Abstract
Background
Person-centered approaches to measuring severity of multimorbidity (≥ 2 chronic conditions) can help clinicians assess the individual experience of multimorbidity and inform effective caregiving and intervention strategies. We examine how limitations in everyday activities attributable to specific chronic conditions act independently and in tandem to influence individual perceptions of multimorbidity severity.
Methods
Data from the Panel Study of Income Dynamics (2005–2021) were used to investigate self-reported limitations in normal daily activities resulting from nine chronic conditions (hypertension, arthritis, diabetes, heart condition [heart disease/heart attack], cancer, lung disease, stroke, depression, and memory loss) in 4 318 adults aged 55–95 (18 878 person-wave observations). We used descriptive and inferential analyses to estimate limitations resulting from specific conditions, limitations attributable to condition combinations, and the contribution of comorbid conditions to condition-specific and overall severity. Follow-up analyses addressed mortality selection using inverse probability weighting and examined cancer type and cancer status/treatment modality among respondents reporting cancer diagnosis.
Results
Of the more prevalent conditions, arthritis was associated with the most severe limitations to normal activities. Memory loss was the least frequent condition reported but resulted in the most severe limitations, and as a comorbid condition, increased limitations reported for most conditions. Inverse probability weighting adjusted models revealed heterogeneity in estimates for some conditions including cancer and cancer survivors tended to report less lethal cancers that were cured or in remission.
Conclusions
Our results suggest that efforts to prevent and treat arthritis and support cognitive function may reduce the severity of multimorbidity experienced by the individual.
Keywords: Multiple chronic conditions, Multiple long-term conditions, Person-centered
Multimorbidity (≥2 coexisting chronic conditions), also referred to as multiple chronic conditions or multiple long-term conditions (1,2), affects the majority of older adults (3,4) and is increasing among generations just entering older adulthood (5). In addition to the substantial monetary costs of multimorbidity levied on individuals and health systems, multimorbidity represents a significant burden to individuals experiencing multiple symptomatic diseases and often requires navigating complex and fragmentary systems of care (6,7). Condition severity is a critical component of the experience and treatment of multimorbidity as the severity of individual conditions may modify the onset, prognosis, and/or severity of concurrent diseases, present barriers to effective treatment (eg, due to adverse effects of polypharmacy), and influence the risk of distal outcomes such as disablement and mortality (8). Examining the severity of chronic conditions, both as distinct conditions and collectively, is key to understanding multimorbidity progression in aging populations (9), and shifting focus from treating single chronic conditions to treating the whole individual affected by multiple conditions supports person-centered treatment approaches essential to managing multimorbidity (2).
Existing approaches to measuring multimorbidity severity take several forms, reflecting different research goals, available data sources, and the complexity of quantifying the individual experience of living with multimorbidity. Assessing global condition burden in the presence of multiple conditions is complicated by the interrelated pathology, treatment, and prognosis of concurrent conditions (8). To address the complexity of measuring severity of several conditions, some studies examine indirect outcomes that reflect the systemic dysregulation of health resulting from multimorbidity. For example, indicators of healthcare utilization have been used as markers of disease severity (10), and others have weighted chronic conditions by national average hospitalization costs (11). A similar approach used to estimate payments for Medicare beneficiaries is the Chronic Illness and Disability Payment System, which ranks clinical severity and expected future costs of illness across body systems and chronic diseases, which are then used to create payment weights (12). Utilization and cost-based measures of multimorbidity severity are valuable from a policy and health management perspective, but these measures obscure the individual experience of living with multimorbidity.
Multimorbidity studies that examine severity at the individual level have used additive scales of symptoms associated with various chronic conditions (eg, Comorbidity Symptom Scale [CSS]) (13) or indices that weight chronic conditions by their impact on physical functioning (the Multimorbidity-Weighted Index [MWI]) (14,15). The CSS measures the severity of 22 conditions and includes a catch-all for other conditions not mentioned, though the CSS includes items that are not representative of the severity of specific chronic conditions (eg, physical mobility, severity of side effects from medications). Similar scales including the Cumulative Illness Rating Scale (16) measure severity of illness related to organ-specific condition categories and require administration by trained clinicians. The MWI is a multimorbidity-specific index that weights chronic conditions based on their association with limitations in physical activities using the Short Form Physical Functioning Scale (SF-36 PF). While operationalizing multimorbidity severity by accounting for the impact of multimorbidity on physical function, the MWI overlooks the impact of multimorbidity on a range of other limitations resulting from comorbid chronic conditions (eg, emotional, social, and sexual).
The physical functioning measures included in the SF-36 PF are a subset of measures from the larger SF-36 that assess overall health-related quality of life (HRQoL) (17). The use of HRQoL as a person-centered indicator of condition severity aligns with the recognition that the single disease paradigm in clinical research and treatment poorly reflects the complexity and difficulty of managing multimorbidity for the individual (2,18,19). Focusing assessment and treatment on the person’s perception of how chronic conditions impede their everyday life shifts emphasis from a priori clinical prognoses to the self-perceived burden of experiencing and managing multimorbidity (20). Extensive research documents the association between multimorbidity and HRQoL using various HRQoL indices (21–23) that usually take the form of validated scales such as the SF-36, some shortened version of the SF-36 (eg, SF-12) (24,25), or another index (21,26). Limitations of these types of scales that prevent more widespread use in large population-based studies include length, emphasis on only the most severe health outcomes, and exclusion of specific chronic conditions (27).
Due to the substantive and practical limitations of existing approaches to measure the perceived severity of multimorbidity, analysis of previously unexamined indicators of chronic condition severity may improve understanding of how chronic conditions, both separately and in tandem, affect the lives of older adults. The Panel Study of Income Dynamics (PSID) is the world’s longest-running household panel survey and collects self-reported information on doctor-diagnosed chronic conditions and the perceived limitations to normal daily activities resulting from each condition, providing a valuable tool to assess the perceived severity of chronic conditions, both as condition-specific limitations and as overall limitations experienced by each respondent based on their specific constellation of chronic conditions. As we are unaware of existing research that leverages condition-specific limitation measures to examine multimorbidity burden, our goal is to contribute a patient-centered analysis of multimorbidity severity as measured by condition-specific limitations to normal daily activities. To this end, we apply descriptive and inferential analyses to (a) quantify perceived limitations resulting from specific chronic conditions, (b) identify the most common and severe condition combinations, (c) estimate the contribution of comorbid conditions to perceived severity of each condition, and (d) examine overall limitations resulting from multimorbidity. We also assess the robustness of our inferential estimates to the potentially biasing effect of mortality selection and examine how cancer type and cancer status and treatment modality may have influenced our primary findings.
Method
Data Source
Observations were drawn from the PSID, a nationally representative longitudinal study of U.S. households beginning in 1968 (28,29). To maintain consistency in question content, our study included biennial observations taken from the 2005–2021 PSID survey waves. The primary population of interest was adults aged 55–95 years of age who reported at least one chronic condition and also reported on the limitations to daily activities caused by that condition (n = 26 062 person-wave observations provided by 6 242 unique respondents). Person-wave observations with missing information on race/ethnicity (n = 118), region of residence (n = 213), or nonpositive individual sampling weights (n = 6 853) were removed, resulting in a final sample of 18 878 person-wave observations attributable to 4 318 unique respondents. Individual sampling weights taken from each respondent’s first eligible observation were used to adjust analyses for the complex sampling design of the PSID.
Measures
Chronic conditions selected for analysis adhere to prevailing definitions of chronic conditions as being prolonged (ie, ≥1 year), requiring consistent medical intervention, and/or limiting daily activities (30,31). In the PSID, respondents are asked if they had ever been told by a doctor whether they had each of the following conditions: hypertension, arthritis, diabetes, heart condition (heart disease/heart attack), cancer, lung disease, stroke, any emotional/nervous/psychiatric problem, or memory loss. To identify those reporting a diagnosis of depression, respondents confirming they had been diagnosed with a psychiatric problem were then asked about their specific diagnoses, using three follow-up questions. Respondents were then asked how much all of their psychiatric conditions limited their normal daily activities. When calculating limitations attributable to depression, we only considered responses where depression was one of the three reported psychiatric conditions, so depression-related limitations may in part reflect comorbid psychiatric conditions (eg, anxiety or bipolar disorder).
