Abstract
Introduction
Despite recommendations, non-surgical treatment modalities in knee and/or hip osteoarthritis (KHOA) are underused. An information campaign was developed targeting patients with early stage KHOA and healthcare professionals (HCPs) to optimise timing of referral to secondary care. This protocol describes the development and design of this information campaign and a randomised controlled trial (RCT) on its effectiveness in impacting healthcare utilisation.
Methods and analysis
The behaviour change wheel was used as a theoretical framework for the campaign design. After an inventory of the literature, a selection was made of factors influencing healthcare use. Effectiveness will be evaluated with a cluster RCT. The study aims to recruit 300 patients in 24 general practices, randomly allocated to intervention or usual care (ratio 1:1). General practitioners and affiliated HCPs are invited to participate in the trial and recruit patients. Patients are eligible to participate if they are Dutch speaking, aged 50–75 years, registered with KHOA at the general practice, without joint replacement nor having considerable walking impairment. The main end point is the difference in rate of referral to hospital care as reported by patients over a period of 18 months. Secondary parameters include quality of care, beliefs about KHOA treatment modalities, physical activity, self-management behaviour and referral rates to secondary care. Patients receive online questionnaires at baseline, 6, 12 and 18 months. Online questionnaires are sent to HCPs at baseline and after 12 months to assess (changes in) beliefs about KHOA treatment modalities.
Ethics and dissemination
All methods are carried out in accordance with relevant guidelines and regulations and ethical approval was waived by the Dutch medical research ethical committee of Arnhem-Nijmegen (file number 2020-7246). Trial results will be communicated to participants and patient representatives via news letters, the public via the Sint Maartenskliniek website and journals of patient organisations and HCPs via congresses and international scientific journals.
Trial registration number
NL9140.
Keywords: knee, hip, primary prevention, public health, rheumatology, self-management
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study protocol includes a systematic, theory-based approach to design an intervention to improve healthcare use among patients with osteoarthritis (OA) in the Netherlands, building a toolbox of theory-based and evidence-based intervention strategies.
The study is conducted in a real patient setting within general practices, making results sufficiently relevant to the real-world context of the Dutch OA population.
Randomisation of general practices is performed via a computer-generated method to ensure minimal bias.
No blinding or allocation concealment is performed for the current trial.
Participants are all from the Nijmegen region, which might influence the generalisability of the study data.
Final results will determine whether characteristics correspond to the general population of Dutch primary care.
Introduction
Osteoarthritis (OA) is a leading cause of disability of posture and movement worldwide and associated with an extremely high economic burden. This burden is largely attributable to the effects of disability, comorbid disease and the expense of treatment. OA is expected to become the most common disease by 2040.1 OA is characterised by pain and stiffness, which can impair daily functioning and decrease physical activity (PA). Although there are no curative treatment options for OA, multiple effective non-surgical and surgical treatment options for reducing pain and improving functioning and quality of life are available. International guidelines recommend a combination of pharmacological and non-pharmacological modalities as primary approach for patients with knee or hip osteoarthritis (KHOA), including psycho-educational interventions to improve self-management and promote PA, exercise therapy, weight reduction and pain medication. In general, a stepped-care approach is advocated,2 3 in which more advanced treatment options are only considered if previous options failed to produce satisfactory results. In other words, joint replacement surgery is only considered for patients with severe pain and reduced functioning once non-surgical treatments become unsuccessful.
Despite recommendations, non-surgical treatment modalities in KHOA are underused,3,14 while timely usage of these treatment modalities is advocated and may prevent untimely surgery. Despite strong evidence supporting their effectiveness, patients and healthcare professionals (HCPs) perceive non-surgical treatment options, such as enhancement of self-management, exercise and weight reduction as unappealing and considered to have ‘low value’.15 On the other hand, advanced treatment options like surgery are considered to be a ‘quick fix’,16 despite the substantial number of patients not satisfied with the results of total joint replacement (TJR).17 18 Undergoing total knee replacement too early may result in little or no benefit in terms of pain relief and functional improvement,19,21 while exposing the patient to the risks of a major operation.22 In addition, early referral to secondary care services, such as the orthopaedic surgeon, might give patients the perception that they will eventually need surgery. This may lead to undervaluation of conservative management,23 and thus negatively affect patient motivation to participate in conservative management.
Another potential hurdle is that general practitioners’ (GPs) and medical specialists’ outcome expectations about non-surgical treatment options often do not match with recommendations from guidelines. Their confidence in competencies of other healthcare providers such as physiotherapists and dietitians is low.8 24 25 As a result, patients with OA may receive conflicting information about effective, non-surgical treatment options from various sources. Receiving conflicting information is associated with undesirable outcomes like non-adherence to treatment.26 27 It is important that patients receive a single, unified perspective from healthcare providers on treatment options and strategies. In addition, negative beliefs or unrealistic thoughts about treatment modalities might influence the choice of treatment.5 6 9 One of those false beliefs, and possibly the most worrisome, is that OA is the result of wear and tear, and that exercise is harmful for the joints, which completely counters the guideline recommendations of regular exercise to prevent functional decline.28 This emphasises the importance that patients receive up-to-date, evidence-based information about the benefits and possible disadvantages of non-surgical and surgical treatment options.
To achieve this, we developed an information campaign that uses a variety of different evidence-based persuasive communication techniques. This article describes both (a) the development and content of this information campaign aimed to increase (1) awareness and knowledge of patients and their HCPs about OA and treatment options and (2) quality of communication and interdisciplinary collaboration, targeting both patients with early stage KHOA and HCPs and (b) the design of a randomised controlled trial (RCT) on the effectiveness of this campaign in impacting patterns of healthcare consumption.29 The primary aim of this intervention is to optimise timing of referral to secondary care.
Methods
Development and content of information campaign
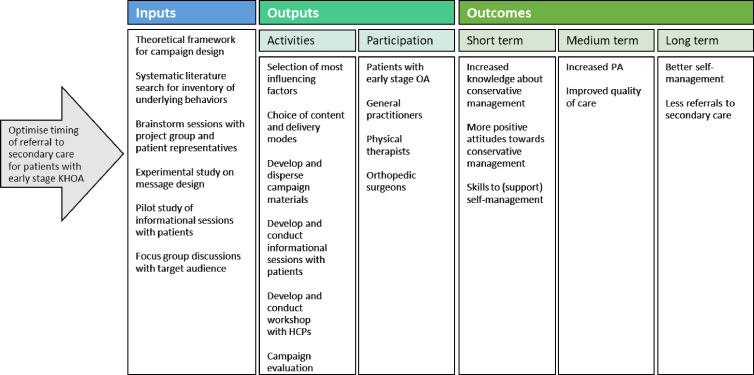
For the development of the current intervention, a project group was formed consisting of members in the fields of behavioural communication (JO, ED), physiotherapy and rheumatology (CHMvdE), orthopaedics (SK) and primary care (HS, WJJA), along with two patient representatives (Jolanda Marneef, Sandra Ahoud). The process of intervention development is shown in the logic model in figure 1. A logic model is a diagram of how an intervention is proposed to work, showing mechanisms by which an intervention influences the proposed outcomes30 (see also O’Cathain et al31 for a framework of actions for intervention development). We will discuss the elements of this logic model in the upcoming paragraphs.
