Abstract
Background
Black/African American women with breast cancer have a disproportionately higher risk of mortality compared to other race groups, although their overall incidence of disease is lower. Despite this, advance care planning (ACP) and consequent code status documentation remain low in this vulnerable patient population. Code status orders (i.e., Full code, Do Not Attempt Resuscitation [DNAR], Do Not Intubate [DNI]) allow consideration of patient preferences regarding the use of aggressive treatments, such as cardiopulmonary resuscitation and intubation. The aim of this study is to characterize presence of code status orders and determine whether race affects code status documentation after the first encounter for breast cancer.
Methods
Data were derived from 7524 women with breast cancer from the University of Chicago Medical Center (UCMC) between 2016 and 2021. Cox regression was used to estimate the effects of race and adjusted for age, ethnicity, inpatient stays, metastatic breast cancer, marital status, and body mass index.
Results
The sample included 60.5% White, 3.6% Asian/Mideast Indian, 28.9% Black/African American, and 7.0% other or unknown race. Results indicate that code status orders after the first breast cancer encounter were uncommon (7.2%). Black/African American race (HR = 2.74; 95% CI: 1.75, 4.28) emerged as a significant factor associated with any code status orders compared to other race groups even when adjusting for covariates.
Conclusions
Code status documentation in this sample of women with breast cancer was low overall, yet rates were higher among Black/African American patients compared to other race groups. In fact, race remains a significant predictor of code status documentation even when accounting for indirect measures of cancer severity. This could be denoting the racial disparities (e.g., higher cancer malignancy such as triple negative breast cancer) in breast cancer mortality risk. Future research is needed to identify factors unique to Black/African American women that would increase code status documentation so that goal concordant care can be prioritized among patients with breast cancer.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-024-13132-6.
Keywords: Code status orders, Advance care planning, Breast cancer, Racial disparities
Introduction
Although overall incidence of breast cancer is lower, Black/African American women have a disproportionately higher risk of mortality [1]. Population-based studies consistently find that race remains an independent predictor of survival [2]. Contributing to these disparities are the often more advanced stages of disease during presentation or diagnosis, higher malignancy of cancer (i.e., triple negative breast cancer), faster tumor growth, earlier metastasis, and insufficient access to screening and care [3–6].
Given the impact of these factors on survival rates for Black/African American women with breast cancer, there is an urgent need to prioritize discussion with patients regarding their end-of-life wishes to ensure congruence with care given. One way to do this is by initiating advance care planning (ACP) conversations early to allow for value-aligned care in this vulnerable patient population. ACP involves conversations with patients about their future clinical care preferences and a key focus is discussion on aggressive life-sustaining interventions such as mechanical ventilation (e.g., intubation) and cardiopulmonary resuscitation (CPR) [7]. The designation regarding the use of intubation and CPR is made through official code status placements in the electronic health record, which include no restrictions on their use (Full code) or specific restrictions such as do-not-attempt-resuscitation (DNAR) or do-not-intubate (DNI). Patients may elect for a DNI or DNAR rather than Full code status because such interventions can cause suffering and subsequent outcomes are often poor [8, 9]. In fact, over 93% of patients with cancer who survive initial resuscitation attempts after in-hospital cardiac arrest eventually die during hospitalization [9]. Specifically, immediate survival had been observed in 45% of the patients, but only 13% of these survivors were alive at hospital discharge. Education of such consequences is a common reason patients with cancer may choose to have orders restricting the use of aggressive interventions earlier in the course of cancer [7]. On the other hand, acute clinical deterioration is also a common reason for restrictive code order placements near the end of life and is related to reduced patient involvement [7, 10]. Therefore, aggressive interventions may conflict with patient values and the designation of a code status order early in the course of cancer care is crucial for maximizing patient engagement [11].
