Abstract
Purpose
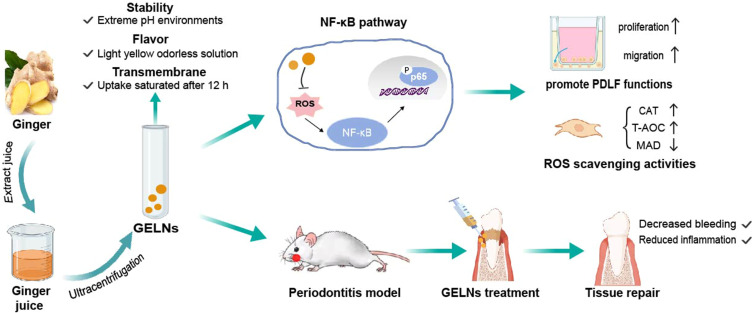
Periodontitis is a chronic inflammatory oral disease that causes defects in periodontal tissue. Conventional therapies are limited, and often lead to high recurrence rates. The emerging concept of medicinal food homology has shed light on the potential of ginger as a therapeutic adjuvant for periodontitis, given its antioxidant and anti-inflammatory properties. However, fresh ginger exhibits poor stability and bioavailability. Ginger exosome-like nanoparticles (GELNs), a derivative of ginger, have not been reported to exert therapeutic effects in periodontitis. This study aimed to explore the therapeutic effects of GELNs on tissue damage caused by periodontitis and their underlying mechanisms of action.
Methods
The GELNs composition was analyzed using a widely targeted metabolome. Stability was assessed using nanoparticle tracking analysis (NTA) and zeta potential measurements, flavor was evaluated using an electronic nose, and membrane penetration was studied using confocal microscopy. A periodontitis model was established in SD rats, periodontal clinical indicators were monitored, and histological changes were assessed using H&E and TRAP staining. Co-culture experiments investigate the antioxidant and reparative abilities of GELNs on periodontal ligament fibroblasts (PDLFs) in inflammatory environment. NF-κB protein expression was examined by immunofluorescence and immunohistochemistry.
Results
The findings revealed that GELNs demonstrated good stability in different environments and mitigated the pungent taste of the raw ginger. In vivo experiments showed that GELNs improved periodontal clinical parameters and pathology compared with ginger juice. In vitro data suggested that GELNs enhanced the proliferation and migration of PDLFs while reducing the reactive oxygen species (ROS) levels by inhibiting the NF-κB signaling pathway in an inflammatory setting.
Conclusion
This study is the first to demonstrate that GELNs have a potential therapeutic effect on periodontitis. GELNs can alleviate oxidative stress (OS) and inflammatory reactions by inhibiting the NF-κB signaling pathway. These findings provide a promising method for the treatment of periodontitis by regulating an unbalanced OS state.
Keywords: ginger exosome-like nanoparticles, periodontitis, tissue repair, oxidative stress, periodontal ligament fibroblasts
Graphical Abstract
Introduction
Periodontitis is a chronic inflammatory disease that affects periodontal supporting tissues, leading to symptoms, such as bleeding gums, swelling, destruction of periodontal ligaments, alveolar bone absorption, and tooth loss. Epidemiological data indicate that periodontitis affects 70–80% of adults.1 Traditional treatment methods focus on eliminating pathogenic microorganisms and preventing bacterial regrowth using mechanical debridement and adjunctive pharmacotherapy.2 Nevertheless, challenges such as mechanical trauma and antibiotic resistance frequently result in suboptimal treatment outcomes and increased rates of recurrence.3
Excessive reactive oxygen species (ROS) and the subsequent induction of high oxidative stress (OS) in cells have been identified as the primary pathogenic factors in the early stages of periodontitis, causing oxidative damage to periodontal tissues.4 In recent decades, there has been growing emphasis on the use of natural foods for the treatment of human diseases, particularly in research involving fresh herbs and plant-based products. The World Health Organization has reported that 25% of medical drugs in developed countries are derived from herbs.5 It is worth mentioning that ginger, a traditional Chinese herbal medicine used for thousands of years, contains a variety of active ingredients with strong antibacterial, anti-inflammatory, antioxidant, and other pharmacological activities, such as gingerol, gingerone and diphenylheptane compounds.6 The efficacy of ginger has been evaluated in various inflammatory diseases, including neurodegenerative diseases and acute kidney injury, etc.7 Preliminary findings and reports on the treatment and prevention of periodontitis have been published. For example, Javid et al found that ginger supplements could reduce OS and improve periodontal status in patients with type 2 diabetes, thereby improving periodontal status.8 Polyphenols in ginger have been shown to promote the antioxidant stress ability of periodontal stem cells, osteogenic differentiation, and periodontal tissue repair.9 However, the taste of fresh ginger is unpleasant and shows high intrinsic clearance (with values above 5 mL/min/g).10 In addition, a clinical study showed that volunteers who received ginger orally three times a day (400 mg/dose) fortnight exhibited mild diarrhea and heartburn on both days of the experiment, and a cumulative dose of more than 6 g of ginger caused strong gastric irritation.11 Therefore, effective exertion of the therapeutic potential of ginger has become an urgent problem.
Ginger exosome-like nanoparticles (GELNs) are natural nanocarriers derived from ginger and are rich in lipids, proteins, RNA, and other active molecules, with sizes ranging from 50 to 500 nm.12 It can not only carry and concentrate the original pharmacologically active ingredients of ginger, but also serve as a drug carrier for information exchange because of its excellent membrane permeability. According to several previous reports, GELNs have been found to fight bacteria and viruses in digestive and nervous systems.13 However, about their anti-inflammatory and antioxidant properties are lack of validation regarding. The active compounds in GELNs that exert these anti-inflammatory effects are not well defined. Furthermore, it is unclear whether GELNs modulate the unbalanced OS state in periodontitis and promote periodontal tissue repair.
In the present study, we extracted GELNs from fresh ginger and compared the effects of GELNs and ginger juice on periodontitis. Our hypothesis suggests that GELNs can ameliorate deficiency of raw materials and regulate excessive ROS levels in the periodontitis microenvironment. We observed the physical characteristics of the GELNs (eg, odor, stability, and transmembrane properties) and analyzed their unique metabolite profiles using a widely targeted metabolome. Our results indicate that GELNs have promising potential for medicinal applications. Furthermore, our study focused on the ability of GELNs to modulate ROS levels in both in vitro and in vivo periodontal inflammatory environments as well as their therapeutic impact on periodontal tissue repair. These findings serve as a basis for future clinical utilization of plant-derived extracellular vesicles in the management of periodontitis.
Materials and Methods
Isolation and Purification of Ginger-Exosome-Like Nanoparticles (GELNs)
The original botanical description of ginger (Zingiber officinale) can be found in the work “Species Plantarum” by Carl von Linné, published in 1753. An early record of ginger in ancient China can be found in the “Analects of Confucius”, where Confucius mentions. We can find the specimen in Chinese Virtual Herbarium (https://www.cvh.ac.cn/spms/list.php?andtaxonName=%E5%A7%9Candoffset=30). In addition, Shanxi Medical University does not require additional approval for plant material research.