Figure 1. Logic model of intervention. HCP, healthcare professional; KHOA, knee and/or hip osteoarthritis; PA, physical activity.
We chose the behaviour change wheel (BCW)32 as a theoretical framework for the campaign design. The BCW offers a synthesis of a wide range of theoretical constructs from different theories of behaviour and behaviour change. It is supported by an extensive list of clearly labelled and defined behavioural change techniques on which to base intervention content.33 A behaviour change technique is an active component of an intervention designed to change behaviour, such as goal setting or framing/reframing. At the heart of the BCW is the Capability, Opportunity, Motivation-Behaviour (COM-B) model, which suggests that behaviour change occurs when there is a change in an individual’s capability, opportunity and/or motivation. A complete description of the model can be found in online supplemental file 1.
We followed a stepwise approach to the intervention design. The first step within the intervention design was to make an inventory of literature concerning underlying behaviours, identifying influencing factors (ie, barriers and facilitators) in the use of conservative treatment among patients with OA and their HCPs. Next, a selection was made of those factors expected to have the largest influence on health behaviours. Third, appropriate content and delivery modes were chosen to develop campaign materials and campaign evaluation methods. We identified behavioural change techniques most likely to bring about change in behaviours with help of the ‘Behavioural Change Technique Theory and Technique tool’, a heat map linking behavioural change techniques to underlying behaviours.34
Inventory of underlying behaviours
We systematically searched the literature for studies on factors influencing KHOA healthcare use (details are provided in online supplemental file 2). In total, 12 articles were identified focusing on influencing factors on patient or HCP level, or both. These factors for using conservative treatment modalities were then mapped against the COM-B model. Table 1 provides a complete overview of the influencing factors to use conservative treatment of patients and HCPs as retrieved from the literature.
Table 1. Influencing factors retrieved from literature.
| COM-B | Influencing factors to use conservative treatment | Source |
| Capability | Health literacy and/or level of health knowledge | (77),(78), (12), (79), (80), (81), (24), (25) |
| Misconceptions about causes of OA | (77), (78), (25), (82), (83) | |
| Physical and/or symptom-related limitations | (77), (78), (12), (83), (84), (85) | |
| Difficulty with sensitive subjects during consultations | (77), (79), (81) | |
| Understanding the importance of a healthy lifestyle | (77), (12), (81), (83) | |
| Understanding the importance to follow guidelines | (77), (78), (79), (81), (24), (25), (83) | |
| OA seen as untreatable and/or TJR seen as inevitable | (77), (81), (24), (25), (82), (85) | |
| Ability to personalise treatment | (78), (81), (25), (82) | |
| Possessing skills that facilitate change | (77), (78), (12), (81), (25), (82), (83) | |
| Opportunity | Access to and awareness of guidelines for conservative treatment and stepped care strategy | (77), (78), (79), (81), (24), (25), (85) |
| Accessibility of information and resources | (77), (78), (12), (83) | |
| Accessibility of treatment and/or environmental factors | (77), (78), (12), (81), (24), (25), (82), (83), (84), (85) | |
| Availability of practical support | (78), (12), (84) | |
| Financial resources and healthcare supplementation | (77), (78), (12), (24), (83), (84), (85) | |
| Access to evidence-based treatments for conservative modalities | (81), (83) | |
| Nature of patient-provider relationship | (81), (25) | |
| Time and/or workload-related factors | (77), (78), (81), (24), (82), (83), (84) | |
| Collaboration between HCPs | (78), (81), (24), (83), (85) | |
| Preference for certain treatment(s) | (77), (78), (12), (24), (25), (83), (84), (85) | |
| Support from environment (social support) | (78), (12), (25), (84), (85) | |
| Opinions of others about treatment options | (78), (84), (85) | |
| Motivation | Concerns about consequences of surgery | (78), (25), (84) |
| Concerns about overexertion or degeneration due to PA | (78), (81), (82), (83), (84), (85) | |
| Concerns about pain medication tolerance and side effects | (78), (25), (84) | |
| Motivation to make lifestyle changes | (78), (81), (83), (84) | |
| Previous experiences with treatments or lifestyle changes | (78), (12), (25), (83), (84), (85) | |
| Trust in competence of the HCP | (78), (81), (24), (25) | |
| Trust in efficacy of treatment | (77), (78), (12), (81), (24), (25), (83), (85) | |
| Trust in ability to make lifestyle changes | (77), (78), (81), (24), (82), (84) |
HCPhealthcare professionalOAosteoarthritisPAphysical activityTJRtotal joint replacement
Choice of content and delivery modes
The primary aim of the campaign is to positively impact beliefs about conservative treatments of patients as well as their healthcare providers. To achieve this, we embedded a variety of different techniques from persuasive communication, including evidence-based message strategies such as framing,35 36 narratives37 38 and metaphors39 40 in written material, an educational programme for patients, and education for HCPs. During multiple brainstorm sessions of the project group, the focal point emerged to focus on promoting conservative treatment in terms of exercise and pain medication. Four themes arose: (1) what is OA, (2) dealing with OA-related pain, (3) alleviate symptoms with PA and (4) understanding pain following PA. Details of this process can be found in online supplemental file 3. Subsequently, a number of key messages were formulated (table 2) on the basis of findings from existing literature10 41 42 and additional brainstorming sessions with the project group as well as patient representatives. During these brainstorming sessions, participants were asked to rate several statements and were invited to make additional suggestions.