Current guidelines recommend that ACP discussions occur following any changes in the treatment plan or prognosis of patients with cancer [12]. Specifically, documentation of the goals of care should occur within one month of a diagnosis with metastatic cancer, within 48 h of admission to any hospital or intensive care unit, and before intervention with mechanical ventilation. It is further advised that ACP discussions occur prior to the initiation of a chemotherapy regimen or invasive procedures due to the potential impact these treatments may have on patients’ decision-making capacity. Considering the significant role of chemotherapy, mastectomies, and other invasive treatments during the treatment of breast cancer as well as the heightened risk of mortality associated with potential metastatic disease (occurring in close to 12% of patients) [13], ensuring the timely documentation of code status is particularly vital. This notion is reiterated by the American Medical Association Code of Medical Ethics which recommends that physicians discuss resuscitative interventions in the early stages of care, while patients maintain their decisional capability [14].
Despite the urgent need and existing recommendations, ACP conversation rates are low in the US and even lower among Black/African American patients [6]. Hence, documentation of code status remains expectedly low among patients with cancer, with only 15.5% of those diagnosed with metastatic breast cancer at a prominent US medical center having a code status order [15]. Moreover, the majority of these discussions are not timely as they often occur during hospitalization [16]. Although no racial differences in code status documentation have been found in patients with metastatic cancer of any kind [15], racial disparities have not been investigated in the code status documentation of patients with breast cancer at any stage of disease. Black/African American patients may benefit the most from increased early documentation due to their disproportionately high rates of death from breast cancer [6]. Without improved documentation, Black/African American patients are hindered from communicating their end-of-life wishes to the healthcare team who may in turn provide resuscitative interventions that deviate from patients’ values [17]. For instance, despite Black/African American patients being more likely to receive life-prolonging care compared to White patients (19.7% vs. 6.9%), Black/African American patients who had end-of-life discussions with their physician were more inclined to opt for symptom-directed care over life-prolonging measures [17]. This may indicate that Black/African American patients may be receiving lower rates of end-of-life discussion, implying that their preferences regarding resuscitative interventions may not be adequately respected.
Given the low rates of code status documentation and the possibility of changes in patient wishes throughout the course of illness, there is a need to characterize the rates of code status documentation to determine which factors affect presence of code status documentation after the first encounter for breast cancer. Previous research has examined the factors associated with ACP (e.g., physician availability [18]), code status documentation (e.g., religious affiliation or higher number of clinic visits [15]) and ACP’s effects on the alignment between patients’ end-of-life care preferences and the care they receive; however, the timing and specific factors associated with code status documentation, an important outcome of ACP discussions, have not been examined in women with breast cancer. Further, these effects have not been investigated among patients with any diagnosis of breast cancer, which encompasses patients in any type of clinical care setting, as well as any phase of disease; this includes the early phases prior to clinical deterioration when patients may have greater ability to communicate their treatment preferences. The aim of this study was to obtain a more comprehensive understanding of code status documentation in patients diagnosed with any stage of breast cancer. This involved characterizing the frequency of code status documentation and examining factors that affect its presence after patients’ first clinical encounter for breast cancer. Additionally, this study aimed to determine factors independently associated with code status documentation in patients with breast cancer and particularly whether race will emerge as a significant factor after controlling for the effects of covariates.
