Abstract
Thyroid angiosarcoma is an extraordinarily sparse malignancy, often populating alpine regions. Clinically, thyroid angiosarcomas tend to be nonspecific in presentation, starkly dependent on site, size, extension, and metastases. Tumors are locally aggressive and can present with sudden onset pain due to intra-nodular hemorrhage and compressive symptoms from sudden expansion. Due to the disease being a scarcely reported entity, there is little scholarship regarding its management. We report an interesting case of a 63-year-old man presenting with a swelling in the neck, incidentally found to be a thyroid angiosarcoma with a first-time reported associated spinal metastasis. The patient has a uniquely presenting thyroid angiosarcoma and is the first patient to present as such within a non-alpine South Asian region
Keywords: Thyroid angiosarcoma , aggressive cancer , palliation , spinal metastasis , non-alpine region , tracheostomy
Introduction
Thyroid Angiosarcoma is an extraordinarily sparse malignancy, often populating alpine regions [1].
This disease customarily presents with multinodular goiters, indicating the role nutritional iodine deficiencies may have as a major contributing factor [2].
Radiation and vinyl chloride exposure have also been established as causative to the development of thyroid angiosarcoma [1].
These tumors have a female preponderance, statistically delineated as 9:3, spanning ages 50 to 80 [3].
Clinically, thyroid angiosarcomas tend to be nonspecific in presentation, starkly dependent on site, size, extension, and metastases [1].
Tumors are locally aggressive and can present with sudden onset pain due to intra-nodular hemorrhage and compressive symptoms from sudden expansion. A vast fraction of these tumors present as painless and large, with sizes ranging from 2.5 cm to 13 cm, averaging 6 cm in size [3].
Metastatic complications include cough, hemoptysis, anemia, and hypercalcemia [3].
Thyroid angiosarcomas can be diagnostically challenging; it is necessary to differentiate from anaplastic carcinoma [4].
In 2000, a classification was detailed by Cutlsn et al, wherein the presence of endothelial differentiation and positive vascular markers was seen to typify thyroid angiosarcomas. If epithelial markers are present, the cancer is labeled an epithelioid angiosarcoma. An angiomatoid anaplastic carcinoma is ascertained by the expression of epithelial and endothelial markers, as well as thyroglobulin. If no vascular markers are expressed, then the tumor is classified as an anaplastic carcinoma with an angiosarcoma-like appearance [5].
Furthermore, it is essential to determine whether the tumor is primary or of metastatic origin [4].
A definitive diagnosis is made ordinarily after a thyroidectomy, which is then further investigated through immunohistochemistry [3].
The limited literature regarding the disease has factored into the fact that there is no gold standard of treatment. Complete radical surgery early on in the disease course seems to have been established as curative in some reported cases. Some papers relay adjuvant radiotherapy as having encouraging outcomes [1].
Due to the disease being a scarcely reported entity, there is little scholarship regarding its management. The prognosis is unfortunate with a 5-year survival rate of 33.3% [1].
Epidemiological studies have delineated a mortality rate amounting to nearly 90% [5].
Patients, subsequently, end up dying in less than 6 months, often regardless of treatment modalities employed, with a small fraction of patients surviving up to 5 years. Early diagnosis is imperative in composing treatment plans particular to individuals. This can only be done so if further research is done to expound upon this rare disease, improve awareness regarding this condition, and aptly commandeering the application of immunohistochemical stains [4].
We report an interesting case of a 63-year-old man presenting with a swelling in the neck, incidentally found to be a thyroid angiosarcoma with a first-time reported associated spinal metastasis. The patient has a uniquely presenting thyroid angiosarcoma and is the first patient to present as such within a non-alpine South Asian region.
History
63-year-old hypertensive for 2 years has a history of lower back pain for a few years, he underwent L4-5 pedicle screw fixation for this. The patient presented to the hospital with complaints of constipation for 7 days, urinary distention for the past 3 days, and myoclonic jerky movements of the body along with fever for the past two days.
The jerky movements progressed with each passing day and were more so in the lower limbs. 2 months ago, his mobility became restricted due to severe lower back pain. The patient’s family also reports irrelevant talk and drowsiness as well. He was brought to the ER with a GCS Of 15/15.
