Abstract
Background
The burden of chronic illnesses, including cardiovascular disease and diabetes, is increasing in low- and middle-income countries. However, health systems often struggle to meet the needs of chronically ill patients. Affordability is crucial in ensuring access to quality healthcare for patients with diabetes mellitus (DM) and evaluating healthcare costs. Therefore, this study aimed to assess the affordability of health services and identify associated factors among DM patients receiving regular follow-ups at Dessie Comprehensive Specialized Hospital in Northeast Ethiopia, 2023.
Methods
A cross-sectional study was conducted among 392 DM patients at Dessie Comprehensive Specialized Hospital (DCSH) from July 1 to 30, 2023. Data was collected using a structured questionnaire and chart review checklist. Systematic random sampling was employed, and the data were analyzed using EPI INFO version 7 and SPSS version 26. The outcome variable, affordability of health services, was measured by five items using a structured questionnaire. Logistic regression analysis was performed to identify significant factors associated at 95% confidence interval using odds ratio.
Results
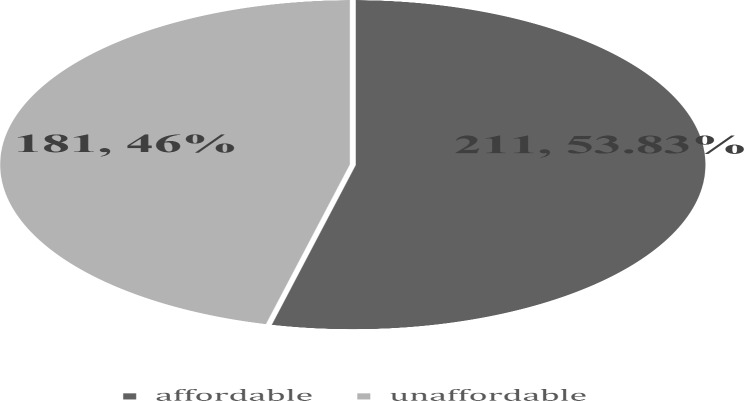
Most participants were married (74.2%), and 55.9% were male. Among the DM patients, 211 (53.83%) found the health services affordable, with an interval of 48.85–58.72% at a 95% confidence interval with a p-value less than 0.05. Factors significantly associated with healthcare affordability included marital status, family size, average monthly income, and brand prescription.
Conclusion
The study revealed that healthcare services were affordable for approximately half of the DM patients. However, this level of affordability falls short of the ideal standard. Improving the affordability and accessibility of healthcare services for DM patients, particularly those from low-income backgrounds, is crucial to ensuring better health outcomes.
Keywords: Affordability, Diabetes mellitus, Patients, Health services
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by elevated blood glucose levels resulting from defects in insulin secretion, insulin action, or both [1]. Globally, the prevalence of diabetes has been on the rise, posing a significant public health challenge. According to the International Diabetes Federation (IDF), the global burden of diabetes is substantial and increasing rapidly. In 2019, an estimated 463 million adults were living with diabetes [2] with a significant number of cases in low- and middle-income countries [3]. It poses significant health challenges globally and requires continuous medical care and self-management to prevent acute complications and reduce the risk of long-term complications [4]. In Ethiopia, the burden of diabetes is also increasing, with a prevalence rate of 5.2% among adults aged 20–79 years in 2019 [5]. Therefore, In Ethiopia, it is rising, exerting considerable pressure on healthcare systems and patients’ financial resources [6].
Affordability is a function of income, spending, and judgments about the value of goods and services for their price. This brief considers affordability as an economic concept, as a kitchen-table budget issue for individuals and families, and as a threshold in current policy [7].
A fundamental need for nation’s at all economic levels is access to affordable basic healthcare.
Global spending as a percentage of Growth Domestic Product (GDP) is still rising, most lately due to the development of potent new treatment regimens for disease cure. These and other very expensive disease treatments are becoming more common, which will have an impact on a wide variety of stakeholders. Few health systems are set up to meet the needs of patients with chronic illnesses, especially those who are underprivileged and have little money to spend on routine care. Because of this, low-income and middle-income countries frequently fail to reduce the rising expense of treating chronic diseases. One of the most common and deadly non-communicable diseases in the world is diabetes (NCDs). It is seen as a major danger to global development and a primary source of mortality, disability, and financial loss [6].
Healthcare affordability is crucial for health system performance and equity, especially in managing chronic diseases like diabetes [7]. Five key measures include Out-of-Pocket Expenditure (OOP), Catastrophic Health Expenditure (CHE), Impoverishment due to Health Expenditure, Health Insurance Coverage, and Affordability Ratio. High OOP can lead to financial strain, CHE causes severe burden, Impoverishment due to Health Expenditure pushes households below the poverty line, and Health Insurance Coverage protects individuals from high costs [8–10].
