Abstract
Background
Polycystic Ovarian Syndrome (PCOS) is a reproductive disorder that significantly impacts women’s quality of life (QOL). Its unclear etiology, whether genetic or environmental, and the treatments associated with it have been widely studied globally.
Research Design and Methods
This study assessed the QOL of 108 women with PCOS, examining both physical and mental symptoms. Participants completed the Short Form-12 (SF-12) questionnaire through a web-based survey to evaluate their QOL scores.
Results
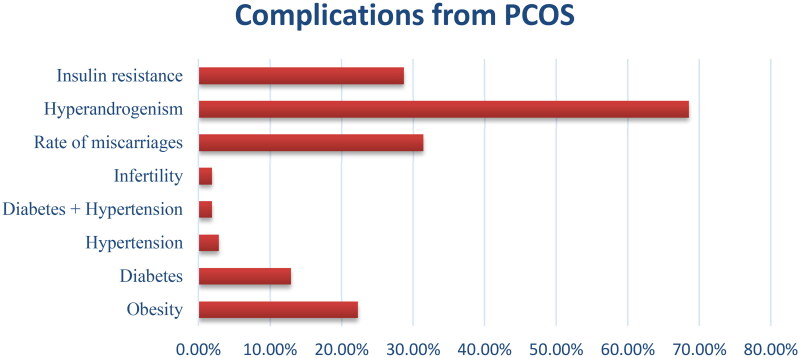
Common symptoms included menstrual irregularity (73.14%), hirsutism (65.7%), acne (62.03%), and obesity (22.22%). Complications such as diabetes mellitus (12.9%), hypertension (2.78%), infertility (1.85%), miscarriages (31.4%), hyperandrogenism (68.51%), and insulin resistance (28.7%) were reported. Patients with infertility had the lowest physical scores (PCS), while those working night shifts had the lowest mental scores (MCS).
Conclusion
PCOS significantly affects QOL, with infertility contributing to the lowest physical scores and night shift work correlating with the lowest mental scores. These findings emphasize the need for integrated psychological and physical care, particularly for young working women with PCOS.
Keywords: Polycystic ovarian syndrome (PCOS), Quality of Life (QOL), SF-12 questionnaire, physical score (PCS), mental score (MCS)
Plain Language Summary
Polycystic Ovarian Syndrome (PCOS) can greatly affect a woman’s quality of life. This study looked at 108 women with PCOS and found common issues such as irregular periods, excess hair growth, acne, and obesity. Many of these women also faced problems like diabetes, high blood pressure, infertility, and miscarriages. Women with these additional health issues reported a lower quality of life. The study particularly focused on young working women and found that their diet, lifestyle, and stress levels play a big role. For those working night shifts, mental well-being was notably affected, highlighting the need for both psychological and physical support in managing PCOS.
Article highlights
Impact on Quality of Life: PCOS significantly affects women’s quality of life, with common symptoms including irregular periods, excess hair growth, acne, and obesity.
Complications: Women with PCOS frequently experience complications such as diabetes, hypertension, infertility, miscarriages, hyperandrogenism, and insulin resistance, which contribute to a poorer quality of life.
Holistic Treatment Need: The study emphasizes the importance of a comprehensive treatment approach to address both physical and psychological aspects of PCOS.
Focus on Working Women: The study highlights the specific challenges faced by young working women with PCOS, particularly those who work night shifts.
Lifestyle and Stress Impact: Diet, lifestyle, and stress levels are closely linked to the severity of PCOS symptoms and overall quality of life.
Mental Well-being: Night shift work is associated with lower mental quality of life, underscoring the need for psychological support in addition to physical treatments for PCOS.
1. Introduction
Polycystic ovarian syndrome (PCOS) stands out as a highly prevalent endocrine disorder, impacting a significant portion of women in their reproductive years on a global scale. Statistics reveal its prevalence in approximately 5-20 percent of the worldwide population. PCOS is identified by a cluster of symptoms, with hyperandrogenism being the foremost manifestation—marked by an overproduction of androgens originating from the ovaries. This primary symptom is often accompanied by additional manifestations, such as ovulatory dysfunction leading to irregularities in the menstrual cycle. Moreover, morphological alterations, exemplified by the presence of preantral follicles commonly referred to as ovarian cysts, contribute to the distinctive features of PCOS [1].
Additionally, there is a heightened incidence of metabolic syndrome, a condition intricately linked with other endocrine disorders such as diabetes. The diminished rates of ovulation associated with this condition may result in infertility and suboptimal neonatal outcomes. The cumulative impact of these factors may contribute to an elevated risk of cardiovascular diseases and cancer [2, 3].
