Abstract
Background
Globally, adolescent depression is prevalent. There is, however, a dearth of studies investigating behavioral intention to professional help-seeking regarding mental health problems among adolescents having probable depression. Based on the Stress Coping Theory, the hypothesis that personal resources and active coping would mediate between interpersonal resources and behavioral intention to professional help-seeking was investigated.
Methods
Students from five junior middle schools, three senior high schools, and one vocational school were selected to participate in the survey from February to March 2022 via convenient sampling. The questionnaire collected participants’ characteristics, depression, peer acceptance/support, resilience, self-compassion, active coping, and behavioral intention to professional help-seeking. The final sample included 1,425 Chinese adolescents having probable depression (Patient Health Questionnaire score ≥ 10). SPSS 23.0 and Mplus 8.3 were employed to analyze the data.
Results
The prevalence of behavioral intention to professional help-seeking was 15.4%. Adjusted for background factors, peer acceptance, resilience, self-compassion, and active coping were significantly associated with behavioral intention to professional help-seeking (ORa ranged from 1.05 to 1.31). The indirect effects via active coping (β = 0.020) and a serial indirect effect via personal resources and active coping (β = 0.029) were statistically significant. The direct effect from interpersonal resources to behavioral intention to professional help-seeking was non-significant.
Conclusion
The prevalence of behavioral intention to professional help-seeking among adolescents with probable depression was low and might render early detection/intervention ineffective. It is important to increase the intention to seek help from professionals. One possibility is to enhance interpersonal/personal resources and active coping.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06271-4.
Keywords: Depression, Chinese adolescents, professional help-seeking; Coping resources; Active coping; Stress Coping Theory
Background
Adolescence is a very fast-developing life stage associated with prevalent mental distress [1]. Globally, about 1/7 of them are suffering from a mental disorder, accounting for 14% of the global disease burden in this age group. Depression is one of the leading illnesses in adolescents [1], resulting in serious consequences such as non-suicidal self-injury and suicide [2]. A meta-analysis of 72 studies reported that the global prevalence of depressive symptoms among adolescents increased from 24 to 37% between 2001 and 2010 [3]. Another meta-analysis reviewing 18 Chinese studies reported the pooled adolescent prevalence of depression of 24.3% (95% CI: 21.3–27.6%) [4]. The COVID-19 pandemic has further increased the prevalence of adolescent depression [5, 6] due to school suspension and changes in social support [7]. The Chinese government has emphasized the need to strengthen students’ mental health, especially in reducing adolescent depression [8].
Professional help-seeking among adolescents at risk of depression is important, as depressive symptoms are detrimental and may worsen over time [1]. Untreated depression, even in mild cases, may lead to depression during adulthood [9]. Globally, only 20% of adolescents suffering from at least one major depressive episode had sought treatment from professionals [10]. Furthermore, the number of mental health problems was negatively associated with attitudes toward professional help-seeking behavior and intention [11]; the severity of depressive symptoms was also negatively associated with professional help-seeking among college students [12]. In a recent study of 367 middle school students with probable depression, only 18% of them had sought professional help [13]. Despite the significance, there is a dearth of studies looking at modifiable factors of professional help-seeking regarding mental health problems and underlying mechanisms among adolescents having depressive symptoms.
It is warranted to increase behavioral intention to professional help-seeking regarding mental health problems (BI-PHSMHP). Professional help-seeking is defined as an adaptive coping process carried out by an adolescent perceiving himself/herself as having personal/psychological/affective needs to pursue help from formal services (e.g., counselors, psychologists, and psychiatrists) to deal with his/her mental health concerns [14, 15]. Behavioral intention, along with orientation and actual behaviors, is part of this professional help-seeking process [14, 15]. Behavioral intention is one of the strongest predictors of subsequent behavior [16]. It plays an important role in behavioral theories. For instance, the Theory of Planned Behavior postulates that behavioral intention determines health-related behaviors, and is in turn determined by attitudes, subjective norms, and perceived control [17]. A study further found that adolescents with depressive symptoms tended to possess weak BI-PHSMHP [18]. Factors associated with the low level of BI-PHSMHP among adolescents having depression included low availability of services [19], worry about stigma [20], low perceived efficacy and negative attitude regarding professional services [20], poor family economic status [21], and low mental health literacy [10].
The Stress Coping Theory was used as this study’s framework. It postulates that coping resources would affect an individual’s coping strategies, which would in turn determine the coping response [22]. In this case, professional help-seeking among those with depression can be seen as a positive coping response to the stress related to depressive symptoms. Coping resources refer to the personal, social, or environmental factors that individuals utilize to manage stress, adversity, or challenging situations [23]. Interpersonal resources are defined as the various forms of social support and relational assets available to individuals within their social networks [24]. Interpersonal resources such as peer support and peer acceptance facilitated problem-solving and coping with harsh situations [24]. Peer support and peer acceptance were associated with professional service-seeking among adolescents [25, 26]. Positive peer relationships promoted professional help-seeking to deal with mental health problems among young men [27]. A cohort study found that positive peer relationships were one of the strongest predictors of professional help-seeking to cope with depression [28].
Psychological resources are important personal resources [29]. In this study, the relationships between two types of personal psychological resources (resilience and self-compassion) and BI-PHSMHP were investigated. Resilience is defined as an individual’s ability to carry on, solve problems, and deal with adversity [30]. The Resiliency Theory postulates that resilience improves health outcomes via strengthening promotive factors including assets and resources at the personal level [31]. Resilience also enhances motivation for help-seeking and hope for recovery [30]. Empirically, a previous study targeting individuals with major depressive disorder found that those with higher levels of resilience were associated with professional help-seeking for depression [32]. Another study conducted in Australian youths also demonstrated that resilience was associated with professional help-seeking intention for emotional issues [33].
Self-compassion is defined as openness and feeling about one’s pain, and experiences of care and kindness toward oneself [34]. Previous studies revealed that self-compassion facilitated help-seeking behaviors through the reduction of stigma and self-stigma towards professional help-seeking among college students [35]. Resilience and self-compassion were also associated with better stress management, positive affect, psychological well-being, health-promoting motivations [36], and BI-PHSMHP [32, 35].
The Stress Coping Theory has been used to explain the mechanism of the association between interpersonal and personal resources and BI-PHSMHP (a coping response) via coping strategies [22]. The theory suggests that such resources would increase active coping, which would, in turn, increase BI-PHSMHP. Empirically, peer support and peer acceptance (interpersonal resources) were positively associated with beneficial coping strategies, such as active coping [37]. A study reported that problem-focused coping significantly mediated the associations between perceived peer support and stigma regarding help-seeking for mental health problems among individuals with mild levels of depressive symptoms [38]. Similarly, resilience and self-compassion contributed to positive coping styles that helped individuals to survive and thrive despite adversity or stress [33, 36]. For instance, resilient depression patients were more likely than other patients to use adaptive coping strategies [39]. Thus, it is expected that coping strategies would mediate between interpersonal/personal resources (peer support, peer acceptance, resilience, and self-compassion) and coping responses (professional help-seeking).
