Abstract
Background
Left-behind children (LBC) refer to those who have been separated from at least one parent for six months or more due to parental migration for work. This phenomenon poses a significant threat to the mental health of over 61 million LBC in China. This study aims to compare the prevalence of mental health symptoms between LBC and non-left-behind children (non-LBC) and to explore the predictive effect of bullying victimization on adolescent mental health problems.
Methods
In 2019, we conducted a cross-sectional analysis involving 28,036 children and adolescents in Mianyang City, Sichuan Province, China, with ages ranging from 8 to 19 years. Mental health symptoms were assessed using the 7-item Generalized Anxiety Disorder (GAD-7) scale and the 9-item Patient Health Questionnaire (PHQ-9). The Delaware Bullying Victimization Scale-Student (DBVS-S) was employed to gather data on experiences of bullying victimization. Information on self-injury was collected by inquiring whether participants had engaged in self-injurious behavior and the reasons for such behavior. Multivariable logistic regression was utilized to analyze the risk and protective factors associated with mental health symptoms, with a particular focus on different types of bullying victimization.
Results
Compared to non-left-behind children (non-LBC), left-behind children (LBC) exhibited a higher prevalence of mental health issues: anxiety symptoms (24.0% vs. 18.0%, p<0.001), depressive symptoms (27.9% vs. 19.4%, p<0.001), and self-injurious behavior (17.7% vs. 12.2%, p<0.001). Among LBC, physical bullying was identified as the most significant predictor of anxiety symptoms (OR = 1.62). Additionally, LBC who experienced verbal bullying had a higher risk of depressive symptoms (OR = 2.23) and self-injurious behaviors (OR = 1.54). Enhanced family functioning, positive teacher-student relationships, and strong peer relationships were found to offer protective effects against mental health problems.
Conclusion
Our results suggested that LBC experienced a higher incidence of mental health symptoms, particularly among those who had been victims of bullying. This underscores the urgent need for supportive strategies focused on the school environment and interpersonal relationships to mitigate negative mental health outcomes for LBC.
Keywords: depression, anxiety, self-injurious behavior, bullying, left-behind children (LBC)
1. Introduction
The urbanization and modernization since China’s Reform and Opening-up have led to a surge in migrant workers, resulting in many individuals moving from their hometowns to seek employment in cities (1). Consequently, a significant number of children and adolescents remain in their rural hometowns due to the high cost of living, education, and healthcare in urban areas. A nationwide survey in China (2014) reported that approximately 61 million children and adolescents were left behind, representing 22.0% of the total child population in China (2). Left-behind children (LBC) typically remain in their original residence for at least six months while one or both parents migrate for work (3, 4). Intuitively, the lack of care and supervision may heighten LBC’s risk for poor nutrition, accidents, and injuries (5). From a developmental psychology perspective, parental absence can impact children’s social development, emotional support, self-regulation, and the development of self-concept (6). Early-life adversity, such as parental absence, may lead to feelings of insecurity and sustained tension, affecting the development of the HPA axis (7, 8). This has a negative impact on the development of attachment relationships (9) and result in decreased emotional support and increased feelings of loneliness (10). Previous studies have also indicated that self-rated health status and parent-child relationships can vertically predict adolescent personality development (11, 12). Thus, parental absence can influence the development of self-identity and the formation of a healthy personality (13, 14). Furthermore, early victimization increases LBC’s susceptibility to mental illness (15, 16), making them more prone to externalized behavioral problems, internalized disorders, and inferiority complexes (17), such as hallucinations, delusions, and emotional problems (18–20). Compared to non-LBC, the incidence of mental health problems among LBC is over 10.0% higher (21). Given this high prevalence, it is crucial that researchers pay increased attention to the current state and risk factors affecting the mental health of LBC.
Bullying is a widespread issue affecting children and adolescents globally (22, 23). Bullying victimization manifests in two primary forms: traditional and cyberbullying. Traditional bullying victimization is characterized by harm inflicted through physical, verbal, or relational aggressive behavior from peers (24). In contrast, cyberbullying involves the deliberate use of electronic media to inflict harm (25). Globally, approximately 10.0% to 30.0% of adolescents experience bullying (26). A cross-sectional study conducted in China reported that the highest self-reported rate of traditional bullying victimization was 66.0%, while the peak rate of cyberbullying victimization was 57.0% (27). In recent years, the reported rates of bullying victimization among children and adolescents in China have ranged from 8.0% to 15.1% (28, 29).
As a traumatic experience, bullying victimization during primary and secondary school years can adversely affect mental health into early adulthood (30, 31). The extent and variety of bullying experienced are directly correlated with increased mental health harm (22). Bullied adolescents reported a range of emotional and behavioral problems, including anxiety (32), depressive symptoms (33), and avoidance behavior (34). A growing body of literature indicates that adolescents who experience bullying are at a heightened risk for developing anxiety and depressive symptoms (35). Consequences of bullying can also include low self-esteem, academic difficulties (36), increased substance abuse (37) and even suicidal ideation or behavior (38–40). Studies have shown that LBC experience higher rates of bullying and greater victimization scores compared to non-LBC (41). The unsafe attachment patterns often associated with being left behind can impair individual abilities and social development, making these children more vulnerable to bullying (42–44). Additionally, factors such as the main caregivers and the duration of parental separation are linked to the extent of bullying victimization (45).
Given the significant long-term impact of bullying on mental health, it is crucial to identify the key risk and protective factors influencing adolescents’ psychological well-being. This focus is vital for disease prevention and health promotion, particularly during adolescence. There is still limited understanding of how different types of bullying victimization relate to mental health outcomes and the protective factors that may mitigate these effects. Using cross-sectional data from students aged 8-19 in China, we aimed to explore the association between various types of bullying victimization and mental health problems, with a particular emphasis on the experiences of being left behind.
2. Methods
2.1. Participants
Sichuan, located in western China, is the fourth most populous province, with a total population exceeding 82 million. The Adolescence Mental Health Promotion Cohort is a prospective cohort including 29,768 children and adolescents recruited from 29 local schools through stratified randomization in Mianyang City, Sichuan Province, China, in 2019. The distribution of students across primary, middle, and high schools was relatively balanced. The overall participation rate was 74.0%, representing approximately 30.0% of students in Santai County. All participants were surveyed through a WeChat applet called Psyclub.
In our research, participants were asked whether they had been separated from their parents for at least six months during childhood (yes or no). Those who answered “yes” were categorized into the LBC group.
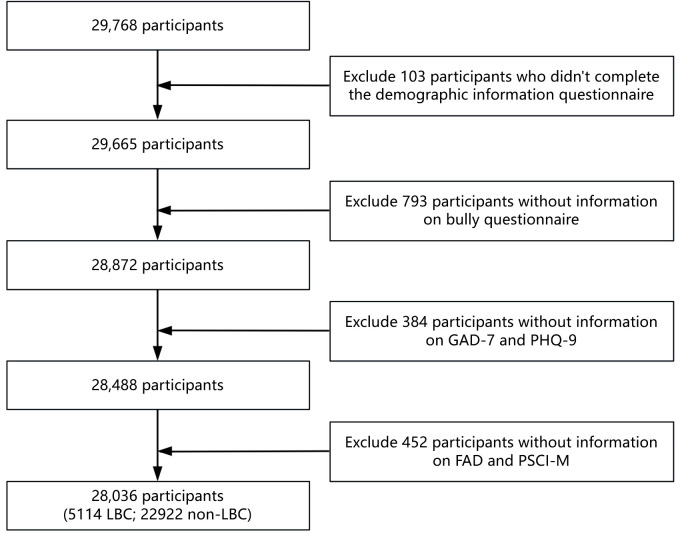
Of the 29,768 participants, 103 were excluded due to incomplete demographic information, including 50 LBC who did not provide details about their primary caregiver during their stay. 793 participants were excluded for failing to complete the bullying exploration questionnaire. An additional 384 were excluded due to missing assessments for anxiety and depression symptoms. Another 452 were excluded from this study as they did not complete the questionnaires on family functioning and perceived school atmosphere. Ultimately, 5114 LBC and 22922 non-LBC were included in the study ( Figure 1 ). Participants were aged 8 to 19 years, with a mean age of 13.5. All participants and their guardians reviewed the evaluation content, purpose, and electronic version of the informed consent form on Psyclub. They confirmed their agreement to participate in the study and signed the informed consent. The study protocol was approved by the Ethics Committee of West China Hospital, Sichuan University [2019-77].
Figure 1.
Sample inclusion flow chart.
2.2. Collection of self-reporting problem information
2.2.1. Primary caregiver
We collected information on the primary caregivers of participants throughout their development (referred to as “caregivers” in the tables), as well as the primary caregivers of left-behind children (LBC) during their absence (referred to as “LBC caregivers” in the tables). Participants were asked via a questionnaire to identify who primarily cared for them during their growth, with options including both parents, father only, mother only, grandparents, and other close relatives. For participants who had not lived with their parents for more than six months, we additionally inquired, “Who primarily takes care of you when your father and/or mother are away?” The response options included father, mother, grandparents, siblings, other close relatives, and others.
2.2.2. Self-injurious behavior
In the basic information questionnaire, participants were asked about their engagement in self-injurious behavior through self-reported questions. Specifically, we inquired, “Have you ever intentionally harmed yourself (e.g., through cutting, burning, or any other means)?” If participants reported self-injurious behavior, we further asked whether the intent behind such behavior was suicidal.
