Supplemental Digital Content is Available in the Text.
Complex regional pain syndrome occurs rarely (<1%) but is not limited to specific surgical procedures. Patients in Germany are rarely supplied with pain therapy and occupational therapy.
Keywords: Complex regional pain syndrome, Incidence, Pain therapy, Claims data, Health services research
Abstract
Introduction:
Complex regional pain syndrome (CRPS) is a rare complication after limb injuries. Early recognition of the symptomatology and interdisciplinary interventions are essential to prevent long-term disability and pain.
Objective:
This article presents results on the incidence of CRPS after surgery in Germany and treatments used by patients with CRPS, using claims data from the BARMER, a German nationwide health care insurance.
Methods:
A total of N = 85,862 BARMER patients with inpatient surgery on the upper or lower limb in 2018 were included. Patients with CRPS were identified by documented International Statistical Classification of Diseases and Related Health Problems-10 diagnosis within 12 months after surgery. For the same period, medication and nonpharmaceutical therapies for inpatient and outpatient care were assessed.
Results:
The overall incidence of CRPS within 12 months after surgery was 0.34%. With 0.60%, the incidence of CRPS after surgeries of the upper limb was 3 times higher than after lower-limb surgeries (0.20%). Women were more frequently affected, and most patients were between 50 and 70 years old. About 80% to 90% of patients with CRPS received physiotherapy and nonopioid pain medication within 12 months after surgery. Approximately 40% to 50% were treated with opioids and/or antineuropathic medication. Cortisone, bisphosphonates, pain therapy, and occupational therapy were rarely claimed.
Conclusion:
We found a low incidence of CRPS after various types of surgeries. Although previous research has focused on distal radius fractures and ankle surgery, our data suggest that clinicians should be aware of CRPS after other types of surgeries as well. Real-world treatment of CRPS does not reflect recommendations in clinical practice guidelines.
1. Introduction
Complex regional pain syndrome (CRPS) is a chronic pain disorder that occurs as a rare complication after fractures or soft-tissue injuries of the upper or lower extremity. The clinical diagnostic criteria include persisting pain that is disproportionate to any inciting event, sensory alterations (hyperesthesia and allodynia), vasomotor symptoms, motor dysfunction, and trophic changes.15
Population-based studies in the United States and the Netherlands report incidence rates of 5.5 and 26.2 per 100,000 person-years, respectively.8,24 Women are affected 3 to 4 times more frequently than men, and CRPS occurs 1.5 to 2 times more often at the upper compared with the lower limb. Most studies indicate an incidence peak in patients around 50 years of age.8,21,24
Fractures represent the most common trigger, which is why most studies report CRPS incidence rates after different types of fractures, eg, 0.36% to 1% after distal radius fractures,11,14,21 0.3% after foot or ankle fractures,5 and 4 to 14% after a wrist fracture.23 Rolls et al.23 observed lower rates in conservatively managed wrist fractures, which suggests that surgical procedures might represent an additional risk factor for developing CRPS. Furthermore, CRPS incidence seems to be higher in patients with motor or sensory nerve injury.10 However, the pathogenesis of CRPS remains poorly understood.13
Although rare, CRPS causes significant individual burden, including prolonged pain, loss of motor function, and compromises to work status.7,22 For a favourable prognosis, early recognition of the symptoms and intervention is believed to be crucial.3 Treatment guidelines recommend multidisciplinary care that includes pharmaceutical and nonpharmaceutical treatments, especially oral medication and physiotherapy and occupational therapy.4 However, high-certainty evidence for the effectiveness of most pharmaceutical interventions for CRPS is still lacking.12 Psychological comorbidities should be evaluated and, if present, targeted by psychotherapy. Nevertheless, short-term access to professional diagnostics and therapy is not always straightforward. Thus, the aim of this evaluation is to describe the incidence of CRPS after different types of surgeries and the health care situation of patients with CRPS in Germany using claims data. We expected to find incidences comparable with those in other Western countries,8,21 with women and middle-aged patients being more frequently affected, and distal radius fractures bearing the highest risk of developing CRPS compared with other limb surgeries. Furthermore, it was hypothesised that real-world health care for patients with CRPS should mirror guideline-based treatment recommendations.