Furthermore, since interpersonal resources such as peer support and peer acceptance were positively associated with personal resources such as resilience [40] and self-compassion [41] among adolescents, it is plausible that personal resources may further mediate between interpersonal resources and coping strategies. Empirically, a recent study indicated that resilience (a personal resource) mediated between perceived social support (an interpersonal resource) and BI-PHSMHP among Australian young people [42]. In addition, perceived peer support was positively associated with resilience among adolescents [42] and trauma-exposed individuals [40]. Maheux and Price reported that peer support increased self-compassion [41]. Peer acceptance also increased resilience and self-compassion [43]. A longitudinal study also revealed that peer acceptance increased self-compassion, which in turn reduced depressive symptoms among adolescents [43]. Thus, personal resources may mediate between interpersonal resources and active coping, resulting in a serial mediation.
Given the background, the present study investigated (1) the prevalence of BI-PHSMHP among Chinese adolescents with probable depression; (2) factors of BI-PHSMHP including interpersonal resources (peer support and peer acceptance), personal resources (resilience and self-compassion), and active coping. It further tested three indirect paths between interpersonal resources and BI-PHSMHP: (1) interpersonal resources → personal resources → BI-PHSMHP, (2) interpersonal resources → active coping→ BI-PHSMHP, and (3) interpersonal resources → personal resources → active coping → BI-PHSMHP (a serial mediation). To our knowledge, no study has investigated these associations and mediations; previous studies only looked at help-seeking intentions in some general adolescent populations [13]. Also, the important Stress Coping Theory has not been applied to investigate professional health-seeking among depressed adolescents. This study hence filled out these knowledge gaps.
Methods
Participants and data collection
Using convenient sampling, an anonymous cross-sectional survey was conducted in nine schools (i.e., five junior middle schools, three senior high schools, and one vocational school) from February to March 2022 in Taizhou city of Zhejiang province, China. The city has a population of 6.1 million people. Students of these schools were invited to participate in the study. Participants self-administered the structured questionnaire in the absence of teachers. This study’s background, purposes, and confidentiality were printed on the cover page of the questionnaire. With the assistance of several trained field workers, students were briefed that the return of the completed questionnaire would imply the provision of informed consent to participate in the study. The students were also briefed that they could quit anytime, and that refusal and incompletion of the questionnaire would bear no consequences. In addition, parents were informed about the studies. They were asked to send a note to the teachers if they did not wish their children to participate in the study; their children would not be invited to participate in the study. Such a procedure has been used in other studies [44]. No incentives were given to the participants. This study was approved by the research ethics committee of the corresponding author’s affiliated institution (No. KNLL-20211011002).
A total of 8,285 participants returned the questionnaire. Those of low quality (i.e., those with at least 20% of all the items involving missing values; n = 114, 1.4%) and failure to pass logical check (i.e., logical inconsistencies between some item responses; n = 615, 7.4%) were excluded from data analysis. Of the remaining 7,556 (91.2%) questionnaires, 1,425 (18.9%) were screened as having probable depression according to the Patient Health Questionnaire (PHQ-9 score ≥ 10) [45]. They constituted the final sample in this study.
Measures
Background characteristics
Such information included school type (junior middle school, senior high school, and vocational school), age, sex, hometown outside Taizhou, whether living with both parents, father’s and mother’s educational level (junior middle school or below, senior high school or equal, and college or above), self-reported academic performance (below average, average, or above average), self-reported household income level (5 points: very low to very high).
BI-PHSMHP
Participants were asked, “In the case of having mental health problems (e.g., anxiety or depressive symptoms), how likely would you seek help from a psychiatrist or a counselor?” Participants were rated on a five-point response (1 = very low to 5 = very high). The item was originally extracted from the Intentions to Seek Counseling Inventory (ISCI), which was used to assess participants’ intention to seek help from professionals if they were experiencing specific mental health problems, including depression and insomnia [46, 47]. The five-point response options were recoded into a binary dependent variable [0 = No (Very low/relatively low/neutral) versus 1 = Yes (relatively high/very high)]. Similar classifications have been made in other published papers [48–50].
Peer acceptance
Peer acceptance was measured by using the 5-item peer acceptance subscale of the 8-item PROMIS peer relationship short-form [51]. Its Chinese version has been validated among Chinese primary school students with acceptable psychometric properties [52]. A sample item is “I feel accepted by my peers”. The scale was assessed with a 5-point Likert scale (1 = never to 5 = always), with higher scores indicating higher levels of peer acceptance. The Cronbach’s alpha of the scale was 0.89 in this study.
Peer support
Peer support was measured by using three items assessing perceived emotional support, instrumental support, and affirmation from classmates and peers. Such assessment had been used in previous Chinese studies and showed satisfactory psychometric properties among adolescents [53]. A sample item was “When you need to talk with someone or emotional support, your classmates would give you adequate support”. The scale was rated with a 7-point Likert scale (0 = strongly disagree to 7 = strongly agree), with higher scores indicating higher levels of perceived peer support. The Cronbach’s alpha was 0.87 in this study.
Resilience
Resilience was assessed by using the 2-item abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC-2) [54]. Its Chinese version has been validated among adults with acceptable psychometric properties [55, 56]. It has also been used among Chinese adolescents, showing acceptable psychometric properties [57, 58]. The two items were “able to adapt to change” and “tend to bounce back after illness or hardship” (0 = not true at all to 4 = true nearly all the time). The Cronbach’s alpha of the scale was 0.80 in this study.
Self-compassion
Self-compassion was assessed by using the 2-item mindfulness subscale of the Self-compassion Scale Short Form (SCS-SF) [34]. Its Chinese version showed acceptable properties and has been validated and used among students and medical workers in previous Chinese studies [59]. The two items were “When I go through tough times, I give myself the care and love I need” and “When something upsets me, I try to keep my emotions in balance” and rated with a 5-point Likert scale (1 = almost never to 5 = almost always). Higher scores indicated higher levels of self-compassion. The Cronbach’s alpha of the scale was 0.80 in this study.”
Active coping
Active coping was assessed using the Brief COPE [60], which evaluated the specific coping strategies used by the participants in response to difficulties and dilemmas. The scale has been validated in Chinese studies and showed satisfactory psychometric properties among adolescents [61]. It consists of 2 items “focus efforts to solve existing difficulties” and “take practical action to improve the current situation” (1 = never to 4 = often). The Cronbach’s alpha of the scale was 0.84 in this study.
Statistical analysis
The Harman single-factor was employed to assess common method bias. It indicates that the common method bias is not a concern if the strongest factor explains less than 40% of the total variance [62]. Descriptive statistics were presented. Pearson correlation coefficients were derived to test the associations between the continuous variables. Univariate logistic regression models were fit to examine the associations between the background factors and BI-PHSMHP. Multiple logistic regression analyses with adjustment for significant background factors were conducted to investigate the associations between the individual independent variables (e.g., peer acceptance, peer support, resilience, self-compassion, and active coping) and BI-PHSMHP. Structural equation modeling (SEM) was performed to test the mediation effect of personal resources and active coping between interpersonal resources and BI-PHSMHP, after adjusting for the background factors that were significantly associated with BI-PHSMHP. The weighted least square mean and variance adjusted (WLSMV) estimator was used. Three latent variables were created. The latent variable of interpersonal resources involved the two variable scores of peer support and peer acceptance. The latent variable of personal resources was derived from the summative scale scores of resilience and self-compassion. The latent variable of active coping was constructed for the two original items of active coping. Satisfactory model fit indices included Comparative Fit Index (CFI) ≥ 0.90, Tucker-Lewis Index (TLI) ≥ 0.90, Root Mean Square Error of Approximation (RMSEA) ≤ 0.08, and Standardized Root Mean Square Residual (SRMR) ≤ 0.08 [63]. SEM was conducted by using Mplus 8.3 while the other analyses by SPSS 23.0. Statistical significance was defined as a two-tailed p-value < 0.05.
