Abstract
Background:
This study was conducted to compare the incidence of postoperative complications related to blood circulation in the treatment of skin defects through the transfer of ultrathin anterolateral thigh (ALT) flaps or conventional ALT flaps.
Methods:
Patients who received ultrathin ALT flap transfer (group A) and conventional ALT flap transfer (group B) due to skin defects at Peking University Shenzhen Hospital from January 2016 to January 2023 were included in this study. The postoperative incidence of ecchymosis, vascular crisis (artery or vein), and flap survival were compared between the 2 groups of patients.
Results:
In group A, 27 patients recovered and 8 patients reported ecchymosis. In addition, 32 patients achieved flap survival, 1 patient had partial flap necrosis, and 2 patients had complete flap necrosis. In group B, 61 patients recovered and 6 patients reported ecchymosis. In addition, 65 patients achieved flap survival, 1 patient had partial flap necrosis, and 1 patient had complete flap necrosis. Compared with group B, the incidence of ecchymosis was significantly higher in group A (P < 0.05).
Conclusions:
Postoperative blood circulation monitoring (especially ecchymosis) is an important part of postoperative nursing observation in the treatment of skin defects with ultrathin ALT flap transfer. There is no significant difference in the incidence of postoperative vascular crisis between ultrathin and conventional ALT flap transfer. However, the incidence of nonvenous crisis ecchymosis after ultrathin ALT flap transfer is significantly higher than that after conventional ALT flap transfer.
Takeaways
Question: To compare the incidence of postoperative blood circulation–related complications in the treatment of skin defects through the transplantation of ultrathin anterolateral thigh (ALT) flaps or conventional ALT flaps.
Findings: Postoperative blood circulation monitoring (especially ecchymosis) is an important aspect of postoperative nursing observation in the treatment of skin defects with ultrathin ALT flap transplantation.
Meaning: The incidence of nonvenous crisis ecchymosis after ultrathin ALT flap transplantation is significantly higher than that after conventional ALT flap transplantation.
INTRODUCTION
The treatment of skin defects with ultrathin anterolateral thigh (ALT) flap transfer was first reported by Hong et al.1 Since then, this technique has been increasingly used in clinical practice.1 Bhadkamkar et al2 found that the ultrathin, fascia-only ALT flap is more useful in skin defects that require thin skin coverage and good contour. Some medical staff have also found that when a flap is provided from the anterior lateral femoral donor area, the probability of complications in the donor area is low. The satisfaction rate of using this flap for treatment is high, and it can be used as a universal donor area.3Ali et al4 also believe that the ultrathin ALT flap is very suitable for folding, intubation, or tamponade, and is important in the reconstruction of the head, face, abdomen, pelvis, perineum, and in the surface reconstruction of trauma wounds. However, with the application of the ALT flap, medical staff have also discovered some possible complications during its use. Similar to conventional ALT flap transfer, this technique is also limited by the complications related to postoperative vascular crisis, which can lead to flap necrosis in severe cases.5 Because there are special observation and management characteristics of skin ecchymosis, blood circulation monitoring is particularly important during postoperative care.6 In our clinical practice, it has been demonstrated that there is a difference in the incidence of postoperative complications related to blood circulation between ultrathin and conventional ALT flap transfer in the treatment of skin defects. Given this problem, this study was designed to retrospectively analyze 102 patients at Peking University Shenzhen Hospital and compare the incidence of complications related to blood circulation between the 2 surgical techniques. These findings are expected to provide theoretical support and practical guidance for the clinical application of 2 surgical methods in the treatment of skin defects.
MATERIALS AND METHODS
Research Objects
In this study, all patients who received conventional or ultrathin ALT flap transfer for skin defects at Peking University Shenzhen Hospital from January 2016 to January 2023 were collected to conduct a retrospective study. This study was approved by the ethics committee of Peking University Shenzhen Hospital.
Inclusion and Exclusion Criteria
The inclusion criteria included (1) patients who underwent conventional (skin flap without the use of ultrathin, fascia layer incision) or ultrathin ALT flap (skin flap with the use of ultrathin, fascia layer incision) transfer at Peking University Shenzhen Hospital from January 2016 to January 2023; (2) patients who had wounds with skin defects and deep tissue exposure that required skin flap repair; (3) patients aged between 18 and 70 years (including 18 and 70 years); (4) patient had no preoperative coagulation abnormalities or thrombophilia; and (5) patients who signed the informed consent form for the surgery.
