Abstract
Children’s exposure to outlets selling, and outdoor advertisements marketing, unhealthy foods is an important risk factor for obesity. Yet few policies address the food retail and/or outdoor advertising environment, and research about children’s perceptions is limited, especially in low- and middle-income countries. We used a participatory, multimodal visual/verbal approach to explore urban-dwelling South African primary school students’ perceptions of unhealthy food outlets and outdoor advertisements they encountered on their journeys to school. Forty-one grade 7 students aged 11–14 years participated in drawing and/or photography activities and elicitation discussions. A mixed-methods, triangulated analysis involving the content analysis and extraction of data from research artefacts (33 journey to school drawings and 10 food advertisement photo collages) and thematic analysis of discussion transcripts was conducted. Drawings depicted 175 food outlets, two-thirds (64%) of which sold only unhealthy foods and 125 advertisements, most of which marketed unhealthy food. Unbranded, deep-fried foods prepared and sold by informal traders and independent shops were prominent. Informal and independent traders also sold unhealthy branded foods. Advertisements were primarily for unhealthy foods, especially branded, sugar-sweetened beverages. Participants thought extensive advertising bans, regulation of the sale of unhealthy food to children and other measures were needed to promote children’s health in urban contexts. The results point to the need for food system-wide approaches that address multiple commercial determinants of health, including ‘big food’ advertising, unhealthy food sales by informal and independent traders and programs to address socio-economic influences such as poverty, unemployment and parents’ poor work conditions.
Keywords: food environment, outdoor food marketing, informal trade, food policy, unhealthy food advertising, obesity prevention, commercial determinants of child nutrition, South Africa
Contribution to Health Promotion.
Urban South African primary school students are exposed primarily to unhealthy food outlets and advertisements as they journey to school.
Informal traders and independent shops are a key source of exposure and access to unbranded, unhealthy foods.
Informal traders and independent shops also sell and advertise ‘big food’ brands to children.
Mandatory policies and laws that comprehensively restrict children’s exposure to unhealthy food marketing and sales are urgently needed.
Food system-wide approaches addressing commercial determinants of children’s nutritional health beyond unhealthy food marketing and sales (e.g. parents’ work conditions and income) are also urgently needed.
BACKGROUND
Children’s attitudes to and knowledge about food, including beverages, and food behaviours such as purchasing and consuming, are shaped by food environments—the physical and social contexts within which people interact with food (Carducci et al., 2021). Commercial entities spanning ‘big food’ (multinational food and beverage companies) to micro-enterprises such as informal traders, purposively shape food environments through the targeted sale and marketing of particular foods, to maximize their profits (Igumbor et al., 2012; da Costa Peres et al., 2020; Gilmore et al., 2023). The influence of food marketing is a composite of power (techniques used to appeal) and exposure (frequency of encounters with advertising) (WHO, 2012). Marketing influence interacts with access to foods, including if, where and at what prices different foods are sold, and other socio-economic factors, to shape people’s food practices, often by encouraging the consumption of unhealthy foods (Walton et al., 2009; Velazquez et al., 2019; Mofokeng, 2023).
What constitutes unhealthy food is contested and often poorly defined. However, the term is widely accepted, and will be used herein, to refer to (sugar and fat) energy-dense, nutrient-poor foods, as well as those that have high sodium content (Chung et al., 2022). Research about children’s exposure to unhealthy food marketing has focused on television marketing to young children (Cairns et al., 2013; WHO, 2022). Marketing regulations have similarly focused on television advertising (Burgaz et al., 2023). Although mandatory (but not voluntary) regulation of advertising during children’s television viewing times has sometimes proven effective in reducing exposure to unhealthy food adverts, it is not yet clear whether this leads to reduced consumption of unhealthy foods (Boyland et al., 2022; Burgaz et al., 2023). The narrow focus on television advertising is insufficient to address the detrimental health effects of unhealthy food marketing such as obesity. Advertising spills over to other media including internet-connected devices (Freeman et al., 2016; Burgaz et al., 2023) and outdoor environments, to which children are repeatedly exposed, including during their daily journeys to and from school (Kelly et al., 2008). Outdoor food and beverage advertising has been recognized as an important area for research and policy intervention for over a decade (Kelly et al., 2008). The importance of considering exposure to unhealthy food outlets and advertisements in unison has been highlighted more recently (Velazquez et al., 2019).
Surveys on the quantity and nature of advertising surrounding schools have been conducted in diverse countries including the Philippines and Mongolia (Kelly et al., 2015), Indonesia (Puspikawati et al., 2021), Mexico (Barquera et al., 2018), Australia (Kelly et al., 2008), New Zealand (Signal et al., 2017), Uganda (Dia et al., 2021) and Canada (Velazquez et al., 2019). These studies have all found branded food advertisements in the vicinity of most schools in their samples, and that most (> 80%) of the advertisements were for unhealthy foods. Several studies have reported increasing the density of advertisements in the areas closest to schools and other child-frequented areas (Chacon et al., 2015; Velazquez et al., 2019; Puspikawati et al., 2021). In Canada, the presence of limited-service food outlets increased advertising prevalence (Velazquez et al., 2019).
Direct associations between the presence of unhealthy food outlets near schools and the increasing prevalence of students affected by obesity were reported in several studies in a systematic review (da Costa Peres et al., 2020). More recent evidence concurs and suggests that food sellers may target socio-economically marginalized children. For example, in China, the odds of a child being affected by obesity increased by 1.49, if there was an above-average number of convenience stores within an 800-m street network buffer of their school (Zhou et al., 2020). A Chilean study found an 88% higher risk of having unhealthy food outlets in low socio-economic compared to high socio-economic neighbourhoods; unhealthy food outlets were found in higher numbers and in closer proximity to schools in the low socio-economic status neighbourhoods (Kain et al., 2024). These findings demonstrate the importance of research that considers outdoor food advertising and food outlets simultaneously.
Gaps and study aim
While evidence regarding outdoor food advertising and outlets has developed rapidly in the past decade, most studies have been conducted in high-income countries. Many have focused on formal advertisements (e.g. billboards, fixed signs) for branded foods, which may not encompass all advertisements, especially in low- and middle-income countries (LMICs) such as South Africa, where much food is marketed and sold through the informal sector (Skinner, 2016; Hodgson et al., 2018). Informal food retail is a significant source of employment, especially for women, and contributes significantly to increasing food security in economically deprived households (Skinner, 2016). Informal traders who make their livelihoods selling unhealthy food, do so in a context where unemployment is high and there are few alternative livelihood options. Recognizing the need for socio-economic development and the contributions of informal trade to it, the South African Constitution enshrines the rights of small businesses, including independent shop owners and informal traders, to market their goods (Hodgson et al., 2018). Qualitative research, including participatory approaches that capture children’s perspectives of their food environments, are needed to provide a more complete picture of food environments (Carducci et al., 2021). We therefore investigated South African children’s perceptions of: (i) their everyday outdoor food environments, with a focus on exposure to food outlets and advertisements on the journey to and from school, and (ii) interventions needed to protect children from the harms of unhealthy food advertisements and outlets.