Results
Results of common method bias test
In this study, the strongest factor extracted from an exploratory factor analysis (EFA) explained 34.1% of the total variance. According to the Harman single-factor criterion, there was no apparent common method bias.
Descriptive analyses
The results are shown in Table 1. Of all the 1,425 participants, the mean (SD) age was 15.13 (1.51) years. The proportions of students sampled from junior middle schools, senior high schools, and vocational schools were 53.8%, 40.8%, and 5.4%, respectively. Slightly over half of the participants were female (54.6%); Taizhou was not the hometown of 17.9% of the participants. About one-third did not live with both parents (31.3%). Over half of the participants’ fathers (64.8%) and mothers (67.7%) had attained middle school or below education. About half (45.1%) self-reported below-average academic performance; 18.4% self-reported very low/low household income levels. The prevalence of BI-PHSMHP was 15.4%. The mean (SD; range) scores regarding peer acceptance, peer support, resilience, self-compassion, and active coping are presented in Table 2.
Table 1.
Participants’ characteristics
| n | % | |
|---|---|---|
| School type | ||
| Junior middle school | 766 | 53.8 |
| Senior middle school | 582 | 40.8 |
| Vocational school | 79 | 5.4 |
| Sex | ||
| Male | 638 | 44.8 |
| Female | 778 | 54.6 |
| Not reported | 9 | 0.6 |
| Hometown outside Taizhou | ||
| No | 1,152 | 80.8 |
| Yes | 255 | 17.9 |
| Not reported | 18 | 1.3 |
| Living with both parents | ||
| Yes | 978 | 68.6 |
| No | 443 | 31.1 |
| Not reported | 4 | 0.3 |
| Father’s education level | ||
| Middle school or below | 924 | 64.8 |
| Senior high school or equal | 319 | 22.4 |
| College or above | 145 | 10.2 |
| Not reported | 37 | 2.6 |
| Mother’s education level | ||
| Middle school or below | 965 | 67.7 |
| Senior high school or equal | 262 | 18.4 |
| College or above | 152 | 10.7 |
| Not reported | 46 | 3.2 |
| Self-reported academic performance | ||
| Below average | 642 | 45.1 |
| Average | 327 | 22.9 |
| Above average | 451 | 31.6 |
| Not reported | 5 | 0.4 |
| Self-reported household income level | ||
| Very low/low | 262 | 18.4 |
| Average | 942 | 66.1 |
| High/very high | 166 | 11.6 |
| Not reported | 55 | 3.9 |
| BI-PHSMHP | ||
| No | 1,205 | 84.6 |
| Yes | 219 | 15.4 |
| Not reported | 1 | 0.1 |
BI-PHSMHP = Behavioral intention to professional help-seeking regarding mental health problems
Table 2.
Pearson correlations
| Mean, SD (range) | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| Peer acceptance | 13.26, 4.85(5–25) | 1 | ||||
| Peer support | 12.07, 4.12(3–21) | 0.49** | 1 | |||
| Resilience | 4.05, 2.08(0–8) | 0.23** | 0.15** | 1 | ||
| Self-compassion | 6.10, 2.19(2–10) | 0.22** | 0.19* | 0.53** | 1 | |
| Active coping | 4.99, 1.51(2–8) | 0.23** | 0.18** | 0.29** | 0.42** | 1 |
SD = Standard deviation; **, p < 0.01
Correlations
As shown in Table 2, peer acceptance, peer support, resilience, self-compassion, and active coping were positively associated with each other (r ranged from 0.15 to 0.53).
Associations between background factors of BI-PHSMHP
Those whose father had attended college/university (reference group: middle school or below; ORu = 1.64, 95% CI: 1.05–2.55, p = 0.030), who self-reported household income level being average (reference group: very low/low; ORu = 1.56, 95% CI: 1.01–2.39, p = 0.043) and good/very good (reference group: very low/low; ORu = 2.31, 95% CI: 1.35–3.97, p = 0.002) were more likely than others to indicate BI-PHSMHP. The associations involving age, sex, hometown outside Taizhou, living with both parents, mother’s educational level, and self-reported academic performance were statistically non-significant (Table 3).
Table 3.
Background factors of BI-PHSMHP
| ORu (95% CI) | p | |
|---|---|---|
| Age | 0.96 (0.87, 1.06) | 0.404 |
| School type | ||
| Junior middle school | Reference = 1 | |
| Senior middle school | 0.81 (0.60, 1.10) | 0.166 |
| Vocational school | 0.57 (0.27, 1.22) | 0.147 |
| Sex | ||
| Male | Reference = 1 | |
| Female | 1.16 (0.87, 1.55) | 0.322 |
| Hometown outside Taizhou | ||
| No | Reference = 1 | |
| Yes | 1.07 (0.74, 1.55) | 0.726 |
| Living with both parents | ||
| Yes | Reference = 1 | |
| No | 0.95 (0.69, 1.30) | 0.731 |
| Father’s education level | ||
| Middle school or below | Reference = 1 | |
| Senior high school or equal | 1.36 (0.97, 1.92) | 0.076 |
| College or above | 1.64 (1.05, 2.55) | 0.030 |
| Mother’s education level | ||
| Middle school or below | Reference = 1 | |
| Senior high school or equal | 1.43 (1.00, 2.04) | 0.052 |
| College or above | 1.37 (0.87, 2.14) | 0.174 |
| Self-reported academic performance | ||
| Below average | Reference = 1 | |
| Average | 1.18 (0.83, 1.69) | 0.355 |
| Above average | 0.94 (0.67, 1.33) | 0.742 |
| Self-reported household income level | ||
| Very low/low | Reference = 1 | |
| Average | 1.56 (1.01, 2.39) | 0.043 |
| High/very high | 2.31 (1.35, 3.97) | 0.002 |
BI-PHSMHP = Behavioral intention to professional help-seeking regarding mental health problems; ORu = Univariate odds ratio; CI = Confidence interval; Missing data was excluded from the analysis
Adjusted factors of BI-PHSMHP
The multiple logistic regression adjusted for the significant background factors showed that peer acceptance (ORa = 1.05, 95% CI = 1.02, 1.08, p = 0.001), resilience (ORa = 1.12, 95% CI = 1.04, 1.20, p = 0.004), self-compassion (ORa = 1.15, 95% CI = 1.07, 1.23, p < 0.001), and active coping (ORa = 1.31, 95% CI = 1.18, 1.45, p < 0.001) were significantly and positively associated with BI-PHSMHP, while peer support was not significantly associated with BI-PHSMHP (ORa = 1.01, 95% CI = 0.97, 1.05, p = 0.672). Such information is presented in Supplementary Table 1.
