Abstract
The rapid advancement of digital health technologies has heightened demand for health data for secondary uses, highlighting the importance of understanding global perspectives on personal information sharing. This article examines stakeholder perceptions and attitudes toward the use of personal health data to improve personalized treatments, interventions, and research. It also identifies barriers and facilitators in health data sharing and pinpoints gaps in current research, aiming to inform ethical practices in healthcare settings that utilize digital technologies. We conducted a scoping review of peer reviewed empirical studies based on data pertaining to perceptions and attitudes towards sharing personal health data. The authors searched three electronic databases–Embase, MEDLINE, and Web of Science–for articles published (2015–2023), using terms relating to health data and perceptions. Thirty-nine articles met the inclusion criteria with sample size ranging from 14 to 29,275. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guidelines for the design and analysis of this study. We synthesized the included articles using narrative analysis. The review captured multiple stakeholder perspectives with an up-to-date range of diverse barriers and facilitators that impact data-sharing behavior. The included studies were primarily cross-sectional and geographically concentrated in high-income settings; often overlooking diverse demographics and broader global health challenges. Most of the included studies were based within North America and Western Europe, with the United States (n = 8) and the United Kingdom (n = 7) representing the most studied countries. Many reviewed studies were published in 2022 (n = 11) and used quantitative methods (n = 23). Twenty-nine studies examined the perspectives of patients and the public while six looked at healthcare professionals, researchers, and experts. Many of the studies we reviewed reported overall positive attitudes about data sharing with variations around sociodemographic factors, motivations for sharing data, type and recipient of data being shared, consent preference, and trust.
Introduction
Background
The rapid advancement of health technologies and subsequent growth in sharing of health data for secondary uses has been widely recognized for its potentially transformative role in strengthening health systems, enhancing healthcare outcomes, and improving the efficacy of medical research [1–3]. Personal health data–collected in the form of routine clinical care or medical research, for instance–can be utilized to monitor population health at a local level, identify groups at risk of disease within a country, or measure progress in health and development on a global scale [4]. Evidence of potential breakthroughs include speeding up diagnoses and improving treatment in fields such as cancer, cardiovascular diseases, and rare diseases [3,5–9]. User-generated data collected through wearable consumer devices could help personalize and improve the management of cardiovascular diseases on multiple levels, ultimately resulting in better outcomes on both an individual and a population-wide scale [6]. Furthermore, COVID-19 has acted as a catalyst for digital transformation, accelerating the adoption of digital technologies across various health sectors [10–12]. This surge is largely due to the need for remote operations and services amid social distancing measures and lockdowns. Businesses and healthcare providers swiftly shifted towards online platforms to continue their operations, leading to a rapid integration of digital tools [10]. The pandemic has also spurred innovations in digital health services, such as telemedicine and remote monitoring, highlighting the essential role of technology in managing public health crises [10,11]. This trend in health data sharing has resulted in potentially long-lasting positive effects on medical research and routine health-care delivery [12–14].
Despite potential benefits, evidence reveals concerns around sharing personal information–such as community perceptions about technology use and perceived risks and benefits of sharing data [15–22]. As health technology becomes increasingly pervasive in healthcare, the expanding use of potentially invasive technologies–continuous user-generated data collected through smartwatches and blood glucose monitoring devices, for example–is likely to lead to greater concerns among users, exacerbating existing problems with willingness to use new technologies [23]. For example, Simpson and colleagues’ narrative review highlights trust and privacy concerns as barriers to the sharing of patient-generated data across multiple settings. In addition, healthcare provider perceptions of a technology are likely to affect treatment delivery, especially if it is not considered sufficiently acceptable [21]. Health data are classified as sensitive personal data that require a high safety and security standard [24]. Improving transparency and standardization of data use can affect user perceptions. Therefore, there is a need to follow principles, such as the ‘FAIR Guiding Principles for scientific data management and stewardship’ to ensure data is findable, available, interoperable, and reusable [25].
Given the fast-paced changes within the field of health technology and data generation, this article reviews current literature around various stakeholder–such as the public, patient, healthcare provider, researcher, and policymaker–perspectives on sharing personal health data as well as identify up-to-date barriers and facilitators within the field.
Our article builds on previous reviews that have explored various aspects of health data sharing through an updated search of current evidence in the post-pandemic era. For example, van Panhuis and others described barriers to sharing routinely collected public health data; identifying six categories including motivational, economic, and ethical [4]. Similarly, Husedzinovic and colleagues reviewed the ethical preferences, revealing that patients often preferred a one-time general consent and needed detailed information on privacy protections [17]. A 2018 scoping review looking more broadly at trust in digital health systems identified trust enablers–such as altruism, ease of use, and sociodemographic factors–and impediments–cost, limited accessibility, and fear of data exploitation [26]. Another 2018 review examined the advantages and drawbacks of data sharing, emphasizing the crucial roles of consent and trust [27]. Esmaeilzadeh and Sambasivan (2017) identified seven factors influencing patient attitudes towards health information exchange, including perceived benefits and concerns, and patient characteristics and preferences. In an academic context, Perrier et al. (2020) point out practical challenges to effective data sharing, such as time constraints, resource shortages, lack of skills among researchers, and infrastructure deficits. Given the changing landscape of health technologies, our review provides an opportunity to explore current barriers and facilitators influencing multiple stakeholder perceptions of health data sharing as well as gaps in the research.
Research objectives
The aim of this article is to review stakeholders’ perceptions and attitudes towards sharing personal data to inform personalized treatments, interventions, and research. We highlight conditions influencing perceptions in the field of health data sharing–such as sociodemographic characteristics, motivational factors, privacy concerns, and trust–as well as gaps in research.
Methods
We designed and implemented this review using guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) checklist as presented in S1 Appendix [28]. This review was not registered.
Search strategy
The authors searched three relevant electronic databases–Embase, MEDLINE, and Web of Science–for peer-reviewed empirical articles using search terms relating to digital health (e.g. mHealth, eHealth, technology, health data, telemedicine, telehealth, mobile applications, smartphone, wearables devices, health information technology, personalized medicine, precision medicine, personal digital assistant, smartphone, big data), perceptions (e.g. perception, trust, confidence, hesitancy), and research type (e.g. qualitative, quantitative, interview, survey). Additionally, we searched citations of identified articles. The authors conducted the search in English and included all articles from 2015 to 2023 in order to incorporate the most relevant and up-to-date evidence from the past decade as this era reflects critical advancements in the development and widespread use of digital health technology. We ran the search on 6 January 2023.
After deduplication using EndNote, two reviewers screened titles and abstracts of the identified records to determine their eligibility based on the predefined inclusion and exclusion criteria. Full-text articles were obtained for all potentially eligible studies and further assessed for inclusion. Any discrepancies between the reviewers were resolved through discussion and consensus, with the involvement of a third reviewer where necessary. The full search strategy for each database is presented in S2 Appendix.
Inclusion and exclusion criteria
Studies were considered eligible for inclusion if they met the following criteria:
Peer-reviewed research papers
Published between 1 Jan 2015 and 1 Jan 2023
Available in English
Empirical studies with primary data (quantitative, qualitative, or mixed)
Address any forms of data sharing such as secondary use of research data already collected, health records, biobank data, big data collected from wearable accessories and other devices or data linkage etc.
Examine attitudes of research participants, patients, members of the public, healthcare professionals
Studies were excluded if they did not meet these criteria or were opinion pieces, editorials, commentaries, or reviews.
Data extraction and synthesis
Data extraction was performed by two reviewers using a standardized data extraction form. From each article, we documented the following: author name, year of publication, country of origin, sample size, study design (e.g. qualitative or quantitative), study population, type of data shared, main findings (including barriers and facilitators to data sharing). S3 Appendix provides the coding framework designed by the authors for data extraction.
The authors employed a descriptive and narrative approach to analyze and present the findings from the included studies. This approach involved identifying common themes and patterns across the studies related to the barriers and facilitators of personal health data sharing. We then synthesized the findings and discussed these in relation to the research objectives, considering the perspectives of different stakeholder groups and the global context of personal health data sharing. We identified the barriers and facilitators to data sharing by charting the key issues reported from each study. As part of data extraction, the results section of each study was reviewed to identify various stakeholder priorities, perspectives, expectations, perceptions, and attitudes toward a particular digital health technology or service.
