Abstract
This cohort study examines the association of reuse of N95 filtering facepiece respirators and N95 filtration efficiency.
Introduction
N95 filtering facepiece respirators (N95s) are designed to filter 95% or more of viral particles and prevent aerosolized transmission, reducing respiratory viral infections among health care clinicians.1 Under routine circumstances, N95s are discarded after 1 patient contact.2 During the COVID-19 pandemic, the Centers for Disease Control and Prevention provided strategies for extended use and limited reuse to manage shortages. Emergency department (ED) workers practiced a combination of both, which we termed reuse.3,4,5 Evidence assessing the impact of reuse on filtration efficiency (FE) in clinical settings is needed to inform conservation practices during N95 shortages. We assessed the association of reuse with N95 FE during the COVID-19 pandemic. We hypothesized that N95s reused for an increasing number of clinical shifts would result in reductions in FE, which would differ by respirator model.
Methods
The Western Copernicus Group institutional review board approved this cohort study. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
We conducted a multicenter, prospective cohort study at 6 United States EDs to assess N95 reuse by physicians, nurse practitioners, and nurses on N95 performance and safety (including FE) from April 2021 to July 2022.6 Respirator models were grouped into 3M1860 (respirator 1), 3M1870 (respirator 2), and Halyard (respirator 3) categories. The primary outcome was FE and reduced FE (below 95%) (eAppendix in Supplement 1). The exposure of interest was reuse, defined based on number of shifts (1, 2, 3, 4, or 5) worn. We reported mean and median FE by shifts worn, stratified by N95 categories, and assessed differences in FE by shift using analysis of variance (ANOVA). A mixed-effect model (including number of shifts used, N95 model, use of skin protectant, and donning and doffing) assessed factors associated with reduced FE. We performed analyses using R version 4.4.1 (R Project for Statistical Computing) with significance set at P < .05. All tests were 2-sided. Data were analyzed from June 2023 to February 2024.
Results
We enrolled 365 participants with N95s assessed for FE. Of these, 188 (52%) were physicians, 221 (61%) were female, and the median (IQR) age was 34 (30-41) years. Additionally, 148 respirators (40.5%) were respirator 1, 119 (32.6%) were respirator 2, and 98 (26.8%) were respirator 3. Wearing N95s for an increasing number of shifts was associated with reduced mean FE (ANOVA P value <.001) (Figure). The proportion of respirators with FE less than 95% increased when they were worn for more shifts—1.8% (95% CI, 0.4%-5.0%) after 1 shift; 10.1% (95% CI, 4.5%-17%) after 2 shifts; and 28.8% (95% CI, 18%-43%) after 3 shifts (Table). The adjusted odd ratio (OR) for reduced FE for 2 shifts of wear was 5.68 (95% CI, 1.43-22.5) and 35.4 (95% CI, 8.67-145) for 3 shifts of wear as compared with 1 shift a wear. The adjusted OR for Halyard was 9.84 (95% CI, 3.76-27.7).
Figure. Boxplot of Percentage Filtration Efficiency by Shifts Worn and by N95s Model.