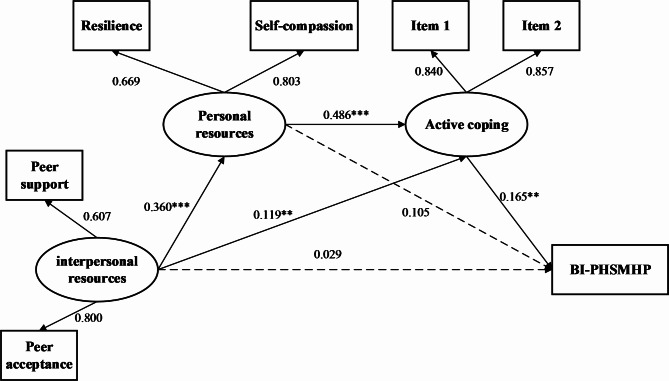
Testing the mediation effects
Figure 1 and Table 4 presents the results of the SEM analysis that adjusted for the significant background factors of BI-PHSMHP. The SEM yielded satisfactory model fit indices (CFI = 0.99, TLI = 0.97, RMSEA = 0.04, SRMR = 0.02). Two of the three indirect paths were statistically significant: (1) the mediation via interpersonal resources → active coping → BI-PHSMHP (standard estimate = 0.020, p = 0.030, 95% CI: 0.006–0.034; mediation effect size = 17.39%), and (2) the serial mediation: interpersonal resources → personal resources → active coping → BI-PHSMHP (standard estimate = 0.029, p = 0.004, 95% CI: 0.012–0.046; mediation effect size = 25.22%). The mediation effect size of personal resources and active coping together was 42.61%. The indirect effect of interpersonal resources via personal resources (without going through active coping) was not statistically significant (p = 0.102). Interpersonal resources showed no significant direct effect on BI-PHSMHP. More detailed information about the diagram can be seen in Supplementary Fig. 1.
Fig. 1.
Structural equation modeling (BI-PHSMHP = Behavioral intention to professional help-seeking regarding mental health problems. Standardized coefficients were reported. **, p < 0.01, ***, p < 0.001. The models were adjusted for background characteristics, including the father’s educational level and self-reported household income level)
Table 4.
Mediation analysis
| Path | β | SE | 95% CI | P | Mediation effect size |
|---|---|---|---|---|---|
| Total effect | 0.115 | 0.052 | (0.014, 0.22) | 0.027 | - |
| Direct effect | |||||
| IR→BI-PHSMHP | 0.029 | 0.060 | (-0.080, 0.138) | 0.632 | - |
| Indirect effect | |||||
| IR→PR→BI-PHSMHP | 0.037 | 0.023 | (-0.005, 0.079) | 0.102 | - |
| IR→AC→BI-PHSMHP | 0.020 | 0.009 | (0.006, 0.034) | 0.030 | 17.39% |
| IR→PR→AC→BI-PHSMHP | 0.029 | 0.010 | (0.012, 0.046) | 0.004 | 25.22% |
BI-PHSMHP = Behavioral intention to professional help-seeking; IR = Interpersonal resources; PR = Personal resources; AC = Active coping; CI = Confidence interval. The models were adjusted for significant background characteristics, including father’s educational level and household income level
Discussion
To our knowledge, this was the first study to report the prevalence of BI-PHSMHP in Chinese adolescents with probable depression. The prevalence of BI-PHSMHP was low. The study tested factors derived from the Stress Coping Model (peer support, peer acceptance, resilience, self-compassion, and active coping), and found two significant mediation paths between interpersonal resources and BI-PHSMHP (i.e., the mediation of interpersonal resources → active coping → BI-PHSMHP and the serial mediation: interpersonal resources → personal resources → active coping → BI-PHSMHP).
The low prevalence of BI-PHSMHP of only 15.4% was consistent with the previous findings claiming that most depressed adolescents were reluctant to seek professional help [13]. As it was reported that only about 40% of those with a behavioral intention performed the behavior in reality [64], the prevalence of actual professional help-seeking is expected to be much lower than 15.4%. Unlike previous studies reporting higher service utilization rates among females than males [64, 65], the sex difference in the prevalence of BI-PHSMHP was statistically non-significant. Females might have higher levels in some of the unstudied factors of BI-PHSMHP but lower levels in other factors. Further studies may investigate the presence/absence of variations in the levels of risk factors of BI-PHSMHP and look at related mediation/suppression effects of these factors between sex and BI-PHSMHP. The explanation of the non-significance is beyond the scope of this study. The finding implies that the promotion of BI-PHSMHP among male and female adolescents is equally important.
This study found a potential socio-economic disparity in BI-PHSMHP, as participants having a better-educated father and perceiving higher income were more likely than others to indicate BI-PHSMHP, despite a disproportionately lower prevalence of adolescent mental distress in lower socioeconomic status groups [66]. The finding corroborates similar studies [67]. Individuals with higher socioeconomic status and higher levels of education often have better access to mental health services due to their financial resources and in general, better knowledge about the disease. The apparent disparity might be related to the ability to access professional services, as private services in China, like in other countries, could be expensive. In 2015, there were 27,733 psychiatrists and psychiatric registrars (2.02 per 100,000 population), 57,591 psychiatric nurses (4.19 per 100,000), and 2,936 mental health services institutions [68] in mainland China. Furthermore, only a very small proportion of these professionals specialize in adolescent mental health [69]. Attention should be given to emergent psychiatric cases involving adolescents who cannot afford private services. Given the scarcity of resources, the country may adopt the stepped care model, which trains well-being officers to handle cases of mild distress and refer those with symptoms and higher risk to screening and psychiatric examinations and follow-ups [70]. The government needs to pay attention to the issue of potential socio-economic disparity.
Early detection and early intervention among adolescents are universally endorsed principles aiming at the reduction of mental distress. Policymakers in China have recognized the importance of early detection and have recently been organizing large-scale screening for depression among students [8]. The low prevalence of BI-PHSMHP might, however, defeat the goal of early detection and early intervention. Previous studies have identified a wide gap between the detection and treatment of depression [71]. Universal screening for adolescent depression in primary care settings has been recommended by Western countries such as the U.S., U.K., and Canada [72]. Some universal screening efforts have also been made in school settings in Western countries [73]. However, screening without follow-ups is not meaningful [73], and may even lead to unintended negative consequences such as anxiety and self-stigma [74]. Untreated adolescent depression increases the risk of developing severe harm, including depression and suicide in adulthood [2].
It is hence urgently warranted to understand the factors of BI-PHSMHP to facilitate the promotion of BI-PHSMHP. Supporting the initial hypotheses, the present study identified significant associations between interpersonal resources/personal resources/active coping and BI-PHSMHP. Such findings corroborate with previous studies. For instance, supportive resources and the ability to adopt problem-solving strategies were associated with stronger intentions to seek help for depression [38]. Peer support and peer acceptance reduce self-stigma and stigma about one’s mental health status, which are known obstacles against the utilization of psychiatry/psychological health services [75]. Looking at the adjusted odds ratios, the association between active coping and BI-PHSIMHP seems to be stronger than other variables and BI-PHSIMHP, which suggests that active coping may play a pivotal role in the help-seeking process, consistent with the findings of Ng et al. [76]. Notably, depressed adolescents tend to have lower interpersonal and personal resources than their counterparts [77]. In general, adolescents with depression are also less likely than others to use active coping strategies [78]. School-based interventions improving acceptance of peers with mental health problems are needed; such interventions have been effective in some cases [79].