He also had a large left-sided neck mass first noticed three months ago; the swelling increased in size rapidly in the past 4 days. The swelling was also associated with hoarseness of voice. On examination, it was located on the left side of the lower neck region approximately 5x6 cm. It was firm and hard in consistency. The trachea was pushed towards the right side. Because of respiratory distress, he was intubated in the emergency room. CT scan of the neck mass showed a large hyperdense mass in the left cervical region encasing the left common carotid artery, encasing and compressing the left internal jugular vein extending from the level of hyoid bone up to the clavicle, inseparable from the left lobe of the thyroid gland. Few internal specks of calcification were seen within this mass. No evidence of necrosis. No cervical lymphadenopathy was appreciated.
CT Head and neck were further concerned for subarachnoid hemorrhage. Heme CSF level in the occipital horn of left lateral ventricle, suggestive of intraventricular extension. Patient status was post multiple spinal surgeries with grade 4 anterolisthesis of L5 over S1 and mild retrolisthesis of L4 over S1. Transpedicular bilateral screws through L5 are noted. Defective posterior arch of L5, destructive changes in the pedicle, and transverse processes of lamina L4.
Large lobular mass with few internal air locules extending into the spinal canal and extending through bilateral neural foramina in prevertebral spaces.
Further workup with an MRI of the lumbar spine with contrast was suggestive of mets. The patient was managed surgically and a biopsy from the lumbar region was taken which showed atypical cellular infiltrate.
Immunohistochemistry was concerning for a vascular neoplasm. A small biopsy was done that showed non-specific necrotic debris with fibrin.
This was followed by a left thyroid lobe biopsy that grossly consisted of multiple tan brown tissue fragments which were collectively measured to be 7.0 x 4.5 x 2.0 cm. The larger fragments were further sectioned to reveal a tan-brown cut surface with few hemorrhages. The biopsy showed a scanty viable tumor with extensive necrosis and a focal viable area showing thyroid follicles encased and infiltrated by atypical cells with vesicular nuclei (Figure 1).
Figure 1.
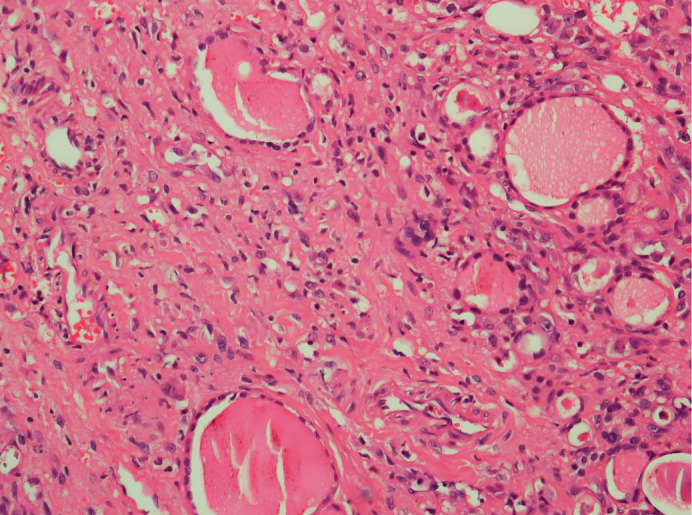
Thyroid follicles with intervening atypical vascular channels lined by pleomorphic cells. Focal lumina shows RBCs; confirming the vascular nature of the infiltrate. (Hematoxylin-eosin, original magnification×20).
Focal vague vaso-formations were seen and the focal lumina showed RBCs. Owing to cytological atypia, positive vascular markers, and the presence of a similar lesion at a distant site, a diagnosis of angiosarcoma was made.
Immunohistochemistry details showed ERG and CD31 positive (Figure 2), whereas, CD34, CKAE1AE3, and TTF-1 were negative. ERG image showed atypical vascular proliferation entrapping thyroid follicles and the CD-31 slide highlighted atypical vascular channels lined by pleomorphic cells.
Figure 2.
