: 16; OME: 20] | 136 (71.2) | [Days: 24; OME: 27] |
| >90 days | 620 (23.6) | [Days: 321; OME: 25] | 137 (23.2) | [Days: 342; OME: 26] | 428 (23.2) | [Days: 318; OME: 24] | 55 (28.8) | [Days: 305; OME: 26] |
^ Median Duration – median cumulative duration for total follow-up period calculated in days; Median OME - To calculate the OME ‘end dose’, all opioids dispensed in the 90-days prior to the last opioid dispensing date (considering the last scripts duration) were identified and averaged using the cumulative days duration in that 90-day period for each person.
## Information suppressed where cell counts ≤10.
a ARIA - Accessibility/Remoteness Index of Australia.
Of patients dispensed opioids post-hospitalisation, 76.4% had a cumulative duration ≤90 days (median = 16 days [Table 2]). Within the single and multiple rib fracture groups, differences in opioid dispensing durations were seen between demographic groups. Female patients had almost double the median duration of opioids than males. Longer median durations of opioid dispensing were also seen in older age patients. However, there was little difference in the duration when stratified by the same demographic characteristics for flail injuries. Patients with flail injuries had the highest median end-dose for most demographic, injury, and hospitalisation characteristics when compared to those with single and multiple rib fractures (Table 2).
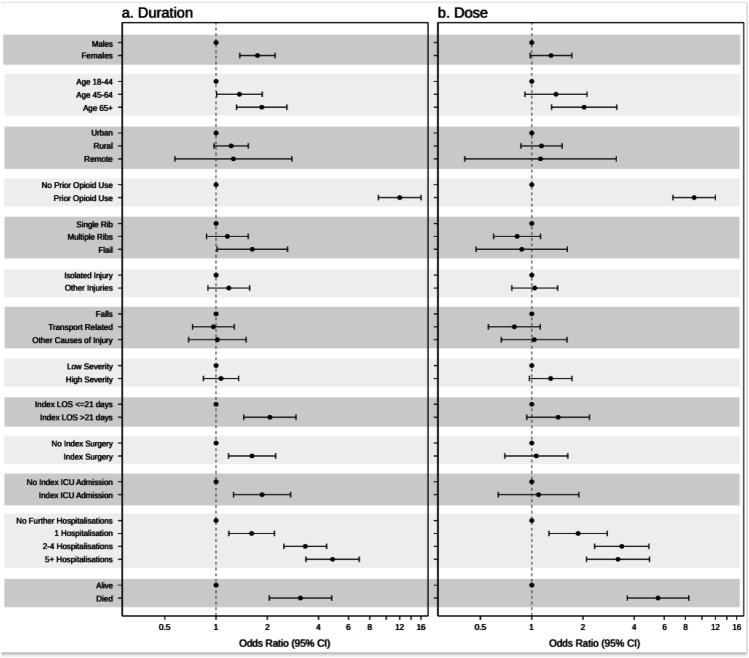
Long-duration opioid dispensing
In total, 620 (23.6%) rib fracture patients had opioids dispensed for greater than 90-days cumulatively across the 2-year follow-up period (median = 321 days [Table 2]). The factor most associated with long-duration dispensing was prior opioid use (Figure 3(a)), with these patients being 12 times more likely than those opioid naïve to have long-duration opioid dispensing post-hospitalisation (OR = 12.00, 95% CI 8.99–16.01). Females and older aged persons continued to have a statistically significant association with long-duration dispensing in the multivariable model (Females OR = 1.75, 95% CI 1.38–2.22; Age 65+ OR = 1.86, 95% CI 1.32–2.61). While the severity of injury and presence of concurrent injuries were not statistically associated with long-duration dispensing (p > .05), several clinical factors including LOS (OR = 2.07, 95% CI 1.45–2.95), surgery performed during the index hospitalisation (OR = 1.63, 95% CI 1.18–2.24) and ICU admission (OR = 1.86, 95% CI 1.27–2.74) were associated with long-duration dispensing. Further hospitalisations, as well as death during the follow-up period, also had a statistically significant association with long-duration opioid dispensing (p < .001) (Figure 3(a)).
Figure 3.
Factors associated with (a) long-duration opioid dispensing (>90 days cumulatively from the day of hospital discharge up to 720 days after), and (b) an increased OME end-dose, for the rib fracture cohort, using multivariable logistic regression showing Odds Ratios and 95% Confidence intervals.