METHODS
We conducted a participatory, multimodal visual/verbal study to generate data about urban South African primary school students’ perceptions of their food environments. A qualitatively driven, mixed-methods approach was employed to analyse the data (Morse, 2016). The study was approved by the Gauteng Department of Education (10 March 2023, ref 8/4/4/1/2) and the University of Witwatersrand Human Research Ethics Committee (Medical) (Approval number M230102 MED22-12-012).
Setting
In South Africa, a middle-income country, one in five adolescents is affected by overweight or obesity (Nwosu et al., 2022). Urban food environments promote unhealthy weight gain, especially in areas of socio-economic marginalization (Ndlovu et al., 2018). For example, the density of fast-food outlets increases with socio-economic deprivation, and supermarket density is highest in the least deprived areas (Ndlovu et al., 2018). This is despite the government’s endorsement of the World Health Organization’s guideline to protect children from the harms of unhealthy food marketing (WHO, 2023) and several initiatives to regulate the marketing and manufacture of unhealthy foods.
A Health Promotion Levy mandating taxation of beverages containing > 4 g sugar per litre, was introduced in 2018. It was associated with significant reductions in sugar-sweetened beverage (SSB) purchases, which were greater amongst socio-economically marginalized populations (Hofman et al., 2021). In 2016, the South African government introduced regulations mandating upper limits on the salt content of processed foods, which was associated with a reduction in sodium consumption (Charlton et al., 2021). Mandatory front-of-package warning labels for foods containing added fat, sugar or salt above a threshold level, and banning child-directed marketing of foods with front-of-package warning labels, were proposed in 2023. However, the regulation containing these provisions, in which the protection of children is a key guiding principle, had not been adopted at the time of writing (South African Government Department of Health, 2023).
In 2008, a child-focused, voluntary code of conduct, the South African Marketing to Children pledge, was introduced. Signatories volunteered to minimize their television and close-to-school marketing of unhealthy foods and avoid using child-directed characters such as cartoons in their advertisements (Yamoah et al., 2021). Evidence suggests that this pledge, which allows ‘big food’ companies to regulate themselves, has been ineffective. Children continue to be exposed to advertising for unhealthy foods on television, including during family viewing time (Yamoah et al., 2021). A study of outdoor advertisements in a large township near Johannesburg, South Africa’s largest urban metropolis, found that SSB advertisements targeted children because they were strategically placed in close proximity to schools, and that most vendors sold and most schools advertised SSBs (Moodley et al., 2015). Another study in urban primary schools reported that more than half of sampled schools sold SSBs within their premises and one-third had SSB advertisements, in 2019 (Erzse et al., 2021).
Participants
Participants were a convenience sample of 41, grade 7 students from five primary schools in Johannesburg, which were purposively sampled for diversity in multidimensional deprivation. South African public schools are classified into quintiles of multidimensional deprivation. Quintile 1 (Q1) schools are located in the most, and quintile 5 (Q5) schools in the least, deprived areas. Quintile 1–3 schools do not charge fees and provide meals through the national school nutrition programme. Quintile 4 and 5 schools receive less government funding and may charge fees and/or provide school meals (South African Government Department of Basic Education, 2023). High levels of economic inequality in South Africa—the richest 10% and 20% of the South African population, respectively, own 85% of wealth and earn 68% of income—mean that Q5 schools are in economically privileged, whereas Q1–4 schools are in economically deprived areas.
Following approval by the Gauteng Department of Education, we purposively selected schools for diversity in deprivation quintiles and invited them to participate by approaching the school principal. Five primary school principals agreed and provided consent for us to invite grade 7 students (aged 11–14 years) from their schools to participate in group drawing or photo collage activities and related elicitation interviews. One school each were in Q1 (School 1), Q5 (School 5) and Q4 (School 4) and two were in Q2 (Schools 2 and 3). From each school, potential participants were invited to participate by their teachers. Those students who volunteered were given an information and consent form for their parents to sign. An assent form was signed by each child immediately before they participated in the research activities, after a verbal explanation of the study by a researcher.
Data collection
Five mixed-gender group drawing activities (one per school), followed by drawing elicitation interviews, were conducted with 34 of the participants (range 4–11 per group). G.C., an experienced participatory researcher who has worked extensively with children, facilitated the activities with assistance from A.E. (both women), and a translator proficient in English, Isizulu and Sesotho K.M. (man) or L.S. (woman). Each participant was asked to draw their journey to school showing the places where food was sold, and as a second step to place a sticker where they saw food advertisements. The researchers annotated the food outlets and advertisements on participants’ drawings during informal conversations. Group drawing elicitation interviews were then conducted in a combination of English (school language for all participants), Isizulu or Setswana (home languages of most participants), depending on the participants’ choice.
Ten students from School 4, three of whom also participated in the group drawing activities, participated in photography activities. They attended a Saturday photography workshop, were provided digital cameras and asked to photograph food advertisements they saw while journeying to and from school for 1 week. For ethical reasons, participants were asked not to include people in their food advertisement photographs. At a second Saturday workshop, one week later, the participants made collages from print-outs of the food advertising photographs they had taken and discussed their collages and their broader food environments. Participants’ perceptions about what should be done to protect children from unhealthy food marketing were also elicited in both drawing and photo discussions.
Dataset and analysis
The dataset consisted of 33 journey to school drawings; 10 photo collages; descriptions of the content of each artefact (drawing or collage) written by M.B. and six English-language transcripts of audio-recorded elicitation discussions (mean 85 min; range 59–131 min) prepared by a multi-lingual assistant. The combined dataset was analysed by M.B. using mixed methods. Content analysis and systematic extraction of data about food outlets and advertisements from journey to school drawings and transcripts of related discussions was the core method. It was supplemented with a thematic analysis of discussion transcripts and artefact content descriptions. Results from the different analytical approaches were triangulated to enhance validity (Morse, 2015) and integrated into the results narrative (Morse, 2016).
Discussion transcripts were analysed thematically, using an abductive technique, that is, drawing on both theory and data to develop codes and themes (Timmermans and Tavory, 2012). A preliminary set of general codes was developed deductively to capture relevant themes in the food environments literature. Data were read and re-read. General codes were applied to the data during the second and third readings. Simultaneously, specific codes were developed abductively and nested within general codes, which were revised where necessary. M.B. developed the codebook (see Supplementary File S1 for the final version) and coded all data using NVivo version 20.
The final codebook included general and specific codes for food, food outlets and food advertisement types (Supplementary File S1), which were developed deductively. Data collected from journey to school drawings within these three codes were systematically extracted by M.B. and entered into a spreadsheet. Any food, outlet or advert that was described in insufficient detail to categorize according to one of the types in the coding frame was classified as ‘unspecified’. Food outlets and advertisements that children included in their drawings but indicated in the discussions that they did not see on their journeys to school were excluded. The codebook and preliminary content and thematic analysis findings were presented to the interdisciplinary research group for peer debriefing, a strategy for increasing internal validity (i.e. ensuring evidence presented supports claims being made) in qualitative research (Morse, 2015). M.B. then revised the codebook based on peer feedback and extracted the data again, using the revised, final codebook (Supplementary File S1). She compared data extracted in the two rounds, documented reasons for discrepancies and prepared a final set of extracted data. Overall agreement between the two rounds of coding was high (89–100% per item and 84–93% per category), when discrepancies explained by changes to the codebook (e.g. revised code definitions) between the two rounds were excluded.