Quality Appraisal
Given its exploratory nature, the authors did not conduct a formal quality appraisal of the included studies for this scoping review. Nonetheless, the methodological rigor and relevance of each study were considered during data extraction and synthesis to ensure that the review findings were based on credible evidence.
Conceptual framework
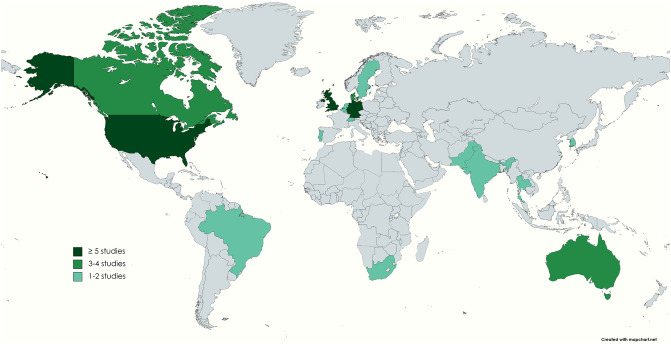
We adapted digital environment elements within the “framework for digital health equity” to create a conceptual framework identifying perceptions of personal health data sharing [29,30]. Our framework–shown below in Fig 1 –incorporates personal, technological, institutional, economic, political, legal, and ethical barriers and facilitators identified in previous reviews [4,26]. The authors utilized this framework to synthesize and present findings from the studies included in this article as this captures key determinants within digital health.
Fig 1. Conceptual framework to identify perceptions of personal health data sharing.
Adapted from Esmaeilzadeh and Sambasivan [30] and Richardson, Lawrence [29].
Results
Search outcome
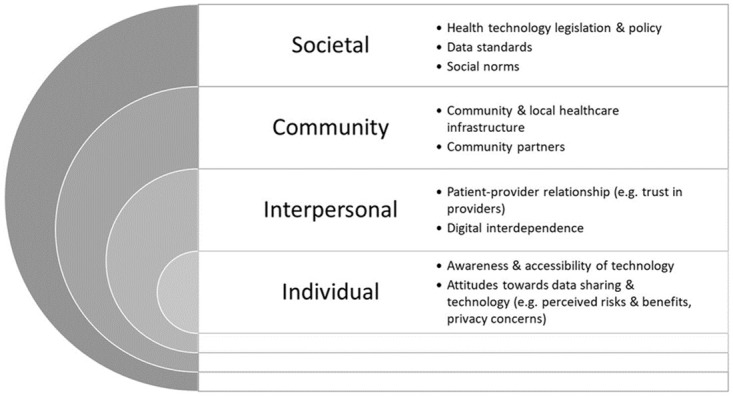
The authors carried out the search on 6 January 2023 and, after deduplication, we identified 1640 citations. Following title and abstract screening of all citations, PA and AB retrieved 52 articles and included these in the full-text screen. Of these, 39 met the inclusion criteria and were considered in our final analysis (Fig 2). One of the 13 excluded articles were later retracted and, therefore, removed from our review [31].
Fig 2. Flow diagram of study selection process.
Study characteristics
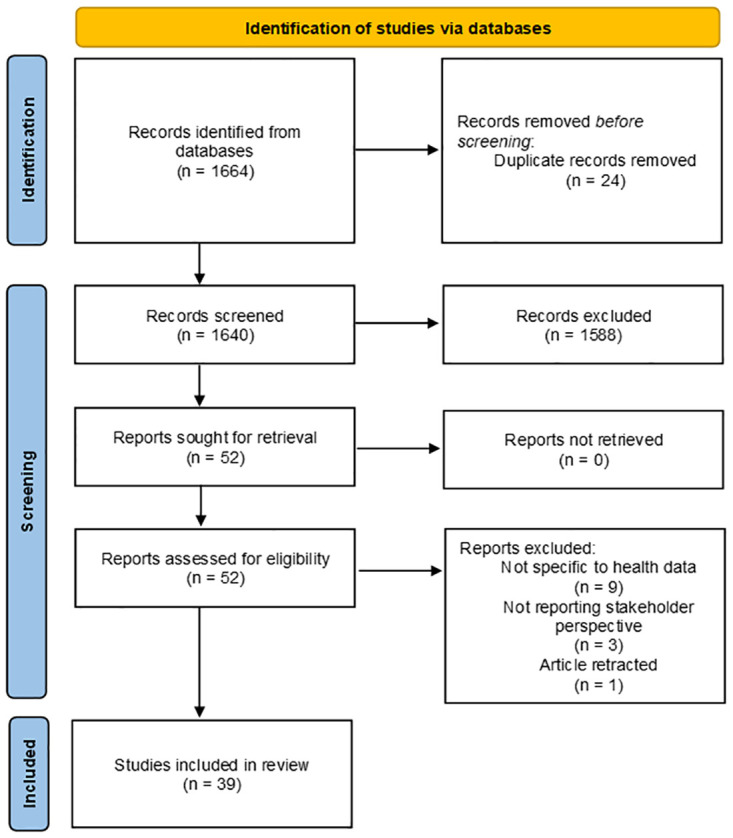
The sample size of the 39 included studies sample size ranged from 14 [32] to 29,275 [33]. Many of the studies had a higher percentage of participants over the age of 40 (n = 21) compared with studies including a higher percentage of those below the age of 40 (n = 4). Most of the included studies were based in high-income countries within North America and Western Europe. The top six most studied countries were the United States (n = 8), the United Kingdom (n = 7, including two multi-country studies), Germany (n = 5), Australia (n = 3), Canada (n = 3), and Denmark (n = 3 multi-country studies). Brazil, India, Pakistan, Thailand, and South Africa represented the only low- and middle-income countries included in our review. Fig 3 illustrates the geographical coverage of the included articles.
Fig 3. Geographical coverage of included articles on health data sharing perspectives.
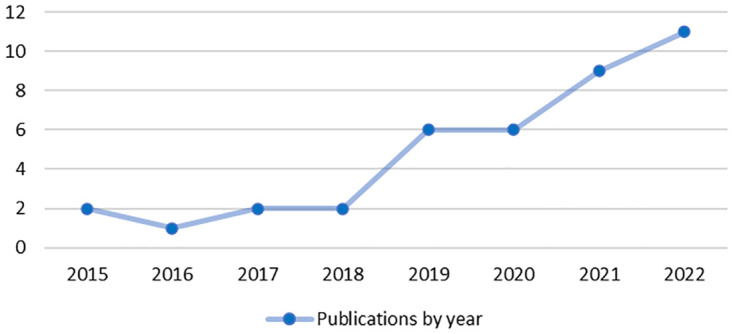
Of the 39 articles included, the greatest number was published in 2022 (n = 11, 28%) and 2021 (n = 9, 23%) with only seven articles (18%) published prior to 2019 (Fig 4). The majority of included studies used quantitative methods (n = 23, 59%) and twelve used qualitative methods (n = 12, 31%). The four remaining articles used both quantitative and qualitative methods (10%). All studies except one [34] utilized a cross-sectional design.
Fig 4. Distribution of publications by year (2015–2022).
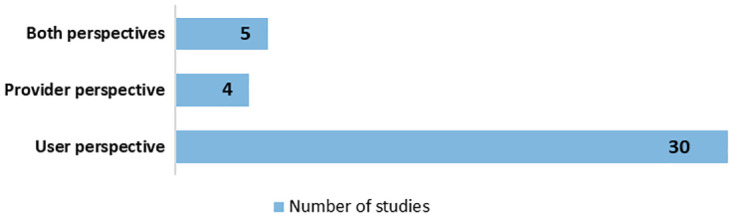
Most of the included studies (n = 34, 87%) looked at one specific type of stakeholder perspective while the remaining five studies (13%) engaged with multiple stakeholder perspectives in their research. Overall, 29 studies (74%) examined the perspectives of ‘user-side’ stakeholders–including patients and the public. Four studies (10%) looked specifically at ‘provider-side’ perspectives–such as researchers and healthcare practitioners–while a further five studies (13%) incorporated both opinions (Fig 5). The perspectives of patients (n = 15) and the public (n = 13) were the most studied followed by healthcare professionals, researchers, scientists, and experts (n = 11). Eighteen studies focused on health conditions such as cancer (n = 4), mental health (n = 4), chronic health conditions (n = 4) or rare diseases (n = 2).
