Abstract
ABSTRACT
Objectives
This study aims to evaluate and compare health outcomes and costs between home hospitalisation and traditional hospitalisation for three common diagnoses—cellulitis, urinary tract infection (UTI) and pneumonia.
Design
A retrospective cohort study.
Setting
Primary care, nationwide.
Participants
1311 patients in home hospitalisation and 992 in traditional hospitalisation.
Interventions
The primary intervention is home hospitalisation, compared with traditional hospitalisation. The intervention was performed according to medical considerations by a specialised team, and this study was done retrospectively to evaluate it.
Primary and secondary outcome measures
Primary measures included healthcare costs, length of hospitalisation, referrals for further medical services and mortality.
Results
Costs of home hospitalisation were lower compared with traditional hospitalisation (6056 vs 9619 NIS for pneumonia, 6011 vs 9767 NIS for cellulitis, 6466 vs 8552 NIS for UTI and p value<0.05). The length of home hospitalisations was shorter for pneumonia and cellulitis (5.01 vs 6.05 days, p value 0.001 and 5.3 vs 6.1 days, p value<0.001, respectively). Likewise, for pneumonia and cellulitis, home-hospitalised patients had fewer ED referrals 30 days after discharge (13.7% vs 24%, p value<0.001 and 13.5% vs 19.8%, p value 0.002, respectively). No differences were found in recurrent hospitalisation and mortality 7 and 30 days after discharge.
Conclusions
Primary care physicians should consider home hospitalisation for these diagnoses as an alternative to traditional hospitalisation. Policymakers should encourage Primary care physicians to use home hospitalisation, as it has financial advantages and better health outcomes.
Keywords: Hospitalization, Health Services, Primary Health Care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Patients were designated for home hospitalisation based on clinical presentation by specialised physicians; so, we cannot assume complete homogeneity.
Only infectious causes of hospitalisation were examined, completely excluding other common causes.
We were unable to conduct matching based on the clinical state of patients at the beginning of hospitalisation.
Specific medical complications and outcomes were not examined, limiting insights.
Choosing specific diagnoses and comparing results between them can help establish the benefits and limitations of home hospitalisation for each.
Introduction
The challenges posed by increased life expectancy, ageing populations and chronic morbidity have become pressing concerns for healthcare systems globally. Simultaneously, there is a documented reduction in the number of hospital beds, facilities and resources.1 Hospital care and services constitute the single largest expenditure in healthcare2 and are significantly higher than community healthcare services, where comparable.2 In addition to their cost, hospitalisations pose a set of unique risks to patients, notably hospital-acquired complications (HACs).3 Those include nosocomial infections, falls, functional decline and cognitive deterioration.4 Addressing these challenges is imperative in mitigating the associated medical and financial risks. One such suggested solution is home hospitalisation, an at-home therapeutic framework for patients with relatively mild conditions. Home hospitalisation is usually defined as providing acute, at-home, short-term, moderately complex medical interventions—that would have otherwise been provided in a hospital environment. This may be an alternative to a full hospitalisation5,8 or to facilitate early discharge, shortening hospital stay length and reducing associated risks and costs.9 10 For the sake of this study, we have defined ‘home hospitalisation’ as a time-limited medical treatment for acute conditions by a professional team at the patient’s home. Naturally, many patients and conditions are unsuitable for this solution. Still, as it is a relatively newly applied concept, the characteristics of patients and conditions likely to benefit from it are still being explored.