The exclusion criteria included (1) patients with hemophilia and other causes of abnormal coagulation function in preoperative examinations and (2) patients who received the treatment with anticoagulant preparations within 24 hours.
Surgical Method
In group A, after anesthesia, the incision edge of the skin flap was designed according to the location of the perforating branch. After the incision on the skin was made, the perforating branches were located and separated from the surrounding tissues on the superficial fascia plane (shallow fat layer). After reaching the vicinity of the perforating branches, the perforating blood vessels were finely dissected and separated along the perforating blood vessels towards the deep part. Finally, the main trunk of the lateral circumflex femoral artery was separated, and the pedicle was transferred to repair the donor area.
In group B, after anesthesia, the incision edge of the skin flap was designed according to the location of the perforating branch. Subsequently, the skin was cut open until the deep fascia layer, and the flap was separated with or without the deep fascia. Finally, the main artery of the lateral circumflex femoral artery was explored below the deep fascia, and the pedicle was dissected and transferred.
Postoperative Treatment
Patients in both groups received routine anti-infective, spasmolytic, analgesic, and anticoagulant treatments after surgery.
Observation Indicators and Measurement Methods
The postoperative blood circulation monitoring was performed on all flaps at an interval of 1 hour based on the observation of the color, ecchymosis and changes, skin temperature, tension, and capillary response of these flaps for a total of 5 days. Meanwhile, the flap type, the general situation of the patient, the wound type, the presence or absence of underlying conditions (such as diabetes), the onset time of vascular crisis (within 1, 3, and 7 days), and the appearance characteristics of ecchymosis (size, progression, vascular crisis, and outcome) were recorded.
Statistical Analyses
SPSS22.0 was used for statistical analyses. The Fisher exact test was conducted to compare the incidence of complications between both groups. A P value less than 0.05 indicated that there was a statistical difference.
RESULTS
Comparison Between Groups A and B
A total of 35 patients who received ultrathin ALT flap transfer and 67 patients who received conventional ALT flap transfer were included in this study. In group A, 8 patients had ecchymosis, 1 patient had venous crisis, and 2 patients had arterial crisis. After exploration, all patients with venous crisis achieved flap survival, whereas those with arterial crisis had complete flap necrosis. In group B, 6 patients had ecchymosis, and all of them presented with venous crises. After exploration, 4 patients achieved flap survival, 1 patient had partial flap necrosis, and 1 patient had complete flap necrosis. There was no statistical difference in the incidence of skin flap crisis between both groups (P > 0.05). However, the incidence of ecchymosis in group A was higher than that in group B. Only a small number of patients with ecchymosis in group A presented with venous crisis, whereas more than half of patients with ecchymosis in group B presented with venous crisis (Table 1).
Table 1.
Incidence of Complications in Groups A and B
| Groups Complication | Ecchymosis | Vascular Crisis, N (%) | P |
|---|---|---|---|
| Ultrathin group A (n = 35) | n = 8 | 8.57 (8.57) | >0.05 |
| Venous crisis (n = 1) Arterial crisis (n = 2) Traumatic ecchymosis (n = 5) |
|||
| Conventional group B (n = 67) | n = 6 | 8.95 (8.95) | |
| Venous crisis (n = 6) |
In this study, the smallest predicted frequency was 1.5 (<5), and the difference in the analysis rate was analyzed based on the Fisher exact test results in the χ2 test table.
Comparison of Postoperative Ecchymosis Between Groups A and B
The appearance of ecchymosis was different between patients with venous crisis, nonvenous crisis, and arterial crisis. Among patients with venous crisis, the ecchymosis was observed in a deeper position, the ecchymosis area expanded with time, and it could subside after vascular exploration. Among patients with nonvascular crises, the ecchymosis area was small, and the severity of ecchymosis was mild, and it could subside spontaneously. Among patients with arterial crisis, the ecchymosis area was large, but there was no venous crisis. In addition, the ecchymosis was dark, accompanied by pale skin and decreased tension (Figs. 1–7).