Increased opioid dose (OME) over time
Of the 2630 patients dispensed opioids post-hospitalisation, 13.7% had an OME end-dose higher than their start-dose (results not shown). Factors associated with an increased opioid end-dose were similar to those associated with long-duration dispensing (Figure 3(b)). The factors most associated with an increased end-dose were prior opioid usage (OR = 9.00, 95% CI 6.75–12.00) and older age (Aged 65+ OR = 2.03, 95% CI 1.31–3.16). Further hospitalisations, as well as death during the follow-up period, also had a statistically significant association with an increased end-dose (p < .001) (Figure 3(b)).
Sensitivity analyses examined whether starting on a higher or lower OME dose impacted the odds of an increased end-dose for each factor. Patients were categorised into higher or lower start OME doses based on whether they had a start-dose above or below the total rib fracture cohort median dose of 20 OMEs. Only interactions between the start-dose and (1) rib fracture group, and (2) further hospitalisations were statistically significant (p < .1).
The sensitivity analysis showed that among patients with flail injuries, those who started with a higher OME were 4.8 times more likely to have an increased end-dose compared to those who started with lower OMEs (OR = 4.76, 95% CI 1.29-17.64). When compared to the total rib fracture cohort receiving opioids, this subgroup had a higher proportion of concurrent injuries (94.1% vs 61.0%) (Supplementary Table 1). Opioid start-dose did not impact the end-dose for the single or multiple rib fracture groups.
The sensitivity analysis also showed that among patients who had no further hospitalisations, those who started with higher OMEs had 3.7 times the odds of having an increased end-dose, compared to those who started with lower OMEs (OR = 3.69, 95% CI 1.75–7.83). When compared to the total rib fracture cohort receiving opioids, this subgroup had a higher proportion of females (43.9% vs 29.4%), older aged persons (48.8% vs 33.8%), prior opioid use (61.0% vs 14.5%), injury from a fall (63.4% vs 43.6%), single rib fractures (31.7% vs 22.5%), isolated fractures (39.0% vs 26.9%) and higher mortality (21.9% vs 6.9%) (Supplementary Table 1). Opioid start-dose did not impact the end-dose for any of the other repeat hospitalisation groups.
Discussion
This study is the first to describe community-based dispensing of opioid medications following acute rib-fracture-related hospitalisation using a large, statewide, whole-of-population cohort. This study adds to a growing understanding of the impact that acute trauma, opioid exposure, and prescribing patterns have on long-term opioid use in the community.
Overall, patients hospitalised with rib fractures were commonly prescribed opioid medications in the community immediately post-hospitalisation. Most rib-fracture patients were male, aged under 65 years of age and were injured through a fall or transport-related mechanism. Unsurprisingly, patients who had multiple rib fractures or a flail injury were more likely to be dispensed opioids in the community, and continue use. Compared to the total trauma reference population from CODI, 13 and an international cohort 1 the percentage of rib-fracture patients dispensed opioids immediately post-hospitalisation was substantially higher, indicating that acute pain associated with rib fractures may be greater than pain in the general trauma population. However, in the majority of cases, the opioids were ceased within 90 days post-hospitalisation, concordant with research from other large Australian registry data. 10
The current study found that opioid-naive rib fracture patients had considerably shorter durations of opioid prescriptions, with a median duration of 23 days. Consistent with the literature,5,31,32 patients most at risk of chronic use and increasing opioid doses were those with pre-injury opioid dispensing. In comparison, a recent study of opioid-naive rib fracture patients reported a 16-days median duration of opioid dispensing. 5 The lower duration reported in this study is likely due to differing study design factors, including a shorter duration of data collection post-injury, the exclusion of additional non-thoracic injuries and surgeries unrelated to rib fixation, and the inclusion of non-admitted patients in their sample. Of concern in the current study, the median duration of opioid dispensing in patients who were not opioid-naive was significantly longer than previously reported. 5
For the 620 patients (23.6% of the cohort) who were dispensed opioids for longer than 90 days, the median duration of prescriptions was 321 days. This finding builds upon the study by Kelderman et al 9 who reported 61% of blunt chest trauma patients in their study reported pain at a median of 11 years after the trauma, 18% experienced shortness of breath and 7.7% severe pain (above 8/10 on the Numerical rating scale). The current study demonstrated the small, but not insignificant cohort (8%), who were still being dispensed opioids at the study endpoint of 2 years. Opioid dispensing for longer than 3 months has previously been reported as being between 2% and 15% for general trauma populations,1,33,34 with the results of the current study indicating the additional pain associated with rib fractures may necessitate a more nuanced approach to both inpatient and outpatient pain management.