After reporting a doctor-diagnosed condition, respondents were then asked a follow-up question about the limitations to daily activities resulting from the specific condition (“How much does this (condition/problem) limit your normal daily activities?”; 0—not at all, 1—just a little, 2—somewhat, 3—a lot). Respondents were not asked additional follow-up questions regarding the type of limitations (eg, physical or mental/operational), resulting in a broad conceptualization of condition-specific limitations as defined by the respondent.
Covariates
Covariates were selected to adjust models for lifecourse social determinants of health, relevant health behaviors, and characteristics of the PSID survey design. Sociodemographic characteristics used to adjust inferential models included sex (male, female), race/ethnicity (White, Black, Latino/a/x, and Other race/ethnicity), marital/partnership status (not married/partnered, married/partnered), education (less than high school, high school graduate, some college, college degree or more), family income (quartiles), family wealth (quartiles), region of residence (South, Northeast, North Central, West), and mother’s education (less than high school, high school graduate, some college, college degree or more). Health behaviors included heavy physical activity (none, 1–3 times per week, >3 times per week), body mass index (BMI; underweight [<18.5 kg/m2], normal weight [18.5–24.9 kg/m2], overweight [25–29.9 kg/m2], or obese [≥ 30 kg/m2]), current smoker (no, yes), and alcohol consumption (no, yes). Due to the survey design of the PSID where a primary respondent is asked to report for their partners, proxy response (no, yes) was included as a covariate. Covariates with missing data (ie, BMI, heavy physical activity, mother’s education, smoking status, alcohol use) were imputed using random forest nonparametric missing value imputation through the R package missForest (32). Supplementary Table 1 presents unimputed descriptive statistics for these variables.
Analytic Methods
Our analytic objectives included (a) examining distributions of limitations reported for each chronic condition separately, (b) examining the average reported limitations for the most common and pernicious multimorbidity combinations, (c) examining how comorbid conditions were associated with the limitations reported for each separate condition, and (d) estimating the association between each condition reported and the overall magnitude of severity across all conditions reported. Weighted univariate descriptive statistics are provided for each respondent’s first eligible observation (ie, ≥1 condition with nonmissing limitation information) and for the complete repeated measures sample. Using each respondent’s first observation, we identified all possible multimorbidity combinations, and then calculated the weighted mean limitation across all reported conditions for those combinations with ≥30 observations.
Inferential analyses were used to address the remaining objectives. To examine how comorbid chronic conditions were associated with the perceived limitations reported for each condition, limitations reported for each condition (referred to here as an index condition) were regressed on all possible comorbid chronic conditions and all covariates in separate multilevel models using distinct samples restricted to those observations reporting the index condition. These models included a random intercept to adjust for repeated observations nested within individuals. For these condition-specific models, the right-skewed integer distribution of condition-specific limitations was modeled using a Poisson distributional assumption.
When examining overall limitations resulting from all reported chronic conditions, we first calculated the average of all reported condition-specific limitations for each person-wave observation. Because we found that a substantial proportion of respondents reported no perceived limitation across all reported conditions, we fit a zero-inflated multilevel model including random intercepts with a logit-link to estimate the likelihood of reporting no limitations (0 = limitation, 1 = no limitation) and a gamma distribution to model nonzero responses while accounting for a nondiscrete continuous right-skewed distribution. To aid interpretability, gamma coefficients were exponentiated, resulting in multiplicative terms. Models were adjusted for individual sampling weights from the first observation with ≥1 reported chronic condition. To reduce the likelihood of Type 1 error when interpreting p values, we only interpreted effects from predictive models with p values <.001.
Sensitivity analyses were used to examine the role of mortality selection on statistical estimates and explore reported cancer type and cancer status and treatment modality among those reporting a cancer diagnosis. We applied inverse probability weighting (IPW) to adjust inferential models for potential bias due to mortality selection (33). Year of death was used to identify those experiencing mortality over the observational period, then the likelihood of not experiencing mortality was estimated in a covariate-adjusted logit model. Predicted individual probabilities were then used to calculate the IPW. The selection and operationalization of variables used as covariates in this model and implementation of the IPW-adjusted analyses (including trimming and weighting procedures) are described in the Supplementary Material.
To probe our primary findings related to cancer severity, we examined descriptive statistics on reported cancer type and cancer status and treatment modality at first report of cancer diagnosis. Respondents could report one of the following cancer types: breast, cervical, colon, lung, lymphoma or leukemia, melanoma, ovarian, prostate, skin (nonmelanoma or unknown), or other. Respondents reporting a cancer diagnosis were then asked whether they were currently in treatment, if the cancer was in remission, or if the cancer was cured. For survey years 2013–2021, respondents not receiving treatment were also identified.
Results
Descriptive Results
Table 1 presents weighted descriptive statistics for each respondent’s first eligible observation and all person-wave observations. Mean age at first observation was 63.21 years (SD = 9.42), 54.83% of the sample was female, 64.51% reported being married/partnered, and racial/ethnic distribution was as follows: 74.88% White, 11.54% Black, 8.24% Latino/a/x, 5.34% other race/ethnicity. We refer the reader to Table 1 for descriptive statistics on other covariates.
Table 1.
Weighted Descriptive Statistics for Sample Postimputation, First Observation With ≥1 Chronic Condition and All Observations With ≥1 Chronic Condition, PSID 2005–2021
| First Observation With ≥1 Chronic Condition (n = 4 318) | All Observations With ≥1 Chronic Condition (n = 18 878) | |||||
|---|---|---|---|---|---|---|
| n | Mean/% | SD | n | Mean/% | SD | |
| Age | 4318 | 63.21 | 9.42 | 18 878 | 67.95 | 9.45 |
| Sex | 4318 | 18 878 | ||||
| Male | 1833 | 45.17% | 7 905 | 44.43% | ||
| Female | 2485 | 54.83% | 10 973 | 55.57% | ||
| Married/partnered | 4318 | 18 878 | ||||
| No | 1763 | 35.49% | 8 244 | 38.76% | ||
| Yes | 2555 | 64.51% | 10 634 | 61.24% | ||
| Race/ethnicity | 4318 | 18 878 | ||||
| White | 2438 | 74.88% | 11 220 | 76.67% | ||
| Black | 1267 | 11.54% | 5 213 | 11.10% | ||
| Latino/a/x | 371 | 8.24% | 1 431 | 7.16% | ||
| Other race/ethnicity | 242 | 5.34% | 1 014 | 5.07% | ||
| Education | 4318 | 18 878 | ||||
| Less than high school | 795 | 14.11% | 3 145 | 12.50% | ||
| High school graduate | 1546 | 35.45% | 6 661 | 34.95% | ||
| Some college | 902 | 21.29% | 4 014 | 21.86% | ||
| College degree or more | 1075 | 29.15% | 5 058 | 30.69% | ||
| Family income quartile | 4318 | 18 878 | ||||
| 1 ($−84 022 to $22 068)* | 1097 | 20.28% | 4 720 | 19.73% | ||
| 2 ($22 078–$44 450)* | 1040 | 22.42% | 4 720 | 23.65% | ||
| 3 ($44 451–$82 200)* | 1071 | 26.04% | 4 719 | 26.72% | ||
| 4 ($82 200–$3 219 550)* | 1110 | 31.25% | 4 719 | 29.89% | ||
| Family wealth quartile | 4318 | 18 878 | ||||
| 1 ($−2 699 990 to $21 500)* | 1221 | 21.22% | 4 720 | 18.84% | ||
| 2 ($21 500–$142 100)* | 1104 | 23.36% | 4 720 | 22.37% | ||
| 3 ($142 200–$457 000)* | 1096 | 28.57% | 4 719 | 27.59% | ||
| 4 ($457 000–$100 555 000)* | 897 | 26.84% | 4 719 | 31.19% | ||
| Vigorous physical activity | 4318 | 18 878 | ||||
| None | 2353 | 51.35% | 10 582 | 53.76% | ||
| 1–3 times per week | 1210 | 29.68% | 5 129 | 28.22% | ||
| >3 times per week | 755 | 18.97% | 3 167 | 18.02% | ||
| BMI | 4318 | 18 878 | ||||
| Underweight (<18.5 kg/m2) | 61 | 1.41% | 326 | 1.65% | ||
| Normal (18.5–24.9 kg/m2) | 1136 | 28.33% | 4 794 | 27.48% | ||
| Overweight (25–29.9 kg/m2) | 1667 | 40.12% | 7 168 | 38.79% | ||
| Obese (≥30 kg/m2) | 1454 | 30.15% | 6 590 | 32.08% | ||
| Mother’s education | 4318 | 18 878 | ||||
| Less than high school degree | 2243 | 44.64% | 9 759 | 44.35% | ||
| HS degree | 1332 | 34.54% | 5 854 | 35.01% | ||
| Greater than high school degree | 743 | 20.82% | 3 265 | 20.64% | ||
| Current smoker | 4318 | 18 878 | ||||
| No | 3661 | 86.34% | 16 615 | 88.76% | ||
| Yes | 657 | 13.66% | 2 263 | 11.24% | ||
| Drink alcohol | 4318 | 18 878 | ||||
| No | 2176 | 45.41% | 9 785 | 47.48% | ||
| Yes | 2142 | 54.59% | 9 093 | 52.52% | ||
| Region | 4318 | 18 878 | ||||
| South | 670 | 19.66% | 2 804 | 18.72% | ||
| Northeast | 1019 | 25.50% | 4 568 | 26.24% | ||
| North Central | 1853 | 34.68% | 8 139 | 35.13% | ||
| West | 776 | 20.16% | 3 367 | 19.91% | ||
| Proxy response | 4318 | 18 878 | ||||
| No | 3105 | 69.75% | 14 068 | 72.56% | ||
| Yes | 1213 | 30.25% | 4 810 | 27.44% | ||
| Year | 4318 | 1 723 | 9.20% | |||
| 2005 | 1723 | 40.08% | 1 801 | 9.66% | ||
| 2007 | 368 | 8.48% | 1 934 | 10.19% | ||
| 2009 | 318 | 6.60% | 2 066 | 10.99% | ||
| 2011 | 335 | 7.97% | 2 138 | 11.18% | ||
| 2013 | 310 | 6.57% | 2 192 | 11.48% | ||
| 2015 | 325 | 7.84% | 2 272 | 11.99% | ||
| 2017 | 306 | 7.07% | 2 388 | 12.63% | ||
| 2019 | 349 | 8.54% | 2 364 | 12.69% | ||
| 2021 | 284 | 6.85% | 1 832 | 12.50% | ||
Notes: BMI = body mass index; PSID = Panel Study of Income Dynamics.
