Abstract
Background
Distinguishing self-limiting (‘trivial’) from potentially consequential spinal pain in childhood and adolescence is crucial to prevent over- or under-medicalization. The aim of this study was to stratify participants for severity of spinal pain and to investigate associations of pain severity with potential consequences of pain and some psychophysical and clinical factors.
Methods
In 2020 and 2021, children and adolescents took part in a voluntary population-based spine screening event across Switzerland organized by the Swiss Chiropractors Association. The screening consisted of a questionnaire (14 questions) based on the Young Spine Questionnaire and a clinical examination by a chiropractor. Three subgroups of pain severity [no pain (including mild, occasional pain), one-sited moderate pain, one-sited severe or moderate/severe pain at multiple sites of the spine] were formed by combining the self-reported measures for pain intensity and pain frequency for two recall periods (lifetime, last week) according to literature. Multivariable logistic regression analyses were conducted to determine the associations between pain severity and potential pain consequences (impact of spinal pain on health and seeking medical advice because of spinal pain), as well as between pain severity and some psychophysical factors (head and/or belly pain, sleep problems, daytime tiredness) and clinical measures [trunk symmetry (rib hump), trunk muscle endurance (plank position)].
Results
Of all participants (N = 457; 6–16 years; mean age = 10.9 ± 3.0 years; 220 boys), those with most severe spinal pain and with one-sited moderate pain in the last week had higher odds for reporting an impact of spinal pain on their health (OR = 13.5, 95%CI = 4.9–36.8; OR = 4.7, 95%CI = 1.5–14.4) and for searching medical advice because of spinal pain (OR = 11.6, 95%CI = 4.5–30.1; OR = 3.9, 95%CI = 1.6–9.2). Headache and/or belly pain (OR = 2.6, 95%CI = 1.2–5.5) and daytime tiredness (OR = 3.2, 95%CI = 1.3–7.9) increased the odds for having most severe pain compared to having no pain. The clinical measures were not associated with pain severity.
Conclusion
Stratification by pain severity, particularly when asked for pain in the last week, might help to minimize over- and under-medicalization of spinal pain in childhood and adolescence. Prospective studies are needed to clarify the relevance of the investigated clinical tests in the context of adolescent spinal pain.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12887-024-05194-z.
Keywords: Adolescent, Back, Child, Consequences, Consequential, Frequency, Intensity, Pain, Psychophysical, Severity, Spinal, Trivial
Introduction
In adults, low back pain (LBP) and neck pain (NP) are the first and fourth leading causes for years lived with disability worldwide [1]. Several studies indicate that these conditions have their onset in childhood or adolescence [2, 3] and that prevalence increases with age, accelerating around the age of 12 to 15 [3, 4]. Only a minority of adolescents (< 10%) repeatedly report pain [5] and seek care for their condition [2]. Nevertheless, adolescents with back or neck pain have an increased risk for suffering from back or neck pain also in adulthood [6]. Thus, it was postulated that the focus of research, prevention and treatment should be shifted from the adult to the young population [7].
As with adults, the first step in the assessment of adolescent spinal pain (lower back, mid back, neck) is to rule out red flags [8]. Likewise, in the majority of adolescent spinal pain no serious underlying pathology can be identified and back and neck pain is classified as non-specific: in a study with more than 200,000 adolescents with LBP, more than 80% had no identifiable diagnosis within one year, 9% had muscle spasm, 5% scoliosis and very few degenerative disc disease and disc herniation, respectively (1–2% each). Serious pathologies such as tumor, fracture, or spondylolisthesis were diagnosed in less than 1% of these patients [9]. In non-specific spinal pain it is essential to early differentiate those children and adolescents who are at risk for a long-term (‘consequential’) pain condition from those with a self-limiting (‘trivial’) pain episode [2], to prevent the former from developing chronic pain and to ensure that the latter are not ‘over-medicalized’ by unnecessary diagnostic and therapeutic activities [10].
Similar to adults, adolescent non-specific spinal pain is regarded as a bio-psychosocial problem [10] and risk factors have been identified in all these domains. In the ‘bio’ domain, older age [11], trunk asymmetry and the diagnosis of scoliosis [12–14], and reduced trunk muscular endurance [14, 15] were reported to be associated with LBP in adolescents. In the ‘psycho’ and in the ‘social’ domain, psychological distress and emotional coping problems [16] and the participation in competitive sports [11] have been suggested as risk factors. Furthermore, headache or abdominal pain [17, 18], sleep problems [19], and daytime tiredness [18] – all factors that share mental and physical qualities and are called ‘psychophysical’ throughout this study - seem to co-exist with chronic pain in children and adolescents. A recent systematic review and meta-analysis of prospective studies found that these factors were predictive for ongoing pain in children and adolescents suffering from pain at baseline [20].
Studies on spinal pain in children and adolescents are rather heterogeneous in terms of defining spinal pain with regard to its temporal course (e.g. ongoing or episodic), the selected recall periods and the delimitation of the spinal areas under study [4, 16, 21–23]. To note, severity of pain is often not assessed at all or described via consequences of pain rather than by precise characterization of pain via pain frequency and pain intensity [21]. To overcome these concerns, the present study was based on a validated questionnaire that assesses spinal pain in childhood and adolescence [23]. The questionnaire was complemented by questions on pain in other body regions, sleep problems and general health with the aim to investigate in a standardized manner whether associations exist between spinal pain severity and (i) consequences of spinal pain (e.g., general health) as well as (ii) psychophysical factors (e.g., pain in other body regions, sleep problems). In addition, a standardized clinical examination was performed to investigate possible associations between spinal pain severity and the results from clinical tests. The findings might improve the understanding of the differences between potentially long-term (‘consequential’) and self-limiting (‘trivial’) spinal pain in childhood and adolescence and might contribute to minimize under- and over-medicalization of the condition.
Method
Participants and setting
This is a cross-sectional observational study using data that was collected on ‘Spine Day’ 2020 and 2021. ‘Spine Day’ is a yearly voluntary and free of charge spine screening examination in children and adolescents organized by the Swiss Chiropractors Association (ChiroSuisse) on the occasion of the World Health’s Organization annual spine day. ‘Spine Day’ is announced throughout Switzerland by advertisements in print and electronic media as well as by flyers in chiropractic practices. Thus, the study sample was self-selected, community-based and consisted of children and adolescents with and without spinal pain of different severity levels between six and 16 years of age. Beforehand the Spine Days, the chiropractors were instructed in detail how to perform the clinical examination at the annual congress of ChiroSuisse. In addition, the participating chiropractors received written instructions.
Ethics approval and consent to participate
On Spine Day, parents or legal guardians gave informed consent for participation in the event. The survey and the clinical examinations were carried out within the framework of Spine Day, were not specific to the present study and the forms (questionnaire and examination form) were held completely anonymous. Under the lead of the Ethics committee of the Canton Zurich all Ethics committees of Switzerland confirmed that this project did not fall within the scope of the Human Research Act (article 2 paragraph 2; https://www.fedlex.admin.ch/eli/cc/2013/617/de#art_2) and thus no authorization was required (BASEC req-2020-00825 and req-2023-01333).
Procedures
While waiting for the clinical examination, participants or their parents/legal guardians filled in a questionnaire (Additional file 1). It can be assumed that with increasing age, the participants completed the questionnaire on their own, while most likely the parents completed the forms for or together with the younger children. However, this was not standardized.
The questionnaire consisted of 14 questions (including sub-questions): the questions 1a, 2a, 3a, and 4 were identical with the Young Spine Questionnaire (YSQ) [23], which has been validated, cross-culturally adapted and translated into German (G-YSQ) [24]. In the YSQ and the G-YSQ, three different spinal regions (neck, mid back and lower back) are asked about separately (illustrated by drawings). For each region, pain frequency is asked for by a four-point Likert scale (‘never’, ‘once or twice’, ‘once in a while’, ‘often’) and pain intensity is rated using the revised faces pain rating scale (rFPS) [25]. The rFPS consists of six faces that indicate increasing pain intensity and can be scored either by 0–5 or by 0–10 [25]. This measure has been reported to be well accepted in children and adolescents between four and 17 years of age, to be the psychometrically soundest measure for pain intensity in school-aged children [26], and to be highly correlated with pain intensity scores measured by a visual analogue scale (r = 0.87–0.93 depending on age) [25]. As an adaptation of the original YSQ, which asks dichotomously for spinal pain in the last week (answer options ‘Yes’ and ‘No’), the questions 1b, 2b, and 3b of the questionnaire used in the present study asked for spinal pain intensity and frequency during the last week (“Have you had pain in the lower back/mid back/neck in the last week?” [23]) as recommended to improve the responsiveness and to reduce recall bias [24]. Similar to the recall period of lifetime, pain frequency was asked for using a four-point Likert scale (‘never’, ‘once or twice’, ‘once in a while (several times a week)’, ‘every day’), and pain intensity using the rFPS. As another extension to the original YSQ, the questionnaire used in the present study included questions on pain in other body regions, e.g. headache or abdominal pain (question 5), as well as on sleep problems and daytime tiredness (question 6) that were based on literature [27–29]. However, in contrast to the latter studies that used recall periods of three [27, 29] or six months [28], the present study used a one-week recall period in order to reduce recall bias and to be consistent with the question on weekly spinal pain. Thus, these questions were formulated by the authors of the present study. Lastly, the question on general health (question 7) was taken from the KIDSCREEN (with permission) [30] and was complemented by a custom-formulated question on the impact of spinal pain on self-rated general health in order to exclude bias by other factors than the spine.