Table 2. Key messages of information campaign.
| The four wisdoms of Dr Bart (English translation, not rhyming) | De vier wijsheden van Dr Bart (Dutch original) |
| Moving your joints helps to relieve symptoms | Het bewegen van je gewrichten helpt klachten te verlichten |
| By strengthening joints and muscles you can reduce complaints | Door gewricht en spieren te versterken kan je klachten beperken |
| If being physically active is difficult due to complaints, know that paracetamol does not harm | Als bewegen door klachten moeilijk gaat, weet dan dat paracetamol niet schaadt |
| If you are struggling to control symptoms, you can always visit your doctor (general practitioner) | Moeite om de klachten te bedwingen, loop dan even bij de huisarts binnen |
The key messages were processed in informational material including (digital) posters and flyers, and an infographic, to be distributed in the general practices and delivered to the patient digitally. The theory behind these key messages is the notion that mere exposure to an object can lead to a more positive attitude towards the object.43 Key messages contained framing (phrasing a statement that describes a choice or outcome in terms of its positive (gain) or negative (loss) features) and testimonials of both a doctor (Dr Bart) and a patient (Babs), based on findings of a previous study of our research group,44 and included rhyme for better processing and stronger persuasiveness of the message.45 46 In addition, the collaboration between the three hospitals, the regional GP cooperatives and the regional physiotherapists association within the project will be emphasised in the material, as messages from a credible source are processed better and have a positive impact on intentions.47,49
Furthermore, we aim to increase knowledge and awareness with two educational sessions given to the patient by a multidisciplinary team of HCPs. The content of these sessions is based on an educational programme developed for a previous pilot study,10 in which consensus-based answers to frequently asked questions (FAQs) about OA and treatment modalities were incorporated. Topics include a general explanation of OA, the importance of PA and a healthy diet, medication, surgery and facilities in the area. Patients also receive a course guide with extensive information on OA and several exercises to help them self-manage the disease. The educational sessions are given by a GP and a physical therapist (PT). The informational material in these sessions are enriched with above-mentioned key messages, experiences of model patients and a social group activity. In addition, an orthopaedic surgeon of each participating hospital participated in an educational video with information about TJR, which is presented at one of the educational sessions and online. Furthermore, online events will be organised every 2 months, in which different disciplines alternately answer questions from patients.
As for the HCP, the primary aims within the campaign are to offer practical skills and tools that facilitate change, to provide them with the necessary information to adhere to guideline recommendations and to improve collaboration. As such, a multidisciplinary workshop is developed about the importance of good communication about OA and consistency of patient information among the different disciplines, simultaneously increasing knowledge and awareness of the stepped-care approach, and on promoting collaboration between healthcare providers. GPs of the intervention group and PTs to whom patients are regularly referred by these GPs will be invited to participate. Healthcare providers will be reminded of several techniques that enhance self-efficacy during patient interviews,50 as self-efficacy is found to be a key mediator of patient health behaviour.51,54 An infographic will be shared to be used during consultations, in order to induce better processing of health information by the patient,55,57 and to act as a check for health professionals to inform patients about all available treatment options.
Campaign materials were developed based on consensus within the project group and the two patient representatives. Pilot versions of campaign materials were evaluated with patients and HCPs in the study area via focus group discussions on aesthetic appreciation, processing fluency and understandability and revised where necessary. As the campaign is a joint effort, informational materials were designed to have a regional ‘look and feel’ by a professional local graphical designer (BuroRub). In addition, the educational video involving orthopaedic surgeons was developed by a team within the Sint Maartenskliniek that is experienced in the creation of audio-visual content. A complete overview of the chosen content and modes of delivery is given in tables3 4. Numbers in parentheses refer to the specific identification number that was assigned to the behavioural change technique in previous literature.58 Definitions of chosen behavioural change techniques can be found in online supplemental file 4. An extensive overview of the intervention framework is provided in online supplemental file 3.
Table 3. Content and delivery modes for patients.
| Content | Mode of delivery | Influencing factor | Behavioural change technique |
| Key messages; answers to FAQs | Informational material | OA seen as untreatable and/or TJR seen as inevitable; trust in efficacy of conservative treatment options; concerns about overexertion or degeneration due to PA; concerns about pain medication tolerance and side effects | Information about health consequences (5.1); framing/reframing (13.2) |
| Exercise guidance/examples;instruction on pain medication in support of PA | Consultations; informational material; educational sessions | Concerns about overexertion or degeneration due to PA; health literacy or level of health knowledge | Instruction on how to perform behaviour (4.1) |
| Experiences of exemplary patients with PA and pain medication | Educational session; informational material | Previous experiences with treatments or lifestyle changes | Demonstration of the behaviour (6.1) |
| Encouragement by HCP | Video; consultations; educational sessions | Opinion of others about treatment options; preference for certain treatment(s) | Credible source (9.1) |
| Overview of group-based PA programmes in the community | Informational material; consultations;educational sessions | Support from environment (practical) | Social support (practical) (3.2) |
| Provide ongoing (professional) support | Training companion; consultations | Support from environment (practical) | Social support (practical) (3.2) |
FAQfrequently asked questionHCPhealthcare professionalOAosteoarthritisPAphysical activityTJRtotal joint replacement
Table 4. Content and delivery modes for HCP.
| Content | Mode of delivery | Influencing factor | Behavioural change technique |
| Development of local professional networks | Accredited postgraduate education | Collaboration between HCPs | Restructuring the social environment (12.2) |
| Training in strategic and effective communication techniques | Accredited postgraduate education | Possessing skills that facilitate change | Instruction on how to perform behaviour (4.1) |
| Create awareness of processes of care and access to effective conservative treatment options | Infographic to be used during consultation | Access to and awareness of guidelines for conservative treatment and stepped care strategy; understanding the importance to follow guidelines | Adding objects to the environment (12.5) |
| Shift focus from ‘cure’ or ‘fix’ by TJR to symptom relief, improved function and quality of life by conservative treatment | Accredited postgraduate education | OA seen as untreatable or TJR seen as inevitable; trust in efficacy of treatment | Review outcome goal(s) (1.7) |
| Overview of evidence-based exercises; guidelines for pain medication | Informational material on exercises and pain medication | Access to evidence-based treatments for conservative modalities | Instruction on how to perform behaviour (4.1) |
| Key messages, answers to FAQs | Accredited postgraduate education; informational material | OA seen as untreatable or TJR seen as inevitable; trust in efficacy of conservative treatment options | Information about health consequences (5.1) |
FAQfrequently asked questionHCPhealthcare professionalOAosteoarthritisTJRtotal joint replacement
Study design
The effect of this information campaign on patterns of healthcare utilisation will be examined in a cluster RCT. After recruitment and baseline assessments of patients and HCPs affiliated with those practices has taken place, 24 participating general practices will be randomised into either the experimental or control group. Then, the information campaign will start in the (reference area of) practices allocated to the experimental group. Data collection comprises online questionnaires (to patients and HCPs), and extraction of electronic patient records (Huisarts Informatie Systeem (HIS)) of participating practices. Recruitment of patients for the study was scheduled between August 2022 and February 2023. The follow-up duration is 18 months. A flow chart of the study design can be found in online supplemental file 5.
Participants
The study population will consist of patients with KHOA within 24 general practices and their related HCPs.