*Minimum and maximum values within quartile, calculated for all observations. Descriptive statistics weighted by person-level weights taken at first eligible observation.
Table 2 presents weighted descriptive statistics for indicators of overall multimorbidity burden, prevalence of each chronic condition, mean limitations reported for all conditions, and condition-specific limitations to daily activities. At first eligible observation, the average number of chronic conditions at first observation was 1.84 (SD = 1.11), 49.13% experienced multimorbidity, and 21.91% (n = 1 028) reported 3 or more conditions. Considering prevalence of the five most common conditions at first observation, 58.69% (n = 2 744) of respondents reported hypertension, 43.97% reported arthritis (n = 1 885), 19.88% (n = 970) reported diabetes, 17.98% (n = 766) reported a heart condition, and 15.73% (n = 615) reported cancer. Lung disease (9.67%, n = 422), stroke (7.29%, n = 345), depression (6.62%, n = 250), and memory loss (4.50%, n = 203) were less common. Across all conditions reported, the mean limitation level at first observation was.73 (SD = 0.88), representing minimal limitations to daily activities attributable to chronic conditions.
Table 2.
Weighted Distributions of Condition-Specific Limitations, First Observation With Specific Condition and All Observations With Specific Condition, PSID 2005–2021
| Multimorbidity Indicators | First Observation With ≥1 Chronic Condition (n = 4 318) | All Observations With ≥1 Chronic Condition (n = 18 878) | ||||
|---|---|---|---|---|---|---|
| N | Mean/% | SD | n | Mean/% | SD | |
| Number of chronic conditions (mean) | 4 318 | 1.84 | 1.11 | 18 878 | 2.13 | 1.21 |
| Multimorbidity (≥ 2 conditions) | 4 318 | 49.13% | 18 878 | 61.88% | ||
| Number of chronic conditions (count) | 4 318 | 18 878 | ||||
| 1 | 2 106 | 50.87% | 6 897 | 38.12% | ||
| 2 | 1 184 | 27.23% | 5 749 | 30.54% | ||
| 3 | 608 | 13.17% | 3 621 | 18.33% | ||
| 4 | 254 | 5.35% | 1 603 | 7.96% | ||
| 5 | 119 | 2.41% | 701 | 3.55% | ||
| 6 | 39 | 0.79% | 243 | 1.19% | ||
| 7 | 7 | 0.18% | 55 | 0.28% | ||
| 8 | 1 | 0.01% | 8 | 0.03% | ||
| 9 | 0 | 0.00% | 1 | 0.01% | ||
| Individual chronic conditions | ||||||
| Hypertension | 4 318 | 18 878 | ||||
| No | 1 574 | 41.31% | 5 429 | 33.03% | ||
| Yes | 2 744 | 58.69% | 13 449 | 66.97% | ||
| Arthritis | 4 318 | 18 878 | ||||
| No | 2 433 | 56.03% | 9 650 | 51.17% | ||
| Yes | 1 885 | 43.97% | 9 228 | 48.83% | ||
| Diabetes | 4 318 | 18 878 | ||||
| No | 3 348 | 80.12% | 13 715 | 75.42% | ||
| Yes | 970 | 19.88% | 5 163 | 24.58% | ||
| Heart condition | 4 318 | 18 878 | ||||
| No | 3 552 | 82.02% | 15 090 | 79.47% | ||
| Yes | 766 | 17.98% | 3 788 | 20.53% | ||
| Cancer | 4 318 | 18 878 | ||||
| No | 3 703 | 84.27% | 15 563 | 80.42% | ||
| Yes | 615 | 15.73% | 3 315 | 19.58% | ||
| Lung disease | 4 318 | 18 878 | ||||
| No | 3 896 | 90.33% | 16 735 | 88.29% | ||
| Yes | 422 | 9.67% | 2 143 | 11.71% | ||
| Stroke | 4 318 | 18 878 | ||||
| No | 3 973 | 92.71% | 16 996 | 90.70% | ||
| Yes | 345 | 7.29% | 1 882 | 9.30% | ||
| Depression | 4 318 | 18 878 | ||||
| No | 4 068 | 93.38% | 17 741 | 93.26% | ||
| Yes | 250 | 6.62% | 1 137 | 6.74% | ||
| Memory loss | 4 318 | 18 878 | ||||
| No | 4 115 | 95.50% | 17 892 | 95.09% | ||
| Yes | 203 | 4.50% | 986 | 4.91% | ||
| Mean limitations | ||||||
| Overall condition severity (range: 0–3) | 4 318 | 0.73 | 0.88 | 18 878 | 0.77 | 0.87 |
| Condition-specific limitations | ||||||
| Hypertension-related limitations | 2 744 | 13 449 | ||||
| Not at all | 1 900 | 73.89% | 9 113 | 71.74% | ||
| Just a little | 406 | 12.92% | 2 125 | 14.42% | ||
| Somewhat | 277 | 8.82% | 1 408 | 9.37% | ||
| A lot | 161 | 4.36% | 803 | 4.47% | ||
| Arthritis-related limitations | 1 885 | 9 228 | ||||
| Not at all | 445 | 25.93% | 1 959 | 22.79% | ||
| Just a little | 544 | 30.21% | 2 682 | 30.50% | ||
| Somewhat | 502 | 26.63% | 2 572 | 28.06% | ||
| A lot | 394 | 17.22% | 2 015 | 18.65% | ||
| Diabetes-related limitations | 970 | 5 163 | ||||
| Not at all | 531 | 59.02% | 2 695 | 55.45% | ||
| Just a little | 209 | 19.21% | 1 165 | 22.16% | ||
| Somewhat | 138 | 14.76% | 798 | 14.75% | ||
| A lot | 92 | 7.01% | 505 | 7.64% | ||
| Heart condition-related limitations | 766 | 3 788 | ||||
| Not at all | 336 | 47.04% | 1 484 | 42.78% | ||
| Just a little | 143 | 18.83% | 749 | 19.68% | ||
| Somewhat | 161 | 19.82% | 878 | 22.67% | ||
| A lot | 126 | 14.31% | 677 | 14.87% | ||
| Cancer-related limitations | 615 | 3 315 | ||||
| Not at all | 429 | 72.89% | 2 387 | 74.53% | ||
| Just a little | 58 | 9.42% | 334 | 10.07% | ||
| Somewhat | 73 | 10.42% | 305 | 8.38% | ||
| A lot | 55 | 7.27% | 289 | 7.02% | ||
| Lung disease-related limitations | 422 | 2 143 | ||||
| Not at all | 151 | 38.49% | 623 | 29.05% | ||
| Just a little | 99 | 21.74% | 490 | 22.69% | ||
| Somewhat | 83 | 18.24% | 531 | 25.52% | ||
| A lot | 89 | 21.53% | 499 | 22.73% | ||
| Stroke-related limitations | 345 | 1 882 | ||||
| Not at all | 126 | 40.92% | 778 | 47.24% | ||
| Just a little | 58 | 16.00% | 291 | 15.09% | ||
| Somewhat | 51 | 16.83% | 329 | 17.38% | ||
| A lot | 110 | 26.25% | 484 | 20.29% | ||
| Depression-related limitations | 253 | 1 148 | ||||
| Not at all | 81 | 34.41% | 378 | 34.80% | ||
| Just a little | 63 | 25.26% | 297 | 27.13% | ||
| Somewhat | 62 | 23.15% | 292 | 24.25% | ||
| A lot | 47 | 17.17% | 181 | 13.81% | ||
| Memory loss-related limitations | 203 | 986 | ||||
| Not at all | 15 | 8.35% | 88 | 9.48% | ||
| Just a little | 41 | 22.37% | 153 | 15.36% | ||
| Somewhat | 60 | 27.05% | 274 | 26.62% | ||
| A lot | 87 | 42.24% | 471 | 48.54% | ||
Notes: PSID = Panel Study of Income Dynamics.
