Abstract
BACKGROUND
Prior studies have shown that preserving the left colic artery (LCA) during laparoscopic radical resection for rectal cancer (RC) can reduce the occurrence of anastomotic leakage (AL), without compromising oncological outcomes. However, anatomical variations in the branches of the inferior mesenteric artery (IMA) and LCA present significant surgical challenges. In this study, we present our novel three dimensional (3D) printed IMA model designed to facilitate preoperative rehearsal and intraoperative navigation to analyze its impact on surgical safety.
AIM
To investigate the effect of 3D IMA models on preserving the LCA during RC surgery.
METHODS
We retrospectively collected clinical dates from patients with RC who underwent laparoscopic radical resection from January 2022 to May 2024 at Fuyang People’s Hospital. Patients were divided into the 3D printing and control groups for statistical analysis of perioperative characteristics.
RESULTS
The 3D printing observation group comprised of 72 patients, while the control group comprised 68 patients. The operation time (174.5 ± 38.2 minutes vs 198.5 ± 49.6 minutes, P = 0.002), intraoperative blood loss (43.9 ± 31.3 mL vs 58.2 ± 30.8 mL, P = 0.005), duration of hospitalization (13.1 ± 3.1 days vs 15.9 ± 5.6 days, P < 0.001), postoperative recovery time (8.6 ± 2.6 days vs 10.5 ± 4.9 days, P = 0.007), and the postoperative complication rate (P < 0.05) were all significantly lower in the observation group.
CONCLUSION
Utilization of a 3D-printed IMA model in laparoscopic radical resection of RC can assist surgeons in understanding the LCA anatomy preoperatively, thereby reducing intraoperative bleeding and shortening operating time, demonstrating better clinical application potential.
Keywords: Rectal cancer, Three-dimensional printing, Inferior mesenteric artery, Left colic artery, Preoperative rehearsal, Intraoperative navigation
Core Tip: Anastomotic leakage is one of the most challenging postoperative complications for surgeons operating on rectal cancer. Preserving the left colic artery significantly reduces the incidence of anastomotic leakage; however, achieving this outcome is technically demanding and time-consuming, particularly for less experienced surgeons. The present study suggests that three-dimensional printing technology can be effectively applied for preoperative simulation to improve intraoperative navigation. This approach helps surgeons optimize the surgical plan, reduces intraoperative bleeding, and shortens operation time.
INTRODUCTION
Colorectal cancer (CRC) is one of the most common malignant cancers of the digestive tract and rectal cancer (RC) worldwide, accounting for approximately one-third of all cases and mortality events associated with CRC[1,2]. Most RC cases are detected at an advanced stage, at which point they pose a significant threat to patient survival. With the increase in life expectancy and the increasingly widespread use of electronic colonoscopy screenings, the incidence of CRC has been gradually rising. The treatment for RC involves a multidisciplinary approach centered on surgery, with significant contributions from medical oncology, radiation oncology, and gastroenterology[3,4]. In clinical practice, the success rates of anus-preserving surgeries for low-lying RC have significantly increased due to several advances in patient care, including the standardization of total mesorectal excision, the adoption of neoadjuvant chemoradiotherapy, the implementation of total neoadjuvant therapy, the application of rectal magnetic resonance imaging, improvements in mechanical stapling technology, and the introduction of improved operating techniques such as transanal total mesorectal excision and intersphincteric resection[5-7]. Anastomotic leakage (AL) is the most serious postoperative complication in RC surgery, causing significant distress for both surgeons and patients[8]. With advancements in laparoscopic surgical techniques and the completion of numerous clinical trials, preservation of the left colic artery (LCA) has been shown to significantly reduce the incidence of AL following operation[9,10].