Inclusion criteria
In order to be eligible to participate in this study, general practices must meet the following criteria:
Affiliated with one of the GP cooperatives.
≥12 registered patients with KHOA eligible to participate.
Willing to provide access to health information system.
Having professional communication with PT(s).
In order to be eligible to participate in this study, HCPs must be one of the following:
A GP working in one of the included practices.
A practice assistant or practice nurse working in one of the included practices.
In order to be eligible to participate in this study, patients must meet all of the following criteria:
Registered with KHOA at the general practice (International Classification of Primary Care: L90, L89).
Age 50–75 years.
Having a painful knee and/or hip for at least the past 3 months.
Having a painful knee and/or hip >15 days of the past month.
Morning stiffness <30 min (knee) and/or <60 min (hip).
Having an email address.
Exclusion criteria
Patients meeting any of the following criteria will be excluded from participation in this study:
Age >75 years.
Unable to communicate and complete online questionnaires in Dutch.
Wheelchair users or a walking distance of <100 m.
Either scheduled or having one or more replacements of hip and/or knee.
Study procedure
Recruitment of general practices and HCPs
General practices affiliated either with the GP cooperative in the Nijmegen area NEO GP care (NEO huisartsenzorg in Dutch) or the Radboudumc Family Medicine Network (Netwerk Huisartsen Praktijken in Dutch) will be invited to participate in the study by the executing researcher (JO) by means of an informational letter and a follow-up telephone call after 1 week. Within the included practices, GPs, practice assistants and practice nurses are asked to participate, and practices are asked to provide contact details of PTs to whom patients are regularly referred. The executing researcher will invite these PTs for the multidisciplinary workshops.
Recruitment and screening procedure of patients
Potential participants (aged 50–75 years and diagnosis of KHOA) will be invited for the study on the basis of extractions from medical records by their GP by means of a standard template letter of invitation. To minimise the influence study information may have on control groups,59 participants in both conditions will receive the same information letter stating that the aim of the study is to monitor and evaluate the quality of care for patients with (probable) OA. The information letter can be found in online supplemental file 6. Consenting patients will be contacted by phone and questioned on the remaining inclusion and exclusion criteria (documented via CastorEDC) by the researcher (JO).
Randomisation, allocation concealment and blinding
To ensure balance between clusters on relevant variables, we will use a constrained randomisation procedure.60 This computer-generated method accommodates multiple covariates, both categorical and continuous. Relevant covariates to be accounted for in the constrained randomisation procedure are: (1) number of patients included, (2) general practice in a healthcare centre (yes/no) and (3) geographical location (outside city area, city centre, city north, city other). No additional allocation concealment or blinding will be performed.
Study parameters
Main study parameter
The primary end point will be the difference in referral rates to secondary care between groups (intervention vs control) as reported by patients over a period of 18 months (treatment for KHOA restricted to primary care (yes/no)).
Secondary study parameters
Secondary study parameters for patients include general health status, pain (at rest and during activity) and daily functioning, pain coping, PA, quality of care, beliefs about KHOA treatment modalities, PT, pain medication and self-management behaviour. In addition, we assess cost-effectiveness of the information campaign compared with usual care; and we assess barriers and facilitators for network collaboration as perceived by HCPs after having attended a multidisciplinary workshop.
Other study parameters
Other study parameters include referral rates to OA healthcare services.
Assessments
Online questionnaire for patients
Data collection comprises online questionnaires (CastorEDC) at baseline and follow-up at 6, 12 and 18 months. The first questionnaire is estimated to take 30 min to complete, the others 20 min. Participants receive an email with a unique link to the questionnaire and are reminded after 2 weeks if they have not yet completed the questionnaire. Each question needs to be answered in order to proceed. To promote participant retention and complete follow-up, participants will be contacted by phone if they have not completed the questionnaire after this reminder. A schedule of the assessments can be found in online supplemental file 7.
Baseline characteristics
Sociodemographic characteristics of patients: gender, birth year, length, weight, living situation (single or cohabiting), education (secondary education or lower (ie, elementary, high school and technical or vocational training); higher education (ie, research universities and universities of applied sciences)).
Disease characteristics: duration of complaints, number of painful knee and hip joints, number of other painful joints, comorbidities (Central Bureau of Statistics Health Survey, Diseases and Disorders).61
General health status
General health status will be assessed by the EuroQol five-dimensional five-level (EQ-5D-5L).62 From the EQ-5D-5L classification system, a utility index will be calculated.
Pain and daily functioning
Pain at rest and pain during activity will be assessed by a standardised Numeric Rating Scale. Daily functioning will be assessed by the Lower Extremity Functional Scale (LEFS).63 The LEFS is a 20-item condition-specific questionnaire designed to be applicable to individuals with musculoskeletal conditions of the lower extremity. Each item of the LEFS scores on a 5-point scale ranging from 0 to 4 points. Accordingly, LEFS scores range from 0 to 80 points, with higher scores representing higher levels of functioning. The Dutch version of the questionnaire is validated in patients with OA.64
Pain coping
To assess passive pain coping behaviour, the ‘resting’ subscale of the pain-coping inventory (PCI)65 will be used. This subscale consists of five statements on a 4-point scale (rarely or never, sometimes, often, very often). As the PCI assesses participants’ typical response to pain across situations and does not assess coping with a specific episode of pain, some modifications of the instructions have been made for assessing specific OA pain episodes.
Physical activity
PA will be measured by the International Physical Activity Questionnaire-Short Form (IPAQ-SF). The IPAQ-SF is a structured questionnaire, consisting of seven open-ended items in which respondents are asked to fill in the number of days and time spent doing vigorous and moderate activities, walking and sitting in the last 7 days. The IPAQ-SF is considered a reasonably valid tool to assess PA.66
Healthcare use
Healthcare use will be assessed by a questionnaire used in previous studies on similar patient populations,67 consisting of the following: which HCPs they visited in the preceding 6-month period related to their KHOA complaints, the number of visits to these professionals, the use of pain medication and medical devices, whether they received additional diagnostics (ie, X-rays, blood tests, MRI) for their KHOA complaints and whether they received a TJR in the hip and/or knee in the preceding 6 months, or if they are on the waiting list for one. Direct medical costs due to OA will be calculated on the basis of the healthcare use questionnaire. Cost prices as stated in the Dutch costing manual will be used to calculate direct medical costs in order to establish cost-effectiveness of the information campaign compared with usual care. The costing manual offers reference prices for a broad range of healthcare services.68
Quality of care
A questionnaire regarding patient-reported quality indicators (QIs) for OA care is used to assess quality of care.69 This OA-QI questionnaire is translated and validated in Dutch by members of our research group according to the forward and backward translation method,70 and consists of 18 binary items (yes/no) related to OA guideline recommendations. Examples of QIs are “Have you been offered a referral to a health professional who can advise you about physical activity and exercise?” and “If you have joint pain, was paracetamol the first pain killer recommended?” In addition, several items of the Consumer Quality Index (CQI) on experiences with the care of the GP and other care providers in the general practice71 of the participants will be used. Items include questions to assess comprehensibility of information and advice as given by the HCPs, cooperation between HCPs and whether they received contradictory information from different HCPs within the practice. The CQI is a standardised method for measuring, analysing and reporting customer experiences in healthcare.72
Beliefs about treatment options
The Treatment beliefs in OsteoArthritis questionnaire is used to determine beliefs about treatment options of patients and HCPs within the general practices. It is a questionnaire based on the theory of planned behaviour, developed and validated by members of our research group.7 It assesses patients’ beliefs about various treatment modalities of hip and knee OA with five modules (PA, pain medication, physiotherapy, injections and TJR) and a total of 60 items consisting of a 5-point Likert scale (agree–disagree). Examples of items are “I think that doing exercise activities involves risks”, “I am afraid of using pain medication” and “My quality of life increases with physiotherapy”.