2.3. Bullying (DBVS-S)
The Delaware Bullying Victimization Scale-Student (DBVS-S) was employed to assess campus bullying victimization. The scale comprises 17 items: four items each for verbal bullying, physical bullying, social/relational bullying, and cyberbullying, plus a 13th item, “I was bullied at this school,” which is not included in the dimension scores but reflects the participant’s perception of being bullied (46). A six-point Likert scale was used to measure the severity of bullying, ranging from “never” (1 point) to “every day” (6 points). The Cronbach’s α for the DBVS-S was 0.906 (47). A score greater than 8 in any dimension was defined as “often,” and any occurrence of bullying was classified as “often” if at least one dimension met this criterion. The Cronbach’s α in our sample was 0.959.
2.4. Anxiety (GAD-7)
The 7-item Generalize Anxiety Disorder (GAD-7) scale was utilized to assess anxiety symptoms. The GAD-7 employs a Likert scale for self-evaluation, ranging from 0 (none at all) to 3 (almost every day). The total score ranges from 0 to 21 points, with higher scores indicating more severe anxiety symptoms. A score of 5 or above suggests the presence of anxiety symptoms, a score of 10 or above indicates moderate anxiety symptoms, and a score of 15 to 21 indicates severe anxiety symptoms (48). The Cronbach’s α of Chinese version of the GAD-7 scale was 0.915, and was 0.893 in our sample (49). In this study, a total score of 10 or higher was considered indicative of significant anxiety symptoms.
2.5. Depression (PHQ-9)
The 9-item Patient Health Questionnaire (PHQ-9) scale was used to assess depressive symptoms. Each item is scored from 0 (none at all) to 3 (almost every day). The total score ranges from 0 to 27 points, with higher scores indicating more severe depressive symptoms. Scores of 5, 10, 15, and 20 points correspond to mild, moderate, moderate and severe, and major depressive disorder (50, 51). The Chinese version of the PHQ-9 has demonstrated good reliability and validity, with a Cronbach’s α of 0.86 (52). A total score of 10 or higher was considered indicative of significant depressive symptoms (53, 54). The Cronbach’s α in this study was 0.898.
2.6. Perceived school atmosphere (PSCI-M)
The Perceived School Climate Inventory-M (PSCI-M) includes five factors: teacher-student relationship, peer relationship, academic pressure, order and discipline, and developmental diversity (55). This study utilized two factors: teacher-student relationship and classmate relationship, with a total of 16 items. The PSCI-M employs a four-point rating from 1 (very inconsistent) to 4 (very consistent). The Cronbach’s α in this study was 0.917. The scoring ranges for teacher-student relationship and peer relationship are 9-36 (scores > 18 were defined as “good”) and 8-32 (scores > 14 were defined as “good”), respectively.
2.7. Family functioning (FAD)
The general functioning subscale of the Family Assessment Device (FAD) is a 12-item measure that assesses overall family functioning (56). The total score ranges from 0 to 4 and is categorized into low, medium, and high levels based on the median. Scores greater than or equal to 1 but less than 2 are rated as “low,” scores from 2 to less than 3 are rated as “medium,” and scores of 3 or higher are rated as “high.” The Cronbach’s α in college students was reported as 0.915 (57). In our sample, the Cronbach’s α was 0.697.
2.8. Covariates
Participants provided demographic information, including gender, age, grade, whether they were an only child, and the occupation and educational level of their parents. Additional data were collected on smoking history, school residency experience, primary caregivers during their stay, and peer relationships. Family environment, perceived school atmosphere, and smoking have been shown to be related to mental health problems (58, 59). Therefore, We classified and included these variables as covariates to adjust our results.
2.9. Statistical analysis
Quantitative variables, given their non-normal distribution, were characterized using the median and interquartile range (IQR). Categorical variables were represented by counts and percentages.
To discern inter-group differences, chi-square tests were applied to categorical variables. For non-normally distributed continuous variables, such as age, Kruskal-Wallis tests were employed.
To assess the association between mental health symptoms and bullying victimization in LBC, multivariate logistic regression analyses were conducted. These analyses were adjusted for various covariates across different models. Odds ratios (OR) were reported along with their corresponding 95% confidence intervals (CI), and statistical significance was considered at p<0.05. All analyses were performed using R software, version 4.2.2.
3. Results
3.1. Differences between LBC and non-LBC
Among the 28,036 students, 5,114 (18.2%) had left-behind experiences. The demographic characteristics and prior experience of LBC and control groups are detailed in Table 1 . Significant differences between the two groups were observed in terms of grades, caregivers, and the occupation and educational level of parents, while no significant gender differences were found. The average age of LBC was 14.05 (SD=2.33), compared to 13.47 (SD=2.40) for non-LBC. Most LBC were in high school (41.2%), whereas non-LBC were predominantly in junior high school (36.9%). Throughout their growth, the primary caregivers for LBC were mainly grandparents (49.6%), while non-LBC were parents (42.4%). Among the surveyed students, a majority of LBC’s parents were blue collar workers (Paternal: 32.5%; Maternal: 33.6%), whereas non-LBC’s parents were predominantly farmers (Paternal: 22.1%; Maternal: 24.1%). Additionally, a smaller proportion of LBC’s parents had a college degree or above (Paternal: 5.7%; Maternal: 4.3%) compared to non-LBC’s parents (Paternal: 11.9%; Maternal: 8.7%).
Table 1.
Differences between LBC and non-LBC, stratified by demographic characteristics and mental health status.
| Variable | non-LBC | LBC | p-value |
|---|---|---|---|
| (n = 22922) | (n = 5114) | ||
| n (%) | n (%) | ||
| Gender | |||
| Female | 11587 (50.5) | 2537 (49.6) | 0.23 |
| Male | 11335 (49.5) | 2577 (50.4) | |
| Age (median[IQR]) | 14.00[12.00, 16.00] | 14.00[12.00, 16.00] | <0.001 |
| Grade | |||
| High school | 7718 (33.7) | 2107 (41.2) | <0.001 |
| Junior high school | 8463 (36.9) | 1744 (34.1) | |
| Primary school | 5996 (26.2) | 973 (19.0) | |
| Vocational school | 745 (3.3) | 290 (5.7) | |
| Caregivers | |||
| Both Parents | 9721 (42.4) | 981 (19.2) | <0.001 |
| Father only | 8174 (35.7) | 1005 (19.7) | |
| Grandparents | 3294 (14.4) | 2534 (49.6) | |
| Mother only | 1414 (6.2) | 352 (6.9) | |
| Other close relatives | 319 (1.4) | 242 (4.7) | |
| Residence experience | |||
| No | 7225 (31.5) | 1200 (23.5) | <0.001 |
| Yes | 15697 (68.5) | 3914 (76.5) | |
| Only child | |||
| No | 14242 (62.1) | 3296 (64.5) | 0.002 |
| Yes | 8680 (37.9) | 1818 (35.5) | |
| Smoking history | |||
| No | 22599 (98.6) | 4991 (97.6) | <0.001 |
| Yes | 323 (1.4) | 123 (2.4) | |
| Paternal education | |||
| College and above | 2718 (11.9) | 291 (5.7) | <0.001 |
| Primary school | 3714 (16.2) | 1073 (21.0) | |
| Secondary school | 15798 (68.9) | 3570 (69.8) | |
| Unknown | 692 (3.0) | 180 (3.5) | |
| Paternal occupation a | |||
| Blue collar | 4823 (21.0) | 1664 (32.5) | <0.001 |
| Farmer | 5066 (22.1) | 1026 (20.1) | |
| Others | 4137 (18.0) | 1066 (20.8) | |
| Self-employed | 4692 (20.5) | 672 (13.1) | |
| White collar | 4204 (18.3) | 686 (13.4) | |
| Maternal education | |||
| College and above | 1990 (8.7) | 218 (4.3) | <0.001 |
| Primary school | 4986 (21.8) | 1371 (26.8) | |
| Secondary school | 15087 (65.8) | 3182 (62.2) | |
| Unknown | 859 (3.7) | 343 (6.7) | |
| Maternal occupation a | |||
| Blue collar | 5120 (22.3) | 1716 (33.6) | <0.001 |
| Farmer | 5533 (24.1) | 1021 (20.0) | |
| Others | 5171 (22.6) | 1274 (24.9) | |
| Self-employed | 4585 (20.0) | 672 (13.1) | |
| White collar | 2513 (11.0) | 431 (8.4) | |
| Verbal bullying | |||
| Often | 2237 (9.8) | 667 (13.0) | <0.001 |
| Seldom | 20685 (90.2) | 4447 (87.0) | |
| Physical bullying | |||
| Often | 1144 (5.0) | 377 (7.4) | <0.001 |
| Seldom | 21778 (95.0) | 4737 (92.6) | |
| Relational bullying | |||
| Often | 1556 (6.8) | 486 (9.5) | <0.001 |
| Seldom | 21366 (93.2) | 4628 (90.5) | |
| Cyber bullying | |||
| Often | 565 (2.5) | 194 (3.8) | <0.001 |
| Seldom | 22357 (97.5) | 4920 (96.2) | |
| Any bullying | |||
| Often | 2773 (12.1) | 832 (16.3) | <0.001 |
| Seldom | 20149 (87.9) | 4282 (83.7) | |
| Teacher-student relationship | |||
| Good | 21651 (94.5) | 4744 (92.8) | <0.001 |
| Poor | 1271 (5.5) | 370 (7.2) | |
| Peer relations | |||
| Good | 21827 (95.2) | 4784 (93.5) | <0.001 |
| Poor | 1095 (4.8) | 330 (6.5) | |
| Family function | |||
| High | 13235 (57.7) | 2317 (45.3) | <0.001 |
| Low | 395 (1.7) | 160 (3.1) | |
| Medium | 9292 (40.5) | 2637 (51.6) | |
| Self-injurious behavior | |||
| For suicide | 656 (2.9) | 253 (4.9) | <0.001 |
| No | 20140 (87.9) | 4207 (82.3) | |
| Not for suicide | 2126 (9.3) | 654 (12.8) | |
| Depressive symptoms | |||
| No | 18486 (80.6) | 3686 (72.1) | <0.001 |
| Yes | 4436 (19.4) | 1428 (27.9) | |
| Anxiety symptoms | |||
| No | 18795 (82.0) | 3889 (76.0) | <0.001 |
| Yes | 4127 (18.0) | 1225 (24.0) | |
aPaternal and maternal occupation were defined as blue collar (including professional skill worker, commercial and service worker, industrial worker), white collar (including cadres of agencies, enterprises and institutions, teacher, soldier), self-employed (defined as individual proprietors and private entrepreneurs), farmer and others (including retired, unemployed, semi-unemployed individuals and others).