The prevalence of diabetes mellitus is relatively high which has serious long-term complications and results in significant economic costs for patients and health systems alike worldwide [11, 12]. Determining the affordability of health services for DM patients and identifying factors influencing it is crucial. As far as my search studies conducted regarding this issue are few.
After all this study will provide evidence for different stakeholders regarding the affordability of health services among DM patients, and it will push them to intervene accordingly. Therefore, this study aimed to fill this gap by examining the affordability of health services and associated factors among diabetes patients under regular follow-up at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia.
Methods
Study area and period
Dessie Comprehensive Specialized Hospital, located in Northeast Ethiopia, is a key health facility providing specialized medical services to the region. It serves as a referral center for various chronic conditions, including diabetes. The hospital offers regular follow-up services for patients with DM, aiming to manage their condition effectively through multidisciplinary approaches involving endocrinologists, dietitians, and diabetes educators.
The study was conducted from July 1 to 30/2023.
Study design and participant characteristics
An institution-based cross-sectional study was employed at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia, 2023. All diabetes mellitus patients on regular follow-up at the diabetes clinic in Dessie Comprehensive Specialized Hospital 2023 who were available during the study period were included.
Sample size determination and sampling procedure
The sample size was determined by using the single population proportion formula by considering 36.1% of patients reported essential medicines as affordable in the Ethiopian study [13]. The sample size for the secondary objective has been calculated, and the highest final sample size was taken. The margin of error is 5% at a 95% confidence level by adding 10% of respondents.
 |
Non-response rate: 10% = 36,
Final sample size (n) = 356 + 36 = 392.
Where;
n = sample size.
Z α/2: Level of confidence at 95%.
P = population proportion = 36.1%.
d: Margin of error = 5%.
After all, the final sample size for this study is 392.
Study Participants from the DCSH diabetes mellitus clinic were selected using systematic random sampling. The average number of diabetes mellitus patients on regular follow-up at the diabetes mellitus clinic daily was estimated at 30 patients, and two months were used for data collection (44 working days). The total number of diabetes mellitus patients in the study period was 1320. The K interval was determined by dividing the total diabetes mellitus patients on follow-up by the final sample size of N/n (1320/392), which enabled us to select participants every 4th unit. The starting number was 2 after being drawn randomly, and then participants selected every 4th interval (2, 6, 10, and 14).
Data collection procedure and quality control
The data was gained from face-to-face participants’ interviews with Amharic speakers from July 1 to 30, 2023.
The data collection tool was translated into Amharic and then back to English to ensure its consistency. The tool was pre-tested on 10% of nurses at Woldia Comprehensive Specialized Hospital for appropriateness two weeks before the actual data collection. Two BSc nurses were trained as data collectors. The questionnaire has three parts: the first is socio-economic demographic characteristics; the second contains questions about disease and treatment-related factors; and the third is the affordability of healthcare. The tool is adapted from different studies [13–17]. During data collection, the supervisor followed the day-to-day data collection process closely and ensured the completeness and consistency of the interview checklist each day before transferring it into computer software. Problems concerned with data collection were corrected early, and non-overlapping numerical codes were given for each question to enter in Epi-Data Manager version 4.6.
Data processing and analysis
After data collection, the data was checked and entered into a computer using Epi Data version 4.6 and exported to SPSS version 26 for data analysis. Descriptive statistics, including frequencies and percentages, were done for all variables. Initially, univariable logistic regression analysis was carried out to see the association between the outcome and each explanatory variable, and then multivariable logistic regression analysis was computed. Multicollinearity among variables was evaluated using VIF (variables found with VIF < 10), and the Hosmer and model fitness were checked using the HosmeLemeshow test, which was found insignificant (0.44). Variables with P-values < 0.05 in multivariable logistic regression analysis were used to declare a significant association.
Variables and operational definition
Affordability of health service was the outcome variable measured as affordable health service: after computing the sum of the five (0–4) Likert scale-based responses of participants, health service is said to be affordable for patients with a score of mean and below the mean score (4 ± 2.4) of computed values [18]. And non-affordable health service: a health service said to be non-affordable if the patient scores above the mean score (4 ± 2.4) of computed values [18].
Socio-demographic characteristics (age, sex, marital status, level of education, employment status, religion, residence, family size, occupation), economic-related factors ( source of finance for care, average transport cost, average expenditure of follow-up, monthly income, monthly follow-up), payment methods (CBHI, OOP, others), and disease- and treatment-related factors (classification of drugs, duration of the disease, family history of DM, types of DM, comorbidity, number of drugs prescribed, additional drugs used, nature of drugs prescription) were the independent variables that affect the outcome variable.
