Abstract
Aims
Pain is the most frequent complaint associated with osteonecrosis of the femoral head (ONFH), but the factors contributing to such pain are poorly understood. This study explored diverse demographic, clinical, radiological, psychological, and neurophysiological factors for their potential contribution to pain in patients with ONFH.
Methods
This cross-sectional study was carried out according to the “STrengthening the Reporting of OBservational studies in Epidemiology” statement. Data on 19 variables were collected at a single timepoint from 250 patients with ONFH who were treated at our medical centre between July and December 2023 using validated instruments or, in the case of hip pain, a numerical rating scale. Factors associated with pain severity were identified using hierarchical multifactor linear regression.
Results
Regression identified the following characteristics as independently associated with higher pain score, after adjustment for potential confounders: Association Research Circulation Osseous classification stage IIIa or IIIb, bone marrow oedema, grade 3 joint effusion, as well as higher scores on pain catastrophizing, anxiety, and central sensitization. The final model explained 69.7% of observed variance in pain scores, of which clinical and radiological factors explained 37%, while psychological and neurophysiological factors explained 24% and demographic factors explained 8.7%.
Conclusion
Multidimensional characteristics jointly contribute to the severity of pain associated with ONFH. These findings highlight the need to comprehensively identify potential contributors to pain, and to personalize management and treatment accordingly.
Cite this article: Bone Joint Res 2024;13(11):673–681.
Keywords: Osteonecrosis of the femoral head, Pain, Multidimensional characteristics, Hierarchical linear regression model, Osteonecrosis of the femoral head (ONFH), pain scoring, bone marrow oedema, anxiety symptoms, joint effusion, linear regression model, variance, hip pain, Epidemiology, t-test
Article focus
This study focuses on exploring the aetiology of pain in osteonecrosis of the femoral head (ONFH), examining various demographic, clinical, radiological, psychological, and neurophysiological factors for their potential contributions to pain in patients with ONFH.
Key messages
Clinical, radiological, psychological, and neurophysiological characteristics contribute substantially to the severity of pain associated with ONFH, while demographic characteristics contribute relatively little.
Association Research Circulation Osseous classification (ARCO) stage III, bone marrow oedema, grade 3 joint effusion, and greater pain catastrophizing, anxiety, and central sensitization independently predict greater pain associated with ONFH, so targeting these problems may alleviate pain.
MRI is effective at identifying causes of pain associated with ONFH, as are assessments of pain catastrophizing, anxiety, and pain sensitization, especially when radiology fails to identify causes.
Strengths and limitations
This study provides the first insights into the aetiology of pain in ONFH, suggesting that multidimensional characteristics may jointly contribute.
A limitation of this study is that it failed to incorporate all potentially important variables (such as pain-related genes) and excluded specific patient groups (e.g. patients who were taking analgesics).
The single-centre, cross-sectional design may introduce a degree of bias into the results, which also constitutes a limitation of this study.
Introduction
Osteonecrosis of the femoral head (ONFH), also known as avascular necrosis of the femoral head, is a refractory joint disease primarily affecting individuals aged between 30 and 60 years.1 Approximately 20 million people around the world currently have ONFH, with the incidence increasing rapidly.2-5
Symptoms of the disorder are pain, deformity, and dysfunction in the hip joint, and most patients initially seek medical help because of pain.1,6 The causes and risk factors for pain in individuals with ONFH are poorly understood, which hampers efforts to personalize pain treatments. Several studies have linked pain severity to the presence of oedema in the femoral head bone marrow,7-9 but additional factors are likely to be important.
These factors may be physical but also psychological, given that pain perception is subjective and therefore influenced by psychological and social factors.10-12 It has been suggested that the aetiology of pain should be considered in a biopsychosocial framework that integrates demographic, clinical, radiological, psychological, and neurobiological characteristics.10,11 Although demographic, clinical, and radiological characteristics are potentially important causes of the pain, they may only explain a part of observed variance in pain scores.13,14 Indeed, pain severity in various musculoskeletal diseases is known to be influenced by psychological factors, including anxiety, depression, and pain catastrophizing.13-16 Recent research has also pointed to contributions from the neurobiological factor of pain sensitization, especially central sensitization, in osteoarthritis, low back pain, and other chronic musculoskeletal diseases.17-19
Increasing evidence has linked pain severity to these multidimensional characteristics in various musculoskeletal diseases,10,13-17 but little is known regarding this association in individuals with ONFH. Therefore, we carry out the present study using cross-sectional questionnaires and hierarchical multivariable linear regression to address the following questions: 1) do multidimensional characteristics jointly contribute to ONFH-related pain?; 2) if so, to what extent can these characteristics contribute to pain in individuals with ONFH?; and 3) which of these characteristics are independently associated with pain severity?