Self-management behaviour
The Patient Activation Measure (PAM)-13 will be used to assess self-management behaviour among patients. The PAM-13 questionnaire73 measures the patient’s self-reported knowledge, skills and confidence to cope with his/her own health with 13 questions consisting of a 4-point Likert scale (totally agree–totally disagree). The PAM-13 questionnaire is scored on a 13–52 scale; a higher score indicates higher level of patient activation. The Dutch version of the PAM-13 shows good psychometric capabilities for measuring patient activation.74
Online questionnaire for healthcare providers
Online questionnaires will be sent to all participating HCPs within the general practices at baseline and 12 months follow-up to assess changes in beliefs. A schedule of the assessments can be found in online supplemental file 7. The following will be assessed:
Professional characteristics (T0 only): geographical work location, medical profession and specialisations, number of years in active practice and practice size.
TOA questionnaire (see above) at baseline and after 12 months.
HIS extractions
Furthermore, data from the information system of participating practices will be used to assess differences in referral rates between intervention and control practices. In the Netherlands, there is a nationwide information system for GPs (HIS). Referral rates to secondary care because of knee and/or hip complaints for all patients between 50 and 75 years, including patients not participating in this study, will be extracted from electronic patient records of all participating practices at baseline and at 12 months. Thus, per practice an aggregated number (number of patients referred in the previous 6 months divided by the number of patients with knee and/or hip complaints) will be derived. These data will also be used to cross-validate self-reported healthcare use of patients.
Sample size
We base our power calculation on the BART (Behandelstrategie ARTrose) study, a cohort study in the region of Nijmegen. In this cohort study, 313 patients with KHOA were recruited by GPs.75 In the BART study, after 2 years treatment of OA was restricted to primary care in 47% of the patients.3 On basis of consensus of the authors, a minimal important difference of 20% was defined.
Assuming that treatment of 50% of the patients in the control group will be restricted to primary care whereas treatment of 70% of the patients in the experimental group will be restricted to primary care and taking intracluster correlation into account, a sample size of 240 patients is needed when α=0.05, 1−β=0.80 and intraclass correlation coefficient=0.05.76 Allowing for 20% loss to follow-up, at least 300 patients are needed to answer the research question.
(Planned) statistical analysis
All statistical analyses will be performed using STATA V.13 (www.STATA.com). Multilevel analysis will be used to account for the hierarchical nature of the data (different levels: patients, GPs and practice). Differences in the primary and secondary outcomes between the two arms (control vs intervention group) at T6, T12 and T18 will be assessed by mixed model repeated measures analyses, adjusting for the covariate treatment group (ie, control or intervention group). Direct medical costs will be computed by multiplying the cost prices with the usage frequency as reported by participants. To determine the incremental cost-effectiveness ratio differences mean costs will be divided by mean difference in quality-adjusted life-years between the two groups as assessed through the EQ-5D-5L questionnaire.
Strengths and limitations of this study
Behaviour change interventions are often poorly described, making it difficult to repeat an intervention accordingly and replicate its effects in subsequent research. This study protocol includes a systematic, theory-based approach to design an intervention to improve healthcare use among patients with OA in the Netherlands, building a toolbox of theory-based and evidence-based intervention strategies. Furthermore, the study is conducted in a real patient setting within general practices, making results sufficiently relevant to the real-world context of the Dutch OA population. However, as participants are all from the Nijmegen region, generalisability might be an issue. A further limitation might be that no blinding or allocation concealment is performed for the current trial. However, randomisation is performed via a computer-generated method to ensure minimal bias.
Trial registration
International Clinical Trial Registry Platform, trial number NL9140, registration date 23 December 2020.
Public and patient involvement
Two patient representatives (JM, SA) from the Netherlands actively collaborated with researchers in a project group during the entire iterative design process of the Becoming Active in Beating osteoarthritiS information campaign, as presented in our ‘Methods’ section. They were involved in the design of the intervention, choice for the theoretical framework, formulation of goals, choice of the applied behaviour change techniques, iterative development of the (graphical) design, content and pilot test among others.
supplementary material
Footnotes
Funding: This work is supported by the Regional Junior Researcher Grant of the Sint Maartenskliniek, Nijmegen and the Radboud University Medical Center, Nijmegen, the Netherlands (grant number: Rv819.52674), contact person: Dagmar Eleveld (Dagmar.Eleveld-Trancikova@radboudumc.nl).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-083496).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods' section for further details.
Contributor Information
Jeanne Oomen, Email: s.oomen@maartenskliniek.nl.
Henk Schers, Email: Henk.Schers@radboudumc.nl.
Enny Das, Email: h.das@let.ru.nl.
Sander Koeter, Email: s.koeter@cwz.nl.
Cornelia HM van den Ende, Email: e.vandenende@maartenskliniek.nl.
Willem JJ Assendelft, Email: pim.assendelft@radboudumc.nl.
References
- 1.Aandoeningen | volksgezondheid toekomst verkenning. https://www.vtv2018.nl/aandoeningen n.d. Available.