Essential medicines are those that satisfy the priority healthcare needs of a population. They are selected with due regard to disease prevalence, public health relevance, evidence of efficacy and safety, and comparative cost-effectiveness. They are intended to be available in functioning health systems at all times, in appropriate dosage forms, of assured quality, and at prices individuals and health systems can afford [19].
Result
Socio-demographic characteristics of health professionals
Out of them, 219 (55.9%) were males, 137 (34.9%) were aged 46–60 years old and only 73 (18.6%) aged below 30 years. The majority of participants, 291 (74.2%), were married, 140 (35.7%) completed primary and secondary education equally, and 216 (55.1%) were Muslim in religion. The majority of participants (318 (81%) were found to live in urban areas; 163 (41%) had less than 3000 ETB in average monthly income; and 239 (61%) had three or fewer family members (Table 1).
Table 1.
Socio-demographic characteristics of DM patients visiting DCSH, 2022/23 (n = 392)
| Variables | Categories | Frequency | |
|---|---|---|---|
| No | % | ||
| Sex | Male | 219 | 55.9 |
| Female | 173 | 44.1 | |
| Age | < 30 | 73 | 18.6 |
| 31–45 | 85 | 21.7 | |
| 46–60 | 137 | 34.9 | |
| > 60 | 97 | 24.7 | |
| Marital status | Single | 40 | 10.2 |
| Married | 291 | 74.2 | |
| Divorced, Widowed, Others | 61 | 15.6 | |
| Religion | Orthodox | 157 | 40.1 |
| Muslim | 216 | 55.1 | |
| Protestant | 19 | 4.8 | |
| Educational status | unable to read and write | 57 | 14.5 |
| primary education | 140 | 35.7 | |
| secondary education | 140 | 35.7 | |
| College and above | 55 | 14.0 | |
| Occupation | Merchant | 63 | 16.1 |
| daily labor | 19 | 4.8 | |
| Gov’t employee | 81 | 20.7 | |
| Non-gov’t employee | 34 | 8.7 | |
| Others | 195 | 49.7 | |
| Residence | Urban | 318 | 81.1 |
| Rular | 74 | 18.9 | |
| Average monthly income | < 3000 | 163 | 41.6 |
| 3000–6000 | 136 | 34.7 | |
| > 6000 | 93 | 23.7 | |
| Family size | <=3 | 239 | 61.0 |
| 4–6 | 135 | 34.4 | |
| > 6 | 18 | 4.6 | |
Economic-related factors
From the total of 392 DM patients who participated in this study, 259 (66%) of them were community-based health insurance users, 163 (41%) had an average monthly income of less than 3000 ETB, and 239 (61%) had an average expenditure of less than 200 ETB per follow-up (Table 2).
Table 2.
Economically related factors of DM patients visiting DCSH, 2023 (n = 392)
| Variables | Categories | Frequency | percentage |
|---|---|---|---|
| Payment method | CBHI | 259 | 66.1 |
| OOP | 115 | 29.3 | |
| Others | 18 | 4.6 | |
| Average monthly income | < 3000 | 163 | 41.6 |
| 3000–6000 | 136 | 34.7 | |
| > 6000 | 93 | 23.7 | |
| Average expenditure per follow-up | < 200 ETB | 239 | 61.0 |
| 200–400 ETB | 88 | 22.4 | |
| > 400 ETB | 65 | 16.6 | |
| Average expenditure per follow-up | < 50 ETB | 292 | 74.5 |
| 50–100 ETB | 19 | 4.8 | |
| 100–150 ETB | 58 | 14.8 | |
| > 150 ETB | 21 | 5.4 | |
| Source of finance | self-sponsored | 307 | 78.3 |
| Family | 35 | 8.9 | |
| government or | 23 | 5.9 | |
| NGO and other | 27 | 6.9 |
Disease and treatment-related factors
Above half, 230 (58.7%) of the participants had type 2 DM, the majority of participants had no comorbidities, only 28 (7%) of them had a family history of DM; and nearly 313 (80%) of prescriptions were essential, followed by 69 (17.6%) of generic prescriptions (Table 3).
Table 3.