Leff et al11 were among the pioneers looking into home hospitalisation’s potential feasibility and efficacy. In their prospective study, 455 elderly patients were treated in a home hospitalisation care model. Results showed that quality standards in the home hospitalisation model were met at rates similar to those of acute hospital care. Other early studies showed promise in alleviating the burden of hospitalisation both financially and medically. A systematic review of alternatives to hospitalisation, including home hospitalisation, suggests they are either superior or non-inferior to traditional hospitalisation in terms of medical outcomes and patient satisfaction for some acute conditions.12 Moreover, a review of 10 randomised controlled trials of home hospitalisation models revealed a significant reduction in mortality after 3 and 6 months.13 The same review reported higher rates of patient satisfaction associated with home hospitalisation. Finally, another study comparing directly between hospitalised and home-hospitalised patients for acute and post-acute transitional care reported significantly lower rates of readmissions and emergency department (ED) revisits, as well as significantly shorter stays for home-hospitalised patients.14
While recently gaining traction, some healthcare systems have been operating hospital-at-home programmes for years and decades, notably in the USA,15 in Australia11 and as ’virtual ward’ models in the UK.16 These programmes vary widely; some involve physical visits by medical staff,11 while others rely on virtual or online communications.10 15
This study focuses on a home hospitalisation model developed by Maccabi Health Services (MHS), Israel’s second-largest healthcare maintenance organisation with over 2.6 million members. MHS is a community-based healthcare provider that historically provided little hospitalisation services directly. The model at the heart of this study is not local but nationwide and is based primarily on community healthcare resources in an organised and centralised fashion. This makes this model unique, as most programmes worldwide are hospital-based and provide services only to the area in the vicinity of the hospital. The aim of this study was to establish the benefits and limitations of home hospitalisations in the context of three specific diagnoses—cellulitis, urinary tract infection (UTI) and pneumonia. These are three common diagnoses that often lead to hospitalisation, especially in older people.
Methods
Study design and setting
The MHS home hospitalisation service has been deployed since 2017 and has expanded gradually. The service is offered to patients over 18 years old for the following conditions: pneumonia, UTIs, cellulitis or erysipelas, wound infection or ulcer, congestive heart failure exacerbation, chronic obstructive pulmonary disease exacerbation, asthma exacerbation, dehydration, electrolytic imbalance and acute pain management. Certain eligibility criteria are in place for patients referred to home hospitalisation to ensure their safety, including being haemodynamically stable and having another person at home. Those deemed unsuitable for home hospitalisation by these criteria are referred directly to the nearest ED or specialised unit. On referral and subsequent receipt of a comprehensive explanation, patients are assigned to a team including a nurse and a physician conducting an admission visit within 4 hours of the referral. Patients are given detailed explanations about the service and the expected care and are required to provide informed consent before proceeding with the service.
Participants
For this retrospective cohort study, we collected data from patients’ home hospitalised for cellulitis, UTI and pneumonia between 1 January 2019 and 31 December 2020. Participants were excluded if they were hospitalised or home-hospitalised 30 days prior, unless referred to home hospitalisation as a direct continuation of hospitalisation. To each of those, we matched a control patient (1:1 ratio) based on gender, age group, primary diagnosis, time of hospitalisation (by quartiles and years) and the hospital they would have been admitted to (based on previous hospitalisations and place of residence). It should be noted that the control group consisted only of patients hospitalised in internal medicine wards and excluded intensive care and COVID-19-specific wards.
Variables
For both the study and the control groups, we collected sociodemographic data, comorbidities, lengths of hospitalisation and rehospitalisation within 30 days, ED referrals (within 7 and 30 days), rehospitalisations (within 7 and 30 days) and costs associated with the hospitalisation and mortality (within 7 and 30 days).
Statistical analysis
To evaluate the matching result, we compared the home hospitalisation cohort before and after matching and compared them to the matched controls using χ2 and an independent t-test. We compared the mean length of hospitalisation and mean cost of hospitalisation between the test and control-matched groups using a paired t-test. Medians of said variables were compared using a Wilcoxon-matched paired signed-rank test. A negative binomial with a log-rank regression model was performed and presented as an adjusted exponent (B) and 95% CI. ED visits, rehospitalisation and death (within 7 and 30 days) were compared using χ2 tests. A multivariate binary logistic regression model was performed and presented as an adjusted OR and 95% CI. Finally, regression models were performed using the ENTER method, controlling for the following variables: hospitalisation type (whether the patient was home hospitalised throughout the entire course of the disease or was referred home after a hospital stay), mean monthly expenses in the year prior to hospitalisation and SES and comorbidities. All statistical analyses were performed with the SPSS V.25 (IBM SPSS Statistics).
Ethical consideration
The ethical committee of Maccabi Healthcare Services approved study #0044–19-MHS in August 2020. The IRB waived informed consent due to the study design.
Patient and public involvement statement
There was no patient or public involvement in this study.
Results
Participants
Between 1 January 2019 and 31 December 2020, 1794 patients were home hospitalised for the three above-mentioned diagnoses; of these, 1470 (82%) were home hospitalised as an alternative to a hospital stay, and 324 (18%) were home hospitalised following a hospital stay to shorten it.