Importantly, this study found that both interpersonal and personal resources have indirect effects on BI-PHSMHP via active coping. The roles of active coping in mediating the effects of coping resources are evident. There were no significant direct effects from personal resources to BI-PHSMHP and from interpersonal resources to BI-PHSMHP. Thus, active coping fully mediated between personal/interpersonal resources and BI-PHSMHP. The findings accord with the Stress Coping Theory [22], which postulates that in the presence of stressors, individuals would appraise the availability of coping resources and are likely to adopt positive coping strategies if the appraisal is affirmative or would otherwise adopt negative coping strategies [80]. The observed mediations are implicative as coping appraisal and coping processes are flexible and modifiable [80]. The findings suggest that the Stress Coping Theory is potentially applicable to guide the design of interventions promoting BI-PHSMHP. Effective interventions increasing active coping have been reported [81].
Personal resources and active coping together showed a strong mediating effect of 42.6% between interpersonal resources and BI-PHSMHP. The significant mediation that personal resources partially mediated between interpersonal resources and active coping is another important and novel finding. The findings suggest a preliminary elaboration of the Stress Coping Model (i.e., interpersonal resources → personal resources → active coping → BI-PHSMHP), which needs further development and confirmation in future studies. Within the Stress Coping Model, it seems that interpersonal resources may increase personal resources, as found by a previous study [82]; a recent study similarly found that resilience significantly mediated between peer support and coping styles in medical residents [83]. It is thus important to improve resilience and self-compassion among depressed adolescents, as such positive psychology attributes affected BI-PHSMHP both via active coping alone or serially via personal resources and then active coping together.
Notably, it is a limitation that we focused only on two types of interpersonal resources (peer support and acceptance), while there are other forms of unstudied interpersonal resources (e.g., family support and teacher support). Peer support and peer acceptance are certainly two important types of interpersonal resources. There are several reasons for focusing on peer support/acceptance. First, previous publications have documented that peer support is a facilitator of health-seeking for depression in the adolescent population [25] and peer acceptance is one of the most important factors in promoting help-seeking among adolescents with mental health problems [26]. Second, adolescents tend to turn to their peers rather than their teachers/parents to seek support and advice [84]. Third, many adolescents would not discuss their emotional problems with their parents and teachers [25], as they might think that adults would not understand their feelings and they might be treated differently [25]. Similarly, this study also focused only on two types of personal resources which are positive psychology attributes (resilience and self-compassion), while there are other forms of positive psychology attributes (e.g., self-affirmation and self-efficacy), as well as other types of personal resources (e.g., self-esteem) [85]. Thus, the findings about the elaboration of the Stress Coping Model are preliminary and subject to consolidations and expansions in future studies. Furthermore, the present study investigated mediation via active coping. Although active coping is important, individuals may, however, use multiple forms of positive coping and/or negative coping strategies (e.g., behavioral disengagement). For instance, those with probable depression were more likely than others to endorse behavioral disengagement as a coping strategy [86]. Future studies need to consider mediation effects involving other negative and/or positive coping strategies.
A remark is that the total effect size was not large (0.115). Researchers have, however, argued that a significant total effect of X on Y (interpersonal resources on BI-PHSIMH in the present study) is not necessary for mediation to occur [87]. In literature, many mediation studies involved relatively mild total effect [88–90]; mediation analysis has been conducted when the association between the independent variable and the dependent variable was mild or even non-significant [88, 91]. Mediation analysis can provide a deeper and more nuanced understanding, revealing the more complex mechanisms and pathways between two variables. There are cases in a crude non-significant association that could have more than one significant pathway working in different directions and neutralizing the strength of the overall association between the two variables [92] to result in a non-significant association. In the present study, the mediation effect size was, however, substantial (42.61%); some associations were also sizable; the findings are hence implicative. For instance, although this study did not test the Stress Coping Theory formally, the significant mediations add knowledge and lend support to this important theory, and are potentially useful in designing interventions to modify some of the studied factors. As the hypothesis was theory-driven and set before the survey, the reporting of the findings does not depend on the findings. As this is a preliminary study, other factors may be investigated in the future.
The study has several other limitations. It did not look at the direct reasons for not intending to seek professional help (e.g., stigma and self-stigma related to mental health illnesses); the hypothesis that the association between interpersonal/personal resources and BI-PHSMHP would be mediated through the reduction in self-stigma/stigma may be tested in future studies. Furthermore, while cognitive awareness is a prerequisite for utilizing psychiatric treatments and related services [93], it is unknown whether the participants were aware of their depressive symptoms. Related mental health literacy and illness perceptions about depression are potentially inadequate [94]. Parental awareness of adolescents’ symptoms is equally important, as decisions over professional help-seeking involving young adolescents are usually made by the parents [95]. Future studies may look at inter-generational effects on BI-PHSMHP. Methodologically, the information on the family’s economic condition was self-reported. Notably, both subjective and objective measures have been used for the purpose [67, 96]. Objective measures (e.g., Fukuoka et al.) may not be feasible in survey settings [97]. Self-reported family income may be unreliable as children may not know about such information [98] and often involve overestimation or underestimation [97]. The literature shows that subjective measures of economic status are important measures commonly used in health-related studies [99, 100]. Gagné et al. also found that self-reported household income level (high versus low) was significantly associated with mental health service use for depression [100]. BI-PHSMHP was measured by a single item 5-point Likert scale. Validation was hence not feasible. It is a limitation that the test-retest reliability test had not been performed. Many other similar studies [101, 102] have used similar single questions. BI-PHSMHP was recoded into a binary dependent variable due to the skewness of the scale and a potentially clear interpretation as the present study investigated intention to seek professional help; interpretation of a scalar dependent variable might be more difficult. Some scales are related to service seeking. Some of them, however, assessed attitudes and others refer to help-seeking for multiple conditions [103]. Another limitation is that adolescents with probable depression might overstate or understate their interpersonal and personal resources. Given the cross-sectional design, no causal relationships can be established; longitudinal studies are needed to test causal effects. Also, random sampling was not used in this study, sampling bias may exist. Data were collected from one city. Thus, cautions are needed when attempting to generalize the results to other regions in China and other countries.
Conclusion
The study presents some important novel findings, including the low prevalence of BI-PHSMHP among adolescents having probable depression, the associations between interpersonal resources/personal resources/active coping and BI-PHSMHP, and the mediations between the two types of resources and BI-PHSMHP via active coping. Such findings support the Stress Coping Theory. It also gives a preliminary elaboration of the theory by considering adding a serial path from interpersonal resources to personal resources to active coping to BI-PHSMHP. The low prevalence of BI-PHSMHP would erode efforts of early detections and lead to late or absence of treatment, and thus severe depression in adulthood. Interventions to improve BI-PHSMHP by improving interpersonal and personal resources and active coping are warranted. Longitudinal studies considering more comprehensive types of interpersonal/personal resources and coping strategies are needed to confirm the findings. Pilot interventions are also urgently needed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We sincerely appreciate the participants for their contributions to this study.
Abbreviations
- BI-PHSMHP
Behavioral intention to professional help-seeking regarding mental health problems
- PHQ-9
The 9-item Patient Health Questionnaire
- SEM
Structural equation modeling
- CFI
Comparative Fit Index
- TLI
Tucker-Lewis Index
- RMSEA
Root Mean Square Error of Approximation
- SRMR
Standardized Root Mean Square Residual
- SPSS
Statistical package for social sciences
- SD
Standard deviation
- CI
Confidence interval
- ORu
Univariate odds ratio
- ORa
Adjusted odds ratio
- IR
Interpersonal resources
- PR
Personal resources
- AC
Active coping
Author contributions
JTFL, YW, YY, and HL conceptualized the study. HL, DBW, YY, AMSW, YW, and JTFL conducted the study. DBW, JHC, YY, and GZ conducted the investigation. HL and YY conducted data analyses and prepared tables and a figure. DBW provided resources. HL, YY, YW and JTFL wrote the main manuscript text. HL, YY, DBW, AMSW, JHC, GZ, YW, and JTFL reviewed and edited the manuscript.