2. Methods
This study was conducted as part of the LOPSTER project,25 a study on the long-term outcome of perioperative pain therapy funded by the German Innovations Fund of the Federal Joint Committee in Germany (G-BA, FKz 01VSF19019). LOPSTER was approved by the ethics committee of the University Hospital Jena (approval number 2020-1952-Daten). The analyses are based on anonymised data from the BARMER, a large German statutory health insurance company with approximately 8.7 million members.1
In Germany, health insurance is mandatory for all residents. This can be through statutory or private health insurance. Most Germans are covered by statutory health insurance, which is funded through contributions from employees and employers. Individuals can choose from various providers, including the BARMER. For the present analyses, BARMER patients were included if they had undergone inpatient surgery of the upper or lower extremity in 2018. This year was chosen to ensure that treatments during a 12-month follow-up period were unaffected by the SARS-CoV-2 epidemic, which reached Germany in January 2020. If patients had more than one hospital stay with a surgical procedure, only the first stay was chosen and defined as the index stay. Surgical procedures were classified into 20 groups, comprising 9 for upper-limb surgery and 11 for lower-limb surgery. To control for a pre-existing diagnosis of CRPS, patients were identified, for whom an International Statistical Classification of Diseases and Related Health Problems-10 code for CRPS had been recorded in the 12 months before surgery. The codes and conditions used to identify CRPS are listed in Table 1.
Table 1.
ICD-10-GM (German modification) codes and conditions for identification of complex regional pain syndrome.
| G90.5x: CRPS type I |
| G90.50: CRPS type I of upper limb; G90.51: CRPS type I of lower limb; G90.59: CRPS type I, site not specified |
| G90.6x: CRPS type II |
| G90.60: CRPS type II of upper limb; G90.61: CRPS type II of lower limb; G90.69: CRPS type II, site not specified |
| G90.7x: CRPS type not specified |
| G90.70: CRPS of upper limb, type not specified; G90.71: CRPS of lower limb, type not specified; G90.79: CRPS, type and site not specified |
| M89.0x: algoneurodystrophy* |
| M89.00: algoneurodystrophy, multiple sites; M89.01: algoneurodystrophy, shoulder; M89.02 algoneurodystrophy, upper arm; M89.03: algoneurodystrophy, forearm; M89.04: algoneurodystrophy: hand; M89.05: algoneurodystrophy, pelvis and thigh; M89.06: algoneurodystrophy, lower leg; M89.07 algoneurodystrophy, ankle and foot; M89.08: algoneurodystrophy, other site; M89.09: algoneurodystrophy: site not specified |
This is an outdated term that should not be used to diagnose CRPS. However, it is still rarely used in general practice, and therefore, it was included.
CRPS, complex regional pain syndrome.
For a period of 12 months after surgery, physiotherapy and occupational therapy were recorded using settlement data from the specific health care professionals; pain therapy and psychotherapy were identified through the respective accounting codes for reimbursement, whereas medication was recorded by prescriptions using the WHO Anatomical Therapeutic Chemical classification. Definitions of variables can be found in the supplemental content, http://links.lww.com/PR9/A262. The incidence of CRPS was calculated stratified by type of surgery, sex, and age groups by decades. The proportions of patients with CRPS receiving specific treatments or medications were calculated, as well as group comparisons (χ2 tests) and odds ratios (OR) regarding health care for patients with vs without CRPS. It is important to note, however, that claims data do not allow for a specific assignment of a certain treatment to the CRPS diagnosis. All analyses were performed using R, and figures were created using Excel.