The oligogenic nature of PCOS is experiencing a rising incidence, attributed to the intricate interplay between genetic and environmental factors [4, 5]. While the genetic origins of the syndrome remain elusive, a familial predisposition is commonly observed, although the exact hereditary connections remain unclear [6]. Beyond genetic influences, environmental factors exert a substantial impact on the syndrome. Notably, dietary choices and sedentary lifestyles emerge as primary concerns, given the contemporary prevalence of processed and fast foods in current diets. These factors contribute to the development of obesity and insulin resistance, culminating in the manifestation of PCOS [7]. Furthermore, they establish robust connections with future risk factors, including but not limited to type 2 diabetes mellitus, hyperinsulinemia, hypertension, and cardiovascular disorders [8]. This multifaceted interplay of genetic and environmental elements underscores the complexity of PCOS etiology and its broader implications for health outcomes.
PCOS diagnosis hinges on three distinct criteria, each with its unique parameters. The National Institute of Health criteria emphasizes two key symptoms: hyperandrogenism and menstrual irregularity. The PCOS Society criteria broaden the scope by considering hyperandrogenism, menstrual irregularity, or the presence of polycystic ovaries detected through ultrasonography. Meanwhile, the Rotterdam criteria adopts a flexible approach, necessitating any two out of three symptoms—hyperandrogenism, menstrual irregularity, and polycystic ovaries on ultrasonography. Despite these diagnostic criteria, establishing a diagnosis in teenagers and adolescent females remains a challenging area. The intricacies of PCOS manifestation in this demographic present complexities that current diagnostic frameworks may not adequately address, thereby warranting further research and refinement in the diagnostic process for this specific population [9].
PCOS significantly impacts the Quality of Life (QOL) experienced by PCOS affected women. A comprehensive cross-sectional study revealed that a majority of patients exhibited notably low scores in their QOL, a factor intricately linked with mental health disturbances, particularly depression [10]. Delving further into this aspect, a study conducted in 2015 meticulously analyzed the effectiveness of a stress management program tailored for women with PCOS. The findings showcased a substantial improvement not only in their QOL but also in mitigating symptoms of depression and anxiety. This underscores the critical interplay between mental well-being, the management of stress, and the overall quality of life in individuals grappling with PCOS. As such, addressing not only the physiological but also the psychological aspects becomes paramount in enhancing the holistic well-being of women affected by this condition [11].
PCOS, being a syndrome with a substantial influence on the Quality of Life (QOL) of women, is further complicated by its association with long-term complications and comorbidities. As a result, there is a critical imperative for early diagnosis and proactive management in these instances [12]. The primary objective of this study is to comprehensively examine and analyze not only the clinical manifestations but also the physical and mental dimensions of Quality of Life linked to PCOS. By delving into these multifaceted aspects, the research aims to provide a refined understanding of the complex interplay between the syndrome and various facets of women’s well-being. This approach underscores the importance of a comprehensive perspective in the diagnosis, management, and overall care of individuals navigating the challenges posed by PCOS.
2. Methods
Between January and May 2020, a cross-sectional study was undertaken, utilizing a web-based survey to evaluate the symptoms and Quality of Life (QOL) of women who self-reported Polycystic Ovarian Syndrome (PCOS). This investigation specifically targeted a demographic of working women, examining those with and without night shifts (defined as those who regularly work at least 3 hours between 11 pm to 6 am). The objective was to gather comprehensive data on the symptoms and QOL experienced by women dealing with PCOS in the context of their work, with a particular focus on the influence of night shifts by following Rotterdam diagnosis criteria. They were asked for three important diagnostic criteria including ovulatory dysfunction, clinical signs of hyperandrogenism and confirmation for present of follicles by ultrasound.
2.1. Ethics approval
The study was conducted in compliance with the Declaration of Helsinki. All patients voluntarily provided informed consent by completing the questionnaire, which clearly outlined the study’s purpose, procedures, and their rights as participants. This ensured that they were fully aware of their involvement and the handling of their information before participating. The study was approved by the Institutional Human Ethics Committee (IHEC), SRM University of Science and Technology, Kattankulathur, Tamil Nadu, India (Ethical number: 1812/IEC/2022).
2.2. Ethical consideration (digital-based study)
The authors prioritize the safety and privacy of data by explicitly informing participants through a questionnaire note and securing consent for their participation. The study includes a representative sample of the local population; however, we recognize the opportunity to further enhance future surveys by more fully capturing the diversity of ethnicities, indigenous populations, and visible minorities. The authors advocate for enhanced digital literacy and widespread discussions regarding the societal advantages of utilizing health data for secondary purposes. They believe that such discussions can address public concerns surrounding routinely collected digital data. Furthermore, this dialogue can inform the development of international guidelines that align with current societal values and expectations.