Compared with non-LBC, LBC reported worse interpersonal relationships, both with peers (non-LBC: 4.8%; LBC: 6.5%) and teachers (non-LBC: 5.5%; LBC: 7.2%). Additionally, a higher proportion of LBC had residence experience (76.5%) and a smoking history (2.4%). LBC also exhibited a higher frequency of bullying problems (LBC: 16.3%; non-LBC: 12.1%).
We also compared the prevalence of anxiety, depressive symptoms and self-injurious behavior between LBC and non-LBC. LBC exhibited a higher prevalence of anxiety symptoms (24.0% vs. 18.0%), depressive symptoms (27.9% vs. 19.4%), and self-injurious behavior (17.7% vs. 12.2%). Meanwhile, the proportion of LBC with suicidal purposes (4.9% vs. 2.9%) and non-suicidal purposes (12.8% vs. 9.3%) was higher compared to non-LBC.
3.2. The mental health status of LBC
Table 2 compared the prevalence of mental health problem among LBC by stratifying them according to demography information, caregivers, and different types of bullying (including verbal, physical, relational, and cyber bullying). Among LBC, girls were more likely to experience anxiety, depressive symptoms, and self-injurious behavior.
Table 2.
Mental health among LBC (n=5114) after stratification by demographic characteristics and life experience.
| Variable | Anxiety symptoms | p-value | Depressive symptoms | p-value | Self-injurious behavior | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| n(yes) | % | n(yes) | % | n(yes) | % | ||||
| 1225 | 24.0 | 1428 | 27.9 | 907 | 17.7 | ||||
| Gender | |||||||||
| Male | 553 | 21.5 | <0.001 | 640 | 24.8 | <0.001 | 375 | 14.6 | <0.001 |
| Female | 672 | 26.5 | 788 | 31.1 | 532 | 21.0 | |||
| Grade | |||||||||
| High school | 545 | 25.9 | <0.001 | 711 | 33.7 | <0.001 | 464 | 22.0 | <0.001 |
| Junior high school | 453 | 26.0 | 479 | 27.5 | 294 | 16.9 | |||
| Primary school | 146 | 15.0 | 135 | 13.9 | 70 | 7.2 | |||
| Vocational school | 81 | 27.9 | 103 | 35.5 | 79 | 27.2 | |||
| LBC Caregivers | |||||||||
| Brother or sister | 35 | 31.8 | 0.046 | 37 | 33.6 | 0.011 | 23 | 20.9 | <0.001 |
| Father | 63 | 26.7 | 59 | 25.0 | 63 | 26.7 | |||
| Grandparents | 816 | 23.5 | 941 | 27.1 | 568 | 16.4 | |||
| Mother | 207 | 24.4 | 247 | 29.1 | 149 | 17.5 | |||
| Other close relatives | 77 | 20.9 | 109 | 29.5 | 84 | 22.8 | |||
| Others | 27 | 33.8 | 35 | 43.8 | 20 | 25.0 | |||
| Smoking history | |||||||||
| No | 1185 | 23.7 | 0.032 | 1377 | 27.6 | 0.001 | 843 | 16.9 | <0.001 |
| Yes | 40 | 32.5 | 51 | 41.5 | 64 | 52.0 | |||
| Verbal bullying | |||||||||
| Seldom | 882 | 19.8 | <0.001 | 1024 | 23.0 | <0.001 | 661 | 14.9 | <0.001 |
| Often | 343 | 51.4 | 404 | 60.6 | 246 | 36.9 | |||
| Physical bullying | |||||||||
| Seldom | 1021 | 21.6 | <0.001 | 1192 | 25.2 | <0.001 | 759 | 16.0 | <0.001 |
| Often | 204 | 54.1 | 236 | 62.6 | 148 | 39.3 | |||
| Relational bullying | |||||||||
| Seldom | 970 | 21.0 | <0.001 | 1127 | 24.4 | <0.001 | 717 | 15.5 | <0.001 |
| Often | 255 | 52.5 | 301 | 61.9 | 190 | 39.1 | |||
| Cyber bullying | |||||||||
| Seldom | 1119 | 22.7 | <0.001 | 1288 | 26.2 | <0.001 | 812 | 16.5 | <0.001 |
| Often | 106 | 54.6 | 140 | 72.2 | 95 | 49.0 | |||
| Any bullying | |||||||||
| Seldom | 818 | 19.1 | <0.001 | 948 | 22.1 | <0.001 | 613 | 14.3 | <0.001 |
| Often | 407 | 48.9 | 480 | 57.7 | 294 | 35.3 | |||
| Teacher-student relationship | |||||||||
| Good | 1091 | 23.0 | <0.001 | 1265 | 26.7 | <0.001 | 786 | 16.6 | <0.001 |
| Poor | 134 | 36.2 | 163 | 44.1 | 121 | 32.7 | |||
| Peer relations | |||||||||
| Good | 1100 | 23.0 | <0.001 | 1272 | 26.6 | <0.001 | 805 | 16.8 | <0.001 |
| Poor | 125 | 37.9 | 156 | 47.3 | 102 | 30.9 | |||
| Family function | |||||||||
| High | 348 | 15.0 | <0.001 | 362 | 15.6 | <0.001 | 229 | 9.9 | <0.001 |
| Low | 82 | 51.3 | 112 | 70.0 | 77 | 48.1 | |||
| Medium | 795 | 30.1 | 954 | 36.2 | 601 | 22.8 | |||
Among LBC, the prevalence of depressive symptoms and self-injurious behavior is higher among those in high school (depressive symptoms: 33.7%; self-injurious: 22.0%) and vocational school (depressive symptoms: 35.5%; self-injurious: 27.2%). LBC whose primary caregiver is their father are more likely to engage in self-injurious behavior (26.7%). Anxiety (33.8%, p<0.05) and depressive symptoms (43.8%, p<0.05) are more prevalent among those with primary caregivers identified as “others”, with brothers or sisters following (anxiety symptoms: 31.8%, p<0.05; depressive symptoms: 33.6%, p<0.05).
LBC with a history of smoking exhibit higher rates of anxiety (32.5% vs. 23.7%), depressive symptoms (41.5% vs. 27.6%) and self-injurious behavior (52.0% vs. 16.9%). LBC who are often bullied show higher rates of anxiety (48.9% vs. 19.1%) and depressive symptoms (57.7% vs. 22.1%) compared to those who are seldom or never bullied, and are more likely to engage in self-injurious behavior (35.3% vs. 14.3%). Compared to other types of bullying, LBC who frequently experience cyberbullying have higher prevalence rates of depressive symptoms (72.2%) and self-injurious behavior (49.0%). Additionally, LBC with poor teacher-student relationships (anxiety symptoms: 36.2%; depressive symptoms: 44.1%; self-injurious: 32.7%) and poor peer relationships (anxiety symptoms: 37.9%; depressive symptoms: 47.3%; self-injurious: 30.9%) also exhibit a higher incidence of mental health problems.
3.3. Mental health risks of different types of bullying
Table 3 examined the effects of different types of bullying on anxiety, depressive symptoms, and self-injurious behavior among LBC. Among LBC, physical bullying showed the most significant positive correlation with anxiety symptoms (OR 2.03, 95% CI 1.54-2.67; Anxiety symptoms - Model B, Table 3 ). Even after adjusting for the effects of different types of bullying, physical bullying remains a significant predictor of anxiety symptoms (OR 1.62, 95% CI 1.11-2.38; Anxiety symptoms - Model C, Table 3 ).
Table 3.