Fig. 1.
Postoperative ecchymosis of the patient. A venous crisis occurred 15 hours after the conventional ALT flap transfer, and thrombus formation at the venous anastomotic site was observed during emergency vascular exploration.
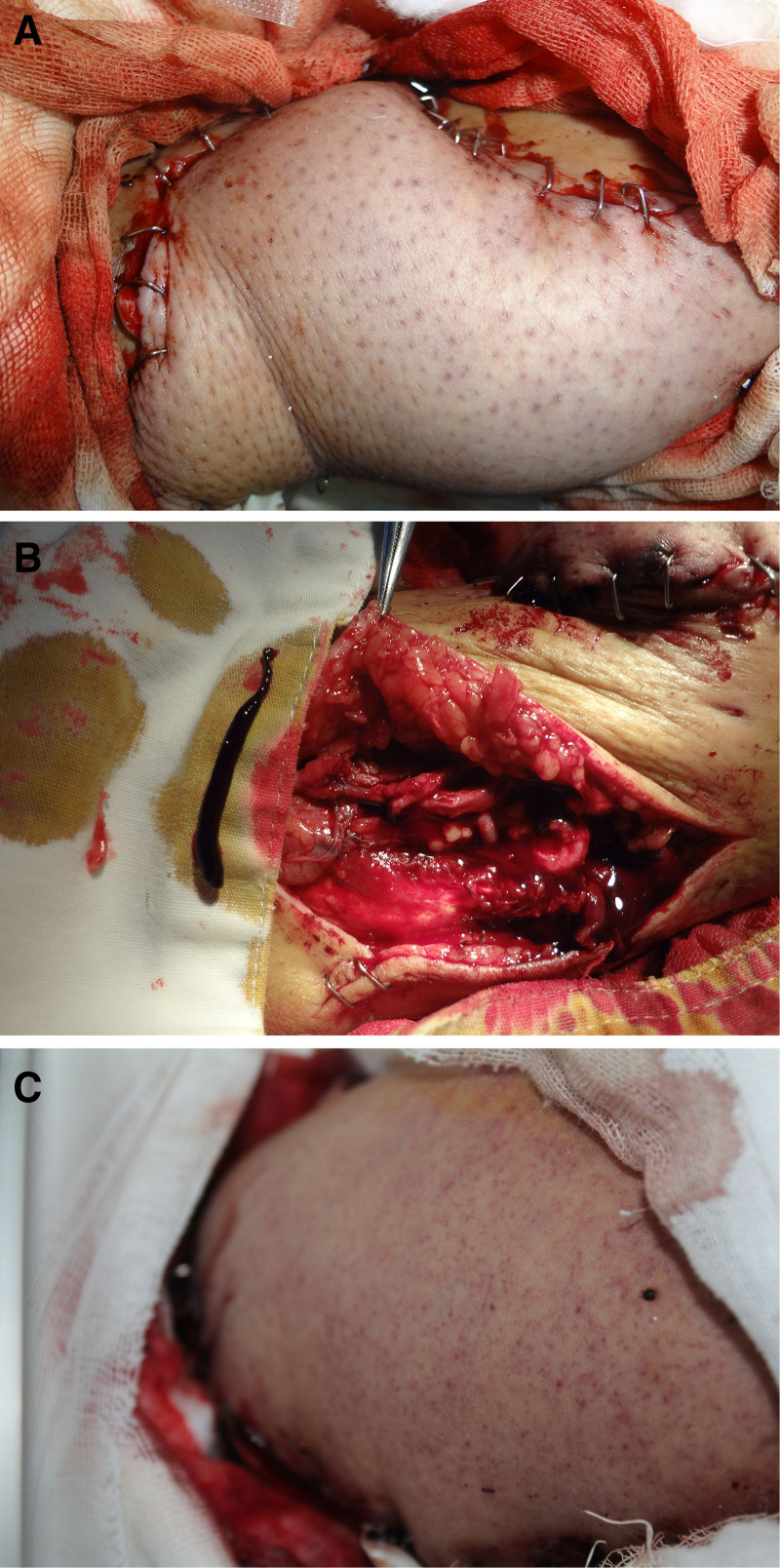
Fig. 7.