Factors contributing to chronic pain after rib fractures are likely to be multifactorial. Previous literature has described that neuropathic pain is both under-recognised and may contribute to up to one third of chronic pain presentations at 3 months after rib fractures. 35 The current study did not collect data on the types of pain experienced and so cannot directly quantify the cohort of patients who may have benefited from alternate analgesic agents. This is an important consideration for future studies on pain management in rib fractures.
The proportion of patients who had opioids dispensed for longer than 3 months was similar in each category of single rib, multiple ribs, and flail, with only flail injuries having an increased likelihood for long-duration dispensing. This finding supports the results of Gordy et al 6 who found that the number of ribs fractured in isolation was not a risk factor for developing chronic pain. Changes in the surgical management of rib fractures, specifically earlier surgical fixation more commonly used since the timeframe of the current study may influence the duration of pain experienced by patients and warrants further investigation.
In the current study, younger patients were less likely to have long-duration opioid dispensing and less likely to have an increased end-dose, compared to older patients, which mirrors previous research 33 but is in contrast to one observational study that reported fewer opioid prescriptions in the elderly population after discharge. 36 The authors commented that their findings were more related to differences in reporting of pain, not necessarily the underlying need for analgesia.
Interestingly, female patients were more likely to have opioids dispensed for longer than 3 months compared to their male counterparts, after accounting for injury severity and other factors. Females also had a higher median duration overall (43 days) than males (24 days). These findings mirror those of Oelreich et al 31 who also identified female sex, older age, and previous opioid use as risk factors for chronic use. Although not statistically significant, females also had higher odds of an increased opioid end-dose. Overall, these findings suggest that pre-injury and demographic risk factors do impact long-term opioid use, and that use can last for 2 years post-hospitalisation.
Patients with recurrent hospital admissions were found to have a higher rate and longer duration of opioid dispensing in the community over the study period. Any recurrent operative intervention would be expected to require distinct analgesic prescribing post-intervention. The current results suggest that prolonged continued prescribing occurs in certain patient groups, increasing their risk of opioid dependence. However, when starting opioid dose was considered, it was the patients with no recurrent admissions, who started on higher doses that were more likely to have an increased opioid dose by the end. Even though this subgroup was small (n = 41), the higher opioid dose should inform discharge planning and closer management of at-risk patients. It may be that recurrent hospitalisations are protective of increased opioid dosing, as patients may be more closely managed.
Recent research has detailed the barriers to de-prescribing in the community, with reflections that opioids commenced in the hospital lack a collaborative weaning plan and do not align with the patient’s expectation that the medications will continue. 37 In addition, previous research has shown that when a multimodal analgesia plan was utilised during the inpatient phase of care, there was a reduction in the daily OME on discharge. 4 Without a collaborative approach to both in-hospital analgesic planning and post-discharge weaning, and increasing the available resources for individualised care, ongoing opioid prescribing is likely to continue despite the recognition of harm. 37
Limitations
Some linkage errors may occur as with all studies using linked administrative data. However, these are minimised by the specialised team at the Statistical Analysis and Linkage Unit dedicated to conducting routine linkages.17,38
Using pharmaceutical claims data for pharmacoepidemiological research is often considered the gold standard data source for ascertaining medication exposure.39–41 A limitation of this type of data is the assumption that the dispensed medication is used in the manner prescribed, and in full. Actual medication use is not known. In the current study, reasons such as a reduction in pain symptoms or the presence of adverse effects may lead a patient to discontinue opioid use before script completion.42,43 However, the concept of non-adherence applies predominantly to the final dispensed script for a patient in the dataset. Individual patients who do not consume their entire prescription are unlikely to request refills, suggesting repeat dispensing indicates full prescription use in the dataset. Given the comprehensive statewide coverage and stringent monitoring of opioid dispensing in Queensland, minor deviations in sample behaviour are unlikely to bias whole-of-population outcomes significantly.
This paper focuses on community opioid dispensing and has no information on inpatient analgesic management strategies. Patients were censored at the time of death. If a person moved out of the State and had opioids dispensed elsewhere, this was not known and could result in a small underestimation of findings. Additionally, the data set was collected before the widespread adoption of regional analgesic strategies in the hospital setting 44 and opioid stewardship program implementation. 45 However, this study provides strong baseline data on which future studies can be compared.