Descriptive statistics weighted by person-level weights taken at first eligible observation.
Distributions of perceived limitations resulting from each condition are available in Table 2 and visualized in Figure 1. Focusing on the three most common conditions, 73.89% (n = 1 900) of those reporting hypertension and 59.02% (n = 531) of those reporting diabetes stated that these conditions did not limit their normal daily activities, though only 25.93% (n = 445) of those with arthritis reported no limitations. Only 13.18% (n = 438) of those with hypertension reported either “somewhat” or “a lot” of limitations attributable to hypertension, while 21.77% (n = 230) of those with diabetes and 43.85% (n = 896) of those with arthritis felt those conditions imposed more severe limitations. Though relatively less common, 39.77% (n = 172) of those with lung disease, 43.08% (n = 161) of those with stroke, 40.32% (n = 109) of those with depression, and 69.29% (n = 147) of those with memory loss reported either “somewhat” or “a lot” of limitation due to these conditions.
Figure 1.
Weighted percentages of condition-specific limitations at first observation reporting the chronic condition, PSID 2005–2021. Weighted by sampling weights taken at first observation. PSID = Panel Study of Income Dynamics.
To examine how unique combinations of chronic conditions were associated with limitations to daily activities, Table 3 presents the mean limitation scores for condition combinations with ≥30 respondents, calculated at participants’ first reported wave with a given combination. The five condition combinations with the greatest average limitations that met the criteria of having ≥30 responses at first eligible observation were: (a) hypertension + arthritis + diabetes + heart condition (n = 36, mean = 1.54, SD = 1.04), (b) hypertension + arthritis + stroke (n = 30, mean = 1.49, SD = 0.88), (c) arthritis + lung disease (n = 38, mean = 1.30, SD = 0.85), (d) hypertension + arthritis + lung disease (n = 44, mean = 1.21, SD = 0.67), and (e) hypertension + arthritis + heart condition (n = 80, mean = 1.10, SD = 0.76). The five most common condition combinations were hypertension + arthritis (n = 361), hypertension + diabetes (n = 202), hypertension + arthritis + diabetes (n = 135), hypertension + heart condition (n = 117), and hypertension + arthritis + heart condition (n = 80).
Table 3.
Weighted Mean of Limitations Reported for Chronic Condition Combinations With ≥30 Observations, PSID 2005–2021
| n | Mean | SD | |
|---|---|---|---|
| Hypertension + arthritis + diabetes + heart condition | 36 | 1.54 | 1.04 |
| Hypertension + arthritis + stroke | 30 | 1.49 | 0.88 |
| Arthritis + lung disease | 38 | 1.30 | 0.85 |
| Hypertension + arthritis + lung disease | 44 | 1.21 | 0.67 |
| Hypertension + arthritis + heart condition | 80 | 1.10 | 0.76 |
| Arthritis + heart condition | 41 | 0.99 | 0.75 |
| Arthritis + diabetes | 44 | 0.96 | 0.72 |
| Hypertension + arthritis + diabetes | 135 | 0.94 | 0.77 |
| Hypertension + arthritis | 361 | 0.87 | 0.77 |
| Hypertension + arthritis + cancer | 36 | 0.80 | 0.73 |
| Hypertension + diabetes + heart condition | 46 | 0.79 | 0.79 |
| Hypertension + stroke | 44 | 0.74 | 0.91 |
| Hypertension + lung disease | 35 | 0.64 | 0.72 |
| Arthritis + cancer | 52 | 0.61 | 0.61 |
| Hypertension + heart condition | 117 | 0.53 | 0.76 |
| Hypertension + diabetes | 202 | 0.40 | 0.69 |
| Hypertension + cancer | 78 | 0.25 | 0.45 |
Notes: PSID = Panel Study of Income Dynamics.
Mean limitation calculated at first observation with condition combination; weighted by sampling weights taken at first observation.
Condition-Specific Limitations Attributable to Comorbid Conditions
Table 4 presents results from the multilevel Poisson models regressing limitations reported for each index condition on all potential comorbid conditions and covariates. Figure 2 presents forest plots of the exponentiated coefficients of interest. We focus on the contribution of comorbid conditions to perceived limitations for each index condition, though Supplementary Table 2 provides statistical estimates for all variables included in each model.
Table 4.