Fig 5. Stakeholder perspectives covered across all included studies.
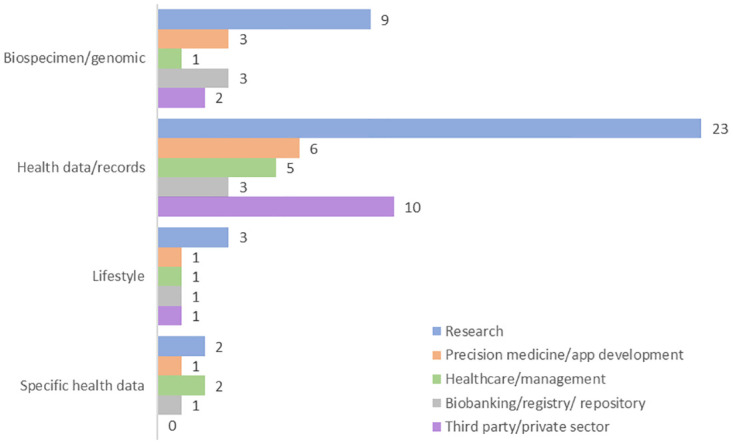
Most studies included information on health data and records (n = 33, 66%) and/or biospecimen or genomic data (n = 10, 19%). In terms of the purpose of shared data, many of the studies focused on secondary data use for research (n = 26, 50%) and/or the private sector (n = 10, 19%). Fig 6 summarizes the type and use of data sharing as reported by included studies.
Fig 6. Trends in type of health data shared by use of data shared.
Tables 1 and 2 below summarize study characteristics as well as type and recipient/purpose of data being shared across all 39 included studies.
Table 1. Summary of study characteristics for included articles.
| First author, year | Country | Topic | Type of health data | Health condition | Research design | Methods | Study population | Age a | Sample size |
|---|---|---|---|---|---|---|---|---|---|
| Cheah, 2015 | Thailand | Stakeholders’ attitudes and experiences about good data sharing practice | Health data for clinical research | - | Qualitative |
- Interview - Focus group |
- Researchers - Community representatives |
Not Reported |
25 |
| Sheikh, 2017 | - Pakistan - Denmark |
Unpacking trust within research participation | Blood sample and health data for genomic research | - | Qualitative | Interview | Research participants | Not Reported |
48 |
| Hate, 2015 | India | Ethical data sharing practice in research involving women and children in urban India | Demographic/ household details, images/videos, and medical records for research | - | Qualitative | - Semi-structured interview - Focus group |
- Researchers - Research participants |
Not Reported |
66 |
| Staunton, 2021 | South Africa |
Stakeholder perspectives on protection of personal health information | Health data for research | - | Qualitative | Semi-structured Interview |
- Doctors - Scientists - Government representatives |
Not Reported |
19 |
| Barnes, 2020 | Canada | Patient perspectives on biobanking | Genomic and personalized health data for research | Stroke | Quantitative | Survey (electronic) |
Patients | 47% 69 | 196 |
| Wiesner, 2018 | Germany | Motivational and privacy aspects of wearable technology used by active citizens | Activity health data | - | Quantitative | Survey | Runners | ≥16 | 845 |
| Vilaza, 2021 | - Denmark - Brazil |
Public attitudes towards digital health repositories | Health data for digital health research repository | - | Quantitative | Survey | Public | 58% 18–27 29% 28–37 |
1600 |
| Kim, 2020 | South Korea |
Public attitudes towards precision medicine | Clinical data, specimens, genetic data, environmental and lifelog data for research and precision medicine | - | Quantitative | Survey (online) |
Public | 26% 50–59 20% 40–49 19% ≥60 |
1500 |
| Lysaght, 2021 | Singapore | Public trust in data sharing for precision medicine | Health data for precision medicine | - | Quantitative | Survey | Public | 40% 40–59 33% 21–39 27% ≥60 |
1000 |
| Nwebonyi, 2022 | Portugal | Public views on health data sharing, access and (re)use | Medical records, genetic and phenotypic data for research and development | Rare diseases |
Quantitative | Survey | - Patients - Informal carers |
58% <18 (patients) 87% >30 (carers) |
651 |
| Braunack-Mayer, 2021 | Australia | Public attitudes of sharing government health data with private sector | Government health data for research and development | - | Quantitative | Survey (online) |
Public | 20% <29 35% 30–49 25% 50–64 18% ≥65 |
2537 |
| Zhang, 2021 | USA | Privacy concerns and data value of mobile mental health systems | Mental health data to improve mental illness management | Mental health |
Quantitative | Survey (online) |
Members of online mental health communities | 42% 26–30 28% 18–25 25% 31–35 |
170 |
| Zhang, 2022 | USA | Public attitudes towards pharmacogenomic testing and statewide database | Pharmacogenomic data for clinical and research purposes | - | Quantitative | Survey (electronic) |
Public | Median: 42–53 | 808 |
| Young, 2022 | USA | Expert perspective on data elements in routine care of patients | Physical function in medical records data to improve care | - | Mixed | - Focus group - Longitudinal eDelphi survey |
- Healthcare experts - Patients |
Mean: 24 (experts) ≥65 (patients) |
26 |
| Wetzels, 2018 | Netherlands | Patient perspectives on health data privacy and management | Health and lifestyle data for healthcare | Cardiac condition | Qualitative | Focus group | Patients | Mean: 67 | 23+5 FGDs |
| Gotzl, 2022 | Germany | Stakeholder perspectives on mobile mental health apps for young people | Personal data to inform mental health app | Mental health |
Mixed | - Focus group - Survey |
- Young adults - Experts |
16–25 | 667+16 FGDs |
| Hutchings, 2022 | Australia | Patients attitudes towards re-use of administrative and clinical trial data | Health and clinical trial data to improve patient care | Breast cancer | Quantitative | -Survey - Interview |
Patients | 43% >65 34% 55–64 23% <54 |
132 |
| Hartmann, 2019 | Germany | Attitudes towards mobile app to self-monitor and manage depression | Health data to inform mobile app | Mental health (depression) |
Quantitative | Survey (online) |
Patients | Mean: 38 | 998 |
| Trinidad, 2020 | USA | Public comfort with sharing health data with third-party commercial companies | Health data sharing with third-party commercial companies | - | Quantitative | Survey | Public | 31% >60 12% 18–29 |
1841 |
| Tosoni, 2022 | Canada | Patient consent preferences on sharing personal health information during COVID-19 | Health data for research and commercial purpose | Cancer | Mixed | - Survey - Focus group |
Patients | Pre-, post-Covid 59%, 76% 50–74 |
417 |
| Tosoni, 2019 | Canada | Patient consent preferences on sharing personal health information with academic healthcare institution | Health data for research | Cancer | Quantitative | Survey | Patients | 59% 50–74 | 222 |
| Summers, 2022 | UK | Public willingness to share data in the context of COVID-19 | Health data for healthcare services | Chronic health conditions | Mixed | Survey (online) |
Public with chronic health conditions | 65% 55–74 | 4764 |
| Spencer, 2016 | UK | Patient perspectives on the use of anonymized health data for research | Health data for research | Chronic health conditions | Qualitative | - Interview - Focus group |
Patients | Mean: 61 | 40 |
| Pletscher, 2022 | Switzerland | Public willingness to share anonymized routinely collected clinical health data | Health data for research | Chronic health conditions | Quantitative | Survey (online) |
- Public - Patients |
Public, patients: 35%, 21% 18–39 43%, 49% 40–64 22%, 30% >64 |
1231 |
| Hassan, 2020 | UK | Public attitudes towards sharing genomic data within NHS | Genomic data for clinical care | - | Qualitative | Focus group | - Patients and family - Public |
- 16–18 (patients) - ≥18 (public) |
44 |
| O’Brien, 2019 | USA | Patient perspectives on linkage of health data | Health data for research | Multiple conditions | Quantitative | Survey (online) |
Patients | 69% 40–65 | 3516 |