The contribution of different types of bullying to anxiety symptoms, depression symptoms and self-injurious behavior among LBC.
| Variable | Anxiety symptoms | Depressive symptoms | Self-injurious behavior | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model Aa | Model Bb | Model Cc | Model Aa | Model Bb | Model Cc | Model Aa | Model Bb | Model Cc | |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Any bullying | |||||||||
| Often | 4.52(3.85-5.32) | 1.89(1.55-2.32) | NA | 5.92(5.01-7.00) | 3.29(2.68-4.04) | NA | 3.85(3.23-4.60) | 2.17(1.78-2.63) | NA |
| Seldom | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Verbal bullying | |||||||||
| Often | 4.66(3.91-5.55) | 1.91(1.54-2.38) | 1.54(1.15-2.06) | 6.07(5.07-7.29) | 3.29(2.64-4.11) | 2.23(1.66-3.00) | 3.81(3.16-4.60) | 2.05(1.66-2.53) | 1.54(1.16-2.04) |
| Seldom | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Physical bullying | |||||||||
| Often | 5.13(4.11-6.43) | 2.03(1.54-2.67) | 1.62(1.11-2.38) | 6.51(5.16-8.24) | 3.24(2.44-4.33) | 1.08(0.72-1.61) | 4.29(3.38-5.43) | 2.09(1.61-2.72) | 1.12(0.77-1.62) |
| Seldom | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Relational bullying | |||||||||
| Often | 4.66(3.82-5.68) | 1.86(1.45-2.38) | 1.37(0.97-1.92) | 6.14(5.00-7.57) | 3.29(2.55-4.26) | 1.52(1.07-2.15) | 4.11(3.32-5.07) | 2.12(1.68-2.68) | 1.33(0.95-1.85) |
| Seldom | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Cyber bullying | |||||||||
| Often | 4.44(3.30-5.98) | 1.35(0.94-1.94) | 0.54(0.33-0.86) | 8.19(5.92-11.49) | 4.94(3.31-7.42) | 1.86(1.12-3.12) | 5.38(3.96-7.32) | 2.48(1.77-3.46) | 1.36(0.88-2.11) |
| Seldom | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
CI, confidence interval; NA, not applicable; OR, odds ratio; Ref., reference.
a. ORs were adjusted for sex, age, grade, paternal occupation, maternal occupation, paternal education, maternal education. Due to the previous analysis finding that there was no significant difference in the prevalence of anxiety among parents with different educational backgrounds, paternal/maternal education level was not included as a covariate in the anxiety model.
b. ORs were additionally adjusted for caregivers, residence experience, smoking history, teacher student relationship, peer relations, and some other mental health problems.
c. ORs were additionally adjusted for other 3 types of bullying.
There was a significant positive correlation between various types of bullying and depressive symptoms among LBC. After adjusting for the effects of different types of bullying, verbal bullying emerged as the most significant predictor of depressive symptoms (OR 2.23, 95% CI 1.66-3.00; Depressive symptoms - Model C, Table 3 ). This was followed by cyber bullying (OR 1.86, 95% CI 1.12-3.12; Depressive symptoms - Model C, Table 3 ) and relational bullying (OR 1.52, 95% CI 1.07-2.15; Depressive symptoms - Model C, Table 3 ).
We also observed a positive correlation between bullying and self-injurious behavior among LBC, with the most significant association found for cyber bullying (OR 2.48, 95% CI 1.77-3.46; Self-injurious behavior - Model B, Table 3 ). After adjusting for different types of bullying, significant associations were observed only for verbal bullying (OR 1.54, 95% CI 1.16-2.04; Self-injurious behavior - Model C, Table 3 ).
3.4. The impact of bullying victims
Table 4 compared the differences between LBC and non-LBC among those who have experienced bullying. The proportion of self-injurious behavior was significantly higher among LBC (for suicide: 14.3%; not for suicide: 21.0%) compared to non-LBC (for suicide: 9.4%; not for suicide: 18.6%), regardless of the intent. Additionally, the prevalence of anxiety (48.9% vs. 44.5%) and depressive symptoms (57.7% vs. 49.6%) was higher among LBC. The severity scores for both anxiety and depressive symptoms were also significantly elevated in LBC compared to non-LBC. Furthermore, the overall family function of non-LBC is higher than that of LBC.
Table 4.
Compared the differences between left-behind and non-left-behind students who have been bullied.
| Variable | non-LBC | LBC | p-value |
|---|---|---|---|
| (n = 2773) | (n = 832) | ||
| n (%) | n (%) | ||
| Teacher-student relationship | |||
| Good | 2458 (88.6) | 725 (87.1) | 0.263 |
| Poor | 315 (11.4) | 107 (12.9) | |
| Peer relations | |||
| Good | 2381 (85.9) | 702 (84.4) | 0.311 |
| Poor | 392 (14.1) | 130 (15.6) | |
| Family function | |||
| High | 965 (34.8) | 240 (28.8) | 0.001 |
| Low | 149 (5.4) | 65 (7.8) | |
| Medium | 1659 (59.8) | 527 (63.3) | |
| Self-injurious behavior | |||
| For suicide | 260 (9.4) | 119 (14.3) | <0.001 |
| No | 1996 (72.0) | 538 (64.7) | |
| Not for suicide | 517 (18.6) | 175 (21.0) | |
| Depression level | |||
| No depression | 653 (23.5) | 148 (17.8) | 0.001 |
| Mild depression | 745 (26.9) | 204 (24.5) | |
| Moderate depression | 645 (23.3) | 225 (27.0) | |
| Moderate and severe depression | 459 (16.6) | 163 (19.6) | |
| Severe depression | 271 (9.8) | 92 (11.1) | |
| Anxiety level | |||
| No anxiety | 618 (22.3) | 147 (17.7) | 0.024 |
| Presence of symptoms | 920 (33.2) | 278 (33.4) | |
| Moderate anxiety | 767 (27.7) | 259 (31.1) | |
| Severe anxiety | 468 (16.9) | 148 (17.8) | |
3.5. Protective factors for the mental health of LBC
Table 5 categorized LBC into four groups based on their experiences with bullying and mental health problems. For LBC who have experienced both bullying and mental health problems (Group 1), good peer relationships (OR 0.35, 95% CI 0.26-0.49, p<0.001) and higher family function (High: OR 0.14, 95% CI 0.09-0.20, p<0.001; Medium: OR 0.36, 95% CI 0.25-0.52, p<0.001) serve as protective factors. Among LBC who did not experience bullying but had mental health problems (Group 2), a good teacher-student relationship (OR 0.76, 95% CI 0.58-0.99, p=0.047) was identified as a protective factor. LBC who had neither experienced bullying nor mental health problems (Group 4) demonstrated that good peer relationships (OR 2.06, 95% CI 1.54-2.79, p<0.001) and higher family function (High: OR 11.47, 95% CI 7.34-18.76, p<0.001; Medium: OR 4.43, 95% CI 2.84-7.22, p<0.001) were associated with better outcomes. Details are shown in Table 5 .
Table 5.
Multinomial logistic regression to independent risk factors for bullying and mental health symptoms among LBC.