Results
The majority (62%) of participants were female. Walking was the most common mode of transport to school. In Schools 1–4, 27 participants walked, two used public transport and one alternated between using public transport and walking to school. All School 1–4 participants typically made the journey to school independently, and some walked with and supervised younger siblings. Conversely, in School 5, all four participants were driven to school by an adult, typically a family member. Most participants made their journey to school in < 20 min. Regardless of the mode of transport, school and area, participants reported being exposed to outlets selling, and advertisements marketing, various unhealthy foods. Three themes which captured how the food environment influenced children’s food practices—exposure to unhealthy food outlets, exposure to unhealthy food advertisements and the broader social environment—as well as a further theme about protecting children from unhealthy food, were developed through the analysis and are presented alongside the content analysis results in the following narrative.
Exposure to unhealthy food outlets
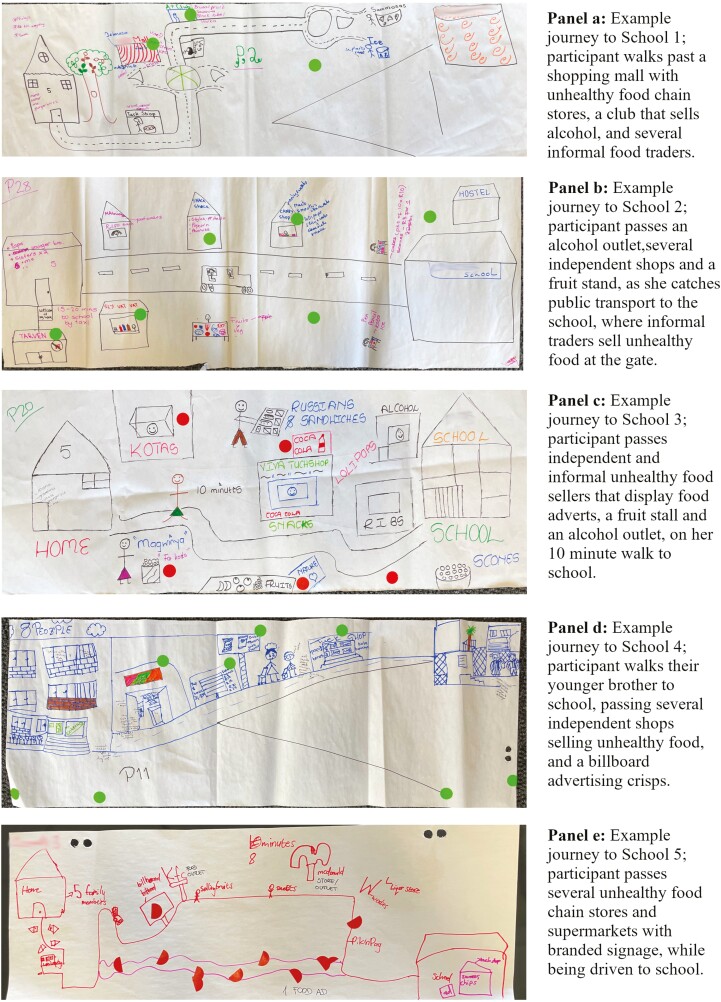
Participants were markedly exposed to outlets selling unhealthy food as they journeyed to and from school. The 33 journey to school drawings (see Figure 1 for examples) depicted 175 (mean 5; range 1–9) food outlets (Table 1). Participants reported that almost two-thirds (64%) sold only foods classified as unhealthy, whereas only one in 10 outlets, all informal fruit traders, sold exclusively food classified as healthy (Table 1). The most common type of food sold by the outlets depicted on journey to school drawings was unhealthy cooked food. Various deep-fried foods—amagwinya (deep-fried wheat dough balls, commonly called fat cakes), hot potato chips, samosas and amakota or sly (respectively, quarter loaves or slices of bread stuffed with hot chips, a price-dependent selection of processed, deep-fried meats, cheese, egg and sauces)—were especially popular and sold in almost half (45%) of all the food outlets (Table 1).
Fig. 1:
Examples of participants’ journey to school drawings.
Table 1:
Food outlets indicated on participants’ journey to school drawings (n = 33), categorized by type and foods sold
| N | % | |
|---|---|---|
| Total number of food outlets | 175 | |
| Type | ||
| Informal | 69 | 39.4 |
| Independent shop | 80 | 45.7 |
| Chain shop | 26 | 14.9 |
| Food sold (type 1) | ||
| Healthy | 19 | 10.9 |
| Unhealthy | 112 | 64.0 |
| Mixed | 30 | 17.1 |
| Unspecified | 14 | 8.0 |
| Food sold (type 2) | ||
| Branded | 18 | 10.3 |
| Unbranded | 75 | 42.9 |
| Mixed | 43 | 24.6 |
| Unspecified | 39 | 22.3 |
| Food sold (type 3) a | ||
| Alcohol | 14 | 8.0 |
| Fruit juice | 2 | 1.1 |
| Healthy cooked | 15 | 8.6 |
| Healthy raw | 30 | 17.1 |
| Salty snacks | 36 | 20.6 |
| Sugary snacks | 50 | 28.6 |
| Sugar-sweetened beverages | 49 | 28.0 |
| Unhealthy cooked | 78 | 44.6 |
| Unhealthy raw | 0 | 0.0 |
| Unspecified | 19 | 10.9 |
| Other | 6 | 3.4 |
aAs multiple food types were sometimes depicted on the same advertisement, percentages sum to more than 100.
Approximately one in four of the food outlets were reported to sell SSBs (28%), including branded, carbonated beverages and homemade, flavoured ice blocks. Healthy raw foods were sold at one in five (20%) outlets and eight participants reported passing outlets selling and advertising alcohol on their journey to school (Table 1). Many participants reported the outlets they drew only sold food classified as unhealthy or included a lone outlet selling fruit (exclusively or together with unhealthy food items) amidst a line of outlets selling unhealthy cooked foods, sugary and salty snacks and SSBs, up to the school gates. Almost all outlets were either independently owned shops (48%) or informal traders (39%) (Table 1). For example, one participant described their journey to school saying:
There is a spaza [informal convenience store] where they sell fat cakes… a tavern, they sell Savannah, Black Label and Heineken. When I carry on walking straight, there is a big tree and… a lady in front of the school that sells sweets, Simbas [crisps], and ice pops, then I enter the school. (School 1)
Participants who walked to school typically drew mostly food outlets selling unhealthy, unbranded foods (Table 1), including amagwinya and amakota. The exception was at School 5, where no participant reported exposure to informal traders at or near the school gates nor passing outlets that sold amakota, and all reported that they never purchased amagwinya, during their journeys to and from school. Participants from School 5 all included branded (chain) food outlets on their journey to school drawings, as did several participants from School 1 who passed a shopping mall. For example, the two participants who passed the same mall on their journey to School 1 indicated it was home to branded burger, fried chicken, pizza and pie outlets. None of the participants from Schools 2, 3 and 4 reported seeing brand-name fast-food outlets on their journeys to school.