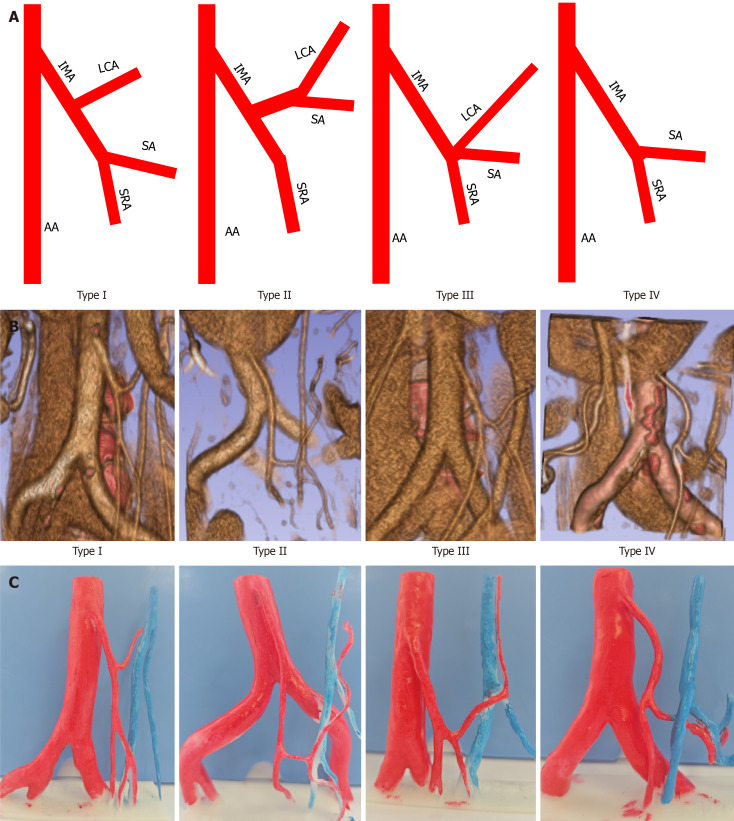
To preserve the LCA during surgery, the surgeon must open the vascular sheath along the inferior mesenteric artery (IMA), and retain the LCA while cutting the sigmoid artery (SA) and the superior rectal artery (SRA)[11]. However, this approach is technically demanding and time-consuming, particularly for less experienced surgeons. The increased surgical difficulty arises from the uncertain anatomical relationships among the branches of the IMA, including the LCA, SA, and SRA[11-13]. Studies have identified four vascular types of the LCA, as follows: (1) Type I, where the LCA arises independently from the IMA; (2) Type II, where the LCA and SA both branch from a common trunk of the IMA; (3) Type III, where the LCA, SA, and SRA all branch at the same location; and (4) Type IV, where the LCA is absent, leaving only the SA and SRA[11,13,14]. Additionally, the length of the IMA trunk and the distance from the origin of the LCA to the root of the IMA shows significant variations among patients[15,16]. Unclear preoperative IMA classification and the origin of the LCA present significant challenges for surgeons. Overcoming this complication is crucial for ensuring surgical success.
Three-dimensional (3D) reconstruction and 3D printing technology can be applied in the medical field to perform preoperative simulation and facilitate intraoperative navigation, thus helping surgeons to select the appropriate surgical plan[17,18]. In addition, 3D printing can aid in the construction of personalized implants, such as hip and knee joints, as well as customized dental crowns, bridges, orthodontic appliances, and implants[19]. Additionally, 3D printing can be used to build precise anatomical models for use in medical education and training, customize 3D-printed surgical guides to help doctors with accurate positioning and cutting, and create personalized drug doses and combinations based on patient needs, thereby enhancing treatment effectiveness and patient compliance[20,21]. However, the use of 3D printing in RC surgery is still in its infancy. In this study, we created a 3D-printed model of the IMA to clarify the morphology of its branches and locate the origin of the LCA prior to surgery. Additionally, we evaluated the role of the 3D-printed model in preoperative rehearsal and intraoperative navigation during laparoscopic RC surgery.
MATERIALS AND METHODS
Patients and study design
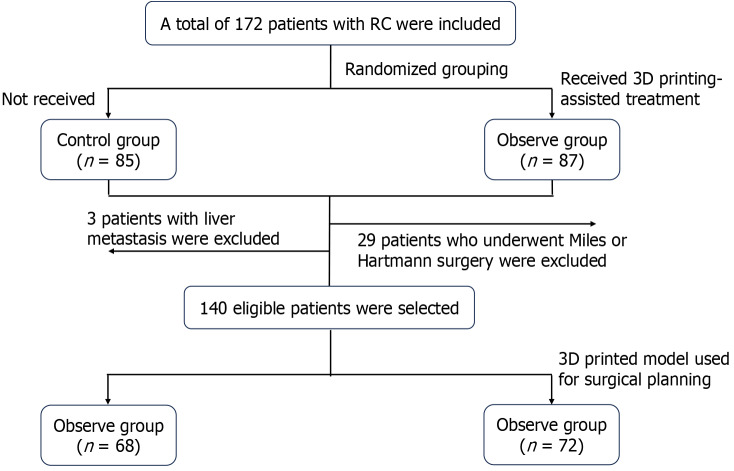
In this retrospective cohort study, participants with RC scheduled to undergo laparoscopic radical resection were divided into a 3D printing group (observation group) and a control group, using a random number table. The study was conducted at Fuyang People’s Hospital from January 2022 to May 2024. The inclusion criteria were as follows: (1) Age over 18 years old; (2) RC confirmed histopathologically prior to operation; (3) Scheduled to undergo laparoscopic radical resection of RC with Dixon reconstruction of the digestive tract; (4) Achievement of R0 resection; (5) Patients with optimal cardiac and pulmonary function; (6) Patients who underwent an abdominal double-phase enhanced scan prior to surgery; and (7) Patients who provided informed written consent to participate in the study. The exclusion criteria were as follows: (1) Occurrence of distant metastasis; (2) Presence of other concurrent malignancies; (3) Surgical procedures which did not include digestive tract reconstruction (Miles or Hartmann); (4) Comorbid severe heart and lung disease; and (5) Comorbid schizophrenia or other mental health disorders, lack of independent behavior ability, or inability to cooperate with treatment. This study was approved by the Ethics Committee of Fuyang People’s Hospital. The study design and flow chart are shown in Figure 1.