Descriptive data
Of the aforementioned participants, cases of repeated hospitalisations and home hospitalisations in 30 days prior were removed—as were cases positive for COVID-19 during the preceding 30 days—resulting in 1311 individuals, of whom 1058 (81%) were exclusively home hospitalised, and 253 (19%) were home hospitalised after a hospital stay. Three-quarters (76%) of these patients were successfully matched, resulting in a final case sample of 992, of whom 792 (80%) were exclusively home hospitalised, and 200 (20%) were home hospitalised after a hospital stay. Most patients in the case sample were diagnosed with cellulitis (40%), whereas pneumonia and UTI accounted for 30% each. Most patients (40%) were over 80 years of age, followed closely (38%) by the 60–80 age group. Patients aged 41–60 constituted 16% of the sample, and those younger than 40 were only 6%. Mean age was 71.6 (SD 17.2). More than half of the patients in this sample were male (54%). The median number of comorbidities per patient was 3; 52% had 3 and 5 comorbidities, 8% had over 6, 16% had 1–2 and 14% had none of the comorbidities we recorded. Most of the patients in this group (53%) were associated with the medium SES group (5–7 in the Israeli Bureau for Statistics categorisation), whereas 27% belonged to the high SES group (8–10) and 20% with the low SES group (1–4). The average monthly cost of medical expenses associated with each patient in the year prior to hospitalisation was 3556.3 New Israeli Shekel (SD 6399.7). 38% of the patients needed help with activities of daily living (ADL). The full characteristics of both the case and the control samples are presented in table 1. While the samples are matched, differences between the groups are noted in the rate of ADL assistance requirement.
Table 1. Characteristics of patients in home hospitalisation (cases) versus patients in traditional hospitalisation (control).
| Home hospitalisation (cases) (n=1311) | Hospitalisation (controls) (n=992) | |
| Gender | ||
| Male | 53% | 54% |
| Female | 47% | 46% |
| Diagnosis | ||
| Cellulitis | 43% | 40% |
| UTI | 31% | 30% |
| Pneumonia | 26% | 30% |
| Age groups | ||
| Under 40 | 7% | 6% |
| 41–60 | 17% | 16% |
| 60–80 | 37% | 38% |
| Over 81 | 39% | 40% |
UTIurinary tract infection
Outcome data
For patients diagnosed with cellulitis, the length of hospitalisation was at least 10% shorter for home-hospitalised patients (figure 1). Likewise, the overall number of hospitalisation days within 30 days of admission was at least 15% shorter for patients in the home hospitalisation group (both statistically significant, p values 0.001). Home-hospitalised patients had fewer referrals to the ED within the 30 days following discharge (OR=0.529, p value<0.001) (figure 2). Rehospitalisation rates at the 7-day and 30-day intervals did not demonstrate statistical significance (p values 0.582 and 0.594, ORs 0.778 and 1.149, respectively). On average, home hospitalisation costs were 30% lower for both initial hospitalisation (figure 3) and the 30 days following discharge (p value<0.001). We found no statistically significant difference in mortality rate between the samples for patients diagnosed with cellulitis. The full analysis for cellulitis is presented in table 2.
Figure 1. Comparison of hospitalisation duration by diagnosis. UTI, urinary tract infection.
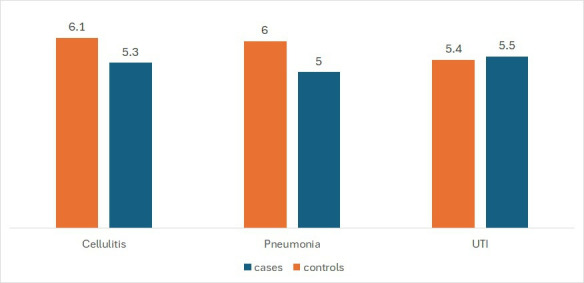
Figure 2. Comparison of recurrent admissions to the emergency department, 7 and 30 days after discharge. UTI, urinary tract infection.
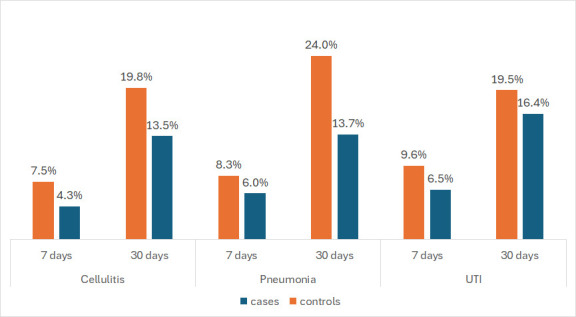
Figure 3. Costs of home hospitalisation compared with traditional hospitalisation. UTI, urinary tract infection.