Ginger exosome-like nanoparticles (GELNs) were isolated by processing fresh ginger through a series of steps. Initially, the cleaned and minced ginger was blended to extract the ginger juice. The ginger juice was sequentially centrifuged at varying speeds (2000g for 20 min, 6000g for 40 min, and 10,000g for 60 min at 4°C) to eliminate large particles and fiber fragments. The supernatant was processed by ultracentrifugation (Beckman Optima Type 70 Ti; Beckman, USA) at 150,000 g for 90 min. Subsequently, the supernatant was removed, and GELNs were obtained by resuspension in 200 μL PBS. The GELNs were then subjected to filtration and centrifugation using an exosome purification kit (Umibio, UR52121). Finally, the isolated GELNs were stored at −80°C for future experiments.
Physicochemical and Component Characterization
GELNs were analyzed using nanoparticle tracking analysis (NTA) (Particle Metrix, Zetaview-PMX120-Z, Germany) to determine their size, concentration distribution, and zeta potential. Micrographs of GELNs were captured using a transmission electron microscope (Hitachi HT-7700, Japan). A BCA protein assay kit (KeyGEN BioTECH KGB2101-100, China) was used to determine the protein concentrations of the GELNs. Extensive targeted metabolomic analysis was performed to further elucidate the composition of GELNs (Wuhan Jinkairui Biotechnology). Additionally, electronic nose testing (Beijing Yingsheng Hengtai Technology) was conducted on both GELNs and ginger juice to analyze the predominant characteristic flavors emitted by the samples.
Intervention on a Rat Ligature-Induced Periodontitis Model
All animal experiments were conducted in accordance with the “Regulations on the Management of Laboratory Animals” and the “Guidelines for the Care and Use of Laboratory Animals” from the Shanxi Province. This study was approved by the Ethics Committee of the Shanxi Medical University (2024–032). Make every effort to reduce the number of rats used and alleviate their suffering. Male SD rats, aged 6–8 weeks, were obtained from the Animal Experimental Center at Shanxi Medical University and housed in a specific pathogen-free environment. The rats were anesthetized with pentobarbital sodium (Merck Millipore) via a peritoneal injection. Subsequently, placing 0.2 mm orthodontic ligature wire around the cervical area of the maxillary right first molars for six weeks to induce periodontitis.
We randomly selected 24 of the above periodontitis model rats for intervention. The rats were randomly assigned tofour groups (N=6/group) as follows: 1) control group (Ctrl), no ligation was performed; 2) ligature group (Perio), rats with untreated ligature-induced periodontitis; 3) GELNs group, rats with ligature-induced periodontitis treated with GELNs; and 4) ginger juice group, rats with ligature-induced periodontitis treated with ginger juice. Subsequently, 25 µL of 100 µg/mL GELNs and ginger juice were injected into the gingiva of the treated molars at the palatal, buccal, mesial, and distal sites once every other day. After two-week period, all rats were euthanized using an anesthetic overdose and tissue samples were collected for further analysis.
Histological Analysis
Three rats were randomly selected from each four groups and the periodontal and bone tissues of the maxilla were completely removed. The samples were fixed in 4% paraformaldehyde for 24 h, washed thoroughly with running water, and soaked in ethylenediaminetetraacetic acid (EDTA) decalcification solution. The fresh decalcification solution was replaced every two days until the needle could be inserted without resistance, indicating successful decalcification. Subsequently, alcohol gradient dehydration was performed, followed by xylene treatment, to ensure transparency. The samples were embedded in paraffin at a slice thickness of 4.0 μm. Histological evaluation was performed using H&E and TRAP staining to assess histological changes and osteoclast counts in the periodontal tissue.
Cell Culture and Stimulation
Periodontal ligament fibroblasts (PDLFs) were cultured in DMEM (Gibco, C11995500BT, Australia) containing 10% FBS (Gibco, 10099–141, Australia) and 1% penicillin-streptomycin solution (Solarbio, P1400, China) at 37°C and 5% CO2. PDLFs were stimulated with or without 1 μg/mL LPS from Porphyromonas gingivalis (P.g) (AbMole, M9542, China) for 24 h to simulate an inflammatory environment.
In vitro Internalization of GELNs
Cells were seeded on 24-chamber slides (Thermo Fisher Scientific, USA) at a density of 5×105 cells/well and cultured overnight at 37 °C. Subsequently, the culture medium was replaced with fresh medium containing GELNs (1μg/mL and 10 μg/mL) previously labeled with PKH 26 (Solarbio, D0030, China), following the manufacturer’s protocol. After 1, 6, 12, and 24 h of incubation, the cells were stained with DAPI and fixed with 4% paraformaldehyde for 10 min. The uptake of GELNs was observed using confocal fluorescence microscopy.
Cell Viability Assay
The Cell Counting Kit-8 (Beyotime, C0038, China) was used to assess cell viability. PDLFs were seeded at a density of 5.0×104 cells/well in a 96-well plates and incubated at 37°C with 5% CO2 for 24h. Subsequently, the culture medium was replaced with 100 µL of fresh medium containing either ginger juice or GELNs at varying concentrations, followed by further incubation for 6, 12, or 24h at 37°C. The negative controls included untreated cells and culture medium alone, which served as cells without the test compound and medium control, respectively. Following treatment, the cells were exposed to 10% CCK-8 reagent for 2h, and absorbance was measured at 562 nm using a microplate reader (SpectraMax plus384, USA). Cell viability was calculated as follows:
Cell Proliferation and Migration
PDLFs were seeded at 5.0×104 cells/well in a 96-well plate at 37 °C with 5% CO2 for 24 h and were divided into four groups: control group (PDLFs), LPS group (PDLFs+LPS), ginger juice group (PDLFs+LPS+3% ginger juice), and GELNs group (PDLFs+LPS+10 μg/mL GELNs). Next, EdU (100 μL) 2X solution was added to each well and incubated for an additional 2 h. The Apollo dye solution (100 μL) was then added to each well and kept in the dark at room temperature for 30 min. Then 100 μL of penetrant was added, followed by rinsing three times with PBS. Nuclei were stained with DAPI and observed using confocal fluorescence microscopy.
PDLFs were cultured at 37°C for 24 h as per the aforementioned above. On the second day, the cells were marked with a 200 μL pipette tip perpendicular to the pore plate, washed with PBS, and placed in serum-free medium. Samples were taken at 0, 12, and 24h time points for imaging. The mean distance between scratches was calculated using the Image J software.
ROS Assay
PDLFs were seeded in 6-well plates at a density of 1.0×105 cells/well and incubated overnight. They were then treated with GELNs or ginger juice, with or without 1 mmol/L H2O2 and 0.1 mg/mL LPS, for 2 h. Subsequently, the cells were incubated with 1 mL/well of DCFH-DA (10 μmol/L) at 37°C for 20 min and fluorescence images were captured using a microscope.
Immunofluorescence
For immunofluorescence analysis of NF-κB/p65 nuclear translocation, PDLFs from the aforementioned groups were pretreated with or without GELNs for 12 h. The cells were fixed with 4% paraformaldehyde, permeabilized with 0.5% Triton-100 for 20 min, and incubated with p65 antibody (Affinity Biosciences, 1:200) for 2 h at room temperature. Subsequently, the cells were treated with an Alexa Fluor 488-conjugated secondary antibody (Servicebio, 1:400) for 1 h at room temperature. Finally, cells were stained with DAPI and observed under a confocal microscope.
