Abstract
Purpose
This study outlines the initiation of an interprofessional education (IPE) program designed for optometry and education students. The program aimed to foster interdisciplinary collaboration and improve the management of eye health in children with special educational needs (SEN) – a vulnerable and underserved group.
Methods
This program incorporated lectures and workshops to impart essential knowledge about SEN and to develop the necessary attitudes and skills for conducting eye examinations. A key component involved vision screenings at two special education schools, where optometry (n = 43) and education students (n = 39) collaborated to serve 170 children with mild to moderate intellectual disabilities. Quantitative data was gathered pre- and post-program using a single-stage, five-level Likert scale. Qualitative insights were drawn from students’ reflective writings to evaluate their learning outcomes, understanding, and confidence in managing eye health for children with SEN.
Results
Of the participants, 37 optometry and 21 education students completed the survey (70.7% response rate). The survey results indicated significant improvements in understanding SEN characteristics (p ≤ 0.013) and increased confidence when conducting eye examinations for children with SEN (p < 0.007) after the training program. The analysis of reflective writings highlighted the program’s beneficial impacts on students. They recognized the value of interprofessional collaboration, reported enhanced professional competence, gained deeper insights into their own and their peers’ roles within multidisciplinary teams, and developed a strengthened sense of social responsibility.
Conclusion
This IPE program proved to be an effective method for enhancing optometry and education students’ knowledge and confidence in managing eye health needs of children with SEN. The findings support the advocacy for continued collaborative efforts between healthcare providers and educators to ensure comprehensive care for this population. Such disciplinary collaboration provides positive evidence in early stages of training in both disciplines.
Clinical trial number
Not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06350-w.
Keywords: Interprofessional education, Healthcare education, Optometry education
Introduction
Cultivating professionalism within healthcare education is pivotal to ensure that future healthcare practitioners are not only technically proficient but also ethically grounded and socially responsible. The integration of Situated Learning Theory (SLT) into healthcare education has been identified as a critical strategy to foster the professional development of healthcare students [1]. The core components of SLT are setting an authentic environment, providing opportunities for students to build relationships with peers, and offering chances to learn from mentors [1–6]. These three components emphasize that learning occurs when students engage in community practices characterized by a shared domain of interest, joint activities, information sharing, relationship building, and development of shared resources for practice [5]. This educational model is particularly relevant for interprofessional education programs aimed at developing interprofessional collaboration skills among students from diverse disciplines. This article presents an interprofessional education initiative which adopts the SLT framework for students in the fields of optometry and education, with the goal of promoting holistic eye care for children with special education needs (SEN).
The intersection of healthcare and education professionals is critical in the developmental trajectory of children with SEN. These children, who may experience a range of physical, mental, and developmental conditions such as intellectual disabilities, attention deficit hyperactivity disorder, or autism spectrum disorder, are frequently at an elevated risk of vision problems [7–9], including uncorrected refractive errors [10, 11] and congenital ocular diseases [12]. For instance, research indicates a significant association between Attention Deficit Hyperactivity Disorder (ADHD) and various vision problems in children [13]. Specific conditions such as astigmatism and hyperopia/hypermetropia both have an OR of 1.79, indicating a higher prevalence among children with ADHD. Strabismus shows a strong link with an OR of 1.93, while unspecified vision problems have an OR of 1.94, suggesting a notable correlation. Particularly, reduced near point of convergence presents a significant risk factor with an OR of 5.02. However, studies have shown that up to 50% of children with SEN suffer from undiagnosed vision issues, which can further complicate their learning and development [7–12, 14]. Despite the high prevalence of visual impairments, eye care for these children is often inadequate or delayed [7, 11, 14]. Their limited communication proficiency and restricted cooperative behavior often impede their ability to effectively express their visual symptoms and problems. This social behavioral barrier can lead to misconceptions about the child’s visual status among healthcare practitioners, schoolteachers, and parents, potentially resulting in delayed treatments and interventions.
Optometrists play a pivotal role in addressing vision problems, yet traditional optometry training may not fully equip practitioners to manage the unique complexities presented by children with SEN. These children often exhibit behavioral and emotional challenges that can complicate eye examinations, making it essential for optometrists to receive specialized training. Similarly, while schoolteachers are in close daily contact with these children and are ideally placed to identify early signs of visual impairment [15], vision care is not typically part of standard teacher education programs. This gap between healthcare and education professionals leads to missed opportunities for early detection and intervention, which can have long-term consequences for both the visual and overall development of children with SEN.
To provide truly comprehensive care, optometry students must be trained not only in addressing vision problems but also in navigating the behavioral and emotional needs of children with SEN. This specialized training would enhance their professional competence and foster empathy, ensuring that these children receive the individualized eye care they require. At the same time, teachers, who often serve as the first line of defense in recognizing potential ocular issues, should be educated on the importance of eye health. By being equipped to detect early signs of vision problems, teachers can help prevent long-term visual impairments.