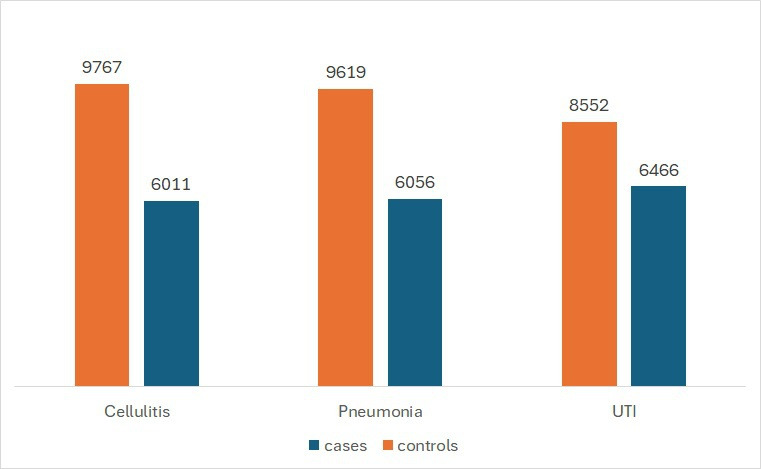
Table 2. Outcomes of patients with cellulitis, home hospitalisation (cases) versus traditional hospitalisation (controls).
| Cases | Controls | Cl | Significance | |
| Mean length of hospitalisation in days (SD) | 5.3 (4.4) | 6.1 (6.8) | 0.664–0.903 | 0.001 |
| ED visits | ||||
| 7 days | 4.3% | 7.5% | 0.218–0.844 | 0.014 |
| 30 days | 13.5% | 19.8% | 0.351–0.796 | 0.002 |
| Rehospitalisations | ||||
| 7 days | 2.3% | 3% | 0.318–1.904 | 0.582 |
| 30 days | 9.3% | 8% | 0.690–1.913 | 0.594 |
| Average total length of hospitalisations (SD) | 6.2 (6.2) | 7.2 (8.3) | 0.632–0.857 | <0.001 |
| Mean costs (in NIS) | ||||
| Index hospitalisation (SD) | 6011 (6718) | 9767 (10761) | 0.538–0.716 | <0.001 |
| Total (SD) | 7366 (9548) | 11 401 (13218) | 0.554–0.736 | <0.001 |
| Mortality | ||||
| 7 days | 1% | 1% | 0.216–4.001 | 0.923 |
| 30 days | 2% | 2.8% | 0.237–1.6 | 0.320 |
EDemergency departmentNISNew Israeli Shekel
For patients diagnosed with pneumonia, the length of hospitalisation was at least 16% shorter at initial hospitalisation and at least 30% shorter in the 30 days after release for home-hospitalised patients (p values<0.001) (figure 1). Home-hospitalised patients had fewer referrals to the ED within the 30 days following discharge (OR=0.208 and p value<0.001) (figure 2). There were no statistically significant differences in the rate of rehospitalisations for 7 days and 30 days, as well as in ED referrals in the 7 days after discharge (ORs 2.207, 0.847 and 0.554; p values 0.146, 0.570 and 0.086, respectively). On average, home hospitalisation costs were 30% lower for both initial hospitalisation and the 30 days following release (p value for both <0.001) (figure 3). We found no statistically significant difference in mortality rate between the samples for patients diagnosed with pneumonia. The full analysis for pneumonia is presented in table 3.