2.3. Questionnaire
The questionnaire, consisting of a total of 28 questions in English language, was meticulously devised to encompass a diverse range of aspects. Among these, 16 questions delved into symptoms and various demographic characteristics. The evaluation of quality of life (QOL) was undertaken through a comprehensive analysis of 12 specific questions derived from the Short Form-12 (SF-12) questionnaire. This particular questionnaire has been recognized as a robust tool for assessing the quality of life concerning both physical and mental health attributes, as highlighted in the relevant literature. The questionnaire, consisting of a total of 28 questions, was meticulously devised to encompass a diverse range of aspects. Among these, 16 questions delved into symptoms and various demographic characteristics.
The factors like obesity, diabetes, hyperandrogenism and insulin resistance was calculated based on the patient responses. Also the rate of miscarriages was calculated based on patient responses to a specific yes or no question asking whether they had experienced any miscarriages before. The percentage was then determined from the number of affirmative responses out of the total number of patients surveyed.
The evaluation of quality of life (QOL) was undertaken through a comprehensive analysis of 12 specific questions derived from the Short Form-12 (SF-12) questionnaire [13, 14]. Upon the collection of data from the participating patients, a systematic assessment was conducted to derive QOL scores, incorporating both physical and mental dimensions. The standard methodology associated with the SF-12 questionnaire was employed to ensure the validity and reliability of the assessment process. Notably, the physical score (PCS) and mental score (MCS) were computed independently, with the resulting scores providing insights into the participants’ respective levels of well-being. It is noteworthy that lower scores on these scales indicated a comparatively poorer quality of life, while higher scores were indicative of a more favorable and positive quality of life experience for each participant.
2.4. Study sample
Reproductive aged women who met the inclusion criteria were included in the study. As it was the web-based self-administered questionnaire, patients self-reported the PCOS who were already diagnosed and facing the symptoms in day to day life.
2.4.1. Inclusion criteria
Working women of reproductive age who are diagnosed with polycystic ovarian syndrome according to Rotterdam criteria were included in the study.
2.4.2. Exclusion criteria
Women who have crossed their reproductive age (>45 years) including postmenopausal women might introduce confounding variables related to hormonal changes associated with menopause and those who are not working were excluded from the study.
2.5. Sample size
The web-based questionnaire link was sent and the sample of 119 answers were obtained in which 11 were not under inclusion criteria due age and work related factors. The Remaining 108 samples were assessed and their scores were calculated. In the methodology of the cross-sectional study, the sample size was determined through rigorous consideration of statistical power and precision criteria, ensuring that it adequately represented the target population and provided meaningful insights into the variables under investigation. Z1-α/2 p(1-p)/d2 was the formula used for the cross-sectional study [15].
2.6. Statistical analysis
The statistical analysis of all gathered data was conducted using GraphPad Prism software version 8.9.2. To scrutinize both inter-group and intra-group variations, with descriptive statistics, Mann- Whitney test and also ariabla two-way analysis of variance (ANOVA) was applied, followed by Tukey’s post hoc analysis for in-depth comparisons. The determination of significance was based on the calculated P-values, with a predetermined threshold set at p < 0.05 for statistical significance in all analyses. This rigorous approach ensured a robust evaluation of the data, employing advanced statistical methods to discern any meaningful differences and associations within and between the groups under investigation.
3. Results
From the inclusion criteria, 108 patients were being assessed; among which the mean age calculated was 25.4 ± 4.7 years. This suggests that 60-70% of the population were youngsters that are affected by PCOS. The study collected height and weight of the patients from which the body mass index (BMI) was determined. The mean BMI was found to be
27.3 ± 3.2 which says that the larger population was overweight. 43.5% population was found to be overweight, 22.22% population were obese and about 37% patients were of normal weight. Other demographic variables included marital status in which 64 (59.3%) of the population were married whereas 44 (40.7%) was unmarried (Table 1).
Table 1.
Demographic characteristics of the patients.
| Demographic variables | Patients (n = 108) | |
|---|---|---|
| Age (years) | 25.4 ± 4.7 | |
| Height (cm) | 159.2 ± 6.4 | |
| Weight (kg) | 69.3 ± 8.03 | |
| BMI | 27.3 ± 3.2 | |
| Obese | 24 (22.22%) | |
| Overweight | 47 (43.5%) | |
| Normal | 37 (34.2%) | |
| Marital Status | Married | 64 (59.3%) |
| Unmarried | 44 (40.7%) | |
| Disease | PCOS | 82 (75.9%) |
| PCOS with other endocrine or gynecological disorders | 26 (24.07%) | |
Data shown in the table as mean ± SD/Percentage. BMI- Body Mass Index.