Statistical Analysis
ANOVA and t-tests were performed using GraphPad Prism 7 software to determine significance levels (*p<0.05, **p<0.01, ***p<0.001).
Results
Characterization and Composition of GELNs
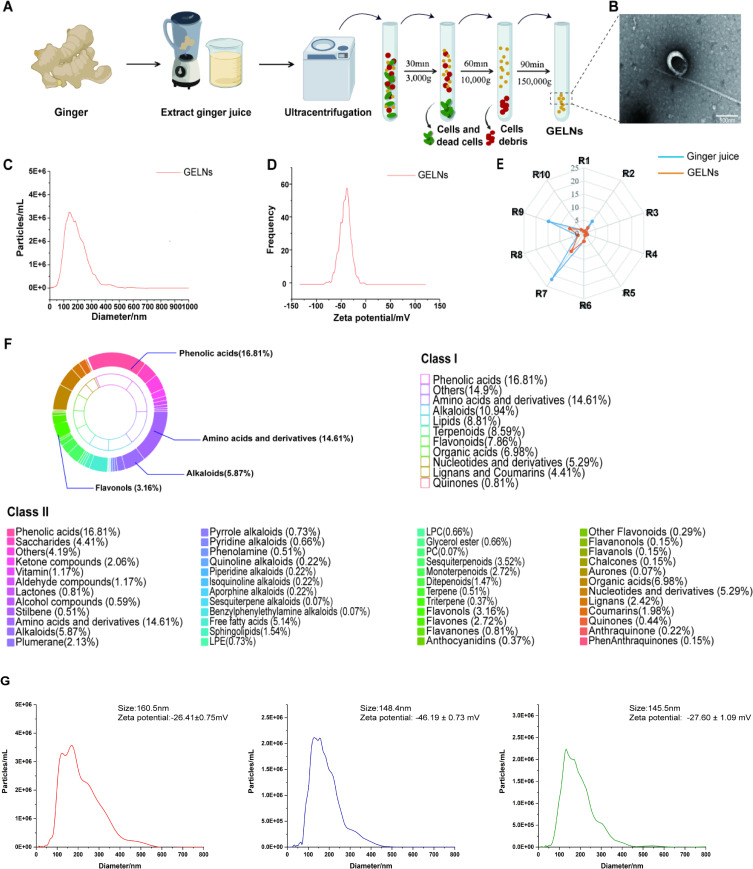
GELNs were isolated from fresh ginger by ultracentrifugation (Figure 1A). Transmission electron microscopy (TEM) revealed morphologically homogeneous GELNs with a uniform round or cup structure (Figure 1B). The size distribution and concentration of GELNs were determined using NTA. GELNs’ average diameter were ~161.2 nm and the original concentration of GELNs was 2.3×1010particles/mL. The zeta potential of the GELNs was negative value (−35.7mV) (Figure 1C and D).
Figure 1.
Isolation and characterization of GELNs. (A) Schematic representation of the method used to isolate and purify GELNs from ginger. (B) Transmission electron microscopy of GELNs, bar: 500 nm. (C) Concentration of GELNs determined by NTA measurement. (D) zeta potential of GELNs. (E) Electronic nose technology detect the flavour differences between GELNs and ginger juice. (F) Widely targeted metabolome analysis the compounds contained in GELNs. (G) Stability of GELNs in different pH environments.
Abbreviations: GELNs, ginger exosome-like nanoparticles.
To better understand the composition and potential biological functions of GELNs, a widely targeted metabolome analysis was employed to identify the compounds present in GELNs. The results showed that phenolic acids, amino acids and derivatives accounted for a considerable proportion of the GELNs (16.81% and 14.61%, respectively). There were also important herbal compounds such as alkaloids (10.96%), terpenoids (8.59%), and flavonoids (7.86%) (Figure 1F). Functional characterization of these compounds showed that they were enriched in metabolic pathways, linoleic acid metabolism, and pathways involving alanine, aspartate, and glutamate metabolisms. In addition, we used electronic nose technology to detect flavor differences between GELNs and ginger juice. This report showed that the odor of ginger juice is more pronounced and stronger than that of GELNs. Significant differences were observed between R7 (related to hydrogen sulfide) and R9 (related to aromatic compounds and organic sulfides) (Figure 1E). According to previous reports, the spicy and pungent taste of ginger is mainly sensed by R3 (related to amino compounds and aromatic components), R8 (related to alcohol compounds and some aromatics), and R9. This suggests that GELNs reduce the perception of spicy and pungent tastes.
To confirm the stability of GELNs under physiological conditions, we mimicked in vivo conditions by suspending GELNs in solutions of different pH (pH 2, 5.5, and 7). The zeta potential is a significant characteristic that can be used to assess stability. In general, the zeta potential was the most stable at an absolute values of approximately 30mV. Compared with PBS-dissolved, the zeta potential absolute value were declined (−26.4mV and −27.6mV) in pH 2 (Figure 1G left) and 7 (Figure 1G right), while increased in pH5.5 (−46.2mV) (Figure 1G middle). Although the zeta potential of GELNs varies at different PH values, their absolute values are all around 30mV, indicating that they are still stable And the size of GELNs remained almost constant at different pH values (Figure 1G).
In summary, GELNs exhibit characteristics similar to extracellular vesicles, containing multiple biologically active compounds and their corresponding pathways, without a pungent smell. This opens up basic and clinical possibilities for future studies.
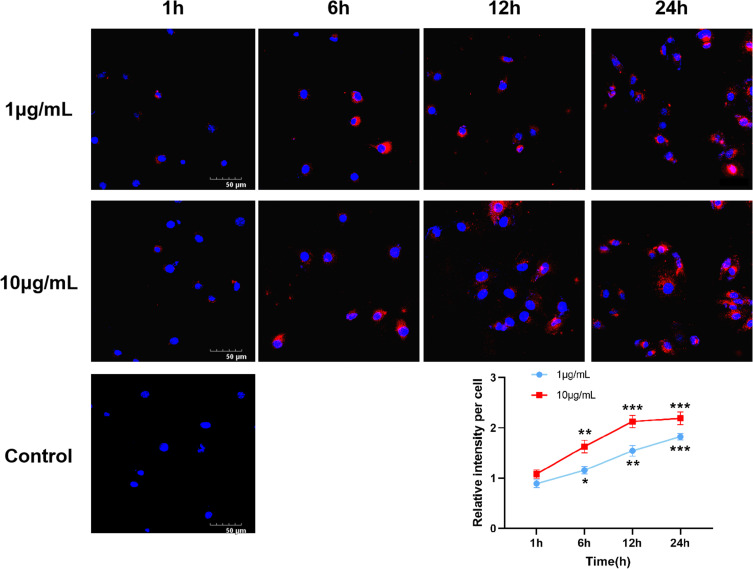
Cellular Uptake of GELNs into PDLFs
To quantitatively assess the cellular uptake of GELNs, PDLFs were treated with different concentrations of 1 or 10 µg/mL GELNs for 1, 6, 12, and 24h, resulting in a time-dependent and concentration-dependent increase in uptake. The distribution of GELNs in the cytoplasm surrounding the nucleus is shown in Figure 2. Saturation of GELNs uptake at 1 µg/mL occurred after 24h, while saturation at 10 µg/mL was rapid and happening after 12h. Based on biosafety findings, the optimal concentration of GELNs was determined to be 10 µg/mL, with 24h post-treatment identified as the optimal time for absorption measurements.