3. Results
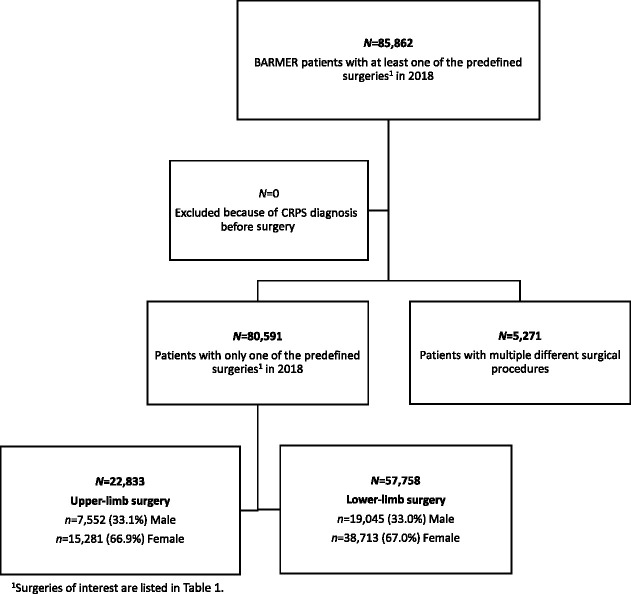
As illustrated in Figure 1, more than 85,000 BARMER patients underwent at least one of the previously defined surgeries in 2018. None of these patients had been diagnosed with CRPS in the 12 months before the procedure. A subgroup of 5,271 patients had received other surgical procedures in addition to those defined for inclusion.
Figure 1.
Flow chart with sample size and subgroups.
Within 12 months after surgery, N = 288 patients (0.34%) of the initial sample received a first-time diagnosis of CRPS. Of those with only 1 surgery, n = 251 patients (0.31%) developed CRPS during the following year. The incidence of CRPS after upper-limb surgery (0.60%, n = 138) was 3 times higher than after lower-limb surgery (0.20%, n = 113). After having had multiple surgical procedures, n = 37 patients (0.70%) were diagnosed with CRPS.
We also analysed the effects of age, sex, and type of surgery as potential risk factors for CRPS after surgery. These calculations are based on the subgroup with one of the defined surgeries only to allow for a unique classification.
3.1. Demography of the cohort in line with known distributions
The association between CRPS and age differed slightly between upper- and lower-limb surgery. Complex regional pain syndrome after upper-limb surgery was most incident in patients aged 50 to 70 years (M = 62.5 years, SD ± 11.4), whereas the peak for CRPS after lower-limb surgery was between 40 to 50 years (M = 59.4 years, SD ± 13.5). A detailed presentation of the percentage of CRPS cases in relation to the total number of patients per age decade can be found in the supplemental content, http://links.lww.com/PR9/A262.
Among females undergoing upper-limb surgery, 0.78% developed CRPS compared with 0.25% among males. For lower-limb surgery, the difference was smaller, with an incidence of CRPS of 0.24% among females and 0.11% among males.
3.2. Type of surgery
The incidence rates of CRPS by surgical groups are shown in Table 2.
Table 2.
Incidence of complex regional pain syndrome after different types of surgery.