| Variable | Group1 a | p-value | Group2 b | p-value | Group3 c | p-value | Group4 d | p-value |
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |||||
| Age | 0.97 (0.88, 1.07) | 0.59 | 1.17 (1.09, 1.25) | <0.001 | 0.84 (0.72, 0.97) | <0.05 | 0.92 (0.86, 0.98) | <0.05 |
| Gender | ||||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Male | 1.18 (0.99, 1.41) | 0.07 | 0.60 (0.53, 0.68) | <0.001 | 1.54 (1.16, 2.05) | <0.05 | 1.33 (1.18, 1.49) | <0.001 |
| Grade | ||||||||
| Primary school | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| High school | 1.00 (0.55, 1.83) | 0.99 | 1.46 (0.93, 2.29) | 0.10 | 0.85 (0.34, 2.12) | 0.72 | 0.86 (0.58, 1.29) | 0.48 |
| Junior high school | 1.47 (1.01, 2.16) | <0.05 | 1.44 (1.06, 1.95) | <0.05 | 0.71 (0.41, 1.23) | 0.22 | 0.80 (0.62, 1.03) | 0.08 |
| Vocational school | 1.26 (0.64, 2.46) | 0.50 | 1.58 (0.96, 2.61) | 0.07 | 1.30 (0.46, 3.64) | 0.62 | 0.69 (0.44, 1.09) | 0.11 |
| Paternal education | ||||||||
| Primary school | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| College and above | 1.26 (0.82, 1.91) | 0.29 | 0.86 (0.61, 1.22) | 0.42 | 1.38 (0.71, 2.60) | 0.33 | 0.96 (0.70, 1.31) | 0.78 |
| Secondary school | 0.81 (0.65, 1.01) | 0.06 | 1.05 (0.89, 1.24) | 0.55 | 0.95 (0.66, 1.38) | 0.77 | 1.08 (0.92, 1.26) | 0.34 |
| Unknown | 1.56 (0.97, 2.45) | 0.06 | 0.73 (0.48, 1.08) | 0.12 | 1.30 (0.56, 2.76) | 0.51 | 0.96 (0.67, 1.37) | 0.82 |
| Maternal education | ||||||||
| Primary school | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| College and above | 0.86 (0.53, 1.38) | 0.54 | 0.93 (0.63, 1.36) | 0.72 | 1.11 (0.54, 2.18) | 0.77 | 1.06 (0.75, 1.49) | 0.76 |
| Secondary school | 0.84 (0.68, 1.04) | 0.12 | 0.93 (0.80, 1.09) | 0.38 | 0.79 (0.56, 1.11) | 0.17 | 1.19 (1.03, 1.37) | <0.05 |
| Unknown | 0.71 (0.47, 1.06) | 0.10 | 0.96 (0.71, 1.28) | 0.78 | 0.73 (0.37, 1.37) | 0.35 | 1.31 (0.99, 1.72) | 0.06 |
| Paternal occupation | ||||||||
| Blue collar | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Farmer | 1.09 (0.77, 1.54) | 0.63 | 0.66 (0.51, 0.86) | <0.05 | 1.59 (0.95, 2.66) | 0.08 | 1.24 (0.98, 1.56) | 0.07 |
| Others | 1.05 (0.78, 1.40) | 0.75 | 1.06 (0.86, 1.31) | 0.59 | 0.72 (0.43, 1.18) | 0.20 | 0.98 (0.81, 1.20) | 0.88 |
| Self-employed | 0.99 (0.68, 1.43) | 0.95 | 0.93 (0.71, 1.21) | 0.60 | 1.17 (0.66, 2.03) | 0.58 | 1.04 (0.81, 1.33) | 0.75 |
| White collar | 1.10 (0.81, 1.51) | 0.53 | 1.00 (0.79, 1.27) | 0.99 | 0.95 (0.57, 1.55) | 0.84 | 0.97 (0.78, 1.21) | 0.79 |
| Maternal occupation | ||||||||
| Blue collar | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Farmer | 0.76 (0.53, 1.09) | 0.14 | 1.27 (0.99, 1.64) | 0.06 | 0.94 (0.55, 1.61) | 0.81 | 0.92 (0.73, 1.17) | 0.51 |
| Others | 0.91 (0.69, 1.21) | 0.52 | 1.16 (0.94, 1.42) | 0.16 | 1.25 (0.79, 1.97) | 0.34 | 0.89 (0.73, 1.07) | 0.22 |
| Self-employed | 0.70 (0.47, 1.03) | 0.07 | 1.08 (0.82, 1.41) | 0.58 | 1.05 (0.59, 1.83) | 0.87 | 1.08 (0.85, 1.39) | 0.52 |
| White collar | 1.15 (0.81, 1.64) | 0.42 | 1.07 (0.80, 1.42) | 0.64 | 1.12 (0.62, 1.99) | 0.69 | 0.85 (0.65, 1.09) | 0.20 |
| LBC Caregivers | ||||||||
| Mother | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Brother or sister | 1.42 (0.79, 2.43) | 0.22 | 0.93 (0.59, 1.46) | 0.77 | 0.21 (0.01, 0.99) | 0.13 | 0.99 (0.65, 1.53) | 0.97 |
| Father | 1.04 (0.68, 1.59) | 0.84 | 0.96 (0.68, 1.33) | 0.80 | 0.52 (0.19, 1.18) | 0.15 | 1.12 (0.82, 1.53) | 0.49 |
| Grandparents | 0.84 (0.66, 1.08) | 0.17 | 0.87 (0.73, 1.04) | 0.13 | 1.14 (0.79, 1.68) | 0.50 | 1.18 (1.00, 1.39) | 0.05 |
| Other close relatives | 0.89 (0.60, 1.30) | 0.55 | 1.02 (0.77, 1.35) | 0.87 | 0.81 (0.40, 1.53) | 0.53 | 1.06 (0.81, 1.38) | 0.67 |
| Others | 1.26 (0.63, 2.35) | 0.49 | 1.02 (0.61, 1.69) | 0.94 | 0.91 (0.21, 2.67) | 0.88 | 0.87 (0.52, 1.43) | 0.58 |
| Residence experience | ||||||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| No | 1.28 (1.01, 1.62) | <0.05 | 0.95 (0.79, 1.15) | 0.62 | 0.92 (0.64, 1.31) | 0.66 | 0.92 (0.78, 1.09) | 0.35 |
| Smoking history | ||||||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| No | 0.69 (0.44, 1.11) | 0.11 | 0.55 (0.37, 0.81) | <0.05 | 1.45 (0.58, 4.87) | 0.48 | 2.47 (1.61, 3.87) | <0.001 |
| Teacher-student relationship | ||||||||
| Poor | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Good | 0.96 (0.69, 1.35) | 0.81 | 0.76 (0.58, 1.00) | <0.05 | 1.16 (0.63, 2.24) | 0.64 | 1.3 (0.99, 1.72) | 0.06 |
| Peer relations | ||||||||
| Poor | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Good | 0.35 (0.26, 0.49) | <0.001 | 1.27 (0.95, 1.73) | 0.11 | 0.54 (0.31, 0.97) | <0.05 | 2.06 (1.54, 2.79) | <0.001 |
| Family function | ||||||||
| Low | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| High | 0.14 (0.09, 0.20) | <0.001 | 0.34 (0.24, 0.48) | <0.001 | 0.99 (0.45, 2.62) | 0.98 | 11.47 (7.34, 18.76) | <0.001 |
| Medium | 0.36 (0.25, 0.52) | <0.001 | 0.7 (0.50, 0.98) | <0.05 | 1.16 (0.53, 3.04) | 0.74 | 4.43 (2.84, 7.22) | <0.001 |
Age, gender, grade, paternal education, maternal education, paternal occupation, maternal occupation, caregivers during left-behind period, residence experience and smoking history were included as covariates in the model.
aGroup1 was LBC who experienced any one or several mental health problems such as anxiety, depression, or self-injurious behavior after experiencing bullying victimization.
bGroup2 was LBC who did not experience bullying victimization but experienced any one or several mental health problems such as anxiety, depression, or self-injurious behavior.
cGroup3 was LBC who did not experience anxiety, depression, or self-injurious behavior after experiencing bullying victimization.
dGroup4 was LBC who did not experience bullying victimization and did not experience anxiety, depression, or self-injurious behavior after experiencing bullying victimization.
4. Discussion
This study systematically examined the prevalence of mental health issues among left-behind children (LBC) and non-LBC in China, focusing on the impact of bullying victimization on anxiety, depression, and self-injurious behaviors. Our findings showed that LBC experienced higher rates of bullying and were more prone to anxiety, depression, and self-injury compared to non-LBC. Among bullied LBC, nearly half displayed anxiety and depressive symptoms, and over one-third engaged in self-harm. The study identified physical bullying as a major predictor of anxiety, while verbal bullying was significantly linked to depression and self-injury. Additionally, LBC showed higher symptom severity and self-injurious behaviors, especially with suicidal intent. Notably, higher family functioning and positive teacher-student and peer relationships offered protective effects against mental health problems in bullied LBC. These findings underscore the need for early interventions to support the mental health of children and adolescents, especially those who are left behind.
Our research indicates that LBC is more susceptible to psychological health problems, including anxiety, depressive symptoms, and self-injurious behavior, aligning with previous findings on the heightened vulnerability of LBC to mental illness (17, 21). The absence of parental protection increases the susceptibility of LBC to feelings of despair and loneliness, which can gradually evolve into feelings of inferiority (60). Existing studies have also reported a higher risk of low self-esteem in LBC, which is one of the most powerful clinical predictors of depression (61). LBC shows more emotional problems, such as loneliness and inferiority, as well as a higher incidence of emotional disorders. The suppression of their emotions may exacerbate mental health problems and potentially lead to suicidal behavior (62). During this process, sufficient care and support from parents can largely eliminate these negative emotions. However, a sustained lack of such support can lead to an escalation of negative emotions, potentially resulting in internalizing problematic behaviors (2).
Our results found that the victimization rate of bullying among children and adolescents is 12.9%. This finding aligns with the range of reported bullying victimization rates in China in recent years (28, 29). Consistent with previous research, our study found that LBC who experienced bullying had a higher incidence of anxiety and depressive symptoms (35). Each type of bullying victimization was associated with anxiety and depressive symptoms among adolescents, emphasizing the detrimental effects of bullying in the development of mental health in adolescents. A longitudinal study conducted in Norway similarly found that experiences of bullying in adolescents could predict subsequent anxiety and depressive symptoms (63). The relationships between various types of bullying victimizations and mental health problems will be discussed below.
The incidence of bullying among LBC was significantly higher than in non-LBC, particularly with respect to verbal bullying. The victimization of LBC bullying is largely related to their living environment. Prolonged lack of parental care and supervision increases their susceptibility to bullying, which may lead to more frequent incidents of bullying (64). Meanwhile, LBC typically experience stronger feelings of loneliness, which also reduces their likelihood of receiving help from others when being bullied (65). There is a strong correlation between bullying and self-esteem levels. Reduced parental support may contribute to a higher likelihood of low self-esteem (21). Existing studies have shown that self-esteem serves as a partial mediator between social anxiety and school bullying victimization, as well as between school life satisfaction and school bullying victimization (66). Improving the level of self-esteem may help reduce LBC’s chances of being bullied (67).
A significant impact of bullying on depressive symptoms was found in our study. Verbal bullying is often accompanied by insults and disapproval from others. According to Beck’s diathesis-stress theory (68), bullying victimization would be considered a stressful life event that can activate cognitive vulnerabilities (specifically self-esteem), leading to significant negative outcomes. Verbal bullying, compared to other types of bullying, has been found to have a greater impact on depressive symptoms and self-injurious behavior. The hopelessness theory of depression, a cognitive diathesis-stress model of depression, proposed that negative life events could lead to negative self-inferences, which in turn, may serve as a proximal contributor to hopelessness-based depression (69). Changes in children’s negative self-perceptions can be influenced by negative evaluations from others. Alterations in self-esteem levels, resulting from these negative self-evaluations, mediate the relationship between negative evaluations in verbal bullying and the development of depressive symptoms (70, 71).