Postoperative ecchymosis of the patient. A, The venous crisis occurred 25 hours after the ultrathin ALT flap transfer for the diabetic foot ulcer. Progressively enlarged ecchymosis with high tension and low skin temperature can be observed. B, Emergency vascular exploration and thrombectomy were performed. After the vein graft was reanastomosed, the ecchymosis changed from dark purple to bright red and completely disappeared 1 week after exploration.
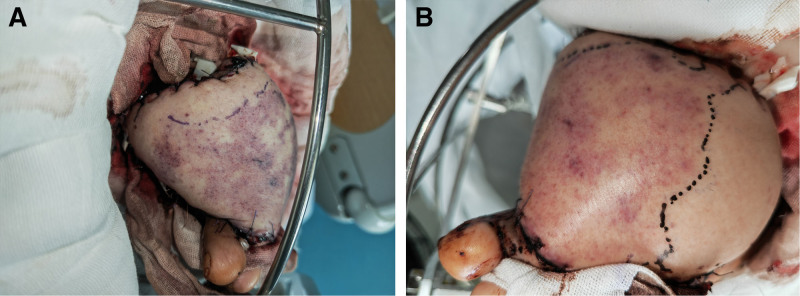
Fig. 2.
Postoperative ecchymosis of the patient. A, A venous crisis occurred on the third day after the transfer of the ultrathin ALT flap for the skin defect on the forearm, and ecchymosis gradually spreading from the periphery of the flap. B, The blood circulation in the ALT flap was improved after vascular exploration of venous crisis, thrombectomy, and reanastomosis. The ecchymosis changed from dark purple to bright red and completely dissipated 7 days after exploration. C, Two months after ALT flap salvage.
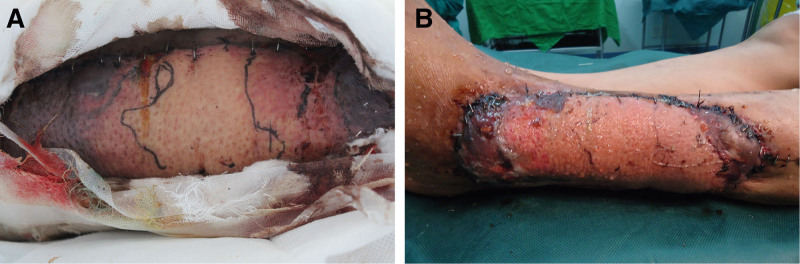
Fig. 3.
Postoperative ecchymosis of the patient. A, The venous crisis occurred 12 hours after the ALT flap transfer for osteomyelitis on the calf. B, The bruised part of the calf was observed after emergency vascular exploration, and necrosis was found in the distal part of the remnant flap 2 weeks after ALT flap transfer.
Fig. 4.
Postoperative ecchymosis of the patient. A, There was widespread scattered ecchymosis and punctate appearance for the ALT flap 5 hours after transfer. B, The venous thrombosis was confirmed at the bedside, the thrombus was removed, and the vein was anastomosed again. C, The ecchymosis changed from dark purple to bright red and completely disappeared 1 week after vascular exploration.