Methods
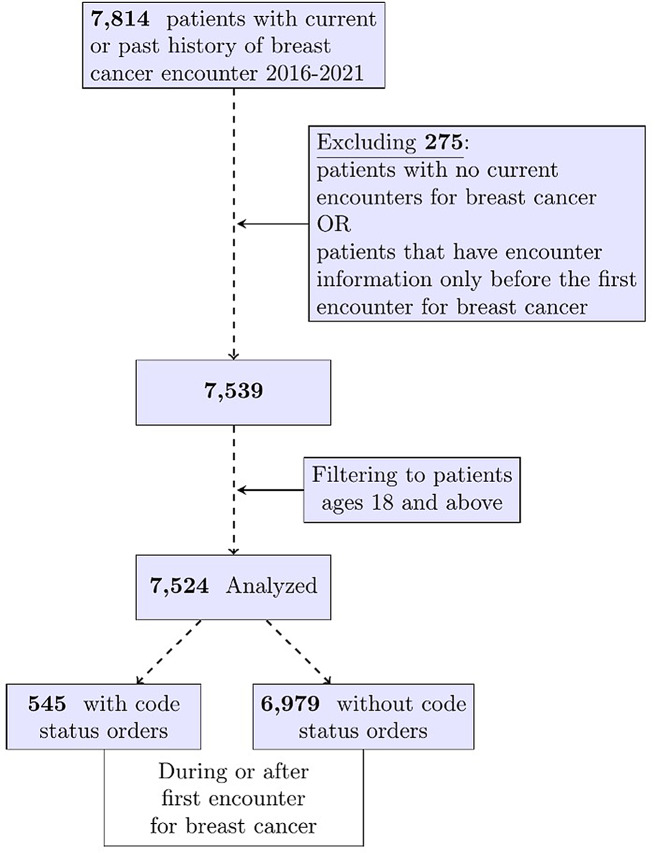
Data were drawn from the electronic health records of a cohort of 7,814 women with a breast cancer diagnosis over a 5-year period (2016–2021) treated at the University of Chicago Medical Center (UCMC), a large, urban medical center with a catchment area serving one of the largest African American communities in the United States [19]. The University of Chicago Institutional Review Board approved the extraction of these data (IRB21-0160). Included were patients with breast cancer 18 years of age or older. Excluded were patients with no encounters at this institution where breast cancer is a diagnosis (ICD-10 codes starting with C50) or those that do not have encounter information after the first encounter for breast cancer (indicating that care was likely transferred to another institution). The final analytic sample included 7524 women with breast cancer. See Fig. 1. for flowchart of cohort selection.
Fig. 1.
Flowchart of cohort selection
Measures
Outcome
Presence of code status documentation was defined as a manually entered code status order (Full code, DNAR, or DNAR/DNI) at the same or any subsequent clinical encounter following the first encounter for breast cancer. The presence of a manually entered Full code order indicates that a discussion regarding treatment preferences occurred and preference toward resuscitative interventions was given. On the other hand, the absence of any code status orders indicates that discussion had not occurred and UCMC policy requires an assumed Full code for these patients. The current study only considers manually entered codes. Covariates. Body mass index (BMI) components (height and weight) are from the earliest available encounter following first breast cancer encounter. Presence of any inpatient stays was defined as a time-dependent variable that remains “No” until the first inpatient encounter and then remains “Yes” until the end of follow-up. Similarly, metastatic breast cancer (Secondary malignant neoplasm of breast; ICD-10 code of C79.81) was defined as a time-dependent variable. Demographic characteristics included age, race, ethnicity, and marital status. Race and ethnicity were included as separate dummy-coded variables as this information was extracted from the electronic health record where information on patient race and ethnicity is recorded separately. This study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [20] Fig. 1.
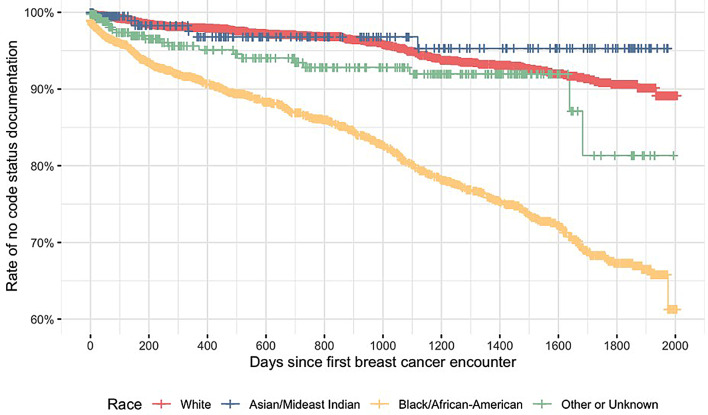
Fig. 2.
Kaplan Meier curve of survival by patient race
Statistical analysis
Continuous variables are described using medians with interquartile ranges and categorical variables are described using frequencies with percentages. Comparison of variables related to code status documentation between patients that died and those that did not die were made using Wilcoxon rank sum and Pearson Chi-squared/Fisher’s exact tests for continuous and categorical variables, respectively.