| Type of surgery | N | CRPS incidence |
|---|---|---|
| Upper-limb surgery | ||
| Open reposition distal radius | 6,581 | 77 (1.17%) |
| Hand resection arthroplasty | 566 | 6 (1.06%) |
| Hand tendon, ligament, and fascia repair | 2,573 | 21 (0.82%) |
| Partial shoulder joint replacement proximal humerus | 129 | 1 (0.78%) |
| Decompression or neurolysis of hand or arm nerves | 930 | 7 (0.75%) |
| Shoulder joint replacement, both conventional and inverse | 1,421 | 4 (0.28%) |
| Shoulder operation | 8,456 | 18 (0.21%) |
| Open reposition proximal humerus | 2,057 | 4 (0.19%) |
| Arthrodesis interphalangeal | 120 | 0 (0.00%) |
| Total for upper-limb surgery | 22,833 | 138 (0.60%) |
| Lower-limb surgery | ||
| Arthrodesis ankle joint open | 412 | 4 (0.97%) |
| Arthroscopy ankle joint operation | 513 | 4 (0.78%) |
| Open reposition distal fibula and tibia | 4,543 | 27 (0.59%) |
| Foot surgery | 3,405 | 17 (0.50%) |
| Knee joint replacement revision | 984 | 4 (0.41%) |
| Arthroscopy knee operation | 11,189 | 18 (0.16%) |
| Hip joint replacement revision | 1,264 | 2 (0.16%) |
| Hip joint replacement | 19,164 | 25 (0.13%) |
| Toe amputation | 1,525 | 2 (0.13%) |
| Removal material femur | 913 | 1 (0.11%) |
| Knee joint replacement | 13,846 | 9 (0.07%) |
| Total for lower-limb surgery | 57,758 | 113 (0.20%) |
CRPS, complex regional pain syndrome.
The highest incidence of about 1% occurred after surgery for distal radius fracture, hand arthroplasty, or arthrodesis of the ankle. All other types of surgeries, with the exception of arthrodesis of interphalangeal joints, were also associated with a risk, albeit small, of developing CRPS.
3.3. Treatment of complex regional pain syndrome after limb surgery
Most patients with CRPS received physiotherapy and nonopioid pain medication within 12 months after surgery (Fig. 2). Almost half were treated with opioids and/or antineuropathic drugs. Only about 20% of patients with CRPS were prescribed cortisone, and even fewer were prescribed bisphosphonates. Occupational therapy, interdisciplinary pain therapy, and outpatient pain therapy were claimed by less than 30%.
Figure 2.
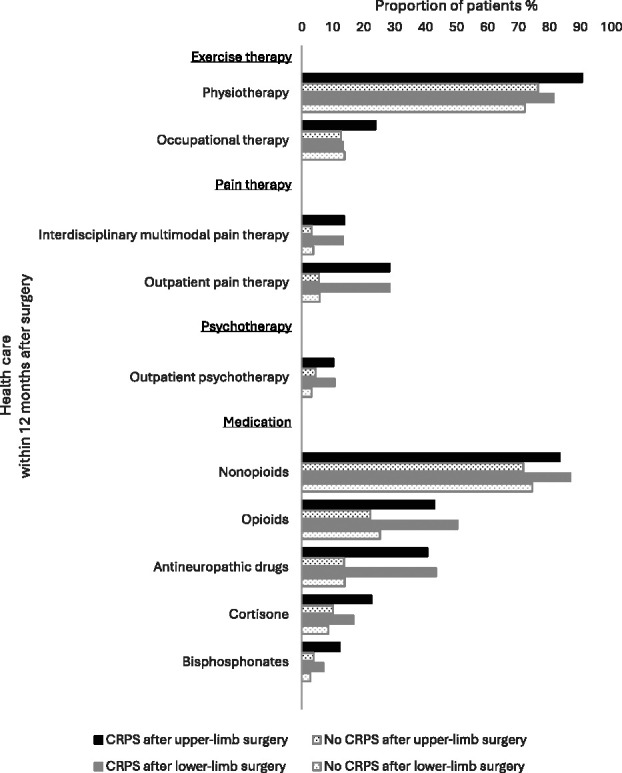
Health care for patients with and without CRPS within 1 year of limb surgery. Overall, physiotherapy and nonopioid medication were frequently claimed after limb surgery. For all treatments, the proportion of patients with CRPS and controls differed significantly, except for occupational therapy after lower-limb surgery. CRPS, complex regional pain syndrome.