As the healthcare landscape continues to evolve, the necessity for a collaborative approach to patient care is becoming increasingly paramount [16, 17]. Interprofessional education has emerged as a revolutionary educational strategy that encourages interactive learning among two or more professions with the primary objective of enhancing collaboration and improving the quality of care [18]. It transcends the traditional boundaries of learning ‘about’ each other’s roles, promoting learning ‘from’ and ‘with’ each other.
Building on the foundations of SLT, we have established an interprofessional education program designed to bridge the gap in knowledge and practice between optometry and education. These two distinct yet intrinsically linked disciplines are unified in our program to create a more contextually rich learning experience. Our objective is to foster interprofessional collaboration that delivers a holistic eye care for children with SEN. Our program not only strives to enhance students’ competence across various levels of healthcare but also aims to instill a sense of empathy for the needs of vulnerable populations. This initiative is intended to shape professional identities and reinforce a commitment to social responsibility among students. In this article, we present preliminary data from the program, evaluating the efficacy of this collaborative model through both quantitative surveys and qualitative analyses of reflective writing.
Methods
This interprofessional education program was conducted in partnership between the School of Optometry at The Hong Kong Polytechnic University (PolyU) and the Institute of Special Needs and Inclusive Education at The Education University of Hong Kong (EdUHK). We employed a mixed-methods design, leveraging a simultaneous triangulation approach to ensure a comprehensive analysis of the data. This approach involved conducting quantitative and qualitative analyses independently and subsequently integrate the results. Such an approach facilitated a thorough examination of student learning outcomes. Additionally, the qualitative data provided complementary insights that enriched and expanded upon the quantitative findings. By combining these two distinct and complementary forms of data, a more comprehensive understanding of the impact of the interprofessional education program on student learning could be obtained.
Interprofessional Educational Program
The core of this education program was the integration of an interprofessional collaborative training into the existing curricula for optometry and education students. This module, grounded in the principles of SLT, involved a cohort of 43 optometry students (year 4) and 39 education students (year 2). It provided a practical, hands-on learning experience that emphasized the application of interdisciplinary knowledge in real-world contexts.
Preparation phase
During the preparation phase, both optometry and education students participated in interdisciplinary workshops designed to lay the foundational knowledge necessary for their respective roles in the project.
Optometry students were immersed in a series of workshops led by lecturers from the Institute of Special Needs and Inclusive Education at EdUHK. These workshops aimed to familiarize optometry students with the characteristics of children with SEN and strategies in handling their emotional needs (Fig. 1A). The content was divided into four modules, each focusing on a specific subtype of SEN:
Fig. 1.

The interprofessional collaborative training program. (A) Workshops provided by the teachers from The Education University of Hong Kong to the year 4 optometry students. (B) Laboratory sessions provided by the School of Optometry to the education students. (C) Vision screenings (visual acuity measure) organized by optometry and education students to serve the local special school students
Intellectual Disabilities: This module explored the diverse range of intellectual disabilities, their impact on communication and comprehension, and appropriate adaptations for eye examinations. Students learned techniques for simplifying instructions, using visual aids, and creating a patient and supportive environment to facilitate cooperation and minimize anxiety.
ADHD: This module focused on understanding the core characteristics of ADHD, including inattention, hyperactivity, and impulsivity, and their potential manifestations during eye examinations. Students learned strategies for managing distractibility, maintaining engagement, and adapting testing procedures to accommodate shorter attention spans. Emphasis was placed on creating a structured and predictable environment to minimize overstimulation and maximize focus.
Autism Spectrum Disorder (ASD): This module delved into the complexities of ASD, focusing on the communication and social interaction challenges frequently encountered during eye examinations. Students learned about the sensory sensitivities common in individuals with ASD and explored strategies for minimizing sensory overload and creating a calming atmosphere. The training emphasized the importance of clear and concise communication, visual supports, and individualized approaches to build rapport and facilitate cooperation.
Specific Learning Disorders: This module focused on understanding the characteristics of dyslexia and other specific learning differences and their impact on children’s learning and overall development. Students explored how these disorders can manifest in various daily tasks and activities, both in academic and everyday settings. This understanding will enable optometry students to provide more informed and tailored guidance to parents, facilitating better communication and collaboration in the child’s overall care.
In parallel, education students engaged in a 6-hour lecture series and a 2-hour practical training delivered by the School of Optometry at PolyU. The focus on these lectures was on pediatric eye care, with an emphasis on the common vision problems among children with SEN. The lectures were structured around the following topics:
Introduction of Optometry in the Context of SEN: This module provided an overview of the role of optometry in supporting children with SEN, emphasizing the crucial link between vision and learning, development, and overall well-being. explored how optometrists and teachers can work together to identify and address visual challenges that may impact a child’s learning and development.
Common Visual Problems in Children with SEN: This module explored prevalent vision problems frequently encountered in children with SEN, including refractive errors (myopia, hyperopia, astigmatism), strabismus (squint), amblyopia (lazy eye), and other visual impairments often associated with specific learning differences, autism spectrum disorder, and other developmental disabilities. The focus was on understanding how these conditions can impact learning and development.