Figure 2.
Cellular uptake of GELNs. Representative fluorescence microscope images of cellular uptake of GELNs at 1 and 10 μg/mL. Scale bars: 50μm. *, ** and *** indicate difference for p<0.05, p<0.01 and p<0.001 in comparison to the cells treated with cell culture media as negative control, respectively, n=3.
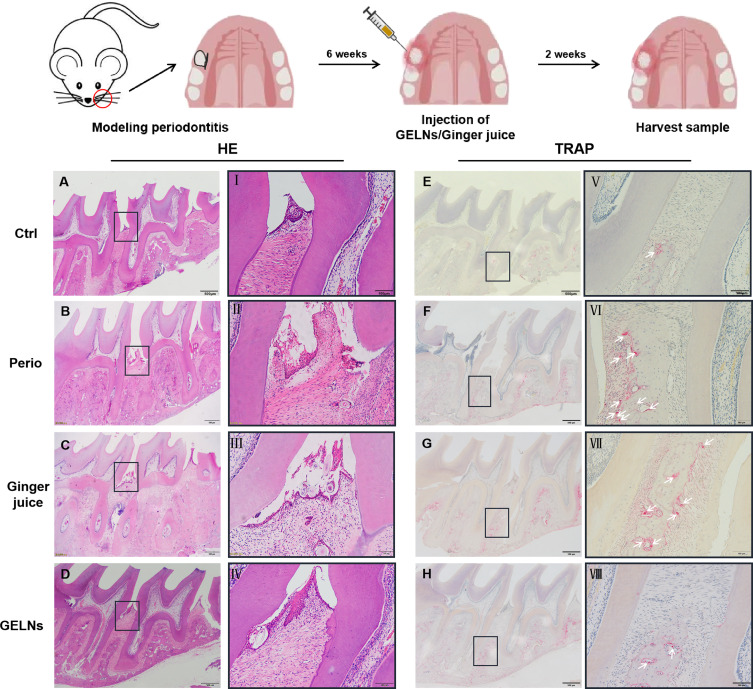
GELNs Mitigate Periodontal Tissue Injury of Ligature-Induced Periodontitis in Rats
To compare the therapeutic effects of GELNs and ginger juice on periodontitis, a general periodontal examination and histological analysis were conducted. The experimental procedure is illustrated in Figure 3. Apart from the Ctrl group, the periodontal morphology and texture of maxillary first molar ligation differed among the three groups. The GELNs group exhibited tough, pink periodontal tissue with a significantly reduced bleeding index (SBI), probing depth (PD), and tooth mobility(TM) compared with the Perio group. The ginger juice group showed slight gingival edema, with clinical indicators between those of the Perio and GELNs groups (Table 1).
Figure 3.
The histological analysis of periodontal tissues in four rat periodontitis models. (A-D) H&E staining of periodontal tissues around the maxillary first molar after 2 weeks treatment of GELNs, scale bar: 500 µm. The I-IV indicate magnification of black rectangle, sacle bar: 100 µm. (E-H) TRAP staining for osteoclast, scale bar: 500 µm. The white arrows in (V-VIII) indicate TRAP-positive (stained red) cells, scale bar: 100 µm.
Table 1.
Results of Periodontal Clinical Indexes in Rats 
| Group | Number of Rats | SBI | PD | TM |
|---|---|---|---|---|
| Ctrl | 6 | 0.66±0.51 | 0.12±0.03 | 0.36±0.24 |
| Perio | 6 | 3.13±0.64* | 1.14±0.25* | 1.69±0.40* |
| Ginger juice | 6 | 2.00±0.82ab | 0.85±0.24a | 1.32±0.31ab |
| GELNs | 6 | 0.73±0.65a | 0.31±0.28a | 0.53±0.27a |
Notes: *Compared with Ctrl, P<0.05; a. Compared with Perio, P<0.05; b. Compared with GELNs, P<0.05.
H&E staining analysis showed that the normal periodontal tissue had orderly arranged periodontal membrane fibers, with the epithelium attached to the enamel-dentin junction, and no obvious inflammatory cell infiltration. Significant tissue destruction was observed in the periodontitis group, accompanied by disorganization of the epithelial layer, irregular pieces of alveolar bone, and hyperemia. Both the GELNs and ginger juice groups showed a trend of reduced inflammatory cell infiltration and increased collagen fiber proliferation. Moreover, the GELNs group showed increased proliferation of periodontal collagen fibers, shallower periodontal pocket depth, and decreased absorption at the alveolar crest (Figure 3A–D).
To assess the effect of GELNs treatment on osteoclast formation in periodontitis rats periodontal tissues, we used TRAP staining to observe osteoclasts. Compared with the Ctrl group, the number of TRAP-positive osteoclasts around the alveolar bone was significantly increased in the Perio group. Following treatment with GELNs and ginger juice, the number of osteoclasts decreased significantly and GELNs showed better inhibition, indicating that GELNs inhibited osteoclast differentiation and reduced bone loss (Figure 3E–H).
The Effects of GELNs on the Function and Anti-Oxidation of PDLFs
PDLFs are vital periodontal tissue cells responsible for maintaining regeneration and reconstruction of periodontal tissue through proliferation and differentiation.14 In periodontitis, PDLFs are vulnerable to ROS attack, leading to cell damage and disruption of periodontal homeostasis. To simulate the in vitro periodontitis environment, PDLFs were induced with LPS and the effects of ginger juice and GELNs on promoting tissue repair were compared.