| Ostherr, 2017 | USA | Trust and privacy in the context of user-generated health data | Health data used outside clinical settings | - | Qualitative | Semi-structured interview |
- Researchers - Health startups - Public |
Not Reported |
32 |
| Ivanova, 2020 | USA | Mental health professionals’ views on patient-controlled data sharing | Health records for consent | Mental health |
Qualitative | Semi-structured interview |
Healthcare professionals (HCP) | Not Reported |
20 |
| Johansson, 2021 | - UK - Norway - Iceland - Sweden |
Public preferences for health data sharing | Digital health data for policymaking | - | Quantitative | - Discrete choice experiment |
Public | Mean: 48–50 | 1967 |
| Shah, 2019 | - Denmark - Sweden - Netherlands - UK |
Participants’ views about data governance post-project | Health data for post-project sharing | Diabetes | Quantitative | Survey | Research participants | 73% ≥61 | 855 |
| Schults, 2019 | Australia | Healthcare practitioner perspectives and experiences of vascular access device data | Vascular access data for clinical quality registry | - | Qualitative | Semi-structured interview |
Healthcare practitioners | Not Reported |
19 |
| Richter, 2021 | Germany | Patient attitude towards data-donation for medical research | Health data for medical research | - | Quantitative | Survey (online) |
Patients | - Survey 1,2: 51–65 29%, 36% (men) 32%, 34% (women) |
508 |
| Amorim, 2022 | Portugal | Perceived benefits and risks of sharing genomic data for research | Genomic data for clinical research | Rare diseases |
Quantitative | Survey (online) |
- Patients - Informal carers - HCP |
56% <18 (patients) 75% 30–49 (carers) 54% >49 (HCP) |
700 |
| Brall, 2021 | Switzerland | Public willingness to participate in personalized health research and biobanking | Health data and biological samples for health research and biobanking | - | Quantitative | Survey (online) |
Public | 20% 55–64 18% 45–54 17% 65-74b |
5086 |
| Broes, 2020 | Belgium | Patients’ attitudes towards re-use of clinical trial samples and data | Health data and blood samples and tumor tissue | Cancer | Qualitative | Interview | Patients | Not Reported |
16 |
| Brown, 2022 | UK | Patients’ attitudes and experiences data sharing | Health and lifestyle data | Chronic health conditions | Qualitative | - Interview - Card sorting |
Patients | Mean: 42 | 14 |
| Buhr, 2022 | Germany | Public attitudes towards data sharing through mobile apps for pandemic research | Test results, contact tracing data, fitness data for research | - | Quantitative | Survey (phone) |
Public | 20% 50–59 19% 40–49 18% ≥70 17% 18–30 |
924 |
| Jones, 2021 | UK | Public opinion on data sharing preferences | Mental and physical health data for research | - | Quantitative | Survey (online) |
- Patients - Carers - Public |
23% 55–65 22% 45-54b |
29,275 |
| Kim, 2019 | USA | Patient perspectives on sharing medical data and biospecimens for research | Health records and biospecimens for research | - | Quantitative | Survey | Patients | Mean: 51 | 1246 |
a: Mean/median age or age range as reported in included articles and rounded up to nearest percentage; a: Percentages calculated from reported proportions by authors.
Table 2. Type and use of health data investigated across included studies.
| First author, year | Type of health data | Use of health data | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Biospecimen/ genomic | Health data and records | Lifestyle | Specific health data |
Research | Precision medicine/app development | Healthcare services/ patient care | Health management | Biobanking/ registry/ repository | Third party/ private sector | |
| Cheah, 2015 | No | Yes | No | No | Yes a | No | No | No | No | No |
| Sheikh, 2017 | Yes | Yes | No | No | Yes | No | No | No | No | No |
| Hate, 2015 | No | Yes | No | No | No | No | No | No | No | No |
| Staunton, 2021 | No | Yes | No | No | Yes | No | No | No | No | No |
| Barnes, 2020 | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes |
| Wiesner, 2018 | No | No | Yes | No | No | No | No | No | No | No |
| Vilaza, 2021 | No | Yes | No | No | Yes | No | No | No | Yes | No |
| Kim, 2020 | Yes | Yes | Yes | No | Yes | Yes | No | No | No | No |
| Lysaght, 2021 | No | Yes | No | No | No | Yes | No | No | No | Yes |
| Nwebonyi, 2022 | Yes | Yes | No | No | Yes | Yes | No | No | No | No |
| Braunack-Mayer, 2021 | No | Yes | No | No | Yes | Yes | No | No | No | Yes |
| Zhang, 2021 | No | Yes | No | Yes | No | No | No | Yes | No | No |
| Zhang, 2022 | Yes | No | No | No | Yes | No | No | No | No | No |
| Young, 2022 | No | Yes | No | No | No | No | Yes | No | No | No |
| Wetzels, 2018 | No | Yes | Yes | No | No | No | Yes | No | No | Yes |
| Gotzl, 2022 | No | Yes | No | Yes b | No | Yes | No | No | No | No |
| Hutchings, 2022 | No | Yes | No | Yes c | No | No | Yes | No | No | No |
| Hartmann, 2019 | No | Yes | No | No | No | Yes | No | No | No | Yes |
| Trinidad, 2020 | No | Yes | No | No | No | No | No | No | No | Yes |
| Tosoni, 2022 | No | Yes | No | No | Yes | No | No | No | No | Yes |
| Tosoni, 2019 | No | Yes | No | No | Yes | No | No | No | No | No |
| Summers, 2022 | No | Yes | No | No | No | No | Yes | No | No | No |
| Spencer, 2016 | No | Yes | No | No | Yes | No | No | No | No | No |
| Pletscher, 2022 | No | Yes | No | No | Yes | No | No | No | No | No |
| Hassan, 2020 | Yes | No | No | No | No | No | Yes | No | No | No |
| O’Brien, 2019 | No | Yes | No | No | Yes | No | No | No | No | No |
| Ostherr, 2017 | No | Yes | No | No | Yes d | No | No | No | No | Yes |
| Ivanova, 2020 | No | Yes | No | No | Yes e | No | No | No | No | No |
| Johansson, 2021 | No | Yes | No | No | Yes f | No | No | No | No | No |
| Shah, 2019 | No | Yes | No | No | Yes g | No | No | No | No | No |
| Schults, 2019 | No | No | No | Yes h | No | No | No | No | Yes | No |
| Richter, 2021 | No | Yes | No | No | Yes g | No | No | No | No | Yes |
| Amorim, 2022 | Yes | No | No | No | Yes | No | No | No | No | No |
| Brall, 2021 | Yes | Yes | No | No | Yes | No | No | No | Yes | No |
| Broes, 2020 | Yes | Yes | No | No | Yes | No | No | No | No | No |
| Brown, 2022 | No | Yes | Yes | No | Yes | No | No | No | No | No |
| Buhr, 2022 | No | No | Yes | Yes i | Yes | No | No | No | No | No |
| Jones, 2021 | No | Yes | No | Yes j | Yes | No | No | No | No | No |
| Kim, 2019 | Yes | Yes | No | No | Yes | No | No | No | No | Yes |
a: Clinical research;
b: Data around mental health;
c: Clinical trial data;
d: Research outside clinical settings;
e: Research on consent;
f: Research to inform policymaking;
g: Including secondary data sharing;
h: Vascular access data;
i: COVID-19 test results and contact tracing information;
j: Mental and physical health data.
Perspectives on data sharing
Most of the studies we reviewed reported overall positive stakeholder attitudes about data sharing with certain factors impeding or facilitating willingness to share. Across the studies, we identified variations in perspectives on data sharing based on sociodemographic characteristics, motivational factors, ethical and privacy concerns, and differing levels of trust. Table 3 highlights the key factors we identified through narrative analysis as well as the level of influence, as outlined earlier in our conceptual framework.