Exposure to several unhealthy foods was mentioned exclusively by participants at only one or two of the schools. For example, sly were only mentioned by participants from Schools 1 and 2 which were in different areas of the same township. Cooked 2-min noodles were only mentioned by participants at School 3 and croissants and ice cream only by participants in School 5. School 5 participants also reported seeing fruit and vegetable sellers and independently owned convenience stores less often, than participants at other schools.
All participants except those at School 5, drew one or more ‘tuckshop’ or ‘spaza shop’, both independently owned convenience stores. Participants reported that although these stores sold some healthy items such as fruit and bread, most of their food products were unhealthy and that children mostly purchased unhealthy foods from these shops. For example, one explained, ‘What I have mostly noticed, in tuckshops, there’s mostly junk food. Like chips, chocolates, sweets, cold drinks [soda, soft drink], ice [blocks, flavoured and sweetened] and all of the stuff which is not good for us’ (School 4). Nonetheless, several participants perceived independent shops selling unhealthy cooked food were providing a service to people in the community. For example, one said it was good to have tuckshops in the community because when ‘you come home late from work you can’t cook and you can buy and eat [unhealthy food from the tuckshops] and get full’ (School 2).
Exposure to unhealthy food advertisements
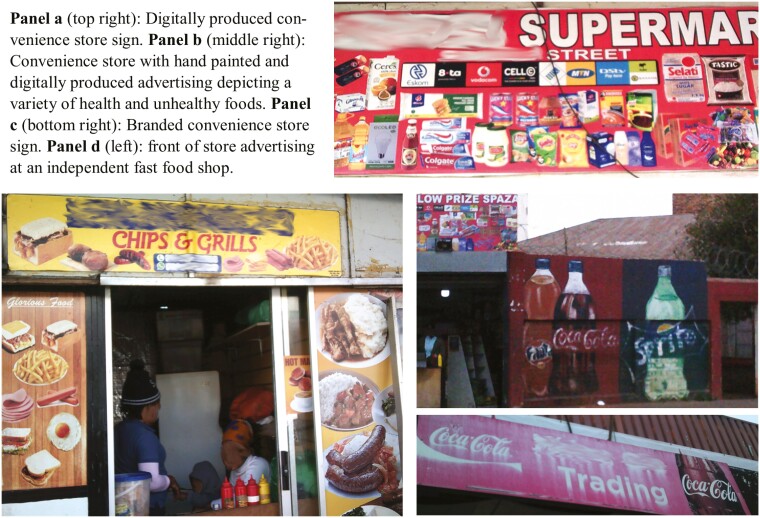
Participants indicated fewer food advertisements on their journey to school drawings than they did food outlets. Many of the independently owned convenience stores they drew were not marked with stickers to indicate they displayed advertisements. However, photo collages and related discussions indicated that many food outlets, especially the convenience and fast-food stores that most participants passed several of, typically displayed multiple front-of-store advertisements (Figure 2, panel b), most commonly advertisements depicting the variety of foods sold inside the shop (Figure 2, panels a and d) and/or shop name signs branded with the logo of a popular SSB (Figure 2, panel c). Furthermore, some participants did not consider the branded signs on chain fast-food outlets as advertising, despite drawing them in a manner that showed they recognized the brand. For example, when queried about what the distinctive capital letter M sign they had drawn represented (Figure 1, panel e), the participant who drew it said the recognizable brand symbol represented the outlet and not an advertisement.
Fig. 2:
Photographs of front-of-store advertising participants at School 4 were exposed to during their journey to school.
Despite not always recognizing, or being consciously aware of their exposure to advertisements, participants placed 125 (mean 4; range 0–8) stickers to indicate food advertisements on their journey to school drawings. Most were either front-of-store (54%) or point-of-sale (17%) adverts attached to independently owned or informal food outlets (Table 2). With the exception of two adverts on fruit stalls, all advertisements marketed unhealthy foods exclusively or in combination with healthy foods (Table 2), for example, a convenience store sign depicting multiple food items that advertised both fruit and salty snacks (Figure 2, Panel a). For example, one participant, ‘It is on all the tuck shops … [a sign showing] the chips they’re selling, the sweets, everything that they are selling, they will paint it [on the wall]. … they do sell bread. And they do also advertise it’ (School 1). Some advertisements were hand-painted and others were digitally produced (Figure 2). Some informal traders marketed their foods by placing simple signs displaying the product name and price on the containers they stored food in, and a few displayed branded food adverts (not necessarily for products that they sold). One participant indicated that informal traders also advertised their products by calling out and asking people to come and buy.
Table 2:
Food advertisements indicated on participants’ journey to school drawings (n = 33), categorized by types of food advertised
| N | % | |
|---|---|---|
| Total number of food advertisements | 125 | 100 |
| Type | ||
| Point of sale | 21 | 16.8 |
| Front of store | 67 | 53.6 |
| Billboard | 8 | 6.4 |
| Leaflet | 2 | 1.6 |
| Unspecified | 18 | 14.4 |
| Other | 9 | 7.2 |
| Food advertised (type 1) | ||
| Healthy | 2 | 1.6 |
| Unhealthy | 9 | 7.2 |
| Mixed | 46 | 36.8 |
| Unspecified | 68 | 54.4 |
| Food advertised (type 2) | ||
| Branded | 36 | 28.8 |
| Unbranded | 8 | 6.4 |
| Mixed | 10 | 8.0 |
| Unspecified | 71 | 56.8 |
| Food advertised (type 3) a | ||
| Alcohol | 4 | 3.2 |
| Fruit juice | 0 | 0 |
| Healthy cooked | 8 | 6.4 |
| Healthy raw | 3 | 2.4 |
| Salty snacks | 8 | 6.4 |
| Sugary snacks | 8 | 6.4 |
| Sugar-sweetened beverages | 29 | 23.2 |
| Unhealthy cooked | 21 | 16.8 |
| Unhealthy raw | 0 | 0.0 |
| Other | 10 | 8.0 |
| Unspecified | 65 | 52.0 |
aAs multiple food types were sometimes depicted on the same advertisement, percentages sum to more than 100.
Participants mentioned a range of power techniques used to market unhealthy foods that they were exposed to on their journeys to school or on screens (television and cell phone). Direct and indirect claims about unhealthy foods, including value, health, social and taste claims, were prominent, although not necessarily recognized by participants to be power techniques. Taste and value claims were most commonly reported as being made indirectly, by depicting foods in advertisements that looked more appetising and/or bigger than they did in real life. For example, participants reported that advertisements made ‘you want to taste [the unhealthy foods shown] … because sometimes on the adverts they make them seem fresh and when you go to the shop they are not fresh’ (School 3) and that ‘in real life, it’s more expensive and the burger is smaller [than in the advertisement]’ (School 4).