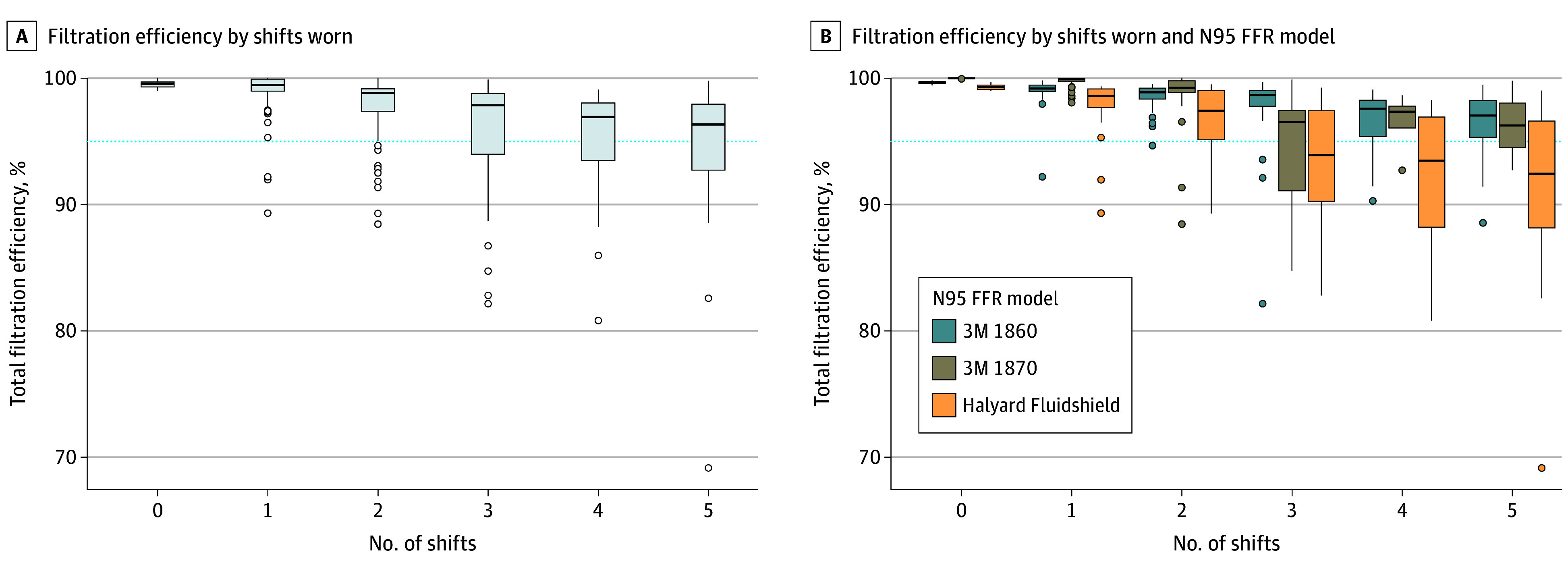
The dotted line indicates 95% filtration efficiency; circles, outliers, edges of boxes, upper and lower quartiles; center line in boxes, median value; whiskers, the minimum and maximum values.
Table. Filtration Efficiency and Proportion Below 95% by Shifts Worn, Stratified by N95s Model.
| Respirator model and shifts worn | No. | Filtration efficiency | ||
|---|---|---|---|---|
| Median (IQR), % | Mean (SD), % | <95%, No. (%)a | ||
| All models | ||||
| 0 | 30 | 99.6 (99.3-99.7) | 99.5 (0.3) | 0 |
| 1 | 170 | 99.5 (99.0-99.9) | 99.2 (1.3) | 3 (1.8) |
| 2 | 89 | 98.8 (97.4-99.2) | 97.8 (2.4) | 9 (10.1) |
| 3 | 52 | 97.9 (94.0-98.8) | 96.0 (4.5) | 15 (28.8) |
| 4 | 29 | 96.9 (93.5-98.0) | 95.2 (4.3) | 10 (34.5) |
| 5 | 25 | 96.3 (92.7-97.9) | 94.2 (6.6) | 10 (40.0) |
| Respirator 1 | ||||
| 0 | 10 | 99.7 (99.6-99.7) | 99.7 (0.1) | 0 |
| 1 | 48 | 99.2 (98.9-99.5) | 99.0 (1.1) | 1 (2.1) |
| 2 | 39 | 98.9 (98.3-99.2) | 98.6 (1.0) | 1 (2.6) |
| 3 | 30 | 98.7 (97.8-99.0) | 97.6 (3.4) | 3 (10.0) |
| 4 | 16 | 97.6 (95.4-98.2) | 96.5 (2.6) | 3 (18.8) |
| 5 | 15 | 97.1 (95.3-98.2) | 96.1 (3.1) | 4 (26.7) |
| Respirator 2 | ||||
| 0 | 5 | 100.0 (100.0-100.0) | 100.0 (0) | 0 |
| 1 | 86 | 99.9 (99.7-100.0) | 99.8 (0.4) | 0 |
| 2 | 19 | 99.2 (98.9-99.8) | 98.3 (3.1) | 2 (10.5) |
| 3 | 8 | 96.5 (91.1-97.4) | 94.3 (5.1) | 3 (37.5) |
| 4 | 4 | 97.3 (96.1-97.8) | 96.5 (2.6) | 1 (25.0) |
| 5 | 2 | 96.3 (94.5-98.0) | 96.3 (5.0) | 1 (50.0) |
| Respirator 3 | ||||
| 0 | 15 | 99.3 (99.1-99.5) | 99.3 (0.2) | 0 |
| 1 | 36 | 98.6 (97.7-99.1) | 98.0 (2.0) | 2 (5.6) |
| 2 | 31 | 97.4 (95.1-99.0) | 96.7 (2.7) | 6 (19.4) |
| 3 | 14 | 93.9 (90.3-97.4) | 93.4 (4.9) | 9 (64.3) |
| 4 | 9 | 93.4 (88.2-96.9) | 92.1 (5.9) | 6 (66.7) |
| 5 | 8 | 92.4 (88.2-96.6) | 89.9 (9.9) | 5 (62.5) |
No. and proportion of all N95s worn for 0, 1, 2, 3, 4, and 5 shifts that had a filtration efficiency below 95%.
Discussion