Table 3. Summary of factors influencing stakeholders’ perceptions of sharing personal health data identified in included studies.
| Level of influencea | Factors | Description & references | |
|---|---|---|---|
| Individual | Sociodemographic characteristics b | ||
| Age | - Variations between age groups: both younger age groupsc [35–38] and older age groups willing to share data [39–41] | ||
| Gender | - Variations by gender: men more likely to share data in different settings [39,42] | ||
| Education | - Variations between education level: more educated more willing to support data sharing for health [35–39,43] | ||
| Motivational factors for data sharing | |||
| Altruism | - Willingness to share data when this is perceived to help others [36,44–48] | ||
| Health conditions | - Willingness to share data when this is perceived to help with personal health condition [32,44,49,50] | ||
| COVID-19 experiences | - Willingness to share data increased during/post COVID [51–53] | ||
| Interpersonal | Ethics and privacy concerns | ||
| Consent preference | - No consensus on best approach to obtain consent but general support across stakeholder groups for one-time consent over explicit consent with some concerns [47,50,54–56] | ||
| Privacy concerns | - Main privacy concerns expressed by all stakeholder groups included lack of transparency, patient rights, privacy breaches, misuse of sensitive and identifiable data, and discrimination against individuals with stigmatized diseases [36,39,47,52,54,56–58] | ||
| Levels of trust | |||
| Trust in providers | - High levels of institutional trust (e.g. sharing data with government) [44,48,53,55] | ||
| Type of data shared | - Less willingness to share identifiable data than anonymized data, and lifestyle data than medical data [47,49–51,58,59] | ||
| Recipient of data shared | - More willingness to share data with research institutions and universities than commercial, private, or third-party entities according to multiple stakeholders [40,49,52,55,59,60] | ||
a Individual and interpersonal levels of influence overlap for ethics and privacy concerns;
b Based on data reported for public/patients;
c As defined and reported by the authors of the studies included in this review.
Sociodemographic characteristics
Results varied across the studies that analyzed the association between sociodemographic characteristics and willingness to share personal health data. Age, education, and gender were among the key sociodemographic characteristics associated with personal health data sharing attitudes. For example, six studies found that more educated participants were more willing to share data [35–39,43], while seven studies reported significant variations by age [35–41] and two by gender [39,42]. It is noteworthy that most of the studies incorporating provider perspectives–such as those of researchers and physicians–did not provide sociodemographic delineations for their participants. For example, two qualitative studies of researchers in Thailand and the US did not report the age of participants [54,61].
Motivational factors
Participants across several studies stated that altruistic benefits of data sharing health outweighed the risks. All stakeholders suggested identified helping others, helping future patients, discovering a cure for untreatable disease or development of effective treatments, and promoting scientific progress as motivators for sharing personal health data [36,43,45,46,48,54,55].
Furthermore, participants with health conditions were supportive of sharing their own health data to improve treatments. For example, nearly 98% of stroke patients in a Canadian study said they would be willing to provide a blood sample to help develop a blood test for stroke. In another multi-country study, 97% of diabetic patients interviewed were supportive of their data being shared for secondary use [60]. O’Brien and colleagues reported that 94% of patients in their US-based study were willing to share health data to help their doctors make better decisions and make new therapies available faster [62].
Experiences of the COVID-19 pandemic also appeared to be a motivating factor for sharing personal health data. A significant proportion of people felt that their own attitudes had shifted due to the COVID-19 pandemic. More people reported being comfortable with sharing private health data with any organization during rather than before the COVID-19 pandemic. More people reported being comfortable with sharing anonymized data than personally identifiable data. Around 67% disagreed or strongly disagreed with sharing their private health data without anonymization [51]. Willingness to share data also varied depending on who the data would be shared with (e.g. government, researchers, health system), highlighting trust as a key determining factor regarding who may have access to shared personal health data and how it may be used in the future [51].
Three studies–based in Canada, the UK, and Germany–looked specifically at the impact of COVID-19 as well as the use of pandemic apps and public willingness to share personal health data [51–53]. More participants reported being comfortable with sharing personal health data during the COVID-19 pandemic rather than before [51]. A significant proportion of people felt that their own attitudes had shifted as a result of the pandemic with more people reported being comfortable with sharing private health data with any organization during rather than before the pandemic.
A Canadian study of cancer patients found that during the pandemic, patients were more comfortable sharing data with all parties (90% vs 79%, p = 0.009), except with commercial entities [52]. In a Germany study exploring the use of pandemic apps, an overwhelming majority (84%) of smartphone users were willing to provide their app data for state-funded research and almost all app users (97%) stated they were willing to share data, while 74% of nonusers supported data sharing via an app [53].
On the other hand, there were concerns around privacy and use of identifiable health data during COVID-19. A UK-based study of chronic health patients found that, post-COVID, almost half of respondents were concerned or very concerned about who would have access to their personal health data in the context of the pandemic and how their personal health data may be used in the future [51].
Ethical and privacy concerns
Of the studies that explored ethics and consent preferences, there was more overall acceptance rather than opposition for sharing data without explicit consent from both users and providers. For example, 76% of participants in a UK study were willing to share data without explicit consent versus 20% who opposed this [33]. Similarly, a Singapore study reported 64% of participants were willing to share de-identified health data with institutions without consent for each study [55]. At the same time, Lysaght and others concluded that the users and uses of data influenced public trust and willingness to share data than either the sensitivity of the data or the consent procedures in Singapore [55]. In another study surveying runners in Germany, 42% stated that they were not concerned if data might be shared without their consent while 35% would not accept sharing data without their consent [42]. At the same time, transparency was strongly desired, particularly with commercialization of data being shared [48,52,56]. Transparency of data used as well as better understanding of data protection was also highlighted by healthcare providers and scientists in a South African study [63].
Participants across various studies predominantly expressed concerns over potential misuse of data, lack of transparency in the process, and sharing of identifiable and sensitive data [36,39,47,52,54,56–58]. For example, participants in a multi-country study were very concerned their data being used in unethical projects (76%), profit making without consent (69%), and cyberattacks (66%) [47]. Researchers and healthcare professionals in Thailand, India, South Africa, and Portugal expressed their concern over data protection and the potential risk of data breaches [45,54,56,63]. The Indian study also highlighted participants’ skepticism around the use of data to harm participants or meet vested interests [56]. Another study examining public comfort with sharing health data with third-party commercial companies revealed that as privacy concerns increased, comfort with sharing health data with third-party commercial companies decreased [38].
Trust
"I’m generally quite trustful of hospitals and GPs [general practitioners]"
- Interviewee [48]
Several included studies investigated the role of trust in data sharing preferences. Overall trust in governmental/public, or government-funded research institutes and organizations was much higher than trust in private organizations–such as private clinics and health insurance companies [40,49,52,53,55,59,60]. On the other hand, researchers in a US-based study perceived that individuals were more resistant to sharing health data for scientific studies compared with companies that sold the devices and apps they used [61]. Overall, there was significant distrust of private health data use by social media platforms (e.g. Facebook and Twitter). For example, Zhang and others reported that most respondents in their US-study trusted health professionals (78%) and researchers (73%) to keep their data private [37]. A 2021 Singapore study also found that respondents most trusted public health institutions and hospitals and that Facebook was the least trusted institution [55]. Most patients and carers surveyed in a Portuguese study perceived trust in research institutions and trust in research teams as very important issues when making decisions about sharing data [64]. Furthermore, participants in the same study who considered trust in research institutions as very important rated higher the importance of being involved in decisions about data sharing, data access, data use, and data reuse [64].
While most studies indicated that people trust their data with the government and health organizations, two studies based in India and South Africa found that respondents were skeptical about sharing personal health data [56,63]. For instance, Staunton and colleagues reported that historical exploitative research, inequitable collaborations, and historical use of biological data has resulted in resistance among many in South Africa to the sharing of personal health data [63].
Types of recipients that participants trusted to share their personal health data with also depended on the type of data being shared. For instance, a study of the German running community found that runners preferred to exchange tracked data with recipients they trusted such as friends (52%), family members (43%), or a physician (32%) [42]. However, another German study surveying mental health patients suggested a low preference (13%) for sharing personal health data with friends [65].
“It is very unclear how the commercial side of health care remains separated from the actual care with these systems.”
- Patient [59]
Most studies that explored the purpose of data being shared found that respondents had a low preference towards sharing health data with insurance companies [49,55,65]. For example, patients interviewed in a Canadian study suggested that they were less supportive of data sharing if a commercial entity was the recipient of the health information (53%) compared with nonprofit organizations such as universities (87%) [49]. Two study showed participants were ambivalent about sharing their health data with commercial actors [61,66].
Discussion
Most studies included in this review reported generally positive perspectives around data sharing from different stakeholders with participants identifying altruism and the development of effective treatments as key motivators for sharing personal health data. Overall, findings from our review suggest relatively higher trust in public or government-funded research institutes and organizations than in private organizations–such as insurance companies, social media companies, and other commercial companies. This is in line with existing global evidence towards widespread general support for data sharing for research purposes [2,67]. Despite evidence of predominantly supportive views towards data sharing, studies also noted concerns around data privacy through data breaches and misuse of data, a lack of trust in commercial use of data, and skepticism around the supposed benefits of data sharing [68].