Drug and treatment-related factors of DM patients visiting DCSH, 2023 (n = 392)
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Types of DM | Type 1 | 162 | 41.3 |
| Type 2 | 230 | 58.7 | |
| Presence of comorbidities | Yes | 108 | 27.6 |
| No | 284 | 72.4 | |
| Family history of DM | Yes | 28 | 7.1 |
| No | 364 | 92.9 | |
| Number of drugs prescribed | One | 244 | 62.2 |
| Two | 65 | 16.6 | |
| 3 and above | 83 | 21.2 | |
| type of treatment | Biguanides | 202 | 51.5 |
| Sulfonylureas | 50 | 12.8 | |
| Insulin | 128 | 32.7 | |
| Mixed | 12 | 3.1 | |
| Nature of prescription | Essential | 313 | 79.8 |
| Generic | 69 | 17.6 | |
| Brand | 10 | 2.6 | |
| Duration of disease | < 10 years | 370 | 94.4 |
| >= 10 years | 22 | 5.6 | |
| Number of follow-ups per month | 1 time | 365 | 93.1 |
| > 1 times | 27 | 6.9 |
Affordability of health service among DM patients
This study assessed the affordability of health service among DM patients on follow up and who were visiting Dessie comprehensive specialized hospital by using five questions. Among the DM patients, 211 (53.83%) found the health services affordable, with an interval of 48.85–58.72% at a 95% confidence interval with a p-value less than 0.05 and it was unaffordable for the rest 181(46.17%) with 41.28–51.15% confidence interval.
For the first question, are there times when you don’t take drugs prescribed by a doctor because of their costs? The majority (290, or 74% of participants) replied that it was rare, and none of them reacted very often. Similarly, 246 (62.8%) of participants reported that they didn’t take laboratory tests or exams because of their costs. A relatively higher number of participants decided not to get health services prescribed by a doctor but not covered by health insurance because of their costs, sometimes 151 (38.5%) and often 40 (10.2%). The majority (344, or 87.8%) of participants revealed that they didn’t face difficulty getting health care services because of the additional costs involved (babysitting, parking, etc.) (See Table 4; Fig. 1).
Table 4.
Affordability of health service-related questionnaires to diabetes patients at the outpatient clinic of DCSH, north-east Ethiopia, 2023
| SN | Questions | Response | ||||
|---|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Often | Very often | ||
| Frequency /Percentage | Frequency /Percentage | Frequency /Percentage | Frequency /Percentage | Frequency /Percentage | ||
| 1 | Are there times when you don’t take drugs prescribed by a doctor because of their costs? | 79/20.2 | 290/74 | 21/5.4 | 2/0.5 | 0 |
| 2 | Are there times when you don’t take laboratory tests or exams because of their costs? | 61/15.6 | 246/62,8 | 76/19.4 | 8/2 | 1/0.3 |
| 3 | Are there times when you decide not to get services prescribed by a doctor but not covered by health insurance because of their costs?151/38.5 40/10.2 | 74/19 | 121/31 | 151/38.5 | 40/10.2 | 6/1.5 |
| 4 | Are there times when you find it difficult to get health care services because of the loss of income it involves? | 168/43 | 158/40.3 | 36/9.2 | 19/4.8 | 11/2.8 |
| 5 | Are there times when you find it difficult to get health care services because of the additional costs it involves (babysitting, parking, etc.)? | 344/87.8 | 44/11.2 | 3/0.8 | 1/0.3 | 0 |
Fig. 1.
Affordability of health service among DM patients visiting Dessie comprehensive specialized hospital, Northeast Ethiopia, 2022/2023
Factors affecting the affordability of health service among DM patients
From socio-demographic factors, only marital status, and religion were variables that were significantly associated with the affordability of health services among DM patients visiting DCSH. The health service was found to be relatively affordable for 56,166 (57%) of married DM patients. With multivariable binary logistic regression analysis, the health service was 76% less likely to be affordable for married DM patients when compared to that of single DM patients (AOR = 0.24, 95% CI 1 715, P-value = 0.010). The odds of affordability of health service among protestant religion followers DM patients were 4.6 times that of orthodox Christian followers (AOR = 4.681, 95% CI 1.145–19.1388, P-value = 0.032). The service was affordable for DM patients aged between 3 and − 45 years (AOR = 4.432, 95% 1.691–11.95% CI 1.691–11.620.6200.002) and 46–60 years (AOR = 3.771, 95% CI 1.033–13.768, P-value = 0.045) 4.4 and 3.7 times, respectively, when compared to that of DM patients aged below 30 years. The affordability of health services was found to be 60% less likely among DM patients having 4–6 family members when compared to those with DM patients who have three or less family size (AOR = 0.401, 95% CI − 0.759, P-value = 0.005) (Table 5).
Table 5.