The clinical examination was a routine clinical musculoskeletal screening for children complemented by a few study-specific tests. The clinical routine included the visual inspection of gait and posture, the screening of spine mobility (range of motion and segmental testing) and hip mobility, and testing of hamstrings length. The tests that were used for the present study were the forward bending test, which screens for the presence of a rib hump and is the most widely used screening test for scoliosis in the school setting [31] and the plank position, which is valid and reliable to test trunk muscle endurance for children between eight and twelve years of age [32]. For the forward bending test, the participants were in a standing position and were instructed to bend forward as far as possible with their hands together and keeping their knees extended. For the plank position, the participants were instructed to position their spine in a neutral position with shoulder, hip and malleolus aligned [33]. As the unlimited plank protocol was shown to be less influenced by e.g. prior experience with the test setting than a 60-seconds or a 90-seconds plank protocol [32], we opted for a protocol with an upper limit of 180 s. This is quasi unlimited, as the 95% percentile is 133 s in the eight to twelve years old children [32]. Thus, despite the age limit of 16 years in the present study, ceiling effects were expected to be negligible. The test was terminated when either a first deviation from a neutral spine alignment could not be corrected or when a second deviation occurred [32].
Data analysis and statistics
The collected data was manually entered by research assistants into REDCap (Research Electronic Data Capture) electronic data capture tools (version 11.2.2), which is a secure, web-based application designed to support data capture for research studies [34]. Correct data entry into REDCap was checked by a second person for 50% of randomly selected data.
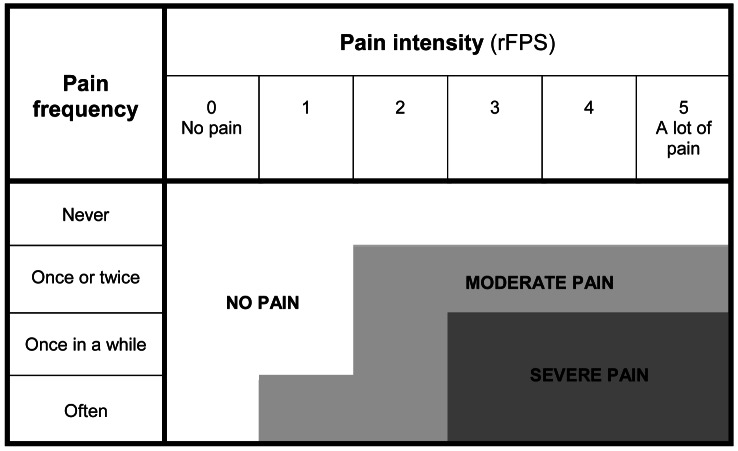
To quantify severity of spinal pain, pain frequency and intensity were combined based on a study by Joergensen and colleagues [35], resulting in three subgroups of pain severity per spinal region (Fig. 1): ‘no pain’, ‘moderate pain’, and ‘severe pain’. Also in accordance with that study [35], we built a composite variable ‘overall spinal pain’ that combined the above levels of pain severity in the three spinal regions: ‘no pain’ (‘no pain’ in each spinal region), ‘one-sited moderate pain’ (‘moderate pain’ in one spinal region), ‘multiple moderate pain’ (‘moderate pain’ in two or three spinal regions), ‘one-sited severe pain’ (‘severe pain’ in one spinal region), and ‘multiple severe pain’ (‘severe pain’ in two or three spinal regions). If different pain severity levels were registered for the three spinal regions, the region with the most severe pain was used for building the composite variable. In order to obtain an ordinal scale (i.e. the levels represent an order) and to ensure reasonable group sizes, the three subgroups ‘one-sited severe pain’, ‘multiple moderate pain’ and ‘multiple severe pain’ were merged. Thus, the final three subgroups of pain severity used in this study were ‘no pain’, ‘one-sited moderate pain’, and ‘one-sited severe or multiple-sited moderate or severe pain’, which were built with lifetime and last week’s data, respectively.
Fig. 1.
The pain severity subgroups ‘no pain’, ‘moderate pain’, and ‘severe pain’ built by combining pain intensity (assessed by the revised Faces Pain Rating Scale rFPS) and pain frequency.
Adapted from Joergensen et al. [35]
The severity subgroups were descriptively analyzed in terms of the participants’ age, gender, consequences of spinal pain (seeking medical advice and school and sports absenteeism because of spinal pain, self-rated health and the impact of spinal pain on self-rated health to exclude potential bias in the variable ‘self-rated health’ by comorbidities), psychophysical factors (sleep, daytime tiredness, head and/or belly pain), and findings from the clinical examination (rib hump, plank position). All categorical variables were dichotomized (Table 1) to (i) prevent small numbers of participants in some subgroups; (ii) discriminate between adolescents with occasional health problems potentially without pathological significance (e.g. daytime tiredness once a week) and those with health problems of potential pathological significance; and (iii) increase the degrees of freedom in the statistical analyses. The categorical variables were statistically compared between the severity subgroups using χ2-tests, and the plank position (continuous variable) was compared using ANOVA with post-hoc Bonferroni correction.
Table 1.
Dichotomization of the categorical variables
| Variable | Answers coded as ‘1’ | Answers coded as ‘0’ |
|---|---|---|
|
Seeking medical advice because of spinal pain School absenteeism because of spinal pain Sport absenteeism because of spinal pain |
‘once in a while’ ‘often’ |
‘never’ ‘once or twice’ |
| Self-rated health |
‘excellent’ ‘very good’ |
‘good’ ‘fair’ ‘poor’ |
| Impact of spinal pain on self-rated health | ‘my health would be clearly better without spinal pain’ |
‘no impact as I have no pain’ ‘no impact’ ‘little impact’ |
|
Sleep problems Daytime tiredness |
‘several times per week’ ‘every night/day’ |
‘no’ ‘once or twice’ |
| Headache and/or belly pain |
‘headache’ ‘belly pain’ ‘headache’ and ‘belly pain’ |
no ‘headache’ no ‘belly pain’ |
To determine the association between pain severity and the potential consequences of spinal pain, multivariable logistic regression analyses, adjusted for age and gender, were performed with self-rated health (0 = good/fair/poor; 1 = excellent/very good), the impact of spinal pain on health (0 = no impact; 1 = impact) and the search for medical advice because of spinal pain (0 = no; 1 = yes) as dependent variables and pain severity (no pain, one-sited moderate pain, one-sited severe or multiple moderate or severe pain) as independent variable. School and sport absenteeism were not statistically analyzed due to very small subgroups. To estimate the impact of the psychophysical variables and the findings from the clinical examination on pain severity, multivariable logistic regression analyses with the dependent variable ‘subgroup of pain severity’ (during lifetime and in the last week; 0=’no pain’, 1=’one-sited moderate pain’, 2=’one-sited severe or multiple moderate or severe pain’) and the independent variables age (continuous variable), gender (‘female’=0, ‘male’=1), sleep problems, daytime tiredness, headache or belly pain, trunk asymmetry/rib hump (for each of the latter four variables: ‘no’=0, ‘yes’=1), and trunk muscle endurance/plank position (continuous variable) were performed. Multivariable logistic regression analyses comparing two groups in each case was chosen because the effects of the predictors were not the same across the levels of the dependent variable (reflected in significant tests of parallel lines), which is a prerequisite for ordinal regression.
The association between spinal pain during lifetime and in the last week was investigated by calculating a Spearman correlation coefficient using the original, non-imputed data. Furthermore, the differences between these two measures were calculated and the median and interquartile range of these differences over all participants were determined.
For the handling of missing data (e.g. 15% for ‘pain severity lifetime’ and for ‘impact of spinal pain on self-rated health’, followed by 13% for ‘daytime tiredness’ and 9% for ‘pain severity last week’), available case analysis was used for descriptive statistics. For all multivariable logistic regression analyses, missing values were imputed (five imputations) and collinearity was tested using tolerance and variance inflation factor (VIF) values. If the tolerance values were > 0.1 and VIF < 10, no collinearity problem was assumed [36]. All analyses were performed using SPSS version 29.0 (IBM Corp., Chicago, IL, USA) and p-values of < 0.05 were considered statistically significant. When comparing the subgroups, the level of significance was adjusted according to the number of comparisons performed (0.05/3 = 0.017).