Research gaps and further research
Our review suggests research on health data sharing in low- and middle-income countries is markedly limited. Data sharing research was geographically concentrated in North America and Western Europe, as previous reviews have illustrated [67]. As a result, there is also a lack of analysis that considers diverse demographic characteristics. Moreover, the majority of studies are cross-sectional, with an absence of standardized studies that span multiple countries or emphasize changes over time. Further comparable research across diverse settings is required to build on current evidence, especially to understand variations between data sharing within high-income countries and low- and middle-income countries (LMICs) [69].
Much of the existing research centers on individual perspectives, primarily examining the views of existing patients. Of the nine studies that engaged with ‘providers’–including healthcare providers, researchers or experts–most did not contextualize or position perceptions from a patient/public-provider relational viewpoint. This leaves out broader layers of analysis, like the interpersonal, community, and societal levels of the digital environment and trust. Key areas–such as technology biases, healthcare infrastructure challenges, and policy implications related to technology–are often sidelined, as highlighted by Richardson et al. (2022). This research gap becomes even more pertinent given that reviewed studies identified institutional trust as a key factor influencing attitudes towards data sharing. How does trust play out across broader healthcare settings and what are some intersecting systemic concerns, for example?
Another similar gap in the research relates to variations in access across different regions, in-country settings, and across sociodemographic groups. As the scope of the included studies did not extend to investigating attitudinal variations across subgroups, none of the studies examine how access to technology may impact attitudes towards equitable data sharing [69]. How would trends in adoption and access to technology–such as limited use of mobile phones by women in rural central India, for example [70]–be reflected in attitudes towards data sharing? In other words, what type of data is being collected, from whom, at what cost, and for whose benefit? There is an absence of comprehensive cost-benefit analyses, signaling an area ripe for further investigation.
There is an urgent need to address the challenges LMICs face when trying to integrate digital health technologies [24]. Further research is essential to address challenges ranging from the need for supportive environments and resources, to infrastructure development for digital transitions, and to improvements in education and capacity building [24,69]. Other challenges to address include internet connectivity, updating older infrastructure, navigating technology ownership issues, and handling concerns related to privacy, security, and the application of global standards [24]. For example, routine health information data represent an underused source of data and could be made more available and further embraced by the research community in LMIC health systems [71].
The rapid rate of development in precision medicines highlights that staying current with research in digital health is essential. There is a pressing need to gather globally comparable evidence that delves into perspectives and attitudes regarding personal health data sharing, especially in low- and middle-income settings. Achieving this would not only aid in standardizing ethical practices but also in documenting global trends. Furthermore, engaging in longitudinal research that examines viewpoints before and after data sharing would be instrumental in figuring out if and how attitudes shift over time. It is also crucial to conduct more detailed qualitative research that looks into the barriers and facilitators of data sharing at every level—from individual to interpersonal, community, and even societal scales. To truly understand the nuances, it is imperative to gather data across varied sociodemographic markers for all stakeholders, emphasizing age and education. Analyzing this data would help in segmenting populations and diving deeper into the varying perspectives on sharing personal health data. An interesting aspect to consider is observing the differences in healthcare delivery systems and understanding their influence on perceptions about data sharing [72]. Such studies can address the lack of evidence around diverse demographics as well as broader global health challenges.
Strengths and limitations
As with any kind of research, our article had both strengths and limitations worth mentioning. This review captured multiple stakeholders’ perspectives on personal health data sharing across various contexts, with a diverse range of barriers and facilitators that impact data-sharing behavior. We searched multiple electronic databases and included both quantitative and qualitative studies. Our research also builds on previous systematic and scoping reviews to contribute towards better understanding the dynamic field of data sharing. Despite these strengths, our review had several limitations. Firstly, the search was restricted to articles published in English, which may have led to the exclusion of relevant studies in other languages. Secondly, the scope of this review focused on perceptions of personal health data sharing. As such, our search strategy may not have captured other relevant information such as health legislation and policies. Thirdly, the narrative synthesis approach used in this review–while effective in identifying common themes and guided by a conceptual framework–may be subject to reviewer bias in the interpretation of the findings. Finally, as this was a scoping review, a formal quality appraisal of the included studies was not conducted.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Data Availability
Articles included in scoping review are available via public databases.
Funding Statement
This work was supported by Moderna. The first author (PA) and third author (LL) were supported by AIR@InnoHK administered by Innovation and Technology Commission. The funding bodies had no role in the design of the study, analysis, and interpretation of data and in writing the manuscript.
References
- 1.World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening. Geneva: 2019. [PubMed]
- 2.Aitken M, de St. Jorre J, Pagliari C, Jepson R, Cunningham-Burley S. Public responses to the sharing and linkage of health data for research purposes: a systematic review and thematic synthesis of qualitative studies. BMC Medical Ethics. 2016;17(1):73. doi: 10.1186/s12910-016-0153-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Subbiah V. The next generation of evidence-based medicine. Nature Medicine. 2023;29(1):49–58. doi: 10.1038/s41591-022-02160-z [DOI] [PubMed] [Google Scholar]
- 4.van Panhuis WG, Paul P, Emerson C, Grefenstette J, Wilder R, Herbst AJ, et al. A systematic review of barriers to data sharing in public health. BMC Public Health. 2014;14:1144. Epub 20141105. doi: 10.1186/1471-2458-14-1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suwinski P, Ong C, Ling MHT, Poh YM, Khan AM, Ong HS. Advancing Personalized Medicine Through the Application of Whole Exome Sequencing and Big Data Analytics. Front Genet. 2019;10:49. Epub 20190212. doi: 10.3389/fgene.2019.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams GJ, Al-Baraikan A, Rademakers FE, Ciravegna F, van de Vosse FN, Lawrie A, et al. Wearable technology and the cardiovascular system: the future of patient assessment. Lancet Digit Health. 2023;5(7):e467–e76. doi: 10.1016/S2589-7500(23)00087-0 . [DOI] [PubMed] [Google Scholar]
- 7.Rabbani B, Nakaoka H, Akhondzadeh S, Tekin M, Mahdieh N. Next generation sequencing: implications in personalized medicine and pharmacogenomics. Mol Biosyst. 2016;12(6):1818–30. doi: 10.1039/c6mb00115g . [DOI] [PubMed] [Google Scholar]
- 8.Hughes A, Shandhi MMH, Master H, Dunn J, Brittain E. Wearable Devices in Cardiovascular Medicine. Circ Res. 2023;132(5):652–70. Epub 20230302. doi: 10.1161/CIRCRESAHA.122.322389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alfano S, Amberg C, Peters N, Salazar P, Vieux-Rochas M, Welton S. Treating rare diseases: How digital technologies can drive innovation2023. https://www.mckinsey.com/industries/life-sciences/our-insights/treating-rare-diseases-how-digital-technologies-can-drive-innovation#/.
