Abstract
Background
Formal evidence regarding the effects of sanctions on population health status and the health system is scarse in Iran. Given the intricate and multifaceted nature of sanctions, a nuanced understanding of their impact is imperative. We aimed to investigate the magnitude and effects of sanctions on population health and healthcare system during the last two decades in Iran.
Design
This is a mixed-methods research. We quantified the impact of sanctions using 28 indicators, i.e. macroeconomic, healthcare resources and health outcomes indicators from 2000 to 2020. The concurrent qualitative study aimed to explore the pathway of the effect by considering perceptions of both patients and health policy makers towards sanctions; Interview data was analyzed using content analysis.
Setting
This study was conducted in Iran at both national and sub-national levels.
Results
Our findings revealed that the trend of 11 indicators (39.2%) had changed after the change point in 2009; four indicators (14.2%) significantly deteriorated after the change point. Further, five indicators revealed significant increases during the sanctions period: Out-of-Pocket payment (OOP), household expenditure on food and mortality rates due to Chronic Obstructive Pulmonary Disease (COPD), thalassemia and hypertension. Our qualitative analysis revealed that patients identified availability, cost and quality of medicines and healthcare services as the most significant challenges that compromised population’s health. From the policy makers’ perspective, the effect of sanctions on health system functions and infrastructures, i.e. economic, political, social, educational and research had significant repercussions on population health.
Conclusion
We could not find compelling evidence to establish significant associations between the imposition of sanctions and the trend of population health. Nevertheless, our qualitative study revealed people’s deteriorating life experiences, e.g. increasing catastrophic health expenditure, limited access to necessary medicine, medical equipment, procedures and interventions, imposed by sanctions, with ultimate reducing impact on the overall quality of life. It seems that sanctions have negatively affected financial and physical access to medication and healthcare services. Nonetheless, Iran has demonstrated remarkable resilience against their highly detrimental effects, maybe due to its established economic infrastructure and healthcare system.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12992-024-01084-2.
Keywords: Economic sanctions, Public health, Healthcare system, Health policy, Iran
Background
Although intermittent international sanctions against Iran has been in place since the 1950s, the revolution of 1979 was the beginning of continuous sanctions. The most recent round of sanctions began in 2001 and intensified in recent years, particularly following the United States’ (US) withdrawal from the Joint Comprehensive Plan of Action (JPOA) in May 2018. Sanctions on Iran were imposed by various countries and international organizations. These sanctions mainly target Iran’s nuclear program and aim to pressure the country to curtail its nuclear activities. The sanctions typically involve restrictions on Iran’s ability to conduct certain financial transactions, trade in certain goods and services, and access international financial markets. They have also included arms embargoes and asset freezes on specific individuals and entities [1]. The initial purpose of sanctions was to constrain Iran’s economic activities, international trade, and military. Nevertheless, due to their far-reaching consequences, the imposed sanctions were perceived to have affected population health and the healthcare system in both direct and indirect manners. For instance, the cost of healthcare services increased, which in turn led to reduced access to and utilization of healthcare services, as well as increased unmet healthcare needs [2–5]. The USA’s Office of Foreign Assets Control (OFAC) reported some efforts to facilitate humanitarian trade in medicine, medical supplies, and equipment despite the sanctions [6]. Nonetheless, mainly due to troublesome banking transactions, Iran continues to face challenges in importing essential medicines and medical equipment [6, 7].
In terms of the impact on Iran’s health outcomes, the sanctions have had significant repercussions. The restrictions on financial transactions have made it difficult for Iran to purchase medical supplies and equipment, leading to shortages in healthcare facilities. This, in turn, has affected the quality of healthcare services and ultimately the health outcomes of the Iranian population. Moreover, the sanctions have also hindered Iran’s ability to access international expertise and advancements in the medical field. This has had implications for the country’s capacity to develop and implement effective healthcare programs and initiatives [7–9].
However, it is important to note that the impact of sanctions on Iran’s health outcomes cannot be viewed in isolation from other factors within the global political economy. The country’s internal policies, economic conditions, healthcare infrastructure, and demographic characteristics also play significant roles in shaping its health outcomes. Additionally, regional conflicts, natural disasters, and global health crises can further exacerbate the challenges faced by Iran’s healthcare system [10–12].
During past four decades, the extensive Primary Health Care (PHC) network and recent initiatives towards Universal Health Coverage (UHC) have led to significantly improved health indices, i.e., life expectancy, neonatal, maternal, and child mortality ratios, vaccination coverage, etc [13, 14]. Nevertheless, there are still approximately six million Iranians with communicable and Non-Communicable Diseases (NCDs) who face significant challenges in access to their essential healthcare [15]. The decline in access to care, particularly essential medicines, poses a significant threat to public health in Iran [15, 16]. These challenges persist despite the principles outlined in the Universal Declaration of Human Rights and various international agreements that affirm access to healthcare, medicines, food, and other essential goods and services as fundamental rights for all global citizens [15, 17–20].
Over the past two decades, the impact of sanctions on Iran’s healthcare system has attracted growing research attention [6, 7, 17, 19, 20]. Our literature review underscores a gap in research concerning the effects of sanctions on public health and the healthcare systems in Iran, including scarce comprehensive and quantitative studies on systematic assessment of the consequences of sanctions on functions and outcome indicators of the health system [21, 22]. Several studies have identified shortages of essential medicines, increased healthcare costs, and deteriorating health outcomes as key effects of sanctions [3, 13]. For instance, one study highlighteddisruptions in Iran’s pharmaceutical supply chains as a result of sanctions, which led to drug shortages that particularly affected patients with chronic and rare diseases [3]. Another work pointed to the increasing prices of healthcare services as a result of economic instability caused by sanctions [23]. While these studies offer invaluable insights, they are often limited in scope, focusing primarily on the immediate impacts of sanctions without a comprehensive examination of long-term health outcomes or the sub-national disparities in healthcare access.
Despite the existing body of work, significant gaps remain in the literature on sanctions and healthcare. Most studies have focused narrowly on specific aspects, such as drug shortages or expert opinions on healthcare policy [3, 6]. These studies, while important, often overlook broader systemic issues such as the impact of sanctions on healthcare infrastructure, workforce availability, and the long-term health outcomes of the population. Moreover, there is a dearth of quantitative studies that track healthcare indicators over extended periods to assess the full impact of sanctions. Few studies have examined the differential impact of sanctions across regions within Iran, despite evidence that sanctions may exacerbate existing regional inequalities in healthcare provision and access [13]. Additionally, most prior research has not integrated the perspectives of patients or healthcare providers, which are crucial for understanding the practical, lived experiences of sanctions.
Our study aims to address these gaps by providing a comprehensive, long-term analysis of the impact of sanctions on Iran’s healthcare system from 2000 to 2020. We utilize a mixed-methods approach, combining quantitative data from 28 healthcare indicators with qualitative insights from interviews with patients and policymakers. This approach allows us to assess the direct and indirect effects of sanctions on the healthcare system at both national and sub-national levels. By incorporating regional data, we explore how sanctions may have worsened existing inequalities in healthcare access and outcomes across provinces. Furthermore, our study adds depth to the current literature by integrating qualitative data on patient and policymaker perspectives, which provides a more nuanced understanding of the ways in which sanctions affect healthcare delivery and health outcomes.
Our work makes several novel contributions, we envisage, to the literature on sanctions and healthcare. First, it is one of the few studies to examine the long-term effects of sanctions on healthcare at both the national and sub-national levels, filling a critical gap in the literature. Second, by using a mixed-methods approach, we offer a more comprehensive understanding of how sanctions impact healthcare, combining both quantitative data on healthcare outcomes and qualitative insights into patient experiences and policy challenges. Third, our findings highlight the resilience of Iran’s healthcare system in certain areas, despite the severe pressures imposed by sanctions, and provides evidence for potential policy interventions that could mitigate the negative effects of future sanctions.
Setting
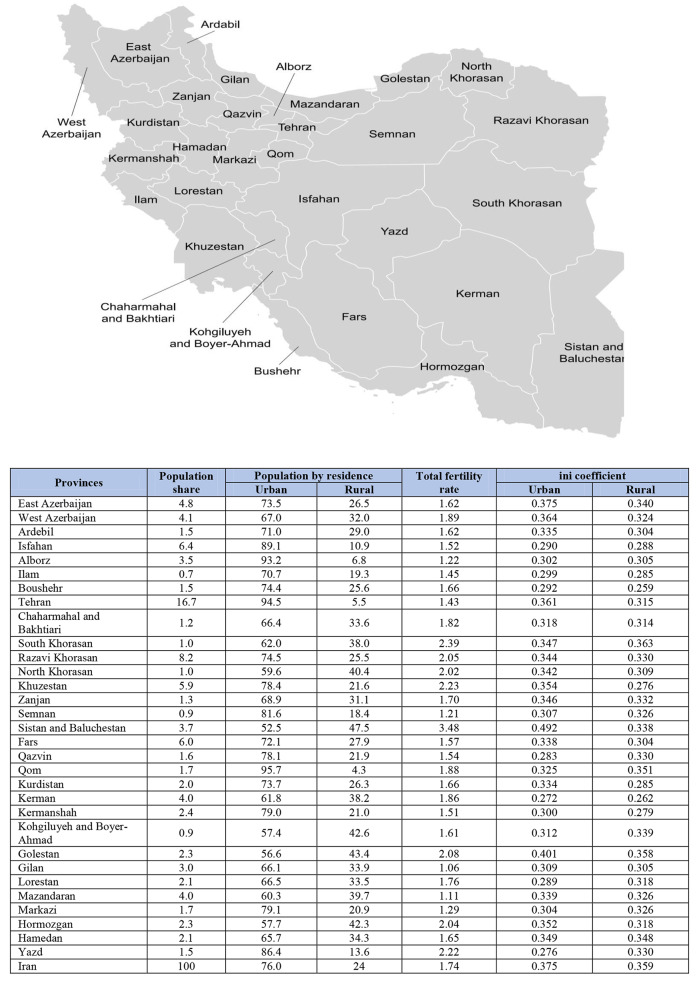
Iran is located in West Asia. Figure 1 presents geographic map of provinces, population proportions and other indicators in 2021. The Ministry of Health and Medical Education (MoHME) serves as the stewardship of the health system in Iran. It operates through a comprehensive network of over 70 universities of medical sciences (UMSs) across 31 provinces. Table 1 presents the summary of main health indicators in Iran.
Fig. 1.
Provinces in Iran, proportion shares and selected indicators for 2021. (Source: Statistical center of Iran)
Table 1.
Summary of main health indicators in Iran
| Population | 88,550.57 (2022) |
| GDP per capita (US$) | US$ 4,669.6 (2022) |
| Current health expenditure (% of GDP) | 5.34 (2020) |
| Life expectancy at birth (Year) | 74 (2021) |
| Healthy life expectancy (HALE) at birth (Year) | 65.2 (2019) |
Methods
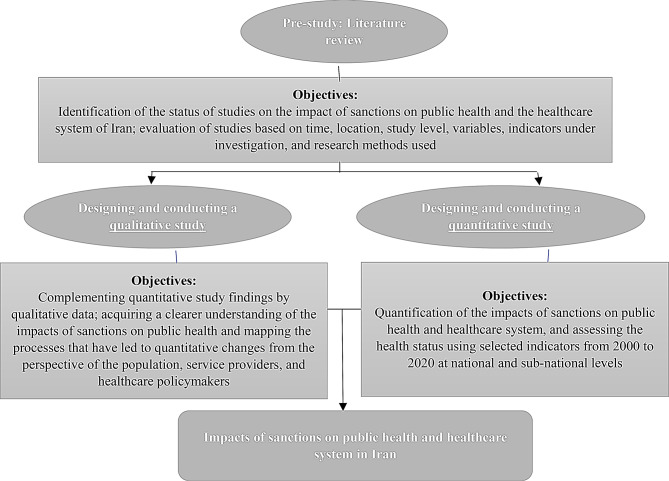
This is a mixed-methods (quantitative/qualitative) study that was conducted during 2019–2022. The quantitative study aimed to measure the effect of sanction on 28 selected healthcare indicators, i.e., macroeconomic, healthcare resources and health outcomes indicators at both national and sub-national levels for the period 2000 until 2020. We used Join Point Regression (JPR) and General Additive Mixed Effect Models (GAMM) to capture changes in trends and relationships between variables. The qualitative study included semi-structured interviews to explore patients and health policy makers’ opinions regarding the effects of sanction. We collected data using in-depth, face to face, semi-structured interviews which were analyzed using content analysis to identify recurring themes and subthemes (Fig. 2) [24].
Fig. 2.
Schematic protocol of study to evaluate the impact of sanctions on health and the healthcare system in Iran
Quantitative study
We conducted a panel data analysis to evaluate the impact of sanctions on public health and the healthcare system from 2000 to 2020 (Fig. 3) at the national and sub-national (provincial) levels in Iran.
Fig. 3.
The timeline of sanctions against Iran, 2000–2020
Study variables
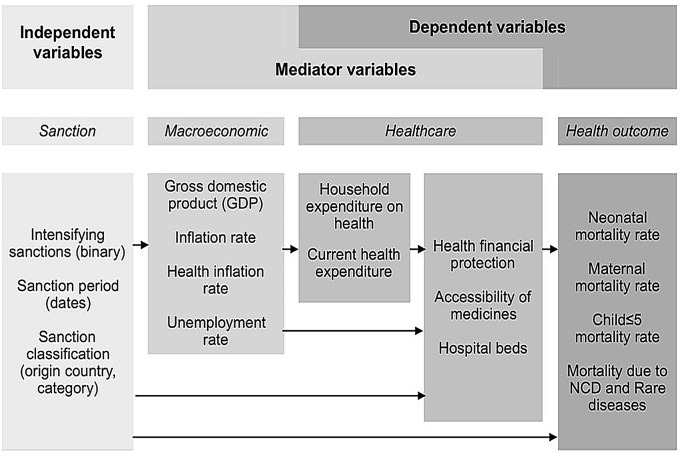
The process of variable selection involved three steps, i.e. literature review, database review and expert panel discussion (Table 2) using three categories of variables: independent, dependent, and mediator variables. Figure 4 illustrates the study variables and their relationships. Appendix 1 provides a detailed list of study variables and their respective sources.
Table 2.
Steps and process of selecting variables
| Indicator selection steps | Description | Number of indicators | |
|---|---|---|---|
| Step 1: Literature review |
- Study period: 2000–2020 - Databases: PubMed/Medline/Scopus - Key words: Sanction*, Economic sanction*, Health*, Medicines*, Variables*, Indicators* Included criteria: Subject, year, English & Persian language |
105 | |
| Step 2: Database review | We searched national and international databases, i.e. various disease registration systems, hospital and pharmaceutical resource registration systems, mortality registration systems, etc., and identified the variables and indicators with available data for the study years, both at the national and provincial level. |
50 (55 indicators were removed) |
|
| Step 3: Expert panel discussion | Through expert panel discussions, which included scientific advisors and members of the study team, we assessed the importance of each variable based on the study objectives and their significance for policymakers. | 28 (50 indicators were removed) | |
| Number of final indicators | Macroeconomic | 3 | |
| Healthcare | 6 | ||
| Health outcomes | 19 | ||
| Sum | 28 | ||
Fig. 4.
The study indicators and their hypothesized relationships
Data collection, tool and management
We collected data from June 2020 until March 2021. For the national-level, we first identified the data sources, asked the relevant organizations to share data, and then extracted them. We recorded the unit of measurement for the indicator and the required years, which enabled us to extract data in various formats. The research team thoroughly reviewed data sources and decided their inclusion by consensus. In case of data discrepancy among various sources, we gave priority to official sources over others.
To organize diverse databases and various types of data, we entered all collected data into 28 Excel worksheets (Appendix 2). All quantitative study data are presented in “Supplementary information 1”. We performed data cleaning to fit the collected data into statistical models. Missing data were present in some of the health and economic indicators, particularly in the provincial-level data. The extent of missing data ranged from 5 to 20%, depending on the indicator, with the primary causes being incomplete data collection at the provincial level, administrative delays, and reporting inconsistencies. The process involved the utilization of the “tidyverse” and “Amelia” packages in the R-4.2.1 software, which uses a multiple imputation approach based on bootstrapping to estimate plausible values for the missing entries. The imputation technique in “Amelia” assumes that the data are Missing At Random (MAR) and uses all available variables to generate multiple imputed datasets. These datasets were then averaged to account for the uncertainty in the imputations, ensuring that the variability introduced by missing data was incorporated into the analysis. We selected this method because of its ability to handle time-series and panel data, making it suitable for our study, which included data from 2000 to 2020. Outlier data management was carried out twice: first before model fitting to identify data anomalies due to registry errors, which were subsequently addressed through revision or omission. We then identified outlier data by conducting residual tests. To address missing data during the pre-processing step, we used the “Amelia” package in the R-4.2.1 software. Because the initial data registry format, referred to as “wide” in statistical terms (illustrated as a longitudinal study), was unsuitable to be used in the R software, we introduced a new variable called “sanction status” based on the sanction period (before, during, and after sanctions) to transform the data format into “long”; see Appendix 3.
Statistical analysis
We used JPR for impact assessment as the main analysis to test the study hypothesis regarding the impact of sanctions on health indicators. Also known as segmented regression or piecewise regression, JPR is a statistical technique used to analyze the relationships between variables when there is a change in the slope of the relationship at a specific point, known as the joint point. JPR allowed us to identify and estimate the location of the joint point, as well as the slopes of the regression lines before and after the joint point. The joint point represents the point at which there is a significant change in the studied indicators, due to a variety of factors such as an intervention, policy change, or natural occurrence. Our assumption was that the sanctions could make changes to the health indicators in this study.
To perform JPR, we divided data into two or more segments. Separate regression lines were then fitted to each segment, allowing for different slopes and intercepts. The joint point was estimated by finding the point where the two segments intersect. We assumed that a single change point existed in the trend of the community health indicators, the year 2009 was selected as the reference point due to its close proximity to the midpoint of the study period. The model was applied at both the provincial and national levels. Graphs were generated using the ggplot2 package, and the change point model was fitted using the mcp package within R-4.2.1 (further details regarding assumptions and statistical inferences can be found in Appendix 4 and [24]).
To validate the robustness of the 2009 change point, we conducted a sensitivity analysis with alternative change points. To address this, we carried out a sensitivity analysis by testing additional potential change points, including years such as 2008 and 2010, which also aligns with key economic developments. The results of this sensitivity analysis indicated that while slight variations exist, the most robust change in the health indicators remains around 2009, supporting our original choice.
Credible intervals were computed using Markov Chain Monte Carlo (MCMC) methods to estimate the posterior distributions of the regression coefficients. The p-values were derived from these intervals, based on whether zero was included in the credible interval, which indicated the statistical significance of the coefficients.
To assess the reliability of the model, we performed residual analysis. Residual plots were inspected for normality and independence, with no clear patterns indicating model misfit. Additionally, we computed Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC) to evaluate the goodness-of-fit of the model. Both AIC and BIC were used to compare models with different numbers of change points, ensuring the best model fit for the data.
We used “mediation analysis” to confirm shifts in trends and quantify the relationships between sanctions and variables. These models allowed for the measurement and estimation of direct and indirect effects, utilizing a mediator variable like the health sector inflation rate on the health outcome variable. In the mediation analysis, two simultaneous regression models were fitted to the data. In the first regression model, the focus was on estimating the effect of sanctions on the mediator variables (macroeconomic indicators and healthcare resources), while the second regression model aimed to estimate the effect of the mediator variables on the health outcome variables. The resulting output of the mediation analysis provided insights into both the direct and indirect effects of sanctions on the health outcome indicators. For mediation analysis, this study utilized the GAMM, which can measure complex functional relationships among other covariates and outcome variables. We selected GAMM over traditional linear models because of its flexibility in handling complex, nonlinear relationships and its capacity to incorporate both fixed and random effects. This was essential for our analysis, which included data from multiple provinces over time, where unobserved heterogeneity may exist. GAMM provides the ability to model random effects, while allowing for smooth, nonparametric relationships between variables, improving the accuracy and interpretability of the mediation analysis. The mediation analysis was conducted using the “medflex” and “mgvc” packages of the R-4.2.1 software.
While the sanctions have undoubtedly had a negative impact on Iran’s health sector, it is essential to consider the broader context of the global political economy and its various dimensions when assessing their overall impact on the country’s health outcomes. We aimed to control for other variables and their impact on health by initially examining the probability of a change in the trend of the health indicators using the JP method. Subsequently, we conducted a Mediation analysis where we included macroeconomic variables for analysis. By incorporating these variables, we sought to consider other factors and crises that could potentially affect public health, because any changes or crises related to these macroeconomic variables (such as GDP, inflation, and unemployment rate) can have an impact on overall economic health.
To ensure the reliability of the collected data across the 28 macroeconomic, healthcare resource, and health outcome indicators, we applied several rigorous statistical techniques. Missing data were addressed using the “Amelia” package for multiple imputation, which provided robust estimates of missing values by accounting for the relationships between variables. The multi-dimensional nature of the data was handled using JPR to identify changes over time, combined with GAMM to model non-linear relationships and random effects. These models were particularly suited for capturing the complex interactions between the macroeconomic and health indicators at both national and sub-national levels. By integrating these advanced statistical approaches, we ensured the reliability of the data and the robustness of our analysis in assessing the impact of sanctions.
Qualitative study
The qualitative phase lasted 20 months, from September 2019 to March 2021.
Participants and data collection
Two researchers (MMK and FE) conducted the interviews, using two generic semi-structured interview guides, developed in alignment with the study objectives, which incorporated input and insights from the study’s scientific advisors, see Appendix 5 and 6. The participants were categorized into two groups:
Patients, including 31 individuals under the coverage of Iran’s Health Insurance Organization (IHIO), provider of basic health insurance to half of Iranian population, who were diagnosed with chronic or rare diseases, selected from specific provinces based on their level of development. These provinces included Tehran, as one of the most affluent provinces; Sistan and Baluchistan, as the least developed provinces; Hamedan and Yazd, representing mid-level provinces. We selected patients randomly and approached them through their phone numbers provided by the IHIO. Due to the COVID-19 pandemic, all interviewed were conducted over telephone. After ensuring privacy and obtaining informed consent for participation and recording, we conducted the interview and made efforts to tailor our questions to accommodate the social status and literacy level of the interviewees. The average interview time was 20 min.
Healthcare providers and experts, who were carefully selected for their specific qualifications, including expertise in sanctions within the health sector, participation in decision-making related to resource allocation, possession of clinical expertise regarding rare diseases, knowledge of national macropolicies and plans, knowledge of the impacts of sanctions on public health, and their interest and willingness to participate in this study. In total, eight experts were interviewed in person for the average of 35 min. Initial introductions with these interviewees took place over the phone prior to the interview session, when we obtained their consent for participation and recording. Following the interviews, the recorded sessions were transcribed verbatim and analyzed.
The interviews and data collection continued until data saturation was reached.
Data analysis
We used an inductive approach to perform content analysis immediately after data collection. Three independent authors (MMK, FE, and HM) systematically reviewed the transcriptions of the interviews to identify recurring themes and sub-themes. We followed a stepwise process:
All interviews were transcribed verbatim, and the transcripts were read multiple times to ensure familiarity with the data.
The researchers independently generated initial codes based on recurring ideas or concepts.
Codes were grouped into categories and sub-themes, which were further organized into broader themes reflecting the participants’ perceptions of the impact of sanctions on healthcare access, availability, and costs.
The three researchers met to discuss discrepancies in coding and to reach consensus on the final themes. These themes were then validated by comparing them with the raw data.
We used MAXQDA 10 for data management and facilitating the analysis.
Results
Quantitative findings
Our findings revealed that the inflation rate, health inflation rate, household health expenditure, out of pocket payment (OOP), neonatal mortality rate (NMR), hypertension mortality rate, myocardial infarction mortality rate (MIMR), multiple sclerosis mortality rate (MSMR), stroke mortality rate (SMR), leukemia mortality rate (LMR) and prostate cancer mortality rate (PCMR) had significant changes after the change point (Cp > 2009). Among these, four indicators, i.e. household health expenditure, NMR, MIMR and PCMR showed a significant increase after Cp ( , while the latter had an increasing trend after the Cp (Upper and Lower of
, while the latter had an increasing trend after the Cp (Upper and Lower of  (Table 3).
(Table 3).
Table 3.
Results of JPR in the study indicators trends
| Row | Indicators1 | Cp (95% credible interval) 2 | β02- β01 (95% credible interval) 3 |
β12 (95% credible interval) 4 |
|---|---|---|---|---|
| 1 | GDP (Million_IRR)(log) | 2003.03(2003.00, 2003.08) | 0.43 (0.33, 0.55) | 0.34 (0.21, 0.50) |
| 2 | Inflation rate (%) | 2,013.93 ( 2011.42, 15.98) | -0.32 (-0.49, -0.16) | 0.01 (-0.01, 0.05) |
| 3 | Health inflation rate (%) | 2013.67(2012.07, 015.61) | -0.51 (-0.60, − 0.42) | 0.03 (0.01, 0.04) |
| 4 | Current health expenditure (Million IRR) | 2001.57(2001.00, 2002.21) | 0.16 (-0.01, 0.31) | 0.21 (0.19, 0.24) |
| 5 | Household health expenditure (%) | 2010.50 (2010.05–2011.00) | 0.34 (0.15, 0.55) | 0.03 (-0.00, 0.05) |
| 6 | Out of Pocket (OOP) (%) | 2011.57 (2006.35, 2014.00) | -0.12 (-0.36, 0.16) | -0.06 (-0.11, 0.01) |
| 7 | Share of household expenditure on food (%) | 2003.76(2003.00,2005.81) | -0.06 (-0.12, 0.00) | -0.06 (-0.08, -0.05) |
| 8 | Total hospital beds | 2003.05(2003.00, 2003.14) | 0.56 (0.46, 0.67) | 0.33 (0.26, 0.42) |
| 9 | Neonatal Mortality (NMR) | 2,013.40 (2012.34, 2014.56) | 0.53 (0.37, 0.68) | 0.00 (-0.03, 0.05) |
| 10 | Under-five mortality rate | 2008.55(2006.00, 2010.69) | -0.05 (-0.29, 0.17) | 0.00 (-0.05, 0.05) |
| 11 | Maternal mortality ratio (MMR) | 2008.70 (2003.00, 2018.89) | -0.16 (-0.36, 0.04) | 0.00 (-0.02, 0.02) |
| 12 | Cardiovascular disease mortality rate | 2008.58 (2006.00, 2011.60) | 0.08 (-0.20, 0.36) | -0.01 (-0.06, 0.04) |
| 13 | Hypertension mortality rate | 2011.02 (2009.90, 2012.41) | -0.70 (-0.89, -0.54) | 0.04 (0.01, 0.07) |
| 14 | Myocardial infraction mortality rate | 2011.15 (2006.00, 2016.38) | 0.34 (0.09, 0.59) | -0.02 (-0.05, 0.03) |
| 15 | Chronic Obstructive Pulmonary Disease (COPD) mortality rate | 2006.22 (2006.00, 2006.50) | -0.34 (-0.44, -0.27) | 0.09 (0.08, 0.11) |
| 16 | Diabetes mortality rate | 2007.01 (2006.002008.65) | -0.36 (-0.53, -0.21) | 0.10 (0.09, 0.12) |
| 17 | Multiple sclerosis mortality rate | 2011.13 (2009.89, 2012.70) | -0.65 (-0.97, -0.34) | 0.05 (0.00, 0.09) |
| 18 | Thalassemia mortality rate | 2007.40(2006.03, 2008.77) | 0.52 (0.32, 0.74) | -0.13 (-0.15, -0.10) |
| 19 | Stroke mortality rate | 2010.64(2006.00, 2015.22) | 0.20 (-0.17, 0.55) | 0.03 (-0.01, 0.07) |
| 20 | Brain tumor mortality rate | 2007.04(2006.00, 2008.79) | -0.73 (-0.86, -0.61) | 0.05 (0.04, 0.07) |
| 21 | Leukemia mortality rate | 2010.38 (2006.00, 2015.09) | 0.02 (-0.78, 0.77) | 0.02 (-0.02, 0.07) |
| 22 | Lung cancer | 2007.50 )2006.00, 2009.37) | 0.03 (-0.34,0.40) | -0.011 (-0.148, 0.13) |
| 23 | Colorectal cancer mortality rate | 2006.16 (2006.00,2006.54) | 0.98 (0.83, 1.14) | 0.12 (0.106, 0.14) |
| 24 | Gastric cancer mortality rate | 2006.27 (2006.00, 2008.35) | 0.63 (0.47, 0.78( | 0.39 (0.087 0.59) |
| 25 | Prostate cancer mortality rate | 2010.746 ( 2010.19, 2011.24) | 0.47 (0.37, 0.56) | 0.039 (0.025, 0.053) |
| 26 | Breast cancer mortality rate | 2006.27 (2006.00,2008.27) | 0.56 (0.41, 0.70) | 0.087 (0.077, 0.097) |
| 27 | Total cancer mortality rate | 2007.46(2006.20, 2009.08) | -0.25 (-0.37, -0.16) | 1.05 )0.03, 0.06) |
1. The logarithm of indices was used to perform these statistical analyses
2. “Cp” shows the join point of each indicator, when the indicator has undergone a specific change (latency time). Based on our hypothesis (Cp > 2009), the changes before 2009 were not due to sanctions
3. “β_01” and “β_02” are the average of indicators before and after Cp. Based on the study hypotheses (Cp > 2009, β_02-β_01 > 0), indicators that revealed a significant change after the sanctions are those with Cp > 2009, and the range (CIs of  does not include zero. If both the upper and lower limits are positive, it was concluded that the average of the examined indicators significantly increased after Cp
does not include zero. If both the upper and lower limits are positive, it was concluded that the average of the examined indicators significantly increased after Cp
4. “β_12” indicates the average change in the indicators after Cp per year; the rate of change of the indicator, showing the extent of increase or decrease in each time unit following Cp. According to our hypothesis (β_12 > 0), if Cp does not include the upper and lower bounds of zero, it can be stated that the examined indicators follow an upward trend after the Cp
.The “Unemployment rate (%)” was omitted because we could not find reliable data at the provincial level
The findings of mediation analysis indicated that OOP expenditure, household expenditure on food, COPD mortality rate, thalassemia mortality rate and hypertension mortality rate, showed a significant increase during the sanctions period (with multiplicative direct effect of 1.15, 1.06, 1.05, 1.02, and 1.01 respectively). In other words, the percentage changes of these indicators during the sanctions were 15%, 6%, 5%, 2%, and 1% more than before the sanctions period (P < 0.05) (Table 4).
Table 4.
Results of mediation analysis; the relationship between healthcare and health indicators and economic sanctions
| Numb | Indicators | Multiplicative direct effect1 | p-value2 |
|---|---|---|---|
| 1 | Household health expenditure (%) | 0.89 | 0.15 |
| 2 | Out of Pocket (%) (OOP) | 1.15 | 0.001 |
| 3 | The share of household expenditure on food (%) | 1.06 | 0.01 |
| 4 | Total hospital beds | 1.00 | 0.001 |
| 5 | Neonatal mortality rate (NMR) | 0.92 | 0.001 |
| 6 | Under-five mortality rate (per 1000 live births) | 0.92 | 0.001 |
| 7 | Maternal mortality ratio MMR) | 0.87 | 0.001 |
| 8 | Cardiovascular disease mortality rate | 0.95 | 0.92 |
| 9 | Hypertension mortality rate | 1.01 | 0/001 |
| 10 | Myocardial infarction mortality rate | 0.96 | 0.06 |
| 11 | COPD mortality rate | 1.05 | 0.41 |
| 12 | Diabetes mortality rate | 0.87 | 0.001 |
| 13 | Multiple sclerosis mortality rate | 0.83 | 0.02 |
| 14 | Thalassemia mortality rate | 1.02 | 0.01 |
| 15 | Stroke mortality rate | 0/91 | 0.06 |
| 16 | Brain tumor mortality rate | 0.86 | 0.001 |
| 17 | Leukemia mortality rate | 0.89 | 0.38 |
| 18 | Lung cancer mortality rate | 0.93 | 0.14 |
| 19 | Colorectal cancer mortality rate | 0.74 | 0.001 |
| 20 | Gastric cancer mortality rate | 0.90 | 0.58 |
| 21 | Prostate cancer mortality rate | 0.94 | 0.01 |
| 22 | Breast cancer mortality rate | 0.92 | 0.001 |
| 23 | Total cancer mortality rate | 0.88 | 0.01 |
1.“Multiplicative direct effect” show the direct impact of sanctions (by considering the mediator variables). It reflects the percentage change in each indicator during the sanction period. The difference of the reported statistic with 1 indicates the percentage of changes. For example, the average of “household health expenditure (%)” in years with sanctions is 11% less than the years without
2. The “p-value” serves as a crucial metric in determining the significance of the impact of sanctions on the studied indicators, providing insight into whether the observed effects on the index are statistically significant
The results indicate that during the sanctions period, families faced a 15% increase in OOP, meaning they had to allocate more of their income to healthcare. Additionally, household expenditure on food rose by 6%, reflecting inflation and restricted imports, leaving less income for other necessities, i.e., healthcare and education. A 5% increase in mortality due to COPD suggests worsened outcomes for individuals with respiratory conditions, likely due to limited access to essential medical supplies and treatment. The 2% increase in thalassemia mortality highlights challenges in accessing life-saving treatments, leading to higher mortality rates for patients with this condition. Furthermore, a 1% rise in hypertension mortality rate signals poorer management of high blood pressure, maybe due to restricted access to medications and preventive care, resulting in more severe health complications such as heart attacks or strokes.
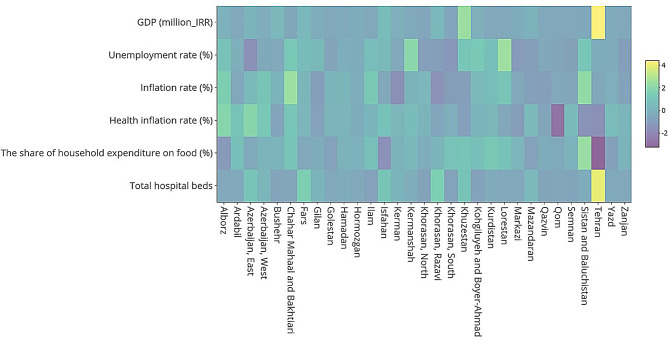
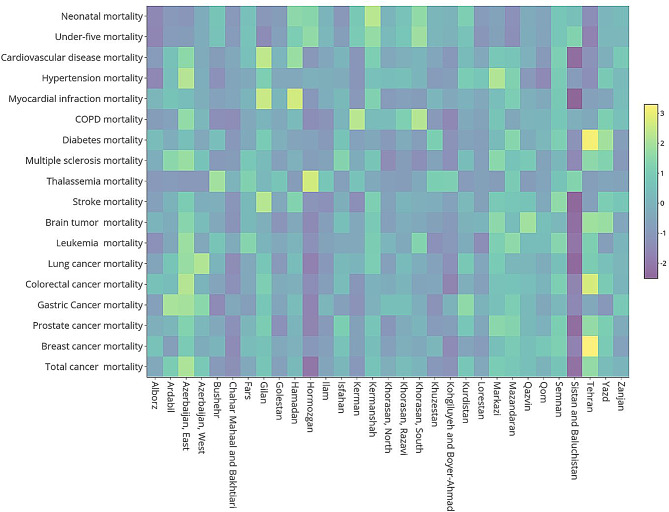
The heat maps in Figs. 5 and 6 illustrate the variation in macroeconomic, healthcare resources, and health outcomes indicators across different provinces during the sanctions period; a greater variation in colors for a given indicator indicates a higher disparity in the mean value of that indicator among different provinces (the homogeneity of colors in each row indicates an equality of the health indicator in the provinces). Indicators such as OOP, household health expenditure, and mortality rates (e.g., COPD and thalassemia) reveal distinct patterns of inequality. For example, the heat map highlights significant disparities in the share of household expenditure on food among provinces, with poorer regions such as Sistan and Baluchestan experiencing higher food expenditures, indicating greater vulnerability to the economic impacts of sanctions. The findings revealed that the level of inequality between provinces was less pronounced in macro-economic and health resources indicators compared to the health outcome indicators.
Fig. 5.
Macroeconomic and healthcare resources indicators among provinces; inequality between provinces according to each indicator
Fig. 6.
Health outcomes indicators among provinces; inequality between provinces according to each indicator
Furthermore, the results highlighted that the most significant differences and inequalities in macro-economic and health resources indicators were observed in the ‘share of household expenditure on food,’ while the least differences were seen in ‘unemployment rate.’ Specifically, the highest share of household expenditure on food was observed in Sistan and Baluchestan, while the lowest was recorded in Tehran. Despite our efforts, we could not find reliable province specific data for the following indicators: current health expenditure (CHE) per capita in purchasing power parity (PPP) intUS$, household expenditure as percentage of current health expenditure (CHE) (%) and, out-of-pocket expenditure as percentage of current health expenditure (CHE) (%) (Fig. 5).
Our findings identified the most significant differences and inequalities among the health system outcome indicators in the cardiovascular disease mortality rate (per 100,000 population), myocardial infarction mortality rate (per 100,000 population), and thalassemia mortality rate (per 100,000 population). There was comparatively less inequality in mortality rates due to various types of cancer across the provinces (no provincial specific data for the MMR available) (Fig. 6).
Qualitative findings
The participants included 31 patients and eight health experts (Table 5). We identified four themes, 17 sub-themes, and 63 codes.
Table 5.
Participants characteristics
| Variables | Statistics | Value | |
|---|---|---|---|
| Patients | Gender | Females (%) | 58 |
| Males (%) | 42 | ||
| Age (years) | Mean (Min-Max) | 36 (12–68) | |
| Type of disease | Diabetes (n) | 6 | |
| Thalassemia (n) | 7 | ||
| Cancer (n) | 5 | ||
| Hemophilia (n) | 4 | ||
| Kidney transplant (n) | 9 | ||
| Policy makers | Age (years) | Mean (Min-Max) | 43 (36–59) |
| Work Experience (years) | Mean (Min-Max) | 8.3 (2–20) | |
| Length of Interview (minutes) | Mean (Min-Max) | 45 (27–65) |
We identified two main themes from patients: “direct effect of sanctions on population health” and “side effects of sanctions on peoples’ lifestyle”. These themes were further divided into four sub-themes presented in Table 6. The primary concern identified among patients was the diminished access and heightened costs of medications and medical interventions. One of a major health challenge reported by the participants was about health expenses as a proportion of total household expenditures; because of that, they had to prioritize other financial obligations over the treatment of chronic diseases or overlook the treatment of chronic diseases.
Table 6.
Themes, sub-themes and codes identified from interviews with patients
| Theme | Sub-theme | Code |
|---|---|---|
| The direct effect of sanctions on population health | Impact of sanctions on availability of medicines and services |
- Medicine shortage and access challenges, especially for orphan drugs - Difficulties in accessing and availability of medical supplies and equipment |
| Impact of sanctions on costs of medicines and services |
- Increased drastic fluctuations in service costs - Increased out-of-pocket payments to access health care and medicines - Medicine shortage following increased prices and impaired access |
|
| Impact of sanctions on quality of medicine and services |
- Replacement of quality medical supplies and equipment with lower-quality material - Obtaining medicines from the black market with questionable quality - Increased counterfeit medical supplies and equipment in the market |
|
| Tendency to prioritize patients within the families |
- Prioritizing comorbidities in favor of treating emergency diseases and ignoring chronic ones - Underemphasizing chronic conditions, due to financial constraints imposed by sanctions, in favor of emergency situations - Prioritizing healthcare needs of multiply ill family members - Re-prioritizing life needs/necessities versus health/disease management needs |
|
| Delayed treatment |
- Ignoring symptoms - Delaying treatment - Treatment complications - Increased treatment cost |
|
| The side effects of sanctions on peoples’ lifestyle (health-related) | Frustration due to inability to improve living conditions |
- Increased living costs - Despair and hopelessness - Increased feelings of instability, especially in financial matters - Uncertainty about the future - Distrust and despondency about the future - Reduced ability to afford and fulfill basic daily necessities, such as food and medical expenses - Reduced ability to afford well-being and cultural activities. |
We identified two main themes from interviews with policy makers: “effect of sanctions on health system” and “impacts of sanctions on infrastructures”. These themes were classified into 10 sub-themes as illustrated in Table 7. Healthcare experts recognized diverse, direct and indirect impacts of sanctions on population health, as well as several negative effects on the healthcare system function. Notably, sanctions were perceived to have contributed to a lack of transparency in major health policies, compromised the quantity and quality of healthcare services, and diminished the motivation of healthcare professionals, particularly specialist physicians. Consequently, challenges emerged in the provision of healthcare services, particularly at the secondary and tertiary levels. Furthermore, sanctions were identified with significant repercussions on general inflation and healthcare-specific inflation, thereby negatively affecting the health and quality of citizens’ life.
Table 7.
Themes, subthemes and codes identified from interviews with policy makers
| Theme | Sub-theme | Code |
|---|---|---|
| The effect of sanctions on health system | Impact of sanctions on health outcomes |
- Reduced quality of life - Increased mortality rates - Increased burden of diseases |
| Impact of sanctions on health system’s governance |
- Inability to define clear future strategies and policies to achieve health improvement due to uncertainties - Inability to utilize legal, supervisory, and policy tools to lead health system functions - Increasing corruption in the healthcare sector as a result of information rents and monopolies created by sanctions - Decreased interpectoral collaborations |
|
| Impact of sanctions on service provision |
- Investors’ reluctance to collaborate with healthcare sector - Weakened healthcare infrastructures - Reduced ratio of specialized human resources to the population preventing the provision of optimal health services - Increased inequality in distribution of hospital resources, especially Intensive Care Unit (ICU) and imaging equipment |
|
| Impact of sanctions on procurement of medicines, medical supplies, and equipment |
- Increased barriers in financial transactions and import procedures for medicines and medical supplies - Reluctance of other countries to sell medical equipment to Iran due to sanctions-imposed consequences - Use of lower quality ingredients in manufacturing generic medicines - Higher prices paid for imported medicines, medical supplies, and equipment, through both imports or domestic production |
|
| Impact of sanctions on healthcare workforce (quality, quantity, and motivation) |
- Reluctance of some medical staff to work within the country - Increased immigration rates out of the country among healthcare experts and staff - Inadequate patient services - Decreased motivation among healthcare staff - Decreased staff concentration due to multiple job commitments |
|
| Impact of sanctions on healthcare system’s financing |
- Increased prices of services and medicines as a result of inflation in the health sector - Increased tariffs of healthcare services - Delayed reimbursements from health insurance organizations to healthcare providers, leading to heightened financial strain on providers - Deterioration of far financing contribution indicators, including increased impoverishment resulting from healthcare costs and the occurrence of catastrophic healthcare expenses. - Increased share of OOP in healthcare costs - Increased informal payments |
|
| The impacts of sanctions on infrastructures (health-related) | Impact of sanctions on economic factors |
- Investments and their management - Financial transactions - Inflation - Increased economic instability |
| Impact of sanctions on political factors |
- Successful implementation of policies and regulations - Management stability - International relations and diplomacy |
|
| Impact of sanctions on social and cultural factors |
- Social capital, happiness, and cooperation - Immigration rate - Social crimes |
|
| Impact of sanctions on education and research |
- Scientific publications - Access to up-to-date scientific resources - Scientific exchange through international seminars and conferences |
The content analysis and quotes are provided in the “supplementary information 2”, also see [25].
Discussion
This study provided an overview of the impact of economic sanctions on health outcome and healthcare system indicators, as well as the perceived experiences of Iranian citizens during 2000–2020.
We identified significant changes in 11 indicators (39.2%) after the change point (Cp > 2009), while four indicators (14.2%) showed a significant increase after Cp (β_02-β_01 > 0). Findings revealed considerable increases in the out-of-pocket expenditure, household expenditure on food, COPD mortality rate, thalassemia mortality rate and hypertension mortality rate, during the study period. The increase in OOP reflects a significant additional financial burden on households. In practical terms, this means that under sanctions, a large number of families had to spend more of their disposable income on healthcare services, which could lead to difficult trade-offs between healthcare and other essential needs such as food, housing, and education. For the average citizen, particularly those in lower-income brackets, this increase in healthcare costs could result in delayed or avoided treatments, worsening health outcomes, and deepening health inequities. The effect is especially severe for patients with chronic illnesses, as continuous medical care becomes more unaffordable, potentially leading to poorer long-term health outcomes and higher mortality rates in vulnerable populations. A 6% rise in household expenditure on food during sanctions reflects the increasing cost of food, likely due to inflation and restricted imports. For the average citizen, this means that a larger portion of their income went towards basic necessities such as food, which might have exacerbated malnutrition and food insecurity, particularly among vulnerable populations, leading to long-term negative health effects, especially for children and the elderly. Increase in the mortality rate due to COPD, Thalassemia and Hypertension during sanctions signals that individuals suffering from these conditions faced worsened outcomes, likely due to restricted access to medication, healthcare services, and medical supplies. The impact of this increase is profound, as it implies that the sanctions contributed to the deterioration of health in those with such diseases, increasing premature deaths, and reducing quality of life, especially for older adults and those in lower socioeconomic groups.
The patterns observed in the heat map align with broader literature suggesting that sanctions exacerbate existing inequalities in healthcare access and economic resilience. Studies have shown that sanctions tend to disproportionately impact lower-income regions, where healthcare infrastructure is already limited [13]. The increased share of household expenditure on food in poorer provinces, coupled with rising out-of-pocket healthcare costs, indicates that sanctions further strained household budgets, forcing difficult trade-offs between healthcare, nutrition, and other necessities. Practically, these interactions highlight the need for targeted policy interventions to mitigate the compounded effects of sanctions on vulnerable populations. The increased inequality across provinces, as visualized in the heat map, suggests that regional disparities in healthcare access are likely to worsen under prolonged sanctions, with long-term health consequences, particularly for chronic disease management.
Despite identifying a significant increasing trend in some cancer mortality rates, i.e. stroke mortality rate and leukemia mortality rate, we did not find significant changes in such indicators. Our qualitative findings explored a wide range of negative effects of sanctions on citizens’ ability to access and receive quality medication and essential treatment interventions. Due to imposing financial hardship, sanctions led to catastrophic healthcare expenses, thereby deteriorating health indicators even further. Moreover, by shrinking healthcare resources, i.e., human and financial resources for health, medical equipment and medications, available healthcare services, as well as targeting the economic, social, and political infrastructures related to health, sanctions may affect the country’s healthcare system.
Despite our expectation, our finding did not present significant changes in the health outcome indicators. This might be partially related to the study period and type of selected indicators. For instance, health outcome indicators are influenced by environmental changes that occur over an extended period and have a lag time, therefore their effects may not be immediately apparent. Our research illustrated that investigating the effects of multidimensional and complex issues such as sanctions might need extended time periods. We propose considering longer time frames to allow an effective lag time of these indicators to elapse. Furthermore, the severity and intensity of sanctions were fluctuating, and potential instability means that the resulting complications may not have had a prolonged duration, preventing their effects from becoming significant when examined at a national level. In particular, indicators such as cancer mortality rates have low treatability and survival rate. Let al.one, local production of numerous medicines and medical equipment might have reduced the consequences of restricted imports. In addition, the extensive PHC network in practice over four decades, amalgamated with major healthcare reforms, i.e., the Family Physician and Universal Rural Health Insurance in 2004, and Health Transformation Plan to achive UHC in 2014, and domestic production of generic medicine have contributed to significant improvements of various health indicators, i.e., maternal and child mortality rates, control of chronic diseases (such as hypertension and diabetes), and access to healthcare services [10, 13, 26].
In line with previous studies, our qualitative findings revealed difficult international financial transactions that have hindered the importation of a significant number of necessary raw materials for medicine production. It was perceived that medicines were produced with lower quality, which might have led to ineffective and prolonged treatment periods, especially for complicated and chronic diseases, ever increasing cost, particularly for orphan drugs, scarcity of imported medicines, supply shortages of vaccines and other essential medical equipment, intensified patients’ dissatisfaction, and ultimately, increased mortality rates (notably among patients suffering from asthma, thalassemia, hemophilia, chronic diseases, blood disorders, multiple sclerosis, HIV/AIDS, and cancers) [3, 21, 27–29].
One study that examined the health-related effects of sanctions across four dimensions (health indicators, food security, medicine and treatment, and air pollution) demonstrated a relatively strong performance of Iran in health indicators for infants, children, and mothers compared to other middle-income countries. Improving medical care during pregnancy, childbirth, and postnatal care within the PHC platform, as well as the percentage of birth attendants in healthcare facilities, might be the main reasons, we envisage, behind infant mortality reduction in Iran [30–32]. We echo evidence form another study that in the absence of sanctions, the trends of infant and maternal mortality reduction might have been even more upward [32].
A comprehensive national and subnational breakdown of the burden of diseases, injuries, and risk factors presented the most substantial negative changes in mortality caused by NCDs - neoplasms in particular - associated with sanctions in Iran, with degrees of inter-provincial inequalities [10]. We found two out of 10 neoplasm mortality rate indicators, i.e. leukemia and prostate cancer showing an increasing trend after the imposition of sanctions, which were unequally distributed at the sub-national level.
There is an overwhelming evidence about the negative impact of sanctions on public food security, one of the main determinants of health [21]. The secondary effects of sanctions on banks, shipping, and insurance further hinder the import of food, raw materials and necessary machinery for food production. Consequently, the production index of certain food products was significantly impaired, with a cumulative effect exacerbating food insecurity in Iran [33]. Our findings revealed a correlation between sanctions and the share of household expenditure on food. This indicates that families are spending a higher percentage of their income on food products or, due to increased prices, are avoiding the purchase of certain products (such as animal-based proteins and dairy), which might result in reduced overall food security.
Studies in Iraq, Cuba, Libya, Venezuela, Iran and recently Russia consistently demonstrate the adverse effects of sanctions on access to public healthcare services [6, 7]. In Cuba, sanctions were associated with a marked escalation in malnutrition, especially among children. There was also an increase in mortality due to water pollution and increased vulnerability to other toxins. Additionally, sanctions caused severe increases in anemia among expecting mothers, typhoid fever, viral hepatitis, scabies, childhood diseases, and hospital infections [33]. The United Nations’ sanctions against former Yugoslavia, Serbia, and Montenegro (1992–2001) increased the incidence of tuberculosis, measles, and typhoid fever, along with higher hospital mortality rates and challenges in procuring food and basic commodities [33]. Similarly, sanctions negatively affected people’s health in North Korea and Venezuela [28, 34]. Although comparing the experiences of different countries is challenging and limited due to contextual variations and heterogeneity, such comparisons reveal common health trends despite differing geopolitical, economic, and social backgrounds. Sanctions can influence citizens’ health both directly and indirectly through various mechanisms [2, 9, 18, 27, 28, 35–40] The bureaucratic and economic barriers imposed by sanctions are likely to elevate challenges in production, import, and distribution of medicines, food, and related goods. Additionally, they result in elevated fuel costs, price surges for essential goods, reduced access to healthcare services and clean water [9, 33]. Moreover, factors such as insurance restrictions, reliance on self-insurance, restricted transportation and port access, decreased welfare, and disruptions in social stability and education, all may have deteriorating effects on public health. Reductions in welfare and disruption of social stability and education play fundamental roles as well. Worse still, shrunk financial resources and reduced human resources for health due to migration of workforce have led to less competent healthcare services, and the academic losses to less competent research activities. The impact of sanctions often intertwines with factors such as internal unrest, war, infrastructure collapse, breakdown of the rule of law, refugees’ movements, and environmental degradation, all of which can substantially affect the health status of the population. In addition, the impact of global challenges on the health of populations and the performance of the health care systems, such as migration movements, climate change effects and pandemics will have to be considered as competing risks, as well as demographic and epidemiologic transitions going on in respective countries [8, 13, 33, 41, 42].
Rigor and limitation of study
To the best of our knowledge, this is one of the few studies with quantitative measurement of the impact of sanctions on health indicators. Measuring the trend of 28 indicators over a 20-year period at both national and provincial levels, identification of the impact of sanctions on health from the perspectives of both the general public and policymakers and an innovative study design combining quantitative and qualitative components are some strengths of this study. Nevertheless, measuring the impact of sanctions on health indicators may require a longer period of observation and measurement. Should this study had primarily focused on the intermediate and process indicators instead of health outcome indicators, it could have provided a clearer illustration of the sanctions’ impact on the country’s population health and healthcare system.
This study had to deal with an intrinsic very high level of complexity due to the various dimensions and factors involved that affect health in addition to the specific pathways of sanctions. For instance, independent from sanctions, Iran has undergone several health policy reforms during the 20 years observation time of the study, which may have severely affected population health and the functioning of the health care system. In addition, similar to other LMICs, epidemiologic transition happening in Iran is associated with major changes, making it difficult to formally distinguish and dissect all these factors from another. Let alone, these factors and dimensions are not independent from each other and are strongly interconnected. Hence, exact identification of the role of international sanctions on health in a country like Iran (and others) remains hard. Also, the methodological constraints inherent in social research, rooted in the intricate fabric of society, pose significant challenges. Of paramount importance is the inherent limitation associated with the inability to fully control all confounding variables, thereby jeopardizing the transparency and validity of the observed effects pertaining to the variable under scrutiny. Unlike the controlled environment of experimental research, the dynamic and multifaceted nature of social studies renders it arduous to account for and manipulate all potential influencing factors, impeding the establishment of unequivocal causal relationships.
For indicators showing a decreasing trend, such as maternal and under-5 mortality rates, one can speculate that these rates might have declined more rapidly in the absence of sanctions.
Mortality rates chosen for investigation with respect to various types of cancers are known for potential lower survival rates and low treatability and might therefore have a low susceptibility to therapeutic interventions. Consequently, access to effective drugs and treatments may only slightly increase survival times, which could explain why mortality rates were not substantially affected by sanctions.
One potential limitation of the JPR model is its assumption of linearity within each segment. Nevertheless, we tested the robustness of our findings by conducting a sensitivity analysis with alternative change points. The consistency of the results across different points reinforces the significance of the detected changes around 2009, likely attributable to the sanctions. This strengthens the validity of our model and conclusions.
The credible intervals and p-values were computed using a Bayesian framework, with the credible intervals reflecting the uncertainty around the estimated coefficients. To further ensure the robustness of our model, we performed a residual analysis and used goodness-of-fit measures, such as AIC and BIC. These diagnostics indicated that the model provided a good fit for the data, with no significant patterns detected in residuals that would suggest model misfit. The consistency of these diagnostics strengthens the confidence in our findings.
The reliability of our dataset, which spans multiple indicators and dimensions, was supported by the use of sound statistical methods. The combination of JPR and GAMM allowed us to manage the complexity of the data while ensuring that the interactions between variables were accurately modeled. These approaches helped mitigate potential biases and provided a reliable framework for assessing the effects of sanctions on macroeconomic conditions and health outcomes.
While our models, including the JPR and GAMM, were designed to analyze the impact of sanctions on economic and health indicators, they face certain limitations. Attributing changes in health outcomes solely to sanctions is challenging, as other factors like healthcare reforms, regional conflicts, and global economic crises may have also played a role. Additionally, unobserved confounders, such as variations in healthcare infrastructure and population behaviors, could introduce bias. Our models, while effective at capturing complex relationships, may not fully account for interactions over time or external shocks (e.g. economic crises, potential impact of climate change) and delayed effects of sanctions. The assumption of linearity in the JPR model may overlook non-linear or lagged responses, suggesting that alternative approaches like time-series models could offer further insights.
Conclusions
This study aimed to investigate the impact of sanctions on key health indicators that reflect the health status of people in Iran. Our results demonstrate that sanctions have led to increased healthcare costs, worsened health outcomes for patients with chronic diseases, and significant regional inequalities in healthcare access. Furthermore, the qualitative component revealed widespread dissatisfaction among patients and healthcare providers, particularly regarding access to essential medicines and the rising financial burden on households. These findings underscore the need for targeted interventions to mitigate the detrimental effects of sanctions on public health. These showed that sanctions could, both directly and indirectly, impact the health of people through imposed sanction consequences, i.e., raised inflation, reduced production, currency devaluation, hard financial transactions with other countries, changes in political behavior, and diplomatic relations between countries.
Although sanctions alone are not the sole immediate cause of disease burdens in the short term, their chronic and long-term effects may be more significant than their acute and immediate impact. Our research revealed that accurately measuring the effects of sanctions on public health, our primary research goal, is a complex undertaking. Sanctions impact both the physical and mental well-being of individuals in various ways. Factors such as declining economic growth leading to reduced average income levels, which can push individuals below the poverty line, deteriorating education quality and quantity, and the increase in social issues and socio-economic disparities, all contribute to a decline in overall health and the widening of health inequalities.
Our study demonstrated that mortality indicators, particularly during the period of sanctions, exhibited an increasing trend. However, we could not demonstrate robust evidence for a significant correlation between these trends and the sanctions imposed on Iran. Nonetheless, our qualitative findings provided reliable support for substantial impact of sanctions on the challenges faced by patients and their families, which underscores the greater need for attention and action from the international communities and human rights organizations. It seems that, considering factors such as Iran’s economic resilience, robust infrastructure and economic resources, and the healthcare network that has bolstered health indicators and improved access to primary healthcare services, it is evident that the healthcare system’s resilience and public health standards are higher in comparison to numerous other countries in the face of sanctions. This resilience will persist as long as the impacts and limitations imposed by sanctions do not impede the country’s capacity to sustain its economic infrastructure.
We advocate the implementation of policies such as promoting prescription of generic drugs, development of clinical guidelines, comprehensive education of patients on the rationale use of medicines, establishment of sustainable financing mechanisms for the supply of medicines and medical equipment, and robust financial protection for vulnerable patients to minimize the impact of sanctions on public health. This can be achieved through improved advocacy, utilizing scientific and empirical evidence, and adopting a comprehensive and intersectoral approach to mitigate the adverse effects of sanctions on population health. International organizations should also have a role in ensuring that sanctions are executed in a manner that does not endanger the well-being of the general population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We gratefully acknowledge the financial support provided by NIMAD for Research in Fundamental Sciences for this research project. Additionally, we would like to express our appreciation to the Ministry of Health and the Statistical Center of Iran for their valuable collaboration in supplying the essential data for this study.
Abbreviations
- OOP
Out-of-Pocket payment
- COPD
Chronic Obstructive Pulmonary Disease
- US
United States
- JPOA
Joint Comprehensive Plan of Action
- OFAC
Office of Foreign Assets Control
- PHC
Primary HealthCare
- UHC
Universal Health Coverage
- JPR
Join Point Regression
- GAMM
General Additive Mixed Effect Model
- IHIO
Iran’s Health Insurance Organization
- NMR
Neonatal Mortality Rate
- MIMR
Myocardial Infarction Mortality Rate
- MSMR
Multiple Sclerosis Mortality Rate
- SMR
Stroke Mortality Rate
- LMR
Leukemia Mortality Rate
- PCMR
Prostate Cancer Mortality Rate
- CHE
Current Health Expenditure
- PPP
Per Capita in Purchasing Power Parity
- HIV
Human Immunodeficiency Virus
- AIDS
Acquired Immunodeficiency Syndrome
Author contributions
AO and AT conceived the research. AT, AO, AK and RM contributed to the study design. EM, MaM, MMK, HM and FE participated in data collection. MK, MoM, EM and MaM analyzed quantitative data. MMK, HM, FE analyzed the qualitative data. AO, AT, AK, RM and MK contributed to data analysis and interpretation. EM drafted the first version of the manuscript. All authors contributed to the intellectual development of the manuscript. EM, AK and RM are co-first authors of this article. AO and AT are both guarantors as corresponding authors.
Funding
This study received financial support from the National Institute for Medical Research Development (NIMAD) in Iran.
Data availability
The data used in this study will be made available upon request after publication and upon correspondence with the researchers. We are committed to ensuring that the data remains accessible to facilitate further research and collaboration in the field.
Declarations
Ethics approval and consent to participate
The ethics approval ID is: IR.NIMAD.REC.1399.111.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Efat Mohamadi, Alexander Kraemer and Reza Majdzadeh are co-first authors.
Contributor Information
Alireza Olyaeemanesh, Email: arolyaee@gmail.com.
Amirhossein Takian, Email: takian@tums.ac.ir.
References
- 1.Katzman K. Iran sanctions. Congressional Research Service Washington, DC; 2011.
- 2.Pakdaman M, Geravandi S, Askari R, Askarishahi M, Afzali HR. The effect of macroeconomic indicators on health-care expenditure in Iran. J Educ Health Promotion. 2019;8. [DOI] [PMC free article] [PubMed]
- 3.Setayesh S, Mackey TK. Addressing the impact of economic sanctions on Iranian drug shortages in the joint comprehensive plan of action: promoting access to medicines and health diplomacy. Globalization Health. 2016;12(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massoumi RL, Koduri S. Adverse effects of political sanctions on the health care system in Iran. J Global Health. 2015;5(2). [DOI] [PMC free article] [PubMed]
- 5.Mohammadi D. US-led economic sanctions strangle Iran’s drug supply. Lancet. 2013;381(9863):279. [DOI] [PubMed] [Google Scholar]
- 6.Namazi S. Sanctions and medical supply shortages in Iran. Viewpoints. 2013;20:1–9. [Google Scholar]
- 7.Butler D. Iran hit by drug shortage: sanctions cause increasing shortfall in medicines and vaccines. Nature. 2013;504(7478):15–7. [DOI] [PubMed] [Google Scholar]
- 8.Golzari S, Ghabili K, Khanli HM, Tizro P, Rikhtegar R. Access to cancer medicine in Iran. Chemotherapy. 2013;3:5. [DOI] [PubMed] [Google Scholar]
- 9.Hashemi-Meshkini A. Making the public health and industrial objectives balanced; the big challenge of Iran’s food and drug organization. Iran J Public Health. 2014;43(5):693. [PMC free article] [PubMed] [Google Scholar]
- 10.Farzadfar F, Naghavi M, Sepanlou SG, Moghaddam SS, Dangel WJ, Weaver ND, et al. Health system performance in Iran: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2022;399(10335):1625–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Arch Iran Med. 2014;17(5):0. [PubMed] [Google Scholar]
- 12.Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: a review article. Iran J Public Health. 2018;47(3):309. [PMC free article] [PubMed] [Google Scholar]
- 13.Sajadi HS, Majdzadeh R. Health system to response to economic sanctions: global evidence and lesson learned from Iran. Globalization Health. 2022;18(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Danaei G, Harirchi I, Sajadi HS, Yahyaei F, Majdzadeh R. The harsh effects of sanctions on Iranian health. Lancet. 2019;394(10197):468–9. [DOI] [PubMed] [Google Scholar]
- 15.Gorji A. Sanctions against Iran: the impact on health services. 2014. [PMC free article] [PubMed]
- 16.Mohamadi E, Takian A, Olyaeemanesh A, Rashidian A, Hassanzadeh A, Razavi M, et al. Health insurance benefit package in Iran: a qualitative policy process analysis. BMC Health Serv Res. 2020;20(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duttagupta S, Yampolsky D, Chowdhury C. Economic sanctions and market access for pharmaceuticals: case studies with Russia, Cuba and Iran. Value Health. 2015;18(7):A569. [Google Scholar]
- 18.Ghalibafian M, Hemmati S, Bouffet E. The silent victims of the US embargo against Iran. Lancet Oncol. 2018;19(11):e580. [DOI] [PubMed] [Google Scholar]
- 19.Asgardoon MH, Hosein M. Adverse impacts of imposing international economic sanctions on health. Arch Iran Med. 2022;25(3):182–90. [DOI] [PubMed] [Google Scholar]
- 20.Hajizadeh M, Nghiem HS. Hospital care in Iran: an examination of national health system performance. Int J Healthc Manag. 2013;6(3):201–10. [Google Scholar]
- 21.Sajadi HS, Yahyaei F, Ehsani-Chimeh E, Majdzadeh R. The human cost of economic sanctions and strategies for building health system resilience: a scoping review of studies in Iran. Int J Health Plann Manag. 2023. [DOI] [PubMed]
- 22.Pintor MP, Suhrcke M, Hamelmann C. The impact of economic sanctions on health and health systems in low-income and middle-income countries: a systematic review and narrative synthesis. BMJ Global Health. 2023;8(2):e010968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masoodi M, Rahimzadeh M. Measuring access to urban health services using Geographical Information System (GIS): a case study of health service management in Bandar Abbas. Iran Int J Health Policy Manage. 2015;4(7):439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebrahimi F, Kraemer A, Mohamadi E, Kiani MM, Majdzadeh R, Mohamadzade M, et al. Study protocol for investigating the Impact of Economic Sanctions on Public Health and Healthcare Systems in Iran: A National and sub-national analysis from 2000 to 2020. Health Scope. 2024;13(3):e134234. [Google Scholar]
- 25.Kiani MM, Mostafavi H, Ebrahimi F, Majdzadeh R, Mohamadi E, Kraemer A, et al. The experiences and perceptions of people with chronic and rare diseases during political-economic sanctions in Iran: a qualitative study. BMC Health Serv Res. 2024;24(1):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doshmangir L, Bazyar M, Majdzadeh R, Takian A. So near, so far: four decades of health policy reforms in Iran, achievements and challenges. Arch Iran Med. 2019;22(10):592–605. [PubMed] [Google Scholar]
- 27.Claborn DM. A narrative review of the role of economic crisis on health and healthcare infrastructure in three disparate national environments. Int J Environ Res Public Health. 2020;17(4):1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giotakos O. Financial crisis and mental health. Psychiatrike = Psychiatriki. 2010;21(3):195–204. [PubMed] [Google Scholar]
- 29.Ghiasvand H, Mohamadi E, Olyaeemanesh A, Kiani MM, Armoon B, Takian A. Health equity in Iran: a systematic review. Med J Islamic Repub Iran. 2021;35:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehryar AH, Ahmad-Nia S, Kazemipour S. Reproductive health in Iran: pragmatic achievements, unmet needs, and ethical challenges in a theocratic system. Stud Fam Plann. 2007;38(4):352–61. [DOI] [PubMed] [Google Scholar]
- 31.Damghanian M, Shariati M, Mirzaiinajmabadi K, Yunesian M, Emamian MH. Socioeconomic inequality and its determinants regarding infant mortality in Iran. Iran Red Crescent Med J. 2014;16(6). [DOI] [PMC free article] [PubMed]
- 32.Khosravi A, Mohamadi E, Sheidaei A, Shafiee G, Heshmat R, Olyaeemanesh A, et al. Child mortality inequalities and socioeconomic determinants of health in Iran, 2016–2018. J Public Health Policy. 2023;44(4):535–50. [DOI] [PubMed] [Google Scholar]
- 33.Moret ES. Humanitarian impacts of economic sanctions on Iran and Syria. Eur Secur. 2015;24(1):120–40. [Google Scholar]
- 34.musavi s, dolatabadi Ab. The impact of economic sanctions on political and economic rights and the health of North Korean citizens. World Politics: Qualitative J. 2022;10(1):221–54. [Google Scholar]
- 35.Durán IP. Health care inequality in Spain after the economic crisis: the health delivery system and the public private sector mix. Global Social Welf. 2016;3(3):179–91. [Google Scholar]
- 36.Nayeri K, López-Pardo CM. Economic crisis and access to care: Cuba’s health care system since the collapse of the Soviet Union. Int J Health Serv. 2005;35(4):797–816. [DOI] [PubMed] [Google Scholar]
- 37.Kokabisaghi F. Assessment of the effects of economic sanctions on iranians’ right to health by using human rights impact assessment tool: a systematic review. Int J Health Policy Manage. 2018;7(5):374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mehrnaz K, Vida V, Abbas K, Abdol Majid C. Impact of economic sanctions on access to noncommunicable diseases medicines in the Islamic Republic of Iran. 2018. [PubMed]
- 39.Baradaran-Seyed Z, Majdzadeh R. Economic sanctions strangle iranians’ health, not just drug supply. Lancet. 2013;381(9878):1626. [DOI] [PubMed] [Google Scholar]
- 40.ROSHAN NA, Mehrbod S. The impacts of economic sanctions on sustainable development: focusing on labor. Cumhuriyet Üniversitesi Fen Edebiyat Fakültesi Fen Bilimleri Dergisi. 2015;36(3):3458–76. [Google Scholar]
- 41.CIRAKLI U, YILDIRIM HH. The impacts of economic crisis on the public health in Turkey: an ARDL bounds testing approach. Hacettepe Sağlık İdaresi Dergisi. 2019;22(2):259–80. [Google Scholar]
- 42.Espinosa L, Mirinaviciute G. Health crisis in Venezuela: status of communicable diseases and implications for the European Union and European Economic Area, May 2019. Eurosurveillance. 2019;24(22):1900308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study will be made available upon request after publication and upon correspondence with the researchers. We are committed to ensuring that the data remains accessible to facilitate further research and collaboration in the field.