Results
Demographics of participants
In total, 457 children and adolescents between six and 16 years with a mean age of 10.9 years (± standard deviation 3.0 years) participated, 191 in 2020 and 266 in 2021.
Of those, 233 were girls, 220 boys, and one child self-identified as having a diverse gender and was excluded from the analysis (together with the three “true” missing values for the variable ‘gender’). Table 2 shows that half of the participants reported having had spinal pain in their life (20.1% one-sited moderate pain and 31.6% one-sited severe or multiple moderate/severe pain) and a quarter had spinal pain during the last week (13.8% one-sited moderate pain and 13.5% one-sited severe or multiple moderate/severe pain). Regarding the different phases of life according to the American Academy of Pediatrics [37], pain severity increased with age [pain severity lifetime: F(2,386) = 33.4, p < 0.001, post-hoc (Bonferroni) p < 0.003 for all comparisons; pain severity last week: F(2,411) = 21.61, p < 0.001, post-hoc (Bonferroni) p < 0.002 for all comparisons apart from the comparison between the subgroup with one-sited moderate pain and that with more severe pain: p = 0.141; values in brackets indicate the degrees of freedom for the effect and for the residuals of the model, respectively]. Pain severity did not differ between genders [lifetime: χ2(2) = 1.60, p = 0.449; last week: χ2(2) = 1.04, p = 0.595; value in brackets indicates the degree of freedom].
Table 2.
Demographics of participants
| Phase of life | N | Age (SD) (missing values N = 0/0.0%) |
Gender (f/m) (missing values N = 4/0.7%) |
Spinal pain severity lifetime (missing values N = 68/14.9%) |
Spinal pain severity last week (missing values N = 43/9.4%) |
||||
|---|---|---|---|---|---|---|---|---|---|
| No pain | One-sited moderate pain | One-sited severe / multiple moderate / multiple severe pain | No pain | One-sited moderate pain | One-sited severe / multiple moderate / multiple severe pain |
||||
|
All participants (6–16 years) |
457 |
10.9 (3.0) |
233/220 (51.4/48.6%) |
188 (48.3%) |
78 (20.1%) |
123 (31.6%) |
301 (72.7%) |
57 (13.8%) |
56 (13.5%) |
|
Childhood (6–10 years) |
211 |
8.2 (1.4) |
103/106 (49.3/50.7%) |
115 (62.5%) |
36 (19.6%) |
33 (17.9%) |
164 (84.1%) |
20 (10.3%) |
11 (5.6%) |
| Early adolescence (11–14 years) | 184 |
12.4 (1.1) |
95/89 (51.6/48.4%) |
65 (41.7%) |
35 (22.4%) |
56 (35.9%) |
117 (70.1%) |
26 (15.6%) |
24 (14.4%) |
| Mid adolescence (15–16 years) | 62 |
15.6 (0.5) |
35/25 (58.3/41.7) |
8 (16.3%) |
7 (14.3%) |
34 (69.4%) |
20 (38.5%) |
11 (21.2%) |
21 (40.4%) |
f = female, m = male, SD = standard deviation
Consequences of spinal pain
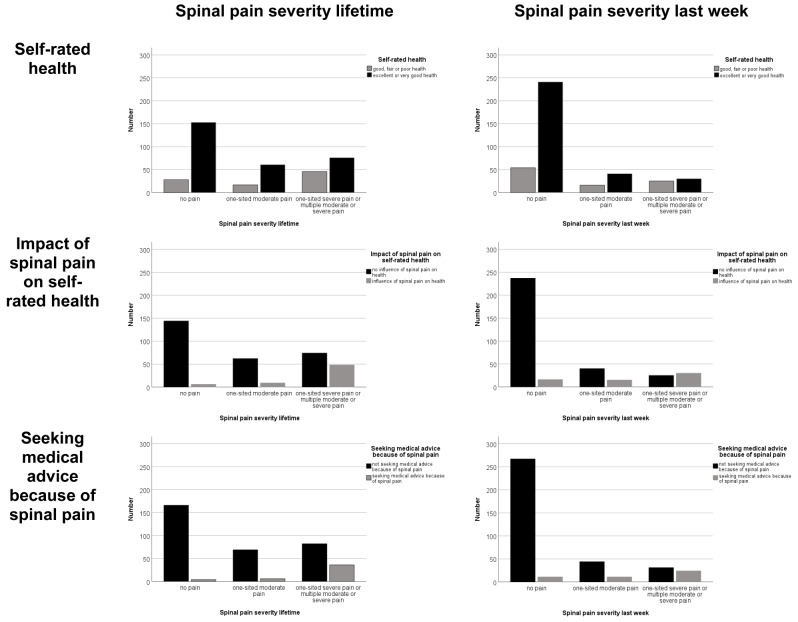
Of all participants, 22.7% indicated good, fair or poor health. The impact of spinal pain on their life was reflected in 17.8% of all participants reporting that their health would be better without spinal pain and in 11.5% seeking medical advice because of spinal pain. In contrast, school or sports absenteeism because of spinal pain was rare. Table 3; Fig. 2 show that the numbers of participants reporting good, fair or poor health, an impact of spinal pain on their health and seeking medical advice because of spinal pain increased with pain severity, and that the severity subgroups, regardless of whether the recall period was lifetime or the last week, significantly differed in these parameters.
Table 3.
Consequences of spinal pain
| Consequence of spinal pain | All (N = 457) | Spinal pain severity lifetime (missing values N = 68/14.9%) |
Spinal pain severity last week (missing values N = 43/9.4%) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| No pain (N = 188/48.3%) |
One-sited moderate pain (N = 78/20.1%) |
One-sited severe / multiple moderate / multiple severe pain (N = 123/31.6%) |
p-value | No pain (N = 301/72.7%) | One-sited moderate pain (N = 57/13.8%) | One-sited severe / multiple moderate / multiple severe pain (N = 56/13.5%) |
p-value | ||
|
Self-rated health Good or fair or poor/ Excellent or very good (%) |
100/340 (22.7%/77.3%) 17 missing values |
28/153 (15.5%/84.5%) 7 missing values |
17/61 (21.8%/78.2%) 0 missing values |
46/76 37.7%/62.3%) 1 missing value |
< 0.001 |
54/241 (18.3%/81.7%) 6 missing values |
16/41 (28.1%/71.9%) 0 missing values |
25/30 (45.5%/55.5%) 1 missing value |
< 0.001 |
|
Impact of spinal pain on health Yes/No (%) |
69/318 (17.8%/82.2%) 70 missing values |
6a/144 (4.0%/96.0/%) 38 missing values |
9/62 (12.7%/87.3%) 7 missing values |
48/74 (39.3%/60.7%) 1 missing value |
< 0.001 |
16a/237 (6.3%/93.7%) 48 missing values |
15/40 (27.3%/72.7%) 2 missing values |
30/25 (54.5%/45.5%) 1 missing value |
< 0.001 |
|
Seeking medical advice because of spinal pain Yes/No (%) |
48/370 (11.5%/88.5%) 39 missing values |
4/166 (2.4%/97.6%) 18 missing values |
6/69 (8.0%/92.0%) 3 missing values |
36/82 (30.5%/69.5%) 5 missing values |
< 0.001 |
11/267 (4.0%/96.0%) 23 missing values |
11/44 (20.0%/80.0%) 2 missing values |
24/31 (43.6%/56.4%) 1 missing value |
< 0.001 |
|
School absenteeism because of spinal pain Yes/No (%) |
4/441 (0.9%/99.1%) 12 missing values |
0/185 (0.0%/100.0%) 3 missing values |
0/77 (0.0%/100.0%) 1 missing value |
4/118 (3.3%/96.7%) 1 missing value |
b |
3/298 (1.0%/99.0%) 3 missing values |
1/56 (1.8%/98.2%) 0 missing values |
2/54 (3.6%/96.4%) 0 missing values |
b |
|
Sports absenteeism because of spinal pain Yes/No (%) |
11/414 (2.6%/97.4%) 32 missing values |
1/171 (0.6%/99.4%) 16 missing values |
0/75 (0.0%/100.0%) 3 missing values |
10/112 (8.2%/91.8%) 1 missing value |
b |
2/279 (0.7%/99.3%) 20 missing values |
4/53 (7.0%/93.0%) 0 missing values |
3/52 (5.5%/94.5%) 1 missing value |
b |
aThere can be an impact of spinal pain on self-rated health despite being in this subgroup, because it includes pain of minimal intensity at low frequency
bNot analyzed statistically due to small numbers of positive answers in all subgroups
bold: statistically significant at the significance level of 0.017 (corrected for multiple comparisons)
Fig. 2.