However, participants also mentioned direct claims, for example advertisements with written statements such as, ‘roars with flavour’, the slogan for a brand of potato crisps that uses a cartoon lion as its mascot. This brand was one of several that children mentioned, which combined the use of taste or value claims, with child-directed characters, including cartoons, children and families. Some participants indicated that the advertisements that attracted them the most portrayed a child eating the advertised food. For example, one said:
In the morning they sell noodles and fat cakes [amagwinya]. The noodles are the Kellogg’s noodles [and] they painted [an advertisement showing] a child eating noodles [on the wall] and when you look at it you want to eat it too. (School 3)
Although branded packaged foods were advertised by independent food outlets, several participants indicated that they only saw branded fast-food advertisements when they travelled to other areas. For example, one said that they saw adverts for branded fast-foods ‘but they are not close to or around the school’ (School 3) and another that ‘I only see [billboard] adverts when I am traveling to another place… Like if I’m going to [names two socio-economically privileged suburbs]’ (School 4).
The broader social environment
Advertising was one of many factors that influenced participants’ food practices. Independent access to unhealthy food enabled, whereas having limited or no money limited, participants’ access to unhealthy food. Many participants in Schools 1–4, who journeyed to school without adult supervision, were regularly (weekly or in some cases daily) given small amounts of money by their parents. Independent shops and informal traders catered to the limited economic means of the students in the areas where they operated by selling unbranded and cheaply priced unhealthy foods that were filling (including amagwinya costing ZAR1-2 each and amakota and sly costing ZAR10 upwards). For example, about half of the participants said their parent or guardian gave them ZAR2-10 daily to weekly, and that they used it almost exclusively to purchase unhealthy food. Some participants indicated they did not use their money to buy healthy food such as fruit, because they got this food from home or from the school nutrition program. Some participants, particularly those at School 1, reported not buying unhealthy food on their way to and from school, because their parents did not give them money.
Participants’ narratives indicated that giving money was partly a strategy parents used to cope with having limited time to prepare food, due to work and other commitments. For example, one participant reported that her mother gave her ZAR25 per day to purchase food for herself and her younger brother as they journeyed independently to and from school. When her mum was short of money, she left ‘[2-minute] noodles in the house, so when I’m back I could cook for my small brother and me’, (School 4) because her mother did not arrive home from work until after 5 pm. She was one of many participants who indicated that their parent/s alternated between giving them money to buy food, providing a lunch box and/or leaving food in the house, depending on how much money, food and time they had available.
Protecting children from unhealthy food advertising and sales
Many participants expressed positive views about the government playing a role in regulating unhealthy food marketing to children but felt that restricting television advertising at specific times was insufficient and would be ineffective in promoting children’s health. For example, one said, ‘I think it’s not going to work because not only are people advertising on TV but when the kids are on their way to school, they still see those adverts around them’ (School 4). Others noted that primary school-age children watched television outside of the early afternoon period during which advertising was self-regulated, especially on the weekends.
Numerous suggestions for additional or alternative regulations were put forward in each of the groups. A few participants perceived a need to advertise healthy foods. Many thought that additional restrictions on the marketing and sale of unhealthy foods to children were needed. They suggested: enforcing existing regulation of television advertising; extending regulation of television advertising to other time slots and social media; reducing or banning unhealthy food advertising completely and involving children, school representatives and parents in determining regulations. Some suggested it was more important to restrict advertising of alcohol than unhealthy foods. Suggestions for regulating unhealthy food sales included: reducing the unhealthy (i.e. salt, sugar and fat) content of processed and prepackaged food; ensuring healthy foods were available in outlets selling unhealthy foods, enforcing existing regulations banning the sale of alcohol to children; introducing restrictions on the times at which unhealthy food could be sold to children; banning selling unhealthy food at or near schools or banning selling unhealthy food to children entirely.
More extensive regulation of unhealthy food marketing or sale to children was however contentious. One participant predicted protests if unhealthy food advertising was completely banned and another that ‘some kids won’t even come to school’, (School 4) if unhealthy food is banned within school premises. To a suggestion from one participant that people under 18 years be banned from eating unhealthy food, another responded, ‘To reach the age of 18 until we eat a burger? It can’t be possible!’ (School 1). Two groups discussed the consumption of unhealthy food as an individual choice and right for children as it was for adults. Several participants felt that extensive sales or advertising bans would deny people’s and businesses’ rights, saying for example, ‘Wouldn’t that stop people’s happiness? And also the companies wouldn’t make as much money’, (School 5) and ‘They are supposed to continue doing business and get the money to feed their families’ (School 1).
Discussion
Our analysis of urban South African primary school students’ journey to school drawings shows that the food outlets and advertisements seen by primary school students journeying to and from school in a major South African city predominately sell or market unhealthy food. This concurs with the results of prior studies, which have been conducted mostly in high-income countries and focused on branded foods, advertised and sold in the formal food sector (WHO, 2022). Conversely, in four of the five settings in our study, informal and small traders sold and marketed much of the unhealthy food primary school students were exposed to, and much of this unhealthy food was unpackaged and unbranded. These results have important implications for policy and other interventions to shape healthier food environments for children in Johannesburg, South Africa and potentially other similar urban environments. They should be considered in relation to the nature of the data and the strengths and limitations of the study.
Strengths and limitations
Participants’ drawings of their journeys to school, the primary source of data analysed, were subjective representations—participants’ perceptions—of their actual exposure to food outlets and advertisements. They represent the food outlets and advertisements that the participants, a convenience sample of students aged 11–14 years and in their final grade of primary school, remember being exposed to, rather than the outlets and advertisements they were actually exposed to. Triangulating different sources of data (drawings, photographs, discussions), suggested that participants’ drawings were a partial representation of their actual exposure to food outlets and outdoor advertisements. The participants did not recall their exposure to a considerable proportion of advertisements, including the multiple advertisements that participants’ photo collages indicated adorned the front of most independent convenience stores. This is unsurprising given the subconscious level at which advertising often exerts its effects, especially on children (Buijzen et al., 2010).
Given the predominance of studies that attempt to objectively measure unhealthy food outlets and advertisements in the vicinity of schools (e.g. Kelly et al., 2008; Chacon et al., 2015; Kelly et al., 2015; Signal et al., 2017; Barquera et al., 2018; Velazquez et al., 2019; Dia et al., 2021; Puspikawati et al., 2021) and limited understanding of children’s perceptions of their food environments (Carducci et al., 2021), we consider the subjective nature of our triangulated dataset a strength, which addresses several limitations of previous studies. Asking children to document their exposures, allowed us to capture informal and independent traders, as well as unbranded foods, that have been excluded from some previous studies (e.g. Signal et al., 2017) but were significant sources of exposure to unhealthy foods for our participants. Documenting children’s perceptions, although it missed some exposures, captured only food outlets and advertisements participants were exposed to, rather than all within a street network or radial buffer of their school. Our study also likely better captured outlets and advertisements that participants paid explicit attention to, compared to studies that count the number of advertisements and/or outlets in a particular area.