Optometric Assessment and Management of Visual Impairments: This module provided an overview of the procedures involved in a comprehensive eye examination for children, explaining the various assessment techniques used to evaluate visual function and ocular health. Different management strategies, such as corrective lenses and vision therapy, were also discussed.
Strategies and Considerations of Conducting Vision Screening in Children with SEN: This module focused on practical strategies for conducting vision screenings in children with SEN. Students learned about different screening methods, adaptations for various SEN profiles, and the importance of effective communication and collaboration with parents, teachers, and optometrists to ensure appropriate follow-up and care. A 2-hour practical training session also provided hands-on experience with vision screening techniques and equipment, reinforcing the concepts covered in the lectures.
Through this mutual exchange of expertise, both groups of students were positioned to gain a holistic view of the needs of children with SEN, fostering a collaborative approach to their care.
Community of practice
Upon acquiring foundational knowledge about SEN, the optometry students transitioned into the community of practice stage of the project. They were divided into four groups, each tasked with the development of a vision screening plan. Under the mentorship of registered optometrists, these groups set out to tailor vision assessment procedures specifically suited for children with SEN. This planning process was informed by insights gained from the initial workshops and aimed at creating a set of tests that were appropriate and sensitive to the unique requirements of SEN children. Additionally, the groups worked on establishing a practical and efficient floor plan for the screening site to facilitate an orderly and efficient screening process.
Concurrently, education students participated in two laboratory sessions designed to introduce and refine eye examination skills (Fig. 1B). These sessions, conducted under the supervision of registered optometrists, provided them with valuable hands-on experience. The practical skills learned during these sessions were crucial, as the students were expected to apply this knowledge later during the actual vision screenings for children with SEN. These laboratory sessions served as a bridge between theoretical understanding and practical application, ensuring that the education students were well-prepared to contribute effectively to the upcoming vision screening initiative.
Vision screening execution
The execution of vision screenings was a key element of our education program, involving a synergistic effort between optometry and education students (Fig. 1C). These vision screenings were conducted at two local special schools, serving a total of 170 children with mild to moderate intellectual disabilities, under the supervision of teachers from both institutions. This practical application was designed to allow students to apply their knowledge in a real-world setting, fostering interdisciplinary collaboration, allowing them to learn from each other, gain insight into the distinct roles of each profession, and develop interprofessional communication skills.
During the vision screenings, the optometry students were primarily responsible for conducting eye examination tests, with specific details outlined in the Appendix. On the other hand, education students focused on addressing the emotional well-being of children with SEN and maintaining an orderly environment during the screenings. Some education students also supported the optometry students by assisting with the administration of eye tests.
In March 2023, four vision screenings were conducted at two local special schools, selected through a convenience sampling approach. These schools catered to students with mild to moderate intellectual disabilities. All students from these two special schools were invited to participate in the vision screenings. Before commencing the vision screenings, written informed consent was obtained from the guardians through the schools. All screening procedures adhered to the tenets of the Declaration of Helsinki and were approved by The Hong Kong Polytechnic University Human Subjects Ethics Subcommittee (HSEARS20230104006).
Reflection and feedback
To evaluate students’ understanding of SEN and their confidence in addressing the eye health issues of children with SEN, two surveys were administered: one before the commencement of the education program (pre-program survey) and another after the completion of the vision screening (post-program survey). The questionnaire utilized a single-stage, five-level Likert scale for responses, ranging from 1 (Strongly disagree) to 5 (Strongly agree). The details of questionnaire are available in Appendix 1. Scores of 4 (Agree) or 5 (Strongly Agree) were considered as indicative of the students’ awareness and comprehension of the respective topics.
Assessment: reflective writing essay
Upon the completion of the vision screenings, students from both the optometry and education disciplines were required to submit a reflective writing essay. This task provided an opportunity for students to reflect on and articulate their learning experiences throughout the interprofessional education program. The reflective essays served as a source of qualitative data, complementing the quantitative findings obtained from the pre- and post-program surveys. The analysis of these reflective essays enriched the overall evaluation of the program’s effectiveness by offering insights into students’ personal experiences, perspectives, and growth throughout the collaborative learning process.
Statistical analysis
Quantitative analysis of the survey data
The Wilcoxon signed-rank test was used to compare pre- and post-program survey scores, with a significance level set at p < 0.05. All statistical analyses for the quantitative data were conducted using JASP v0.17.1 (JASP Team, Netherlands).
Qualitative analysis of the reflective writing essay
To dissect the qualitative aspects of the students’ learning experiences, inductive content analysis was conducted using NVivo software (version 14, Lumivero, United States). To ensure a systematic and rigorous analysis of the qualitative data collected from reflective writing essays, a coding procedure was implemented. Each participant was assigned anonymous codes (e.g., O1, O2 for optometry students and E1, E2 for education students) to maintain confidentiality while allowing for specific attribution during analysis.