Methods
Participants
The analysis conducted here was carried out within the framework of a larger research initiative, “Common physiological and psychological problems in patients with ONFH”, at our medical centre, the largest orthopaedic hospital in the central region of our country, where more than 5,000 ONFH patients come for treatment annually. This initiative, including the current study, was approved by the Ethics Committee of Luoyang Orthopedic Hospital of Henan Province (2023ZXKT0004-01), and all participants provided written informed consent for their anonymized medical data to be collected, analyzed, and published for research purposes. The analysis described here was performed according to the STROBE statement.20
Participants were prospectively enrolled if they were diagnosed with ONFH at our medical centre between July and December 2023. Two experienced surgeons (CY, CS) jointly diagnosed ONFH based on clinical and radiological findings. Disagreements about diagnosis were resolved through discussion with a third experienced surgeon (YL). Patients were excluded from the analysis described here if they had Perthes’ disease (“paediatric ONFH”); if they had ever undergone surgery for ONFH or, in the preceding three months, shockwave therapy for ONFH; if they concomitantly had another serious hip disease; if they had ever undergone surgery for intertrochanteric or subtrochanteric fracture; if they were currently taking analgesics or drugs against anxiety or depression; or if they were unable to understand the questionnaires in the study.
Study size
Power calculations based on 19 covariates in a hierarchical linear regression model indicated a minimal sample of 167 patients in order to achieve power of 0.9 and significance of 0.05 for an intermediate effect size of f = 0.15. The recruitment period was optimized to ensure an adequate number of participants.
Assessments and data collection
After diagnosis at our medical centre, patients were asked to provide demographic data on age, sex, intensity of regular physical labour, smoking, drinking, and number of comorbidities. BMI was determined during a routine physical examination.
Various clinical and radiological characteristics of ONFH were also recorded, including: aetiology and duration of osteonecrosis; involvement of one or both femoral heads; stage on the Association Research Circulation Osseous (ARCO) scale;21 and presence of bone marrow oedema and grade of joint effusion, both based on 3.0 T MRI within one week of diagnosis. On MRI, bone marrow oedema was defined as areas of diffuse, hypointense signal on T1-weighted images that occurred around the femoral head and neck beyond the necrotic lesion and which overlapped with areas of hyperintense signal on fat-suppressed T2-weighted images.7-9 The severity of hip joint effusion was graded based on coronal MRI as described in Huang et al7 and Mitchell et al:22 absence of fluid was categorized as grade 0; minimal fluid, grade 1; sufficient fluid to surround the femoral neck, grade 2; or distension of capsule recesses, grade 3.
The frequency and severity of anxiety symptoms were evaluated using the Generalized Anxiety Disorder Scale-7.23 The total score on the seven items ranges from 0 to 21, with higher scores indicating more severe symptoms. The frequency and severity of depression symptoms were evaluated using the Patient Health Questionnaire-9.24 The total score on the nine items ranges from 0 to 27, with higher scores indicating more severe symptoms. Pain catastrophizing (strongly negative and exaggerated thoughts in anticipation of painful stimulation)7 was evaluated using the Pain Catastrophizing Scale.25 The total score on the 13 items ranges from 0 to 52, with higher scores indicating greater pain catastrophizing. Central sensitization was evaluated using the Central Sensitization Inventory,26 for which the total score on the 25 items ranges from 0 to 100, with higher scores corresponding to more severe central sensitization. All four psychological or neurobiological questionnaires employed in our study are universally recognized for their robust reliability and validity, with a proven track record of successful application within the musculoskeletal disease population.13,14,16 To ensure utmost precision and minimize the potential for misinterpretation or ambiguity in our patients’ responses, our experienced survey personnel meticulously elaborated on every questionnaire item to each patient prior to commencement of the survey process.
Participants reported their worst hip pain during the previous 24 hours using a numerical rating scale ranging from 0 (“no pain”) to 10 (“worst pain imaginable”).27 The hip pain score for patients with bilateral osteonecrosis was defined as the higher of the two hip pain scores.