Funding
This project was funded by Science and Technology Program of Wenzhou (Y2020068).
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable requests.
Declarations
Ethics approval and consent to participant
This study was approved by the Medical Research Ethics Committee of the Affiliated Wenzhou Kangning Hospital of Wenzhou Medical University (No. KNLL-20211011002). Informed consent was obtained from all participants and their parents.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hui Lu and Yanqiu Yu contributed equally to this work.
Contributor Information
Yili Wu, Email: wuyili@wmu.edu.cn.
Joseph T.F. Lau, Email: jlau@cuhk.edu.hk
References
- 1.World Health Organization. Adolescents mental health. 2021. https://www.who.int/zh/news-room/fact-sheets/detail/adolescent-mental-health. Accessed 27 Apr 2023.
- 2.Başgöze Z, Wiglesworth A, Carosella KA, Klimes-Dougan B, Cullen KR. Depression, Non-suicidal Self-Injury, and suicidality in adolescents: common and distinct precursors, correlates, and outcomes. J Psychiatr Brain Sci. 2021;6:e210018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shorey S, Ng ED, Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br J Clin Psychol. 2022;61:287–305. [DOI] [PubMed] [Google Scholar]
- 4.Tang X, Tang S, Ren Z, Wong DFK. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: a systematic review and meta-analysis. J Affect Disord. 2019;245:498–507. [DOI] [PubMed] [Google Scholar]
- 5.Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2022;52:3222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Zhao J, Ross B, Ma Z, Zhang J, Fan F, et al. Longitudinal trajectories of depression and anxiety among adolescents during COVID-19 lockdown in China. J Affect Disord. 2022;299:628–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li X, Wu H, Meng F, Li L, Wang Y, Zhou M. Relations of COVID-19-Related stressors and Social Support with Chinese College Students’ psychological response during the COVID-19 pandemic. Front Psychiatry. 2020;11. [DOI] [PMC free article] [PubMed]
- 8.Ministry of Education of the People’s Republic of China. Notice of the Ministry of Education and Seventeen Other Departments on the Issuance of the Special Action Plan to Comprehensively Strengthen and Improve Student Mental Health in the New Era (2023–2025). 2023. http://www.moe.gov.cn/srcsite/A17/moe_943/moe_946/202305/t20230511_1059219.html. Accessed 4 Jun 2023.
- 9.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of Depression in adolescents and Young adults. Pediatrics. 2016;138:e20161878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh S, Zaki RA, Farid NDN. A systematic review of depression literacy: knowledge, help-seeking and stigmatising attitudes among adolescents. J Adolesc. 2019;74:154–72. [DOI] [PubMed] [Google Scholar]
- 11.Chen H, Fang X, Liu C, Hu W, Lan J, Deng L. Associations among the number of mental health problems, stigma, and seeking help from psychological services: a path analysis model among Chinese adolescents. Child Youth Serv Rev. 2014;44:356–62. [Google Scholar]
- 12.Chang H. Depressive symptom manifestation and help-seeking among Chinese college students in Taiwan. Int J Psychol. 2007;42:200–6. [Google Scholar]
- 13.Zhao M, Hu M. A multilevel model of the help-seeking behaviors among adolescents with mental health problems. Front Integr Nuerosci. 2022;16. [DOI] [PMC free article] [PubMed]
- 14.Barker G, Nascimento M, Deva M, Talukder K. Adolescents, social support and help-seeking behaviour: an international literature review and programme consultation with recommendations for action. WHO/Instituto Promundo. 2001. https://iris.who.int/bitstream/handle/10665/43778/9789241595711_eng.pdf
- 15.Rickwood D, Thomas K, Bradford S. Help-seeking measures in mental health: a rapid review. 2012.
- 16.Zorrilla MM, Modeste N, Gleason PC, Sealy D-A, Banta JE, Trieu SL. Depression and help-seeking intention among young adults: the theory of Planned Behavior. null. 2019;50:236–44. [Google Scholar]
- 17.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 18.Dardas LA, Silva SG, Van De Water B, Vance A, Smoski MJ, Noonan D, et al. Psychosocial correlates of Jordanian adolescents’ help-seeking intentions for Depression: findings from a nationally Representative School Survey. J School Nurs. 2019;35:117–27. [DOI] [PubMed] [Google Scholar]
- 19.Shi W, Shen Z, Wang S, Hall BJ. Barriers to Professional Mental Health help-seeking among Chinese adults: a systematic review. Front Psychiatry. 2020;11. [DOI] [PMC free article] [PubMed]
- 20.Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. 2020;20:293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: a systematic review. Clin Psychol Rev. 2020;75:101812. [DOI] [PubMed] [Google Scholar]
- 22.Lazarus R, Folkman S. Stress, Appraisal, and Coping. 1984.
- 23.Taylor SE, Stanton AL. Coping Resources, Coping Processes, and Mental Health. Annu Rev Clin Psycho. 2007;3 Volume 3, 2007:377–401. [DOI] [PubMed]
- 24.Buchwald P. The relationship of individual and communal state-trait coping and interpersonal resources as trust, empathy and responsibility. Anxiety Stress Coping. 2003;16:307–20. [Google Scholar]
- 25.Fröjd S, Marttunen M, Pelkonen M, Von Der Pahlen B, Kaltiala-Heino R. Adult and peer involvement in help-seeking for depression in adolescent population: a two-year follow-up in Finland. Soc Psych Psych Epid. 2007;42:945–52. [DOI] [PubMed] [Google Scholar]
- 26.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynch L, Long M, Moorhead A, Young, Men. Help-Seeking, and Mental Health Services: exploring barriers and solutions. Am J Mens Health. 2018;12:138–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fröjd S, Marttunen M, Pelkonen M, von der Pahlen B, Kaltiala-Heino R. Adult and peer involvement in help-seeking for depression in adolescent population. Soc Psych Psych Epid. 2007;42:945–52. [DOI] [PubMed] [Google Scholar]
- 29.Chi X-L, Huang Q-M, Liu X-F, Huang L-Y, Hu M-J, Chen Z-J, et al. Self-compassion and resilience mediate the relationship between childhood exposure to domestic violence and posttraumatic growth/stress disorder during COVID-19 pandemic. WJP. 2021;11:1106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18:76–82. [DOI] [PubMed] [Google Scholar]
- 31.Zimmerman MA. Resiliency theory: a strengths-based Approach to Research and Practice for Adolescent Health. Health Educ Behav. 2013;40:381–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schomerus G, Appel K, Meffert PJ, Luppa M, Andersen RM, Grabe HJ, et al. Personality-related factors as predictors of help-seeking for depression: a population-based study applying the behavioral model of Health services Use. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1809–17. [DOI] [PubMed] [Google Scholar]
- 33.Grove C, Marinucci A, Montagni I. Australian Youth Resilience and Help-Seeking during COVID-19: a cross-sectional study. Behav Sci. 2023;13:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18:250–5. [DOI] [PubMed] [Google Scholar]
- 35.Heath PJ, Brenner RE, Lannin DG, Vogel DL. Self-compassion moderates the relationship of perceived public and anticipated self-stigma of seeking help. Stigma Health. 2018;3:65–8. [Google Scholar]
- 36.Brenner RE, Vogel DL, Lannin DG, Engel KE, Seidman AJ, Heath PJ. Do self-compassion and self-coldness distinctly relate to distress and well-being? A theoretical model of self-relating. J Couns Psychol. 2018;65:346–57. [DOI] [PubMed] [Google Scholar]
- 37.Bigatti SM, Wagner CD, Lydon-Lam JR, Steiner JL, Miller KD. Depression in husbands of breast cancer patients: relationships to coping and social support. Support Care Cancer. 2011;19:455–66. [DOI] [PubMed] [Google Scholar]
- 38.Talebi M, Matheson K, Anisman H. The stigma of seeking help for mental health issues: mediating roles of support and coping and the moderating role of symptom profile: the stigma of seeking help. J Appl Soc Psychol. 2016;46:470–82. [Google Scholar]
- 39.Min J-A, Yu JJ, Lee C-U, Chae J-H. Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Compr Psychiatr. 2013;54:1190–7. [DOI] [PubMed] [Google Scholar]
- 40.Sippel LM, Pietrzak RH, Charney DS, Mayes LC, Southwick SM. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. 2015;20.