Figure 1.
Flowchart of this retrospective case control study. RC: Rectal cancer; 3D: Three dimensional.
Construction of 3D IMA model
Enhanced computed tomography (CT) images were imported in DICOM format into 3D modeling software (3D Slicer 5.2.2 and Mimics 19.0) for 3D reconstruction. The abdominal aorta (AA), left iliac artery, right iliac artery, IMA, LCA, SA, SRA, and inferior mesenteric vein were selected for 3D reconstruction. Using the ‘multiple slice edit’ function, the target arteries and veins were marked in the transverse, sagittal, and coronal planes. The surface of the 3D virtual model was refined using a smoothing process. After confirmation that there were no reconstruction errors by another 3D reconstruction technician, the IMA model was 3D-printed in white resin material using a high-precision SLA 3D printer. The 3D models were subsequently cured, polished, and color-coded, with red representing arteries and blue representing veins. The completed model was subsequently provided to the surgeon prior to the surgery for preoperative evaluation and surgical planning. Before entering the operating room, the model was disinfected with 75% alcohol. The model was positioned next to the laparoscopic monitor to assist with intraoperative navigation of the LCA’s origin and course, and the types of IMA. We confirmed the successful preservation of the LCA based on our intraoperative observations as well as postoperative CT evaluations.
Observation index
The basic characteristics of the two groups were assessed through the evaluation of seven factors: Gender, age, clinical stage, diverting stoma, neoadjuvant therapy, tumor location, and IMA types. We subsequently analyzed additional factors, including the operating time, intraoperative blood loss, number of lymph nodes dissected, and occurrences of lymph vessel and nerve invasion. We further considered tumor invasion depth (T stage), presence of lymph node metastasis (N stage), time of stay in the hospital, postoperative recovery time, costs, and the incidence of postoperative complications, including AL, intestinal obstruction, and wound infection. Postoperative recovery time was defined as the interval from surgery to hospital discharge, whereas hospital stay duration refers to the time from admission to discharge.
Statistical analysis
Using GraphPad Prism 8 software for statistical analysis, measurement data were analyzed using the Student’s t-test or Mann-Whitney U test, while enumeration data were analyzed using the χ2 or Fisher's exact tests. Statistical significance was set at P < 0.05.
RESULTS
IMA types and 3D printing models
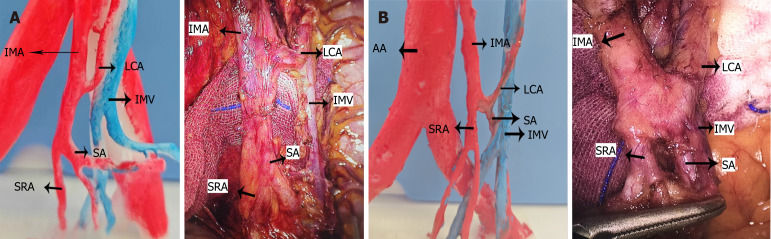
We performed 3D reconstruction and printed 3D models based on the patients’ preoperative enhanced CT images, as shown in Figure 2 and Supplementary Table 1. The 3D printing group included 35, 16, 20, and 1 cases of IMA type I, II, III, and IV, respectively. The mean distance from the origin of the LCA to the root of the IMA was 42.4 ± 9.2 mm, ranging from 17.1 to 70.4 mm. A comparison between photos obtained during operation and the 3D printing IMA model is shown in Figure 3.
Figure 2.