Table 3. Outcomes of patients with pneumonia, home hospitalisation (cases) versus traditional hospitalisation (controls).
| Cases | Controls | Cl | Significance | |
| Mean length of hospitalisation in days (SD) | 5.01 (4.6) | 6.05 (7.1) | 0.588–0.841 | <0.001 |
| ED visits | ||||
| 7 days | 6% | 8.3% | 0.282–1.087 | 0.086 |
| 30 days | 13.7% | 24% | 0.232–0.594 | <0.001 |
| Rehospitalisations | ||||
| 7 days | 4.3% | 1.7% | 0.759–6.420 | 0.146 |
| 30 days | 9% | 9.3% | 0.478–1.503 | 0.570 |
| Average total length of hospitalisations (SD) | 5.7 (5.1) | 7.1 (8.8) | 0.479–0.682 | <0.001 |
| Mean costs (in NIS) | ||||
| Index hospitalisation (SD) | 6056 (7148) | 9619 (11326) | 0.513–0.714 | <0.001 |
| Total (SD) | 6869 (8084) | 11 326 (13984) | 0.498–0.693 | <0.001 |
| Mortality | ||||
| 7 days | 3.3% | 5.3% | 0.231–1.227 | 0.139 |
| 30 days | 8.3% | 10.3% | 0.408–1.271 | 0.258 |
EDemergency departmentNISNew Israeli Shekel
For patients diagnosed with UTI, we report no statistically significant variation in length of hospitalisation, both initially and in the 30 days following discharge (p values 0.292 and 0.182, respectively) (figure 1). We were also unable to detect a difference in ED referrals (for the first 7 days, p value 0.128; for 30 days, p value 0.161) (figure 2) and in rehospitalisation rates (for the first 7 days, OR 0.786 and p value 0.605; for 30 days, OR 1.199 and p value 0.517). Costs for home hospitalisation were, on average, 10% lower for initial hospitalisation (p value<0.001) (figure 3). We found no statistically significant difference in mortality rate between the samples for patients diagnosed with cellulitis. The full analysis for UTI is presented in table 4.
Table 4. Outcomes of patients with UTI, home hospitalisation (cases) versus traditional hospitalisation (controls).
| Cases | Controls | Cl | Significance | |
| Mean length of hospitalisation in days (SD) | 5.5 (4.1) | 5.4 (5.2) | 0.755–1.09 | 0.292 |
| ED visits | ||||
| 7 days | 6.5% | 9.6% | 0.329–1.151 | 0.128 |
| 30 days | 16.4% | 19.5% | 0.461–1.137 | 0.161 |
| Rehospitalisations | ||||
| 7 days | 3.1% | 3.8% | 0.316–1.955 | 0.605 |
| 30 days | 10.9% | 9.6% | 0.693–2.074 | 0.517 |
| Average total length of hospitalisations (SD) | 6.3 (5.6) | 6.1 (6.5) | 0.737–1.060 | 0.182 |
| Mean costs (in NIS) | ||||
| Index hospitalisation (SD) | 6466 (6351) | 8552 (8203) | 0.645–0.902 | 0.002 |
| Total (SD) | 7741 (8631) | 9649 (10 257) | 0.691–0.969 | 0.020 |
| Mortality | ||||
| 7 days | 2% | 2.7% | 0.262–2.405 | 0.682 |
| 30 days | 4.8% | 7.8% | 0.271–1.119 | 0.099 |
EDemergency departmentUTIurinary tract infection
Discussion
Main results
This retrospective cohort study aimed to assess the potential benefits and limitations of the community-based home hospitalisation model by exploring three common diagnoses—cellulitis, pneumonia and UTI. These diagnoses comprised approximately half of all home hospitalisation cases during the study period. All three can be serious and life-threatening, especially in older people, and are common causes of hospitalisations.
Costs for all diagnoses were reduced in home hospitalisation. In two of the three diagnoses (cellulitis and pneumonia), we demonstrated that the length of hospitalisation was significantly shorter in home-hospitalised patients. Fewer ED referrals were documented for the same diagnoses compared with traditional hospitalisations. We did not find significant differences in hospitalisations or mortality 7 and 30 days after discharge.