The impact of Black/African American race, ethnicity, age during first encounter, marital status, inpatient stays, and metastatic breast cancer on code status documentation was assessed using Kaplan-Meier curves and log-rank tests [21]. Variables with significant log-rank tests were assessed for the Cox proportional hazard (PH) [22] assumption imposed by the model using the scaled Schoenfeld residuals test. This indicates that the hazard ratio for a given covariate is constant over time and an extended version of the Cox model can be fit using an interaction between the covariate and time. A model with Black/African American race and ethnicity as the only covariates and a multivariate model with all the covariates were fit to compare the hazard ratio estimates for Black/African American race. The outcome of interest was presence of any code status orders. Time to code status documentation is defined as the number of days from the first breast cancer encounter to the first encounter where code status was documented. Patients who have died without any code status orders were censored given that death from breast cancer is unlikely to occur unexpectedly and there would likely be ample opportunity to place a code status order. Statistical significance was defined as p-value < 0.05. All analyses were conducted using R version 4.2.1.
Results
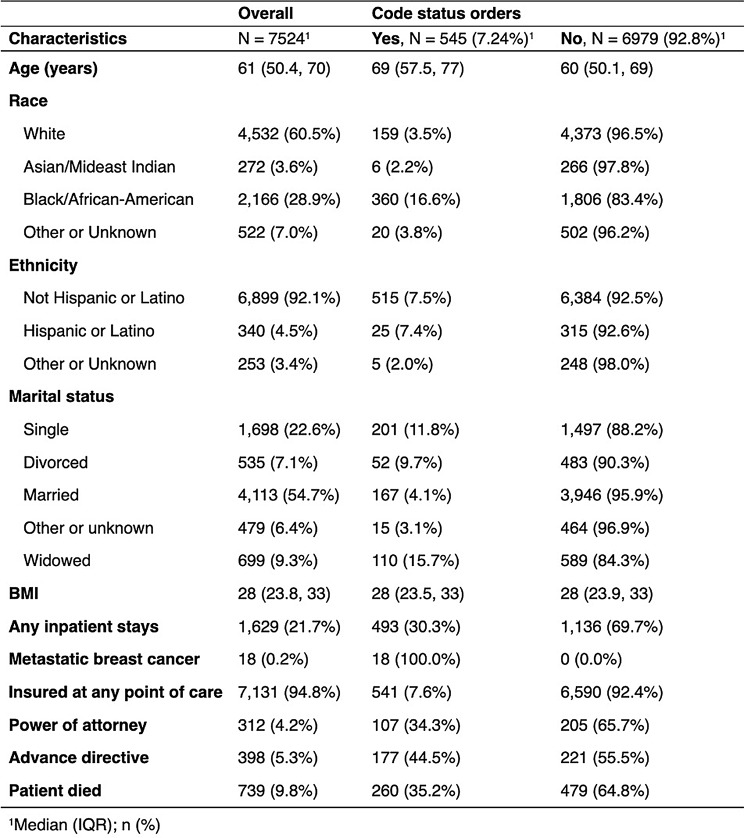
Our sample included 545 (7.2%) patients with code status documentation after the first breast cancer encounter and 6979 (92.8%) patients without. The median (IQR) age of our sample was 61 (50.4, 70.0). The majority of the sample was White (60.5%) or Black/African American (28.9%). We found that among patients with code status orders, 107 (34.3%) had a power of attorney and 177 (44.5%) had an advance directive. In contrast, among patients patients without code status orders, 205 (65.7%) had a power of attorney and 221 (55.5%) had an advance directive. Table 1 shows the descriptive characteristics of the sample stratified by presence of code status documentation.
Table 1.
Descriptive characteristics of women with breast cancer stratified by presence of code status orders
Supplementary Table 1 shows information on code status documentation such as code status, timing, and clinical setting stratified by patient mortality. In sum, women who died had a higher number of code status orders (2 vs. 1; p-value < 0.001) and less time until the first code status was documented (336 vs. 747 days; p-value < 0.001). Their first, second, and last code status orders were more likely to be DNAR or DNAR/DNI and occur in an inpatient hospital setting (all p-values < 0.001). Only 22 (< 0.1%) patients had code status documentation at the first breast cancer encounter. Most patients had only one (n = 323) or two (n = 115) code status orders documented but the maximum was 16. Two-hundred twenty-two patients had any code status transitions (two or more code status orders). Of those, the first code was Full for 99 (44.6%), DNAR for 18 (8.1%), and DNAR/DNI for 105 (47.3%) patients. The last code was Full for 84 (37.8%), DNAR for 22 (9.9%), and DNAR/DNI for 116 (52.3). See Supplementary Fig. 1.