Overview of the four types of inferior mesenteric artery classification. A: Schematic diagrams; B: Based on enhanced computed tomography display; C: Display using three-dimensional printing models. AA: Abdominal aorta; IMA: Inferior mesenteric artery; LCA: Left colic artery; SA: Sigmoid artery; SRA: Superior rectal artery.
Figure 3.
Clinical application of three-dimensional inferior mesenteric artery model in laparoscopic radical resection with preservation of the left colic artery. A: Comparison between the three-dimensional printed model and intraoperative photograph (inferior mesenteric artery type I); B: Comparison between the three-dimensional printed model and intraoperative photograph (inferior mesenteric artery type III). AA: Abdominal aorta; IMA: Inferior mesenteric artery; LCA: Left colic artery; IMV: Inferior mesenteric vein; SA: Sigmoid artery; SRA: Superior rectal artery.
Clinical characteristics
Between January 2022 and May 2024, 172 RC patients who underwent laparoscopic radical resection were included (Figure 1). Among them, 3 patients with liver metastasis who underwent laparoscopic radical resection of RC and partial hepatectomy were excluded. A further 29 patients who underwent abdominoperineal resection (Miles) or laparoscopic radical resection of RC without digestive tract reconstruction (Hartmann) were further excluded. Finally, a total of 140 eligible patients were selected and randomly divided into two groups. The control group (n = 68) underwent surgery without the use of a 3D printing model for preoperative rehearsal and intraoperative navigation, while the observation group (n = 72) underwent surgery following the construction of a 3D printing model. The two groups had similar baseline characteristics, including gender, age, clinical stage, diverting stoma, neoadjuvant therapy, tumor location, and IMA type (P > 0.05). Detailed baseline characteristics are shown in Table 1.
Table 1.
Baseline characteristics of the enrolled rectal cancer patients
|
Characteristic
|
The control group (n = 68)
|
The observation group (n = 72)
|
t/χ2
|
P value
|
| Age (years) | ||||
| mean ± SD | 64.9 ± 12.4 | 66.2 ± 10.5 | 0.636 | 0.513 |
| Median (IQR) | 67.0 (59.0-73.0) | 69.0 (60.0-72.0) | 0.644 | |
| Gender | 0.759 | 0.448 | ||
| Male | 43 | 41 | ||
| Female | 25 | 31 | ||
| Clinical stage | 0.752 | 0.687 | ||
| I | 25 | 23 | ||
| II | 20 | 26 | ||
| III | 23 | 23 | ||
| Diverting stoma | 1.703 | 0.192 | ||
| Yes | 46 | 41 | ||
| No | 22 | 31 | ||
| IMA types | 1.947 | 0.584 | ||
| I | 28 | 35 | ||
| II | 19 | 16 | ||
| III | 21 | 20 | ||
| IV | 0 | 1 | ||
| Neoadjuvant therapy | 0.176 | 0.675 | ||
| Yes | 24 | 23 | ||
| No | 44 | 49 | ||
| Tumor location | 0.471 | 0.790 | ||
| High | 19 | 17 | ||
| Middle | 35 | 41 | ||
| Low | 14 | 14 |
IQR: Interquartile range; IMV: Inferior mesenteric vein.
Perioperative characteristics
Patient perioperative characteristics are shown in Table 2. Operating time (174.5 ± 38.5 minutes in observation group vs 198.5 ± 49.6 minutes in control group, P = 0.002) and intraoperative blood loss (43.9 ± 31.3 mL in observation group vs 58.2 ± 30.8 mL in control group, P = 0.005) were significantly lower in the observation group than in control group. However, there were no significant differences between the two cohorts in number of lymph node dissections, lymph vessel or nerve invasion, depth of tumor invasion, presence of lymph node metastasis, AL occurrence, wound infection, or intestinal obstruction. However, the duration of hospitalization (13.1 ± 3.1 days observation group vs 15.9 ± 5.6 days in control group, P < 0.001), postoperative recovery time (8.6 ± 2.6 days observation group vs 10.5 ± 4.9 days in control group, P < 0.007), and cost of care (35.1 ± 5.9 thousand RMB in observation group vs 40.1 ± 10.1 thousand RMB in control group, P < 0.001) were all significantly lower in the observation group than in the control group. Finally, the incidence of postoperative complications was significantly lower in the observation group than the control group (P < 0.05).
Table 2.