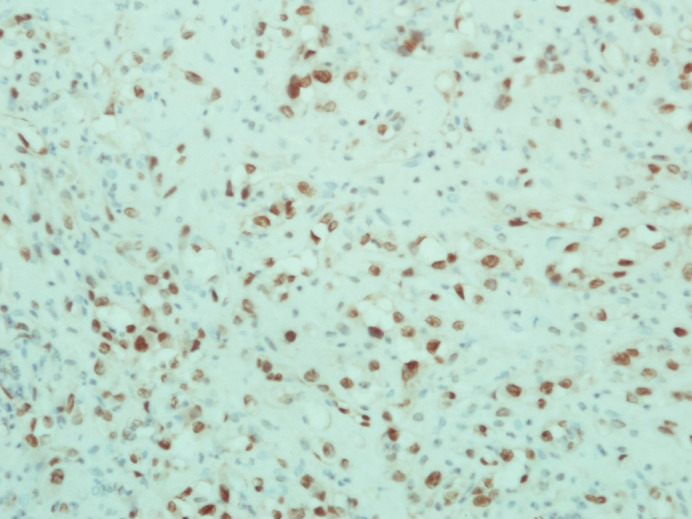
Immunohistopathological image highlighting atypical vascular channels lined by pleomorphic cells. (CD31 stain, original magnification×40).
Due to the advanced stage of the cancer, the patient was managed palliatively with an NG tube for bowel decompression and a Foley catheter for urinary retention. A permanent tracheostomy was made to help the patient breathe better. The patient was referred to neurosurgery but they were lost to follow up as they chose to switch providers.
Discussion
Thyroid angiosarcoma (TAS) has been heralded as a contentious classification, specifically as it is considered a vascular mutation of an anaplastic carcinoma as opposed to a true sarcoma [1].
The World Health Organization’s latest classification of tumors of endocrine organs labeled TAS as a discrete entity under the umbrella of vascular tumors [6].
Contrary to typical presentations of TAS, specific to alpine regions, there have been reports of individuals from non-alpine regions presenting with thyroid angiosarcoma. This contributes to speculation that there are a myriad of etiological factors unknown to us and involved in the pathogenesis of this disease [4].
Within the scope of TAS literature, there seems to be an increasing preponderance of individuals from non-alpine regions presenting with this malignancy. Our patient, with no ties to alpine or mountainous regions in general, serves as a stark reminder of this fact.
De Felice et al. have detailed a total of 61 patients to have been diagnosed with TAS in literature published on this topic [3].
When considering Asia, which is noticeably geographically and environmentally different from alpine regions, there is a reported case of TAS from China. The patient, additionally, also had a pre-existing goiter [1].
This is quite unlike our patient, whose TAS presentation was unusually an incidental finding. Within South Asia, the first reported case of TAS was from Iran. Pakistan, itself, has had no reported cases of TAS, which necessitates the importance of further reporting to expound upon the epidemiological factors of TAS, to better diagnostics, treatment, and management of this condition.
TAS prognosis is poor, particularly due to its rapid spread to cervical lymph nodes, lungs, and bone marrow [7].
It has been known to metastasize to soft tissue, brain, and skin [8].
Metastases to the duodenum and large bowel have also been reported [4].
Our patient has presented with spinal metastases that have not been reported in thyroid angiosarcoma literature. Only one case of thyroid papillary cancer has been reported wherein spinal metastasis is seen [9].
This atypical presentation serves to further augment the literature regarding this sparsely reported condition.
Grossly, this tumor is a singular nodule suffused with blood compressing the thyroid [6].
A cytological analysis can be challenging, due to an inadequate presence of cells and an associated presence of necrosis. A definitive diagnosis is made after a thyroidectomy and an immunohistochemical analysis [4].
Analogous to what is recommended in the literature, this was also done for our patient. An initial small biopsy proved to be too little to make a proper diagnosis, leaving us with an inconclusive diagnosis and a suspicion of malignancy. It therefore became necessary for us to do an immunohistochemical analysis after a large biopsy. In angiosarcoma, cells tend to express endothelial markers (factor VIII; CD31; CD34), at times epithelial markers, and cytokeratin (CK) [5].
Our patient’s immunohistochemistry unveiled the expression of endothelial markers (ERG and CD31), aiding in determining a diagnosis of TAS.
Due to the rarity of this condition, there is little consensus on how a case of thyroid angiosarcoma should be managed. Some papers, however, divulge radiotherapy for angiosarcomas of the head and neck as an adjunctive treatment that has been known to improve survival rates; asserting that chemotherapy alone is not effective [2].
The poor prognosis of TAS has been established in the literature. Collini et al presented six cases with a median follow-up of 59 months. Two of those six patients had local relapses within merely 5 months. These patients had a mortality from the disease that was much earlier than patients who had no such local recurrence [10].
Another case series, maintains local recurrence as a predictor of adverse outcomes, particularly in patients with complete resection of a primary soft tissue sarcoma [11].