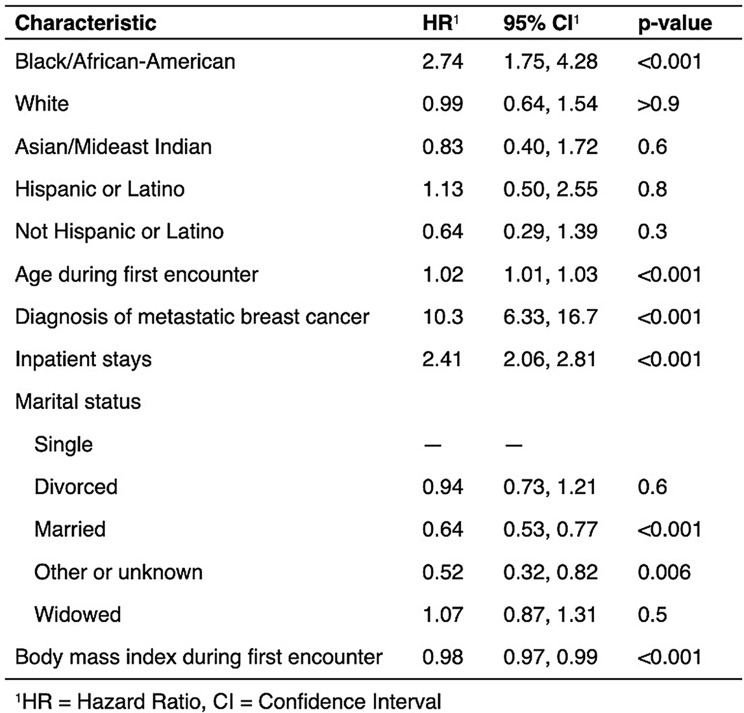
The Schoenfeld residuals test indicated that age does not meet the PH assumption (p-value < 0.001). We therefore assessed a time-interaction with this variable and found a very small effect size (HR < 1.001; p-value < 0.001) and therefore opted for a parsimonious model without an age by time interaction. Increased rate of code status documentation was seen for Black/African American patients (HR = 3.11; 95% CI: 1.87, 5.20) compared to other race groups in the unadjusted model. The multivariate model which adjusted for race and ethnicity as dummy variables, age at first encounter, diagnosis of metastatic breast cancer, prior inpatients stays, marital status, and BMI at first encounter (Table 2) showed greater than twice the likelihood of code status documentation for Black/African American (HR = 2.74; 95% CI: 1.75, 4.28) patients compared to patients in all other race groups. Increased likelihood was also seen for those with any inpatient stays compared to those without prior inpatient stays at any given time point (HR = 2.41; 95% CI: 2.06, 2.81) and those with metastatic breast cancer compared to those who do not currently have metastatic breast cancer (HR = 10.30, 95% CI: 6.33, 16.7). Additionally, there was increased likelihood of code status documentation as age during the first encounter increased (HR = 1.02, 95% CI: 1.01, 1.03). Decreased likelihood was seen for married patients compared to single patients (HR = 0.64; 95% CI: 0.53, 0.77) and those with a marital status that was other or unknown (HR = 0.52; 95% CI: 0.32, 0.82). There was also a decreased likelihood of code status documentation as BMI during the first encounter increased (HR = 0.98, 95% CI: 0.97, 0.99).
Table 2.
Adjusted cox proportional hazard model of code status documentation
Discussion
The current study of women with breast cancer aimed to characterize code status orders and their transitions as well as examine factors associated with presence of code status orders after the first encounter for breast cancer. We find that code status orders were overall low in this patient sample, but lower in White patients. No differences in BMI were found between patients with and without code status orders. However, presence of an advance directive was lower in patients that did have code status orders indicating that these components may not be encompassed by a broad advance care planning discussion.