Nonetheless, empirical research shows that people, especially children, pay attention to advertisements that they do not consciously remember seeing. This type of implicit or peripheral processing is more likely to result in brand recognition and loyalty than explicit or central processing and is a fundamental component of the insidious ways that advertising works (Buijzen et al., 2010). Because of their still-developing knowledge of the persuasive intent of advertising, older children and young adolescents such as the participants in our study, are more likely than their older counterparts to process advertisements implicitly. Advertisers may capitalize on children’s limited knowledge of their persuasive intent, for example by integrating advertising messages into the storyline or modifying the content style in ways that limit the likelihood a child will recognize them as advertising (Buijzen et al., 2010). Hand-painted advertisements that mimic public art but are sponsored by corporations to market their SSBs, noodles and other branded foods, are an example of modified content style. Participants in our study indicated they were commonplace in socio-economically deprived areas.
Our method did not capture the advertisements and outlets that caught our participants’ attention implicitly but were forgotten. This is one of the unavoidable limitations of studying children’s perceptions. Furthermore, our study was resource and time limited; the data we collected provided novel insights but did not ‘saturate’ the topic. We included students from a single grade in five schools in urban Gauteng, selected purposively for diversity. The participants were interviewed by researchers who had no existing relationships with them, and most of the data were collected in English, a second language for most participants, who typically did not speak in their first languages, although they were given the option to. While the results likely provide insights for, and readers may translate them to other similar settings on a case-by-case basis, they are not intended to be generalized. However, the results are novel and have significant policy implications, which we discuss below. Further research about the nature of children’s exposure to unhealthy food outlets and outdoor advertisements in other areas of South Africa and other LMICs, amongst students of different ages, in different setting, is warranted.
Informal and independent unhealthy food traders
In the urban South African settings for our study, participants attending schools in multidimensionally deprived areas (Schools 1–4) commonly encountered informal traders and independent shops selling unpackaged, deep-fried foods. These small food retailers, who make their livelihoods selling unhealthy foods and have a constitutionally enshrined right to do so (Hodgson et al., 2018), position themselves strategically, near schools and sometimes outside the school gates. These independent and informal traders tended to sell unhealthy foods that were profitable and tailored to the limited socio-economic means of the students—cheap, unbranded foods that did not easily spoil, such as packaged snacks and sweets and/or carbohydrate-rich, deep-fried foods.
Locating food outlets close to socio-economically deprived schools is a strategy previously reported of the formal food retailers (da Costa Peres et al., 2020; Kain et al., 2024) that have to date been the focus of regulations. South Africa’s proposed front-of-package labelling regulations exempt foods ‘produced for sale by a small producer or a street vendor’ (South African Government Department of Health, 2023, section 46, p79). Yet these were the foods participants in our study were most commonly exposed to, and most able to access. Regulating only foods sold by larger retailers is unlikely to be enough to reduce primary school students’ exposure to advertising for or consumption of unhealthy foods. Our results demonstrate a need to also regulate informal food trading and the sale of unbranded foods produced by small traders in South Africa. Restricting food sales near schools through zoning laws has been successful in some places (da Costa Peres et al., 2020). In South Africa, such regulations may prove challenging to implement because the rights of informal traders to market their goods are constitutionally enshrined (Hodgson et al., 2018) albeit in tension with children’s right to healthy food environments (Mofokeng, 2023). In the South African context, informal traders may need to be supported and incentivized to make alternative and/or improved incomes. Non-policy interventions, such as working with (or creating jobs for) informal food sellers to increase the availability of and demand for affordable and nutritious food options aligned with national dietary guidelines, may be valuable. Any interventions in this area would need to be sensitive to the socio-economically marginalized status of most informal traders (Hodgson et al., 2018), who, as noted by participants, are often selling unhealthy foods so that they can feed their own families.
Extending restrictions on ‘big food’ advertising, nonetheless, remains important. Many informal traders and most independent stores our participants encountered on their journeys to school also sold branded products, especially carbonated SSBs, crisps and sweets. These would be subject to proposed front-of-package labelling regulations should they be enacted, and are included in the current voluntary ban on television advertising targeting children. A robust body of evidence has documented the effects of advertising on children’s food preferences, practices and socio-cultural norms (Chung et al., 2022). Enacting mandatory restrictions on unhealthy food advertising targeting children is essential but must transcend banning advertising during children’s television viewing times or the use of child-directed characters and gifts. Our results indicate (unsurprisingly) that primary school-age children watch television outside the times at which unhealthy food advertising is currently self-regulated in South Africa. They also see screen-based adverts on cell phones and outdoor advertisements, especially front-of-store and point-of-sale paintings and signs.
Importance of food system-wide approaches
Our results highlight the importance of food system-wide approaches, which combine policies that regulate unhealthy food marketing by ‘big food’ companies, with policy and non-policy interventions to address the marketing and sale of unhealthy food more broadly, and other commercial determinants of health (Gilmore et al., 2023). Interventions that influence children’s food preferences and choices, such as advertising or subsidising the purchase of fruits and other healthy foods, have been successful in other settings (Burgaz et al., 2023) and were perceived by participants in our study to be important. Another important step would be regulating the advertising of unhealthy food to children more broadly, including outdoor advertisements children see as they journey to school. If adopted South Africa’s proposed front-of-package labelling regulations will ban ‘child-directed’, but not other types of marketing, of any product with a front-of-package warning (South African Government Department of Health, 2023). However, child-directed marketing is defined in the regulation according to the content of advertisements (e.g. adverts depicting cartoons, families or other child-directed characters). The regulation does not consider advertising that is strategically placed in locations frequented by children, such as nearby schools, to be child-directed. Regulating unhealthy food advertising that is child-directed because it is strategically placed in child-frequented outdoor environments in South Africa could be an important next-step in the move towards complete advertising bans on unhealthy food (as has been achieved for tobacco and alcohol in some jurisdictions) (Chung et al., 2022).
Policy interventions to regulate and reduce the amount of fat, sugar and salt added to processed foods are another promising option, mentioned by participants in our study, that could form part of a food systems-wide approach. South Africa’s existing regulations on the amount of sugar in beverages and salt in processed foods have been effective in reducing sugar and salt consumption, respectively (Charlton et al., 2021; Hofman et al., 2021). Levies on soft drinks have also had positive effects in high-income countries (Boyland et al., 2022). Expanding South Africa’s health promotion levy to other unhealthy foods, including those with added salt and fat could be explored, as could pegging the levy to inflation and imposing stricter limits or higher levies on the unhealthy content of already regulated foods.
Food preferences and cultures, geographic proximity to different types of food outlets and socio-economics were suggested by our data to be inter-related. There were several important distinctions in the types of foods, outlets and adverts which participants attending schools in more and less disadvantaged areas, were exposed to. While these findings must be treated with caution given the small number of schools in our study, they are theoretically feasible. Food practices are shaped by a broad range of socio-economic factors, including family structure, adult influence over and supervision of children’s food choices, disposable income, historic circumstances and cultural beliefs (Mofokeng, 2023). Further research about the socio-economic, geographic and cultural factors influencing children’s food practices in post-Apartheid South Africa is warranted.