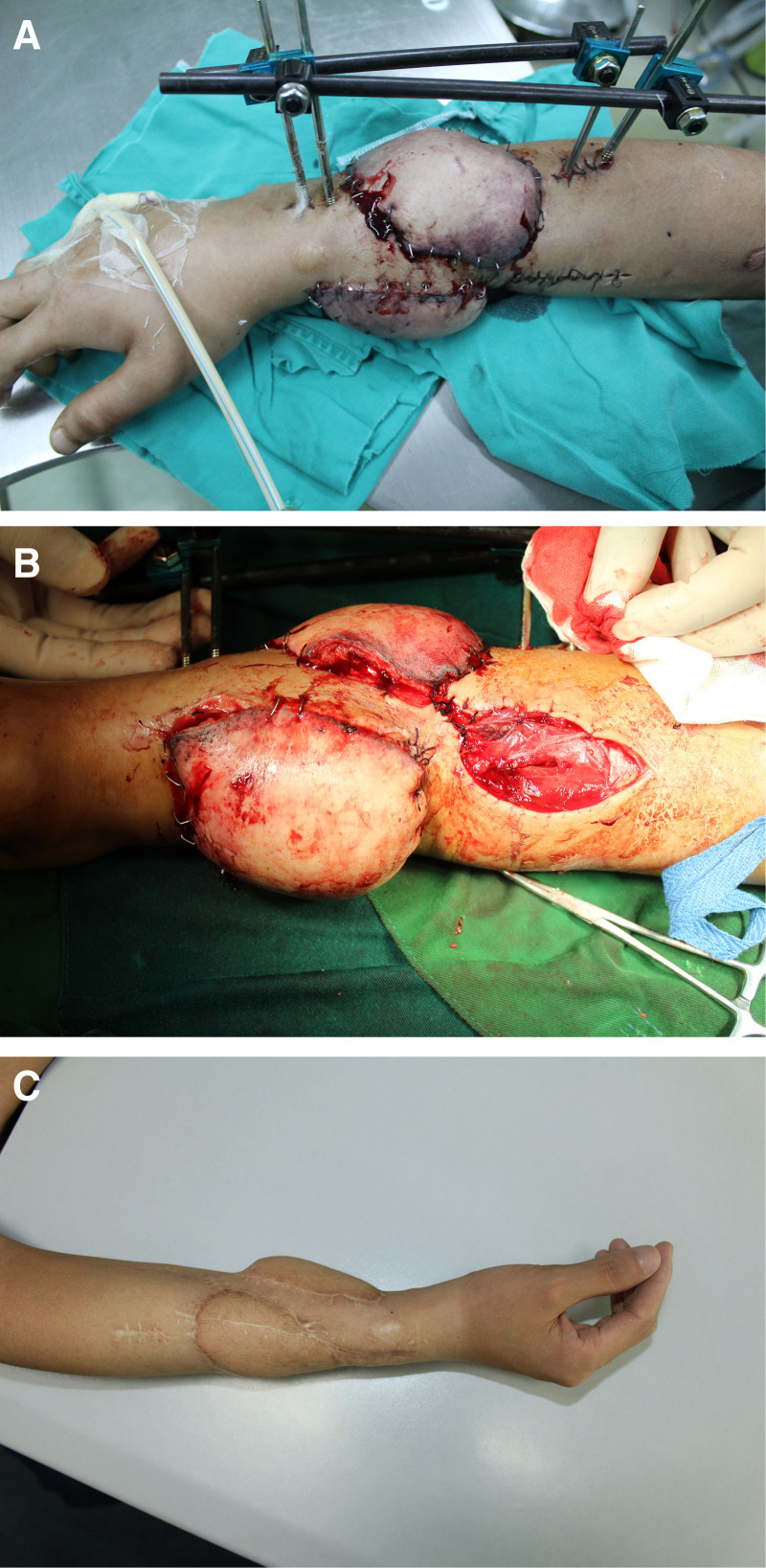
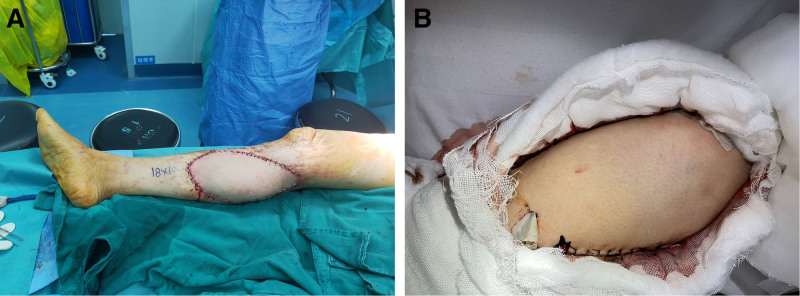
Fig. 5.
Postoperative ecchymosis of the patient. A, The ultrathin ALT flap transfer was performed after extended resection of squamous cell carcinoma on the calf. B, On the second day after transfer, widespread and scattered ecchymosis appeared, and the skin temperature, tension, and capillary response of the flap were within a normal range. It can be judged as a traumatic ecchymosis in the ultrathin ALT flap, and the lesion completely subsided 7 days after transfer. The traumatic ecchymosis of the ultrathin ALT flap with a scattered appearance and bluish purple disappeared spontaneously 1 week after transfer.