Among the study population, 82 (75.9%) were diagnosed with PCOS alone and 26 (24.07%) were diagnosed with PCOS and other endocrine or gynecological disorders. Among 24.07%, 19 (17.59%) were diabetic, 3 (2.78%) had hypertension, 2 (1.85%) had both diabetes and hypertension and 2 (1.85%) had other endocrine problems. As far as cardinal symptoms is concerned 79 (73.14%) had irregular menstruation in which 40 (37.03%) had amenorrhea, which means that they missed their menstruation last month, 18 (16.67%) had Oligomenorrhea which is very little menstrual bleeding during the menstruation and 21(19.44%) had menorrhagia which is very heavy bleeding during the menstruation. Additionally, the symptoms like acne and hirsutism were reported by 67 (62.03%) and 71 (65.7%) respectively. Weight gain was also observed in 63 (53.33%) women in the last 3 months which can be observed in Table 2.
Table 2.
Clinical characteristics of patients.
| Clinical characteristics | Frequency, n (%) | |
|---|---|---|
| BMI | Obesity | 24 (22.22%) |
| Diabetes mellitus | Diabetes | 14 (12.9%) |
| Prediabetes | 7 (6.4%) | |
| Menstrual flow | Normal/ Regular | 29 (26.8%) |
| Amenorrhea (Absence of three or more consecutive periods) | 40 (37.03%) | |
| Oligomenorrhea (Menstrual periods occurring at intervals greater than 35 days, with fewer than 9 periods in a year) | 18 (16.67%) | |
| Menorrhagia (heavy bleeding) | 21 (19.44%) | |
| Acne | Yes | 67 (62.03%) |
| No | 41 (37.96%) | |
| Hirsutism | Yes | 71 (65.7%) |
| No | 37 (34.25%) | |
| Comorbidities | Diabetes mellitus | 19 (17.59%) |
| Hypertension | 3 (2.78%) | |
| Diabetes and Hypertension | 2 (1.85%) | |
| Other endocrine disorders | 2 (1.85%) | |
| Weight gain in last 3 months | Yes | 63 (58.33%) |
| No | 45 (41.67%) | |
| Quality of Life (QOL) | Excellent | 6 (5.55%) |
| Very good | 12 (11.11%) | |
| Good | 41 (37.96%) | |
| Fair | 37 (34.25%) | |
| Poor | 12 (11.11%) | |
Data showed in the table as mean (Percentage). BMI- Body Mass Index
Overall QOL was analysed from excellent, very good, good, fair and poor based on these categories derived from the questionnaire responses with the percentage of only 6 (5.55%) in excellent QOL, 12 (11.11%) in very good QOL, 41 (37.96%) with good QOL, 37 (34.25%) with fair QOL and 12 (11.11%) with poor QOL. The QOL was assessed from the SF-12 questionnaire which describes the physical activity limited in their life because of the symptoms of PCOS and also affects the mental health of the patients which is also assessed by the questionnaire.
In PCOS patients, if it is not diagnosed and specific therapy is not obtained promptly, this can lead to serious complications like obesity (22.22%), diabetes (12.90%), infertility (1.85%), miscarriages (31.40%), hyperandrogenism (68.51%) and insulin resistance (28.7%). Figure 1 gives the complications observed in the study population (Figure 1).
Figure 1.
Complications from PCOS. Prevalence of Co-morbid Complications in Participants with PCOS
Factors affecting QOL like all cardinal symptoms- irregular menstruation (amenorrhea, oligomenorrhea and menorrhagia), acne, hirsutism, the comorbidities like diabetes and hypertension, complications like hyperandrogenism, rate of miscarriages, infertility etc. was analysed against the QOL for each condition (Table 3). Working conditions like night shifts were also assessed in the study population against QOL. QOL good to poor was observed in the patients with menstrual irregularities, acne and hirsutism. Whereas, very few with cardinal symptoms had excellent and very good QOL. P value was determined by comparing the different rating from excellent to poor by one way ANOVA using the number of patients rated their health through the questionnaire.
Table 3.
Factors affecting quality of life.