Interpretation
Our findings, particularly the shortened lengths of hospitalisation, appear to be supported by existing literature on home hospitalisations. Reduced length of hospitalisation has been noted repeatedly, as were reduced readmissions.17,19 In line with our findings, an RCT from the USA reported that home hospitalisation for acute patients is characterised by reduced costs, fewer readmissions within 30 days, and fewer tests and studies conducted.18 The same study found that patients at home were more mobile18; mobility in hospitalisation is associated with better results.20 An examination of research on home care for acutely ill patients has elucidated additional advantages, including improvements in sleep, enhanced physical activity and mitigation of administrative challenges.21 Notably, patients express higher satisfaction and receptiveness towards home hospitalisation, with a considerable proportion expressing a preference for it over conventional alternatives.11 19 22 Subsequent investigations should explore the impact of these benefits on patient outcomes and the healing process. However, it is crucial to acknowledge the variability of such findings across diverse populations and studies, with some studies reporting no discernible benefits in terms of mortality and median length of hospitalisation associated with home hospitalisation.23,25
Our choice of diagnoses to examine is based on their prevalence, burden to the healthcare system and potential complications. In our study, patients with cellulitis had lower costs, shorter hospitalisations and fewer recurrent ED visits after discharge compared with traditional hospitalisation. Past studies suggest patients with this condition prefer at-home care,26 and that at-home treatment is feasible and safe for many.27,29 While studied less often, perhaps due to the higher rates of complications and severity, at-home treatment of pneumonia for suitable patients can be safe and effective,30 31 as is the case for UTI.32 33
The conclusions from this study are applicable in two aspects. This study establishes the feasibility and efficacy of home hospitalisation, particularly in community and national settings. This study demonstrates that this system is not only possible but is likely to be more cost-effective and with better health-related outcomes. In addition, this study further established the benefit of this model for specific diagnoses. Elderly patients with comorbidities constitute the majority of our sample; coincidently, these are the same type of patients physicians tend to be most apprehensive to discharge or choose not to hospitalise. Interestingly, these are also among the patients most vulnerable to HACs. The second application of this study’s findings is clinical and more direct. Having the option to refer patients to home hospitalisation and being aware of its benefits can help clinicians make better and more informed decisions. Improving health outcomes at a lower cost to healthcare systems appears to be a potential result of educated deployment of this model.
Strengths and limitations
This study has several strengths, rendering it particularly applicable and relevant. First, this study uses a large and comprehensive dataset over relatively extended time periods; this benefit is directly derived from MHS’ position as a primary care organisation. Second, this study aimed explicitly to identify the relevance of home hospitalisation in the context of specific diagnoses. This increases our knowledge and understanding of the proper use of home hospitalisation models. Third, this study looks at both the financial costs and medical benefits of the model; those aspects are explored concurrently to view this solution realistically, considering the practical constraints inherent in addressing the needs of both patients and the healthcare system.
Along with the strengths mentioned above, this study has several limitations that should be considered. First, the model in this study is community-based. At its heart, this is not a problematic feature but a major advantage of the model. It is efficient and dynamic because MHS is able to provide care at home through an already deployed infrastructure of assigned professionals. Yet, this feature may hinder the reproducibility of this model and limit the use of its conclusions across other systems. One should consider that this study was conducted in Israel, where healthcare is highly accessible, and community-based healthcare is the backbone of health services. Second, patients in this sample were deemed suitable for home hospitalisation by a highly experienced team after a referral from a primary care physician—we cannot assume the health outcomes would be identical under different circumstances. Unlike the referring physicians, we are not privy to the severity and presentation of the patient’s condition prior to care; this also prevents us from matching disease severity beyond what is indicated by the inclusion criteria. Third, we looked only into three infectious disease diagnoses, rendering this study not directly applicable to other common causes of hospitalisation. Fourth, we did not examine the satisfaction of patients, which is an important variable in this case. We hope future efforts help fill this gap and advance our understanding of home hospitalisation models' potential benefits and limitations.
Implications
The findings of this study provide insight into employing alternatives to traditional hospitalisation in a manner that benefits both healthcare systems and patients. As hospitals become overcrowded and burdened, the healthcare system should consider and develop community-based alternatives. Patients with infectious diseases such as pneumonia, cellulitis and UTI could be considered for home hospitalisation, which can benefit them and the healthcare system.
Conclusions
In this retrospective cohort study, we found that home hospitalisation for pneumonia, cellulitis and UTI is associated with lower costs compared with traditional hospitalisation. The length of home hospitalisation and recurrent admission to the ED after discharge were lower for pneumonia and cellulitis. We did not find a significant difference in rehospitalisation or mortality. PCPs should consider home hospitalisation for these diagnoses as an alternative to traditional hospitalisation. Policymakers should encourage PCPs to use home hospitalisation, when appropriate, as it has financial advantages in addition to better health outcomes. Future research should focus on longer follow-up periods and different diagnoses suitable for home hospitalisation.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-085347).
Data availability free text: The data is not available due to ethical restrictions.
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Ilan Yehoshua, Email: yehoshua_i@mac.org.il.