Statistical analysis
Data were analyzed statistically using Python 3.11.5 and a significance threshold of p < 0.05. Continuous data were expressed as mean (SD) if normally distributed; otherwise, they were expressed as median (IQR). Intergroup differences in the two types of continuous data were assessed for significance using, respectively, independent-samples t-test or Mann-Whitney U test. Categorical data were expressed as percentages, and intergroup differences were assessed using the chi-squared test. Characteristics were compared between patients who completed all the surveys mentioned above and those who did not in order to assess the potential of non-responder bias.
Relative contributions to pain severity by demographic, clinical, radiological, psychological, and neurophysiological variables were estimated using hierarchical multivariable linear regression. In the first step (model 1), only demographic factors were considered, to which we then added clinical and radiological factors (model 2), and finally psychosocial and neurobiological factors (model 3). The regression coefficient B of each variable indicates how much the pain score increases for each one-unit increase in that variable when all other variables are held constant. The standardized regression coefficient β of each variable indicates its relative contribution to pain score. Both the multiple explained variance (R2) and explained variance adjusted for number of variables in the model (adjusted R2) were calculated for all models.
Results
Of the 512 patients invited to participate in the study, 63 refused and 156 failed to satisfy all the inclusion criteria or met at least one exclusion criterion. Of the 293 patients for whom clinical and demographic data were collected, 250 completed all questionnaires and were included in the final analysis (Figure 1). This final group did not differ significantly from the larger group of 293 in basic demographic characteristics (Table I).
Fig. 1.
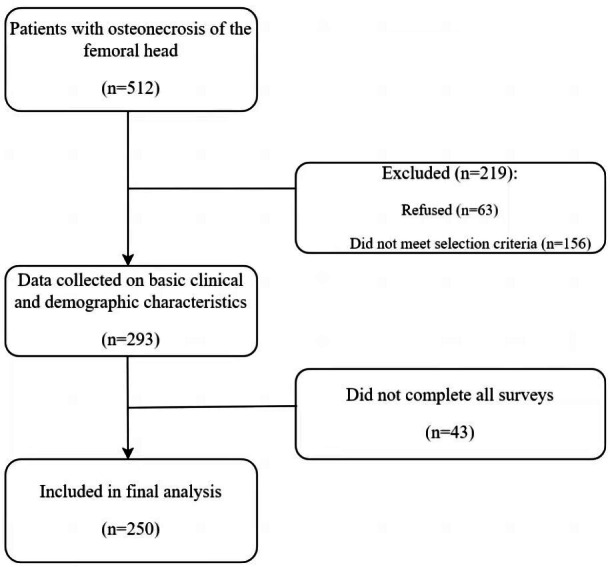
Flowchart of participant selection.
Table I.
Comparison of basic demographic characteristics between patients who were retained in the study and those who were excluded because of incomplete data.
| Characteristic | Retained (n = 250) |
Excluded (n = 43) |
p-value |
|---|---|---|---|
| Mean age, yrs (SD) | 42.1 (7.9) | 43.0 (11.5) | 0.614* |
| Male sex, n (%) | 154 (61.6) | 28 (65.1) | 0.788† |
| Mean BMI, kg/m2 (SD) | 24.2 (2.4) | 24.6 (3.4) | 0.423* |
| Intensity of physical labour, n (%) | 0.557† | ||
| None | 20 (8.0) | 5 (11.6) | |
| Light | 58 (23.2) | 7 (16.3) | |
| Moderate | 102 (40.8) | 16 (37.2) | |
| Heavy | 70 (28.0) | 15 (34.9) | |
| Smoking habits, n (%) | 0.485† | ||
| Never | 91 (36.4) | 15 (34.9) | |
| Former | 8 (3.2) | 3 (7.0) | |
| Current | 151 (60.4) | 25 (58.1) | |
| Drinks alcohol, n (%) | 0.297† | ||
| Never | 126 (50.4) | 20 (46.5) | |
| Former | 36 (14.4) | 3 (7.0) | |
| Occasionally | 44 (17.6) | 12 (27.9) | |
| Regularly | 44 (17.6) | 8 (18.6) | |
| Comorbidities, n (%) | 0.454† | ||
| None | 42 (16.8) | 8 (18.6) | |
| One | 141 (56.4) | 20 (46.5) | |
| Two or more | 67 (26.8) | 15 (34.9) |
Independent-samples t-test.
Chi-squared test.