Consequences of spinal pain for the three subgroups of pain severity in lifetime (left column) and during the last week (right column)
There was a statistically significant association between pain severity and self-rated health [lifetime: χ2(2) = 20.06, p < 0.001; last week: χ2(2) = 19.93, p < 0.001], the impact of back pain on self-rated health [lifetime: χ2(2) = 57.99, p < 0.001; last week: χ2(2) = 80.22, p < 0.001] and the search for medical advice [lifetime: χ2(2) = 51.76, p < 0.001; last week: χ2(2) = 73.25, p < 0.001].
Table 4 shows that in the multivariable logistic regression models adjusted for age and gender (imputed data), participants with one-sited severe spinal pain or pain in multiple spinal sites in the last week had, compared to those without pain, significantly lower odds for reporting excellent or very good health (OR = 0.39, 95%CI = 0.19–0.81). This also applied when reporting this condition in lifetime (OR = 0.49, 95%CI = 0.26–0.90), but the result was not statistically significant when the significance level was corrected for multiple comparisons. The subgroup with most severe spinal pain had significantly higher odds for reporting an impact of spinal pain on their health (during lifetime: OR = 14.07 95%CI = 44.47–44.26; in the last week: OR = 13.45, 95%CI = 4.91–36.83) and for searching medical advice because of spinal pain (during lifetime: OR = 9.95, 95%CI = 3.24–30.59; in the last week: OR = 11.60, 95%CI = 4.47–30.11). The subgroup of participants with one-sited moderate pain in the last week, either during lifetime or in the last week, did not report reduced self-rated health, but reported more impact of spinal pain on health (OR = 4.71, 95%CI = 1.54–14.43) and sought more often medical advice for spinal pain (OR = 3.89, 95%CI = 1.64–9.21) than the participants without spinal pain. No collinearity was observed (tolerance values between 0.89 and 1.00, VIF values between 1.00 and 1.12).
Table 4.
Multivariable logistic regression model for the consequences of spinal pain as dependent variables and pain severity as independent variable
| Self-rated health (0 = good/fair/poor; 1 = excellent/very good) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Spinal pain severity lifetime | Spinal pain severity last week | |||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | 3.27 (0.50) | < 0.001 | 3.14 (0.50) | < 0.001 | ||||
| Age | -0.12 (0.04) | 0.004 | 0.89 | 0.82–0.96 | -0.12 (0.04) | 0.005 | 0.89 | 0.82–0.97 |
| Gender (f = 0, m = 1) | -0.65 (0.25) | 0.010 | 0.52 | 0.32–0.85 | -0.63 (0.25) | 0.010 | 0.53 | 0.33–0.86 |
| One-sited severe pain or multiple pain sites (= 1) versus no pain (= 0) | -0.72 (0.31) | 0.023a | 0.49 | 0.26–0.90 | -0.94 (0.37) | 0.013 | 0.39 | 0.19–0.81 |
| One-sited moderate pain (= 1) versus no pain (= 0) | -0.18 (0.37) | 0.626 | 0.84 | 0.41–1.73 | -0.40 (0.39) | 0.308 | 0.67 | 0.31–1.47 |
| Impact of spinal pain on self-rated health (0 = no impact; 1 = impact) | ||||||||
| Spinal pain severity lifetime | Spinal pain severity last week | |||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | -3.48 (0.73) | < 0.001 | -2.77 (0.72) | < 0.001 | ||||
| Age | 0.03 (0.06) | 0.680 | 1.03 | 0.90–1.17 | 0.02 (0.06) | 0.734 | 1.02 | 0.90–1.17 |
| Gender (f = 0, m = 1) | -0.02 (0.38) | 0.955 | 0.98 | 0.44–2.17 | -0.02 (0.34) | 0.959 | 0.98 | 0.50–1.94 |
| One-sited severe pain or multiple pain sites (= 1) versus no pain (= 0) | 2.64 (0.55) | < 0.001 | 14.07 | 4.47–44.26 | 2.60 (0.48) | < 0.001 | 13.45 | 4.91–36.83 |
| One-sited moderate pain (= 1) versus no pain (= 0) | 1.39 (0.69) | 0.061 | 4.02 | 0.93–17.32 | 1.55 (0.52) | 0.010 | 4.71 | 1.54–14.43 |
| Search for medical advice because of spinal pain (0 = no; 1 = yes) | ||||||||
| Spinal pain severity lifetime | Spinal pain severity last week | |||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | -6.06 (1.15) | < 0.001 | -5.45 (0.96) | < 0.001 | ||||
| Age | 0.23 (0.08) | 0.005 | 1.26 | 1.08–1.46 | 0.22 (0.07) | 0.003 | 1.25 | 1.08-1,44 |
| Gender (f = 0, m = 1) | -0.26 (0.35) | 0.470 | 0.77 | 0.38–1.56 | -0.34 (0.36) | 0.348 | 0.71 | 0.35–1.45 |
| One-sited severe pain or multiple pain sites (= 1) versus no pain (= 0) | 2.30 (0.57) | < 0.001 | 9.95 | 3.24–30.59 | 2.45 (0.47) | < 0.001 | 11.60 | 4.47–30.11 |
| One-sited moderate pain (= 1) versus no pain (= 0) | 1.08 (0.69) | 0.124 | 2.93 | 0.74–11.60 | 1.36 (0.44) | 0.002 | 3.89 | 1.64–9.21 |
CI = confidence interval, f = female, m = male, OR = odds ratio
bold: statistically significant (significance level = 0.017; corrected for multiple comparisons)
a statistically not significant (significance level = 0.017; corrected for multiple comparisons)
Association of pain severity with psychophysical factors and findings from the clinical examination
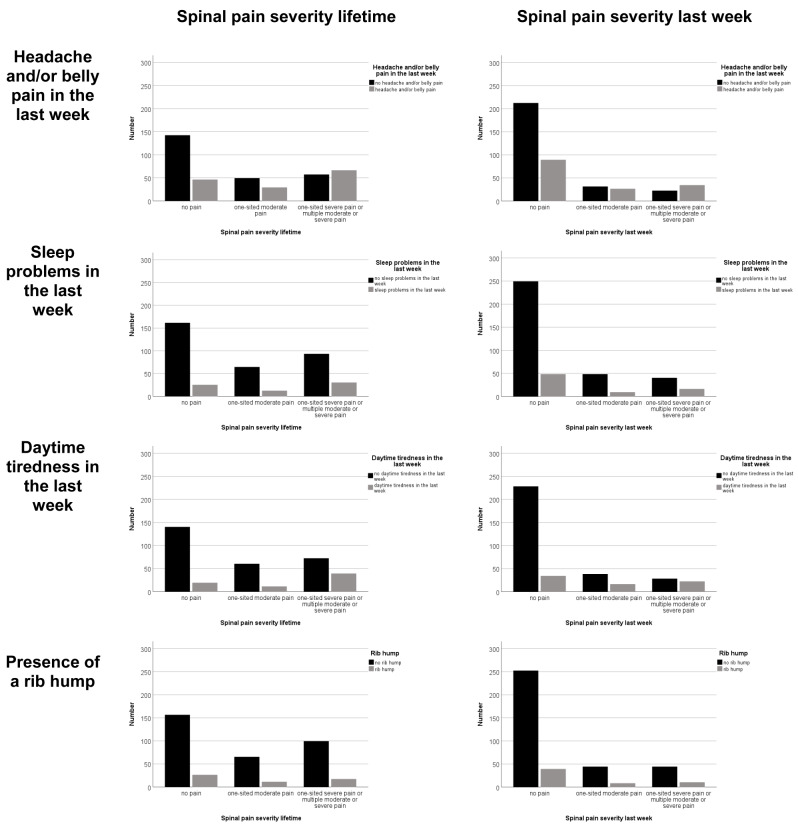
Table 5; Fig. 3 show that more than a third of the participants reported having head and/or belly pain during the last week and almost every fifth reported sleep problems and day tiredness. Trunk asymmetry was present in 14% of the participants, and plank position was held on average for 76 s. There was a significant association between pain severity in both recall periods, during lifetime and in the last week, and head and/or belly pain and between pain severity and daytime tiredness. Sleep problems, the presence of a rib hump and plank holding time were not associated with pain severity.
Table 5.