- 10.Amankwah-Amoah J, Khan Z, Wood G, Knight G. COVID-19 and digitalization: The great acceleration. J Bus Res. 2021;136:602–11. Epub 20210811. doi: 10.1016/j.jbusres.2021.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin L, Hou Z. Combat COVID-19 with artificial intelligence and big data. Journal of Travel Medicine. 2020;27(5). doi: 10.1093/jtm/taaa080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maxwell L, Shreedhar P, Dauga D, McQuilton P, Terry RF, Denisiuk A, et al. FAIR, ethical, and coordinated data sharing for COVID-19 response: a scoping review and cross-sectional survey of COVID-19 data sharing platforms and registries. Lancet Digit Health. 2023;5(10):e712–e36. doi: 10.1016/S2589-7500(23)00129-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dron L, Kalatharan V, Gupta A, Haggstrom J, Zariffa N, Morris AD, et al. Data capture and sharing in the COVID-19 pandemic: a cause for concern. Lancet Digit Health. 2022;4(10):e748–e56. doi: 10.1016/S2589-7500(22)00147-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cosgriff CV, Ebner DK, Celi LA. Data sharing in the era of COVID-19. Lancet Digit Health. 2020;2(5):e224. Epub 20200428. doi: 10.1016/S2589-7500(20)30082-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonomi L, Huang Y, Ohno-Machado L. Privacy challenges and research opportunities for genomic data sharing. Nat Genet. 2020;52(7):646–54. Epub 20200629. doi: 10.1038/s41588-020-0651-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hassan L, Dalton A, Hammond C, Tully MP. A deliberative study of public attitudes towards sharing genomic data within NHS genomic medicine services in England. Public Underst Sci. 2020;29(7):702–17. Epub 20200715. doi: 10.1177/0963662520942132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Husedzinovic A, Ose D, Schickhardt C, Fröhling S, Winkler EC. Stakeholders’ perspectives on biobank-based genomic research: systematic review of the literature. European Journal of Human Genetics. 2015;23:1607–14. doi: 10.1038/ejhg.2015.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lynch F, Meng Y, Best S, Goranitis I, Savulescu J, Gyngell C, et al. Australian public perspectives on genomic data storage and sharing: Benefits, concerns and access preferences. Eur J Med Genet. 2023;66(1):104676. Epub 20221205. doi: 10.1016/j.ejmg.2022.104676 . [DOI] [PubMed] [Google Scholar]
- 19.Takashima K, Maru Y, Mori S, Mano H, Noda T, Muto K. Ethical concerns on sharing genomic data including patients’ family members. BMC Med Ethics. 2018;19(1):61. Epub 20180618. doi: 10.1186/s12910-018-0310-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zarate OA, Brody JG, Brown P, Ramirez-Andreotta MD, Perovich L, Matz J. Balancing Benefits and Risks of Immortal Data: Participants’ Views of Open Consent in the Personal Genome Project. Hastings Cent Rep. 2016;46(1):36–45. Epub 20151217. doi: 10.1002/hast.523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simpson E, Brown R, Sillence E, Coventry L, Lloyd K, Gibbs J, et al. Understanding the Barriers and Facilitators to Sharing Patient-Generated Health Data Using Digital Technology for People Living With Long-Term Health Conditions: A Narrative Review. Front Public Health. 2021;9:641424. Epub 20211123. doi: 10.3389/fpubh.2021.641424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bezuidenhout L. To share or not to share: Incentivizing data sharing in life science communities. Dev World Bioeth. 2019;19(1):18–24. Epub 20180122. doi: 10.1111/dewb.12183 . [DOI] [PubMed] [Google Scholar]
- 23.Nadal C, Sas C, Doherty G. Technology Acceptance in Mobile Health: Scoping Review of Definitions, Models, and Measurement. J Med Internet Res. 2020;22(7):e17256. Epub 20200706. doi: 10.2196/17256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. Global strategy on digital health 2020–2025. Geneva: 2021.
- 25.Wilkinson MD, Dumontier M, Aalbersberg IJ, Appleton G, Axton M, Baak A, et al. The FAIR Guiding Principles for scientific data management and stewardship. Scientific Data. 2016;3(1):160018. doi: 10.1038/sdata.2016.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adjekum A, Blasimme A, Vayena E. Elements of Trust in Digital Health Systems: Scoping Review. J Med Internet Res. 2018;20(12):e11254. Epub 13.12.2018. doi: 10.2196/11254 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howe N, Giles E, Newbury-Birch D, McColl E. Systematic review of participants’ attitudes towards data sharing: a thematic synthesis. J Health Serv Res Policy. 2018;23(2):123–33. doi: 10.1177/1355819617751555 . [DOI] [PubMed] [Google Scholar]
- 28.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. Epub 20180904. doi: 10.7326/M18-0850 . [DOI] [PubMed] [Google Scholar]
- 29.Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. npj Digital Medicine. 2022;5(1):119. doi: 10.1038/s41746-022-00663-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Esmaeilzadeh P, Sambasivan M. Patients’ support for health information exchange: a literature review and classification of key factors. BMC Med Inform Decis Mak. 2017;17(1):33. Epub 20170404. doi: 10.1186/s12911-017-0436-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He Y, He Q, Li L, Wang W, Zha W, Liu Q. Factors Affecting Willingness on Sharing of Electronic Health Records Data: A Survey on Chinese Residents. J Oncol. 2022;2022:5280792. Epub 20220711. doi: 10.1155/2022/5280792 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Brown R, Coventry L, Sillence E, Blythe J, Stumpf S, Bird J, et al. Collecting and sharing self-generated health and lifestyle data: Understanding barriers for people living with long-term health conditions—a survey study. Digit Health. 2022;8:20552076221084458. Epub 20220307. doi: 10.1177/20552076221084458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones LA, Nelder JR, Fryer JM, Alsop PH, Geary MR, Prince M, et al. Public opinion on sharing data from health services for clinical and research purposes without explicit consent: an anonymous online survey in the UK. BMJ Open. 2022;12(4):e057579. Epub 20220427. doi: 10.1136/bmjopen-2021-057579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Young DL, Fritz JM, Kean J, Thackeray A, Johnson JK, Dummer D, et al. Key Data Elements for Longitudinal Tracking of Physical Function: A Modified Delphi Consensus Study. Phys Ther. 2022;102(4). doi: 10.1093/ptj/pzab279 . [DOI] [PubMed] [Google Scholar]
- 35.Brall C, Berlin C, Zwahlen M, Ormond KE, Egger M, Vayena E. Public willingness to participate in personalized health research and biobanking: A large-scale Swiss survey. PLoS One. 2021;16(4):e0249141. Epub 20210401. doi: 10.1371/journal.pone.0249141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pletscher F, Mändli Lerch K, Glinz D. Willingness to share anonymised routinely collected clinical health data in Switzerland: a cross-sectional survey. Swiss Med Wkly. 2022;152:w30182. Epub 20220616. doi: 10.4414/smw.2022.w30182 . [DOI] [PubMed] [Google Scholar]
- 37.Zhang L, Jacobson PA, Johnson ANK, Gregornik DB, Johnson SG, McCarty CA, et al. Public Attitudes toward Pharmacogenomic Testing and Establishing a Statewide Pharmacogenomics Database in the State of Minnesota. J Pers Med. 2022;12(10). Epub 20220930. doi: 10.3390/jpm12101615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trinidad MG, Platt J, Kardia SLR. The public’s comfort with sharing health data with third-party commercial companies. Humanit Soc Sci Commun. 2020;7(1). Epub 20201111. doi: 10.1057/s41599-020-00641-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim H, Kim HR, Kim S, Kim E, Kim SY, Park HY. Public Attitudes Toward Precision Medicine: A Nationwide Survey on Developing a National Cohort Program for Citizen Participation in the Republic of Korea. Front Genet. 2020;11:283. Epub 20200512. doi: 10.3389/fgene.2020.00283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim J, Kim H, Bell E, Bath T, Paul P, Pham A, et al. Patient Perspectives About Decisions to Share Medical Data and Biospecimens for Research. JAMA Netw Open. 2019;2(8):e199550. Epub 20190802. doi: 10.1001/jamanetworkopen.2019.9550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tosoni S, Voruganti I, Lajkosz K, Habal F, Murphy P, Wong RKS, et al. The use of personal health information outside the circle of care: consent preferences of patients from an academic health care institution. BMC Medical Ethics. 2021;22(1):29. doi: 10.1186/s12910-021-00598-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wiesner M, Zowalla R, Suleder J, Westers M, Pobiruchin M. Technology Adoption, Motivational Aspects, and Privacy Concerns of Wearables in the German Running Community: Field Study. JMIR Mhealth Uhealth. 2018;6(12):e201. Epub 20181214. doi: 10.2196/mhealth.9623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hutchings E, Butcher BE, Butow P, Boyle FM. Attitudes of Australian breast cancer patients toward the secondary use of administrative and clinical trial data. Asia Pac J Clin Oncol. 2023;19(2):e12–e26. Epub 20220620. doi: 10.1111/ajco.13734 . [DOI] [PubMed] [Google Scholar]