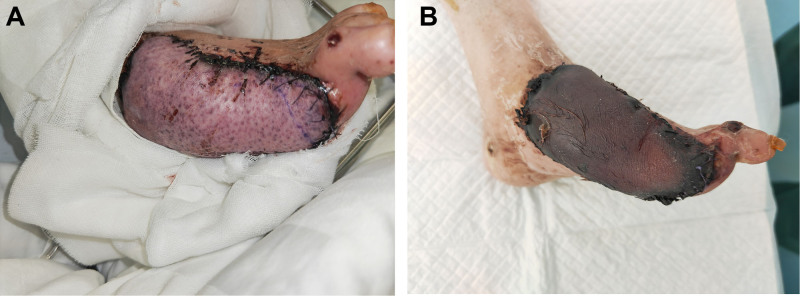
Fig. 6.
Postoperative ecchymosis of the patient. A, The ecchymosis of the skin flap was observed on the third day after the ultrathin ALT flap transfer for the diabetic foot ulcer, accompanied by low skin temperature and tension and the disappearance of capillary reaction, which can be attributed to arterial crisis. B, The complete flap necrosis occurred 3 weeks after transfer.
DISCUSSION
As a commonly used flap in reconstructive surgery, the ALT flap was first reported by Song et al.7 At present, this flap is one of the most common flaps in clinical practice.7 In 2014, Hong et al reported the ultrathin ALT flap based on the supermedical plane.7 This technique has become increasingly used in clinical practice. A vascular crisis is the most severe complication in free tissue transfer, such as flaps.8 After ultrathin ALT flap transfer, vascular crises may also occur, which may result in flap necrosis.9 It is of great significance to conduct rigorous blood circulation monitoring, detect vascular crises, and conduct vascular exploration and repair after surgery.10 The timely diagnosis of vascular crisis and early exploration can eliminate this complication in 75% of patients after flap transfer. At the same time, the proportion and necessity of using ultrathin skin flaps will decrease for patients with low body mass index values. Female patients have thick thigh fat, and even if their body mass index values are low, the necessity of using ultrathin skin flaps is much higher than that of men. Generally, ultrathin skin flaps are needed to meet the requirement of a skin flap thickness of 3–5 mm.
It is important to conduct blood supply monitoring, and it is also an important part of postoperative nursing. With the advancement of technology, some new techniques, such as pulse oxygen saturation monitoring of the skin flap, implantable ultrasound Doppler vascular pedicle blood circulation monitoring, and infrared photography of skin flap blood circulation monitoring, have been continuously reported and applied to blood circulation monitoring after skin flap transfer.11–13 However, in clinical nursing and medical practice, skin flap blood circulation, skin temperature, skin tension, capillary response, and color are still the main indicators in postoperative nursing observation and cannot be replaced by new techniques. In this study, patients who received ultrathin ALT flap transfer (35 cases) and conventional ALT flap transfer (67 cases) for skin defects were selected, and the incidence of postoperative complications related to blood circulation was compared between these patient groups. There was no significant difference in the incidence of vascular crisis between the groups. This also verified the safety of the ultrathin ALT flap, which was consistent with the statistical results of Hong et al.1
As a dangerous signal of blood circulation diseases in skin flaps, ecchymosis has received widespread attention from medical staff.14 Prasetyono and Adianto15 maintained that ecchymosis, especially widespread ecchymosis, indicated a crisis in the artery or vein of the vessel pedicle. In this study, the probability of postoperative ecchymosis in group A was higher than that in group B. However, there was no significant difference in the incidence of vascular crisis ecchymosis between the groups. Moreover, nonvascular crisis ecchymosis had a significantly lighter color and smaller area compared with vascular crisis ecchymosis. It was found that the ecchymosis can spontaneously subside within 7–10 days after transfer without the onset of skin necrosis. This may be explained by the nonvascular crisis ecchymosis of the ultrathin skin flap and the cutting of the ultrathin skin flap being within a depth range of 5 mm from the body surface. In addition, it was corroborated that the separation of the superficial fascia adipose layer in the transfer process was also a type of soft-tissue injury, which can induce posttraumatic skin ecchymosis on the body surface. It may appear 1–3 days after transfer, with a lighter color and a dispersed range. However, this complication was not accompanied by diseases related to blood circulation, such as decreased skin temperature, increased skin tension, and disappearance of capillary reactions. Moreover, it may spontaneously subside 1–2 weeks after transfer, without the onset of skin flap necrosis.