During the 12-month follow-up period, a significantly higher proportion of patients with CRPS after upper-limb surgery received the investigated treatments compared with patients without CRPS after upper-limb surgery (all χ2(1) ≥ 8.75, P < 0.01). Also after lower-limb surgery, all treatments were claimed more frequently by patients with CRPS than controls (all χ2(1) ≥ 4.45, P < 0.05), except for occupational therapy (χ2(1) = 0.00, ns).
As shown in Table 3, the odds of receiving pain therapy and antineuropathic drugs were 4 to 6.5 times higher in patients with CRPS than in controls, suggesting that these treatments can most likely be attributed to the CRPS condition. The odds ratios (ORs) for bisphosphonates and cortisone were comparable with those for opioids. The lowest ORs occurred for exercise therapy after lower-limb surgery, indicating a rather unspecific usage of physiotherapy and occupational therapy in this subgroup.
Table 3.
Odds ratios for receiving treatment within 12 months after surgery.
| Treatment | Upper-limb surgery | Lower-limb surgery | ||||
|---|---|---|---|---|---|---|
| N CRPS | N noCRPS | OR [95% CI] | N CRPS | N noCRPS | OR [95% CI] | |
| Exercise therapy | ||||||
| Physiotherapy | 125 (90.6%) | 17,324 (76.3%) | 2.98 [1.75, 5.55] | 92 (81.4%) | 41,541 (72.1%) | 1.70 [1.08, 2.80] |
| Occupational therapy | 33 (23.9%) | 2,875 (12.7%) | 2.17 [1.44, 3.17] | 15 (13.3%) | 7,972 (13.8%) | 0.95 [0.53, 1.59] |
| Pain therapy | ||||||
| Interdisciplinary multimodal pain therapy | 19 (13.8%) | 740 (3.3%) | 4.74 [2.82, 7.54] | 15 (13.3%) | 2,154 (3.7%) | 3.94 [2.20, 6.59] |
| Outpatient pain therapy | 39 (28.3%) | 1,270 (5.6%) | 6.65 [4.52, 9.58] | 32 (28.3%) | 3,318 (5.8%) | 6.47 [4.23, 9.65] |
| Psychotherapy | ||||||
| Outpatient psychotherapy | 14 (10.1%) | 1,025 (4.5%) | 2.39 [1.31, 4.02] | 12 (10.6%) | 1876 (3.3%) | 3.53 [1.84, 6.17] |
| Medication | ||||||
| Nonopioids | 115 (83.3%) | 16,245 (71.6%) | 1.99 [1.29, 3.19] | 98 (86.7%) | 42,923 (74.5%) | 2.24 [1.34, 4.02] |
| Opioids | 59 (42.8%) | 5,026 (22.2%) | 2.63 [1.86, 3.68] | 57 (50.4%) | 14,565 (25.3%) | 3.01 [2.08, 4.36] |
| Antineuropathic drugs | 56 (40.6%) | 3,101 (13.4%) | 4.32 [3.05, 6.06] | 49 (43.4%) | 8,006 (13.9%) | 4.75 [3.26, 6.88] |
| Cortisone | 31 (22.5%) | 2,275 (10.0%) | 2.60 [1.71, 3.84] | 19 (16.8%) | 4,942 (8.6%) | 2.16 [1.28, 3.45] |
| Bisphosphonates | 17 (12.3%) | 853 (3.8%) | 3.60 [2.08, 5.83] | 8 (7.1%) | 1,575 (2.3%) | 2.71 [1.21, 5.23] |
CRPS, complex regional pain syndrome; OR, odds ratios.
4. Discussion
Using claims data, we found a low rate of CRPS after limb surgery when groups of surgical procedures were chosen as the first criterion. In addition to previous literature, we were able to show that not only distal radius fractures or wrist and ankle surgery are at risk of developing CRPS but also other groups of shoulder or knee surgery. Upper-limb surgery and multiple and revision surgeries were associated with higher CRPS incidence rates. This should be considered in clinical aftercare and when planning future studies for the early detection of CRPS. Also, the anatomical or physiological conditions that might contribute to the lower incidence of CRPS after knee surgery compared with ankle surgery should be investigated in the future.