Multivariable analysis of the affordability of health service among DM patients visiting DCSH, 2022/23 (n = 392)
| Variables | Category | Affordability of service | 95% C.I. | |||
|---|---|---|---|---|---|---|
| affordable | Non-affordable | COR | AOR | p-value | ||
| Religion | Orthodox | 82 | 75 | 1 | 1 | |
| Muslim | 122 | 94 | 0.534(0.200-1.426) | 0.95 (0.554–1.645) | 0.866 | |
| Protestant | 7 | 12 | 0.449(0.170-1.186) | 4.68 (1.145–19.138) | 0.032 | |
| Marital status | single | 18 | 22 | 1 | 1 | |
| Married | 166 | 125 | 0.598 (0.343-0.643) | 0.24(0.083–0.715) | 0.010 | |
| others | 27 | 34 | 0.971 (0.435-2.165) | 0.26( 0.068–1.008) | 0.051 | |
| Family size | <=3 | 115 | 124 | 1 | 1 | |
| 4–6 | 85 | 50 | 1.694(0.635-0.819) | 0.40(0.212- 0.759) | 0.005 | |
| > 6 | 11 | 7 | 0.924(0.337-2.538) | 0.310(0.085- 1.136) | 0.077 | |
| Treatment type | Biguanides | 102 | 100 | 1 | 1 | |
| sulfonylureas | 32 | 18 | 0.700(0.215 − 2.280) | 0.46 (0.202–1.087) | 0.077 | |
| Insulin | 72 | 56 | 0.402 (0.111-0.852) | 0.36 (0.0141-0 0.961) | 0.041 | |
| Mixed | 5 | 7 | 0.556(0.167-1.844) | 0.69 (0.121–3.944) | 0.676 | |
| Average expenditure per follow-up | < 200 ETB | 113 | 126 | 1 | 1 | |
| 200–400 ETB | 51 | 37 | 2.912(1.598–5.303) | 0.67 (0.353-1.301) | 0.242 | |
| > 400 ETB | 47 | 18 | 0.34(0.951-3.772) | 00.23 (0.101-0.548) | 0.001 | |
| Payment method | CBHI | 124 | 135 | 1 | 1 | |
| OOP | 80 | 35 | 0.402(0.693-0.943) | 0.15 (0.072–0.345) | 0.000 | |
| Others | 7 | 11 | 1.44 | 0.83 (0.247–2.814) | 0.769 | |
| Average monthly income | <3000 ETB | 82 | 81 | 1 | 1 | |
| 3000–6000 ETB | 78 | 58 | 0.75(0.720-1.999) | 1.33 (0.695–2.541) | 0.390 | |
| > 6000 ETB | 51 | 42 | 0.52(0.531-9.995) | 3.38 (1.366–8.363) | 0.008 | |
| Prescription type | Essential | 171 | 142 | 1 | 1 | |
| Generic | 33 | 36 | 1.31(0.492 − 7.63) | 1.30 (0.671–2.503) | 0.441 | |
| Brand | 7 | 3 | 0.52(0.608-9.995) | 0.17 (0.033–0.917) | 0.039 | |
Average monthly income, payment method, and average expenditure per follow-up were found significant economical related factors which determine the affordability of health services among DM patients. The odds of affordable health service among DM patients having an average monthly income above 6000 ETB was 3.4 times that of those DM patients having an average monthly income ≤ 3000 ETB (AOR = 3.379, 95% CI 1.366–8.363, P-value = 0.001). on the other hand, the affordability of health service among DM patients who have an average expenditure of more than 400 Ethiopian birr was found 74% less likely when compared to those who expend < 200 ETB per follow-up (AOR = 0.236, 95% CI 0.101-0.548, P-value = 0.008). Similarly, the affordability of health service among DM patients who were using out-of-pocket payment methods was 84% less likely when compared to those who were using CBHI (AOR = 0.157, 95% CI 0.072–0.345, P-value = 0.000) (Table 5).
This study demonstrated that there was a significant association between the affordability of health services and the nature of drug prescription and treatment type from variables categorized under disease and treatment-related factors. The health service was affordable 83% and 63% less likely among DM patients with brand prescription (AOR = 0.174, 95% CI 0.033–0.917, P-value = 0.039) and insulin treatment type (AOR = 0.368, 95% CI 0.141–0.961, P-value = 0.041) respectively (Table 5).
Discussion
This study aimed to assess the affordability of health services and associated factors among DM patients visiting DCSH 202/2023. Hence, the current study showed that the affordability of health services among DM patients was 53.8% (95% CI, 47.9–58.2). This figure illustrates that the health care service was not affordable for nearly half of DM patients which seeks attention. Global reports from low, middle and high-income countries reflected similar figures and strengthened the fact that healthcare affordability has long been a top concern for patients [2, 19, 20]. Particularly these reports indicate that managing diabetes is an expensive condition [7]. The average annual expenditure of DM patients for treatment of DM in this study was found to be 4100 ETB ($81). It is in line with a systematic search of eight suitable studies carried out in poor and lower middle-income nations which shows type 2 diabetes mellitus treatment expenses ranged from USD 29.91 to USD 237.38 per person annually [5]. The reason behind this similarity might be the nature of the disease and healthcare provision approach across the globe said to be almost similar which made patients invest in the same way and amount. Again the cost of the disease is UN disputable even for patients living in developed countries [19].