Conclusion
Efforts to reduce opioid prescribing and use within the community are paramount, with increasing recognition of the negative outcomes associated with long-term and higher-dose use. Trauma patients, and in particular patients with rib fractures, are an important focus group for quality improvement initiatives aimed at improving outcomes and reducing the reliance on opioid medications. Further research is required to explore the effects of opioid stewardship and the role of different inpatient multimodal analgesia strategies on community opioid prescribing practices after sustaining rib fractures.
Supplemental Material
Supplemental Material for Community opioid dispensing after rib fracture injuries: CODI study by Williamson Frances, Proper Melanie, Shibl Rania, Cramb Susanna, McCreanor Victoria, Warren JacelleJ, and Cameron Cate in British Journal of Pain
Author contributions: Literature search: FW
Study conception and design: MP, RS, SMC, VM, JW, CMC
Data collection/management: RS, SMC, VM, CMC
Data analysis: JW, CMC
Data interpretation: FW, MP, RS, SMC, VM, JW, CMC
Writing: FW, CMC
Critical Review of the Manuscript: FW, MP, RS, SMC, VM, JW, CMC
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a Royal Brisbane and Women’s Hospital Foundation Grant. SMC receives funding from an NHMRC Investigator Grant (#2008313).
Disclosure: I, Dr Frances Williamson, attest on behalf of all authors, that we had full access to the data of the study, conducted all data analyses independently from any funding entity, and take complete responsibility for the integrity and accuracy of the data reported in the manuscript.
Supplemental Material: Supplemental material for this article is available online.
Ethical statement
Ethical approval
Ethics approval with a waiver of consent was obtained from the Royal Brisbane and Women’s Hospital Human Research Ethics Committee (HREC/2018/QRBW/48236) as the study met the low risk criteria. Additional approval was obtained for the release of confidential information for the purposes of research under the provision of Section 80 of Public Health Act (PHA) 2005, Queensland (QCOS/033343/RD007954).
Informed consent
Informed consent was not sought for the present study because it utilised linked statewide deidentified administrative health data, with low risk to participants. It was impractical to obtain consent for the retrospective cohort of over 150,000 people in the main cohort, some of whom were deceased. All linkage was conducted centrally within the Statistical Services Branch of Queensland Health. Researchers were provided deidentified data, with some demographic fields aggregated to further protect identities, such as 5 year age groups instead of individual age, and area level geographic groups instead of individual residential postcodes. Additional Public Health Act (PHA) approval was required due to the waiver of consent for the release of the data for research purposes.
ORCID iDs
Williamson Frances https://orcid.org/0000-0002-5476-1791
Cramb Susanna https://orcid.org/0000-0001-9041-9531
McCreanor Victoria https://orcid.org/0000-0002-0589-8521
Cameron Cate https://orcid.org/0000-0003-1476-5744
References
- 1.Duchesne J, Laflamme L, Lu L, et al. Post-injury benzodiazepine and opioid use among older adults involved in road traffic crashes: a Swedish register-based longitudinal study. Br J Clin Pharmacol 2022; 88: 764–772. DOI: 10.1111/bcp.15019. [DOI] [PubMed] [Google Scholar]
- 2.Karamchandani K, Klick JC, Linskey Dougherty M, et al. Pain management in trauma patients affected by the opioid epidemic: a narrative review. J Trauma Acute Care Surg 2019; 87: 430–439. DOI: 10.1097/TA.0000000000002292. [DOI] [PubMed] [Google Scholar]
- 3.Kourouche S, Buckley T, Munroe B, et al. Development of a blunt chest injury care bundle: an integrative review. Injury 2018; 49: 1008–1023. DOI: 10.1016/j.injury.2018.03.037. [DOI] [PubMed] [Google Scholar]