Psychophysical variables and findings from the clinical examination
| All (N = 457) | Spinal pain severity lifetime (missing values N = 68/14.9%) |
Spinal pain severity last week (missing values N = 43/9.4%) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No pain (N = 188/48.3%) |
One-sited moderate pain (N = 78/20.1%) |
One-sited severe / multiple moderate / multiple severe pain (N = 123/31.6%) |
p-value | No pain (N = 301/72.7%) |
One-sited moderate pain (N = 57/13.8%) | One-sited severe / multiple moderate / multiple severe pain (N = 56/13.5%) |
p-value | ||
|
Head and/or belly pain Yes/No (%) |
162/295 (35.4%/64.6%) 0 missing values |
46/142 (24.5%/75.5%) 0 missing values |
29/49 (37.2%/62.8%) 0 missing values |
66/57 (53.7%/46.3%) 0 missing values |
< 0.001 |
89/212 (29.6%/70.4%) 0 missing values |
26/31 (45.6%/54.4%) 0 missing values |
22/34 (39.3%/60.7%) 0 missing values |
< 0.001 |
|
Daytime tiredness Yes/No (%) |
77/319 (19.4%/80.6%) 61 missing values |
19/140 (11.9%/88.1%) 29 missing values |
11/60 (15.5%/84.5%) 7 missing values |
39/72 (35.1%/64.9%) 12 missing values |
< 0.001 |
34/228 (13.0%/87.0%) 39 missing values |
16/38 (29.6%/70.4%) 3 missing values |
22/28 (44.0%/56.0%) 6 missing values |
< 0.001 |
|
Sleep problems Yes/No (%) |
76/368 (17.1%/82.9%) 13 missing values |
25/161 (13.4%/86.6%) 2 missing values |
12/64 (15.8%/84.2%) 2 missing values |
30/93 (24.4%/75.6%) 0 missing values |
0.042a |
48/249 (8.8%/91.2%) 4 missing values |
9/48 (15.8%/84.2%) 0 missing values |
16/40/ (28.6%/71.4%) 0 missing values |
0.076 |
|
Trunk asymmetry Yes/No (%) |
60/371 (13.9%/86.1%) 26 missing values |
26/156 (14.3%/85.7%) 6 missing values |
11/65 (14.5%/85.5%) 2 missing values |
17/99 (14.7%/85.3%) 7 missing values |
0.996 |
39/252 (13.4%/86.6%) 10 missing values |
8/44 (15.4%/84.6%) 5 missing values |
10/44 (18.5%/81.5%) 2 missing values |
0.600 |
|
Plank position (SD) (s) |
76.0 (± 49.7) 32 missing values |
68.5 (± 46.7) 14 missing values |
75.9 (± 44.3) 3 missing values |
80.6 (± 53.4) 4 missing values |
0.104 |
71.7 (± 47.6) 21 missing values |
81.2 (± 52.6) 1 missing value |
80.1 (± 51.3) 3 missing values |
0.262 |
SD = standard deviation
bold: statistically significant at the significance level of 0.017 (corrected for multiple comparisons)
a statistically not significant at the significance level of 0.017 (corrected for multiple comparisons)
Fig. 3.
Psychophysical variables and findings from the clinical examination for the three subgroups of pain severity in lifetime (left column) and during the last week (right column)
Table 6 shows that in the multivariable logistic regression models adjusted for age and gender (imputed data), the subgroup with most severe pain had, compared to the participants without pain, statistically significantly higher odds for reporting head and/or belly pain (most severe spinal pain during lifetime: OR = 2.3, 95%CI = 1.2–4.3; in the last week: OR = 2.6, 95%CI = 1.2–5.5). In addition, compared to having no spinal pain the report of one-sited severe pain or pain at multiple sites in the last week increased the odds for reporting daytime tiredness (OR = 3.2, 95%CI = 1.3–7.9). There was no collinearity between the independent variables: tolerance values were between 0.75 and 0.96 and VIF values between 1.04 and 1.34.
Table 6.
Multivariable logistic regression model for the psychophysical variables and findings from the clinical examination as independent variables and pain severity as dependent variable
| No pain (= 0) versus one-sited moderate pain (= 1) | ||||||||
|
Spinal pain severity lifetime Nagelkerke R2 = 0.09, Hosmer-Lemeshow = 0.47 (original data) |
Spinal pain severity last week Nagelkerke R2 = 0.07, Hosmer-Lemeshow = 0.99 (original data) |
|||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | -2.69 (0.59) | < 0.001 | 0.07 | 0.02–0.22 | -3.44 (0.65) | < 0.001 | 0.03 | 0.01–0.12 |
| Age | 0.16 (0.06) | 0.005 | 1.18 | 1.05–1.31 | 0.11 (0.06) | 0.049a | 1.12 | 1.00–1.26 |
| Gender (f = 0, m = 1) | -0.31 (0.28) | 0.256 | 0.73 | 0.43–1.26 | 0.07 (0.32) | 0.826 | 1.07 | 0.57–2.03 |
| Head and/or belly pain (No = 0, Yes = 1) | 0.51 (0.29) | 0.079 | 1.66 | 0.94–2.91 | 0.48 (0.31) | 0.120 | 1.61 | 0.88–2.94 |
| Sleep problems (No = 0, Yes = 1) | 0.16 (0.42) | 0.710 | 1.17 | 0.51–2.67 | -0.28 (0.44) | 0.527 | 0.76 | 0.32–1.80 |
| Daytime tiredness (No = 0, Yes = 1) | 0.03 (0.46) | 0.950 | 1.03 | 0.41–2.58 | 0.98 (0.44) | 0.033a | 2.66 | 1.09–6.52 |
| Rib hump (No = 0, Yes = 1) | 0.02 (0.41) | 0.963 | 1.02 | 0.45–2.29 | -0.10 (0.45) | 0.824 | 0.91 | 0.38–2.80 |
| Plank position | 0.001 (0.003) | 0.801 | 1.00 | 0.99–1.01 | 0.003 (0.003) | 0.413 | 1.00 | 1.00–1.01 |
| One-sited moderate pain (= 0) versus one-sited severe or multiple moderate or severe pain (= 1) | ||||||||
|
Spinal pain severity lifetime Nagelkerke R2 = 0.15, Hosmer-Lemeshow = 0.77 (original data) |
Spinal pain severity last week Nagelkerke R2 = 0.13, Hosmer-Lemeshow = 0.86 (original data) |
|||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | -2.11 (0.74) | 0.005 | 0.12 | 0.03–0.52 | -2.19 (1.00) | 0.028 | 0.11 | 0.02–0.79 |
| Age | 0.18 (0.07) | 0.011 | 1.20’ | 1.01–1.40 | 0.16 (0.08) | 0.047a | 1.18 | 1.00–1.38 |
| Gender (f = 0, m = 1) | 0.39 (0.32) | 0.230 | 1.48 | 0.78–2.80 | -0.27 (0.44) | 0.537 | 0.76 | 0.32–1.81 |
| Head and/or belly pain (No = 0, Yes = 1) | 0.39 (0.35) | 0.265 | 1.47 | 0.74–2.93 | 0.40 (0.46) | 0.390 | 1.49 | 0.60–3.70 |
| Sleep problems (No = 0, Yes = 1) | 0.33 (0.44) | 0.452 | 1.39 | 0.59–3.29 | 0.92 (0.52) | 0.079 | 2.51 | 0.90–7.01 |
| Daytime tiredness (No = 0, Yes = 1) | 0.82 (0.40) | 0.041a | 2.27 | 1.04–4.95 | 0.05 (0.49) | 0.924 | 1.05 | 0.39–2.79 |
| Rib hump (No = 0, Yes = 1) | -0.30 (0.48) | 0.534 | 0.74 | 0.28–1.94 | 0.07 (0.55) | 0.894 | 1.08 | 0.37–3.14 |
| Plank position | 0.003 (0.003) | 0.748 | 1.00 | 0.99–1.01 | -0.002 (0.005) | 0.661 | 1.00 | 0.99–1.01 |
| No pain (= 0) versus one-sited severe or multiple moderate or severe pain (= 1) | ||||||||
|
Spinal pain severity lifetime Nagelkerke R2 = 0.29, Hosmer-Lemeshow = 0.86 (original data) |
Spinal pain severity last week Nagelkerke R2 = 0.25, Hosmer-Lemeshow = 0.83 (original data) |
|||||||
| B (SE) | p value | OR | CI (OR) | B (SE) | p value | OR | CI (OR) | |
| Intercept | -4.44 (0.60) | < 0.001 | 0.01 | 0.00–0.04 | -5.49 (0.80) | < 0.001 | 0.00 | 0.00–0.02 |
| Age | 0.32 (0.06) | < 0.001 | 1.38 | 1.23–1.54 | 0.25 (0.06) | < 0.001 | 1.28 | 1.13–1.45 |
| Gender (f = 0, m = 1) | 0.04 (0.29) | 0.888 | 1.04 | 0.58–1.86 | -0.25 (0.39) | 0.523 | 0.78 | 0.36–1.71 |
| Head and/or belly pain (No = 0, Yes = 1) | 0.83 (0.31) | 0.011 | 2.30 | 1.22–4.33 | 0.96 (0.37) | 0.012 | 2.61 | 1.24–5.51 |
| Sleep problems (No = 0, Yes = 1) | 0.53 (0.39) | 0.177 | 1.70 | 0.78–3.70 | 0.47 (0.39) | 0.229 | 1.59 | 0.75–3.40 |
| Daytime tiredness (No = 0, Yes = 1) | 0.78 (0.37) | 0.037a | 2.19 | 1.05–4.57 | 1.18 (0.44) | 0.011 | 3.24 | 1.33–7.92 |
| Rib hump (No = 0, Yes = 1) | -0.29 (0.38) | 0.456 | 0.75 | 0.35–1.60 | 0.04 (0.46) | 0.939 | 1.04 | 0.42–2.54 |
| Plank position | -0.001 (0.003) | 0.809 | 1.00 | 0.99–1.01 | 0.003 (0.004) | 0.502 | 1.00 | 0.99–1.01 |
CI = confidence interval, f = female, m = male, OR = odds ratio
bold: statistically significant (significance level = 0.017; corrected for multiple comparisons)
a statistically not significant (significance level = 0.017; corrected for multiple comparisons)
Correlation between spinal pain during lifetime and last week
The correlation between spinal pain during lifetime and during the last week was 0.60 (p < 0.001) when considering the three subgroups of pain severity. The median of the difference between these two measures calculated over all participants was 0 with an interquartile range of 1. Approximately half (58.6%) of the participants were in the same severity subgroup for pain during lifetime and in the last week, 38% reported more severe spinal pain during lifetime compared to the last week, and 3.5% of the participants reported the experience of higher pain severity in the last week than during lifetime (non-imputed data).