The reflective writing essays were analysed using grounded theory methodology [19] to ensure a systematic and comprehensive approach to the development of themes. The analysis began with a thorough reading of all essays to immerse ourselves in the data and grasp the foundational ideas and concepts conveyed by the students. This immersion was followed by open coding, a process where key textual elements were identified and labeled with codes as an initial step towards categorizing the information. Two researchers independently analysed the data set. Findings were brought together in meetings to reach consensus on themes and ensure a transparent and in-depth coding process.
The coding process focused on extracting students’ reflections across several domains: their experiences with interprofessional collaboration, the applications of knowledge in practical settings, the program’s impacts on their empathy towards children with SEN, and the influence on their professional self-identity. This initial coding generated a wide array of codes, which were meticulously examined for discernible patterns and relationships.
Through an iterative process of comparing and contrasting these codes, we distilled the data into more focused categories. These categories were further refined and clustered into four distinct learning themes that encapsulated the transformative experiences of the students throughout the program:
Professional Interactions: This theme captured students’ insights into the dynamics of working with professionals from other disciplines and the enhancement of team-based care. It encompassed their reflections on interprofessional collaboration, communication, and the integration of diverse perspectives in providing comprehensive care.
Bridging the Gap Between Theory and Practice: This theme focused on students’ reflections on the integration of academic knowledge with practical experiences and the resultant growth in professional competence. It explored their ability to apply theoretical concepts in real-world settings and the development of practical skills through hands-on learning opportunities.
Social Responsibility: Awareness of the societal role and impact of their professions on children with SEN and the broader community. It encompassed their reflections on the importance of empathy, inclusivity, and their responsibility to advocate for and serve vulnerable populations.
Professional identity: This theme centered on the development of a sense of self within the professional context and the evolution of professional values and ethics. It captured students’ reflections on their personal and professional growth, shaping their identifies as future healthcare and educational professionals, and the reinforcement of ethical principles guiding their practice.
Results
Quantitative results
The pre- and post-program surveys were completed by 58 students – 37 optometry students and 21 education students (Table 1). Initially, a significant lack of knowledge about the specific needs of children with SEN was found, particularly among the optometry students. Prior to the education program, only 5% of optometry students acknowledged a sufficient understanding of the unique characteristics of children with SEN (responses of Agree or Strongly Agree as shown in Fig. 2). Moreover, none of the optometry students had received any previous training on managing children with SEN, highlighting a gap in the standard optometry curriculum. The rest of the questionnaire aimed to evaluate optometry students’ self-confidence in conducting eye examinations for children with SEN. Prior to the educational intervention, a small percentage felt confident in gaining the trust of children with SEN (21.62%), streamlining the vision assessment (16.21%), and overcoming the challenges encountered by children with SEN during eye examinations (21.62%).
Table 1.
Survey results (median [range]) for optometry and education students before and after attending the interprofessional collaborative training program
| Optometry students | Education students | |||||
|---|---|---|---|---|---|---|
| Pre- | Post- | p | Pre- | Post- | p | |
| Understanding and confidence in addressing the needs of SEN children | ||||||
| Understanding of the characteristics of SEN | 3 [4 to 1] | 3 [5 to 1] | < 0.001 | 3 [5 to 2] | 3 [5 to 3] | 0.013 |
| Confidence in supporting emotional well-being of SEN children | 2 [4 to 1] | 3 [5 to 1] | < 0.001 | 3 [4 to 2] | 3 [4 to 2] | 0.115 |
| Developing effective communication with SEN children | 2 [4 to 1] | 3 [4 to 1] | < 0.001 | 3 [5 to 2] | 3 [4 to 1] | 0.499 |
| Proficiency in conducting vision assessment for SEN children (Optometry Students) | ||||||
| Gaining trust of SEN children | 3 [4 to 1] | 4 [5 to 2] | < 0.001 | |||
| Establishing a streamlined process for vision assessment | 3 [5 to 1] | 4 [5 to 2] | < 0.001 | |||
| Overcoming the challenges associated with assessing SEN children | 3 [4 to 1] | 4 [5 to 1] | 0.007 | |||
| Comprehending the role of optometrists (Education students) | ||||||
| Maintaining eye health | 4 [5 to 2] | 4 [5 to 3] | 0.279 | |||
| Prescribing glasses or contact lenses | 5 [5 to 3] | 5 [5 to 3] | 0.402 | |||
| Detecting eye diseases | 3 [5 to 1] | 4 [5 to 3] | 0.018 | |||
| Providing visual training | 3 [5 to 1] | 4 [5 to 2] | 0.023 | |||
p: probability values for Wilcoxon signed-rank test; pre-: pre-program, post-: post-program
Fig. 2.