Addressing the commercial determinants of childhood overweight and obesity broadly
Our findings draw attention to the influence of two related, commercial determinants of health that have received limited attention in the literature on preventing childhood overweight and obesity—parents’ work arrangements and labour policies (Gilmore et al., 2023). In LMICs such as South Africa, our results suggest that high unemployment, long working hours and low minimum wages mean that urban parents often have no choice but to be absent when their children are making choices about or purchasing food, and thus cannot encourage healthier, or restrict unhealthy, choices. That most participants made their journey to school alone, and many indicated that their parents were still at work when they arrived home, is unsurprising in the urban South African context. However, the impact of parents’ work arrangements, on children’s food purchasing and consumption has received limited attention. Lack of employment opportunities also drives people to informally trade unhealthy foods close to or outside of schools to make a living. These results indicate that policies to improve working conditions, ensure parents have the flexibility they need to be with their children, and more broadly address poverty and wealth and income inequality in South Africa, would be important components of food system-wide approaches to optimally address children’s right to health.
Conclusion
Urban South African primary school students are frequently exposed to unhealthy food outlets and advertisements as they journey to and from schools. Many advertisements are for unbranded, unpackaged foods sold by informal traders and independent shops. To optimally protect children from the harms of unhealthy food advertising and sales, food system-wide approaches that centre on children’s right to health, are essential. Such approaches would need to address the rights of employees and the self-employed to better working conditions and higher incomes, while expanding regulation of unhealthy food advertising to outdoor and internet-based media as well as small producers and traders. Furthermore, interventions to promote alternative, healthier food cultures are needed if food systems in urban South Africa are to enable children the nutrition they require to fulfil their constitutionally enshrined right to health.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the schools, and primary school students who participated in the study, as well as the school principals and teachers and Ms Sandra Ntebe, who assisted with participant recruitment.
Contributor Information
Michelle R Brear, SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA), School of Public Health, Faculty of Health Sciences, University of Witwatersrand, 2nd floor, School of Public Health Building, Wits Education Campus, 27 St Andrews Road, Parktown, Johannesburg, 2193, Gauteng, South Africa; Global and Women’s Health, School of Public Health and Preventive Medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, 553 St Kilda Road, Melbourne, Victoria, 3004, Australia.
Agnes Erzse, SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA), School of Public Health, Faculty of Health Sciences, University of Witwatersrand, 2nd floor, School of Public Health Building, Wits Education Campus, 27 St Andrews Road, Parktown, Johannesburg, 2193, Gauteng, South Africa.
Glynis Clacherty, African Centre for Migration and Society, School of Social Sciences, Faculty of Humanities, Second Floor, Solomon Mahlangu House, East Campus, University of the Witwatersrand, Braamfontein, 2000, Gauteng, South Africa.
Lebogang Seutlwadi, School of Humanities, The Independent Institution of Education, Varsity College, 11 Riverview Park, Janadel Avenue, Midrand, 1686, Gauteng, South Africa.
Sameera Mahomedy, SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA), School of Public Health, Faculty of Health Sciences, University of Witwatersrand, 2nd floor, School of Public Health Building, Wits Education Campus, 27 St Andrews Road, Parktown, Johannesburg, 2193, Gauteng, South Africa.
Kabelo Maleke, SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA), School of Public Health, Faculty of Health Sciences, University of Witwatersrand, 2nd floor, School of Public Health Building, Wits Education Campus, 27 St Andrews Road, Parktown, Johannesburg, 2193, Gauteng, South Africa.
Susan Goldstein, SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA), School of Public Health, Faculty of Health Sciences, University of Witwatersrand, 2nd floor, School of Public Health Building, Wits Education Campus, 27 St Andrews Road, Parktown, Johannesburg, 2193, Gauteng, South Africa.
AUTHOR CONTRIBUTIONS
Michelle R. Brear: Conceptualization, Data curation, Formal analysis, Validation, Writing—original draft. Agnes Erzse: Conceptualization, Investigation, Data curation, Methodology, Project administration, Writing—review and edit. Glynis Clacherty: Conceptualization, Methodology, Investigation, Writing—review and edit. Lebo Seutlwadi: Investigation, Review and edit. Sameera Mahomedy: Supervision, Resources, Writing—review and edit. Kabelo Maleke: Investigation, Writing—review and edit. Susan Goldstein: Conceptualization, Funding acquisition, Methodology, Supervision, Writing—review and edit.
FUNDING
Financial support comes from the UNC Global Food Research Program (grant number 5124184), with additional support from the SAMRC/Wits Centre for Health Economics and Decision Science—PRICELESS SA (grant number 23108).
CONFLICT OF INTEREST
None declared.
DATA AVAILABILITY
The data underlying this article cannot be shared publicly due to ethical considerations regarding participant privacy. The data will be shared on reasonable request to the corresponding author.
REFERENCES
- Barquera, S., Hernández-Barrera, L., Rothenberg, S. J. and Cifuentes, E. (2018) The obesogenic environment around elementary schools: food and beverage marketing to children in two Mexican cities. BMC Public Health, 18, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyland, E., McGale, L., Maden, M., Hounsome, J., Boland, A. and Jones, A. (2022) Systematic review of the effect of policies to restrict the marketing of foods and non‐alcoholic beverages to which children are exposed. Obesity Reviews, 23, e13447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buijzen, M., Van Reijmersdal, E. A. and Owen, L. H. (2010) Introducing the PCMC model: an investigative framework for young people’s processing of commercialized media content. Communication Theory, 20, 427–450. [Google Scholar]
- Burgaz, C., Gorasso, V., Achten, W. M., Batis, C., Castronuovo, L., Diouf, A.. et al. (2023) The effectiveness of food system policies to improve nutrition, nutrition-related inequalities and environmental sustainability: a scoping review. Food Security, 15, 1313–1344. [Google Scholar]
- Cairns, G., Angus, K., Hastings, G. and Caraher, M. (2013) Systematic reviews of the evidence on the nature, extent and effects of food marketing to children. A retrospective summary. Appetite, 62, 209–215. [DOI] [PubMed] [Google Scholar]
- Carducci, B., Oh, C., Roth, D. E., Neufeld, L. M., Frongillo, E. A., L’Abbe, M. R.. et al. (2021) Gaps and priorities in assessment of food environments for children and adolescents in low- and middle-income countries. Nature Food, 2, 396–403. [DOI] [PubMed] [Google Scholar]
- Chacon, V., Letona, P., Villamor, E. and Barnoya, J. (2015) Snack food advertising in stores around public schools in Guatemala. Critical Public Health, 25, 291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton, K. E., Corso, B., Ware, L., Schutte, A. E., Wepener, L., Minicuci, N.. et al. (2021) Effect of South Africa’s interim mandatory salt reduction programme on urinary sodium excretion and blood pressure. Preventive Medicine Reports, 23, 101469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, A., Zorbas, C., Riesenberg, D., Sartori, A., Kennington, K., Ananthapavan, J.. et al. (2022) Policies to restrict unhealthy food and beverage advertising in outdoor spaces and on publicly owned assets: a scoping review of the literature. Obesity Reviews, 23, e13386. [DOI] [PubMed] [Google Scholar]