In our study, physical bullying emerged as the primary risk factor for anxiety symptoms. Physical bullying involves threats or injuries to an individual’s body and damage to personal property.
Research on interpersonal violence has identified somatic symptoms, such as headaches, chronic abdominal pain, and sleep disorders, as common consequences of physical and sexual abuse, bullying, and adolescent violence in children (72). A meta-analysis indicated that individuals targeted by bullying are at a higher risk for anxiety, depression, alcohol misuse, and substance abuse compared to those who are not targeted (37). Physical bullying poses a direct threat to the physical safety of children. Pain memory resulting from bullying is a multidimensional subjective experience, encompassing sensation (e.g., pain intensity), emotion (e.g., fear-related emotions), and contextual factors (e.g., time, place, and individuals involved) (73, 74). The encoding of pain stimuli involves the medial prefrontal cortex (mPFC) and the anterior cingulate gyrus (ACC) (75). Under the influence of situational factors, there is an overlap between pain and fear systems, resulting in avoidance behaviors (76). This overlap increases the likelihood of anxiety disorders, which are characterized by symptoms of anxiety, fear, nervousness and worry (77).
The association between family functioning and mental health is consistent with previous research, indicating that students with high family functioning are at a lower risk for developing mental health problems, including anxiety and depression symptoms (62, 78). Olson’s circular pattern theory posits that family functioning encompasses emotional connections, family rules, communication, and the effectiveness of coping with external events within the family system (79). The theory identifies three dimensions of family functioning: family intimacy, family adaptability, and family communication. Studies have shown that a strong parent-child relationship within the family environment effectively reduces the risk of emotional and behavioral problems, thereby mitigating the negative impact of parental absence on LBC (80). Conversely, adolescents who experience communication difficulties with their parents are more susceptible to psychological problems (81). Empirical analysis of longitudinal data revealed the crucial role of parent-child relationships in individual personality development, with positive relationships and support from parents helping to prevent potential negative emotional effects (11). This implies the need to foster emotional and informational understanding among family members through proactive communication practices, such as active listening, empathy, and supportive language, along with engaging in family activities. Such practices strengthen the resilience of families and individuals in the face of environmental changes and partially offset any functional deficiencies within the family (42, 80).
Consistent with previous studies, positive teacher-student and peer relationships within the school environment have been found to benefit the mental health of LBC who experience bullying (82, 83). Enhanced interpersonal quality reduces the persistence of bullying by encouraging bullied students to actively seek help (84). Additionally, supportive teacher-student relationships and peer relationships can reduce loneliness experiences by improve self-identity (85). Previous studies have demonstrated the importance of strong social connections and resources for mental health following adverse events, as they can provide motivation, alleviate loneliness, and bolster resilience during stressful situations or life adversities (86, 87). The development of supportive interpersonal relationships and accurate self-awareness in children requires significant attention and emphasis from both society and educational institutions.
In summary, our research provides valuable insights for the screening and intervention of mental health problems among children and adolescents. In addition to the above suggestions, schools and relevant education departments should promote routine mental health assessments and enhance both the evidence base and data accessibility. Advance the application of artificial intelligence in screening, monitoring and service provision within the realm of mental health.
5. Strengths and Limitations
Our study examined developmental changes in children and adolescents aged 8-19 years to provide guidance for early prevention and intervention throughout their growth. Meanwhile, according to the ecological systems theory (88), we considered the impact of family, school and significant others on the mental health of children and adolescents and included these variables in our analysis. Our results also reveal that self-injurious behaviors with suicidal intent are more prevalent among LBC. his underscores the need for policymakers and mental health professionals to implement comprehensive mental health screening and care services for LBC and other children in similar environments. Several limitations should be noted. First, our study is based on a cross-sectional survey. Longitudinal data is still needed to establish causal relationships between bullying victimization and mental health problems. Second, our study focused solely on bullying victimization without addressing other forms of bullying. In addition, while previous research highlights the significance of family environment and economic status on LBC’s physical and mental health (62), we did not collect data on confounding factors such as family economic status, parenting styles, and self-evaluation. Future studies should aim to include these factors for a more comprehensive analysis.
6. Conclusions
Our research indicates that the incidence of mental health problems among Chinese LBC is relatively high. Specifically, LBC with a history of smoking and those whose primary caregivers are not parents, grandparents, or siblings warrant special attention. Furthermore, as a significant risk factor for mental health problems, bullying victimization necessitates attention due to its detrimental effects: physical bullying exacerbates anxiety symptoms, verbal bullying contributes to depressive symptoms, and self-injurious behaviors. High family functioning and positive school interpersonal relationships are crucial protective factors in the psychological development of children and adolescents. Future studies should develop various risk prediction models for a broader range of mental health problems, focusing on psychological interventions tailored to the specific characteristics of different populations.
Acknowledgments
We would like to thank our colleagues and volunteers for their support.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (No. 81801359 to XL), Swedish Research Council (No. 2018-00648 to XL), West China Hospital COVID-19 Epidemic Science and Technology Project (No. HX-2019-nCoV-019 to WZ), and Sichuan University Emergency Grant (No. 2020scunCoVyingji1005 to WZ).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
WZ: Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. YF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. SZ: Data curation, Formal analysis, Software, Writing – original draft. XL: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing. YJ: Conceptualization, Investigation, Writing – review & editing. YY: Conceptualization, Formal analysis, Investigation, Software, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Jingzhong Y, Lu P. Differentiated childhoods: impacts of rural labor migration on left-behind children in China. J Peasant Stud. (2011) 38:355–77. doi: 10.1080/03066150.2011.559012 [DOI] [PubMed] [Google Scholar]
- 2. Wang L, Mesman J. Child development in the face of rural-to-urban migration in China: A meta-analytic review. Perspect Psychol Sci. (2015) 10:813–31. doi: 10.1177/1745691615600145 [DOI] [PubMed] [Google Scholar]
- 3. Duan CR. A study on children left behind. Population Res. (2005) 2005:29–36. doi: 10.3969/j.issn.1000-6087.2005.01.004 [DOI] [Google Scholar]
- 4. Fan F, Su L, Gill MK, Birmaher B. Emotional and behavioral problems of Chinese left-behind children: a preliminary study. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:655–64. doi: 10.1007/s00127-009-0107-4 [DOI] [PubMed] [Google Scholar]
- 5. Luo J, Peng X, Zong R, Yao K, Hu R, Du Q, et al. The status of care and nutrition of 774 left-behind children in rural areas in China. Public Health Rep. (2008) 123:382–9. doi: 10.1177/003335490812300319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Amato PR. Children's adjustment to divorce: Theories, hypotheses, and empirical support. J Marriage Family. (1993) 55:23–38. doi: 10.2307/352954 [DOI] [Google Scholar]
- 7. Turecki G, Meaney MJ. Effects of the social environment and stress on glucocorticoid receptor gene methylation: A systematic review. Biol Psychiatry. (2016) 79:87–96. doi: 10.1016/j.biopsych.2014.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farrell C, Doolin K, O' Leary N, Jairaj C, Roddy D, Tozzi L, et al. DNA methylation differences at the glucocorticoid receptor gene in depression are related to functional alterations in hypothalamic-pituitary-adrenal axis activity and to early life emotional abuse. Psychiatry Res. (2018) 265:341–8. doi: 10.1016/j.psychres.2018.04.064 [DOI] [PubMed] [Google Scholar]