Reasons for the low incidence in our data could be missed or delayed diagnosis in real-world conditions. General practitioners, who are the first points of contact for patients after hospital discharge, are probably not very familiar with the rare condition of CRPS. It may be that, in general practice, especially less severe cases with a spontaneous favorable course are less well identified than in prospective studies. Also, CRPS without previous surgery is not included in our data.
Fortunately, we found that more than 80% of patients with CRPS had access to physiotherapy, which is considered essential for functional restauration.17 Occupational therapy and interdisciplinary pain therapy were less frequently claimed. Possible reasons for this could be undertreatment, less necessity, or difficulties for patients to access these services within a 12-month period. Antineuropathic pain medication such as gabapentinoids or antidepressants, especially amitriptyline, are used frequently in CRPS26 and were prescribed to about 40% of patients with CRPS. Although recommended in the German CRPS guideline,4 bisphosphonates and cortisone were rarely used. Other nonsteroidal anti-inflammatory drugs, here nonopioid pain medication, were applied far more often. Opioids were prescribed just as frequently as antineuropathic medications, although they are recommended as second- or third-line therapy in low doses.16 However, evidence-based pharmaceutical recommendations are lacking,12 and the evaluation of treatment efficacy is beyond the scope of this article.
Most patients claimed physiotherapy and nonopioid medication, reflecting a broad indication of these treatments after limb surgery. Pain therapy and antineuropathic drugs seem to be used specifically for CRPS, whereas occupational therapy, cortisone, and bisphosphonates could be applied more specifically. According to our findings, especially treatment of lower-limb CRPS does not follow guideline recommendations.
However, these conclusions must be drawn tentatively. It remains unclear whether the prescription of a particular drug, as well as physiotherapy or occupational therapy, can be attributed to the diagnosis of CRPS or some other medical condition that we did not assess. The same applies to psychotherapy. In our sample, 10% of the patients with CRPS received outpatient psychotherapy within 1 year of surgery. Psychotherapy is indicated for patients with CRPS with high levels of anxiety, pain-related fear, and disability.2 However, given a 12-month prevalence of approximately 30% for mental disorders in the general German population,18–20 patients in our cohort may have received psychotherapy because of other, unrelated mental issues. An additional limitation is that we could not include CRPS without previous surgery. Complex regional pain syndrome can occur spontaneously or after minor injuries that do not require surgical intervention.6,9 To estimate the incidence of these cases as well, an additional control group without limb surgery during the study period would have been necessary. As it is not feasible to generate a healthy control group from claims data, prospective studies are needed to overcome this limitation. Furthermore, the inclusion of algoneurodystrophy in our analysis needs to be discussed. This was performed to increase sensitivity, although algoneurodystrophy is an outdated term that should not be used to describe CRPS. As a general limitation to the secondary analysis of claims data, we must acknowledge that the coding of diagnoses and procedures for billing purposes depends on coding practices, patients' help-seeking behavior, as well as the specific composition of health insurance policyholders.
Analyzing claims data from a large German health insurance company, we found a low incidence of CRPS (<1%) after various types of surgeries. Although previous research has focused mainly on distal radius fractures11,21 and ankle surgery,5 our data suggest that CRPS is not limited to a specific type of injury or surgery. Particularly after multiple or revision surgeries, clinicians from different medical disciplines should be aware of CRPS when providing follow-up care. Low-threshold access to adequate treatment, especially occupational therapy, and pain therapy, should be provided promptly to target pain and disability, thereby increasing the chances of a favourable prognosis.7
In summary, we found a very low incidence in real-world data compared with prospective studies. Correspondingly, the treatment reality demonstrates that more information to all stakeholders about guideline-based diagnostics and treatment of CRPS is necessary. Future studies can use these data as a basis for prevention and early detection of CRPS.