In patients with code status orders, we observed greater frequency of code status orders in patients who died, who also had less time until the first code status order and were more likely to have restrictive code status orders (i.e., DNAR, DNAR/DNI). Code status documentation during the first breast cancer encounter was very uncommon. This is consistent with research showing that the time from first encounter to clinical deterioration can be long for patients with breast cancer and corroborates previous studies’ observations [7, 10] that code status orders may be prompted by acute clinical deterioration near the end of life. Indirect measures of clinical deterioration measures in patients with breast cancer may include weight loss [23], inpatient hospital stays [24], and metastatic cancer [25], which are all associated with greater mortality risk. Indeed, the Cox model indicated that indirect measures of cancer severity such as lower BMI, metastatic breast cancer, and inpatient hospital stays emerge as independent predictors of code status documentation. However, this is particularly alarming as previous research suggests that code status changes associated with clinical deterioration are related to lower patient engagement [7]. This is likely due to the resulting urgency of being asked to make decisions shortly after being informed of the current prognosis. There is therefore a salient need to maximize patient engagement by initiating conversation about end of life wishes well before a considerable clinical deterioration occurs in this patient population. Failing to do so may result in patients being unable to sufficiently communicate their treatment preferences and receiving aggressive end-of-life care that does not align with their values.
Moreover, our finding that patients who are not partnered are more likely to have code status documentation may be attributed to their heightened awareness of the importance of advance care planning, as they lack reliance on family to make end of life decisions [26].
Lastly, we find that Black/African American race is associated with higher likelihood of code status documentation compared to other race groups. This difference remained even when accounting for indirect measures of cancer severity such as BMI, inpatient hospital stays and metastatic breast cancer. Despite the initial expectation that ACP conversations and subsequent code status orders may be lower in Black/African American patients with breast cancer given similar findings for ACP in overall patient populations [6], our study findings present the opposite. However, this finding may reflect racial disparities in the risk of mortality such as higher malignancy of cancer in Black/African American patients at the initial encounter [3]. A possibility is that healthcare providers may be recognizing and addressing the increased mortality risk faced by Black/African American patients, which prompts the discussion of end-of-life care. This promotes goal-concordant care and may foster improved trust and physician-communication which may ultimately improve patient outcomes. Additional research is needed to understand the effects of staging and disease severity on code status documentation. This is underscored by the possibility that the care team may be prompted to initiate discussion on code status if the clinical findings from imaging and laboratory tests indicate a more aggressive form of breast cancer, as is more likely the case with Black/African American patients, even if clinical deterioration has not occurred. This study is among the first to examine code status documentation specifically among patients with breast cancer, so there is currently limited information on existing interventions aimed at improving this aspect and future research is needed in this area.
It is shown that ACP not only enhances the alignment between patient preferences with the care they receive, but also improves patient-physician communication and fosters greater patient trust. This is especially important for Black/African American patients who are more likely to experience distrust towards their care team or have concerns about discrimination, factors which may contribute to delays in seeking care or receiving a timely diagnosis [3]. Finally, ACP may also mitigate the growing concern of the overtreatment of breast cancer through the use of mastectomies, particularly in Black/African American women who face a higher risk of this in cases when they view the surgeon as having the primary role in decision-making [27]. By encouraging shared decision-making, ACP can empower patients to actively participate in their care, promoting more equitable treatment outcomes.
Limitations
Although consideration of the time between code status documentation and death may be important to ensure that code status discussions occur well before clinical deterioration or death, we did not have information on the date of death for over half the patients with code status orders who died. Future work is needed to determine the frequency of code status orders placed following clinical deterioration for this patient population. Another limitation of this study is the absence of insurance status adjustment in our model due to the instability of insurance coverage across clinical encounters. The patients included in the cohort were treated over a five-year period during which insurance status may have changed multiple times. This instability could influence access and quality of healthcare services including ACP discussions, potentially impacting the timing and frequency of code status orders. Further, we did not have information on breast cancer stage which is a direct measure of disease severity. Instead, we used indirect measures including inpatient hospital stays and metastatic cancer to characterize the relationship between code status documentation and clinical deterioration. Additionally, we recognize the importance of patient-clinician communication in influencing advance care planning (ACP) and end-of-life care. However, our EHR-extracted data did not include standardized measures of patient-clinician communication and, therefore, we were not able to account for this in our analysis. Further, we opted not to account for socioeconomic status in our analysis because its relationship to ACP is inconclusive and the available proxies (e.g., zip code, health insurance, income, and education) are frequently outdated or incomplete in the EHR [28]. Lastly, there are known limitations to using race and ethnicity as covariates in regression models when race and ethnicity interact with other covariates or the outcome. We were not able to include robust measures of socioeconomic status in our model, and therefore, it is unclear whether results are related to differences in racial groups or effects of unmeasured social disadvantage.