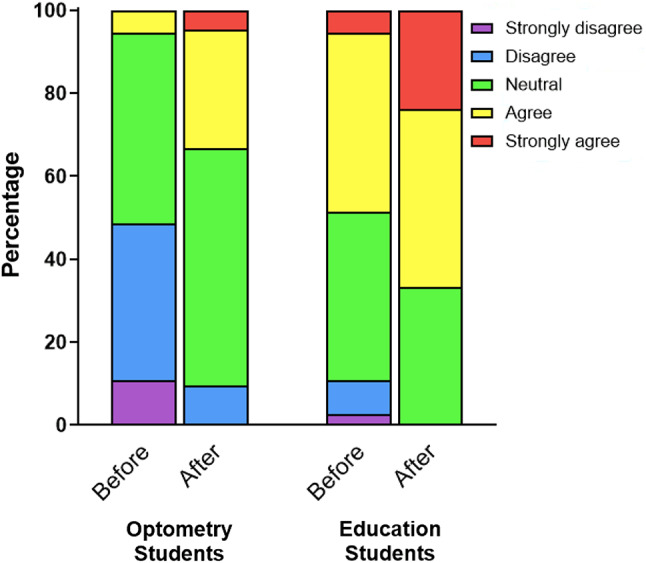
Ratings of optometry and education students on their understanding of the characteristics of children with special educational needs before and after the training program. Responses are presented as percentages for each rating category (strongly disagree, disagree, neutral, agree, strongly agree)
On the other hand, education students demonstrated a higher level of initial knowledge, with 34% indicating their understanding of the characteristics of children with SEN (Fig. 2). The questionnaire for these students concentrated on their comprehension of the optometry profession. The findings indicated that over 85% of these students were aware of common optometric responsibilities, such as maintaining eye health and prescribing glasses and contact lenses. Nonetheless, their awareness of optometrists’ capabilities in detecting eye diseases and providing vision therapy was limited, with only 38.10% and 33.33%, respectively, recognizing these roles.
After completing this interprofessional education program, both optometry and education students exhibited a significant improvement in the survey scores associated with their understanding of SEN (Table 1, Wilcoxon signed-rank test, both p < 0.001). The percentage of optometry students who reported an understanding of SEN increased tenfold to approximately 50% as indicated in the post-program survey (Fig. 2). Moreover, optometry students also demonstrated increased confidence in gaining trust (54.05%), streamlining vision assessments (59.46%), and overcoming the challenges of eye examination for children with SEN (51.34%), with the median survey scores improved significantly (Wilcoxon signed-rank test, p ≤ 0.007).
Similarly, the education students showed substantial growth in their comprehension of SEN, with the percentage doubling to 67% after completing the program (Fig. 2). Their understanding of the optometrist’s roles, particularly regarding eye disease detection and the provision of visual training, increased significantly to 80.95% and 71.43%, respectively, with the median survey scores improved significantly (Wilcoxon signed-rank test, p ≤ 0.023).
Qualitative results
In our qualitative analysis, we examined a total of 60 reflections, 41 from optometry students and 19 from education students, to gain deeper insights into their personal and professional development after participating in the interprofessional education program.
Professional interactions
Optometry students pinpointed the acquisition of effective communication skills with children who have SEN, a competency they attributed to the expertise shared by education students. The students acknowledged and valued individual strengths and appreciated the importance of interprofessional collaboration. O2 reflected, “The students studying at The Education University of Hong Kong had experience with it, and they taught us how to understand students with special needs. I was fortunate to learn how to effectively communicate with students who have special needs.”
The ability to manage the emotional needs in children with SEN was another skill emphasized by the students. O8 admitted, “In terms of taking care of the emotional needs of SEN students, EdUHK students surely did a better job than me! Those skills will be especially useful when I am taking care of patients with special needs in the clinic in future.”
The vision screening conducted in partnership was identified as a pivotal component of the program. Students valued the insights gained through collaboration with peers from the other discipline. O10 shared, “This vision screening provided me a precious opportunity to cooperate with students studying special need education from The Education University of Hong Kong (EdUHK). It allowed us to exchange the knowledge and experiences between two professions.”
Similarly, E4 student stated, “This experience has also made me more aware of the importance of professional collaboration and teamwork. Only through collaboration and communication can we provide better services and comprehensive support to students.”
Bridging the gap between theory and practice
Most optometry and education students noted that the vision screening provided their first hands-on encounter with children who have SEN. E6 indicated, “Since our lessons were typically in the classroom and on campus, we rarely had the chance to interact with students with special educational needs. Therefore, this was a valuable opportunity to learn how to communicate with them and how to handle challenges.”
Optometry students reported an increase in confidence when handling children with SEN. O12 candidly shared, “Honestly, before the event, I lacked confidence in my ability to conduct visual screenings for these children. However, through the workshop, I learned that effective communication is vital. One effective method to alleviate their stress during the check-up is to accurately describe the test and obtain verbal consent and confirmation before initiating the procedure.”
Students also commented that they acquired practical skills from interacting with experienced supervisors during the vision screening. O26 stated, “My supervisors are optometrists from PolyU. They are very experienced and familiar with the routine of a vision screening, thus providing us with a lot of useful tips and reminders on the procedures of carrying out various eye examinations.”