Disclosures
H.R. received consultant fees from Gruenenthal and Orion and financial support for a study by Algiax. W.M. received consultant fees from Tafalgie, Kyowa, Mundipharma, Grünenthal, Ethypharm, and Spectrum Therapeutics. His institution received research support from European Commission, Gemeinsamer Bundesausschuss (GBA), Medtronic, Pfizer, Mundipharma, Grünenthal, and Vertanical. K.T., N.R., J.D., D.S., and G.K. have no conflicts of interest.
Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A262.
Acknowledgements
This project was supported by the German Innovation Fund Project LOPSTER (01VSF19019).
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painrpts.com).
Contributor Information
Karolin Teichmüller, Email: Teichmue_K@ukw.de.
Norman Rose, Email: Norman.Rose@med.uni-jena.de.
Johannes Dreiling, Email: Johannes.Dreiling@med.uni-jena.de.
Daniel Schwarzkopf, Email: Daniel.Schwarzkopf@med.uni-jena.de.
Winfried Meißner, Email: Winfried.Meissner@med.uni-jena.de.
Heike L. Rittner, Email: rittner_h@ukw.de.
References
- [1].BARMER. Daten und Fakten zur BARMER, 2023. Available at: https://www.barmer.de/ueberuns/barmer/unternehmen-1056674. Accessed October 13, 2023. [Google Scholar]
- [2].Bean DJ, Johnson MH, Heiss-Dunlop W, Lee AC, Kydd RR. Do psychological factors influence recovery from complex regional pain syndrome type 1? A prospective study. PAIN 2015;156:2310–8. [DOI] [PubMed] [Google Scholar]
- [3].Birklein F, O'Neill D, Schlereth T. Complex regional pain syndrome: an optimistic perspective. Neurology 2015;84:89–96. [DOI] [PubMed] [Google Scholar]
- [4].Birklein F. Diagnostik und Therapie komplexer regionaler Schmerzsyndrome (CRPS), S1-Leitlinie, 2018. Available at: www.dgn.org/leitlinien. Accessed October 13, 2023. [Google Scholar]
- [5].Bullen M, Lang C, Tran P. Incidence of Complex Regional Pain Syndrome I following foot and ankle fractures using the Budapest criteria. Pain Med 2016;17:2353–9. [DOI] [PubMed] [Google Scholar]
- [6].Bussa M, Guttilla D, Lucia M, Mascaro A, Rinaldi S. Complex regional pain syndrome type I: a comprehensive review. Acta Anaesthesiol Scand 2015;59:685–97. [DOI] [PubMed] [Google Scholar]
- [7].Cave SA, Reynolds LM, Tuck NL, Aamir T, Lee AC, Bean DJ. Anxiety, disability, and pain predict outcomes of complex regional pain syndrome: an 8-year follow-up of a prospective cohort. J Pain 2023;24:1957–67. [DOI] [PubMed] [Google Scholar]
- [8].de Mos M, de Bruijn AG, Huygen FJ, Dieleman JP, Stricker BH, Sturkenboom MC. The incidence of complex regional pain syndrome: a population-based study. PAIN 2007;129:12–20. [DOI] [PubMed] [Google Scholar]
- [9].de Rooij AM, Perez RSGM, Huygen FJ, van Eijs F, van Kleef M, Bauer MCR, van Hilten JJ, Marinus J. Spontaneous onset of complex regional pain syndrome. Eur J Pain 2010;14:510–3. [DOI] [PubMed] [Google Scholar]
- [10].Demir SE, Ozaras N, Karamehmetoğlu SS, Karacan I, Aytekin E. Risk factors for complex regional pain syndrome in patients with traumatic extremity injury. Ulus Travma Acil Cerrahi Derg 2010;16:144–8. [PubMed] [Google Scholar]
- [11].Dijkstra PU, Groothoff JW, ten Duis HJ, Geertzen JH. Incidence of complex regional pain syndrome type I after fractures of the distal radius. Eur J Pain 2003;7:457–62. [DOI] [PubMed] [Google Scholar]