Sharon Baruch Gez, Email: gezsharon@gmail.com.
Bar Cohen, Email: cobar@post.bgu.ac.il.
Beatriz Hemo, Email: hemo.bea@gmail.com.
Angela Irony, Email: angelair@assuta.co.il.
Khaled Abou Houssien, Email: abu_hus_h@mac.org.il.
Omri Shental, Email: shental_o@mac.org.il.
Shirley Shapiro Ben David, Email: shapira_sr@mac.org.il.
Limor Adler, Email: adler_l@mac.org.il.
Data availability statement
No data are available.
References
- 1.Meydan C, Haklai Z, Gordon B, et al. Managing the increasing shortage of acute care hospital beds in Israel. J Eval Clin Pract. 2015;21:79–84. doi: 10.1111/jep.12246. [DOI] [PubMed] [Google Scholar]
- 2.McWilliams A, Tapp H, Barker J, et al. Cost analysis of the use of emergency departments for primary care services in Charlotte, North Carolina. N C Med J . 2011;72:265–71. [PubMed] [Google Scholar]
- 3.Saczynski JS, Lessard D, Spencer FA, et al. Declining length of stay for patients hospitalized with AMI: impact on mortality and readmissions. Am J Med. 2010;123:1007–15. doi: 10.1016/j.amjmed.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warner JL, Zhang P, Liu J, et al. Classification of hospital acquired complications using temporal clinical information from a large electronic health record. J Biomed Inform. 2016;59:209–17.:S1532-0464(15)00288-9. doi: 10.1016/j.jbi.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leff B, Montalto M. Home hospital-toward a tighter definition. J Am Geriatr Soc. 2004;52:2141. doi: 10.1111/j.1532-5415.2004.52579_1.x. [DOI] [PubMed] [Google Scholar]
- 6.Shepperd S, Doll H, Angus RM, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2008:CD007491. doi: 10.1002/14651858.CD007491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levi B, Borow M, Wapner L, et al. Home Hospitalization Worldwide and in Israel. Isr Med Assoc J. 2019;21:565–7. [PubMed] [Google Scholar]
- 8.Gaillard G, Russinoff I. Hospital at home: A change in the course of care. J Am Assoc Nurse Pract. 2023;35:179–82. doi: 10.1097/JXX.0000000000000814. [DOI] [PubMed] [Google Scholar]
- 9.Gonçalves-Bradley DC, Iliffe S, Doll HA, et al. Early discharge hospital at home. Cochrane Database Syst Rev. 2017;6:CD000356. doi: 10.1002/14651858.CD000356.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leong MQ, Lim CW, Lai YF. Comparison of Hospital-at-Home models: a systematic review of reviews. BMJ Open. 2021;11:e043285. doi: 10.1136/bmjopen-2020-043285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143:798–808. doi: 10.7326/0003-4819-143-11-200512060-00008. [DOI] [PubMed] [Google Scholar]
- 12.Conley J, O’Brien CW, Leff BA, et al. Alternative Strategies to Inpatient Hospitalization for Acute Medical Conditions: A Systematic Review. JAMA Intern Med. 2016;176:1693–702. doi: 10.1001/jamainternmed.2016.5974. [DOI] [PubMed] [Google Scholar]
- 13.Shepperd S, Iliffe S, Doll H, et al. Admission avoidance hospital at home. Status Date New Search Stud Content Updat No Change Conclus Publ. 2016.