Education students acknowledged the newfound importance of eye care in their professional perspective. E14 reflected, “After doing the service, I have gained a precious experience. And it makes me to have higher interest in getting to know more about eye checking. I have never gotten to know the knowledge about this before attending this course, and I seldom do eye check as I think that it is not that important. However, after taking the course and do the service, I understand that it is very crucial to protect our eyes well in our young age.”
Social responsibility
A notable number of students articulated a deepened understanding of their social responsibility, including the upholding ethical standards, promoting community welfare, and the necessity of taking action for societal betterment.
This concept of social responsibility is exemplified by the following student’s reflections: “As a community member, I see numerous opportunities for future involvement in community service initiatives. These may include volunteering my time and resources, advocating for regular eye screenings, and encouraging others to participate, all of which can have a positive impact.”
Interaction with children, a point often discussed by the lecturer from the EdUHK, led E18 to a significant realization: “I have learned more about these children and realized they are not as ‘scary’ as society often portrays them. Therefore, we should actively debunk these negative stereotypes and foster a more welcoming environment for their growth.”
E19 shared a similar sentiment, stating, “This screening experience has equipped me to contribute to society in the future. I can participate in or organize vision screening programs, such as screenings for diabetic retinopathy, school screenings, and community screenings for the elderly.”
These reflections underscore the importance of social responsibility as a key learning outcome in education. They highlight the needs for individuals to not only understand their societal roles but also to actively engage in ethical conduct and community betterment. Such engagement is crucial for cultivating a society that is equitable, just, and respectful of every individual’s dignity.
Professional identity
Many optometry students expressed a newfound clarity regarding their professional identity as future healthcare practitioners. O26 observed, “As a primary healthcare provider, we should be equipped with the ability to carry out eye examination not only to the general public, but also special patient groups that are even more in need.”
O28 highlighted the preventative aspect of their role, stating, “As a primary healthcare professional, providing preventive care to the public is one of our major responsibilities. Visual screening can help identify the students with visual problems and refer them for treatment, which prevents the worsening of ocular conditions and minimize its impact on other developmental aspects of the students.” Yet another student echoed a similar sentiment, stating, “Through this screening activity, I have come to understand that within the community, there are individuals with specific needs that may require optometrists to play an active role in providing specialized eye care services.”
This education program has evidently strengthened the professional identity of the optometry students, instilling in them a greater sense of their potential impact and the vital role they play in healthcare.
Discussion
This interprofessional education program has integrated the theoretical constructs of SLT framework into undergraduate training, bridging healthcare and education disciplines. Interprofessional education has emerged as an increasingly important concept in enhancing healthcare delivery [20–22] and has been demonstrated to considerably improve patient care outcomes [23]. Our program extends beyond the conventional healthcare-oriented interprofessional education program [17, 18] by engaging with educational professionals, thereby enriching the learning experience for students preparing to support children.
The collaborative nature of this program is theoretically grounded, with literature suggesting substantial benefits for school-aged populations when education and healthcare professionals work in tandem [24]. However, the process of integrating healthcare and educational disciplines is sometimes challenging. These include a tendency for professionals to work within isolated departmental boundaries, the complexity of cases encountered by each professional, inconsistent availability of professionals, and disagreements regarding the best course of action for student support [24]. Our interprofessional education initiative seeks to mitigate these barriers by fostering early interprofessional engagement and knowledge sharing between optometry and education students. Introducing such collaboration at the undergraduate level is poised to enhance mutual understanding and reduce potential conflicts that may arise in their later professional practice. Collaborating on the shared goal of vision screening further promotes communication and cooperation skills among students, laying the groundwork for future teamwork.
Moreover, this interprofessional education program highlights the cultivation of professionalism within healthcare delivery. Central to the curriculum are structured activities that promote the recognition of interprofessional roles. The inclusion of real-world vision screening allows students to experience and navigate the complexities of professional healthcare and educational environments, along with rigorous self-assessment through reflective essays. These components are meticulously designed to instill a cohesive value among students from diverse disciplines, advocating for reflective practice and mutual respect among different professionals [25].
The efficacy of our interprofessional education program has been substantiated through both qualitative and quantitative evaluations, encompassing survey data and analyses of student reflective writings. Quantitatively, our surveys indicated that this interprofessional education program significantly elevated the awareness of SEN among future optometrists and teachers. Particularly noteworthy is the marked increase in optometry students’ awareness of SEN characteristics, which surged from a mere 5% prior to the program to approximately 50% following the program, highlighting a substantial enhancement in their understanding. This education program also bolstered optometry students’ confidence in conducting eye examinations for children with SEN and deepened education students’ understanding of optometrists’ role in eye care management. Qualitatively, students indicated an emergent recognition of the value of interprofessional collaboration. They also expressed an elevated sense of social responsibility and an enriched understanding of both their own and their peers’ professional roles. The pedagogical approach adopted in this program, with its emphasis on experiential learning, reflective practice, and interprofessional engagement, aligns with contemporary educational practices and holds promise for adaptation across diverse educational settings. These outcomes suggest that our IPE model is extensible to broader healthcare contexts, offering a scalable approach to improve services for vulnerable populations, such as children with SEN.