- 41.Maheux A, Price M. The indirect effect of social support on post-trauma psychopathology via self-compassion. Pers Indiv Differ. 2016;88:102–7. [Google Scholar]
- 42.Ishikawa A, Rickwood D, Bariola E, Bhullar N. Autonomy versus support: self-reliance and help-seeking for mental health problems in young people. Soc Psychiatry Psychiatr Epidemiol. 2023;58:489–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu N, Hou Y, Chen P, You J. Peer Acceptance and Nonsuicidal Self-injury among Chinese adolescents: a longitudinal Moderated Mediation Model. J Youth Adolescence. 2019;48:1806–17. [DOI] [PubMed] [Google Scholar]
- 44.Li J-B, Mo PKH, Lau JTF, Su X-F, Zhang X, Wu AMS, et al. Online social networking addiction and depression: the results from a large-scale prospective cohort study in Chinese adolescents. J Behav Addict. 2018;7:686–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cash TF, Begley PJ, McCown DA, Weise BC. When counselors are heard but not seen: initial impact of physical attractiveness. J Couns Psychol. 1975;22:273–9. [Google Scholar]
- 47.Kelly AE, Achter JA. Self-Concealment and Attitudes Toward Counseling in University Students.
- 48.Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen Y, et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory Workers: cross-sectional online survey. J Med Internet Res. 2021;23:e24673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen YQ, et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 Years: cross-sectional online survey. JMIR Pediatr Parent. 2020;3:e24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parental. acceptability of HPV vaccination for boys and girls aged 9–13 years in China – A population-based study. Vaccine. 2018;36:2657–65. [DOI] [PubMed]
- 51.Devine KA, Willard VW, Hocking MC, Stapleton JL, Rotter D, Bukowski WM, et al. PROMIS peer relationships short form: how well does Self-Report Correlate With Data from peers? J Pediatr Psychol. 2018;43:1059–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fan L, Liu B, Jin Z, Zhu X. The validation of Chinese Version of the victimization Subscale of the revised peer experiences Questionnaire. Int J Environ Res Public Health. 2021;18:2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu Y, Peng L, Mo PKH, Yang X, Cai Y, Ma L, et al. Association between relationship adaptation and internet gaming disorder among first-year secondary school students in China: mediation effects via social support and loneliness. Addict Behav. 2022;125:107166. [DOI] [PubMed] [Google Scholar]
- 54.Vaishnavi S, Connor K, Davidson JRT. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007;152:293–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ni MY, Li TK, Yu NX, Pang H, Chan BHY, Leung GM, et al. Normative data and psychometric properties of the Connor–Davidson Resilience Scale (CD-RISC) and the abbreviated version (CD-RISC2) among the general population in Hong Kong. Qual Life Res. 2016;25:111–6. [DOI] [PubMed] [Google Scholar]
- 56.Zhang X, Mo Y, Yan C, Li Y, Li H. Psychometric properties of two abbreviated Connor–Davidson resilience scales in Chinese infertile couples. Qual Life Res. 2021;30:2405–14. [DOI] [PubMed] [Google Scholar]
- 57.Hou WK, Tong H, Liang L, Li TW, Liu H, Ben-Ezra M, et al. Probable anxiety and components of psychological resilience amid COVID-19: a population-based study. J Affect Disord. 2021;282:594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lai AY, Lee L, Wang M, Feng Y, Lai TT, Ho L et al. Mental Health impacts of the COVID-19 pandemic on International University Students, related stressors, and coping strategies. Front Psychiatry. 2020;11. [DOI] [PMC free article] [PubMed]
- 59.Meng R, Yu Y, Chai S, Luo X, Gong B, Liu B, et al. Examining psychometric properties and measurement invariance of a Chinese version of the Self-Compassion Scale -Short Form (SCS-SF) in nursing students and medical workers. Psychol Res Behav Ma. 2019;12:793–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carver CS. You want to measure coping but your protocol’ too long: consider the brief cope. Int J Behav Med. 1997;4:92–100. [DOI] [PubMed] [Google Scholar]
- 61.Tang KNS, Chan CS, Ng J, Yip C-H. Action type-based Factorial structure of brief COPE among Hong Kong Chinese. J Psychopathol Behav Assess. 2016;38:631–44. [Google Scholar]
- 62.Kock N. Harman’s single factor test in PLS-SEM: Checking for common method bias. 2021.
- 63.McDonald RP, Ho M-HR. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7:64–82. [DOI] [PubMed] [Google Scholar]
- 64.Ando S, Nishida A, Usami S, Koike S, Yamasaki S, Kanata S, et al. Help-seeking intention for depression in early adolescents: Associated factors and sex differences. J Affect Disord. 2018;238:359–65. [DOI] [PubMed] [Google Scholar]
- 65.Boyd C, Hayes L, Nurse S, Aisbett D, Francis K, Newnham K, et al. Preferences and intention of rural adolescents toward seeking help for mental health problems. RRH. 2011. 10.22605/RRH1582. [PubMed] [Google Scholar]
- 66.Knowles G, Gayer-Anderson C, Beards S, Blakey R, Davis S, Lowis K, et al. Mental distress among young people in inner cities: the Resilience, ethnicity and AdolesCent Mental Health (REACH) study. J Epidemiol Community Health. 2021;75:515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Magaard JL, Seeralan T, Schulz H, Brütt AL. Factors associated with help-seeking behaviour among individuals with major depression: a systematic review. PLoS ONE. 2017;12:e0176730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xiang Y, Ng CH, Yu X, Wang G. Rethinking progress and challenges of mental health care in China. World Psychiatry. 2018;17:231–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chinese National Bureau of Statistics. The seventh population census. 2020. http://www.stats.gov.cn/sj/pcsj/rkpc/7rp/zk/indexch.htm. Accessed 23 Aug 2023.