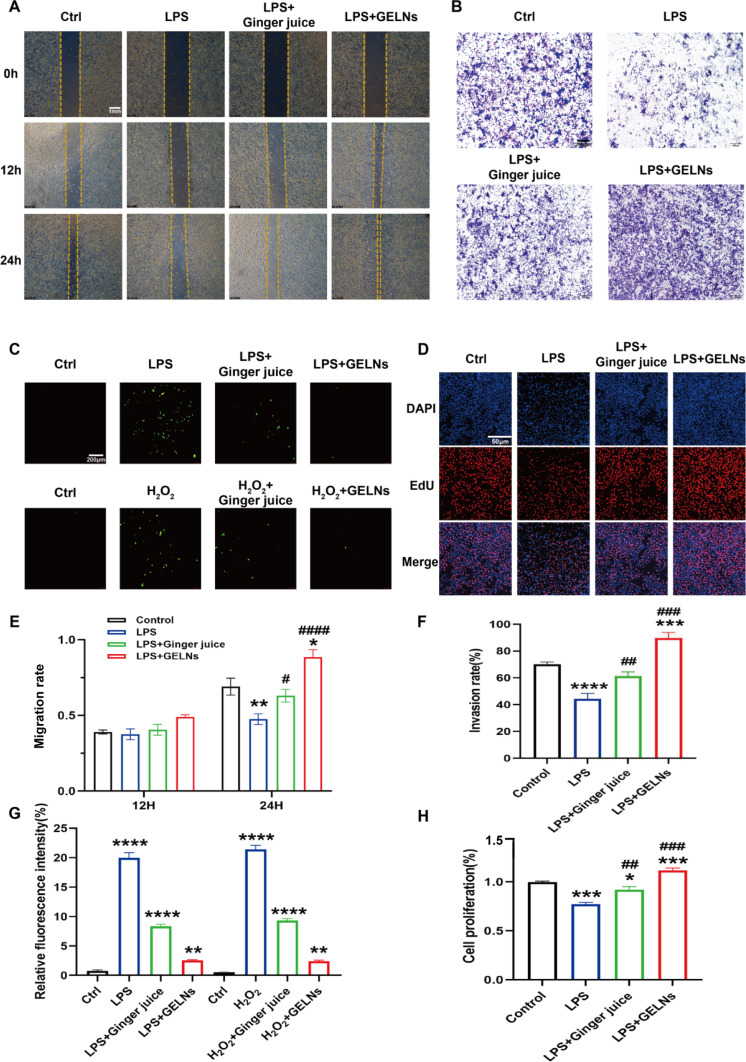
Cell migration is essential for tissue healing. To compare the effects of GELNs and ginger juice on the migration of PDLFs in an inflammatory environment, a scratch-wound assay was performed. PDLFs were stimulated with LPS for 12 h and then treated with either 10 μg/mL GELNs or 3% ginger juice in a serum-free culture medium for 0, 12, or 24 h. Compared with the serum-free DMEM control, the results showed that GELNs group exhibited significant migration of PDLFs cells at 24 h. The migration levels in the ginger juice group were similar to those in the blank control group. However, the cell migration ability was severely inhibited after LPS treatment, indicating that in an inflammatory environment, the migration ability of PDLFs cells was hindered, which is unfavorable for tissue healing (Figure 4A). The extent of migration was quantified and is presented as a histogram (Figure 4E). Additionally, the Transwell assay, another widely used method to evaluate cell migration found the invasion rate increased by 40% after GELNs intervention compared with LPS group, confirming that GELNs has a strong ability to promote migration (Figure 4B and F).
Figure 4.
The proliferation, migration and antioxidant effect of GELNs on PDLFs. (A) Cell scratch test result of GELNs intervened PDLFs after 12 and 48h, scale bar: 1 mm. (B)The effect of GELNs on PDLFs invasion after 24h, scale bar: 100 µm. (C) Detection of intracellular ROS levels by DCFH-DA, scale bar: 200 µm. (D) EdU effects on proliferation of PDLFs, scale bar: 50 µm. (E) Quantitation of the migration results. (F) The number of invading cells are presented as percent of invading cells. (G) Quantitative measurements the relative fluorescence intensity. (H) Quantitative measurements the proliferation of EdU-labeled PDLFs. *, **,*** and **** indicate difference for p<0.05, p<0.01, p<0.001 and p<0.0001 in comparison to Ctrl, respectively. #, ##,###and #### indicate difference for p<0.05, p<0.01, p<0.001 and p<0.0001 in comparison to LPS, respectively. n=3.
Abbreviations: DCFH-DA, 2’,7’-Dichlorofluorescin diacetate; PDLFs, periodontal ligament fibroblasts; ROS, reactive oxygen species.
EdU, a thymidine nucleoside analog, accurately reflects cell proliferation through EdU labeling. The number of EdU-positive cells in the GELNs group was significantly higher than that in the LPS group (34.48%). Additionally, cells treated with ginger juice showed higher numbers compared to the LPS group but were still lower than those in the Ctrl and GELNs groups (Figure 4D and H).
Furthermore, to assess the impact of GELNs on cellular damage caused by OS, PDLFs were stimulated with H2O2 and LPS to mimic exogenous and endogenous ROS (Figure 4C). DCFH-DA results showed that the green fluorescence intensity of the H2O2 and LPS groups significantly increased 20 times compared to that of the Ctrl group. After GELNs treatment, the intracellular green fluorescence intensity decreased by 4 times compared with that in the H2O2 and LPS groups (Figure 4G). These results demonstrated that GELNs have potent antioxidant properties and can effectively scavenge ROS from various sources to protect cells from OS damage.
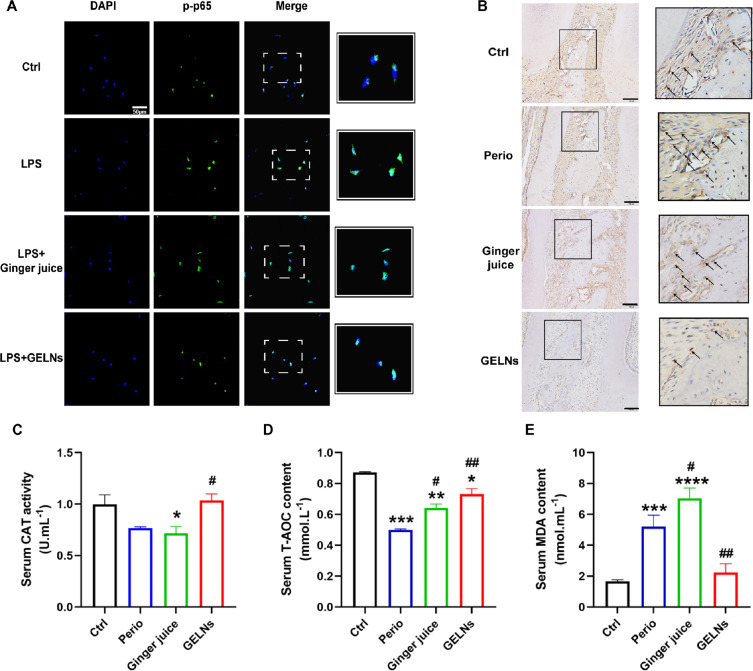
GELNs Inactivate NF‑κB Pathway for Antioxidant Effect
Activation of the NF-κB signaling pathway induces the release of inflammatory factors and accumulation of oxidative free radicals, disrupting the original balance and leading to periodontitis. p65, a subunit of the NF-κB family, activates this pathway and regulates cellular inflammatory response within cells.15 Phosphorylation and nuclear translocation of p65 signify activation of the NF-κB pathway. Our immunofluorescence results revealed increased fluorescence of p-p65 stimulated by LPS compared to that in the Ctrl group, with translocation to the nucleus. Conversely, the p-p65 protein levels in the GELNs group were significantly lower than those in the LPS group, which inhibited nuclear translocation. In the ginger juice group, p-p65 fluorescence remained in the nucleus, overlapping with blue fluorescence (Figure 5A).
Figure 5.
The antioxidant mechanism of GELNs. (A) The nuclear translocation of p-p65, scale bar: 50μm. (B) Immunohistochemical images of NF-κB from different groups, scale bar: 100μm (left of Figure 5B). The right side is a magnification of the black box on the left (scale bar:50μm). The NF-κB positive cells are marked with black arrows. (C-E) CAT, T-AOC, MDA activity. Data are shown as the mean±SD, n=3. *, **,*** and **** indicate difference for p<0.05, p<0.01, p<0.001 and p<0.0001 in comparison to Ctrl, respectively. # and ## indicate difference for p<0.05, p<0.01 in comparison to Perio, respectively.