Estimates From Multilevel Poisson Regression Predicting Limitations to Normal Daily Activities Reported for Each Chronic Condition by Comorbid Conditions, PSID 2005–2021
| Part 1* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Conditions | Hypertension Limitations | Arthritis Limitations | Diabetes Limitations | Heart Condition Limitations | Cancer Limitations | |||||
| IRR | CI | IRR | CI | IRR | CI | IRR | CI | IRR | CI | |
| Hypertension | 1.01 | 1.00–1.02 | 1.09 | 1.07–1.12*** | 1.02 | 1.00–1.05 | 0.97 | 0.93–1.00 | ||
| Arthritis | 1.21 | 1.19–1.23*** | 1.07 | 1.05–1.09*** | 1.11 | 1.09–1.13*** | 0.99 | 0.96–1.03 | ||
| Diabetes | 1.27 | 1.24–1.29*** | 1.07 | 1.05–1.09*** | 0.97 | 0.94–1.00 | 0.93 | 0.89–0.98 | ||
| Heart condition | 1.22 | 1.20–1.24*** | 1.06 | 1.05–1.07*** | 1.16 | 1.13–1.19*** | 1.08 | 1.03–1.12*** | ||
| Cancer | 1.03 | 1.01–1.06 | 1.01 | 1.00–1.02 | 1.05 | 1.02–1.08 | 0.96 | 0.94–0.98*** | ||
| Lung disease | 1.16 | 1.13–1.18*** | 1.05 | 1.04–1.06*** | 0.96 | 0.94–0.99 | 1.12 | 1.09–1.14*** | 0.87 | 0.84–0.90*** |
| Stroke | 1.17 | 1.15–1.20*** | 0.98 | 0.97–1.00 | 1.01 | 0.98–1.04 | 1.06 | 1.03–1.09*** | 1.04 | 0.99–1.09 |
| Depression | 0.97 | 0.95–0.99 | 1.09 | 1.07–1.11*** | 1.04 | 1.01–1.07 | 1.05 | 1.02–1.08*** | 0.91 | 0.86–0.96*** |
| Memory loss | 1.16 | 1.13–1.18*** | 1.07 | 1.05–1.09*** | 1.24 | 1.21–1.28*** | 1.25 | 1.22–1.28*** | 1.04 | 0.99–1.10 |
| Random effects | ||||||||||
| Intercept variance | 3.87 | 0.77 | 2.18 | 1.31 | 6.42 | |||||
| Residual variance | 13.90 | 2.01 | 9.18 | 5.49 | 33.30 | |||||
| ICC | 0.78 | 0.72 | 0.81 | 0.81 | 0.84 | |||||
| N | 3 304 | 2 695 | 1 459 | 1 275 | 1 124 | |||||
| Observations | 13 449 | 9 228 | 5 163 | 3 788 | 3 315 | |||||
| Conditional R2 | 0.79 | 0.73 | 0.82 | 0.82 | 0.86 | |||||
| Part 2* | ||||||||||
| Conditions | Lung disease limitations | Stroke limitations | Depression limitations | Memory loss limitations | ||||||
| IRR | CI | IRR | CI | IRR | CI | IRR | CI | |||
| Hypertension | 1.07 | 1.05–1.10*** | 1.05 | 1.01–1.09 | 0.97 | 0.92–1.01 | 1.14 | 1.09–1.18*** | ||
| Arthritis | 1.11 | 1.08–1.14*** | 1.06 | 1.03–1.09*** | 1.11 | 1.06–1.15*** | 0.97 | 0.94–1.00 | ||
| Diabetes | 0.95 | 0.92–0.99 | 1.33 | 1.27–1.39*** | 0.98 | 0.92–1.04 | 1.16 | 1.11–1.22*** | ||
| Heart condition | 1.06 | 1.03–1.08*** | 0.96 | 0.93–1.00 | 1.12 | 1.08–1.17*** | 1.10 | 1.06–1.15*** | ||
| Cancer | 1.08 | 1.05–1.11*** | 1.14 | 1.09–1.19*** | 0.97 | 0.92–1.02 | 0.97 | 0.92–1.02 | ||
| Lung disease | 1.08 | 1.04–1.11*** | 1.09 | 1.04–1.14*** | 0.99 | 0.95–1.04 | ||||
| Stroke | 1.00 | 0.97–1.03 | 0.99 | 0.93–1.05 | 1.07 | 1.02–1.11 | ||||
| Depression | 1.11 | 1.08–1.15*** | 0.96 | 0.92–1.00 | 1.12 | 1.08–1.17*** | ||||
| Memory loss | 1.04 | 1.01–1.08 | 1.45 | 1.41–1.50*** | 1.20 | 1.15–1.25*** | ||||
| Random effects | ||||||||||
| Intercept variance | 1.19 | 1.51 | 1.27 | 0.47 | ||||||
| Residual variance | 5.23 | 6.97 | 5.92 | 0.89 | ||||||
| ICC | 0.82 | 0.82 | 0.82 | 0.66 | ||||||
| N | 873 | 701 | 494 | 533 | ||||||
| Observations | 2 143 | 1 882 | 1 137 | 986 | ||||||
| Conditional R2 | 0.82 | 0.84 | 0.84 | 0.68 | ||||||
CI = confidence interval; ICC = intraclass correlation coefficient; IRR = incidence rate ratio; PSID = Panel Study of Income Dynamics.
* Part 1 presents estimates from models predicting limitations reported for hypertension, arthritis, diabetes, heart condition, and cancer. Part 2 presents estimates from models predicting limitations reported for lung disease, stroke, depression, and memory loss. Models adjusted for age, age squared, sex, race/ethnicity, education, household income, household wealth, region of residence, body mass index, mother’s education, smoking status, alcohol consumption, and proxy response; weighted by sampling weights taken at first observation.
*** p < .001.
Figure 2.
Forest plots of incidence rate ratios with 95% confidence intervals from weighted multilevel Poisson regression predicting limitations to daily activities for each index condition by comorbid conditions, PSID 2005–2021. Models adjusted for following covariates: age, age squared, sex, race/ethnicity, education, household income, household wealth, region of residence, body mass index, mother’s education, smoking status, alcohol consumption, and proxy response. Weighted by sampling weights taken at first observation. PSID = Panel Study of Income Dynamics.
The majority of reported comorbid conditions increased the likelihood of reporting a limitation related to each index condition. Concentrating on the comorbid conditions that demonstrated the strongest associations with reporting greater limitation for each index condition, diabetes and heart condition were the comorbid conditions that demonstrated the strongest associations with hypertension-related limitations. For example, reporting diabetes as a comorbid condition increased expected hypertension-related limitations by 27% (incidence rate ratio [IRR] = 1.27, CI = 1.24–1.29, p < .001), and reporting a heart condition increased expected hypertension-related limitations by 22% (IRR = 1.22, CI = 1.20–1.24, p < .001). Depression, memory loss, and diabetes appeared to contribute the most to limitations reported for arthritis, though the magnitude of estimates was similar for all significantly associated conditions. Notably, the contribution of comorbid diabetes to limitations reported for hypertension was substantially greater than the observed association between arthritis-specific limitations and comorbid diabetes (IRR = 1.07, CI = 1.05–1.09, p < .001).
Memory loss and heart condition were relatively strong predictors of diabetes-related limitations, and memory loss, lung disease, and arthritis demonstrated relatively strong associations with limitations reported for a heart condition. Interestingly, comorbid lung disease and depression reduced limitations reported due to cancer. Comorbid arthritis, depression, cancer, hypertension, and heart condition contributed to increasing limitations reported due to lung disease, and memory loss and diabetes were comparatively strong predictors of stroke-related limitations. Memory loss, heart condition, arthritis, and lung disease were positively associated with depression-related limitations, and diabetes, hypertension, depression, and heart condition increased the expected limitations resulting from memory loss.
Overall Severity of Condition-Specific Limitations
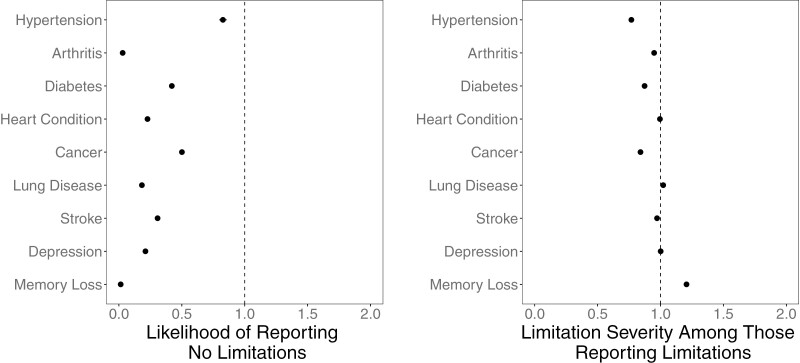
Estimates from the zero-inflated gamma models examining the contribution of each condition to the mean limitations reported for all conditions are reported in Table 5 and visualized as a forest plot in Figure 3. Supplementary Table 3 presents estimates for all variables included in the model. For the zero-inflated portion of the model, reporting any of the nine chronic conditions significantly reduced the likelihood of reporting zero limitations. Reporting memory loss reduced the likelihood of reporting no limitations by 98.56% (b = −4.24, exp(b) = 0.01, CI = 0.01–0.02, p < .001), and reporting arthritis reduced the likelihood of reporting no limitations by 96.98% (b = −3.50, exp(b) = 0.03, CI = 0.03–0.03, p < .001). Considering comorbid conditions that had the weakest association with likelihood of reporting any condition-related limitation, hypertension, cancer, and diabetes reduced the odds of reporting no disease-related limitations by 17.30%, 49.84%, and 58.10%, respectively.
Table 5.