| Clinical characteristics | Quality of Life |
P value | |||||
|---|---|---|---|---|---|---|---|
| Excellent (n) | Very good (n) | Good (n) | Fair (n) | Poor (n) | |||
| Obesity | Yes | 1 | 1 | 14 | 6 | 2 | 0.4702 |
| No | 5 | 11 | 27 | 31 | 10 | ||
| Diabetes mellitus | Diabetes | 0 | 3 | 9 | 1 | 1 | 0.0478 |
| Prediabetes | 0 | 1 | 5 | 1 | 0 | ||
| Menstrual flow | Normal/ Regular | 3 | 1 | 13 | 11 | 1 | 0.0064 |
| Amenorrhea (missed your periods) | 1 | 5 | 10 | 12 | 5 | ||
| Oligomenorrhea (very little menstrual bleeding) | 1 | 2 | 5 | 7 | 3 | ||
| Menorrhagia (heavy bleeding) | 1 | 4 | 3 | 12 | 3 | ||
| Acne | Yes | 4 | 11 | 37 | 10 | 5 | 0.6168 |
| No | 2 | 1 | 4 | 27 | 7 | ||
| Hirsuitism | Yes | 4 | 11 | 38 | 12 | 6 | 0.6194 |
| No | 2 | 1 | 3 | 25 | 6 | ||
| Comorbidities | Diabetes mellitus | 0 | 4 | 12 | 2 | 1 | 0.4379 |
| Hypertension | 1 | 0 | 1 | 1 | 0 | ||
| Diabetes and Hypertension | 0 | 0 | 2 | 0 | 0 | ||
| Infertility | 0 | 0 | 0 | 1 | 1 | ||
| Rate of miscarriages | Yes | 1 | 3 | 15 | 7 | 8 | 0.3653 |
| No | 5 | 9 | 26 | 30 | 4 | ||
| Hyperandrogenism | Yes | 5 | 7 | 32 | 21 | 9 | 0.3121 |
| No | 1 | 5 | 9 | 16 | 3 | ||
| Insulin resistance | Yes | 0 | 4 | 19 | 4 | 4 | 0.4419 |
| No | 6 | 8 | 22 | 33 | 8 | ||
| Weight gain in last 3 months | Yes | 4 | 10 | 35 | 9 | 5 | 0.5663 |
| No | 2 | 2 | 6 | 28 | 7 | ||
| Night shifts | Yes | 1 | 2 | 17 | 19 | 8 | 0.0400 |
| No | 5 | 10 | 24 | 18 | 4 | ||
Data analysed and p value determined from one way ANOVA through Graph pad prism software
QOL scores were calculated from the SF-12 questionnaire with the standard procedure. In QOL, both PCS and MCS was analysed. The mean PCS score was 30.6 ± 5.56 and the mean MCS score was found to be 40.8 ± 3.53. The score determines the mental and physical health of the patients, the maximum score an individual can get if they are excellent in physical and mental health, therefore the maximum score is calculated for a healthy woman to be 56.5 and 60.7 for PCS and MCS respectively [16–18]. The mean score observed was very less than the maximum perfect score calculated for the excellent quality of life. The QOL score was analysed for the ratings from excellent to poor. Also the graph was obtained for the PCS and MCS score which shows a descending graph from excellent to poor ratings.
4. Discussion
This investigation focuses on examining the impact of PCOS symptoms and complications on the Quality of Life (QOL) of patients, delving into the analysis of both the physical and mental scores associated with their overall well-being. A cohort of 108 voluntary participants, comprised of reproductive-age working women, partook in an online survey to undergo a comprehensive evaluation of their QOL in relation to PCOS symptoms and complications. The participants were stratified based on various demographic factors such as age, height, weight, BMI, marital status, engagement in night shifts, and the current status of their symptoms and comorbidities. The mean age of the patients was found to be 25.4, indicating a notable prevalence of PCOS within the younger demographic [19]. This observation may be attributed to lifestyle factors, dietary choices, and stress levels prevalent in this age group. Furthermore, the study scrutinized the prevalence of night shifts among women, revealing that 43.5% of participants engaged in night shifts as part of their professional responsibilities. This included individuals in healthcare professions such as nurses, doctors, and paramedics, as well as those in various other sectors such as IT professionals and call center employees. This multifaceted analysis provides a nuanced understanding of the demographic characteristics and occupational factors associated with PCOS and its implications for the overall well-being of working women. Some common complications observed in the patients were found to be obesity, hyperandrogenism, insulin resistance, diabetes, infertility and miscarriages.
PCOS is characterized by intricate features, rendering its diagnosis challenging. If left untreated, the condition can give rise to complications, incorporating numerous risk factors, as corroborated by the findings of this study. Various investigations have sought to gauge the Quality of Life (QOL) in women with PCOS, employing diverse questionnaires and surveys. For instance, a study involving 30 young adult females with PCOS revealed significant impacts across all questionnaire domains, including emotions, body hair, weight, infertility, and menstrual problems. These effects extended to psychosocial and physiological stress, resulting in an overall very poor QOL [20]. Another study emphasized the importance of addressing poor health-related quality of life (HRQOL) in PCOS patients beyond the conventional treatment for physical symptoms. This approach involved utilizing interviews and open-ended questions to allow patients to express concerns related to their QOL. The findings underscored the intricate interplay of physical, psychological, and social aspects in a woman’s life, shedding light on their discomfort, which in turn had notable mental repercussions [21]. These insights advocate for a comprehensive approach to PCOS care, recognizing the multifaceted impact it has on various dimensions of a woman’s well-being.