Abbreviations: CAT, catalase; MDA, malondialdehyde; T-AOC, total antioxidant capacity.
Immunohistochemical staining was performed to quantify NF-κB protein expression in the rats from the four groups. The results indicated that NF-κB expression was lower in the GELNs group than in the Perio group, suggesting that GELNs may inhibit the NF-κB signaling pathway and reduce inflammatory responses (Figure 5B). NF-κB plays a crucial role in the cellular defense against OS and activates various antioxidant enzymes. Following GELNs treatment, NF-κB-associated antioxidant indicators, such as catalase (CAT) and total antioxidant capacity (T-AOC), were significantly increased in the serum (Figure 5C and D), while malondialdehyde (MDA) levels, an indicator of OS, were reduced in the GELNs group (Figure 5E). These results indicated that GELNs effectively reduced ROS levels in periodontitis and had good antioxidant properties.
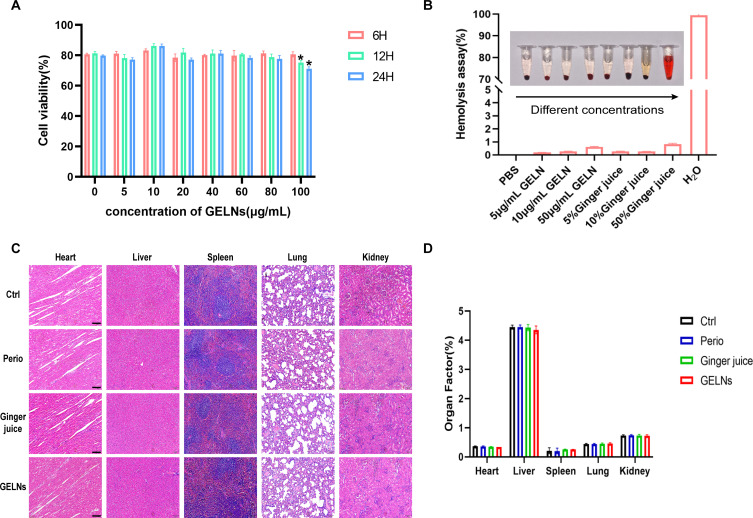
Biosafety Evaluation of GELNs
Prior to clinical translation, the biosafety evaluation of GELNs is essential. According to the well-established ISO 10993.5, medical materials are considered non-cytotoxic when the cell viability rate is greater than 70%.16 CCK8 assays revealed no obvious cytotoxicity of GELNs towards PDLFs at concentrations of up to 100 μg/mL (Figure 6A).
Figure 6.
In vitro and in vivo biosafety evaluation of GELNs. (A) Viabilities of PDLFs after incubation with GELNs at different concentrations for 6h,12h,24h, n=3.* indicate difference for p<0.05 in comparison to 6h. (B) Hemolysis test under different concentrations of GELNs and ginger juice by using blood of rats, n=3. (C) H&E staining of main organs slices from four group rats, scale bar:100 μm. (D) The organs coefficients, n=3.
The hemolytic effects were assessed using whole-rat blood samples. Three concentrations of GELNs (5, 10, 50 μg/mL) and ginger juice (5%, 10%, 50%) were mixed with blood and incubated at 37°C for 30min. Compared with the negative control (PBS, which was regarded as having a 0% hemolysis rate) and the positive control (H2O, which was regarded as having a 100% hemolysis rate), the hemolysis rates of GELNs and ginger juice were less than 1%, indicating good biocompatibility (Figure 6B).
Next, the biosafety of the GELNs in vivo was examined. H&E staining for histological analysis of the main organs (heart, liver, spleen, lung, and kidney) did not reveal any clear evidence of organ damage in any group. Organ coefficients, as a major index of chronic toxicity, were also calculated and revealed no significance in any of the groups (Figure 6C and D). Thus, these results demonstrate that GELNs have excellent biosafety and promising potential for biological applications.
Discussion
The widespread epidemic and high recurrence rate of periodontitis not only impact numerous patients but also impose a substantial burden on the social economy and public health system. Current periodontal therapies, which often involve mechanical trauma and antibiotic-based drug therapy, face challenges, such as drug resistance, leading to weakened efficacy.17 In addition, long-term inflammation-induced tissue damage affects aesthetics and results in bad breath, poor implant stability, and poor prosthesis retention.18 The primary objective of periodontitis treatment is to restore damaged periodontal support tissues. Hence, developing a rapid and effective strategy to alleviate inflammation and promote periodontal tissue repair is crucial for effective management of periodontitis.
“Huang Di Nei Jing” mentions that “the foundation of health lies in nourishing oneself through food”. The body can obtain anti-inflammatory and antioxidant substances from the diet, such as polyphenols and flavonoids, which cannot be produce on its own.19 Although medicinal foods cannot replace drugs, they can help regulate body functions and support human health. Numerous clinical studies have demonstrated that healthy food consumption and dietary habits can assist in periodontitis treatment. Ginger, a plant rich in complex bioactive compounds, contains the majority of compounds (such as gingerol and terpene) identified through mass spectrometry.20 These compounds endow ginger with medicinal properties, making it a valuable choice for disease prevention and a balanced diet. However, some pharmacological compounds, such as 10-gingerol and 6-gingerol, are thermally unstable, 95% stuck to the membrane, and are unable to enter the central nervous system through passive diffusion.21 Exosomes are vesicles with phospholipid bilayer membranes that traverse biological barriers and serve as carriers of information exchange.22 Unlike mammalian exosomes, plant exosomes do not require a tightly controlled culture environment and can be produced on a large scale at lower costs and with higher yields.23 According to our testing, the particle size of GELNs did not change significantly under the condition of PH=2, indicating good stability. However, owing to the vast diversity of plants and the intricacies of their tissues, research on the composition and biogenetic mechanisms of plant exosomes is still immature. In this study, for the first time, we utilized a widely targeted metabolomic approach to analyze the chemical compounds of GELNs and identified the presence of antioxidant compounds, such as flavonoids and phenolic acids, in the vesicles. Furthermore, lipid spectrum analysis revealed that the GELNs predominantly consisted of phosphatidic acid, sphingolipids, and digalactosyldiacylglycerol. Phosphatidic acid is highly fusogenic and plays a crucial role in vesicle uptake process.24 These findings suggest that GELNs can transport pharmacologically active ingredients that can be internalized by cells to exert their effects. Moreover, the clinical applications of exosomes are advancing. Wang et al locally encapsulated an injectable hydrogel onto turmeric exosomes and delivered vesicles to the heart infarction in the form of a gel, prolonging the existence time of the drugs.25 In the future, combining plant exosomes with oral healthcare products such as mouthwashes and toothpastes could prove to be an effective strategy for enhancing oral health protection.