The result of this study was higher than that of finding from Eastern Uganda, the health service for the management of DM was affordable for a small number of diabetic patients (5.7%) [21]. This variation might be due to the set-up where the study was conducted. The study in Uganda was conducted at a tertiary care hospital with higher expenditure per prescription (11 USD), the current study was conducted for services to manage DM at the DCSH, it was believed that the charge for health care services at tertiary care centers was relatively higher [22] and parallel to this the affordability of service for patients may decrease.
Again the result of this study was higher than another study conducted locally at Jimma Ethiopia showed that the affordability of essential medicines was only 36.1% [13]. This inconsistency might be due to the difference in target population; the current study was conducted among DM patients while the study at Jimma was conducted among patients diagnosed with DM, hypertension, and other communicable diseases. The average expenditure is supposed to be increased as the number of diseases considered, in line with the affordability of health services for patients with a number of pathological problems might decline.
Age and marital status were among the socio-demographic factors that were significantly associated with the affordability of health services among DM patients visiting Dessie Comprehensive Specialized Hospital. With multivariable binary logistic regression analysis, the service was affordable for DM patients aged between 31 and 45 years and 46–60 years, 4.4 and 3.7 times respectively when compared to that of DM patients aged below 30 years. Again the affordability of health service was found 60% less likely among DM patients having 4–6 family members when compared to those DM patients who have three and less family size.
The finding of this study was supported by a result gained from a systematic review conducted to evaluate the cost of treating type 1 and type 2 DM. The study revealed that age was among the Socio-demographic factors which determine the affordability of DM treatments significantly [5]. Again a study in Thailand reported that age was mentioned as a determinant factor which affects the affordability of healthcare costs for diabetic patients [4]. Another study in Ghana highlighted that older adults are also more susceptible to economic dangers, the senior population is burdened by high healthcare costs and services are not affordable for them [23]. The study conducted at Jimma Ethiopia reported there was a significant association between service affordability and the age of patients. Health service was found affordable for patients aged 30–44 and 45–64 years by those aged 65 years and above. Almost all of the studies mentioned above were in line with the current study in this regard. This similarity among these studies might be linked to the state of productivity through age. The age group between 30 and 60 years is the age of productivity when people engage in better-yielding work and put themselves on a stable life [24]. As a result, their productivity enables them to pay for services easily when compared to those above 60 with minimal income, retirement issues, and those aged below 30 which is a period of searching for income sources and struggling for independence.
The socio-demographic factor that was associated significantly with the affordability of health service was marital status as the affordability of health service was 76% less likely for married DM patients when compared to that of single DM patients. In the same way, the study conducted at Jimma showed that being married and single was significantly associated with the non-affordability of health services when compared to widowed patients. The cause for this consistency among these studies and the current study might be patients engaged in marriage were more likely to get a child (the number of dependent families) which will increase their expenses for daily living, as a result, their ability to pay for medical service could decrease and in turn, health services become unaffordable for them.
This study revealed that the average monthly income and payment method were found to have significant economic-related factors which determine the affordability of health services among DM patients. The odds of affordable health services among DM patients having an average monthly income above 6000 ETB ($120) was 3.4 times that of those DM patients having an average monthly income ≤ 3000 ETB ($60). On the other hand, the affordability of health services among DM patients who were using out-of-pocket payment methods was 84% less likely when compared to those who were using community-based health insurance.
Likewise, the study at Jimma revealed that patients having an average monthly income of $ 51–115and $ 116–170 were associated with affordability of services at p-value < 0.001 when compared to those who have less. These results showed similar figures, the reason behind this might be due to the increased ability of patients to pay for services as their income becomes better.
The current study identified that patients using out-of-pocket payment methods were less likely to afford payment for services. Similarly, payment methods (out-of-pocket) were significantly associated with higher healthcare costs in a study in Thailand [22]. Again, reviews from low and middle-income countries showed that Out-of-pocket expense (OOP) payments are the primary source of healthcare financing and continue to be a cause for non-affordable healthcare costs in LMICs [7]. It may be due to that pocket method exposing them to unpredictable expenses while other payment methods like CBHI makes patients invest in their health with a plan and make service affordable to them as the coast for the service is not determined by number and quality of service they gained (payment done annually regardless of service they will get). This makes them not to worry about payment.