Conclusions
Code status documentation in this sample of women with breast cancer was low overall, yet rates were higher among Black/African American patients. Future research is needed to identify factors unique to Black/African American women that would further increase code status documentation. Understanding these factors will help shape interventions to ensure that goal-concordant care can be prioritized among patients with breast cancer.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Supplementary Fig. 1 Code status transitions: From first to last
Supplementary Material 2: Supplementary Table 1 Descriptive characteristics of patients with code status orders by mortality.
Acknowledgements
The authors wish to acknowledge the contributions of the University of Chicago Center for Research Informatics for their assistance in data extraction.
Abbreviations
- ACP
Advance care planning
- DNAR
Do Not Attempt Resuscitation
- DNI
Do Not Intubate
- UCMC
University of Chicago Medical Center
- CPR
Cardiopulmonary resuscitation
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
- BMI
Body mass index
Author contributions
PPP: Conceptualization, Methodology, Formal analysis, Writing—original draft. HM: Methodology, Writing—review & editing. DV: Conceptualization. CH: Project administration. JM: Writing—review & editing. MKA: Conceptualization. PIM: Conceptualization, Methodology, Writing—review & editing. MMT: Conceptualization, Methodology, Data curation, Supervision, Funding acquisition, Writing—review & editing.
Funding
This work was supported by the National Cancer Institute under grant number P20 CA233307 (MMT).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The University of Chicago Institutional Review Board approved the extraction and use of these data from electronic health records. The requirement to obtain informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Cancer Society. Cancer Facts and Figures for African Americans 2019–2021. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf
- 2.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA: a cancer journal for clinicians. 2019 Nov;69(6):438–51. [DOI] [PubMed]
- 3.Jones CEL, Maben J, Jack RH, et al. A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open. 2014;4(2):e004076. 10.1136/bmjopen-2013-004076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, Alo RA, Payton M, Tchounwou PB. Health and racial disparity in breast Cancer. Adv Exp Med Biol. 2019;1152:31–49. 10.1007/978-3-030-20301-6_3. PMID: 31456178; PMCID: PMC6941147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Batina NG, Trentham-Dietz A, Gangnon RE, Sprague BL, Rosenberg MA, Stout NK, Fryback DG, Alagoz O. Variation in tumor natural history contributes to racial disparities in breast cancer stage at diagnosis. Breast Cancer Res Treat. 2013;138:519–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgement, religiousness, and treatment preferences. J Clin Oncol. 2007;26(25):4131–7. 10.1200/JCO.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Jawahri A, Lau‐Min K, Nipp RD, Greer JA, Traeger LN, Moran SM, D’Arpino SM, Hochberg EP, Jackson VA, Cashavelly BJ, Martinson HS. Processes of code status transitions in hospitalized patients with advanced cancer. Cancer. 2017;123(24):4895–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee MR, Yu KL, Kuo HY, Liu TH, Ko JC, Tsai JS, Wang JY. Outcome of stage IV cancer patients receiving in-hospital cardiopulmonary resuscitation: a population-based cohort study. Sci Rep. 2019;9(1):9478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reisfield GM, Wallace SK, Munsell MF, Webb FJ, Alvarez ER, Wilson GR. Survival in cancer patients undergoing in-hospital cardiopulmonary resuscitation: a meta-analysis. Resuscitation. 2006;71(2):152–60. [DOI] [PubMed] [Google Scholar]