In rat ligature-induced periodontitis models, GELNs effectively alleviated gum swelling and reduced the depth of the periodontal pockets. Histological analysis revealed that GELNs outperformed ginger juice in enhancing the proliferation of periodontal collagen fibers, decreasing inflammatory cell counts, and reducing alveolar bone absorption. In vitro experiments, PDLFs, which are the primary cells of the periodontal membrane, play a crucial role in maintaining periodontal tissue regeneration and repair by producing and breaking down extracellular matrix components.14 Excessive ROS levels in periodontitis not only cause dysfunction of neutrophils and macrophage inflammatory polarization, also can hinder the regenerative capacity of PDLFs, leading to reduced tissue repair ability and delayed healing of periodontal defects.26 Recent research suggests that cells can enhance their oxidative defense by consuming antioxidants, thereby preventing or delaying cell damage caused by free radicals. Cavalla et al demonstrated that ROS can boost the activity of gelatin-soluble matrix metalloproteinases and trigger the release of proinflammatory cytokines from PDLFs, exacerbating periodontal tissue damage. In addition, elevated ROS levels can induce mitochondrial dysfunction, ultimately resulting in PDLF apoptosis.27 The antioxidant properties of ginger have been proven. While, at present, there is no report on GELNs antioxidant. Therefore, the discovery that GELNs can regulate oxidative stress to improve periodontitis is also one of the innovation points of this article. We revealed that PDLFs treated with lipopolysaccharide (LPS) inhibited proliferation and migration. The effect of ginger juice on PDLF function was similar to that of the control group, maintaining the original migratory ability of PDLFs without promoting it. Following GELNs intervention in PDLFs, cell proliferation and migration were significantly enhanced, laying the foundation for tissue regeneration and repair.
The pharmacological activity is crucial for the application of GELNs. Our data indicate that GELNs demonstrate antioxidant effects both in vivo and in vitro. Exogenous and endogenous ROS levels were simulated using lipopolysaccharide (LPS) and H2O2. DCFH-DA revealed that groups treated with H2O2 and LPS exhibited the highest green fluorescence intensity. Following intervention with GELNs, there was a significant reduction in intracellular green fluorescence intensity. Antioxidant enzymes such as CAT, MDA, and T-AOC play a role in protecting against the toxic effects of ROS under normal physiological conditions. Our study demonstrated that GELNs can elevate the levels of T-AOC and CAT, which are typically underexpressed in inflammatory environments, while decreasing the level of MDA. ROS act as a double-edged sword, participating in cell signaling at normal levels but causing OS and direct damage to cells and tissues when present in excess.28 Previous research has shown that GELNs can induce the expression of the antioxidant gene heme oxygenase-1 (HO-1) and the anti-inflammatory cytokine IL-10 in macrophages, thereby protecting mice from colitis induced by sodium glucan sulfate.26 Our findings align with existing evidence supporting the strong antioxidant properties of GELNs and their excellent stability in harsh environments. The NF-κB pathway responds to cytokines, free radicals, and other stimuli and plays a central role in inflammation, immune response, and OS.29 ROS can activate the NF-κB pathway and exacerbate inflammatory responses. The literature indicates that nuclear translocation of p-p65 is activated in a periodontitis environment, leading to increased expression of inflammatory factors such as IL-1β and TNF-α, suggesting a link between NF-κB signaling pathway activation and persistent inflammation in periodontal tissue.30 In the present study, p-p65 exhibited nuclear translocation in response to an LPS-induced inflammatory environment. Some cells in the ginger juice group showed this phenomenon. However, in the GELNs group, the nuclear translocation of p-p65 was notably reduced, and the expression of NF-κB was also decreased, as confirmed by immunohistochemistry. These results suggest that GELNs effectively suppressed the activation of the NF-κB signaling pathway in the periodontal tissues of rats with periodontitis, ultimately mitigating ROS.
Although we utilized a widely targeted metabolome to analyze the components and enrichment pathways of GELNs in this study, its physiological purpose remains largely unknown. Moving forward, we plan to validate the target components individually and engineer vesicles to gain insight into the antioxidant properties of GELNs. Furthermore, we chose ginger juice as the control group by maintaining a consistent total protein concentration and filtering it through a 0.22 micron membrane prior to testing to ensure sterility. However, ginger juice contains a variety of bioactive and inactive components, which pose a challenge in determining the appropriate dosage. Future research should focus on identifying properly purified controls and conducting precise dose analysis. Periodontitis is a chronic inflammatory condition associated with the pathogenesis of an ROS environment. Studies have shown that patients with chronic periodontitis exhibit significantly higher M1-M2 ratios in their gingival tissues along with elevated neutrophil counts that trigger the production of TNF-α and IL-8. Therefore, in subsequent studies, we will further investigate the impact of GELNs on immune responses, regulation of macrophage polarization, and modulation of inflammatory factors.
Conclusion
In summary, GELNs exhibit superior stability, transmembrane ability, non-toxicity, and odorlessness. Furthermore, GELNs demonstrated enhanced therapeutic efficacy in treating periodontitis compared with ginger juice, effectively stimulating the regeneration and repair of periodontal tissue. In vitro experiments revealed that GELNs can promote the proliferation and migration of PDLFs and exert antioxidant effects by inhibiting the NF-κB signaling pathway, thus efficiently eliminating ROS. This study introduces a novel approach for managing periodontitis by modulating the OS within the periodontal environment.
Funding Statement
This work was supported by the National Natural Science Foundation of China (82071155, 82271023, 82301052), Basic Research Program of Shanxi Province (Distinguished Young Scholars)(202203021223006), Traditional Chinese Medicine Administration Research of Shanxi (2024ZYYC073), Graduate Education Innovation Project of Shanxi Province (2023SJ139), Health Commission of Shanxi Province (No. 2022XM14), and the Natural Science Foundation of Shanxi Province (202203021222266, 202203021212368, 202303021212132, 202303021212131, 202403021212211).