- [12].Ferraro MC, Cashin AG, Wand BM, Smart KM, Berryman C, Marston L, Moseley GL, McAuley JH, O'Connell NE. Interventions for treating pain and disability in adults with complex regional pain syndrome- an overview of systematic reviews. Cochrane Database Syst Rev 2023;6:CD009416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Goebel A, Baranowski A, Maurer K, Ghiai A, McCabe C, Ambler G. Intravenous immunoglobulin treatment of the complex regional pain syndrome: a randomized trial. Ann Intern Med 2010;152:152–8. [DOI] [PubMed] [Google Scholar]
- [14].Groenveld TD, Boersma EZ, Blokhuis TJ, Bloemers FW, Frolke JPM. Decreasing incidence of complex regional pain syndrome in The Netherlands: a retrospective multicenter study. Br J Pain 2022;16:214–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med 2007;8:326–31. [DOI] [PubMed] [Google Scholar]
- [16].Harden RN, McCabe CS, Goebel A, Massey M, Suvar T, Grieve S, Bruehl S. Complex regional pain syndrome: practical diagnostic and treatment guidelines, 5th edition. Pain Med 2022;23(suppl 1):S1–S53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Harden RN, Swan M, King A, Costa B, Barthel J. Treatment of complex regional pain syndrome: functional restoration. Clin J Pain 2006;22:420–4. [DOI] [PubMed] [Google Scholar]
- [18].Jacobi F, Hofler M, Siegert J, Mack S, Gerschler A, Scholl L, Busch MA, Hapke U, Maske U, Seiffert I, Gaebel W, Maier W, Wagner M, Zielasek J, Wittchen HU. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the mental health module of the German health interview and examination survey for adults (DEGS1-MH). Int J Methods Psychiatr Res 2014;23:304–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jacobi F, Hofler M, Strehle J, Mack S, Gerschler A, Scholl L, Busch MA, Hapke U, Maske U, Seiffert I, Gaebel W, Maier W, Wagner M, Zielasek J, Wittchen HU. Twelve-months prevalence of mental disorders in the German health interview and examination survey for adults—mental health module (DEGS1-MH): a methodological addendum and correction. Int J Methods Psychiatr Res 2015;24:305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jacobi F, Wittchen HU, Holting C, Hofler M, Pfister H, Muller N, Lieb R. Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS). Psychol Med 2004;34:597–611. [DOI] [PubMed] [Google Scholar]
- [21].Jo YH, Kim K, Lee BG, Kim JH, Lee CH, Lee KH. Incidence of and risk factors for Complex Regional Pain Syndrome Type 1 after surgery for distal radius fractures: a population-based study. Sci Rep 2019;9:4871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Johnson S, Cowell F, Gillespie S, Goebel A. Complex regional pain syndrome what is the outcome?—a systematic review of the course and impact of CRPS at 12 months from symptom onset and beyond. Eur J Pain 2022;26:1203–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Rolls C, McCabe C, Llewellyn A, Jones GT. What is the incidence of complex regional pain syndrome (CRPS) Type I within four months of a wrist fracture in the adult population? A systematic review. Hand Ther 2020;25:45–55. [Google Scholar]
- [24].Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. PAIN 2003;103:199–207. [DOI] [PubMed] [Google Scholar]
- [25].Schwarzkopf D, Long-term outcome of perioperative pain therapy assessed based on routine data (LOPSTER). Anaesthesist 2020;69:844–6. [DOI] [PubMed] [Google Scholar]
- [26].Shermon S, Fazio KM, Shim R, Abd-Elsayed A, Kim CH. Prescription trends in complex regional pain syndrome: a retrospective case-control study. Brain Sci 2023;13:1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A262.