Vascular crisis ecchymosis initially appears at the periphery of the skin flap. Therefore, surgeons and nurses are required to closely observe the appearance of the skin flap after transfer. It is important to comprehensively assess the skin flap to avoid missing early peripheral ecchymosis. Prasetyono and Adianto15 confirmed that extensive ecchymosis occurred more than 1 hour after the occurrence of arterial and venous crises. This further highlighted the importance of performing early observation of the appearance of the entire flap. Under this circumstance, vascular exploration should be performed in time.
Venous ecchymosis often appears from the periphery and gradually spreads to the entire skin flap. It may be accompanied by increased skin flap tension, shortened capillary response in the early stage, prolonged or even disappeared capillary response in the later stage, and decreased skin temperature. In this study, the incidence of venous crisis was higher than that of arterial crisis. This indicated that ultrathin flaps cannot result in an increased incidence of venous crisis.16 If there is an abnormality in the blood circulation monitoring of the flap, timely vascular exploration contributes to the survival of flaps.17 In this study, flap necrosis occurred in both groups after vascular exploration. It was found that 2 patients with complete flap necrosis were identified more than 2 hours after the onset of vascular crisis. In contrast, other patients with successfully rescued flaps were identified within 1 hour after the onset of vascular crisis. This suggested that vascular exploration should be performed in time. Nevertheless, this conclusion should be verified based on more samples. In addition, it was also found that the ecchymosis gradually subsided after vascular exploration, which took about 1 week. The ecchymosis color changed from dark purple to bright red. Subsequently, the ecchymosis became increasingly lighter and eventually disappeared.
Currently, various advanced techniques have been used in clinical practice to continuously and dynamically monitor the blood circulation of flaps.18,19 This can provide information on vascular crises in time. However, these techniques are limited by the complex procedures, high costs, and requirements for special technical equipment, which also limit their clinical application. In this study, conventional techniques were used to observe these skin flaps. Despite a retention effect in the observation of skin flap color and ecchymosis, these conventional techniques can still achieve a favorable effect, which can provide a benchmark for postoperative care of patients in the clinical treatment based on ultrathin ALT flap transfer.
Nevertheless, there are also certain limitations in this study. First of all, this study only involves a single-center retrospective case analysis, and the hierarchy of evidence is not high. In the future, it is necessary to conduct a multicenter prospective randomized controlled study to provide more powerful evidence support. In addition, the sample size in our study is relatively small, and hence, a study based on a large sample size should be conducted to verify the conclusions of this study.
In conclusion, postoperative care is an important aspect of postoperative blood circulation monitoring for ultrathin ALT flap transfer. In this study, it was found that there was no significant difference in the incidence of vascular crisis between ultrathin and conventional ALT flap transfer. However, there was an increase in the incidence of nonvascular crises and plaques in ultrathin ALT flap transfer. With the assistance of other blood circulation monitoring techniques during postoperative care, the survival of flaps may be improved by timely detection and treatment of vascular crisis through observing the color of ecchymosis.
DISCLOSURES
The authors have no financial interest to declare in relation to the content of this article. This research was supported by grants from the National Natural Science Foundation of China (Nos. 82172432 and 82102568), Shenzhen Key Medical Discipline Construction Fund (No. SZXK023), Shenzhen “San-Ming” Project of Medicine (No. SZSM202211038), Shenzhen Science and Technology Program (Nos. JCYJ2022 0818102815033, KCXFZ20201221173411031, and JCYJ20210324110214040), Guangdong Basic and Applied Basic Research Foundation (Nos. 2022B1515120046, 2022A1515220111, and 2021A1515012586), and the Scientific Research Foundation of Peking University Shenzhen Hospital (No. KYQD2021099).
PATIENT CONSENT
Written informed consent was obtained from the participant(s) for the publication of this case report, and written informed consent was also obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Footnotes
Published online 21 November 2024.
Disclosure statements are at the end of this article, following the correspondence information.