While the outcomes of this interprofessional education program suggest a promising impact on optometry and education students’ learning and professional development, several limitations warrant consideration. First, the program was piloted with a limited sample size, focusing exclusively on students from the optometry and education disciplines. Although we are currently implementing the second phase of the program with a new cohort, the generalizability of our findings to other healthcare disciplines remains uncertain. Second, due to administrative constraints, the interprofessional education program was conducted with all students in the class, precluding the use of a control group. This limitation restricts our ability to isolate the specific effects of the IPE framework from the general improvements expected from any training intervention. Additionally, our evaluation methods relied on self-reported surveys and reflective writings, introducing a potential for response bias that could affect the results. Lastly, without longitudinal follow-up, it is challenging to verify whether the enhancements in awareness and confidence observed will lead to sustained behavioral changes and improvements in professional practice. A more extended period of evaluation is essential to fully understand the long-term effects that this interprofessional education program may have on both students and society.
In conclusion, children with SEN represent a particularly vulnerable segment of our community, necessitating focused attention on their ocular health due to the high incidence of visual impairments associated with these individuals [26–28]. However, their visual issues often go undetected or undocumented, largely due to their communication barriers [28]. Our vision screening results indicate that approximately half of the children with SEN failed the screening, and a majority of their parents (56.96%) were unaware of their existing vision problems (refer to Appendix 2). In an effort to address the rising ocular health concerns among children, particularly within the Asian Chinese demographic [29–33], our interprofessional education program aims to develop a new generation of proficient and compassionate optometrists and educators equipped to meet the needs of children with SEN. Through this collaborative approach, we aspire to facilitate equitable eye care access for all, including those in vulnerable groups. The encouraging preliminary results of our project provide a solid foundation for the adoption of this pedagogical approach in healthcare education. However, further research is necessary to evaluate the long-term effects of our program within the community.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our gratitude to the teachers and lab tutors who contributed to this project. We would also like to thank the staff at Hong Chi Morninghill School and Buddhist To Chi Fat She Yeung Yat Lam Memorial School for coordinating the vision screenings and providing support.
Author contributions
K.W wrote the main manuscript text and prepared Table 1. T.W.L prepared all figures. All authors reviewed the manuscript.
Funding
This project was supported by PolyU Teaching Development Grants (LTG22-25/IICA/27).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Human ethics and consent to participate
Written informed consent was obtained from the guardians through the schools. All screening procedures adhered to the tenets of the Declaration of Helsinki and were approved by The Hong Kong Polytechnic University Human Subjects Ethics Subcommittee (HSEARS20230104006).
Consent to publish
The individual(s) depicted have been made aware of the intended use of the image and have provided their consent.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Birden H, Glass N, Wilson I, Harrison M, Usherwood T, Nass D. Teaching professionalism in medical education: a best evidence Medical Education (BEME) systematic review. BEME Guide 25 Med Teacher. 2013;35(7):e1252–66. [DOI] [PubMed] [Google Scholar]
- 2.Lave J, Wenger E. Situated learning: legitimate peripheral participation. Cambridge University Press; 1991.
- 3.Wenger E. Communities of practice: learning as a social system. Syst Think. 1998;9(5):2–3. [Google Scholar]
- 4.Wenger EC, Snyder WM. Communities of practice: the organizational frontier. Harvard Business Rev. 2000;78(1):139–46. [Google Scholar]
- 5.Wenger-Trayner E, Fenton-O’Creevy M, Hutchinson S, Kubiak C, Wenger-Trayner B. Learning in landscapes of practice: boundaries, identity, and knowledgeability in practice-based learning. Routledge; 2014.