Abbreviations
CAT, catalase; DCFH-DA, 2’,7’-Dichlorofluorescin diacetate; EDTA, ethylenediaminetetraacetic acid; GELNs, ginger exosome-like nanoparticles; HO-1, heme oxygenase-1; MDA, malondialdehyde; NTA, nanoparticle tracking analysis; OS, oxidative stress; PDLFs, periodontal ligament fibroblasts; ROS, reactive oxygen species; T-AOC, total antioxidant capacity; TEM, transmission electron microscope; TRAP, tartrate-resistant acid phosphatase.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
- 1.Wang Y, Ni B, Xiao Y, Lin Y, Zhang Y. A novel nomogram for predicting risk of hypertension in US adults with periodontitis: national health and nutrition examination survey (NHANES) 2009-2014. Medicine. 2023;102(51):e36659. doi: 10.1097/MD.0000000000036659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanz M, Herrera D, Kebschull M, et al. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47 Suppl 22(Suppl 22):4–60. doi: 10.1111/jcpe.13290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huck O, Stutz C, Gegout PY, et al. Nanomedicine and periodontal regenerative treatment. Dent Clin North Am. 2022;66(1):131–155. doi: 10.1016/j.cden.2021.06.005 [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Wang T, Tu Y, et al. ROS-scavenging biomaterials for periodontitis. J Mater Chem B. 2023;11(3):482–499. doi: 10.1039/D2TB02319A [DOI] [PubMed] [Google Scholar]
- 5.Khbrani AH, Al-Shahrani AA, Alzahrani HG, et al. Role and common types of herbal medicine used for oral health in the Middle-East. Int J Community Med Public Health. 2022;10(1):402. doi: 10.18203/2394-6040.ijcmph20223322 [DOI] [Google Scholar]
- 6.Crichton M, Davidson AR, Innerarity C, et al. Orally consumed ginger and human health: an umbrella review. Am J Clin Nutr. 2022;115(6):1511–1527. doi: 10.1093/ajcn/nqac035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ballester P, Cerdá B, Arcusa R, Marhuenda J, Yamedjeu K, Zafrilla P. Effect of ginger on inflammatory diseases. Mol. 2022;27(21):7223 doi: 10.3390/molecules27217223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zare Javid A, Bazyar H, Gholinezhad H, et al. The effects of ginger supplementation on inflammatory, antioxidant, and periodontal parameters in type 2 diabetes mellitus patients with chronic periodontitis under non-surgical periodontal therapy. A double-blind, placebo-controlled trial. Diabetes, Metab Syndr Obes Targets Ther. 2019;12:1751–1761. doi: 10.2147/DMSO.S214333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu J, Lu Y, Liu J, Jin C, Meng Y, Pei D. Influence of epigallocatechin-3-gallate in promoting proliferation and osteogenic differentiation of human periodontal ligament cells. BMC Oral Health. 2019;19(1):73 doi: 10.1186/s12903-019-0768-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mukkavilli R, Yang C, Singh Tanwar R, Ghareeb A, Luthra L, Absorption AR. Absorption, Metabolic stability, and pharmacokinetics of ginger phytochemicals. Mol. 2017;22(4):553 doi: 10.3390/molecules22040553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali BH, Blunden G, Tanira MO, Nemmar A. Some phytochemical, pharmacological and toxicological properties of ginger (Zingiber officinale Roscoe): a review of recent research. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc. 2008;46(2):409–420. doi: 10.1016/j.fct.2007.09.085 [DOI] [PubMed] [Google Scholar]
- 12.Zhu H, He W. Ginger: a representative material of herb-derived exosome-like nanoparticles. Front Nutr. 2023;10:1223349. doi: 10.3389/fnut.2023.1223349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mao Y, Han M, Chen C, et al. A biomimetic nanocomposite made of a ginger-derived exosome and an inorganic framework for high-performance delivery of oral antibodies. Nanoscale. 2021;13(47):20157–20169. doi: 10.1039/D1NR06015E [DOI] [PubMed] [Google Scholar]
- 14.Naruishi K. Biological roles of fibroblasts in periodontal diseases. Cells. 2022;11(21):3345. doi: 10.3390/cells11213345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Almoiliqy M, Wen J, Qaed E, et al. Protective effects of cinnamaldehyde against mesenteric ischemia-reperfusion-induced lung and liver injuries in rats. Oxid Med Cell Longev. 2020;2020:4196548. doi: 10.1155/2020/4196548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg MA, Gafurov MR, Murzakhanov FF, et al. Mesoporous iron(III)-doped hydroxyapatite nanopowders obtained via iron oxalate. Nanomater Basel Switz. 2021;11(3):811. doi: 10.3390/nano11030811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Darby I. Risk factors for periodontitis & peri-implantitis. Periodontol 2000. 2022;90(1):9–12. doi: 10.1111/prd.12447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nibali L, Gkranias N, Mainas G, Di Pino A. Periodontitis and implant complications in diabetes. Periodontol 2000. 2022;90(1):88–105. doi: 10.1111/prd.12451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qu S, Yu S, Ma X, Wang R. “Medicine food homology” plants promote periodontal health: antimicrobial, anti-inflammatory, and inhibition of bone resorption. Front Nutr. 2023;10:1193289. doi: 10.3389/fnut.2023.1193289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahomoodally MF, Aumeeruddy MZ, Rengasamy KRR, et al. Ginger and its active compounds in cancer therapy: from folk uses to nano-therapeutic applications. Semin Cancer Biol. 2021;69:140–149. doi: 10.1016/j.semcancer.2019.08.009 [DOI] [PubMed] [Google Scholar]
- 21.Bekkouch O, Dalli M, Harnafi M, et al. Ginger (Zingiber officinale Roscoe), lemon (Citrus limon L.) juices as preventive agents from chronic liver damage induced by CCl4: a biochemical and histological study. Antioxid Basel Switz. 2022;11(2):390. doi: 10.3390/antiox11020390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rehman FU, Liu Y, Zheng M, Shi B. Exosomes based strategies for brain drug delivery. Biomaterials. 2023;293:121949. doi: 10.1016/j.biomaterials.2022.121949 [DOI] [PubMed] [Google Scholar]
- 23.Fang Z, Liu K. Plant-derived extracellular vesicles as oral drug delivery carriers. J Control Release. 2022;350:389–400. doi: 10.1016/j.jconrel.2022.08.046 [DOI] [PubMed] [Google Scholar]
- 24.Zhang M, Viennois E, Prasad M, et al. Edible ginger-derived nanoparticles: a novel therapeutic approach for the prevention and treatment of inflammatory bowel disease and colitis-associated cancer. Biomaterials. 2016;101:321–340. doi: 10.1016/j.biomaterials.2016.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu K, Wang Y, Yang H, et al. Injectable decellularized extracellular matrix hydrogel containing stromal cell-derived factor 1 promotes transplanted cardiomyocyte engraftment and functional regeneration after myocardial infarction. ACS Appl Mater Interfaces. 2023;15(2):2578–2589. doi: 10.1021/acsami.2c16682 [DOI] [PubMed] [Google Scholar]
- 26.Zhang YL, An Y, Sun LJ, et al. NADPH-dependent ROS accumulation contributes to the impaired osteogenic differentiation of periodontal ligament stem cells under high glucose conditions. Front Endocrinol. 2023;14:1152845. doi: 10.3389/fendo.2023.1152845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cavalla F, Osorio C, Paredes R, et al. Matrix metalloproteinases regulate extracellular levels of SDF-1/CXCL12, IL-6 and VEGF in hydrogen peroxide-stimulated human periodontal ligament fibroblasts. Cytokine. 2015;73(1):114–121. doi: 10.1016/j.cyto.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 28.Yu Y, Zhao S, Gu D, et al. Cerium oxide nanozyme attenuates periodontal bone destruction by inhibiting the ROS-NFκB pathway. Nanoscale. 2022;14(7):2628–2637. doi: 10.1039/D1NR06043K [DOI] [PubMed] [Google Scholar]
- 29.Wibisana JN, Okada M. Encoding and decoding NF-κB nuclear dynamics. Curr Opin Cell Biol. 2022;77:102103. doi: 10.1016/j.ceb.2022.102103 [DOI] [PubMed] [Google Scholar]
- 30.Fu J, Ni C, Ni HD, et al. Spinal Nrf2 translocation may inhibit neuronal NF-κB activation and alleviate allodynia in a rat model of bone cancer pain. J Neurochem. 2021;158(5):1110–1130. doi: 10.1111/jnc.15468 [DOI] [PMC free article] [PubMed] [Google Scholar]