- 4.Burton SW, Riojas C, Gesin G, et al. Multimodal analgesia reduces opioid requirements in trauma patients with rib fractures. J Trauma Acute Care Surg 2022; 92: 588–596. DOI: 10.1097/TA.0000000000003486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalton MK, Chaudhary MA, Andriotti T, et al. Patterns and predictors of opioid prescribing and use after rib fractures. Surgery 2020; 168: 684-689. DOI: 10.1016/j.surg.2020.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Gordy S, Fabricant L, Ham B, et al. The contribution of rib fractures to chronic pain and disability. Am J Surg 2014; 207: 659–662. DOI: 10.1016/j.amjsurg.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Fabricant L, Ham B, Mullins R, et al. Prolonged pain and disability are common after rib fractures. Am J Surg 2013; 205: 511–515. DOI: 10.1016/j.amjsurg.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Battle CE, Young K, Evans PA. Chronic pain in blunt chest wall trauma: a pilot study. Trauma 2016; 18: 261–265. DOI: 10.1177/1460408616638689. [DOI] [Google Scholar]
- 9.Kelderman I, Dickhoff C, Bloemers FW, et al. Very long-term effects of conservatively treated blunt thoracic trauma: a retrospective analysis. Injury 2024; 55: 111460. DOI: 10.1016/j.injury.2024.111460. [DOI] [PubMed] [Google Scholar]
- 10.Gisev N, Buizen L, Hopkins RE, et al. Five-year trajectories of prescription opioid use. JAMA Netw Open 2023; 6: e2328159. DOI: 10.1001/jamanetworkopen.2023.28159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed RN, Schurr MJ. Acute pain in the trauma patient. Curr Trauma Rep 2020; 6: 147–153. DOI: 10.1007/s40719-020-00198-3. [DOI] [Google Scholar]
- 12.Cameron CM, McCreanor V, Shibl R, et al. Community Opioid Dispensing after Injury (CODI): protocol for a population-based data linkage study. JMIR Res Protoc 2022; 11: e36357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cameron CM, Shibl R, Cramb S, et al. Community opioid dispensing after injury (CODI): cohort characteristics and opioid dispensing patterns. Injury 2023; 55: 111216. DOI: 10.1016/j.injury.2023.111216. [DOI] [PubMed] [Google Scholar]
- 14.Queensland Health . Queensland hospital admitted patient data collection (QHAPDC). https://www.health.qld.gov.au/hsu/collections/qhapdc (2023), accessed 26 Feb 2024.
- 15.Queensland Government . Births, deaths, Marriages and divorces. https://www.qld.gov.au/law/births-deaths-marriages-and-divorces (2023), accessed 18 Aug 2023.
- 16.Hollingworth SA, Symons M, Khatun M, et al. Prescribing databases can be used to monitor trends in opioid analgesic prescribing in Australia. Aust N Z J Public Health 2013; 37: 132–138. DOI: 10.1111/1753-6405.12030. [DOI] [PubMed] [Google Scholar]
- 17.Queensland Health . Queensland data linkage framework. https://www.health.qld.gov.au/__data/assets/pdf_file/0030/150798/qlddatalinkframework.pdf (2020), accessed 18 February 2021.
- 18.Queensland Government . Health (drugs and poisons) regulation 1996 (QLD). Brisbane: Queensland Government, 1996. [Google Scholar]
- 19.Theraputic Goods Administration . Standard for the uniform scheduling of medicines and poisons (SUSMP). Health Do, 2021. https://www.tga.gov.au/publication/poisons-standard-susmp2021.
- 20.Queensland Government . Queensland opioid treatment program. https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/medicines/monitored-medicines/queensland-opioid-treatment-program (2022), accessed 02 November 2022.
- 21.Vallmuur K, McCreanor V, Cameron C, et al. Three Es of linked injury data: episodes, encounters and events. Inj Prev 2021; 27: 479–489. DOI: 10.1136/injuryprev-2020-044098. [DOI] [PubMed] [Google Scholar]
- 22.IHACPA . Independent health and aged care pricing authority. ICD-10-AM/ACHI/ACS Twelfth Edition 2022. https://www.ihacpa.gov.au/resources/icd-10-amachiacs-twelfth-edition (accessed 06 Feb 2023). [Google Scholar]
- 23.Stephenson S, Henley G, Harrison JE, et al. Diagnosis based injury severity scaling: investigation of a method using Australian and New Zealand hospitalisations. Inj Prev 2004; 10: 379–383. DOI: 10.1136/ip.2004.005561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Australian Insititute of Health and Welfare. Henley G, Harrison JE. Injury severity scaling: a comparison of methods for measurement of injury severity. Canberra: AIHW, 2009. [Google Scholar]
- 25.Dayal S, Wren J, Wright C. Mapping injury severity scores against hospitalisation day stays for injury priority areas (excluding workplace injury). Public Health Intelligence HaDSSD. Wellington: Ministry of Health, 2008. [Google Scholar]
- 26.Australian Bureau of Statistics . Australian statistical geography standard (ASGS): volume 5 - remoteness structure. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 (2018).