- da Costa Peres, C. M., Gardone, D. S., Costa, B. V. L., Duarte, C. K., Pessoa, M. C. and Mendes, L. L. (2020) Retail food environment around schools and overweight: a systematic review. Nutrition Reviews, 78, 841–856. [DOI] [PubMed] [Google Scholar]
- Dia, O. E. W., Løvhaug, A. L., Rukundo, P. M. and Torheim, L. E. (2021) Mapping of outdoor food and beverage advertising around primary and secondary schools in Kampala city, Uganda. BMC Public Health, 21, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzse, A., Christofides, N., Stacey, N., Lebard, K., Foley, L. and Hofman, K. (2021) Availability and advertising of sugar sweetened beverages in South African public primary schools following a voluntary pledge by a major beverage company: a mixed methods study. Global Health Action, 14, 1898130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman, B., Kelly, B., Vandevijvere, S. and Baur, L. (2016) Young adults: beloved by food and drink marketers and forgotten by public health? Health Promotion International, 31, 954–961. [DOI] [PubMed] [Google Scholar]
- Gilmore, A. B., Fabbri, A., Baum, F., Bertscher, A., Bondy, K., Chang, H. -J.. et al. (2023) Defining and conceptualising the commercial determinants of health. The Lancet, 401, 1194–1213. [DOI] [PubMed] [Google Scholar]
- Hodgson, T., Clark, M., Potter, A., Wilson S. and Parkenson, C. (2018) Informal Trade in South Africa. Legislation, Case Law and Recommendations for Local Government. SALGA South African Local Government Association, Pretoria, Gauteng, South Africa. [Google Scholar]
- Hofman, K. J., Stacey, N., Swart, E. C., Popkin, B. M. and Ng, S. W. (2021) South Africa’s Health Promotion Levy: excise tax findings and equity potential. Obesity Reviews, 22, e13301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igumbor, E. U., Sanders, D., Puoane, T. R., Tsolekile, L., Schwarz, C., Purdy, C.. et al. (2012) “Big food,” the consumer food environment, health, and the policy response in South Africa. PLoS Medicine, 9, e1001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kain, J., Sandoval, M. H., Orellana, Y., Cruz, N., Díez, J. and Weisstaub, G. (2024) Socio-spatial segregation of unhealthy food environments across public schools in Santiago, Chile. Nutrients, 16, 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, B., Cretikos, M., Rogers, K. and King, L. (2008) The commercial food landscape: outdoor food advertising around primary schools in Australia. Australian and New Zealand Journal of Public Health, 32, 522–528. [DOI] [PubMed] [Google Scholar]
- Kelly, B., King, L., Jamiyan, B., Chimedtseren, N., Bold, B., Medina, V. M.. et al. (2015) Density of outdoor food and beverage advertising around schools in Ulaanbaatar (Mongolia) and Manila (The Philippines) and implications for policy. Critical Public Health, 25, 280–290. [Google Scholar]
- Mofokeng, T. (2023) Food, Nutrition and the Right to Health—report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. United Nations. [Google Scholar]
- Moodley, G., Christofides, N., Norris, S. A., Achia, T. and Hofman, K. J. (2015) Obesogenic environments: access to and advertising of sugar-sweetened beverages in Soweto, South Africa, 2013. Preventing Chronic Disease, 12, E186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse, J. M. (2015) Critical analysis of strategies for determining rigor in qualitative inquiry. Qualitative Health Research, 25, 1212–1222. [DOI] [PubMed] [Google Scholar]
- Morse, J. M. (2016) Mixed Method Design: Principles and Procedures. Routledge, NY. [Google Scholar]
- Ndlovu, N., Day, C., Aagaard-Hansen, J., Sartorius, B. and Hofman, K. (2018) Assessment of food environments in obesity reduction: a tool for public health action. South African Health Review, 2018, 115–123. [Google Scholar]
- Nwosu, E., Fismen, A. S., Helleve, A., Hongoro, C., Sewpaul, R., Reddy, P.. et al. (2022) Trends in prevalence of overweight and obesity among South African and European adolescents: a comparative outlook. BMC Public Health, 22, 2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puspikawati, S. I., Dewi, D. M. S. K., Astutik, E., Kusuma, D., Melaniani, S. and Sebayang, S. K. (2021) Density of outdoor food and beverage advertising around gathering place for children and adolescent in East Java, Indonesia. Public Health Nutrition, 24, 1066–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signal, L. N., Stanley, J., Smith, M., Barr, M., Chambers, T. J., Zhou, J.. et al. (2017) Children’s everyday exposure to food marketing: an objective analysis using wearable cameras. International Journal of Behavioral Nutrition and Physical Activity, 14, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner, C. (2016) Informal food retail in Africa: a review of evidence. Consuming Urban Poverty Project Working Paper No. 2. African Centre for Cities, University of Cape Town, pp. 1– 39. [Google Scholar]
- South African Government Department of Basic Education. (2023) Schools Masterlist Data. Gauteng Province. https://www.education.gov.za/Programmes/EMIS/EMISDownloads.aspx (last accessed 11 October 2024).
- South African Government Department of Health. (2023) Regulations relating to the labelling and advertising of food stuffs [R. 3337, Draft for public comment]. https://www.gov.za/sites/default/files/gcis_document/202304/48460rg11575gon3337.pdf (last accessed 11 October 2024).
- Timmermans, S. and Tavory, I. (2012) Theory construction in qualitative research: from grounded theory to abductive analysis. Sociological Theory, 30, 167–186. [Google Scholar]
- Velazquez, C. E., Daepp, M. I. and Black, J. L. (2019) Assessing exposure to food and beverage advertisements surrounding schools in Vancouver, BC. Health & Place, 58, 102066. [DOI] [PubMed] [Google Scholar]
- Walton, M., Pearce, J. and Day, P. (2009) Examining the interaction between food outlets and outdoor food advertisements with primary school food environments. Health & Place, 15, 841–848. [DOI] [PubMed] [Google Scholar]
- WHO, World Health Organization. (2012) A Framework for Implementing the Set of Recommendations on the Marketing of Foods and Non-Alcoholic Beverages to Children. https://iris.who.int/bitstream/handle/10665/80148/9789241503242_eng.pdf?sequence=1 (last accessed 11 October 2024).
- WHO, World Health Organization. (2022) Food Marketing Exposure and Power and Their Associations with Food-Related Attitudes, Beliefs and Behaviours: A Narrative Review. https://iris.who.int/bitstream/handle/10665/351521/9789240041783-eng.pdf?sequence=1 (last accessed 11 October 2024).
- WHO, World Health Organization. (2023) Taking Action to Protect Children from the Harmful Impact of Food Marketing: A Child Rights-Based Approach. https://iris.who.int/bitstream/handle/10665/370355/9789240047518-eng.pdf?sequence=1 (last accessed 11 October 2024).
- Yamoah, D. A., De Man, J., Onagbiye, S. O. and Mchiza, Z. J. (2021) Exposure of children to unhealthy food and beverage advertisements in South Africa. International Journal of Environmental Research and Public Health, 18, 3856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, S., Cheng, Y., Cheng, L., Wang, D., Li, Q., Liu, Z.. et al. (2020) Association between convenience stores near schools and obesity among school-aged children in Beijing, China. BMC Public Health, 20, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to ethical considerations regarding participant privacy. The data will be shared on reasonable request to the corresponding author.