Perioperative characteristics of rectal cancer patients
|
Characteristic
|
The control group (n = 68)
|
The observation group (n = 72)
|
t/χ2
|
P value
|
| Operating time (minute) | ||||
| mean ± SD | 198.5 ± 49.6 | 174.5 ± 38.2 | 3.188 | 0.002 |
| Median (IQR) | 200.0 (165.0-225.0) | 170.0 (150.0-208.8) | 0.004 | |
| Intraoperative blood loss (mL), mean ± SD | 58.2 ± 30.8 | 43.9 ± 31.3 | 2.857 | 0.005 |
| Number of lymph node dissections, mean ± SD | 14.5 ± 5.1 | 14.8 ± 5.5 | 0.336 | 0.738 |
| Lymph vessel invasion | 0.776 | 0.438 | ||
| Yes | 21 | 18 | ||
| No | 47 | 54 | ||
| Nerve invasion | 1.582 | 0.554 | ||
| Yes | 15 | 13 | ||
| No | 53 | 59 | ||
| T | 0.416 | 0.677 | ||
| T1/T2 | 24 | 28 | ||
| T3/T4 | 44 | 44 | ||
| N | 0.237 | 0.813 | ||
| N0 | 45 | 49 | ||
| N+ | 23 | 23 | ||
| Postoperative recovery time (day) | ||||
| mean ± SD | 10.5 ± 4.9 | 8.6 ± 2.6 | 2.754 | 0.007 |
| Median (IQR) | 9.0 (8.0-10.75) | 8.0 (7.0-9.0) | 0.001 | |
| Duration of stay in the hospital (days) | ||||
| mean ± SD | 15.9 ± 5.6 | 13.1 ± 3.1 | 3.639 | 0.001 |
| Median (IQR) | 14.0 (13.0-18.0) | 12.5 (11.0-14.8) | 0.001 | |
| Cost (thousand RMB) | ||||
| mean ± SD | 40.1 ± 10.1 | 35.1 ± 5.9 | 2.105 | 0.001 |
| Median (IQR) | 38.7 (34.7-42.7) | 35.1 (31.4-38.6) | 0.001 | |
| Intestinal obstruction | 0.432 | |||
| Yes | 4 | 2 | ||
| No | 64 | 70 | ||
| Anastomotic leakage | 0.265 | |||
| Yes | 5 | 2 | ||
| No | 63 | 70 | ||
| Wound infection | 0.356 | |||
| Yes | 3 | 1 | ||
| No | 65 | 71 | ||
| Postoperative complications | 4.026 | 0.048 | ||
| Yes | 12 | 5 | ||
| No | 54 | 67 |
IQR: Interquartile range.
DISCUSSION
Preserving the anus and reconstructing the digestive tract are critical aspects of RC surgery in clinical practice. However, AL remains a common and serious postoperative complication, posing a major concern for surgeons. Studies have shown that preserving the LCA can enhance blood supply to the anastomosis, and reduce the risk of AL. However, the IMA exhibits various types and variations, with the origin of the LCA from the IMA differing significantly among patients. According to this study, the distance from the origin of the LCA to the root of the IMA is 42.4 ± 9.2 mm ranging from 17.1 mm to 70.4 mm. Prior research has identified four common types of anatomical variations of the IMA: In type I, the LCA branches off from the IMA early and separately, while the SA and SRA subsequently branch together from the IMA. In type II, the LCA and SA initially branch together from the IMA, then, after traveling a certain distance, the LCA branches off separately from the common trunk. Further, the SRA branches off independently from the IMA. In type III, the LCA, SA, and SRA branch together from the IMA. In type IV, the LCA is absent, with only the SA and SRA being present[11,14]. Preoperative identification of the IMA types and LCA anatomical variations is crucial for the successful completion of laparoscopic RC resection with LCA preservation. In this article, we propose the use of 3D printing technology to preoperatively identify IMA types and LCA anatomical variations, as well as to conduct preoperative rehearsals. During surgery, the 3D model serves as a navigational aid, thereby reducing the difficulty of LCA-preserving procedures. In our study, we found that the operating time (174.5 ± 38.5 minutes in observation group vs 198.5 ± 49.6 minutes in control group, P = 0.002) and intraoperative blood loss (43.9 ± 31.3 mL in observation group vs 58.2 ± 30.8 mL in control group, P = 0.005) were both significantly lower in the 3D printing group than in control group. As such, we surmised that utilizing a 3D-printed model could help surgeons to effectively locate the LCA during surgery, thereby reducing the difficulty and increasing the safety of the procedure. Some studies have previously suggested that 3D printing models can improve the comprehension and assessment of blood vessels, thereby effectively mitigating intraoperative hemorrhage. This notion aligns with the findings of the present study[22,23].