- 9. Zeegers MAJ, Colonnesi C, Stams GJM, Meins E. Mind matters: A meta-analysis on parental mentalization and sensitivity as predictors of infant-parent attachment. Psychol Bull. (2017) 143:1245–72. doi: 10.1037/bul0000114 [DOI] [PubMed] [Google Scholar]
- 10. Koopmans Y, Nelemans SA, Bosmans G, Van Den Noortgate W, Van Leeuwen K, Goossens L. Perceived parental support and psychological control, DNA methylation, and loneliness: longitudinal associations across early adolescence. J Youth Adolesc. (2023) 52:1995–2011. doi: 10.1007/s10964-023-01822-6 [DOI] [PubMed] [Google Scholar]
- 11. Cao X, Liu X. Understanding the role of parent−Child relationships in conscientiousness and neuroticism development among chinese middle school students: A cross-lagged model. Behav Sci (Basel). (2023) 13:876–91. doi: 10.3390/bs13100876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cao X, Ji S. Bidirectional relationship between self-rated health and the big five personality traits among Chinese adolescents: a two-wave cross-lagged study. Humanities Soc Sci Commun. (2024) 11:200. doi: 10.1057/s41599-024-02699-x [DOI] [Google Scholar]
- 13. Barbour RF. Attachment and Loss. Vol. 1. Attachment. By John Bowlby. London: The Hogarth Press and Institute of Psycho-Analysis. 1969. Pp. 428. Price 63s. British Journal of Psychiatry. (1970) 116:102-3. doi: 10.1192/bjp.116.530.102 [DOI] [Google Scholar]
- 14. Keizer R, Helmerhorst KOW, van Rijn-van Gelderen L. Perceived quality of the mother-adolescent and father-adolescent attachment relationship and adolescents' Self-esteem. J Youth Adolesc. (2019) 48:1203–17. doi: 10.1007/s10964-019-01007-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moreno-Manso JM, García-Baamonde ME, Guerrero-Barona E, Blázquez-Alonso M, Pozueco-Romero JM, Godoy-Merino MJ. Psychosocial adaptation of young victims of physical neglect. J Child Abuse Rev. (2017) 26:364–74. doi: 10.1002/car.v26.5 [DOI] [Google Scholar]
- 16. Hildyard KL, Wolfe DA. Child neglect: developmental issues and outcomes. Child Abuse Negl. (2002) 26:679–95. doi: 10.1016/s0145-2134(02)00341-1 [DOI] [PubMed] [Google Scholar]
- 17. Hetherington EM, Bridges M, Insabella GM. What matters? What does not? Five perspectives on the association between marital transitions and children's adjustment. Am Psychol. (1998) 53:167–84. doi: 10.1037//0003-066x.53.2.167 [DOI] [PubMed] [Google Scholar]
- 18. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. (2012) 38:734–40. doi: 10.1093/schbul/sbs049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kennedy SC, Tripodi SJ, Pettus-Davis C. The relationship between childhood abuse and psychosis for women prisoners: assessing the importance of frequency and type of victimization. Psychiatr Q. (2013) 84:439–53. doi: 10.1007/s11126-013-9258-2 [DOI] [PubMed] [Google Scholar]
- 20. Sitko K, Bentall RP, Shevlin M, O'Sullivan N, Sellwood W. Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: an analysis of the National Comorbidity Survey. Psychiatry Res. (2014) 217:202–9. doi: 10.1016/j.psychres.2014.03.019 [DOI] [PubMed] [Google Scholar]
- 21. Tang W, Wang G, Hu T, Dai Q, Xu J, Yang Y, et al. Mental health and psychosocial problems among Chinese left-behind children: A cross-sectional comparative study. J Affect Disord. (2018) 241:133–41. doi: 10.1016/j.jad.2018.08.017 [DOI] [PubMed] [Google Scholar]
- 22. Olweus D. School bullying: development and some important challenges. Annu Rev Clin Psychol. (2013) 9:751–80. doi: 10.1146/annurev-clinpsy-050212-185516 [DOI] [PubMed] [Google Scholar]
- 23. Wan Ismail WS, Nik Jaafar NR, Sidi H, Midin M, Shah SA. Why do young adolescents bully? Experience in Malaysian schools. Compr Psychiatry. (2014) 55 Suppl 1:S114–20. doi: 10.1016/j.comppsych.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 24. Wang J, Nansel TR, Iannotti RJ. Cyber and traditional bullying: differential association with depression. J Adolesc Health. (2011) 48:415–7. doi: 10.1016/j.jadohealth.2010.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cole DA, Zelkowitz RL, Nick E, Martin NC, Roeder KM, Sinclair-McBride K, et al. Longitudinal and incremental relation of cybervictimization to negative self-cognitions and depressive symptoms in young adolescents. J Abnorm Child Psychol. (2016) 44:1321–32. doi: 10.1007/s10802-015-0123-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lv J, Ren H, Guo X, Meng C, Fei J, Mei H, et al. Nomogram predicting bullying victimization in adolescents. J Affect Disord. (2022) 303:264–72. doi: 10.1016/j.jad.2022.02.037 [DOI] [PubMed] [Google Scholar]
- 27. Xiao Y, Jiang L, Yang R, Ran H, Wang T, He X, et al. Childhood maltreatment with school bullying behaviors in Chinese adolescents: A cross-sectional study. J Affect Disord. (2021) 281:941–8. doi: 10.1016/j.jad.2020.11.022 [DOI] [PubMed] [Google Scholar]
- 28. Li L, Jing R, Jin G, Song Y. Longitudinal associations between traditional and cyberbullying victimization and depressive symptoms among young Chinese: A mediation analysis. Child Abuse Negl. (2023) 140:106141. doi: 10.1016/j.chiabu.2023.106141 [DOI] [PubMed] [Google Scholar]
- 29. Yu Q, Wu S, Twayigira M, Luo X, Gao X, Shen Y, et al. Prevalence and associated factors of school bullying among Chinese college students in Changsha, China. J Affect Disord. (2022) 297:62–7. doi: 10.1016/j.jad.2021.10.010 [DOI] [PubMed] [Google Scholar]
- 30. Baiden P, Stewart SL, Fallon B. The mediating effect of depressive symptoms on the relationship between bullying victimization and non-suicidal self-injury among adolescents: Findings from community and inpatient mental health settings in Ontario, Canada. Psychiatry Res. (2017) 255:238–47. doi: 10.1016/j.psychres.2017.05.018 [DOI] [PubMed] [Google Scholar]
- 31. Li J, Jin Y, Xu S, Wilson A, Chen C, Luo X, et al. Effects of bullying on anxiety, depression, and posttraumatic stress disorder among sexual minority youths: network analysis. JMIR Public Health Surveill. (2023) 9:e47233. doi: 10.2196/47233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Williford A, Boulton A, Noland B, Little TD, Kärnä A, Salmivalli C. Effects of the KiVa anti-bullying program on adolescents' depression, anxiety, and perception of peers. J Abnorm Child Psychol. (2012) 40:289–300. doi: 10.1007/s10802-011-9551-1 [DOI] [PubMed] [Google Scholar]
- 33. Selkie EM, Kota R, Chan YF, Moreno M. Cyberbullying, depression, and problem alcohol use in female college students: a multisite study. Cyberpsychol Behav Soc Netw. (2015) 18:79–86. doi: 10.1089/cyber.2014.0371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Menesini E, Modena M, Tani F. Bullying and victimization in adolescence: concurrent and stable roles and psychological health symptoms. J Genet Psychol. (2009) 170:115–33. doi: 10.3200/gntp.170.2.115-134 [DOI] [PubMed] [Google Scholar]
- 35. Lai W, Li W, Guo L, Wang W, Xu K, Dou Q, et al. Association between bullying victimization, coping style, and mental health problems among Chinese adolescents. J Affect Disord. (2023) 324:379–86. doi: 10.1016/j.jad.2022.12.080 [DOI] [PubMed] [Google Scholar]
- 36. Chan HCO, Wong DSW. The overlap between school bullying perpetration and victimization: assessing the psychological, familial, and school factors of chinese adolescents in hong kong. J Child Family Stud. (2015) 24:3224–34. doi: 10.1007/s10826-015-0125-7 [DOI] [Google Scholar]
- 37. Moore SE, Norman RE, Suetani S, Thomas HJ, Sly PD, Scott JG. Consequences of bullying victimization in childhood and adolescence: A systematic review and meta-analysis. World J Psychiatry. (2017) 7:60–76. doi: 10.5498/wjp.v7.i1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ford R, King T, Priest N, Kavanagh A. Bullying and mental health and suicidal behaviour among 14- to 15-year-olds in a representative sample of Australian children. Aust N Z J Psychiatry. (2017) 51:897–908. doi: 10.1177/0004867417700275 [DOI] [PubMed] [Google Scholar]
- 39. van Geel M, Vedder P, Tanilon J. Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: a meta-analysis. JAMA Pediatr. (2014) 168:435–42. doi: 10.1001/jamapediatrics.2013.4143 [DOI] [PubMed] [Google Scholar]
- 40. Peng Z, Klomek AB, Li L, Su X, Sillanmäki L, Chudal R, et al. Associations between Chinese adolescents subjected to traditional and cyber bullying and suicidal ideation, self-harm and suicide attempts. BMC Psychiatry. (2019) 19:324. doi: 10.1186/s12888-019-2319-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zhang H, Chi P, Long H, Ren X. Bullying victimization and depression among left-behind children in rural China: Roles of self-compassion and hope. Child Abuse Negl. (2019) 96:104072. doi: 10.1016/j.chiabu.2019.104072 [DOI] [PubMed] [Google Scholar]