Several studies have substantiated the impact of hirsutism and weight gain or obesity as primary contributors to the physical aspects of QOL in individuals with PCOS [22]. The outcomes derived from our study align with these findings, revealing a noteworthy prevalence of hirsutism at 62.03% and confirming weight gain in 58.33% of participants over the past three months. Additionally, 22.22% of women identified as obese exhibited varying levels of QOL, ranging from good to poor. Furthermore, acne emerged as a prevalent concern, affecting 62.03% of women and constituting a significant aspect of the physical dimension of PCOS. The repercussions of these physical symptoms extend beyond the bodily realm, significantly influencing the psychological well-being of women, particularly among teenagers and young adults [23]. This study exploration underscores the interconnected nature of physical and psychological manifestations in PCOS, emphasizing the need for comprehensive care strategies that address both the visible and concealed aspects of this complex syndrome.
Concerns related to self-identity, encompassing issues such as weight gain, obesity, acne, and hirsutism, have been identified as potential precursors to diminished mental scores in QOL or adverse mental health outcomes [24]. Within the context of our study, the average MCS scores reflected these challenges, with obesity demonstrating a mean MCS of 41.5, hirsutism at 39.8, and acne at 42.3. These scores deviate significantly from those associated with a normal healthy individual. The research further delved into the impact of night shifts on mental well-being, revealing that individuals working during night shifts exhibited the lowest MCS score (29.4 ± 1.7). This decline in mental scores was attributed to disruptions in the circadian rhythm caused by night shift schedules. A cross-sectional study conducted in 2020, specifically focusing on nurses engaged in night shifts, discovered irregular menstrual cycles in 30% of the participants. Additionally, the study identified a heightened risk of developing PCOS associated with a frequent occurrence of night shifts [25]. In a prospective cross-sectional study, the investigation extended to the association between shiftwork and sleep duration. The findings indicated that women with less than six hours of sleep faced an elevated risk of experiencing menstrual irregularities and insulin resistance. Conversely, an improvement in sleep duration was linked to a potential reduction in the risks of complications such as infertility and diabetes mellitus [26]. These insights underscore the intricate relationship between lifestyle factors, work schedules, and various health outcomes in the context of PCOS, emphasizing the importance of a holistic approach to patient care.
Moreover, the challenges associated with PCOS extend beyond its primary symptoms, incorporating distressing elements such as menstrual irregularities, coexisting conditions like diabetes, and complex complications like miscarriage and infertility. The intricate nature of managing and treating these multifaceted aspects significantly contributes to the overall stress experienced by women affected by the syndrome. In our study, a comprehensive analysis was conducted to scrutinize the prevalence of symptoms and complications within the population under consideration. The evaluation extended to a meticulous assessment and measurement of the QOL, encompassing both PCS and MCS. This holistic exploration aimed to capture the diverse and interconnected dimensions of the challenges posed by PCOS, emphasizing the need for a nuanced and integrated approach in addressing the varied aspects of this complex condition.
The study’s robustness is underscored by several notable strengths. Foremost among these is its extensive reach facilitated by the digital cross-sectional questionnaire approach, which permits the involvement of participants from diverse geographical locations. This inclusivity enhances the generalizability of the study’s findings, offering a more comprehensive understanding across varied populations. Additionally, the digital survey methodology streamlines the data collection process, presenting a swifter and more efficient means of gathering responses from a larger participant pool compared to conventional methods. Another noteworthy strength lies in the enhanced participant comfort associated with responding to sensitive questions in a digital format. This format ensures heightened confidentiality and reduces the potential for social desirability bias, allowing participants to express themselves more freely. Moreover, the cost-effectiveness of digital surveys is a significant advantage, as it minimizes expenses related to printing, distribution, and data entry, presenting a more economical alternative compared to traditional paper-based approaches. Furthermore, the study benefits from the real-time data analysis afforded by digital platforms, enabling the swift identification of emerging trends and patterns. This capability not only enhances the timeliness of the study but also facilitates a dynamic and responsive approach to data interpretation. Collectively, these strengths underscore the efficacy and versatility of the digital cross-sectional questionnaire methodology in contemporary research settings.