Enhanced CT of the abdomen or pelvis is commonly applied as a preoperative examination for RC, and is widely applied in clinical practice. Although enhanced CT scans can be used to detect the IMA and LCA, it remains challenging for surgeons to mentally visualize the data as precise 3D images. Additionally, classification of the IMA using enhanced CT is difficult and prone to errors. Furthermore, surgeons may forget the specific location of the LCA and become confused, as their attention is focused on the ongoing surgical procedure. In this study, we 3D-printed accurate IMA models preoperatively, and provided them to the surgical team for practice and visualization. Generally, the 3D reconstruction of the IMA took approximately 20 minutes, 3D printing required around 150 minutes, and the coloring process lasted approximately 25 minutes. Surgical team used the 3D models for preoperative rehearsal, determining the steps required to preserve the LCA during the operation. Additionally, the surgical team placed the 3D models next to the laparoscopic television monitor during the operation, thus enabling rapid identification of the LCA through comparison of the anatomical features of the IMA with the 3D model during the surgical procedure. During surgery, we measured and compared the size of the 3D model with the actual vascular anatomy of the patients using sterile silk, which revealed negligible differences.
In this study, we found that postoperative recovery time (8.6 ± 2.6 days vs 10.5 ± 4.9 days, P < 0.007), duration of hospitalization (13.1 ± 3.1 days vs 15.9 ± 5.6 days, P < 0.001), and cost of care (35.1 ± 5.9 vs 40.1 ± 10.1, P < 0.05) were all significantly lower in the observation group than the control cohort. Preoperative identification of the LCA location and IMA types enables the surgeon to develop a personalized and precise surgical plan, thereby avoiding excessive traction of the LCA during surgery, and minimizing thermal injury to the LCA from ultrasonic and electric scalpels[24]. Shorter surgical duration and reduced intraoperative blood loss can both significantly decrease the incidence of postoperative complications[25,26].
Nevertheless, we acknowledge that there may be some biases and limitations to our results. First, this study was a single-center retrospective cohort study, and its design was therefore not as robust or reliable as that of a prospective cohort study. To overcome this limitation, we plan to perform a multicenter, prospective randomized controlled clinical trial in the future to further explore this issue. Furthermore, our analysis did not reveal any significant reduction in the incidence of AL and intestinal obstruction in the observation group, which could be attributed to the limited sample size. Subsequently, we included all complications in our analysis and observed significant differences. In the present study, we only collected data regarding AL, wound infection and postoperative intestinal obstruction as indicators of postoperative complications, neglecting other complications, such as pneumonia, deep vein thrombosis, and gastroparesis, among others. Therefore, we plan to conduct a prospective randomized controlled clinical trial in the future to further investigate these questions. Further, it should be noted that the printing material is inelastic and cannot be pulled or manipulated as in the operation. Furthermore, due to the traction applied during surgery, the spatial orientation of the IMA branches may differ somewhat from the model (Figure 3). Additionally, the creation of 3D models involves both time and cost. In future studies, we plan to assess the cost-effectiveness of 3D models across different clinical scenarios to identify more economically viable solutions. Further, our 3D printing model focuses solely on IMA classification and the location of the LCA, excluding other critical tissues and organs (e.g., the ureters and pelvic organs). Organs such as the ureters and pelvic organs play significant anatomical roles, which may guide the surgeon into the correct anatomical spaces. We plan to further refine the 3D models in future studies and to explore their applications across various clinical scenarios.
CONCLUSION
Overall, the present study showed that utilizing 3D printing IMA models in laparoscopic radical resection of RC can significantly enhance the surgeon’s understanding of the complex anatomy of the IMA prior to surgery. Preoperative rehearsal and intraoperative navigation using the IMA model demonstrated considerable clinical application potential. This approach could help to reduce intraoperative bleeding, shorten operating time, and promote faster postoperative recovery in patients.
ACKNOWLEDGEMENTS
Grateful thanks to the Fuyang People’s Hospital 3D Printing Center for their selfless assistance.
Footnotes
Institutional review board statement: All procedures involving human participants were in accordance with the ethical standards of the institutional and national research committees and Helsinki Declaration and its later amendments. The study was approved by the institutional review board, Approval No. [2024]48.
Informed consent statement: Signed informed consent was obtained from all participants. Patient anonymity has been maintained.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
STROBE statement: The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Sano W S-Editor: Wang JJ L-Editor: A P-Editor: Wang WB
Contributor Information
Zong-Xian Zhao, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Zong-Ju Hu, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China. hzj130123@126.com.
Run-Dong Yao, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Xin-Yu Su, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Shu Zhu, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Jie Sun, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Yuan Yao, Department of Anorectal Surgery, Fuyang People’s Hospital, Fuyang 236000, Anhui Province, China.