Considering how widespread the metastasis of the tumor was and the debilitating nature of TAS, our patient was sent home for palliation.
Conclusion
The paper describes an interesting case of a 63-year-old man presenting incidentally as a case of thyroid angiosarcoma.
Our patient is the first reported case of TAS in Pakistan, and the first worldwide to have associated spinal metastasis.
The unwonted presentation, coupled with the scarcity of scholarship regarding TAS, highlights the import of our reporting.
A myriad of factors can contribute to misdiagnosing TAS, particularly constraints when it comes to knowledge and awareness regarding this rare disease.
Our reported case serves to supplement the discussion regarding this scantily reported malignancy.
Ethical consideration
Before writing the manuscript, written informed consent was taken from the patient and his family to publish his findings anonymously.
Authorship statement
All authors meet the ICMJE authorship criteria.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interests
The authors declare no conflict of interest for this article.
References
- 1.Bala NM, Simões P, Aragüés JM, Veiga R, Guerra S, Valadas C. Non-alpine primary thyroid angiosarcoma. Arch Endocrinol Metab. 2022;66(3):425–428. doi: 10.20945/2359-3997000000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sapalidis K, Kefes N, Romanidis K, Zarogoulidis P, Pantea S, Rogoveanu OC, Rogoveanu I, Vagionas A, Zarampouka K, Tsakiridis K, Kesisoglou I. Thyroid angiosarcoma-rare case or hard to find. Curr Health Sci J. 2020;46(4):433–437. doi: 10.12865/CHSJ.46.04.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kondapalli A, Redd L, DeBlanche L, Oo Y. Primary angiosarcoma of thyroid. BMJ Case Rep. 2019;12(6):e228862–e228862. doi: 10.1136/bcr-2018-228862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benbella L, Elouarith I, Ouazzani HEL, Bernoussi Z, Lahlou MK, Zouaidia F. Thyroid angiosarcoma: a case report and review of literature. Int J Surg Case Rep. 2022;97:107358–107358. doi: 10.1016/j.ijscr.2022.107358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ladurner D, Tötsch M, Luze T, Bangerl I, Sandbichler P, Schmid KW. Das maligne Hämangioendotheliom der Schilddrüse. Pathologie, Klinik und Prognose [Malignant hemangioendothelioma of the thyroid gland. Pathology, clinical aspects and prognosis] Wien Klin Wochenschr. 1990;102(9):256–259. [PubMed] [Google Scholar]
- 6.Lam AK. Pathology of endocrine tumors update: World Health Organization new classification 2017-other thyroid tumors. AJSP Rev Rep. 2017;22(4):209–216. [Google Scholar]
- 7.Goh SG, Chuah KL, Goh HK, Chen YY. Two cases of epithelioid angiosarcoma involving the thyroid and a brief review of non-Alpine epithelioid angiosarcoma of the thyroid. Arch Pathol Lab Med. 2003;127(2):E70–3. doi: 10.5858/2003-127-e70-TCOEAI. [DOI] [PubMed] [Google Scholar]
- 8.Innaro N, Succurro E, Tomaino G, Arturi F. Nonalpine thyroid angiosarcoma in a patient with Hashimoto thyroiditis. Case Rep Oncol Med. 2013;2013:901246–901246. doi: 10.1155/2013/901246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toshkezi G, Galgano M, Libohova S, Marawar S. Isolated spinal metastasis with spinal cord compression leads to a diagnosis of a follicular thyroid carcinoma. Cureus. 2015;7(10):e346–e346. doi: 10.7759/cureus.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collini P, Barisella M, Renne SL, Pizzi N, Mattavelli D, Stacchiotti S, Mattavelli F. Epithelioid angiosarcoma of the thyroid gland without distant metastases at diagnosis: report of six cases with a long follow-up. Virchows Arch. 2016;469(2):223–232. doi: 10.1007/s00428-016-1964-3. [DOI] [PubMed] [Google Scholar]
- 11.Lahat G, Tuvin D, Wei C, Anaya DA, Bekele BN, Lazar AJ, Pisters PW, Lev D, Pollock RE. New perspectives for staging and prognosis in soft tissue sarcoma. Ann Surg Oncol. 2008;15(10):2739–2748. doi: 10.1245/s10434-008-9970-6. [DOI] [PubMed] [Google Scholar]