- 14.Federman AD, Soones T, DeCherrie LV, et al. Association of a Bundled Hospital-at-Home and 30-Day Postacute Transitional Care Program With Clinical Outcomes and Patient Experiences. JAMA Intern Med. 2018;178:1033–40. doi: 10.1001/jamainternmed.2018.2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis G, Wright L, Vaithianathan R. Multidisciplinary case management for patients at high risk of hospitalization: comparison of virtual ward models in the United kingdom, United States, and Canada. Popul Health Manag. 2012;15:315–21. doi: 10.1089/pop.2011.0086. [DOI] [PubMed] [Google Scholar]
- 16.Caplan GA, Sulaiman NS, Mangin DA, et al. A meta-analysis of “hospital in the home.”. Med J Aust. 2012;197:512–9. doi: 10.5694/mja12.10480. [DOI] [PubMed] [Google Scholar]
- 17.Walsh B, Lyons S, Smith S, et al. Does formal home care reduce inpatient length of stay? Health Econ. 2020;29:1620–36. doi: 10.1002/hec.4158. [DOI] [PubMed] [Google Scholar]
- 18.Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Ann Intern Med. 2020;172:77–85. doi: 10.7326/M19-0600. [DOI] [PubMed] [Google Scholar]
- 19.Zolot J. At-Home Hospital Care Reduces Readmissions and Length of Stay, Enhances Patient Satisfaction. AJN Am J Nurs. 2018;118:13. doi: 10.1097/01.NAJ.0000546363.97759.db. [DOI] [PubMed] [Google Scholar]
- 20.Kalisch BJ, Lee S, Dabney BW. Outcomes of inpatient mobilization: a literature review. J Clin Nurs. 2014;23:1486–501. doi: 10.1111/jocn.12315. [DOI] [PubMed] [Google Scholar]
- 21.Levine DM, Pian J, Mahendrakumar K, et al. Hospital-Level Care at Home for Acutely Ill Adults: a Qualitative Evaluation of a Randomized Controlled Trial. J Gen Intern Med. 2021;36:1965–73. doi: 10.1007/s11606-020-06416-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kastengren M, Frisk L, Winterfeldt L, et al. Implementation of Sweden’s first digi-physical hospital-at-home care model for high-acuity patients. J Telemed Telecare. 2024:1357633X241232176. doi: 10.1177/1357633X241232176. [DOI] [PubMed] [Google Scholar]
- 23.Montalto M, Chu MY, Ratnam I, et al. The treatment of nursing home-acquired pneumonia using a medically intensive Hospital in the Home service. Med J Aust. 2015;203:441–2. doi: 10.5694/mja15.00672. [DOI] [PubMed] [Google Scholar]
- 24.Arsenault-Lapierre G, Henein M, Gaid D, et al. Hospital-at-Home Interventions vs In-Hospital Stay for Patients With Chronic Disease Who Present to the Emergency Department: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4:e2111568. doi: 10.1001/jamanetworkopen.2021.11568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barkai G, Amir H, Dulberg O, et al. “Staying at Home”: A pivotal trial of telemedicine-based internal medicine hospitalization at a nursing home. Digit Health. 2022;8:20552076221125958. doi: 10.1177/20552076221125958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gabel C, Ko LN, Dobry AS, et al. Patient preference for cellulitis treatment: At-home care is preferred to hospital-based treatment. J Am Acad Dermatol. 2021;85:767–8. doi: 10.1016/j.jaad.2020.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Corwin P, Toop L, McGeoch G, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. BMJ. 2005;330:129. doi: 10.1136/bmj.38309.447975.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rentala M, Andrews S, Tiberio A, et al. Intravenous Home Infusion Therapy Instituted From a 24-Hour Clinical Decision Unit For Patients With Cellulitis. Am J Emerg Med. 2016;34:1273–5. doi: 10.1016/j.ajem.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 29.Ong BS, Ngian VJJ, Yeong C, et al. Out Of Hospital And In Hospital Management Of Cellulitis Requiring Intravenous Therapy. Int J Gen Med. 2019;12:447–53. doi: 10.2147/IJGM.S230054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernandez C, Tukpah A-M, Mitchell HM, et al. Hospital-Level Care at Home for Patients With Acute Respiratory Disease: A Descriptive Analysis. Chest. 2023;163:891–901. doi: 10.1016/j.chest.2022.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Regalado de Los Cobos J, Aizpuru Barandiaran F, Oceja Barrutieta E, et al. Efficacy of hospital at home (HaH) in the treatment of community-acquired pneumonia (CAP) with different degrees of severity. Med Clin (Barc) 2010;135:47–51. doi: 10.1016/j.medcli.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 32.Salazar A, Estrada C, Porta R, et al. Home hospitalization unit: an alternative to standard inpatient hospitalization from the emergency department. Eur J Emerg Med. 2009;16:121–3. doi: 10.1097/MEJ.0b013e32831cbae2. [DOI] [PubMed] [Google Scholar]
- 33.Gallardo S, Antón A, Larruscain I, et al. Effectiveness of a home hospitalization program for patients with urinary tract infection after discharge from an emergency department. Emerg Rev Soc Espanola Med Emerg. 2017;29:313–9. [PubMed] [Google Scholar]