- 27.Nielsen S, Degenhardt L, Hoban B, et al. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf 2016; 25: 733–737. DOI: 10.1002/pds.3945. [DOI] [PubMed] [Google Scholar]
- 28.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 2009; 10: 113–130. DOI: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dowell D, Ragan KR, Jones CM, et al. Prescribing opioids for pain - the new CDC clinical practice guideline. N Engl J Med 2022; 387: 2011–2013. DOI: 10.1056/NEJMp2211040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Treede RD, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain 2015; 156: 1003–1007. DOI: 10.1097/j.pain.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Oelreich E, Eriksson M, Brattstrom O, et al. Risk factors and outcomes of chronic opioid use following trauma. Br J Surg 2020; 107: 413–421. DOI: 10.1002/bjs.11507. [DOI] [PubMed] [Google Scholar]
- 32.Chaudhary MA, von Keudell A, Bhulani N, et al. Prior prescription opioid use and its influence on opioid requirements after orthopedic trauma. J Surg Res 2019; 238: 29-34. DOI: 10.1016/j.jss.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Daoust R, Paquet J, Moore L, et al. Early factors associated with the development of chronic pain in trauma patients. Pain Res Manag 2018; 2018: 7203218. DOI: 10.1155/2018/7203218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carre S, Carrie C, Petit L, et al. Rib fracture displacement is a strong predictor for long-term opioid requirement in blunt chest trauma patients. Injury 2020; 51: 1686–1688. DOI: 10.1016/j.injury.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Carrie C, Guemmar Y, Cottenceau V, et al. Long-term disability after blunt chest trauma: don't miss chronic neuropathic pain. Injury 2019; 50: 113–118. DOI: 10.1016/j.injury.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 36.Heindel P, Ordoobadi A, El Moheb M, et al. Patient-reported outcomes 6 to 12 months after isolated rib fractures: a nontrivial injury pattern. J Trauma Acute Care Surg 2022; 92: 277–286. DOI: 10.1097/ta.0000000000003451. [DOI] [PubMed] [Google Scholar]
- 37.Hamilton M, Mathieson S, Gnjidic D, et al. Barriers, facilitators, and resources to opioid deprescribing in primary care: experiences of general practitioners in Australia. Pain 2022; 163: e518–e526. DOI: 10.1097/j.pain.0000000000002340. [DOI] [PubMed] [Google Scholar]
- 38.Harron K, Dibben C, Boyd J, et al. Challenges in administrative data linkage for research. Big Data Soc 2017; 4: 2053951717745678. DOI: 10.1177/2053951717745678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mellish L, Karanges EA, Litchfield MJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Res Notes 2015; 8: 634. DOI: 10.1186/s13104-015-1616-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gnjidic D, Du W, Pearson SA, et al. Ascertainment of self-reported prescription medication use compared with pharmaceutical claims data. Public Health Res Pract 2017; 27. DOI: 10.17061/phrp27341702. [DOI] [PubMed] [Google Scholar]
- 41.Dalli LL, Andrew NE, Cadilhac DA, et al. Agreement between pharmaceutical claims data and patient-reported medication use after stroke. Int J Pharm Pract 2021; 29: 397–399. DOI: 10.1093/ijpp/riab032. [DOI] [PubMed] [Google Scholar]
- 42.Allin S, Bayoumi AM, Law MR, et al. Comparability of self-reported medication use and pharmacy claims data. Health Rep 2013; 24: 3–9. [PubMed] [Google Scholar]
- 43.Kubiak CA, Lee JC, Hamill JB, et al. Agreement between patient-reported pain medication use and electronic medical record data in surgical amputation patients. Plast Reconstr Surg Glob Open 2023; 11: e5415. DOI: 10.1097/GOX.0000000000005415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schug SAPGM, Scott DA, Alcock M, et al. Acute pain management: scientific evidence. 5th ed., 2020. Melbourne. [Google Scholar]
- 45.Australian Commission on Safety and Quality in Health Care . Opioid analgesic stewardship in acute pain clinical care standard – acute care edition. Sydney: ACSQHC, 2022. https://www.safetyandquality.gov.au/publications-and-resources/resource-library/opioid-analgesic-stewardship-acute-painclinical-care-standard-2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Community opioid dispensing after rib fracture injuries: CODI study by Williamson Frances, Proper Melanie, Shibl Rania, Cramb Susanna, McCreanor Victoria, Warren JacelleJ, and Cameron Cate in British Journal of Pain