The study’s constraints may be susceptible to selection bias since it hinges on individuals possessing access to and proficiency in using digital devices, potentially excluding those with limited technological access or skills. There’s a likelihood that participants with specific interests or experiences related to the study topic may be more predisposed to respond, introducing response bias and the potential over-representation of particular perspectives. The generalizability of findings may be restricted, as populations without internet access or those less inclined to engage in online surveys may not be fully represented, limiting the external validity of the study. Challenges in ensuring comprehensive data may arise in digital surveys, with participants potentially skipping questions or abandoning the survey, leading to non-response bias. Additionally, the limitations of digital surveys may manifest in their inability to capture nuanced responses due to the absence of in-depth probing achievable in face-to-face interview formats. Technical impediments such as compatibility issues, internet connectivity problems, or challenges related to devices may impede participation and data collection, particularly among older or less technologically literate populations. A limitation of our study is the absence of age-matched controls, which may affect the generalizability of the findings and limit our ability to fully isolate the impact of night shift work on quality of life. It focused exclusively on reproductive-age working women with a mean age of 25.4 years, which limits the generalizability of the findings to individuals with PCOS across different age groups and life stages. The data on dietary and lifestyle factors such as exercise were not accumulated. The future studies can target age-matched controls to better account for potential confounding factors and provide a more precise understanding of how night shift work independently influences quality of life with a broader age range. This will allow us to draw stronger conclusions and offer insights that are more applicable across different age groups.
5. Conclusion
PCOS is linked to intricate symptoms that detrimentally impact the overall quality of life and well-being of affected women across physical, mental, and social dimensions within society. The questionnaire employed to assess the Quality of Life (QOL) of women underscored the pervasive impact of numerous symptoms, contributing to a diminished QOL and elevating stress levels for patients. Consequently, the management of PCOS should extend beyond addressing merely the physical symptoms. A comprehensive approach involves providing mental health support through counseling, tailored to individual clinical symptoms and emotional distress. This holistic strategy aims to gradually alleviate stress and mitigate risk factors associated with the syndrome. Emphasis is also placed on regulating sleep patterns, advocating for a consistent six-hour sleep duration, as a means to counteract PCOS linked to chronobiological factors. This multifaceted approach underscores the necessity for a comprehensive and personalized management strategy to enhance the overall well-being of individuals grappling with PCOS.
Acknowledgement
The authors acknowledge the healthcare professionals and supervisors of SRM Institute of Science and Technology, Tamil Nadu for the support and guidance during the research.
Funding Statement
The authors declare that no funds, grants, or any other support were received during the research, preparation, publication of this manuscript.
Author contributions
RFB drafted the manuscript and performed critical revisions, contributed to the conception or design of the study, and was involved in data acquisition, analysis, and interpretation. CV provided supervision throughout the process and approved the final version of the manuscript. SM approved the version for publication and agrees to be accountable for all aspects of the work, ensuring that any questions regarding accuracy or integrity are appropriately addressed and resolved.
Disclosure statement
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
* These references provide information on background, need of the study, and aim of the work
- 1.Azziz R, Carmina E, Chen Z, et al. Polycystic ovary syndrome. Nat Rev Dis Prim. 2016;2(1):16057. Available from: https://www.nature.com/articles/nrdp201657. doi: 10.1038/nrdp.2016.57 [DOI] [PubMed] [Google Scholar]
- 2.Teede H, Deeks A, Moran L.. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8(1):41. Available from: https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-8-41. doi: 10.1186/1741-7015-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navaratnarajah R, Pillay O, Hardiman P.. Polycystic ovary syndrome and endometrial cancer. Semin Reprod Med. 2008;26(1):062–071. Available from: http://www.thieme-connect.de/DOI/DOI? doi: 10.1055/s-2007-992926 [DOI] [PubMed] [Google Scholar]
- 4.Ndefo UA, Eaton A, Green MR.. Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. P T. 2013;38(6):336–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23946629. [PMC free article] [PubMed] [Google Scholar]
- 5.Brady C, Mousa SS, Mousa SA.. Polycystic ovary syndrome and its impact on women’s quality of life: More than just an endocrine disorder. Drug Healthc Patient Saf. 2009;9:9–15. Available from: http://www.dovepress.com/polycystic-ovary-syndrome-and-its-impact-on-womenrsquos-quality-of-lif-peer-reviewed-article-DHPS. doi: 10.2147/dhps.s4388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diamanti-Kandarakis E, Kandarakis H, Legro RS.. The role of genes and environment in the etiology of PCOS. Endocrine. 2006;30(1):19–26. doi: 10.1385/ENDO:30:1:19 [DOI] [PubMed] [Google Scholar]