- 10.Abrams HR, Nipp RD, Traeger L, Lavoie MW, Reynolds MJ, Ufere NN, Wang AC, Boateng K, LeBlanc TW, El-Jawahri A. Code status transitions in patients with high-risk acute myeloid leukemia. Blood Adv. 2022;6(14):4208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caissie A, Kevork N, Hannon B, Le LW, Zimmermann C. Timing of code status documentation and end-of-life outcomes in patients admitted to an oncology ward. Support Care Cancer. 2014;22:375–81. [DOI] [PubMed] [Google Scholar]
- 12.Walling A, Lorenz KA, Dy SM, Naeim A, Sanati H, Asch SM, Wenger NS. Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008;26(23):3896–902. [DOI] [PubMed] [Google Scholar]
- 13.Peart O. Metastatic breast cancer. Radiol Technol. 2017;88(5):M519–39. [PubMed] [Google Scholar]
- 14.American Medical Association. Code of Medical Ethics, 6/2016 update. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-5.pdf
- 15.Temel JS, Greer JA, Admane S, Solis J, Cashavelly BJ, Doherty S, Heist R, Pirl WF. Code status documentation in the outpatient electronic medical records of patients with metastatic cancer. J Gen Intern Med. 2010;25:150–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Einstein DJ, Einstein KL, Mathew P. Dying for advice: code status discussions between resident physicians and patients with advanced cancer—a national survey. J Palliat Med. 2015;18:535–41. [DOI] [PubMed] [Google Scholar]
- 17.Mack JW, Paulk ME, Viswanath K, Prigerson HG. Racial disparities in the outcomes of communication on medical care received near death. Arch Intern Med. 2010;170(17):1533–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crooks J, Trotter S, Clarke G. How does ethnicity affect presence of advance care planning in care records for individuals with advanced disease? A mixed-methods systematic review. BMC Palliat Care. 2023;22(1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim KE, Randal F, Johnson M, Quinn M, Maene C, Hoover S, Richmond-Reese V, KL Tangka F, Joseph DA, Subramanian S. Economic assessment of patient navigation to colonoscopy‐based colorectal cancer screening in the real‐world setting at the University of Chicago Medical Center. Cancer. 2018;124(21):4137–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–81. [Google Scholar]
- 22.Hess KR. Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat Med. 1995;14(15):1707-23. 10.1002/sim.4780141510. PMID: 7481205. [DOI] [PubMed]
- 23.Cespedes Feliciano EM, Kroenke CH, Bradshaw PT, Chen WY, Prado CM, Weltzien EK, Castillo AL, Caan BJ. Postdiagnosis weight change and survival following a diagnosis of early-stage breast cancer. Cancer Epidemiol Biomarkers Prev. 2017;26(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanson LC, Ernecoff NC, Wessell KL, Lin FC, Milowsky MI, Collichio FA, Wood WA, Rosenstein DL. Mortality risk for patients with stage IV cancer and acute illness hospitalization. J Pain Symptom Manag. 2021;61(4):797–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taskindoust M, Thomas SM, Sammons SL, Fayanju OM, DiLalla G, Hwang ES, Plichta JK. Survival outcomes among patients with metastatic breast cancer: review of 47,000 patients. Ann Surg Oncol. 2021;28(12):7441–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lo TJ, Ha NH, Ng CJ, Tan G, Koh HM, Yap PL. Unmarried patients with early cognitive impairment are more likely than their married counterparts to complete advance care plans. Int Psychogeriatr. 2017;29(3):509–16. [DOI] [PubMed] [Google Scholar]
- 27.Pak LM, Morrow M. Addressing the problem of overtreatment in breast cancer. Expert Rev Anticancer Ther. 2022;22(5):535–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barwise A, Juhn YJ, Wi CI, Novotny P, Jaramillo C, Gajic O, Wilson ME. An individual housing-based socioeconomic status measure predicts advance care planning and nursing home utilization. Am J Hospice Palliat Medicine®. 2019;36(5):362–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Supplementary Fig. 1 Code status transitions: From first to last
Supplementary Material 2: Supplementary Table 1 Descriptive characteristics of patients with code status orders by mortality.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.