- 2.Smink AJ, van den Ende CHM, Vliet Vlieland TPM, et al. Effect of stepped care on health outcomes in patients with osteoarthritis: an observational study in Dutch general practice. Br J Gen Pract. 2014;64:e538–44. doi: 10.3399/bjgp14X681337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barten DJA, Smink A, Swinkels ICS, et al. Factors Associated With Referral to Secondary Care in Patients With Osteoarthritis of the Hip or Knee After Implementation of a Stepped‐Care Strategy. Arthritis Care & Research . 2017;69:216–25. doi: 10.1002/acr.22935. [DOI] [PubMed] [Google Scholar]
- 4.Smink AJ, van den Ende CHM, Vliet Vlieland TPM, et al. “Beating osteoARThritis”: development of a stepped care strategy to optimize utilization and timing of non-surgical treatment modalities for patients with hip or knee osteoarthritis. Clin Rheumatol. 2011;30:1623–9. doi: 10.1007/s10067-011-1835-x. [DOI] [PubMed] [Google Scholar]
- 5.Hofstede SN, Marang-van de Mheen PJ, Vliet Vlieland TPM, et al. Barriers and Facilitators Associated with Non-Surgical Treatment Use for Osteoarthritis Patients in Orthopaedic Practice. PLoS One. 2016;11:e0147406. doi: 10.1371/journal.pone.0147406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selten EM, Vriezekolk JE, Geenen R, et al. Reasons for Treatment Choices in Knee and Hip Osteoarthritis: A Qualitative Study. Arthritis Care & Research . 2016;68:1260–7. doi: 10.1002/acr.22841. [DOI] [PubMed] [Google Scholar]
- 7.Selten EMH, Vriezekolk JE, Schers HJ, et al. Development of the “Treatment beliefs in knee and hip OsteoArthritis (TOA)” questionnaire. BMC Musculoskelet Disord. 2017;18:402. doi: 10.1186/s12891-017-1762-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selten EMH, Vriezekolk JE, Nijhof MW, et al. Barriers Impeding the Use of Non-pharmacological, Non-surgical Care in Hip and Knee Osteoarthritis: The Views of General Practitioners, Physical Therapists, and Medical Specialists. J Clin Rheumatol . 2017;23:405–10. doi: 10.1097/RHU.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 9.Smith TO, Purdy R, Lister S, et al. Attitudes of people with osteoarthritis towards their conservative management: a systematic review and meta-ethnography. Rheumatol Int. 2014;34:299–313. doi: 10.1007/s00296-013-2905-y. [DOI] [PubMed] [Google Scholar]
- 10.Claassen AAOM, Schers HJ, Koëter S, et al. Preliminary effects of a regional approached multidisciplinary educational program on healthcare utilization in patients with hip or knee osteoarthritis: an observational study. BMC Fam Pract. 2018;19:82. doi: 10.1186/s12875-018-0769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dosanjh S, Matta JM, Bhandari M, et al. The final straw: a qualitative study to explore patient decisions to undergo total hip arthroplasty. Arch Orthop Trauma Surg. 2009;129:719–27. doi: 10.1007/s00402-008-0671-1. [DOI] [PubMed] [Google Scholar]
- 12.Petursdottir U, Arnadottir SA, Halldorsdottir S. Facilitators and barriers to exercising among people with osteoarthritis: a phenomenological study. Phys Ther. 2010;90:1014–25. doi: 10.2522/ptj.20090217. [DOI] [PubMed] [Google Scholar]
- 13.Thorstensson CA, Roos EM, Petersson IF, et al. How do middle-aged patients conceive exercise as a form of treatment for knee osteoarthritis? Disabil Rehabil. 2006;28:51–9. doi: 10.1080/09638280500163927. [DOI] [PubMed] [Google Scholar]
- 14.Snijders GF, den Broeder AA, van Riel PLCM, et al. Evidence-based tailored conservative treatment of knee and hip osteoarthritis: between knowing and doing. Scand J Rheumatol. 2011;40:225–31. doi: 10.3109/03009742.2010.530611. [DOI] [PubMed] [Google Scholar]
- 15.Lambert BL, Butin DN, Moran D, et al. Arthritis care: comparison of physicians’ and patients’ views. Semin Arthritis Rheum. 2000;30:100–10. doi: 10.1053/sarh.2000.9203. [DOI] [PubMed] [Google Scholar]
- 16.Sutton L, Jose K, Betzold A, et al. Understanding the management of osteoarthritis: A qualitative study of GPs and orthopaedic surgeons in Tasmania, Australia. Osteoarthr Cartil Open . 2021;3:100218. doi: 10.1016/j.ocarto.2021.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–72. doi: 10.1016/j.pain.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 18.Lindberg MF, Miaskowski C, Rustøen T, et al. Preoperative Pain, Symptoms, and Psychological Factors related to Higher Acute Pain Trajectories during Hospitalization for Total Knee Arthroplasty. PLoS One. 2016;11:e0161681. doi: 10.1371/journal.pone.0161681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quintana JM, Escobar A, Arostegui I, et al. Health-related quality of life and appropriateness of knee or hip joint replacement. Arch Intern Med. 2006;166:220–6. doi: 10.1001/archinte.166.2.220. [DOI] [PubMed] [Google Scholar]
- 20.Ghomrawi HMK, Mushlin AI, Kang R, et al. Examining Timeliness of Total Knee Replacement Among Patients with Knee Osteoarthritis in the U.S.: Results from the OAI and MOST Longitudinal Cohorts. J Bone Joint Surg Am. 2020;102:468–76. doi: 10.2106/JBJS.19.00432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riddle DL, Perera RA, Jiranek WA, et al. Using surgical appropriateness criteria to examine outcomes of total knee arthroplasty in a United States sample. Arthritis Care Res (Hoboken) 2015;67:349–57. doi: 10.1002/acr.22428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parvizi J, Sullivan TA, Trousdale RT, et al. Thirty-Day Mortality After Total Knee Arthroplasty. J Bone Joint Surg Am Vol. 2001;83:1157–61. doi: 10.2106/00004623-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Haskins R, Henderson JM, Bogduk N. Health professional consultation and use of conservative management strategies in patients with knee or hip osteoarthritis awaiting orthopaedic consultation. Aust J Prim Health. 2014;20:305–10. doi: 10.1071/PY13064. [DOI] [PubMed] [Google Scholar]
- 24.Okwera A, May S. Views of general practitioners toward physiotherapy management of osteoarthritis-a qualitative study. Physiother Theory Pract. 2019;35:940–6. doi: 10.1080/09593985.2018.1459987. [DOI] [PubMed] [Google Scholar]
- 25.Alami S, Boutron I, Desjeux D, et al. Patients’ and practitioners’ views of knee osteoarthritis and its management: a qualitative interview study. PLoS ONE. 2011;6:e19634. doi: 10.1371/journal.pone.0019634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpenter DM, DeVellis RF, Fisher EB, et al. The effect of conflicting medication information and physician support on medication adherence for chronically ill patients. Patient Educ Couns. 2010;81:169–76. doi: 10.1016/j.pec.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carpenter DM, Elstad EA, Blalock SJ, et al. Conflicting medication information: prevalence, sources, and relationship to medication adherence. J Health Commun. 2014;19:67–81. doi: 10.1080/10810730.2013.798380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Federatie medisch specialisten: conservatieve behandeling van artrose in heup of knie 2012-2013