Estimates From Multilevel Zero-Inflated Gamma Model Predicting Overall Limitations to Normal Daily Activities Attributable to Chronic Conditions, PSID 2005–2021
| Zero-Inflated Model | b | Overall Limitations | |
|---|---|---|---|
| Exp(b) | Exp(b) CI | ||
| Hypertension | −0.19 | 0.83 | 0.80–0.86*** |
| Arthritis | −3.50 | 0.03 | 0.03–0.03*** |
| Diabetes | −0.87 | 0.42 | 0.40–0.44*** |
| Heart condition | −1.48 | 0.23 | 0.22–0.24*** |
| Cancer | −0.69 | 0.50 | 0.48–0.52*** |
| Lung disease | −1.70 | 0.18 | 0.17–0.19*** |
| Stroke | −1.18 | 0.31 | 0.29–0.33*** |
| Depression | −1.56 | 0.21 | 0.20–0.23*** |
| Memory loss | −4.24 | 0.01 | 0.01–0.02*** |
| Gamma model | |||
| Hypertension | −0.26 | 0.77 | 0.76–0.77*** |
| Arthritis | −0.05 | 0.95 | 0.94–0.95*** |
| Diabetes | −0.14 | 0.87 | 0.87–0.88*** |
| Heart condition | 0.00 | 1.00 | 0.99–1.00 |
| Cancer | −0.17 | 0.84 | 0.84–0.85*** |
| Lung disease | 0.02 | 1.02 | 1.02–1.03*** |
| Stroke | −0.03 | 0.97 | 0.97–0.98*** |
| Depression | 0.00 | 1.00 | 0.99–1.01 |
| Memory loss | 0.19 | 1.21 | 1.20–1.21*** |
| Random effects | |||
| Intercept variance | 0.13 | ||
| Residual variance | 0.25 | ||
| ICC | 0.66 | ||
| N | 4 318 | ||
| Observations | 18 878 | ||
| Conditional R2 | 0.72 | ||
b = beta coefficient; CI = confidence interval; Exp(b) = exponentiated beta; ICC = intraclass correlation coefficient; PSID = Panel Study of Income Dynamics.
Results from generalized linear mixed models with logit model predicting zero limitations and gamma distribution for respondents reporting condition-related limitations, random intercepts; models adjusted for age, age squared, sex, race/ethnicity, education, household income, household wealth, region of residence, body mass index, mother’s education, smoking status, alcohol consumption, and proxy response; weighted by sampling weights taken at first observation; exponentiated coefficients from the zero-inflated model can be interpreted as follows: a one-unit change in predictor X is associated with 1 − exp(b)% increase/decrease in the likelihood of reporting no limitations; exponentiated gamma coefficients can be interpreted as follows: a one-unit change in predictor X is associated with an estimated percent increase/decrease in the count of outcome Y.
*** p < .001.
Figure 3.
Forest plots of exponentiated estimates from weighted multilevel zero-inflated model predicting likelihood of reporting no limitations and severity of limitations among those with limitations, PSID 2005–2021. Models adjusted for following covariates: age, age squared, sex, race/ethnicity, education, household income, household wealth, region of residence, body mass index, mother’s education, smoking status, alcohol consumption, and proxy response. Weighted by sampling weights taken at first observation. PSID = Panel Study of Income Dynamics.
For those reporting some limitations, memory loss and lung disease were the two conditions associated with greater–than-average limitations among those experiencing some limitations. Respondents diagnosed with memory loss had 20.92% greater expected limitations than those not reporting memory loss (b = 0.19, exp(b) = 1.21, CI = 1.20–1.21, p < .001), and expected limitations were 2.02% greater for those reporting lung disease (b = 0.02, exp(b) = 1.02, CI = 1.02–1.03, p < .001). Respondents experiencing limitations who reported hypertension, cancer, or diabetes had fewer expected limitations than average among those reporting some limitations. Those reporting arthritis or stroke also had fewer limitations, though the magnitude of these estimates was small.
Sensitivity Analyses
Follow-up analyses replicated our primary results using a trimmed sample adjusted for IPW. Supplementary Table 4 presents descriptive statistics for the trimmed sample adjusted for individual weights and IPW, and Supplementary Table 5 presents statistical estimates from the logit model estimating the likelihood of not experiencing mortality over the observational period. Supplementary Table 6 includes estimates from the IPW-adjusted multilevel Poisson models for condition-specific limitations, and Supplementary Table 7 contains estimates from the IPW-adjusted multilevel zero-inflated gamma models used to predict presence and severity of limitation across all reported conditions.
The comorbid conditions that were found to have the strongest associations with each index condition were generally stable in the IPW-adjusted Poisson models, though there were some interesting variations in which conditions were significantly associated with each index condition. Variation in estimates related to cancer was especially pronounced. For example, hypertension and arthritis emerged as significant predictors of cancer-related limitations, and the association between cancer-related limitations and depression was reduced to nonsignificance. Cancer also emerged as a relatively strong predictor of limitations resulting from depression, and the negative association between limitations due to memory loss and comorbid cancer was significant in the IPW-adjusted models.
When adjusting the zero-inflated model of overall limitations for IPWs, the association between each condition and likelihood of reporting any limitation remained stable, excluding the effect of hypertension, which was reduced to nonsignificance. Associations between each condition and the magnitude of limitations among those reporting some limitations were also generally robust to adjustment for IPWs, though heart condition emerged as a significant yet weak predictor of limitation severity.
Supplementary Table 8 presents the distribution of reported cancer type at first report of a cancer diagnosis. There were 612 valid reports of cancer type at first report of prior cancer diagnosis, with breast cancer (23.69%, n = 145), other cancer type (19.61%, n = 120), skin cancer (14.87%, n = 91), and prostate cancer (13.56%, n = 83) being the four most common cancer types. Supplementary Table 9 presents the distribution of cancer status and treatment modality at first report of cancer diagnosis grouped by year (2005–2011 and 2013–2021). For both groupings of interview year, the majority of respondents reported their cancer had been cured (2005–2011, n = 283, 68.03%; 2013–2021, n = 123, 66.49%), followed by reporting that their cancer was in remission (2005–2011, n = 70, 16.83%; 2013–2021, n = 29, 15.68%). Between 12% and 15% of respondents reporting a prior cancer stated they were currently seeking treatment, and for interview years 2013–2021, about 6% (n = 11) reported they had cancer but were not seeking treatment.
Conclusion
Taking a person-centered approach to examining limitations to daily activities resulting from chronic conditions, our study identified that condition prevalence and severity of limitations resulting from a given condition are both important inputs to understanding multimorbidity severity at the population level. We also found that specific comorbid conditions influence the perceived limitations reported for an index condition. Our results indicate that specific chronic conditions are uniquely associated with the likelihood of experiencing any limitation and the magnitude of limitations among those reporting some limitations to daily activities. Sensitivity analyses generally supported the primary findings, though heterogeneity across missing data treatments and characteristics related to cancer type and treatment status may have influenced some associations.
Though respondents with hypertension reported few limitations, the high prevalence of hypertension resulted in this condition being a component of the five most frequent condition combinations and four of the five most severe combinations. As a contributor to condition-specific and overall condition-related limitations, hypertension was not a strong or consistent predictor of limitation severity. Diabetes, heart condition, and arthritis were comorbid conditions that demonstrated relatively strong associations with hypertension-related limitations, indicating that the presence of potentially more debilitating comorbid conditions may influence a patient’s perception of how less detrimental conditions such as hypertension limit their daily activities. This suggests that older adults experiencing multimorbidity may have difficulty determining which condition is leading to their limitations, meaning clinicians can support older adults with multimorbidity by educating the patient on how their array of conditions (both independently and in tandem) may result in limitations to their daily activities. Guidance on the prioritization of treatment and lifestyle modifications would help the patient identify and address the conditions that are most likely resulting in the experience of limitation.
Of the more prevalent conditions, arthritis appeared to be associated with the most severe limitations to daily activities. Arthritis was a component of the ten disease combinations with the greatest limitation scores. As a comorbid condition, arthritis was identified as a consistent predictor of perceived limitations for all index conditions excluding cancer and memory loss, though these associations were significant in the IPW-adjusted models. Arthritis also had a relatively strong association with the likelihood of reporting any limitation due to all reported conditions. The fact that arthritis was not positively associated with magnitude of limitations in the zero-inflated model was interesting, but this may be related to heterogeneity in the degree of functional limitation and lack of clear diagnostic criteria for arthritis, meaning some respondents may have been diagnosed with arthritis for relatively minor symptoms, while others may experience severe pain and mobility limitation. As a common musculoskeletal condition that can result in severe limitations to normal daily activities, a patient’s arthritis status appears to be an important target for those working to reduce the burden of multimorbidity on the individual’s daily routines and activities.