- 6.Durning SJ, Artino AR. Situativity theory: a perspective on how participants and the environment can interact: AMEE Guide 52. Med Teach. 2011;33(3):188–99. [DOI] [PubMed] [Google Scholar]
- 7.Ezeh EI, Ibanga AA, Duke RE. Visual status of special needs children in special education schools in Calabar, Cross River State, Nigeria. Nigerian Postgrad Med J. 2018;25(3):161–5. [DOI] [PubMed] [Google Scholar]
- 8.Woodhouse JM, Davies N, McAvinchey A, Ryan B. Ocular and visual status among children in special schools in Wales: the burden of unrecognised visual impairment. Arch Dis Child. 2014;99(6):500–4. [DOI] [PubMed] [Google Scholar]
- 9.Little J-A, Saunders K. A lack of vision: evidence for poor communication of visual problems and support needs in education statements/plans for children with SEN. Public Health. 2015;129(2):143–8. [DOI] [PubMed] [Google Scholar]
- 10.Sobrado P, Suárez J, García-Sánchez FA, Usón E. Refractive errors in children with cerebral palsy, psychomotor retardation, and other non-cerebral palsy neuromotor disabilities. Dev Med Child Neurol. 1999;41(6):396–403. [DOI] [PubMed] [Google Scholar]
- 11.Thankappan B, Sidhan N, Aparna K. Ocular disorders in children with autism in special schools. J Med Sci Clinc Res. 2017;5:25199–203. [Google Scholar]
- 12.Kaur G, Thomas S, Jindal M, Bhatti S. Visual function and ocular status in children with disabilities in special schools of Northern India. J Clin Diagn Research: JCDR. 2016;10(10):NC01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellato A, Perna J, Ganapathy PS, Solmi M, Zampieri A, Cortese S, Faraone SV. Association between ADHD and vision problems. A systematic review and meta-analysis. Mol Psychiatry. 2023;28(1):410–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi KY, Wong HY, Cheung HN, Tseng JK, Chen CC, Wu CL, et al. Impact of visual impairment on balance and visual processing functions in students with special educational needs. PLoS ONE. 2022;17(4):e0249052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du K, Huang J, Guan H, Zhao J, Zhang Y, Shi Y. Teacher-to-parent communication and vision care-seeking behaviour among primary school students. Hong Kong Med J. 2022;28(2):152–60. [DOI] [PubMed] [Google Scholar]
- 16.Gautama MSN, Kharismawati FA, Astuti LF, Maulidyati M, Hidayatulloh A. Collaboration between interprofessional education (IPE) and interprofessional collaborative practice (IPCP) in health education: a narrative review. J Holist Nurs Sci. 2023;10(2).
- 17.Sanko JS, Hartley GW, Mckay ME, Drevyn EM, Mandel DW, Gerber KS et al. Insights into learning among physical therapy, Medical, and nursing students following a Simulation-Based, Interprofessional Patient Safety Course. Cureus. 2023;15(3). [DOI] [PMC free article] [PubMed]
- 18.McNair R, Brown R, Stone N, Sims J. Rural interprofessional education: promoting teamwork in primary health care education and practice. Aust J Rural Health. 2001;9(6):S19–26. [PubMed] [Google Scholar]
- 19.Corbin J, Strauss A. Basics of grounded theory: techniques and procedures for developing grounded theory. Thousand Oaks, CA, USA: Sage; 2014. [Google Scholar]
- 20.D’amour D, Oandasan I. Interprofessionality as the field of interprofessional practice and interprofessional education: an emerging concept. J Interprof Care. 2005;19(sup1):8–20. [DOI] [PubMed] [Google Scholar]
- 21.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes. Cochrane Database Syst Reviews. 2013;(3). [DOI] [PMC free article] [PubMed]
- 22.Schot E, Tummers L, Noordegraaf M. Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration. J Interprof Care. 2020;34(3):332–42. [DOI] [PubMed] [Google Scholar]
- 23.Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Reviews. 2017;(6). [DOI] [PMC free article] [PubMed]
- 24.Timperi T, Vornanen RH, Kasanen K, Mönkkönen K. What matters in low-threshold collaboration? Perceptions of interprofessional collaboration between education and social and healthcare professionals in Finnish primary schools. J Interprof Care. 2024:1–9. [DOI] [PubMed]
- 25.McNair RP. The case for educating health care students in professionalism as the core content of interprofessional education. Med Educ. 2005;39(5):456–64. [DOI] [PubMed] [Google Scholar]
- 26.Gunn A, Cory E, Atkinson J, Braddick O, Wattam-Bell J, Guzzetta A, Cioni G. Dorsal and ventral stream sensitivity in normal development and hemiplegia. NeuroReport. 2002;13(6):843–7. [DOI] [PubMed] [Google Scholar]
- 27.Ghasia F, Brunstrom J, Gordon M, Tychsen L. Frequency and severity of visual sensory and motor deficits in children with cerebral palsy: gross motor function classification scale. Invest Ophthalmol Vis Sci. 2008;49(2):572–80. [DOI] [PubMed] [Google Scholar]
- 28.Little J-A, McCullough S, McClelland J, Jackson AJ, Saunders KJ. Low-contrast acuity measurement: does it add value in the visual assessment of down syndrome and cerebral palsy populations? Investig Ophthalmol Vis Sci. 2013;54(1):251–7. [DOI] [PubMed] [Google Scholar]
- 29.Elhusseiny AM, Eleiwa TK, Yacoub MS, George J, ElSheikh RH, Haseeb A, et al. Relationship between screen time and dry eye symptoms in pediatric population during the COVID-19 pandemic. Ocul Surf. 2021;22:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma D, Wei S, Li S-M, Yang X, Cao K, Hu J, et al. Progression of myopia in a natural cohort of Chinese children during COVID-19 pandemic. Graefe’s Archive Clin Experimental Ophthalmol. 2021;259:2813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal S, Bhartiya S, Mithal K, Shukla P, Dabas G. Increase in ocular problems during COVID-19 pandemic in school going children-a survey based study. Indian J Ophthalmol. 2021;69(3):777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liang Y, Leung T-W, Lian JT, Kee C-S. Significant increase in astigmatism in children after study at home during the COVID-19 lockdown. Clin Experimental Optometry. 2022:1–9. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