- 29.Panagioti M, Richardson G, Small N, et al. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14:356.:356. doi: 10.1186/1472-6963-14-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kellogg W. Logic Model Development Guide. 2004. Michigan: WK Kellogg Foundation; 2017. [Google Scholar]
- 31.O’Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9:e029954. doi: 10.1136/bmjopen-2019-029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 34.Johnston M, Carey RN, Connell Bohlen LE, et al. Development of an online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus. Transl Behav Med. 2021;11:1049–65. doi: 10.1093/tbm/ibaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Keefe DJ, Jensen JD. The Relative Persuasiveness of Gain-Framed and Loss-Framed Messages for Encouraging Disease Detection Behaviors: A Meta-Analytic Review. J Commun. 2009;59:296–316. doi: 10.1111/j.1460-2466.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 36.O’Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Health Commun. 2007;12:623–44. doi: 10.1080/10810730701615198. [DOI] [PubMed] [Google Scholar]
- 37.Green M, Brock T. In the Mind’s Eye: Transportation-Imagery Model of Narrative Persuasion. In: Narrative Impact: Social and Cognitive Foundations. edn. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2002. pp. 315–41. [Google Scholar]
- 38.Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol. 2000;79:701–21. doi: 10.1037//0022-3514.79.5.701. [DOI] [PubMed] [Google Scholar]
- 39.Tanaka K. Advertising Language: A Pragmatic Approach to Advertisements in Britain And. Japan: Routledge; 1994. [Google Scholar]
- 40.Tanaka K. The pun in advertising: A pragmatic approach. Lingua. 1992;87:91–102. doi: 10.1016/0024-3841(92)90027-G. [DOI] [Google Scholar]
- 41.Barker F, Atkins L, de Lusignan S. Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. Int J Audiol. 2016;55 Suppl 3:S90–8. doi: 10.3109/14992027.2015.1120894. [DOI] [PubMed] [Google Scholar]
- 42.Chou L, Ellis L, Papandony M, et al. Patients’ perceived needs of osteoarthritis health information: A systematic scoping review. PLoS One. 2018;13:e0195489. doi: 10.1371/journal.pone.0195489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zajonc RB. Attitudinal effects of mere exposure. J Pers Soc Psychol. 1968;9:1–27. doi: 10.1037/h0025848. [DOI] [Google Scholar]
- 44.Oomen JMH, Ende CH van den, Schers HJ, et al. BABS on a mission: an experimental study on the effects of message framing and the use of a patient testimonial on intentions of osteoarthritis patients to adhere to treatment advice. In Review. doi: 10.21203/rs.3.rs-2701276/v1. Preprint. [DOI]
- 45.McGlone MS, Tofighbakhsh J. Birds of a feather flock conjointly (?): rhyme as reason in aphorisms. Psychol Sci. 2000;11:424–8. doi: 10.1111/1467-9280.00282. [DOI] [PubMed] [Google Scholar]
- 46.Laplante C, Smith S, Kotowski M, et al. An Initial Investigation into Naturally Occurring Loss- and Gain-Framed Memorable Breast Cancer Messages. Commun Q. 2012;60:1–16. doi: 10.1080/01463373.2012.642269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jones LW, Sinclair RC, Courneya KS. The Effects of Source Credibility and Message Framing on Exercise Intentions, Behaviors, and Attitudes: An Integration of the Elaboration Likelihood Model and Prospect Theory 1. J Applied Social Pyschol. 2003;33:179–96. doi: 10.1111/j.1559-1816.2003.tb02078.x. [DOI] [Google Scholar]
- 48.Bates BR, Romina S, Ahmed R, et al. The effect of source credibility on consumers’ perceptions of the quality of health information on the Internet. Med Inform Internet Med. 2006;31:45–52. doi: 10.1080/14639230600552601. [DOI] [PubMed] [Google Scholar]
- 49.Tormala ZL, Briñol P, Petty RE. Multiple Roles for Source Credibility Under High Elaboration: It’s all in the Timing. Soc Cogn. 2007;25:536–52. doi: 10.1521/soco.2007.25.4.536. [DOI] [Google Scholar]
- 50.Jerant A, Kravitz RL, Azari R, et al. Training residents to employ self-efficacy-enhancing interviewing techniques: randomized controlled trial of a standardized patient intervention. J Gen Intern Med. 2009;24:606–13. doi: 10.1007/s11606-009-0946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aljasem LI, Peyrot M, Wissow L, et al. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 52.Brus H, van de Laar M, Taal E, et al. Determinants of compliance with medication in patients with rheumatoid arthritis: the importance of self-efficacy expectations. Patient Educ Couns. 1999;36:57–64. doi: 10.1016/s0738-3991(98)00087-1. [DOI] [PubMed] [Google Scholar]
- 53.Friedman LC, Nelson DV, Webb JA, et al. Dispositional optimism, self-efficacy, and health beliefs as predictors of breast self-examination. Am J Prev Med. 1994;10:130–5. [PubMed] [Google Scholar]
- 54.Mahoney CA, Thombs DL, Ford OJ. Health belief and self-efficacy models: their utility in explaining college student condom use. AIDS Educ Prev. 1995;7:32–49. [PubMed] [Google Scholar]
- 55.Hawley ST, Zikmund-Fisher B, Ubel P, et al. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns. 2008;73:448–55. doi: 10.1016/j.pec.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 56.Houts PS, Doak CC, Doak LG, et al. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173–90. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 57.Arcia A, Suero-Tejeda N, Bales ME, et al. Sometimes more is more: iterative participatory design of infographics for engagement of community members with varying levels of health literacy. J Am Med Inform Assoc. 2016;23:174–83. doi: 10.1093/jamia/ocv079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carey RN, Connell LE, Johnston M, et al. Behavior Change Techniques and Their Mechanisms of Action: A Synthesis of Links Described in Published Intervention Literature. Ann Behav Med. 2018;53:693–707. doi: 10.1093/abm/kay078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smelt AFH, van der Weele GM, Blom JW, et al. How usual is usual care in pragmatic intervention studies in primary care? An overview of recent trials. Br J Gen Pract . 2010;60:e305–18. doi: 10.3399/bjgp10X514819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lorenz E, Gabrysch S. Covariate-constrained Randomization Routine for Achieving Baseline Balance in Cluster-randomized Trials. The Stata Journal: Promoting communications on statistics and Stata. 2017;17:503–10. doi: 10.1177/1536867X1701700214. [DOI] [Google Scholar]
- 61.Vragenlijsten gezondheidsenquête vanaf. 2014. https://www.cbs.nl/nl-nl/onze-diensten/methoden/onderzoeksomschrijvingen/aanvullende-onderzoeksbeschrijvingen/vragenlijsten-gezondheidsenquete-vanaf-2014 Available.