We found the number of shifts of reuse and respirator model were associated with reduced FE. While associated with minimal reduction in FE after 1 shift, after 3 shifts almost one-third of respirators did not filter 95% of particles. This reduction in FE differed by filtering facepiece respirator model. Limitations included observational design; because this was an observational study conducted within a larger study of N95 fit failure, randomization to the exposure was not feasible. Also, respirator effectiveness depends heavily on use in clinical practice, and FE is just 1 factor that contributes to the protection filtering facepiece respirators provide. Adherence to user instructions and fit are other factors, and it is important to note that all N95s had failed fit testing or were deemed unsuitable for further wear.2,6 Our findings suggest that while FE is preserved in N95s after a single shift of wear, ongoing reuse is significantly associated with reduced filtration performance.
eAppendix. Filtration Efficiency Measurement Protocol
Reuse N95 Group Members
Data Sharing Statement
References
- 1.NIOSH guide to the selection and use of particulate respirators. The National Institute for Occupational Health and Safety. Accessed October 23, 2022. https://www.cdc.gov/niosh/docs/96-101/default.html
- 2.Fisher EM, Shaffer RE. Considerations for recommending extended use and limited reuse of filtering facepiece respirators in health care settings. J Occup Environ Hyg. 2014;11(8):D115-D128. doi: 10.1080/15459624.2014.902954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055. doi: 10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- 4.de Perio MA, Dowell CH, Delaney LJ, et al. Strategies for optimizing the supply of N95 filtering facepiece respirators during the coronavirus disease 2019 (COVID-19) pandemic. Disaster Med Public Health Prep. 2020;14(5):658-669. doi: 10.1017/dmp.2020.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Infection control guidance: SARS-CoV-2. Accessed September 18, 2024. https://www.cdc.gov/covid/hcp/infection-control/?CDC_AAref_Val=https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- 6.Wang RC, Degesys NF, Fahimi J, et al. ; Reuse N95 Group . Incidence of fit test failure during N95 respirator reuse and extended use. JAMA Netw Open. 2024;7(1):e2353631. doi: 10.1001/jamanetworkopen.2023.53631 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Filtration Efficiency Measurement Protocol
Reuse N95 Group Members
Data Sharing Statement