- 7.Rutkowska AZ, Diamanti-Kandarakis E.. Polycystic ovary syndrome and environmental toxins. Fertil Steril. 2016;106(4):948–958. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0015028216627280. doi: 10.1016/j.fertnstert.2016.08.031 [DOI] [PubMed] [Google Scholar]
- 8.Christakou CD, Diamanti-Kandarakis E.. Role of androgen excess on metabolic aberrations and cardiovascular risk in women with polycystic ovary syndrome. Women’s Heal. [Internet]. 2008;4(6):583–594. Available from: http://journals.sagepub.com/doi/10.2217/17455057.4.6.583. doi: 10.2217/17455057.4.6.583 [DOI] [PubMed] [Google Scholar]
- 9.El Hayek S, Bitar L, Hamdar LH, et al. Poly cystic ovarian syndrome: an updated overview. Front Physiol. 2016;7:124. doi: 10.3389/fphys.2016.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sidra S, Tariq MH, Farrukh MJ, et al. Evaluation of clinical manifestations, health risks, and quality of life among women with polycystic ovary syndrome. PLoS One 2019;14(10), e0223329. doi: 10.1371/journal.pone.0223329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stefanaki C, Bacopoulou F, Livadas S, et al. Impact of a mindfulness stress management program on stress, anxiety, depression and quality of life in women with polycystic ovary syndrome: a randomized controlled trial. Stress. 2015;18(1):57–66. doi: 10.3109/10253890.2014.974030 [DOI] [PubMed] [Google Scholar]
- 12.Brewer M, Pawelczak M, Kessler M, et al. A review of polycystic ovarian syndrome in adolescents. Minerva Pediatr. 2010;62(5):459–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20940680. [PubMed] [Google Scholar]
** These articles focus on the methodological approaches employed for the study
- 13.Benson S, Hahn S, Tan S, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: results of an internet-based survey in Germany. Hum Reprod. 2009;24(6):1446–1451. doi: 10.1093/humrep/dep031 [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y, Zhou F, Sun Y.. Assessment of health-related quality of life using the SF-36 in Chinese cervical spondylotic myelopathy patients after surgery and its consistency with neurological function assessment: a cohort study. Health Qual Life Outcomes. 2015;13(1):39. doi: 10.1186/s12955-015-0237-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charan J, Biswas T.. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35(2):121–126. doi: 10.4103/0253-7176.116232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montazeri A, Vahdaninia M, Mousavi SJ, et al. The 12-item medical outcomes study short form health survey version 2.0 (SF-12v2): a population-based validation study from Tehran, Iran. Health Qual Life Outcomes 2011;9(1):12. doi: 10.1186/1477-7525-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong G. SF-12 and SF-36 health survey. In: Encyclopedia of gerontology and population aging. Cham: Springer International Publishing; 2021. p. 4490–4493. doi: 10.1007/978-3-030-22009-9_426 [DOI] [Google Scholar]
- 18.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries. J Clin Epidemiol. 1998;51(11):1171–1178. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0895435698001097. doi: 10.1016/s0895-4356(98)00109-7 [DOI] [PubMed] [Google Scholar]
*** These articles includes comparison of prior studies with obtained results
- 19.Lewandowski KC, Płusajska J, Horzelski W, et al. Prevalence of dyslipidaemia and pre-diabetes among women with polycystic ovary syndrome (PCOS): do we overestimate cardiovascular risk? Horm Metab Res. 2019;51(08):539–545. doi: 10.1055/a-0896-4144 [DOI] [PubMed] [Google Scholar]
- 20.Chadha C, Kataria J, Chugh P, et al. Quality of life in young adult females with PCOS. Indian J Physiother Occup Ther - An Int J. [Internet]. 2019;13(1):40. Available from: http://www.indianjournals.com/ijor.aspx?target=ijor:ijpot&volume=13&issue=1&article=008. doi: 10.5958/0973-5674.2019.00008.X [DOI] [Google Scholar]
- 21.Taghavi SA, Bazarganipour F, Hugh-Jones S, et al. Health-related quality of life in Iranian women with polycystic ovary syndrome: a qualitative study. BMC Womens Health 2015;15(1):111. doi: 10.1186/s12905-015-0272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khomami MB, Tehrani FR, Hashemi S, et al. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 2015;10(4), e0123608 doi: 10.1371/journal.pone.0123608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ching HL, Burke V, Stuckey BGA.. Quality of life and psychological morbidity in women with polycystic ovary syndrome: body mass index, age and the provision of patient information are significant modifiers. Clin Endocrinol (Oxf). 2007;66(3):373–379. doi: 10.1111/j.1365-2265.2007.02742.x [DOI] [PubMed] [Google Scholar]
- 24.Deeks AA, Gibson-Helm ME, Paul E, et al. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Hum Reprod. 2011;26(6):1399–1407. doi: 10.1093/humrep/der071 [DOI] [PubMed] [Google Scholar]
- 25.Mayama M, Umazume T, Watari H, et al. Frequency of night shift and menstrual cycle characteristics in Japanese nurses working under two or three rotating shifts. J Occup Health. 2020;62(1):e12180. doi: 10.1002/1348-9585.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lim AJR, Huang Z, Chua SE, et al. Sleep duration, exercise, shift work and polycystic ovarian syndrome-related outcomes in a healthy population: A cross-sectional study. PLoS One [Internet]. 2016;11(11):e0167048. doi: 10.1371/journal.pone.0167048 [DOI] [PMC free article] [PubMed] [Google Scholar]