- 62.Rabin R, Gudex C, Selai C, et al. From translation to version management: a history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. V Health. 2014;17:70–6. doi: 10.1016/j.jval.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 63.Binkley JM, Stratford PW, Lott SA, et al. The Lower Extremity Functional Scale (LEFS): Scale Development, Measurement Properties, and Clinical Application. Phys Ther. 1999;79:371–83. [PubMed] [Google Scholar]
- 64.Hoogeboom TJ, de Bie RA, den Broeder AA, et al. The Dutch Lower Extremity Functional Scale was highly reliable, valid and responsive in individuals with hip/knee osteoarthritis: a validation study. BMC Musculoskelet Disord. 2012;13:117. doi: 10.1186/1471-2474-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kraaimaat FW, Evers AWM. Pain-coping strategies in chronic pain patients: psychometric characteristics of the pain-coping inventory (PCI) Int J Behav Med. 2003;10:343–63. doi: 10.1207/s15327558ijbm1004_5. [DOI] [PubMed] [Google Scholar]
- 66.van Poppel M, Chin A Paw M, Mechelen W. Reproduceerbaarheid en validiteit van de Nederlandse versie van de International Physical Activity Questionnaire (IPAQ) Tijdschr voor Gezondheidswetenschappen (TSG) 2004;7 [Google Scholar]
- 67.Oomen JMH, Peters YAS, van den Ende CH, et al. Quality of knee osteoarthritis care in the Netherlands: a survey on the perspective of people with osteoarthritis. BMC Health Serv Res. 2022;22:631. doi: 10.1186/s12913-022-08014-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kanters TA, Bouwmans CAM, van der Linden N, et al. Update of the Dutch manual for costing studies in health care. PLoS One . 2017;12:e0187477. doi: 10.1371/journal.pone.0187477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Østerås N, Garratt A, Grotle M, et al. Patient-reported quality of care for osteoarthritis: development and testing of the osteoarthritis quality indicator questionnaire. Arthritis Care Res (Hoboken) 2013;65:1043–51. doi: 10.1002/acr.21976. [DOI] [PubMed] [Google Scholar]
- 70.Pelle T, Bevers K, van der Palen J, et al. Development and evaluation of a tailored e-self-management intervention (dr. Bart app) for knee and/or hip osteoarthritis: study protocol. BMC Musculoskelet Disord. 2019;20:398. doi: 10.1186/s12891-019-2768-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Overzicht van alle cqi-vragenlijsten. https://www.zorginzicht.nl/ontwikkeltools/ontwikkelen/overzicht-van-alle-cqi-vragenlijsten n.d. Available.
- 72.Delnoij D, Hendriks M. De CQ-index: het meten van klantervaringen in de zorg. TVGW. 2008;86:440–6. doi: 10.1007/BF03082141. [DOI] [Google Scholar]
- 73.Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rademakers J, Nijman J, van der Hoek L, et al. Measuring patient activation in The Netherlands: translation and validation of the American short form Patient Activation Measure (PAM13) BMC Public Health. 2012;12:577. doi: 10.1186/1471-2458-12-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smink AJ, Dekker J, Vliet Vlieland TPM, et al. Health care use of patients with osteoarthritis of the hip or knee after implementation of a stepped-care strategy: an observational study. Arthritis Care Res (Hoboken) 2014;66:817–27. doi: 10.1002/acr.22222. [DOI] [PubMed] [Google Scholar]
- 76.Hemming K, Eldridge S, Forbes G, et al. How to design efficient cluster randomised trials. BMJ . 2017;358:j3064. doi: 10.1136/bmj.j3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Egerton T, Nelligan RK, Setchell J, et al. General practitioners’ views on managing knee osteoarthritis: a thematic analysis of factors influencing clinical practice guideline implementation in primary care. BMC Rheumatol . 2018;2:30.:30. doi: 10.1186/s41927-018-0037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Spitaels D, Vankrunkelsven P, Desfosses J, et al. Barriers for guideline adherence in knee osteoarthritis care: A qualitative study from the patients’ perspective. J Eval Clin Pract. 2017;23:165–72. doi: 10.1111/jep.12660. [DOI] [PubMed] [Google Scholar]
- 79.Allison K, Setchell J, Egerton T, et al. In Theory, Yes; in Practice, Uncertain: A Qualitative Study Exploring Physical Therapists’ Attitudes Toward Their Roles in Weight Management for People With Knee Osteoarthritis. Phys Ther. 2019;99:601–11. doi: 10.1093/ptj/pzz011. [DOI] [PubMed] [Google Scholar]
- 80.Allison K, Delany C, Setchell J, et al. A qualitative study exploring the views of individuals with knee osteoarthritis on the role of physiotherapists in weight management: A complex issue requiring a sophisticated skill set. Musculoskeletal Care . 2019;17:206–14. doi: 10.1002/msc.1391. [DOI] [PubMed] [Google Scholar]
- 81.Selten EMH, Vriezekolk JE, Nijhof MW, et al. Barriers Impeding the Use of Non-pharmacological, Non-surgical Care in Hip and Knee Osteoarthritis: The Views of General Practitioners, Physical Therapists, and Medical Specialists. JCR J Clin Rheumatol. 2017;23:405–10. doi: 10.1097/RHU.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 82.Holden MA, Nicholls EE, Young J, et al. UK‐based physical therapists’ attitudes and beliefs regarding exercise and knee osteoarthritis: Findings from a mixed‐methods study. Arthritis & Rheumatism . 2009;61:1511–21. doi: 10.1002/art.24829. [DOI] [PubMed] [Google Scholar]
- 83.MacKay C, Hawker GA, Jaglal SB. Qualitative study exploring the factors influencing physical therapy management of early knee osteoarthritis in Canada. BMJ Open. 2018;8:e023457. doi: 10.1136/bmjopen-2018-023457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Selten EM, Vriezekolk JE, Geenen R, et al. Reasons for treatment choices in knee and hip osteoarthritis: a qualitative study. Osteoarthr Cartil. 2016;24:S489. doi: 10.1016/j.joca.2016.01.897. [DOI] [PubMed] [Google Scholar]
- 85.O’Brien P, Bunzli S, Ayton D, et al. What are the patient factors that impact on decisions to progress to total knee replacement? A qualitative study involving patients with knee osteoarthritis. BMJ Open. 2019;9:e031310. doi: 10.1136/bmjopen-2019-031310. [DOI] [PMC free article] [PubMed] [Google Scholar]