This study demonstrated that there was a significant association between the affordability of health services and the nature of drug prescriptions and treatment types based on variables categorized under disease and treatment-related factors. The health service was 83% less likely among DM patients with brand prescriptions. The study in Uganda showed that affordability went down with the order of drugs by brand [21]. The study mentioned that the percentage of prescriptions of drugs by generic name and from the essential medicine and health supplies list of Uganda was 82.6% and 81%, respectively, and by far it was 17% and 79% in the current study, respectively, which is against the WHO standard of 100% [21]. According to the report from Nepal, the majority of prescriptions were by brands (54.7%) [25]. The link between brand prescription and higher cost might be that drugs with brand prescription will narrow patient’s chances of getting drugs with different trade names with consideration of cost and force them to buy the ordered brand only. As a result, patients may not be able to afford the cost of it.
This study mentioned that the health service was 63% less likely among DM patients with insulin treatment types. Similarly, the study in Uganda reflected that patients with insulin therapy were 17.8 times more unaffordable than patients treated with biguanides [21]. Again, medication therapies for type 2 diabetes non-insulin treatment were affordable in the Iranian study [26]. Similarly, a study in Thailand reported that diabetic patients taking insulin had significantly higher healthcare costs [22]. The reason behind this could be the relatively higher price of insulin, which makes it less likely to be an affordable health service [14].
Limitations of this study
Since a cross-sectional study design was used in this study, it can’t show us a causal relationship between outcome and explanatory variables.
Conclusion
This study showed that healthcare services at Dessie Comprehensive Specialized Hospital were found affordable for nearly half of diabetes mellitus patients, which was low when compared to the ideal affordability of health services. Age, marital status, average monthly income, payment method, nature of drug prescription, and treatment type were among the factors that came into play to determine the affordability of health services among diabetes mellitus patients.
Acknowledgements
The authors acknowledged Wollo University, the College of Medicine and Health Sciences, the School of Public Health, and the Department of Public Health for the support and facilitation of the research work. The authors also acknowledged all data collectors, supervisors, and DCSH staff for their contribution to this research.
Abbreviations
- CHE
Catastrophic Health Expenditure
- DCSH
Dessie Comprehensive Specialized Hospital
- DM
Diabetes Mellitus
- EMs
Essential Medications
- GDP
Gross Domestic Product
- HPs
Health Posts
- IDF
International Diabetes Federation
- LMICs
Low- and middle-income nations
- NCDs
Non-Communicable Diseases
- OPD
Out-Patient Department
- OOP
Out-of-pocket
- SPSS
Statistical Package for Social Science
- USD
United States Dollar
- WHO
World Health Organization
Authors’ contributions
The authors confirm contribution to the paper as follows: study conception and design: WG, Author; data collection: AMM and AM, Authors; analysis and Interpretation of results: YT, and EMG Author; draft manuscript preparation: All authors reviewed the results and approved the final version of the manuscript.
Funding
to conduct this study the investigators didn’t receive any grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
All relevant data are within the manuscript.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical Review committee of College of Medicine and Health Sciences at Wollo University, with reference number CMHS/789/2016, on July 1, 2023, and supporting letter was taken from the Dessie Comprehensive Specialized Hospital in the study area. The study was conducted following the ethical principles of the Declaration of Helsinki. This study adhered to ethical guidelines, ensuring the study participants’ privacy, confidentiality, and voluntary participation. Written informed consent was obtained from all participants before data collection. Participants were informed of their right to withdraw from the study at any time without any consequences. Confidentiality was maintained throughout the study. The study protocol was submitted to the relevant ethical review committee of College of Medicine and Health Sciences at Wollo University for approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Supplement1):S81–90. [DOI] [PubMed] [Google Scholar]
- 2.Pandey AR, Aryal KK, Shrestha N, Sharma D, Maskey J, Dhimal M. Burden of diabetes mellitus in Nepal: an analysis of global burden of disease study 2019. J Diab Res 2022;2022(1):4701796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T, Owens DR, Thomas RL, Song S, Wong J, Chan JC. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia. 2021;64:275–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor SJ, Pinnock H, Epiphaniou E, Pearce G, Parke HL, Schwappach A, Purushotham N, Jacob S, Griffiths CJ, Greenhalgh T, Sheikh A. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS practical systematic review of self-management support for long-term conditions). Health Serv Delivery Res. 2014;2(53):1–580. [PubMed] [Google Scholar]
- 5.Abebe S, Paulos W, Tschopp R. Diabetes prevalence and associated factors in the adult population aged 25–64 in the Humbo districts of Woliata Zone, 2020. Int J Diabetes Endocrinol. 2023;8(1):21–7. 10.11648/j.ijde.20230801.15.