Discussion
Summary of main findings
The sample of this study was population-based and consisted of Swiss children and adolescents between six and 16 years of age (with or without spinal pain) who underwent a spinal screening that included a questionnaire and a chiropractic clinical examination. Of the 457 participants, approximately half (52%) reported having experienced at least moderate spinal pain in their life, and a quarter (27%) in the last week. Approximately a third (32%) reported the experience of severe spinal pain at one site or of moderate or severe pain at multiple sites in life and 14% in the last week. With regard to the consequences of spinal pain, the participants in the subgroup with most severe pain, regardless of asked for spinal pain in lifetime or in the last week, and the participants with moderate pain at one spinal site in the last week, rated their health significantly worse because of spinal pain and sought more often medical advice because of this condition than did the participants without spinal pain. With regard to the psychophysiological parameters, the participants in the subgroup with most severe pain reported more co-existing head and/or belly pain (when asked for spinal pain in lifetime and in the last week) and daytime tiredness (only when asked for spinal pain in the last week) than the subgroup without spinal pain. However, the participants with moderate pain at one spinal site, regardless of during lifetime or in the last week, did not differ in these numbers from those without spinal pain. The clinical tests for trunk muscle endurance and trunk asymmetry were not associated with pain severity at all.
The finding that 13.5% of all participants in the present study reported severe pain (either severe pain in one spinal area or at least moderate pain in more than one spinal area) is consistent with the results of a study by Aartun and colleagues [21]. That study was also based on the YSQ and thus investigated the three spinal areas neck, mid back, and lower back separately. Although the authors did not merge pain intensity and pain frequency to a combined measure for pain severity, they found a group of 13.6% (95% CI: 11.8–15.6) of the 1300 participants between 11 and 13 years of age who reported frequent pain of high intensity. For a similar age group (11 to 14 years), the present study found that 14.4% of the participants reported most severe pain (severe pain in one spinal area or at least moderate pain in more than one spinal area). Not surprisingly, pain severity was associated with the measures for consequences of pain. Notably, not only the participants in the subgroup with most severe pain, but also those in the subgroup with moderate pain at one spinal site in the last week, but not during lifetime, reported higher impact of their spinal pain on health and seeking medical advice because of spinal pain more frequently than those in the ‘no pain’-subgroup (that in fact includes very mild occasional pain). Thus, early recognition of those children and adolescents who reported impaired self-rated health because of spinal pain is highly relevant. Even moderate pain in one spinal area in the last week can have a negative impact on the lives of these young people. This might remain hidden when asking for longer recall periods: e.g., Watson and colleagues asked schoolchildren for LBP in the last month and reported that seeking health care was rare [38]. The results of the present study suggest that asking in detail for pain frequency and pain intensity in the last week is superior to asking for lifetime pain when it comes to distinguish potentially consequential from self-limiting (‘trivial’) spinal pain in childhood and adolescence. However, there is no gold standard for the best recall period as this is always a trade-off between bias (e.g. recall bias) and precision of the depicted pattern [39].
With regard to the association between clinical parameters and pain severity, the present study considered only trunk asymmetry and trunk muscle endurance because these two variables have previously been shown to be associated with spinal pain in childhood and adolescence [14, 15]. However, regardless of pain severity, the present study found no association between these parameters and spinal pain (e.g., not even in the subgroup with most severe pain). Together with the findings of a school-based 2-years prospective study by Aartun and colleagues [40], which found no predictive value of tests for trunk extensor muscle endurance and scoliosis, this finding questions the relevance of these tests. Prospective studies in community-based as well as clinical settings are needed to clarify the value of these tests in the prognosis of (i) the onset of spinal pain in previously pain-free children and adolescents and (ii) the clinical course/trajectory of children and adolescents with spinal pain.
With regard to the association between psychophysical variables and pain severity, most severe pain was associated with co-existing head and/or belly pain (when asked for spinal pain in lifetime and in the last week) and daytime tiredness (only when asked for spinal pain in the last week). In line, a large study in adults reported that the number of co-existing pain sites reflected the severity and impact of a pain condition [41]. Also in children and adolescents, co-existence of abdominal pain, headache and spinal pain has been reported before [17, 18] and an association with school stress had been shown [42]. Furthermore, a systematic review on prospective studies on risk factors for ongoing pain in children and adolescents with persisting pain regardless of etiology reported weekly day tiredness and weekly abdominal pain to be risk factors for the presence of pain at follow-up after one year [20].
In line with the results of the present study, Watson and colleagues reported in a similar study no association between LBP and mechanical factors (body mass index, school bag weight, heavy lifting, physical activity), but strong associations with emotional problems [18]. The results of both studies, notably investigating different mechanical aspects, supports the notion that spinal pain in childhood and adolescence is not a local, mechanical condition but might rather indicate a general “vulnerability” to stress and pain [43]. This vulnerability might be induced by mechanisms of central sensitization that can, despite the absence of any structural pathology, lead to pain hypersensitivity [44] as shown in a systematic review in children with various pain conditions [45]. In line, a study that used quantitative sensory testing in pediatric patients with chronic back pain identified a pain-sensitive cluster with low thermal and pressure pain thresholds [46]. Furthermore, there is evidence that an increased reactivity of the Hypothalamic-Pituitary-Adrenal (HPA) axis, induced e.g. by an adverse event in childhood [47], can predispose to pain [48, 49]. There seems to exist a link between pain vulnerability and early life stress, e.g. preterm birth including the (noxious) experience of neonatal care [50], childhood traumata and the experience of parental chronic pain [51], that can predispose to pain via changes in endogenous pain modulatory mechanisms and increased levels of inflammatory biomarkers [50, 51].
Altogether, the participants in the subgroup with most severe pain in the present study might be regarded at risk for consequential pain and disability in the future as they not only reported an impact of their spinal pain on health and often sought medical advice because of spinal pain but also complained about co-existing headache and belly pain. The early identification of these children and adolescents is a prerequisite for initiating appropriate treatment and management that potentially lessens individual suffering and reduces health costs by proper allocation of resources. Even the children and adolescents who reported moderate pain at one site in the last week deserve particular attention. They did not report worse self-rated health than those in the ‘no pain’ subgroup. Nevertheless, the perceived impairment of self-rated health by spinal pain as well as the frequent search for medical advice could have implications for adulthood. In contrast, those children and adolescents who experienced moderate spinal pain (which includes the whole spectrum from frequent mild pain to intense rare pain) in one spinal area during lifetime did not differ from the ‘no pain’ subgroup with regard to both, the consequences of spinal pain and associated psychophysical factors. This condition, together with very mild and rare pain that is included per definition in the ‘no pain’ subgroup, might thus be regarded as self-limiting (‘trivial’). These conditions should not be ‘over-medicalized’ and reassurance that the condition is not serious and recommendation for staying active [52] might be sufficient to manage those children and adolescents.