- 42. Eslinger PJ, Anders S, Ballarini T, Boutros S, Krach S, Mayer AV, et al. The neuroscience of social feelings: mechanisms of adaptive social functioning. Neurosci Biobehav Rev. (2021) 128:592–620. doi: 10.1016/j.neubiorev.2021.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zeanah CH, Gleason MM. Annual research review: Attachment disorders in early childhood–clinical presentation, causes, correlates, and treatment. J Child Psychol Psychiatry. (2015) 56:207–22. doi: 10.1111/jcpp.12347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wen X, Shu Y, Qu D, Wang Y, Cui Z, Zhang X, et al. Associations of bullying perpetration and peer victimization subtypes with preadolescent's suicidality, non-suicidal self-injury, neurocognition, and brain development. BMC Med. (2023) 21:141. doi: 10.1186/s12916-023-02808-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yan H, Chen J, Huang J. School bullying among left-behind children: the efficacy of art therapy on reducing bullying victimization. Front Psychiatry. (2019) 10:40. doi: 10.3389/fpsyt.2019.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bear G, Yang C, Harris A, Mantz L, Boyer D, Hearn S. Technical Manual for Delaware School Surveys. (2019) (University of Delaware and Delaware Department of Education; ). [Google Scholar]
- 47. Xie JS, Lv YX, Bear GG, Yang C, Marshall SJ, Gong R, et al. Revision of chinese version of delaware bullying victimization scale-student in adolescents. Chin J Clin Psychol. (2018) 26:259–63. doi: 10.16128/j.cnki.1005-3611.2018.02.011 [DOI] [Google Scholar]
- 48. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 49. Seo JG, Park SP. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. (2015) 16:97. doi: 10.1186/s10194-015-0583-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. Bmj. (2019) 365:l1476. doi: 10.1136/bmj.l1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021 [DOI] [PubMed] [Google Scholar]
- 53. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Cmaj. (2012) 184:E191–6. doi: 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Moriarty AS, Gilbody S, McMillan D, Manea L. Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): a meta-analysis. Gen Hosp Psychiatry. (2015) 37:567–76. doi: 10.1016/j.genhosppsych.2015.06.012 [DOI] [PubMed] [Google Scholar]
- 55. GE MG, Yibing Y. The development of junior high school students' Perceived school climate inventory. J psychol Sci. (2006) 29:460–4. doi: 10.16719/j.cnki.1671-6981.2006.02.056 [DOI] [Google Scholar]
- 56. Chen JL, Kennedy C, Kools S, Slaughter RE, Franck L, Kong SK, et al. Culturally appropriate family assessment: analysis of the Family Assessment Device in a pediatric Chinese population. J Nurs Meas. (2003) 11:41–60. doi: 10.1891/jnum.11.1.41.52063 [DOI] [PubMed] [Google Scholar]
- 57. Li Y, Wang Y, Jiang J, Valdimarsdóttir UA, Fall K, Fang F, et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol Med. (2021) 51:1952–4. doi: 10.1017/s0033291720001555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Vijayakumar N, Whittle S. A systematic review into the role of pubertal timing and the social environment in adolescent mental health problems. Clin Psychol Rev. (2023) 102:102282. doi: 10.1016/j.cpr.2023.102282 [DOI] [PubMed] [Google Scholar]
- 59. Houtepen LC, Heron J, Suderman MJ, Fraser A, Chittleborough CR, Howe LD. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: A prospective cohort study in the UK. PLoS Med. (2020) 17:e1003031. doi: 10.1371/journal.pmed.1003031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wang J, Zou J, Luo J, Liu H, Yang Q, Ouyang Y, et al. Mental health symptoms among rural adolescents with different parental migration experiences: A cross-sectional study in China. Psychiatry Res. (2019) 279:222–30. doi: 10.1016/j.psychres.2019.03.004 [DOI] [PubMed] [Google Scholar]
- 61. Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. (2013) 139:213–40. doi: 10.1037/a0028931 [DOI] [PubMed] [Google Scholar]
- 62. Fellmeth G, Rose-Clarke K, Zhao C, Busert LK, Zheng Y, Massazza A, et al. Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet. (2018) 392:2567–82. doi: 10.1016/s0140-6736(18)32558-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ringdal R, Bjørnsen HN, Espnes GA, Bradley Eilertsen ME, Moksnes, et al. Bullying, social support and adolescents' mental health: Results from a follow-up study. Scand J Public Health. (2021) 49:309–16. doi: 10.1177/1403494820921666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Peprah P, Asare BY, Nyadanu SD, Asare-Doku W, Adu C, Peprah J, et al. Bullying Victimization and Suicidal Behavior among adolescents in 28 Countries and Territories: A Moderated Mediation Model. J Adolesc Health. (2023) 73:110–7. doi: 10.1016/j.jadohealth.2023.01.029 [DOI] [PubMed] [Google Scholar]
- 65. Ling H, Fu E, Zhang J-R. Effects of separation age and separation duration among left-behind children in China. Soc Behav Pers. (2015) 43:241–53. doi: 10.2224/sbp.2015.43.2.241 [DOI] [Google Scholar]
- 66. Triantoro S, Yunita A. The efficacy of art therapy to reduce anxiety among bullying victims. Int J Res Stud Psychol. (2014) 3:77–88. doi: 10.5861/ijrsp.2014.829 [DOI] [Google Scholar]
- 67. Tsaousis I. The relationship of self-esteem to bullying perpetration and peer victimization among schoolchildren and adolescents: A meta-analytic review. Aggression Violent Behav. (2016) 31:186–99. doi: 10.1016/j.avb.2016.09.005 [DOI] [Google Scholar]
- 68. Disner SG, Beevers CG, Haigh EA, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. (2011) 12:467–77. doi: 10.1038/nrn3027 [DOI] [PubMed] [Google Scholar]
- 69. Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. psychol Rev. (1989) 96:358–72. doi: 10.1037/0033-295X.96.2.358 [DOI] [Google Scholar]
- 70. Cole DA, Martin JM, Powers B. A competency-based model of child depression: a longitudinal study of peer, parent, teacher, and self-evaluations. J Child Psychol Psychiatry. (1997) 38:505–14. doi: 10.1111/j.1469-7610.1997.tb01537.x [DOI] [PubMed] [Google Scholar]
- 71. Zhong M, Huang X, Huebner ES, Tian L. Association between bullying victimization and depressive symptoms in children: The mediating role of self-esteem. J Affect Disord. (2021) 294:322–8. doi: 10.1016/j.jad.2021.07.016 [DOI] [PubMed] [Google Scholar]
- 72. Rivara F, Adhia A, Lyons V, Massey A, Mills B, Morgan E, et al. The effects of violence on health. Health Aff (Millwood). (2019) 38:1622–9. doi: 10.1377/hlthaff.2019.00480 [DOI] [PubMed] [Google Scholar]
- 73. Williams ACC, Craig KD. Updating the definition of pain. Pain. (2016) 157:2420–3. doi: 10.1097/j.pain.0000000000000613 [DOI] [PubMed] [Google Scholar]
- 74. Babel P. The influence of state and trait anxiety on the memory of pain. Pain Med. (2017) 18:2340–9. doi: 10.1093/pm/pnw354 [DOI] [PubMed] [Google Scholar]
- 75. Tseng MT, Kong Y, Eippert F, Tracey I. Determining the neural substrate for encoding a memory of human pain and the influence of anxiety. J Neurosci. (2017) 37:11806–17. doi: 10.1523/jneurosci.0750-17.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vogt BA. Pain and emotion interactions in subregions of the cingulate gyrus. Nat Rev Neurosci. (2005) 6:533–44. doi: 10.1038/nrn1704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Craske MG, Stein MB. Anxiety. Lancet. (2016) 388:3048–59. doi: 10.1016/s0140-6736(16)30381-6 [DOI] [PubMed] [Google Scholar]
- 78. Lema-Gómez L, Arango-Paternina CM, Eusse-López C, Petro J, Petro-Petro J, López-Sánchez M, et al. Family aspects, physical fitness, and physical activity associated with mental-health indicators in adolescents. BMC Public Health. (2021) 21:2324. doi: 10.1186/s12889-021-12403-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Olson DH. Circumplex Model of Marital and Family Systems: Assessing family functioning. In: Normal family processes, 2nd ed. The Guilford Press, New York, NY, US: (1993). p. 104–37. [Google Scholar]
- 80. Havighurst SS, Radovini A, Hao B, Kehoe CE. Emotion-focused parenting interventions for prevention and treatment of child and adolescent mental health problems: a review of recent literature. Curr Opin Psychiatry. (2020) 33:586–601. doi: 10.1097/yco.0000000000000647 [DOI] [PubMed] [Google Scholar]
- 81. Silva K, Robles RJ, Friedrich E, Fisher Thiel M, Ford CA, Miller VA. Stereotyped beliefs about adolescents and parent and teen well-being: the role of parent-teen communication. J Early Adolescence. (2020) 41:886–904. doi: 10.1177/0272431620961446 [DOI] [Google Scholar]
- 82. Biernbaum MA, Lotyczewski BS. Bullying and School Climate: Associations and Group Differences. (2015) (Goodman Street, Suite D103, Rochester, NY: Children's Institute, 274 N.). [Google Scholar]
- 83. Montero-Carretero C, Pastor D, Santos-Rosa FJ, Cervelló E. School climate, moral disengagement and, empathy as predictors of bullying in adolescents. Front Psychol. (2021) 12:656775. doi: 10.3389/fpsyg.2021.656775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Gregory A, Cornell D, Fan X, Sheras P, Shih T.-H, Huang F. Authoritative school discipline: High school practices associated with lower bullying and victimization. J Educ Psychol. (2010) 102:483–96. doi: 10.1037/a0018562 [DOI] [Google Scholar]
- 85. Fuxia C, Fujuan Z. The characteristics and relationships of peer attchment, self-concept and loneliness of students in reform school. psychol Dev Educ. (2010) 26:73–80. doi: 10.16187/j.cnki.issn1001-4918.2010.01.012 [DOI] [Google Scholar]
- 86. Cruwys T, Haslam SA, Dingle GA, Haslam C, Jetten J. Depression and social identity: an integrative review. Pers Soc Psychol Rev. (2014) 18:215–38. doi: 10.1177/1088868314523839 [DOI] [PubMed] [Google Scholar]
- 87. Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. (2020) 291:113216. doi: 10.1016/j.psychres.2020.113216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ceci SJ. Urie bronfenbrenner (1917-2005). Am Psychol. (2006) 61:173–4. doi: 10.1037/0003-066x.61.2.173 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.