Data sharing statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 3.Benson AB, Venook AP, Al-Hawary MM, Azad N, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Garrido-Laguna I, Grem JL, Gunn A, Hecht JR, Hoffe S, Hubbard J, Hunt S, Jeck W, Johung KL, Kirilcuk N, Krishnamurthi S, Maratt JK, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Patel H, Pedersen K, Saltz L, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stotsky-Himelfarb E, Tavakkoli A, Willett CG, Gregory K, Gurski L. Rectal Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20:1139–1167. doi: 10.6004/jnccn.2022.0051. [DOI] [PubMed] [Google Scholar]
- 4.Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Garrido-Laguna I, Grem JL, Gunn A, Hoffe S, Hubbard J, Hunt S, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Patel H, Pedersen K, Saltz L, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Johnson-Chilla A, Gurski LA. NCCN Guidelines Insights: Rectal Cancer, Version 6.2020. J Natl Compr Canc Netw. 2020;18:806–815. doi: 10.6004/jnccn.2020.0032. [DOI] [PubMed] [Google Scholar]
- 5.Piozzi GN, Baek SJ, Kwak JM, Kim J, Kim SH. Anus-Preserving Surgery in Advanced Low-Lying Rectal Cancer: A Perspective on Oncological Safety of Intersphincteric Resection. Cancers (Basel) 2021;13 doi: 10.3390/cancers13194793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fokas E, Schlenska-Lange A, Polat B, Klautke G, Grabenbauer GG, Fietkau R, Kuhnt T, Staib L, Brunner T, Grosu AL, Kirste S, Jacobasch L, Allgäuer M, Flentje M, Germer CT, Grützmann R, Hildebrandt G, Schwarzbach M, Bechstein WO, Sülberg H, Friede T, Gaedcke J, Ghadimi M, Hofheinz RD, Rödel C German Rectal Cancer Study Group. Chemoradiotherapy Plus Induction or Consolidation Chemotherapy as Total Neoadjuvant Therapy for Patients With Locally Advanced Rectal Cancer: Long-term Results of the CAO/ARO/AIO-12 Randomized Clinical Trial. JAMA Oncol. 2022;8:e215445. doi: 10.1001/jamaoncol.2021.5445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collard M, Lefevre JH. Ultimate Functional Preservation With Intersphincteric Resection for Rectal Cancer. Front Oncol. 2020;10:297. doi: 10.3389/fonc.2020.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zarnescu EC, Zarnescu NO, Costea R. Updates of Risk Factors for Anastomotic Leakage after Colorectal Surgery. Diagnostics (Basel) 2021;11 doi: 10.3390/diagnostics11122382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fan YC, Ning FL, Zhang CD, Dai DQ. Preservation versus non-preservation of left colic artery in sigmoid and rectal cancer surgery: A meta-analysis. Int J Surg. 2018;52:269–277. doi: 10.1016/j.ijsu.2018.02.054. [DOI] [PubMed] [Google Scholar]
- 10.Li Z, Zhou Y, Xu L, Xie L. Safety and efficacy of left colic artery preservation in laparoscopic anterior resection for lower rectal cancer. Future Oncol. 2023;19:1485–1494. doi: 10.2217/fon-2023-0475. [DOI] [PubMed] [Google Scholar]
- 11.Wang KX, Cheng ZQ, Liu Z, Wang XY, Bi DS. Vascular anatomy of inferior mesenteric artery in laparoscopic radical resection with the preservation of left colic artery for rectal cancer. World J Gastroenterol. 2018;24:3671–3676. doi: 10.3748/wjg.v24.i32.3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luo Y, Li R, Wu D, Zeng J, Wang J, Chen X, Huang C, Li Y, Yao X. Long-term oncological outcomes of low anterior resection for rectal cancer with and without preservation of the left colic artery: a retrospective cohort study. BMC Cancer. 2021;21:171. doi: 10.1186/s12885-021-07848-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen J, Wang M, Chen Y, Chen S, Xiao J, Fan X, Yang J, He B. A clinical study of inferior mesenteric artery typing in laparoscopic radical resections with left colonic artery preservation of rectal cancer. World J Surg Oncol. 2022;20:292. doi: 10.1186/s12957-022-02762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kobayashi M, Morishita S, Okabayashi T, Miyatake K, Okamoto K, Namikawa T, Ogawa Y, Araki K. Preoperative assessment of vascular anatomy of inferior mesenteric artery by volume-rendered 3D-CT for laparoscopic lymph node dissection with left colic artery preservation in lower sigmoid and rectal cancer. World J Gastroenterol. 