Strengths and limitations
The major strengths of the present study are its comprehensive characterization of spinal pain, including the three different spinal areas, assessing pain frequency and intensity with two recall periods, and asking for consequences of spinal pain and potentially associated factors. Nevertheless, this population-based study has several inherent limitations. Because both, the participants and the chiropractors participated voluntarily in the screening event, selection bias is likely to be present, which does not allow generalizing the study results. However, the large heterogeneity in terms of participants’ age and their dispersed origins from all over Switzerland increases the study’s external validity. As a further limitation, the questions that were either adapted (sub-questions on pain frequency and pain intensity during the last week) or added to the validated questionnaires (questions on co-existing pain, sleep problems and impact of spinal pain on health) were neither validated nor pilot-tested. Nevertheless, the relevance of these factors in the context of pain in childhood and adolescence has been shown [20]. With regard to the clinical examination, the present study included only two parameters, for which there is evidence for playing a role in adolescent spinal pain (rib hump/scoliosis: [12, 13, 53]; trunk muscle endurance: [54–56]). However, the present study found no association of these two parameters with pain severity, which might be explained by several methodological differences: the studies on the association of rib hump/scoliosis and spinal pain focused either on LBP [12, 13], relied on self-report [12], or found an association only in girls [53]. The studies on trunk muscle endurance tested either the endurance of back muscles using the Biering-Sorensen test [54, 55] or the abdominal muscles using a sit-up test [56]. The plank position as used in this study, tests both, the back muscles and predominantly the abdominal muscles [57]. Thus, these different assessments might not be directly comparable. In any case, the inclusion of only two clinical parameters does not exclude the possibility that other clinical parameters would have been associated with spinal pain severity. With a view to the assessment of the psychophysical parameters, they were based on self-report and it was not standardized whether the children, their parents or both filled in the questionnaire. Answers of parents and children are not interchangeable [58] with spinal pain and tiredness being under-reported and under-rated by the parents [59], but the wide age range of study participants in the present study did hardly allow for standardization. Furthermore, although the study population was relatively large, the small number of participants in the extreme categories of pain severity did not allow for further subdividing pain severity (e.g. no pain, moderate pain at one site, severe pain at one site, moderate pain at multiple sites, and severe pain at multiple sites). However, looking at those categories separately might give further insight into potentially consequential spinal pain that requires adequate treatment. Lastly, this cross-sectional study shows associations, but does not allow inferring causality. Prospective studies are needed that (i) start with a pain free cohort of children early in childhood and investigate the occurrence and interaction of potential pain sites and (ii) follow the children and adolescents of the different subgroups of pain severity into early adulthood to depict the development of the pain patterns. Preferably, such studies include, besides psychophysical and mechanical variables, also psychological measures such as anxiety and sensitivity to anxiety (fear of anxiety), which both were shown to be relevant in the development of chronic pain conditions in children and adolescents [60, 61].
Conclusion
This study showed an association between some consequences of spinal pain (impact of spinal pain on self-rated health, seeking medical advice because of spinal pain) as well as some psychophysical factors (head and/or belly pain and daytime tiredness) and pain severity, while no such association was observed for the investigated clinical factors (trunk asymmetry, trunk muscle endurance). Thus, stratification by pain severity might help to minimize under- and over-medicalization of spinal pain in childhood and adolescence by distinguishing between potentially consequential and self-limiting pain conditions. However, prospective studies are needed that follow children and adolescents of different subgroups of pain severity into early adulthood to verify the suggestions of the present study on how to differentiate between potentially consequential and self-limiting spinal pain conditions. Prospective studies are also needed to clarify the relevance of the investigated clinical tests in the context of adolescent spinal pain as the present study found no association of those to pain severity.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the involved chiropractors for collecting the data and Lucas Tauschek and Simon Carisch for building the database.
Author contributions
BW, MHS and PSch conceptualized the study. CK and BW performed the data analysis. CK wrote the first manuscript draft, which was finalized by BW and PSch. All authors contributed to and approved the final manuscript.
Funding
BW received salary support from the Swiss Chiropractors’ Association ChiroSuisse, which is not bound to any specific project. The funder did not have any specific role in this project.
Data availability
The datasets used in the current study are available from the corresponding author on request
Declarations
Ethics approval and consent to participate
The questionnaire and the examination form used for this study were completely anonymous. An approval from the ethics review board of the Canton of Zurich was requested, but was by law not necessary (BASEC req-2020-00825 and req-2023-01333).
Consent for publication
Not applicable (completely anonymous data).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Disease and Injury Incidence and, Prevalence Collaborators G. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamper SJ, Henschke N, Hestbaek L, Dunn KM, Williams CM. Musculoskeletal pain in children and adolescents. Braz J Phys Ther. 2016;20(3):275–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kjaer P, Wedderkopp N, Korsholm L, Leboeuf-Yde C. Prevalence and tracking of back pain from childhood to adolescence. BMC Musculoskelet Disord. 2011;12:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain: a systematic overview of the research literature. Spine. 2007;32(23):2630–7. [DOI] [PubMed] [Google Scholar]
- 5.Junge T, Wedderkopp N, Boyle E, Kjaer P. The natural course of low back pain from childhood to young adulthood - a systematic review. Chiropr Man Ther. 2019;27:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C. The course of low back pain from adolescence to adulthood: eight-year follow-up of 9600 twins. Spine (Phila Pa 1976). 2006;31(4):468–72. [DOI] [PubMed] [Google Scholar]
- 7.Hestbaek L, Leboeuf-Yde C, Kyvik KO. Are lifestyle-factors in adolescence predictors for adult low back pain? A cross-sectional and prospective study of young twins. BMC Musculoskelet Disord. 2006;7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frosch M, Mauritz MD, Bielack S, Blodt S, Dirksen U, Dobe M et al. Etiology, risk factors, and diagnosis of Back Pain in Children and adolescents: evidence- and Consensus-based interdisciplinary recommendations. Child (Basel). 2022;9(2). [DOI] [PMC free article] [PubMed]
- 9.Yang S, Werner BC, Singla A, Abel MF. Low back Pain in adolescents: a 1-Year analysis of eventual diagnoses. J Pediatr Orthop. 2017;37(5):344–7. [DOI] [PubMed] [Google Scholar]
- 10.Stinson J, Connelly M, Kamper SJ, Herlin T, Toupin April K. Models of care for addressing chronic musculoskeletal pain and health in children and adolescents. Best Pract Res Clin Rheumatol. 2016;30(3):468–82. [DOI] [PubMed] [Google Scholar]
- 11.Calvo-Munoz I, Kovacs FM, Roque M, Gago Fernandez I, Seco Calvo J. Risk factors for low back Pain in Childhood and Adolescence: a systematic review. Clin J Pain. 2018;34(5):468–84. [DOI] [PubMed] [Google Scholar]
- 12.Kovacs FM, Gestoso M, Gil del Real MT, Lopez J, Mufraggi N, Mendez JI. Risk factors for non-specific low back pain in schoolchildren and their parents: a population based study. Pain. 2003;103(3):259–68. [DOI] [PubMed] [Google Scholar]
- 13.Nissinen M, Heliovaara M, Seitsamo J, Alaranta H, Poussa M. Anthropometric measurements and the incidence of low back pain in a cohort of pubertal children. Spine. 1994;19(12):1367–70. [DOI] [PubMed] [Google Scholar]
- 14.Potthoff T, de Bruin ED, Rosser S, Humphreys BK, Wirth B. A systematic review on quantifiable physical risk factors for non-specific adolescent low back pain. J Pediatr Rehabil Med. 2018;11(2):79–94. [DOI] [PubMed] [Google Scholar]
- 15.Noll M, Kjaer P, Mendonca CR, Wedderkopp N. Motor performance and back pain in children and adolescents: a systematic review. Eur J Pain. 2022;26(1):77–102. [DOI] [PubMed] [Google Scholar]
- 16.Beynon AM, Hebert JJ, Hodgetts CJ, Boulos LM, Walker BF. Chronic physical illnesses, mental health disorders, and psychological features as potential risk factors for back pain from childhood to young adulthood: a systematic review with meta-analysis. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European section of the cervical. Spine Res Soc. 2020;29(3):480–96. [DOI] [PubMed] [Google Scholar]