- 70.Adewuya AO, Adewumi T, Momodu O, Olibamoyo O, Adesoji O, Adegbokun A, et al. Development and feasibility assessment of a collaborative stepped care intervention for management of depression in the mental health in primary care (MeHPriC) project, Lagos, Nigeria. Psychol Med. 2019;49:2149–57. [DOI] [PubMed] [Google Scholar]
- 71.US Preventive Services Task Force. Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2009;123:1223–8. [DOI] [PubMed] [Google Scholar]
- 72.Sudhanthar S, Thakur K, Sigal Y, Turner J. Improving validated depression screen among adolescent population in primary care practice using electronic health records (EHR). BMJ Qual Improv Rep. 2015;4:u209517w3913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Law WC, McClanahan R, Weismuller PC. Depression Screening in the School setting: identification of the depressed adolescent. NASN School Nurse. 2017;32:364–70. [DOI] [PubMed] [Google Scholar]
- 74.Kluemper A, Heath L, Loeb D, Kroehl M, Trinkley K. Depression-related stigma among primary care providers. Mental Health Clinician. 2021;11:175–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yu S, Kowitt SD, Fisher EB, Li G. Mental Health in China: Stigma, Family obligations, and the potential of peer support. Community Ment Hlt J. 2018;54:757–64. [DOI] [PubMed] [Google Scholar]
- 76.Ng R, Ang RP, Ho M-HR. Coping with anxiety, Depression, anger and aggression: the Mediational Role of Resilience in adolescents. Child Youth Care Forum. 2012;41:529–46. [Google Scholar]
- 77.Ida AK, Christie-Mizell CA. Racial Group Identity, Psychosocial Resources, and depressive symptoms: exploring ethnic heterogeneity among Black americans. Sociol Focus. 2012;45:41–62. [Google Scholar]
- 78.Hussong AM, Midgette AJ, Thomas TE, Coffman JL, Cho S. Coping and Mental Health in Early Adolescence during COVID-19. Res Child Adoles Psy. 2021;49:1113–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang X, Peng S, Li H, Peng Y. How Depression Stigma affects attitude toward help seeking: the Mediating Effect of Depression Somatization. soc Behav pers. 2015;43:945–53. [Google Scholar]
- 80.Cheng C, Wang H, Ebrahimi OV. Adjustment to a New Normal: coping flexibility and Mental Health issues during the COVID-19 pandemic. Front Psychiatry. 2021;12. [DOI] [PMC free article] [PubMed]
- 81.Yu H, Li M, Li Z, Xiang W, Yuan Y, Liu Y, et al. Coping style, social support and psychological distress in the general Chinese population in the early stages of the COVID-19 epidemic. BMC Psychiatry. 2020;20:426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Labrague L, los Santos JAD, Falguera C. Social and emotional loneliness among college students during the COVID-19 pandemic: the predictive role of coping behaviours, social support, and personal resilience. 2021. [DOI] [PubMed]
- 83.Xu C, Wang Y, Wang Z, Li B, Yan C, Zhang S et al. Social support and coping style of medical residents in China: the mediating role of psychological resilience. Front Psychiatry. 2022;13. [DOI] [PMC free article] [PubMed]
- 84.Hashmi K, Fayyaz HN. Adolescence and Academic Well-Being: parents, teachers, and students’ perceptions. J Educ Educational Dev. 2022;9:27–47. [Google Scholar]
- 85.Peter C, Müller R, Cieza A, Geyh S. Psychological resources in spinal cord injury: a systematic literature review. Spinal Cord. 2012;50:188–201. [DOI] [PubMed] [Google Scholar]
- 86.Wilson CJ, Rickwood D, Deane FP. Depressive symptoms and help-seeking intentions in young people. Clin Psychol. 2007;11:98–107. [Google Scholar]
- 87.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. [DOI] [PubMed] [Google Scholar]
- 88.Zia B, Mackenzie C. Internalized Stigma negatively affects attitudes and intentions to seek psychological help among western muslims: testing a Moderated serial mediation model. Stigma Health. 2021;9.
- 89.Yang J, Li Y, Gao R, Chen H, Yang Z. Relationship between mental health literacy and professional psychological help-seeking attitudes in China: a chain mediation model. BMC Psychiatry. 2023;23:956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kantar A, Yalçın İ. Masculine gender role stress and attitudes towards seeking psychological help: serial mediation by Self-Stigma and Self-Compassion. Curr Psychol. 2023;43:1–11. [Google Scholar]
- 91.Tsai I-C, Kao Y-C, Lien Y-J. Serial indirect effects of psychosocial causal beliefs and stigma on help-seeking preferences for depression. Curr Psychol. 2023;42:13637–47. [Google Scholar]
- 92.Shrout P, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol Methods. 2002;7:422–45. [PubMed] [Google Scholar]
- 93.Ibrahim N, Amit N, Shahar S, Wee L-H, Ismail R, Khairuddin R, et al. Do depression literacy, mental illness beliefs and stigma influence mental health help-seeking attitude? A cross-sectional study of secondary school and university students from B40 households in Malaysia. BMC Public Health. 2019;19:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang C, Cramer KM, Cheng H-L, Do KA. Associations between Depression literacy and Help-Seeking Behavior for Mental Health Services among High School Students. School Mental Health. 2019;11:707–18. [Google Scholar]
- 95.Jeong YM, McCreary LL, Hughes TL. Qualitative study of depression literacy among Korean American parents of adolescents. J Psychosoc Nurs Men. 2018;56:48–56. [DOI] [PubMed] [Google Scholar]
- 96.Matar JL, Laletas S, Lubman DI. Mental Health concerns and help-seeking behaviors among adolescents in high socioeconomic status groups: a scoping review. Adolesc Res Rev. 2024;9:93–134. [Google Scholar]
- 97.Fukuoka Y, Rankin SH, Carroll DL. Systematic bias in self-reported annual household incomes among unpartnered elderly cardiac patients. Appl Nurs Res. 2007;20:205–9. [DOI] [PubMed] [Google Scholar]
- 98.Dang J, Cheng M, Ye C. Depression from Overestimation: income, Perception Bias and Children’s Mental Health in China’s Rural households. Sustainability. 2020;12:870. [Google Scholar]
- 99.Gabilondo A, Rojas-Farreras S, Rodráguez A, Ferníndez A, Pinto-Meza A, Vilagut G, et al. Use of primary and specialized Mental Health Care for a major depressive episode in Spain by ESEMeD respondents. PS. 2011;62:152–61. [DOI] [PubMed] [Google Scholar]
- 100.Gagné S, Vasiliadis H-M, Préville M. Gender differences in general and specialty outpatient mental health service use for depression. BMC Psychiatry. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Schomerus G, Matschinger H, Angermeyer MC. The stigma of psychiatric treatment and help-seeking intentions for depression. Eur Arch Psychiatry Clin Neurosci. 2009;259:298–306. [DOI] [PubMed] [Google Scholar]
- 102.Yang X, Ding N, Tu X, Zhao C, Xu H, Lai X, et al. The role of illness representations of internet gaming disorder (IGD) in help-seeking intention among undergraduates: a longitudinal study. Addict Behav. 2022;128:107233. [DOI] [PubMed] [Google Scholar]
- 103.Hammer J, Spiker D, Dimensionality. Reliability, and predictive evidence of validity for three help-seeking Intention instruments: ISCI, GHSQ, and MHSIS. J Couns Psychol. 2018;65. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable requests.