2006;12:553–555. doi: 10.3748/wjg.v12.i4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou J, Chen J, Wang M, Chen F, Zhang K, Cong R, Fan X, Yang J, He B. A study on spinal level, length, and branch type of the inferior mesenteric artery and the position relationship between the inferior mesenteric artery, left colic artery, and inferior mesenteric vein. BMC Med Imaging. 2022;22:38. doi: 10.1186/s12880-022-00764-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ke J, Cai J, Wen X, Wu X, He Z, Zou Y, Qiu J, He X, He X, Lian L, Wu X, Zhou Z, Lan P. Anatomic variations of inferior mesenteric artery and left colic artery evaluated by 3-dimensional CT angiography: Insights into rectal cancer surgery - A retrospective observational study. Int J Surg. 2017;41:106–111. doi: 10.1016/j.ijsu.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Khorsandi D, Fahimipour A, Abasian P, Saber SS, Seyedi M, Ghanavati S, Ahmad A, De Stephanis AA, Taghavinezhaddilami F, Leonova A, Mohammadinejad R, Shabani M, Mazzolai B, Mattoli V, Tay FR, Makvandi P. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021;122:26–49. doi: 10.1016/j.actbio.2020.12.044. [DOI] [PubMed] [Google Scholar]
- 18.Zoabi A, Redenski I, Oren D, Kasem A, Zigron A, Daoud S, Moskovich L, Kablan F, Srouji S. 3D Printing and Virtual Surgical Planning in Oral and Maxillofacial Surgery. J Clin Med. 2022;11 doi: 10.3390/jcm11092385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson LA, Christie M, Blackburn BE, Mahan C, Earl C, Pelt CE, Peters CL, Gililland J. 3D-printed titanium metaphyseal cones in revision total knee arthroplasty with cemented and cementless stems. Bone Joint J. 2021;103-B:150–157. doi: 10.1302/0301-620X.103B6.BJJ-2020-2504.R1. [DOI] [PubMed] [Google Scholar]
- 20.Qi W, Qian J, Zhou W, Li J, Mao B, Wen A, Zhao Y, Pan J, Wang Y. 3D-printed titanium surgical guides for extraction of horizontally impacted lower third molars. Clin Oral Investig. 2023;27:1499–1507. doi: 10.1007/s00784-022-04769-3. [DOI] [PubMed] [Google Scholar]
- 21.Teich S, Bocklet M, Evans Z, Gutmacher Z, Renne W. 3D printed implant surgical guides with internally routed irrigation for temperature reduction during osteotomy preparation: A pilot study. J Esthet Restor Dent. 2022;34:796–803. doi: 10.1111/jerd.12847. [DOI] [PubMed] [Google Scholar]
- 22.Mari FS, Nigri G, Pancaldi A, De Cecco CN, Gasparrini M, Dall'Oglio A, Pindozzi F, Laghi A, Brescia A. Role of CT angiography with three-dimensional reconstruction of mesenteric vessels in laparoscopic colorectal resections: a randomized controlled trial. Surg Endosc. 2013;27:2058–2067. doi: 10.1007/s00464-012-2710-9. [DOI] [PubMed] [Google Scholar]
- 23.Lu F, Qiu L, Yu P, Xu DL, Miao YC, Wang G. Application of a three-dimensional printed pelvic model in laparoscopic radical resection of rectal cancer. Front Oncol. 2023;13:1195404. doi: 10.3389/fonc.2023.1195404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aarts MA, Okrainec A, Glicksman A, Pearsall E, Victor JC, McLeod RS. Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc. 2012;26:442–450. doi: 10.1007/s00464-011-1897-5. [DOI] [PubMed] [Google Scholar]
- 25.Yl MK, Patil NS, Mohapatra N, Sindwani G, Dhingra U, Yadav A, Kale P, Pamecha V. Temporary Portocaval Shunt Provides Superior Intraoperative Hemodynamics and Reduces Blood Loss and Duration of Surgery in Live Donor Liver Transplantation: A Randomized Control Trial. Ann Surg. 2024;279:932–944. doi: 10.1097/SLA.0000000000006200. [DOI] [PubMed] [Google Scholar]
- 26.Maheshwer B, Drager J, John NS, Williams BT, LaPrade RF, Chahla J. Incidence of Intraoperative and Postoperative Complications After Posterolateral Corner Reconstruction or Repair: A Systematic Review of the Current Literature. Am J Sports Med. 2021;49:3443–3452. doi: 10.1177/0363546520981697. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.