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Hong JP, Choi DH, Suh H. A new plane of elevation: the superficial fascial plane for perforator flap elevation. J Reconstr Microsurg. 2014;30:491–496. [DOI] [PubMed] [Google Scholar]
- 2.Bhadkamkar MA, Wolfswinkel EM, Hatef DA, et al. The ultra-thin, fascia-only anterolateral thigh flap. J Reconstr Microsurg. 2014;30:599–606. [DOI] [PubMed] [Google Scholar]
- 3.Wolff KD, Kesting M, Thurmüller P, et al. The anterolateral thigh as a universal donor site for soft tissue reconstruction in maxillofacial surgery. J Craniomaxillofac Surg. 2006;34:323–331. [DOI] [PubMed] [Google Scholar]
- 4.Ali RS, Bluebond-Langner R, Rodriguez ED, et al. The versatility of the anterolateral thigh flap. Plast Reconstr Surg. 2009;124:e395–e407. [DOI] [PubMed] [Google Scholar]
- 5.He J, Qing L, Wu P, et al. Customized reconstruction of complex soft tissue defects in the upper extremities with variants of double skin paddle anterolateral thigh perforator flap. Injury. 2021;52:1771–1777. [DOI] [PubMed] [Google Scholar]
- 6.Tenland K, Memarzadeh K, Berggren J, et al. Perfusion monitoring shows minimal blood flow from the flap pedicle to the tarsoconjunctival flap. Ophthalmic Plast Reconstr Surg. 2019;35:346–349. [DOI] [PubMed] [Google Scholar]
- 7.Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984;37:149–159. [DOI] [PubMed] [Google Scholar]
- 8.Peng LL, Xu LY, Wang SH, et al. Development and usability of a mobile interactive application (VCPW) for vascular crisis prewarning after skin flap transplantation. JPRAS Open. 2023;37:109–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang W, Xie WG, Yang F, et al. Clinical application of lobulated transplantation of free anterolateral thigh perforator flap in the treatment of electric burns of limbs. Zhonghua Shao Shang Za Zhi. 2019;35:790–797. [DOI] [PubMed] [Google Scholar]
- 10.Giesen T, Politikou O, Tami I, et al. Retrograde free venous flaps for extremity reconstruction: a roadmap. Medicina (Kaunas). 2022;58:1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vakharia KT, Henstrom D, Lindsay R, et al. Color doppler ultrasound: effective monitoring of the buried free flap in facial reanimation. Otolaryngol Head Neck Surg. 2012;146:372–376. [DOI] [PubMed] [Google Scholar]
- 12.Spingel JH, Polat JK. Microvascular flap reconstruction by otolaryngologists: prevalence, postoperative care, and monitoring techniques. Laryngoscope. 2007;117:485–490. [DOI] [PubMed] [Google Scholar]
- 13.Oda H, Beker L, Kaizawa Y, et al. A novel technology for free flap monitoring: pilot study of a wireless, biodegradable sensor. J Reconstr Microsurg. 2020;36:182–190. [DOI] [PubMed] [Google Scholar]
- 14.Uslu A. Use of a perforator/subcutaneous pedicled propeller flap for reconstruction of lower eyelid defects. J Plast Reconstr Aesthet Surg. 2019;72:119–124. [DOI] [PubMed] [Google Scholar]
- 15.Prasetyono TOH, Adianto S. The relationship between oxygen saturation and color alteration of a compromised skin flap: experimental study on the rabbit. Arch Plast Surg. 2013;40:505–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong HH, Hong JP, Suh HS. Thin elevation: a technique for achieving thin perforator flaps. Arch Plast Surg. 2018;45:304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patial T, Kaur A, Mittal R. Use of intra operative fluorescein dye for prediction of flap viability. Pol Przegl Chir. 2022;95:46–52. [DOI] [PubMed] [Google Scholar]
- 18.Shen AY, Lonie S, Lim K, et al. Free flap monitoring, salvage, and failure timing: a systematic review. J Reconstr Microsurg. 2021;37:300–308. [DOI] [PubMed] [Google Scholar]
- 19.Kyriacou PA, Zaman T, Pal SK. Photoplethysmography in postoperative monitoring of deep inferior epigastric perforator (DIEP) free flaps. Physiol Meas. 2021;41:124001. [DOI] [PubMed] [Google Scholar]