- 6.Watkins JB. Affordability of healthcare: a global crisis. Value Health. 2018;21(3):280–2. [DOI] [PubMed] [Google Scholar]
- 7.Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low-and middle-income countries: a systematic review. BMJ Global Health. 2019;4(1):e001258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman T, Gasbarro D, Alam K. Financial risk protection from out-of-pocket health spending in low-and middle-income countries: a scoping review of the literature. Health Res Policy Syst. 2022;20(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nazir MA, AlGhamdi L, AlKadi M, AlBeajan N, AlRashoudi L, AlHussan M. The burden of diabetes, its oral complications, and their prevention and management. Open Access Macedonian J Med Sci. 2018;6(8):1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forum nq. Measuring Affordability from the Patient’s Perspective. 2022.
- 11.Zarei L, Peymani P, Moradi N, Kheirandish M, Mirjalili M, Zare M. Affordability of medication therapy in diabetic patients: a scenario-based assessment in Iran’s health system context. Int J Health Policy Manag. 2022;11(4):443–52. [DOI] [PMC free article] [PubMed]
- 12.Yunka TT, Mogas SB, Zawdie B, Tamiru D, Tesfaye Y, Kebede A, et al. The hidden burden of diabetes mellitus in an urban community of southwest Ethiopia. Diabetes Metab Syndr Obes: Targets Ther. 2020;13:2925. [DOI] [PMC free article] [PubMed]
- 13.Obakiro SB, Kiyimba K, Napa A, Kanyike AM, Mayoka WJ, Nnassozi AG, et al. Appropriateness and affordability of prescriptions to diabetic patients attending a tertiary hospital in Eastern Uganda: A retrospective cross-sectional study. PloS one. 2021;16(1):e0245036. [DOI] [PMC free article] [PubMed]
- 14.Assefa B, Wondimu A, Abrha S, Dinda SC, Demeke B, Gebre-Samuel N, et al. Pharmacoeconomic evaluation of anti-diabetic treatment at Ayder Referral Hospital, Mekelle, Ethiopia. Age (Years). 2014;35(56):4308. [Google Scholar]
- 15.Shrestha R, Ghale A, Chapagain BR, Gyawali M, Acharya T. Survey on the availability, price, and affordability of selected essential medicines for non-communicable diseases in community pharmacies of Kathmandu valley. SAGE open Med. 2017;5:2050312117738691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussien M. Access to essential medicines in primary health care units of South Wollo Zone, Ethiopia. Open Access Libr J. 2015;2(01):1. [Google Scholar]
- 17.Cheng Q, Lazzarini PA, Gibb M, Derhy PH, Kinnear EM, Burn E, et al. A cost‐effectiveness analysis of optimal care for diabetic foot ulcers in Australia. Int Wound J. 2017;14(4):616–28. [DOI] [PMC free article] [PubMed]
- 18.Nagarathna R, Madhava M, Patil SS, Singh A, Perumal K, Ningombam G, et al. Cost of Management of Diabetes Mellitus: A Pan India Study. Ann Neurosci. 2020;27(3-4):190–2. [DOI] [PMC free article] [PubMed]
- 19.Hub hcv. Making Healthcare Affordable: Finding a Common Approach to Measure Progress. 2017.
- 20.Yuldashov Jamshid T. Healthcare Affordability. 2023. p. 105–20. 10.1007/978-3-031-19719-2_5. [Google Scholar]
- 21.Chaikledkaew U, Pongchareonsuk P, Chaiyakunapruk N, Ongphiphadhanakul B. Factors affecting health‐care costs and hospitalizations among diabetic patients in Thai public hospitals. Value Health. 2008;11:S69–S74. [DOI] [PubMed]
- 22.Acquah-Hagan G, Boateng D, Appiah-Brempong E, Twum P, Amankwa Atta J, Agyei-Baffour P. Availability and Affordability of Primary Health Care Among Vulnerable Populations in Urban Kumasi Metropolis: Family Health Perspective. Health Equity. 2022;6(1):345–55. [DOI] [PMC free article] [PubMed]
- 23.Mathewos Oridanigo E, Beyene Salgedo W, Gebissa Kebene F. Affordability of Essential Medicines and Associated Factors in Public Health Facilities of Jimma Zone, Southwest Ethiopia. Adv Pharmacol Pharm Sci. 2021;2021:1–9. [DOI] [PMC free article] [PubMed]
- 24.Beran D, Ewen M, Laing R. Constraints and challenges in access to insulin: a global perspective. Lancet Diabetes Endocrinol. 2016;4(3):275–85. Office Dcm. administrative and astronomical information of Dessie city administration. 2012. [DOI] [PubMed]
- 25.Haggerty JL, Levesque J-F. Development of a measure of health care affordability applicable in a publicly funded universal health care system. Can J Public Health. 2015;106(2):e66–71. [DOI] [PMC free article] [PubMed]
- 26.Börsch-Supan A, Weiss M. Productivity and age: Evidence from work teams at the assembly line. J Econ Ageing. 2016;7:30–42.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript.