Abstract
Abstract
Objective
We evaluate change in low back pain (LBP) intensity and interference as the mechanism by which chiropractic care affects other biopsychosocial factors in US active-duty military members.
Design
We conducted secondary, exploratory mediation analysis of pragmatic, multisite, clinical trial (NCT01692275) post results using natural effect modeling. Mediators were the 6-week values of Patient-Reported Outcomes Measurement Information System (PROMIS)-29 pain interference and intensity. Outcomes were 12-week values of other PROMIS-29 biopsychosocial subdomains. Models evaluated overall and individual factor contribution and were adjusted for baseline age, sex, LBP duration, LBP intensity and mediator and outcome values.
Setting
Three US military treatment facilities.
Participants
750 US active-duty military members with LBP.
Interventions
Trial participants received 6 weeks of treatment with chiropractic care plus usual medical care or usual medical care alone.
Results
In multiple mediator models, pain interference and pain intensity explained much of the effect of chiropractic care on physical function (proportion mediated=0.77, 95% CI 0.43 to 2.0), fatigue (0.62, 95% CI 0.30 to 1.0), sleep disturbance (0.49, 95% CI 0.31 to 1.5) and social roles (0.81, 95% CI 0.50 to 2.0). Mental health was not evaluable due to the low prevalence of symptoms reported. The combined models of pain interference and pain intensity did not have a higher proportion mediated than the individual pain intensity models except for fatigue outcome models.
Conclusion
Pain intensity appeared to be the mechanism by which much of the change in biopsychosocial factors occurred and should be considered a key clinical indicator for improvement in biopsychosocial health when chiropractic care is added to usual medical care for US active-duty military members.
Keywords: COMPLEMENTARY MEDICINE, PAIN MANAGEMENT, EPIDEMIOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Our use of clinical trial data addresses bias due to confounding of treatment–mediator relationship and differences between patients who choose complementary health approaches and those who do not.
Our sensitivity analysis indicates that our results are not likely to be explained by confounding factors that are unaccounted for.
We were unable to assess patient beliefs due to lack of measurement in the parent trial.
We were unable to assess mental health outcomes due to low prevalence of reporting symptoms.
Transportability outside of US military personnel may be limited.
Introduction
Whole-person healthcare has been hypothesised to affect biological, social, behavioural and environmental health factors and to best addressed with the use of integrative healthcare approaches that include both conventional treatment and complementary health approaches.1 Complementary health approaches include a wide array of therapies categorised as nutritional, psychological, physical or combinations of these categories.1 One of the most commonly used complementary health approaches in the USA is chiropractic care.2
Chiropractic care is a multimodal treatment including, but not limited to, manual therapy, therapeutic exercise, patient education, lifestyle factor recommendations and self-care recommendations.3,5 These interventions target patient beliefs, psychosocial function and physical pain,4 consistent with the biopsychosocial model.6 Mechanistic research of manual therapy has previously demonstrated effects on physical processes such as joint stiffness,7 8 temporal summation9 10 and muscle activity,11,13 which are associated with changes in pain. Contemporary models of manual therapy mechanisms include a wide range of physical processes along with non-specific and psychological effects.14
The mechanisms of whole-health treatment approaches targeting biopsychosocial health are not as well understood as the specific biological mechanisms of manual therapies. The biopsychosocial model itself has been scrutinised for vagueness in its lack of classifying components as causally related,15 which is necessary to understand how interventions affect biopsychosocial health. Though not without its drawbacks, a starting point for understanding causal components of the biopsychosocial model is to use a reductionist approach to evaluate how changes in pain lead to changes in subsequent physical, psychological and social health.15 The approach of evaluating effects on pain as the mechanism by which health improves due to chiropractic care is supported by patients seeking chiropractic care to specifically address their back and neck pain,16 the most common interventions delivered by chiropractors being recommended in clinical practice guidelines for pain,17 and pain being a common target of chiropractic care.3
Mediation analysis is an approach that can be used to evaluate the mechanism of treatment approaches.18 Mediation analysis evaluates differences in an outcome associated with exposure/treatment occurring through intermediate stages, or mediator variables.18 This type of analysis has been performed to evaluate mechanisms of numerous pain interventions, including tai chi,19 yoga20 21 and physical therapy.21,23 Important mechanisms of these treatments include physical factors such as sleep and exercise,20 and patient beliefs such as self-efficacy,20 catastrophising19 22 and patient expectation.23
Our previous exploratory analysis indicated that factors such as physical function, fatigue, sleep disturbance and social activity were moderate mediators of the effect of chiropractic care on pain interference and to a small degree on pain intensity.24 It remains to be determined if chiropractic care affects whole health factors including physical, mental and social health through its effect on pain, or if these changes occur more directly. The aim of this exploratory study is to evaluate changes in pain as the process by which chiropractic care affects biopsychosocial outcomes. Our primary research question was “Do pain interference and pain intensity mediate the effect of chiropractic care on physical function, fatigue, sleep disturbance, anxiety, depression, and satisfaction with social roles for US active-duty military with LBP?”
Methods
We used A Guideline for Reporting Mediation Analyses guidance,25 which is based on the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) framework,26 to enhance quality and transparency of reporting in this manuscript.
Study design and data source
This is a secondary, exploratory analysis of a deidentified dataset produced from a pragmatic, multisite, clinical trial evaluating usual medical care plus chiropractic care versus usual medical care alone for US active-duty military members with low back pain (LBP).27 The trial was preregistered on clinical trials.gov (NCT01692275), IRB approved and all participants provided written consent. A deidentified dataset was used for these analyses. The analysis plan for this exploratory analysis was not published or registered but was developed before analysis.
The parent trial resulted in greater improvement for US active duty military when chiropractic care was added to usual medical care for the primary outcomes of LBP intensity and disability28 and secondary outcomes of satisfaction with care, perceived improvement28 and Patient-Reported Outcomes Measurement Information System (PROMIS)-29 domains.29 The trial consisted of 6 weeks of treatment and up to 12 visits with a study chiropractor. Because the parent trial was a pragmatic clinical trial, care was delivered as usual rather than prescribed by trial procedures to improve the applicability and generalisability of the study findings. Chiropractic care subcomponents delivered during the trial were generally consistent with what is reported on average in current chiropractic analysis surveys.3 A more thorough description of specific treatments provided is published elsewhere.5 Participants were not prohibited from seeking additional treatment from other providers at any time.
Participants
Trial participants were recruited from three US military medical facilities: Walter Reed in Bethesda, Maryland, Naval Medical Center San Diego in San Diego, California, and Naval Hospital Pensacola in Pensacola, Florida, beginning on 28 September 2012. Recruitment occurred via referrals from medical physicians, study chiropractic clinicians and participant self-referral based on study recruitment flyers. Last participant follow-up occurred 12 weeks after enrolment and was concluded on 13 February 2016.
Participants were active-duty military members between the ages of 18 and 50 years old seeking treatment in the military treatment facilities for musculoskeletal LBP. Potential participants were excluded if they had a condition for which spinal manipulative therapy, the signature intervention associated with chiropractic care, was contraindicated, radiculopathy that required diagnostic testing or surgery, a recent spine fracture or surgery, or a post-traumatic stress disorder diagnosis.
Sample size
The trial was powered for each site to detect between-group differences of 1.2 points in pain intensity and 2.4 points on the Roland-Morris Disability questionnaire.28 This resulted in a sample size of 125 participants per arm at each site, totaling 750 participants. This mediation analysis was not planned at the time the trial was conducted; therefore, an a priori powered sample size was not possible, making it possible that our analysis would be underpowered.
Effects of interest
For these analyses, the total effect is the total difference in effect between treatment arms on physical function, fatigue, sleep disturbance, anxiety, depression and satisfaction with participation in social roles. The total natural direct and total natural indirect effects are subcomponents of the total effect. The total natural direct effect is the difference in effect on outcomes between treatment arms that did not occur through mediators under evaluation, but rather directly or through unmeasured mediators. The total natural indirect effect is the difference in effect on outcomes between treatment arms that occurred through effects on pain interference and/or pain intensity. The proportion mediated is the total natural indirect effect divided by the total effect.
Measurement
Intervention/exposure
We followed the intention-to-treat principle by defining exposure in our models as assignment to intervention arm (usual medical care plus chiropractic care or usual medical care alone). Ninety-three per cent of participants in the arm allocated to receive chiropractic care had a visit with a study chiropractor. Seventy-one per cent in the chiropractic care arm and 73% of those in the usual medical care alone arm had at least one visit with a medical provider in the 6-week treatment period.
Patient-Reported Outcomes Measurement Information System30
Participant health was assessed using the PROMIS-29 profile V.1.0 at baseline, 6 weeks and 12 weeks. The PROMIS-29 profile consists of 29 questions. The profile assesses physical health with the domains of pain intensity, pain interference, physical function, fatigue and sleep; mental health with the domains of anxiety and depression; and social health with the domain of satisfaction with participation in social roles.31 Pain intensity is assessed with a single question, while each of the other domains consists of four questions. Participant responses are used to generate T-scores for each domain. Domains are scaled such that a T-score of 50 corresponds to the general population average for that domain. Participants with scores higher than 50 have more of the measure than the population average, with one SD equal to a 10-point difference from 50.31 To improve the ease of interpretation and decrease conflicting positive and negative estimates which can negatively impact the estimation of proportion mediated,18 we transformed physical function and satisfaction with participation in social roles T-scores in our mediation analyses. These were transformed by taking 100-T-score to make a higher T-score an indicator of poorer health across all of the PROMIS-29 domains.
Outcomes, mediators and confounding
The 12-week values of PROMIS-29 physical function, fatigue, sleep disturbance, anxiety, depression and satisfaction with participation in social roles were the outcomes for the models. Online supplemental table S1 of the supplemental appendix contains a description of the measurement of the outcomes and select baseline covariates. We evaluated the 6-week values of PROMIS-29 pain interference and pain intensity as mediators in our models. We considered the baseline values of the mediators and outcomes as causes of confounding of the mediator–outcome relationship and the baseline factors of sex, age, LBP duration and pain intensity which were used in adaptive allocation to account for causal factors of assignment to exposure.
Causal assumptions
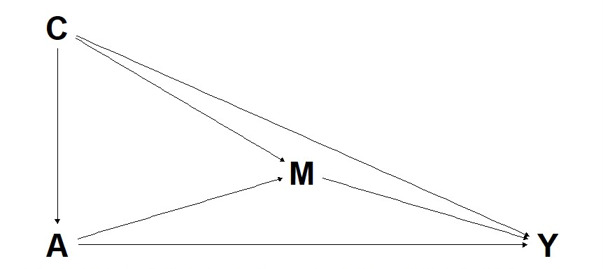
Figure 1 graphically displays the causal model for these analyses. The assumptions are that some of the difference in effect of usual medical care plus chiropractic care and usual medical care alone on biopsychosocial factors occur through the mediators of pain interference and pain intensity. It is also assumed that mediator–outcome confounding is accounted for by adjusting for the baseline values of the PROMIS-29 measures considered in these analyses.
Figure 1. Directed acyclic graph displaying the causal assumptions of models examining the mediation of the effect of treatment on biopsychosocial health factors. A: treatment group; M: mediators; Y: outcome; C: confounding factors.
Statistical methods
Descriptive statistics were tabulated and reported by treatment group. We conducted our mediation and sensitivity analyses using R statistical software (V.4.2.2)32 and the CMAverse package.33 We used the natural effect modelling approach34 and assumed that assignment to treatment arm did not cause confounding of the association between mediator and outcome.
We conducted natural effect multiple mediator models for each outcome with the 6-week PROMIS measures of pain interference and pain intensity as mediators. The models were adjusted for confounding by baseline values of the mediators and outcomes. We also adjusted models for the baseline covariates of self-reported sex, age, and LBP duration.
Exposure–mediator interaction terms were assessed35 and included if they changed total natural indirect and total natural direct effect estimates or improved model fit.18 We used direct counterfactual imputation as described by Vansteelandt et al36 to account for missing data. We used multiple imputation by chained equations with 25 imputations and the CMAverse default of five iterations to impute missing mediator and outcome values and 1000 bootstrap samples to generate bias-corrected standard errors and 95% CIs. We calculated total effect, total natural indirect effect and total natural direct effect on the difference scale. In this analysis, the difference scale indicates the difference in effect between usual medical care alone versus usual medical care plus chiropractic care, with negative values favouring the usual medical care plus chiropractic care arm. In addition to these effects, we calculated and reported the proportion mediated.
The estimation of individual mediator effects is limited by the counterfactual framework of multiple mediator models such as natural effect models.37 To better understand the effect of pain interference and pain intensity individually, we compared single mediator natural effect models with the multiple mediator model for each outcome. Individual mediator models may have inflated estimates compared with multiple mediator models which account for correlation between mediators.18 The comparison of single mediator models to the multiple mediator model shows if the mediation effect is better explained with multiple mediators or if a single mediator may be sufficient as a mechanism.18
Sensitivity analyses
We evaluated the effect of missing data by repeating the multiple-mediator models using complete case analysis and the potential effect of unmeasured confounding by calculating E-values.38
Patient and public involvement
None.
Results
Participants
All participants had LBP at baseline with approximately half of the participants having chronic LBP (3 months or greater duration) and half experiencing acute LBP. This sample of US active-duty military members had a mean of 31 years of age with females making up 23%. Table 1 displays additional baseline characteristics of participants included in this study. Data were more complete for the 6-week measures than the 12-week measures but were not differentially reported by treatment arm. Data completeness is described in greater detail in online supplemental table S2 of the supplemental appendix.
Table 1. Baseline characteristics of participants allocated to usual medical care plus chiropractic care versus usual medical care alone (n=750).
| Variable | UMC (n=375) | UMC+CC (n=375) |
| Age, years, mean (SD) | 30.8 (8.8) | 30.9 (8.7) |
| Sex, n (%) | ||
| Male | 287 (76.5) | 288 (76.8) |
| Female | 88 (23.5) | 87 (23.2) |
| Race, n (%) | ||
| White | 252 (67.2) | 255 (68.0) |
| Black or African American | 72 (19.2) | 77 (20.5) |
| Asian | 20 (5.3) | 10 (2.7) |
| Native Hawaiian or Other Pacific Islander | 2 (0.5) | 7 (1.9) |
| American Indian or Alaska Native | 2 (0.5) | 0 (0) |
| Multiracial | 8 (2.1) | 6 (1.6) |
| Unspecified | 19 (5.1) | 20 (5.3) |
| Ethnicity, n (%) | ||
| Not Hispanic or Latino | 286 (76.3) | 300 (80.0) |
| Hispanic or Latino | 66 (17.6) | 52 (13.9) |
| Unspecified | 23 (6.1) | 23 (6.1) |
| Current LBP episode duration, n (%) | ||
| < 7 days | 81 (21.6) | 73 (19.5) |
| 7 days to <16 days | 40 (10.7) | 33 (8.8) |
| 16 days to <1 month | 23 (6.1) | 37 (9.9) |
| 1–3 months | 40 (10.7) | 39 (10.4) |
| > 3 months to <6 months | 23 (6.1) | 25 (6.7) |
| 6 months to <1 year | 28 (7.5) | 27 (7.2) |
| 1 year or more | 140 (37.3) | 141 (37.6) |
| PROMIS Pain intensity, 0–10, mean (SD) | 5.0 (1.9) | 5.0 (1.9) |
| PROMIS Pain interference, T-score, mean (SD) | 58.9 (7.2) | 60.0 (7.1) |
| PROMIS Physical function, T-score, mean (SD)* | 56.8 (7.1) | 56.8 (7.3) |
| PROMIS Sleep disturbance, T-score, mean (SD) | 55.5 (7.6) | 55.0 (7.8) |
| PROMIS Fatigue, T-score, mean (SD) | 51.5 (9.8) | 51.8 (10.2) |
| PROMIS Anxiety, T-score, mean (SD) | 48.1 (9.0) | 48.7 (8.7) |
| PROMIS Depression, T-score, mean (SD) | 45.0 (6.9) | 45.8 (7.1) |
| PROMIS Social Role, T-score, mean (SD)* | 54.6 (9.1) | 55.1 (8.9) |
Transformed (100-T-score) to make a higher score indicative of worse health; .
LBP, low back pain; PROMIS, Patient-Reported Outcomes Measurement Information SystemUMC, usual medical care; UMC+CC, usual medical care plus chiropractic care
Compared with the general population (T-score=50), at baseline, the participants demonstrated worse mean pain interference, physical function, sleep disturbance and satisfaction with participation in social roles and approximately average mean fatigue. At baseline, 79% of participants reported better than population average depression with 67% having a T-score=41, equivalent to the minimum response value for all depression questions. Similar values were noted for anxiety with 46% reporting 0 anxiety symptoms and 58% having less anxiety symptoms than the population average. This distribution created a heavily right-skewed distribution which prevented a meaningful evaluation of mediation of anxiety and depression outcomes in this sample.
Outcomes and estimates
We did not include exposure–mediator interactions in our final models due to having little effect on total natural direct and total natural indirect effect estimates and not improving the fit of the model. The results of mediation by both pain interference and pain intensity on each of the model outcomes are shown in table 2.
Table 2. Total, natural direct and natural indirect effects occurring through pain interference and pain intensity of chiropractic care on physical function, fatigue, sleep disturbance and social roles.
| Model outcome | Effect | Estimate | SE | 95% CI | P value |
| Physical function | TNDE | −0.54 | 0.59 | −1.60 to 0.72 | 0.494 |
| TNIE | −1.66 | 0.34 | −2.23 to −0.96 | <0.001 | |
| Total effect | −2.21 | 0.62 | −3.13 to −0.77 | <0.001 | |
| Proportion mediated | 0.77 | 3.68 | 0.43 to 2.00 | 0.006 | |
| Fatigue | TNDE | −1.01 | 0.80 | −2.73 to 0.43 | 0.158 |
| TNIE | −1.62 | 0.39 | −2.37 to −0.85 | <0.001 | |
| Total effect | −2.63 | 0.82 | −4.29 to −1.05 | 0.004 | |
| Proportion mediated | 0.62 | 1.09 | 0.30 to 1.65 | 0.002 | |
| Sleep disturbance | TNDE | −1.15 | 0.67 | −2.13 to 0.45 | 0.204 |
| TNIE | −1.11 | 0.29 | −1.90 to −0.74 | <0.001 | |
| Total effect | −2.26 | 0.66 | −3.36 to −0.87 | 0.006 | |
| Proportion mediated | 0.49 | 3.42 | 0.31 to 1.49 | 0.008 | |
| Social roles | TNDE | −0.49 | 0.73 | −1.88 to 0.96 | 0.548 |
| TNIE | −1.94 | 0.43 | −2.97 to −1.32 | <0.001 | |
| Total effect | −2.43 | 0.78 | −4.06 to −1.12 | <0.001 | |
| Proportion mediated | 0.81 | 0.71 | 0.50 to 1.97 | 0.004 |
Physical function and social roles are transformed to make a higher score a worse outcome, consistent with other PROMIS-29 measures. A negative effect estimate favours the usual medical care plus chiropractic care treatment arm over the usual medical care alone arm.
PROMISPatient-Reported Outcomes Measurement Information SystemTNDE, total natural direct effect; TNIE, total natural indirect effect
Table 3 shows the proportion mediated by pain interference and pain intensity individually and combined. The difference in total effect favoured the chiropractic care arm for all outcomes evaluated. The total effect difference was of consistent magnitude across domains with physical function =−2.21 (95% CI −3.13 to −0.77), fatigue =−2.63 (95% CI −4.29 to −1.05), sleep disturbance =−2.26 (95% CI −3.36 to −0.87) and social roles = −2.43 (95% CI −4.06 to −1.12). Pain interference and pain intensity were estimated to mediate about half of the effect on sleep disturbance (proportion mediated=0.49, 95% CI 0.31 to 1.49), to up to 81% of the effect on satisfaction with participation in social roles (proportion mediated =0.81, 95% CI 0.50 to 1.97). In each model, the estimate of the natural direct effect was much smaller than the natural indirect effect indicating that much of the difference between treatment arms on the outcomes occurred through pathways including pain interference and pain intensity rather than directly or through unmeasured mediators.
Table 3. Proportion of total effect mediated by individual mediators and combined.
| Model outcome | Mediator(s) | Estimate | SE | 95% CI | P value |
| Physical function | Pain interference | 0.57 | 0.27 | 0.31 to 1.20 | 0.002 |
| Pain intensity | 0.84 | 1.22 | 0.50 to 2.29 | 0.004 | |
| Combined | 0.77 | 3.68 | 0.43 to 2.00 | 0.006 | |
| Fatigue | Pain interference | 0.36 | 0.20 | 0.18 to 0.91 | <0.001 |
| Pain intensity | 0.57 | 0.63 | 0.35 to 1.72 | 0.006 | |
| Combined | 0.62 | 1.09 | 0.30 to 1.65 | 0.002 | |
| Sleep disturbance | Pain interference | 0.34 | 22.64 | 0.14 to 0.76 | 0.004 |
| Pain intensity | 0.73 | 0.60 | 0.32 to 1.76 | 0.008 | |
| Combined | 0.49 | 3.42 | 0.31 to 1.49 | 0.008 | |
| Social roles | Pain interference | 0.45 | 0.31 | 0.25 to 1.13 | <0.001 |
| Pain intensity | 0.94 | 0.72 | 0.53 to 2.22 | <0.001 | |
| Combined | 0.81 | 0.71 | 0.50 to 1.97 | 0.004 |
Individual mediator models indicated less mediation by pain interference than pain intensity for all outcomes. The inclusion of pain interference did not produce additional mediation of the effect for physical function, sleep disturbance or social roles. The addition of pain interference to the model resulted in a combined model mediating 62% (proportion mediated=0.62, 95% CI 0.30 to 1.65) of the effect on fatigue, while the pain intensity alone model mediated 57% (proportion mediated=0.57, 95% CI 0.35 to 1.72).
Sensitivity parameters
Complete case analysis did not produce substantially different effect estimates from our models with multiple imputation. The E-values used to assess unmeasured confounding are reported in table 4. The E-values for the total natural indirect effects were consistent across outcome models. For the total natural indirect effects in each model to be nullified, an unmeasured confounder would require an association of 2.13 times the total effect observed in the physical function model, 1.92 times the total effect observed for the fatigue model, 1.89 times the total effect observed in the sleep disturbance model and 2.02 times the total effect observed in the social roles model.
Table 4. Risk ratio and E-values for natural direct, natural indirect and total effects.
| Model outcome | Risk ratio | 95% CI | E-value | 95% LCL |
| Physical function | ||||
| TNDE | 0.94 | 0.83 to 1.07 | 1.31 | 1.0 |
| TNIE | 0.84 | 0.78 to 0.90 | 1.68 | 1.47 |
| Total effect | 0.79 | 0.69 to 0.90 | 1.85 | 1.47 |
| Fatigue | ||||
| TNDE | 0.92 | 0.809 to 1.038 | 1.407 | 1.0 |
| TNIE | 0.88 | 0.826 to 0.931 | 1.542 | 1.36 |
| Total effect | 0.80 | 0.707 to 0.912 | 1.797 | 1.42 |
| Sleep disturbance | ||||
| TNDE | 0.91 | 0.798 to 1.034 | 1.434 | 1.0 |
| TNIE | 0.89 | 0.840 to 0.933 | 1.511 | 1.35 |
| Total effect | 0.81 | 0.708 to 0.914 | 1.792 | 1.42 |
| Social roles | ||||
| TNDE | 0.96 | 0.848 to 1.084 | 1.255 | 1.0 |
| TNIE | 0.85 | 0.788 to 0.910 | 1.644 | 1.43 |
| Total effect | 0.81 | 0.712 to 0.925 | 1.767 | 1.38 |
LCL reported as minimum value of 1.0 for estimates that were not statistically significant.
LCL, lower confidence limit; TNDE, total natural direct effect; TNIE, total natural indirect effect
Discussion
Much of the effect of chiropractic care on physical function, fatigue, sleep disturbance and satisfaction with participation in social roles for active-duty military with LBP appears to be mediated by effects on pain intensity. Multiple mediator models had wide CIs that exceeded the 1.0 upper bounds for proportion mediated indicating that some variables in the multiple mediator models took on opposite signs from one another and that the natural indirect estimates are likely a more reliable estimate than the proportion mediated.18 When evaluated as a sole mediator, pain interference mediated the effects at a moderate level; when pain intensity was accounted for, pain interference did not add to the proportion of the effect mediated except for the model with fatigue as the outcome. Our other work, evaluates the mediation of chiropractic care’s effect on pain interference and pain intensity by physical function, fatigue, sleep disturbance, anxiety, depression and social roles and resulted in more modest effect estimates.24 Based on the previous findings, we hypothesised that it may be likely that pain intensity, a simpler measure, may have a stronger impact as a mediator of more complex biopsychosocial health measures than the reverse. Our current findings are consistent with this hypothesis.
Our use of clinical trial data that include a comparison group helps explain how additional improvement in biopsychosocial health measures occurs when chiropractic care is added to usual medical care for US active-duty military members by accounting for regression to the mean and natural course of disease. Though the possibility of mediator–outcome confounding still exists, our sensitivity analysis indicated that unmeasured confounding would have to be large and is not likely to nullify the natural indirect effects observed.
Patient definition of recovery from LBP is diverse and may not simply be a reduction in pain intensity39; rather, patients may place more emphasis on function and biopsychosocial health.39 Our findings suggest that changes in pain intensity are an important pathway through which additional health outcomes beyond pain are likely affected. A better understanding of this pathway helps to explain how the biopsychosocial health effects, attributed to complementary health approaches such as chiropractic care, may occur. This has potential implications for the treatment of patients with LBP. For clinicians delivering chiropractic care, a focus on treatment and tracking of pain intensity as an outcome appears to be an important intermediate factor for improving biopsychosocial outcomes. For clinicians referring patients to chiropractic care, pain intensity appears to be a good clinical indicator for evaluating patient response to treatment. This work assesses the pathways of the effect of chiropractic care on patient-reported outcomes; additional work is needed to better understand patient characteristics associated with improvement to better inform referral practices for this care.
Our approach to mediation analysis in this manuscript was different from others examining yoga,20 21 tai-chi,19 physical therapy,21,23 fear-avoidance belief interventions,40 operant graded activity41 and back skills training.42 In those analyses of data from participants with LBP, patient beliefs or other biopsychosocial factors were evaluated as the mediators of the effect on pain intensity or pain-related disability outcomes. Based on our findings, when evaluating interventions that target pain intensity and pain interference, such as chiropractic care, it appears appropriate to also evaluate the mediation of effect on biopsychosocial health factors by changes in pain. This change to pathway evaluation has potential to help better explain mechanisms of biopsychosocial health improvement for other interventions targeting pain.
Limitations
The sample for this study included US active-duty military sample who were young and predominantly male. It is unclear if treatment mechanisms are similar in non-military populations. Due to the sample, we were unable to assess the mediation of mental health outcomes in this study. The trial excluded those with a diagnosis of post-traumatic stress disorder and there was a low prevalence of mental health symptoms reported. It is well documented that military members are reluctant to report mental health symptoms and that there are challenges in studying military mental health.43,45 Though participants in the sample reported low prevalence of mental health symptoms they did report that they were adversely affected by fatigue at baseline. Though fatigue is classified as a physical domain in the PROMIS-29 questionnaire, fatigue symptoms are associated with mental illness in clinical practice.46 We therefore suspect that the low reporting of mental health symptoms may be due, in part, to reporting bias rather than simply a characteristic of the sample. The lack of mental health symptom reporting limits transportability to other populations that may be more likely to report mental health symptoms. Further, mediation analysis should be performed in a sample reporting mental health symptoms to better understand if effects on mental health are mediated by changes in pain. Differences in the delivery of care in the military treatment facilities including availability/access to care may further limit transportability to the general population.
This preliminary mediation analysis leaves many questions to be addressed about the effects of chiropractic care. We were not able to assess mediation of pain outcomes occurring through changes in patient beliefs. Patient beliefs such as self-efficacy, catastrophising and patient expectation have been identified as important mediators of the effect of tai chi,19 yoga and stretching20 and physical therapy22 23 on pain-related disability. Whether patient beliefs are important mediators of chiropractic care, outcomes mediated by pain intensity, or moderators of mediation has yet to be determined. Our analysis evaluated the effect of adding chiropractic care to usual medical care for US active-duty military as delivered in the military treatment facilities. Altering the components delivered as part of chiropractic care or the care pathway has the potential to change the factors appearing as important mediators of biopsychosocial outcomes. We did not evaluate baseline characteristics as moderators of the mediation effect. Baseline characteristics, such as the difference in mediation by the presence of acute or chronic pain at baseline, need further exploration. This would require distinct theoretical causal models and address a different question than we sought to address in this preliminary, exploratory analysis.
Our use of a time-lagged assessment in which the mediators were measured at 6 weeks and outcomes at 12 weeks does not completely address the issue of temporality; we can’t be entirely sure that the change in mediators preceded the change in outcomes rather than changing simultaneously. The 6-week time point was the end of the chiropractic care treatment period. Therefore, an alternative way to interpret our findings is that the mediators were of sustained improvement following a 6-week period of chiropractic care.
Conclusion
The effect of chiropractic care on biopsychosocial health factors appeared to be largely mediated by changes in pain intensity. This mediation effect was larger than previously found when evaluating biopsychosocial health factors as mediators of pain outcomes, indicating that the pathway through pain intensity is likely more important to explain changes in health due to chiropractic care. Our results require confirmation in diverse populations, including civilians and those experiencing mental health symptoms to determine if these mechanisms differ by patient characteristics. Pain intensity may be the best indicator for improvement due to chiropractic care as it is both one of the factors most affected and the mechanism by which most of the change in biopsychosocial health appears to occur. This information may be useful in tracking patient progress when evaluating response to chiropractic care treatment.
supplementary material
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The data used for these analyses were collected as part of a clinical trial supported by grant W81XWH-11-2-0107 to the RAND Corporation from the Chiropractic Research Program of the Congressionally Directed Medical Research Programs, US Army, and US Department of Defense.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-083509).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: The pragmatic clinical trial was approved by the Palmer College of Chiropractic institutional review board (#2010G137). All participants provided written consent for participation in the trial. This manuscript reports an analysis of a deidentified dataset and not human subjects research, so further ethical approval was not required.
Data availability free text: The deidentified dataset for this manuscript was provided by Palmer College of Chiropractic under a data use agreement. Reasonable data requests must be made to Palmer College of Chiropractic at research@palmer.edu to obtain data access.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Zacariah K Shannon, Email: zacariah.shannon@palmer.edu.
Cynthia R Long, Email: long_c@palmer.edu.
Elizabeth Chrischilles, Email: e-chrischilles@uiowa.edu.
Christine Goertz, Email: christine.goertz@duke.edu.
Robert Wallace, Email: robert-wallace@uiowa.edu.
Carri Casteel, Email: carri-casteel@uiowa.edu.
Ryan M Carnahan, Email: ryan-carnahan@uiowa.edu.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.Complementary, alternative, or integrative health: what’s in a name? NCCIH. [29-Jan-2023]. https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name Available. Accessed.
- 2.Clarke TC, Barnes PM, Black LI, et al. Use of Yoga, Meditation, and Chiropractors Among U.S. Adults Aged 18 and Over. NCHS Data Brief. 2018:1–8. [PubMed] [Google Scholar]
- 3.National board of chiropractic examiners. Practice analysis of chiropractic. 2020
- 4.Vining RD, Shannon ZK, Salsbury SA, et al. Development of a Clinical Decision Aid for Chiropractic Management of Common Conditions Causing Low Back Pain in Veterans: Results of a Consensus Process. J Manipul Physiol Ther. 2019;42:677–93. doi: 10.1016/j.jmpt.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ziegler A-ML, Shannon Z, Long CR, et al. Chiropractic Services and Diagnoses for Low Back Pain in 3 U.S. Department of Defense Military Treatment Facilities: A Secondary Analysis of a Pragmatic Clinical Trial. J Manipulative Physiol Ther. 2021;44:690–8. doi: 10.1016/j.jmpt.2022.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 7.Fritz JM, Koppenhaver SL, Kawchuk GN, et al. Preliminary investigation of the mechanisms underlying the effects of manipulation: exploration of a multivariate model including spinal stiffness, multifidus recruitment, and clinical findings. Spine (Phila Pa 1976) 2011;36:1772–81. doi: 10.1097/BRS.0b013e318216337d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewitte V, Cagnie B, Barbe T, et al. Articular dysfunction patterns in patients with mechanical low back pain: A clinical algorithm to guide specific mobilization and manipulation techniques. Man Ther. 2015;20:499–502. doi: 10.1016/j.math.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Penza CW, Horn ME, George SZ, et al. Comparison of 2 Lumbar Manual Therapies on Temporal Summation of Pain in Healthy Volunteers. J Pain. 2017;18:1397–408. doi: 10.1016/j.jpain.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bishop MD, Beneciuk JM, George SZ. Immediate reduction in temporal sensory summation after thoracic spinal manipulation. Spine J. 2011;11:440–6. doi: 10.1016/j.spinee.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed WR, Long CR, Kawchuk GN, et al. Neural Responses to Physical Characteristics of a High-velocity, Low-amplitude Spinal Manipulation: Effect of Thrust Direction. Spine (Phila Pa 1976) . 2018;43:1–9. doi: 10.1097/BRS.0000000000001344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reed WR, Pickar JG, Sozio RS, et al. Characteristics of Paraspinal Muscle Spindle Response to Mechanically Assisted Spinal Manipulation: A Preliminary Report. J Manipul Physiol Ther. 2017;40:371–80. doi: 10.1016/j.jmpt.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reed WR, Pickar JG. Paraspinal Muscle Spindle Response to Intervertebral Fixation and Segmental Thrust Level During Spinal Manipulation in an Animal Model. Spine (Phila Pa 1986) 2015;40:E752–9. doi: 10.1097/BRS.0000000000000915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bialosky JE, Beneciuk JM, Bishop MD, et al. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J Orthop Sports Phys Ther. 2018;48:8–18. doi: 10.2519/jospt.2018.7476. [DOI] [PubMed] [Google Scholar]
- 15.Bolton D, Gillett PG. The biopsychosocial model of health and disease: new philosophical and scientific developments. Palgrave Pivot; 2019. The biopsychosocial model 40 years on. [PubMed] [Google Scholar]
- 16.Coulter ID, Hurwitz EL, Adams AH, et al. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine (Phila Pa 1976) 1976;27:291–6. doi: 10.1097/00007632-200202010-00018. [DOI] [PubMed] [Google Scholar]
- 17.Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:514–30. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 18.VanderWeele T. Explanation in causal inference: methods for mediation and interaction. Oxford University Press; 2015. [Google Scholar]
- 19.Hall AM, Kamper SJ, Emsley R, et al. Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement Ther Med. 2016;25:61–6. doi: 10.1016/j.ctim.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Sherman KJ, Wellman RD, Cook AJ, et al. Mediators of yoga and stretching for chronic low back pain. Evid Based Complement Alternat Med. 2013;2013:130818. doi: 10.1155/2013/130818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joyce CT, Chernofsky A, Lodi S, et al. Do Physical Therapy and Yoga Improve Pain and Disability through Psychological Mechanisms? A Causal Mediation Analysis of Adults with Chronic Low Back Pain. J Orthop Sports Phys Ther. 2022;52:470–83. doi: 10.2519/jospt.2022.10813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smeets RJEM, Vlaeyen JWS, Kester ADM, et al. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7:261–71. doi: 10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 23.Cheing G, Vong S, Chan F, et al. Testing a path-analytic mediation model of how motivational enhancement physiotherapy improves physical functioning in pain patients. J Occup Rehabil. 2014;24:798–805. doi: 10.1007/s10926-014-9515-8. [DOI] [PubMed] [Google Scholar]
- 24.Shannon ZK, Long CR, Chrischilles EA, et al. Effect of chiropractic care on low back pain for active-duty military members: Mediation through biopsychosocial factors. PLoS One. 2024;19:e0310642. doi: 10.1371/journal.pone.0310642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee H, Cashin AG, Lamb SE, et al. A Guideline for Reporting Mediation Analyses of Randomized Trials and Observational Studies: The AGReMA Statement. JAMA. 2021;326:1045–56. doi: 10.1001/jama.2021.14075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D, Schulz KF, Simera I, et al. Guidance for developers of health research reporting guidelines. PLoS Med. 2010;7:e1000217. doi: 10.1371/journal.pmed.1000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goertz CM, Long CR, Vining RD, et al. Assessment of chiropractic treatment for active duty, U.S. military personnel with low back pain: study protocol for a randomized controlled trial. Trials. 2016;17:70. doi: 10.1186/s13063-016-1193-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goertz CM, Long CR, Vining RD, et al. Effect of Usual Medical Care Plus Chiropractic Care vs Usual Medical Care Alone on Pain and Disability Among US Service Members With Low Back Pain: A Comparative Effectiveness Clinical Trial. JAMA Netw Open . 2018;1:e180105. doi: 10.1001/jamanetworkopen.2018.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hays RD, Shannon ZK, Long CR, et al. Health-Related Quality of Life Among United States Service Members with Low Back Pain Receiving Usual Care Plus Chiropractic Care vs Usual Care Alone: Secondary Outcomes of a Pragmatic Clinical Trial. Pain Med. 2022;23:1550–9. doi: 10.1093/pm/pnac009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.PROMIS Health Organization and PROMIS Cooperative Group PROMIS. 2023. [18-Dec-2023]. https://www.healthmeasures.net/explore-measurement-systems/promis Available. Accessed.
- 31.PROMIS Health Organization and PROMIS Cooperative Group Intro to PROMIS. 2023. [18-Dec-2023]. https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis Available. Accessed.
- 32.R Core Team R: a language and environment for statistical computing. 2023
- 33.Shi B, Choirat C, Coull BA, et al. CMAverse: A Suite of Functions for Reproducible Causal Mediation Analyses. Epidemiology (Sunnyvale) 2021;32:e20–2. doi: 10.1097/EDE.0000000000001378. [DOI] [PubMed] [Google Scholar]
- 34.Vansteelandt S, VanderWeele TJ. Natural Direct and Indirect Effects on the Exposed: Effect Decomposition under Weaker Assumptions. Biometrics. 2012;68:1019–27. doi: 10.1111/j.1541-0420.2012.01777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137–50. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vansteelandt S, Bekaert M, Lange T. Imputation Strategies for the Estimation of Natural Direct and Indirect Effects. Epidemiol Methods. 2012;1:131–58. doi: 10.1515/2161-962X.1014. [DOI] [PubMed] [Google Scholar]
- 37.Bellavia A, Valeri L. Decomposition of the Total Effect in the Presence of Multiple Mediators and Interactions. Am J Epidemiol. 2018;187:1311–8. doi: 10.1093/aje/kwx355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haneuse S, VanderWeele TJ, Arterburn D. Using the E-Value to Assess the Potential Effect of Unmeasured Confounding in Observational Studies. JAMA. 2019;321:602–3. doi: 10.1001/jama.2018.21554. [DOI] [PubMed] [Google Scholar]
- 39.Hush JM, Refshauge K, Sullivan G, et al. Recovery: What does this mean to patients with low back pain? Arthritis & Rheumatism . 2009;61:124–31. doi: 10.1002/art.24162. [DOI] [PubMed] [Google Scholar]
- 40.Mansell G, Hill JC, Main CJ, et al. Mediators of Treatment Effect in the Back In Action Trial: Using Latent Growth Modeling to Take Change Over Time Into Account. Clin J Pain. 2017;33:811–9. doi: 10.1097/AJP.0000000000000463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leeuw M, Goossens MEJB, van Breukelen GJP, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain. 2008;138:192–207. doi: 10.1016/j.pain.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 42.Fordham B, Ji C, Hansen Z, et al. Explaining How Cognitive Behavioral Approaches Work for Low Back Pain: Mediation Analysis of the Back Skills Training Trial. Spine (Phila Pa 1976) . 2017;42:E1031–9. doi: 10.1097/BRS.0000000000002066. [DOI] [PubMed] [Google Scholar]
- 43.Greene-Shortridge TM, Britt TW, Castro CA. The stigma of mental health problems in the military. Mil Med. 2007;172:157–61. doi: 10.7205/milmed.172.2.157. [DOI] [PubMed] [Google Scholar]
- 44.Schreiber M, McEnany GP. Stigma, American military personnel and mental health care: challenges from Iraq and Afghanistan. J Ment Health. 2015;24:54–9. doi: 10.3109/09638237.2014.971147. [DOI] [PubMed] [Google Scholar]
- 45.Clement S, Schauman O, Graham T, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- 46.Thomas S, Jenkins R, Burch T, et al. Promoting Mental Health and Preventing Mental Illness in General Practice. London J Prim Care (Abingdon) 2016;8:3–9. doi: 10.1080/17571472.2015.1135659. [DOI] [PMC free article] [PubMed] [Google Scholar]