In models examining how comorbid conditions contributed to the perceived severity of limitations caused by each index condition, memory loss was associated with greater limitations reported for all conditions excluding cancer (though memory loss was only significantly associated with perceived limitations due to lung disease in the IPW-adjusted models). Memory loss was the least frequently reported condition, yet those reporting memory loss experienced the most severe limitations to normal activities. Cognitive impairment is a particularly debilitating age-related condition when reported as a comorbid condition, indicating how the significant limitations resulting from memory loss may increase the severity of comorbid conditions due to factors such as ineffective management of comorbid conditions. When considering a patient’s perceived limitations resulting from their specific constellation of chronic conditions, assessment of cognitive status is critical to identifying the individual-level burden of comorbid conditions.
Another notable finding from the condition-specific limitation models was heterogeneity in the effect of comorbid conditions across index conditions. For example, the association between limitations reported for hypertension or stroke and comorbid diabetes was substantially greater than the associations between limitations reported for arthritis and comorbid diabetes. Similarly, memory loss was more strongly associated with limitations reported for stroke, heart condition, and diabetes than arthritis. These findings speak to the complex etiology, treatment, and personal management of multimorbidity, as some conditions such as memory loss appear to play a primary role in the perceived limitations attributable to almost all index conditions, while others such as diabetes were strongly associated with limitations reported for some conditions, but not others. Several factors including duration, treatment/control, sequencing of condition onset, and amplification of limitations resulting from greater numbers of conditions with putatively similar pathogenesis (eg, components of cardiometabolic multimorbidity including diabetes, heart disease, and stroke) may be at play and require further investigation to identify potential mechanisms through which comorbid conditions differentially influence perceived limitations reported for specific chronic conditions.
Though examining the association between each index condition and comorbid conditions is insightful, assessment of total limitations attributable to all reported chronic conditions provides a more holistic view of how the individual’s day-to-day experience is affected by multimorbidity. Reporting any chronic condition increased the likelihood of experiencing some perceived limitation to daily activities, with conditions including memory loss and arthritis being most strongly associated with reporting some perceived limitation, and memory loss and lung disease being the two conditions that were positively associated with magnitude/severity of limitations. Reflecting findings from the index-condition models, memory loss resulted in significant limitations in overall daily activities and warrants continued research and clinical investments to guide policy initiatives. Lung disease also has a significant impact on daily activities related to restrictions on movement caused by shortness of breath and fatigue (34,35) and represents another focal condition where timely and effective treatment may reduce the collective impact of age-related chronic conditions on the daily activities of older adults.
Results from sensitivity analyses adjusting for potential bias due to mortality selection generally supported the primary findings, but notable differences emerged that may speak to the increased risk of mortality associated with specific conditions. In the primary models predicting limitations resulting from a specific index condition, both lung disease and depression were negatively associated with limitations resulting from a cancer diagnosis. In the cancer-related limitation model estimated on the trimmed sample with adjustment for IPW, lung disease continued to display a negative association with cancer-related limitations, but the effect of depression was reduced to nonsignificance, the effect of arthritis emerged as positive, and both hypertension and heart condition emerged as having significant negative associations with cancer-related limitations. As a predictor, the effect of cancer on limitations reported for each index condition also showed substantial variation (eg, in the IPW models, the effect of cancer was positively associated with limitations reported for diabetes and depression and was negatively associated with limitations due to memory loss, and the association between lung disease limitations and comorbid cancer was reduced to nonsignificance). This variability across missing data treatments may reflect some survivorship bias among those diagnosed with cancer, as cancer is the second leading cause of death among U.S. adults aged 55 and older (36), survival time after diagnosis with cancer is lower than other chronic conditions (37), and cancer displayed a relatively strong negative association with survivorship in logit models used to estimate IPWs.
Follow-up descriptive analysis of reported cancer type and treatment modality revealed support for the conclusion that lower–than-expected cancer-related limitations and inconsistent associations may be partially attributed to overrepresentation of cancer survivors experiencing less lethal cancers with lower mortality rates. As both skin and prostate cancers were included in prior cancer diagnoses and represented a substantial proportion of cancer diagnoses reported, the relatively low average severity of cancer-related limitations may reflect that cancer survivors in the dataset are those who experienced less virulent forms of cancer. The majority of respondents who provided information on cancer status and treatment modality reported cancers that were cured or in remission, again indicating that varying rates of mortality across cancer types may have influenced our findings. Further research examining details including age of cancer diagnosis and treatment adherence would help better understand the role of cancer in person-centered multimorbidity severity.
Limitations and Future Directions
Our study is among the first to report on perceived limitations resulting from specific chronic conditions in a large population-based panel study, but there are constraints on the inferences that can be drawn from our work. Given the method of collecting information on psychiatric diagnoses and related limitations in the PSID, depression-related limitations included limitations related to depression as well as several comorbid psychiatric conditions. While we limited respondents to those who reported depression, comorbid psychiatric conditions may have contributed to reported severity of limitations due to depression.
Other factors restricting the applicability of our findings include a limited set of chronic conditions and the self-reported nature of the conditions examined. Possible chronic conditions were restricted to those conditions included in the PSID. Though our analyses included several conditions identified as relevant for inclusion in multimorbidity indices (38), some suggested conditions were not available in the PSID. We also prioritized conditions included in other large population-based health surveys. A wider array of conditions may have enabled identification of other multimorbidity patterns and comorbidities associated with multimorbidity severity, and future work should attempt to replicate our findings using a more inclusive set of conditions. Finally, as all doctor-diagnosed conditions were self-reported, and substantial variability in self-report of chronic conditions over time has been documented (39,40), our results may be susceptible to errors in self-reporting of conditions. Linkage to health records is unavailable for recent PSID waves, limiting our ability to validate the self-reported conditions.
This study represents a novel examination of perceived disease severity resulting from multimorbidity and can inform those working to reduce the impact of chronic conditions on the daily lives of aging adults. Perceptions of how each condition affects one’s daily activities are relative and depend on the other chronic conditions the person may experience. Focusing on comorbid conditions that are both responsive to intervention and associated with the greatest perceived limitation to daily life (eg, arthritis) may help reduce the overall burden of disease. Our work also highlights the importance of accounting for the prevalence and severity of age-related conditions as they occur and co-occur in individuals when attempting to estimate the population health burden of multimorbidity severity. Important suggested extensions of this work include further validation of condition-specific limitations (eg, what specific activities are limited by each condition), testing how individual characteristics moderate the impact of comorbid conditions on condition-specific limitations, and assessing whether multimorbidity indices may benefit from incorporating limitation-weighted conditions when predicting system and policy-relevant outcomes such as hospitalization and mortality.
Supplementary Material
Acknowledgments
N.J.B. lead data curation, project administration, and visualization. A.R.Q. lead funding acquisition. N.J.B., C.N., and A.R.Q. contributed equally to conceptualization, investigation, methodology, formal analyses, and writing of the original draft and revision.
Contributor Information
Nicholas J Bishop, Human Development and Family Science Program, Norton School of Human Ecology, University of Arizona, Tucson, Arizona, USA.
Corey Nagel, College of Nursing, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA; Department of Biostatistics, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA.
Ana R Quiñones, Department of Family Medicine, and the OHSU-PSU School of Public Health, Oregon Health & Science University, Portland, Oregon, USA.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health (R01AG055681 and RF1AG058545 to A.R.Q.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None.