- 44.Sheikh Z, Hoeyer K. "That is why I have trust": unpacking what ’trust’ means to participants in international genetic research in Pakistan and Denmark. Med Health Care Philos. 2018;21(2):169–79. doi: 10.1007/s11019-017-9795-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Amorim M, Silva S, Machado H, Teles EL, Baptista MJ, Maia T, et al. Benefits and Risks of Sharing Genomic Data for Research: Comparing the Views of Rare Disease Patients, Informal Carers and Healthcare Professionals. Int J Environ Res Public Health. 2022;19(14). Epub 20220719. doi: 10.3390/ijerph19148788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Broes S, Verbaanderd C, Casteels M, Lacombe D, Huys I. Sharing of Clinical Trial Data and Samples: The Cancer Patient Perspective. Front Med (Lausanne). 2020;7:33. Epub 20200211. doi: 10.3389/fmed.2020.00033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nunes Vilaza G, Coyle D, Bardram JE. Public Attitudes to Digital Health Research Repositories: Cross-sectional International Survey. J Med Internet Res. 2021;23(10):e31294. Epub 20211029. doi: 10.2196/31294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spencer K, Sanders C, Whitley EA, Lund D, Kaye J, Dixon WG. Patient Perspectives on Sharing Anonymized Personal Health Data Using a Digital System for Dynamic Consent and Research Feedback: A Qualitative Study. J Med Internet Res. 2016;18(4):e66. Epub 15.04.2016. doi: 10.2196/jmir.5011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barnes R, Votova K, Rahimzadeh V, Osman N, Penn AM, Zawati MnH, et al. Biobanking for Genomic and Personalized Health Research: Participant Perceptions and Preferences. Biopreserv Biobank. 2020;18(3):204–12. doi: 10.1089/bio.2019.0090 . [DOI] [PubMed] [Google Scholar]
- 50.Götzl C, Hiller S, Rauschenberg C, Schick A, Fechtelpeter J, Fischer Abaigar U, et al. Artificial intelligence-informed mobile mental health apps for young people: a mixed-methods approach on users’ and stakeholders’ perspectives. Child and Adolescent Psychiatry and Mental Health. 2022;16(1):86. doi: 10.1186/s13034-022-00522-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Summers C, Griffiths F, Cave J, Panesar A. Understanding the Security and Privacy Concerns About the Use of Identifiable Health Data in the Context of the COVID-19 Pandemic: Survey Study of Public Attitudes Toward COVID-19 and Data-Sharing. JMIR Form Res. 2022;6(7):e29337. Epub 7.7.2022. doi: 10.2196/29337 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tosoni S, Voruganti I, Lajkosz K, Mustafa S, Phillips A, Kim SJ, et al. Patient consent preferences on sharing personal health information during the COVID-19 pandemic: "the more informed we are, the more likely we are to help". BMC Med Ethics. 2022;23(1):53. Epub 20220520. doi: 10.1186/s12910-022-00790-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buhr L, Schicktanz S, Nordmeyer E. Attitudes Toward Mobile Apps for Pandemic Research Among Smartphone Users in Germany: National Survey. JMIR Mhealth Uhealth. 2022;10(1):e31857. Epub 24.1.2022. doi: 10.2196/31857 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cheah PY, Tangseefa D, Somsaman A, Chunsuttiwat T, Nosten F, Day NP, et al. Perceived Benefits, Harms, and Views About How to Share Data Responsibly: A Qualitative Study of Experiences With and Attitudes Toward Data Sharing Among Research Staff and Community Representatives in Thailand. J Empir Res Hum Res Ethics. 2015;10(3):278–89. doi: 10.1177/1556264615592388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lysaght T, Ballantyne A, Toh HJ, Lau A, Ong S, Schaefer O, et al. Trust and Trade-Offs in Sharing Data for Precision Medicine: A National Survey of Singapore. Journal of Personalized Medicine. 2021;11(9):921.: doi: 10.3390/jpm11090921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hate K, Meherally S, Shah More N, Jayaraman A, Bull S, Parker M, et al. Sweat, Skepticism, and Uncharted Territory: A Qualitative Study of Opinions on Data Sharing Among Public Health Researchers and Research Participants in Mumbai, India. J Empir Res Hum Res Ethics. 2015;10(3):239–50. doi: 10.1177/1556264615592383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ivanova J, Grando A, Murcko A, Saks M, Whitfield MJ, Dye C, et al. Mental health professionals’ perceptions on patients control of data sharing. Health Informatics J. 2020;26(3):2011–29. Epub 20200108. doi: 10.1177/1460458219893845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang D, Lim J, Zhou L, Dahl AA. Breaking the Data Value-Privacy Paradox in Mobile Mental Health Systems Through User-Centered Privacy Protection: A Web-Based Survey Study. JMIR Ment Health. 2021;8(12):e31633. Epub 24.12.2021. doi: 10.2196/31633 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wetzels M, Broers E, Peters P, Feijs L, Widdershoven J, Habibovic M. Patient Perspectives on Health Data Privacy and Management: "Where Is My Data and Whose Is It?". Int J Telemed Appl. 2018;2018:3838747. Epub 20181202. doi: 10.1155/2018/3838747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shah N, Coathup V, Teare H, Forgie I, Giordano GN, Hansen TH, et al. Sharing data for future research-engaging participants’ views about data governance beyond the original project: a DIRECT Study. Genet Med. 2019;21(5):1131–8. Epub 20180928. doi: 10.1038/s41436-018-0299-7 . [DOI] [PubMed] [Google Scholar]
- 61.Ostherr K, Borodina S, Bracken RC, Lotterman C, Storer E, Williams B. Trust and privacy in the context of user-generated health data. Big Data & Society. 2017;4(1):2053951717704673. doi: 10.1177/2053951717704673 [DOI] [Google Scholar]
- 62.O’Brien EC, Rodriguez AM, Kum HC, Schanberg LE, Fitz-Randolph M, O’Brien SM, et al. Patient perspectives on the linkage of health data for research: Insights from an online patient community questionnaire. Int J Med Inform. 2019;127:9–17. Epub 20190406. doi: 10.1016/j.ijmedinf.2019.04.003 . [DOI] [PubMed] [Google Scholar]
- 63.Staunton C, Tschigg K, Sherman G. Data protection, data management, and data sharing: Stakeholder perspectives on the protection of personal health information in South Africa. PLoS One. 2021;16(12):e0260341. Epub 20211220. doi: 10.1371/journal.pone.0260341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nwebonyi N, Silva S, de Freitas C. Public Views About Involvement in Decision-Making on Health Data Sharing, Access, Use and Reuse: The Importance of Trust in Science and Other Institutions. Frontiers in Public Health. 2022;10. doi: 10.3389/fpubh.2022.852971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hartmann R, Sander C, Lorenz N, Böttger D, Hegerl U. Utilization of Patient-Generated Data Collected Through Mobile Devices: Insights From a Survey on Attitudes Toward Mobile Self-Monitoring and Self-Management Apps for Depression. JMIR Ment Health. 2019;6(4):e11671. Epub 20190403. doi: 10.2196/11671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Braunack-Mayer A, Fabrianesi B, Street J, O’Shaughnessy P, Carter SM, Engelen L, et al. Sharing Government Health Data With the Private Sector: Community Attitudes Survey. J Med Internet Res. 2021;23(10):e24200. Epub 20211001. doi: 10.2196/24200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Perrier L, Blondal E, MacDonald H. The views, perspectives, and experiences of academic researchers with data sharing and reuse: A meta-synthesis. PLoS One. 2020;15(2):e0229182. Epub 20200227. doi: 10.1371/journal.pone.0229182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Watts G. Data sharing: keeping patients on board. Lancet Digit Health. 2019. [Google Scholar]
- 69.Evertsz N, Bull S, Pratt B. What constitutes equitable data sharing in global health research? A scoping review of the literature on low-income and middle-income country stakeholders’ perspectives. BMJ Glob Health. 2023;8(3). doi: 10.1136/bmjgh-2022-010157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Scott K, Shinde A, Ummer O, Yadav S, Sharma M, Purty N, et al. Freedom within a cage: how patriarchal gender norms limit women’s use of mobile phones in rural central India. BMJ Global Health. 2021;6(Suppl 5):e005596. doi: 10.1136/bmjgh-2021-005596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hung YW, Hoxha K, Irwin BR, Law MR, Grépin KA. Using routine health information data for research in low- and middle-income countries: a systematic review. BMC Health Serv Res. 2020;20(1):790. Epub 20200825. doi: 10.1186/s12913-020-05660-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ghafur S, Van Dael J, Leis M, Darzi A, Sheikh A. Public perceptions on data sharing: key insights from the UK and the USA. Lancet Digit Health. 2020;2(9):e444–e6. Epub 20200724. doi: 10.1016/S2589-7500(20)30161-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Articles included in scoping review are available via public databases.