- 17.Swain MS, Henschke N, Kamper SJ, Gobina I, Ottova-Jordan V, Maher CG. An international survey of pain in adolescents. BMC Public Health. 2014;14:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DP, Silman AJ, et al. Low back pain in schoolchildren: the role of mechanical and psychosocial factors. Arch Dis Child. 2003;88(1):12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beales DJ, Smith AJ, O’Sullivan PB, Straker LM. Low back pain and comorbidity clusters at 17 years of age: a cross-sectional examination of health-related quality of life and specific low back pain impacts. J Adolesc Health: Official Publication Soc Adolesc Med. 2012;50(5):509–16. [DOI] [PubMed] [Google Scholar]
- 20.Pate JW, Hancock MJ, Hush JM, Gray K, Pounder M, Pacey V. Prognostic factors for pain and functional disability in children and adolescents with persisting pain: a systematic review and meta-analysis. Eur J Pain. 2020;24(4):722–41. [DOI] [PubMed] [Google Scholar]
- 21.Aartun E, Hartvigsen J, Wedderkopp N, Hestbaek L. Spinal pain in adolescents: prevalence, incidence, and course: a school-based two-year prospective cohort study in 1,300 danes aged 11–13. BMC Musculoskelet Disord. 2014;15:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hill J, Keating J. Risk factors for the first episode of low back pain in children are infrequently validated across samples and conditions: a systematic review. J Physiotherapy. 2010;56:237–44. [DOI] [PubMed] [Google Scholar]
- 23.Lauridsen HH, Hestbaek L. Development of the young spine questionnaire. BMC Musculoskelet Disord. 2013;14:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyiro L, Potthoff T, Siegenthaler MH, Riner F, Schweinhardt P, Wirth B. Translation and validation of the German version of the Young Spine Questionnaire. BMC Pediatr. 2021;21(1):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain. 2001;93(2):173–83. [DOI] [PubMed] [Google Scholar]
- 26.Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125(1–2):143–57. [DOI] [PubMed] [Google Scholar]
- 27.El-Metwally A, Salminen JJ, Auvinen A, Kautiainen H, Mikkelsson M. Lower limb pain in a preadolescent population: prognosis and risk factors for chronicity–a prospective 1- and 4-year follow-up study. Pediatrics. 2005;116(3):673–81. [DOI] [PubMed] [Google Scholar]
- 28.HBSC. Health Behaviour in School-Aged Children - Survey protocols: WHO; [ https://hbsc.org/publications/survey-protocols/
- 29.Mikkelsson M, El-Metwally A, Kautiainen H, Auvinen A, Macfarlane GJ, Salminen JJ. Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain. 2008;138(3):681–7. [DOI] [PubMed] [Google Scholar]
- 30.Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5(3):353–64. [DOI] [PubMed] [Google Scholar]
- 31.Lee CF, Fong DY, Cheung KM, Cheng JC, Ng BK, Lam TP, et al. Referral criteria for school scoliosis screening: assessment and recommendations based on a large longitudinally followed cohort. Spine. 2010;35(25):E1492–8. [DOI] [PubMed] [Google Scholar]
- 32.Boyer C, Tremblay M, Saunders TJ, McFarlane A, Borghese M, Lloyd M, et al. Feasibility, validity and reliability of the plank isometric hold as a field-based assessment of torso muscular endurance for children 8–12 years of age. Pediatr Exerc Sci. 2013;25(3):407–22. [DOI] [PubMed] [Google Scholar]
- 33.Cowley PM, Fitzgerald S, Sottung K, Swensen T. Age, weight, and the front abdominal power test as predictors of isokinetic trunk strength and work in young men and women. J Strength Cond Res. 2009;23(3):915–25. [DOI] [PubMed] [Google Scholar]
- 34.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joergensen AC, Hestbaek L, Andersen PK, Nybo Andersen AM. Epidemiology of spinal pain in children: a study within the Danish National Birth Cohort. Eur J Pediatr. 2019;178(5):695–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Field A. Discovering statistics using SPSS. 3rd ed. Los Angeles: SAGE; 2018. [Google Scholar]
- 37.Hardin AP, Hackell JM, Committee On P, Ambulatory M. Age Limit of Pediatrics. Pediatrics. 2017;140(3). [DOI] [PubMed]
- 38.Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DP, Silman AJ, et al. Low back pain in schoolchildren: occurrence and characteristics. Pain. 2002;97(1–2):87–92. [DOI] [PubMed] [Google Scholar]
- 39.Norquist JM, Girman C, Fehnel S, DeMuro-Mercon C, Santanello N. Choice of recall period for patient-reported outcome (PRO) measures: criteria for consideration. Qual Life Res. 2012;21(6):1013–20. [DOI] [PubMed] [Google Scholar]
- 40.Aartun E, Hartvigsen J, Hestbaek L. Validity of commonly used clinical tests to diagnose and screen for spinal Pain in adolescents: a School-based Cohort Study in 1300 Danes aged 11–15 years. J Manip Physiol Ther. 2016;39(2):76–87. [DOI] [PubMed] [Google Scholar]
- 41.Tanguay-Sabourin C, Fillingim M, Guglietti GV, Zare A, Parisien M, Norman J, et al. A prognostic risk score for development and spread of chronic pain. Nat Med. 2023;29(7):1821–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hjern A, Alfven G, Ostberg V. School stressors, psychological complaints and psychosomatic pain. Acta Paediatr. 2008;97(1):112–7. [DOI] [PubMed] [Google Scholar]
- 43.Egloff N, Dung C, Ott R. [Not available]. Ther Umsch. 2017;74(5):254–60. [DOI] [PubMed] [Google Scholar]
- 44.Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339–56. [DOI] [PubMed] [Google Scholar]
- 45.Pas R, Ickmans K, Van Oosterwijck S, Van der Cruyssen K, Foubert A, Leysen L, et al. Hyperexcitability of the Central Nervous System in Children with Chronic Pain: a systematic review. Pain Med. 2018;19(12):2504–14. [DOI] [PubMed] [Google Scholar]
- 46.Ocay DD, Loewen A, Premachandran S, Ingelmo PM, Saran N, Ouellet JA, et al. Psychosocial and psychophysical assessment in paediatric patients and young adults with chronic back pain: a cluster analysis. Eur J Pain. 2022;26(4):855–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tidmarsh LV, Harrison R, Ravindran D, Matthews SL, Finlay KA. The influence of adverse childhood experiences in Pain Management: mechanisms, processes, and trauma-informed care. Front Pain Res (Lausanne). 2022;3:923866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McBeth J, Chiu YH, Silman AJ, Ray D, Morriss R, Dickens C, et al. Hypothalamic-pituitary-adrenal stress axis function and the relationship with chronic widespread pain and its antecedents. Arthritis Res Ther. 2005;7(5):R992–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McBeth J, Silman AJ, Gupta A, Chiu YH, Ray D, Morriss R, et al. Moderation of psychosocial risk factors through dysfunction of the hypothalamic-pituitary-adrenal stress axis in the onset of chronic widespread musculoskeletal pain: findings of a population-based prospective cohort study. Arthritis Rheum. 2007;56(1):360–71. [DOI] [PubMed] [Google Scholar]
- 50.Goffaux P, Lafrenaye S, Morin M, Patural H, Demers G, Marchand S. Preterm births: can neonatal pain alter the development of endogenous gating systems? Eur J Pain. 2008;12(7):945–51. [DOI] [PubMed] [Google Scholar]
- 51.Delgado-Sanchez A, Brown C, Sivan M, Talmi D, Charalambous C, Jones AKP. Are we any closer to understanding how chronic Pain develops? A systematic search and critical narrative review of existing Chronic Pain Vulnerability models. J Pain Res. 2023;16:3145–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hebert JJ, Beynon AM, Jones BL, Wang C, Shrier I, Hartvigsen J, et al. Spinal pain in childhood: prevalence, trajectories, and diagnoses in children 6 to 17 years of age. Eur J Pediatr. 2022;181(4):1727–36. [DOI] [PubMed] [Google Scholar]
- 53.Wirth B, Knecht C, Humphreys K. Spine Day 2012: spinal pain in Swiss school children- epidemiology and risk factors. BMC Pediatr. 2013;13:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Astfalck RG, O’Sullivan PB, Straker LM, Smith AJ. A detailed characterisation of pain, disability, physical and psychological features of a small group of adolescents with non-specific chronic low back pain. Man Therap. 2010;15(3):240–7. [DOI] [PubMed] [Google Scholar]
- 55.Bernard JC, Bard R, Pujol A, Combey A, Boussard D, Begue C, et al. Muscle assessment in healthy teenagers, comparison with teenagers with low back pain. Ann Readapt Med Phys. 2008;51(4):263–83. [DOI] [PubMed] [Google Scholar]
- 56.Jones MA, Stratton G, Reilly T, Unnithan VB. Biological risk indicators for recurrent non-specific low back pain in adolescents. Br J Sports Med. 2005;39(3):137–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Youdas JW, Coleman KC, Holstad EE, Long SD, Veldkamp NL, Hollman JH. Magnitudes of muscle activation of spine stabilizers in healthy adults during prone on elbow planking exercises with and without a fitness ball. Physiother Theory Pract. 2018;34(3):212–22. [DOI] [PubMed] [Google Scholar]
- 58.Kamper SJ, Dissing KB, Hestbaek L. Whose pain is it anyway? Comparability of pain reports from children and their parents. Chiropr Man Ther. 2016;24:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sundblad GM, Saartok T, Engstrom LM. Child-parent agreement on reports of disease, injury and pain. BMC Public Health. 2006;6:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jastrowski Mano KE, O’Bryan EM, Gibler RC, Beckmann E. The co-occurrence of Pediatric Chronic Pain and anxiety: a theoretical review of a developmentally informed Shared Vulnerability Model. Clin J Pain. 2019;35(12):989–1002. [DOI] [PubMed] [Google Scholar]
- 61.Tegethoff M, Belardi A, Stalujanis E, Meinlschmidt G. Comorbidity of Mental disorders and Chronic Pain: Chronology of Onset in adolescents of a National Representative Cohort. J pain: Official J Am Pain Soc. 2015;16(10):1054–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used in the current study are available from the corresponding author on request