References
- 1. Khunti K, Sathanapally H, Mountain P.. Multiple long term conditions, multimorbidity, and co-morbidities: we should reconsider the terminology we use. BMJ. 2023;383:2327. https://doi.org/ 10.1136/bmj.p2327 [DOI] [PubMed] [Google Scholar]
- 2. Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers. 2022;8(1):48. https://doi.org/ 10.1038/s41572-022-00376-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. https://doi.org/ 10.1093/epirev/mxs009 [DOI] [PubMed] [Google Scholar]
- 4. Buttorff C, Ruder T, Bauman M.. Multiple chronic conditions in the United States. RAND Corporation; 2017. https://www.rand.org/pubs/tools/TL221.html [Google Scholar]
- 5. Bishop NJ, Haas SA, Quiñones AR.. Cohort trends in the burden of multiple chronic conditions among aging U.S. adults. J Gerontol B Psychol Sci Soc Sci. 2022;77(10):1867–1879. https://doi.org/ 10.1093/geronb/gbac070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosbach M, Andersen JS.. Patient-experienced burden of treatment in patients with multimorbidity—a systematic review of qualitative data. PLoS One. 2017;12(6):e0179916. https://doi.org/ 10.1371/journal.pone.0179916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lehnert T, Heider D, Leicht H, et al. Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420. https://doi.org/ 10.1177/1077558711399580 [DOI] [PubMed] [Google Scholar]
- 8. Boyd CM, Weiss CO, Halter J, Han KC, Ershler WB, Fried LP.. Framework for evaluating disease severity measures in older adults with comorbidity. J Gerontol A Biol Sci Med Sci. 2007;62(3):286–295. https://doi.org/ 10.1093/gerona/62.3.286 [DOI] [PubMed] [Google Scholar]
- 9. Quiñones AR, Allore HG, Botoseneanu A, Newsom JT, Nagel CL, Dorr DA.. Tracking multimorbidity changes in diverse racial/ethnic populations over time: issues and considerations. J Gerontol A Biol Sci Med Sci. 2020;75(2):297–300. https://doi.org/ 10.1093/gerona/glz028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rizzo A, Jing B, Boscardin WJ, Shah SJ, Steinman MA.. Can markers of disease severity improve the predictive power of claims-based multimorbidity indices? J Am Geriatr Soc. 2023;71(3):845–857. https://doi.org/ 10.1111/jgs.18150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stone CL. A population-based measure of chronic disease severity for health planning and evaluation in the United States. AIMS Public Health. 2020;7(1):44–65. https://doi.org/ 10.3934/publichealth.2020006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kronick R, Gilmer T, Dreyfus T, Lee L.. Improving health-based payment for Medicaid beneficiaries: CDPS. Health Care Financ Rev. 2000;21(3):29–64. [PMC free article] [PubMed] [Google Scholar]
- 13. Crabtree HL, Gray CS, Hildreth AJ, O’Connell JE, Brown J.. The Comorbidity Symptom Scale: a combined disease inventory and assessment of symptom severity. J Am Geriatr Soc. 2000;48(12):1674–1678. https://doi.org/ 10.1111/j.1532-5415.2000.tb03882.x [DOI] [PubMed] [Google Scholar]
- 14. Wei MY, Kabeto MU, Langa KM, Mukamal KJ.. Multimorbidity and physical and cognitive function: performance of a new multimorbidity-weighted index. J Gerontol A Biol Sci Med Sci. 2018;73(2):225–232. https://doi.org/ 10.1093/gerona/glx114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wei MY, Kawachi I, Okereke OI, Mukamal KJ.. Diverse cumulative impact of chronic diseases on physical health-related quality of life: implications for a measure of multimorbidity. Am J Epidemiol. 2016;184(5):357–365. https://doi.org/ 10.1093/aje/kwv456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41(3):237–248. https://doi.org/ 10.1016/0165-1781(92)90005-n [DOI] [PubMed] [Google Scholar]
- 17. Ware JE, Snow KK, Kosinski M, Gandek B.. SF-36 Health Survey Manual & Interpretation Guide. The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 18. van Weel C, Schellevis FG.. Comorbidity and guidelines: conflicting interests. Lancet. 2006;367(9510):550–551. https://doi.org/ 10.1016/S0140-6736(06)68198-1 [DOI] [PubMed] [Google Scholar]
- 19. Van Oostrom SH, Picavet HSJ, Van Gelder BM, et al. Multimorbidity and comorbidity in the Dutch population-data from general practices. BMC Public Health. 2012;12:715. https://doi.org/ 10.1186/1471-2458-12-715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leplege A, Gzil F, Cammelli M, Lefeve C, Pachoud B, Ville I.. Person-centredness: conceptual and historical perspectives. Disabil Rehabil. 2007;29(20–21):1555–1565. https://doi.org/ 10.1080/09638280701618661 [DOI] [PubMed] [Google Scholar]
- 21. Klompstra L, Ekdahl AW, Krevers B, Milberg A, Eckerblad J.. Factors related to health-related quality of life in older people with multimorbidity and high health care consumption over a two-year period. BMC Geriatr. 2019;19:187. https://doi.org/ 10.1186/s12877-019-1194-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gu J, Chao J, Chen W, et al. Multimorbidity and health-related quality of life among the community-dwelling elderly: a longitudinal study. Arch Gerontol Geriatr. 2018;74:133–140. https://doi.org/ 10.1016/j.archger.2017.10.019 [DOI] [PubMed] [Google Scholar]
- 23. Fortin M, Hudon C, Dubois MF, Almirall J, Lapointe L, Soubhi H.. Comparative assessment of three different indices of multimorbidity for studies on health-related quality of life. Health Qual Life Outcomes. 2005;3:74. https://doi.org/ 10.1186/1477-7525-3-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larsen FB, Pedersen MH, Friis K, Glümer C, Lasgaard M.. A latent class analysis of multimorbidity and the relationship to socio-demographic factors and health-related quality of life. PLoS One. 2017;12(1):e0169426. https://doi.org/ 10.1371/journal.pone.0169426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ware JE. SF-36 Health Survey update. Spine. 2002;25:3130–3139. https://doi.org/ 10.1097/00007632-200012150-00008 [DOI] [PubMed] [Google Scholar]
- 26. Hunt SM, McEwen J.. The development of a subjective health indicator. Sociol Health Illn. 1980;2(3):231–246. https://doi.org/ 10.1111/1467-9566.ep11340686 [DOI] [PubMed] [Google Scholar]
- 27. Wallace RB, Herzog AR.. Overview of the health measures in the Health and Retirement Study. J Hum Resour. 1995;30:S84–S107. https://doi.org/ 10.2307/146279 [DOI] [Google Scholar]
- 28. McGonagle KA, Schoeni RF, Sastry N, Freedman VA.. The Panel Study of Income Dynamics: overview, recent innovations, and potential for life course research. Longit Life Course Stud. 2012;3(2):188–210. https://doi.org/ 10.14301/llcs.v3i2.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson DS, McGonagle KA, Freedman VA, Sastry N.. Fifty years of the Panel Study of Income Dynamics: past, present, and future. Ann Am Acad Polit Soc Sci. 2018;680(1):9–28. https://doi.org/ 10.1177/0002716218809363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. US Department of Health and Human Services. Multiple chronic conditions—a strategic framework: optimum health and quality of life for individuals with multiple chronic conditions. HHS; 2010. https://www.hhs.gov/sites/default/files/ash/initiatives/mcc/mcc_framework.pdf [Google Scholar]
- 31. Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK.. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. https://doi.org/ 10.5888/pcd10.120239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stekhoven DJ, Bühlmann P.. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–118. https://doi.org/ 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- 33. Weuve J, Tchetgen Tchetgen EJ, Glymour MM, et al. Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology. 2012;23(1):119–128. https://doi.org/ 10.1097/EDE.0b013e318230e861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kaptain RJ, Helle T, Patomella AH, Weinreich UM, Kottorp A.. New insights into activities of daily living performance in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2021;16:1–12. https://doi.org/ 10.2147/COPD.S264365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Annegarn J, Meijer K, Passos VL, et al. ; Ciro+ Rehabilitation Network. Problematic activities of daily life are weakly associated with clinical characteristics in COPD. J Am Med Dir Assoc. 2012;13(3):284–290. https://doi.org/ 10.1016/j.jamda.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 36. Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, provisional mortality on CDC WONDER online database. 2024. http://wonder.cdc.gov/mcd-icd10-provisional.html [Google Scholar]
- 37. Rizzuto D, Melis RJF, Angleman S, Qiu C, Marengoni A.. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. 2017;65(5):1056–1060. https://doi.org/ 10.1111/jgs.14868 [DOI] [PubMed] [Google Scholar]
- 38. Ho ISS, Azcoaga-Lorenzo A, Akbari A, et al. Measuring multimorbidity in research: Delphi consensus study. BMJ Med. 2022;1(1):e000247. https://doi.org/ 10.1136/bmjmed-2022-000247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cigolle CT, Nagel CL, Blaum CS, Liang J, Quiñones AR.. Inconsistency in the self-report of chronic diseases in panel surveys: developing an adjudication method for the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2018;73(5):901–912. https://doi.org/ 10.1093/geronb/gbw063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Quiñones AR, Melekin A, Cigolle CT, Nagel CL.. Disputes of self-reported chronic disease over time: the role of race, ethnicity, nativity, and language of interview. Med Care. 2019;57(8):625–632. https://doi.org/ 10.1097/MLR.0000000000001148 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.