The final group of 250 patients (61.6% male, n = 154) had a mean age of 42.1 years (SD 7.9) and had ONFH for a mean of 20.4 months (SD 12.9). The disease was in ARCO stage III in nearly half the patients (46.8%, 117/250). Most patients (70.8%, 177/250) showed bone marrow oedema, and all showed hip joint effusion. Mean scores on the surveys were as follows: Pain Catastrophizing Scale 22.2 (SD 12.5); Generalized Anxiety Disorder Scale-7 6.2 (SD 3.7); Patient Health Questionnaire-9 4.3 (SD 3.2); and Central Sensitization Inventory 23.4 (SD 13.8). Mean pain score on the numerical rating scale was 5.0 (SD 1.6). Detailed radiological, psychological, and neurophysiological characteristics of the final study population are shown in Table II and Supplementary Table i.
Table II.
Clinical, radiological, psychological, and neurophysiological characteristics of the final study population (n = 250).
| Characteristic | Value |
|---|---|
| Involvement of only one femoral head, n (%) | 170 (68.0) |
| Aetiology of osteonecrosis, n (%) | |
| Alcohol | 71 (28.4) |
| Steroid | 77 (30.8) |
| Trauma | 61 (24.4) |
| Other* | 41 (16.4) |
| Median duration of osteonecrosis, mths (IQR) | 24.0 (9.8 to 30.0) |
| ARCO stage, n (%) | |
| I | 25 (10.0) |
| II | 63 (25.2) |
| III | 117 (46.8) |
| IIIa | 61 (24.4) |
| IIIb | 56 (22.4) |
| IV | 45 (18.0) |
| Bone marrow oedema, n (%) | 177 (70.8) |
| Joint effusion grade, n (%) | |
| 0 | 0 (0) |
| 1 | 54 (21.6) |
| 2 | 86 (34.4) |
| 3 | 110 (44.0) |
| Mean Pain Catastrophizing Scale score (SD) | 22.2 (12.5) |
| Median Generalized Anxiety Disorder-7 score (IQR) | 5.0 (3.0 to 9.0) |
| Median Patient Health Questionnaire-9 score (IQR) | 4.0 (2.0 to 6.0) |
| Median Central Sensitization Inventory score (IQR) | 21.0 (11.2 to 34.8) |
| Mean maximum hip pain score on numerical rating scale (SD) | 5.0 (1.6) |
Idiopathic osteonecrosis or secondary osteonecrosis from other conditions such as sickle cell disease.
ARCO, Association Research Circulation Osseous classification.
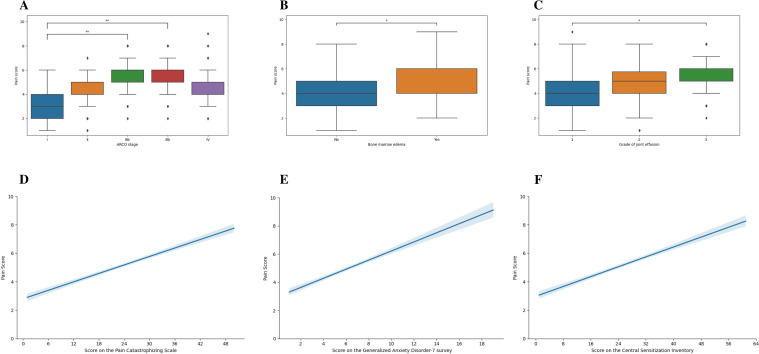
In hierarchical regression, Model 1 showed a significant association between female sex and higher pain score, which persisted in Model 2. Model 2 also showed significant associations with ARCO stages IIIa or IIIb, longer ONFH duration, bone marrow oedema, and grade 3 joint effusion. Adding psychological and neurophysiological characteristics in Model 3, in contrast, identified the following variables as significantly associated with higher pain score: ARCO stage IIIa or IIIb, bone marrow oedema, grade 3 joint effusion, as well as higher scores on the Pain Catastrophizing Scale, Generalized Anxiety Disorder-7, and Central Sensitization Inventory (Figure 2, Table III). The largest contributors to the association with higher pain score were ARCO stage IIIa (β = 0.362), ARCO stage IIIb (β = 0.352), and score on the Pain Catastrophizing Scale (β = 0.393).
Fig. 2.
Correlations in the final sample of 250 patients between self-reported hip pain scores on a numerical rating scale and a) Association Research Circulation Osseous (ARCO) stage, b) presence or absence of bone marrow oedema, c) grade of joint effusion, d) score on the Pain Catastrophizing Scale, e) score on the Generalized Anxiety Disorder-7 survey, and f) score on the Central Sensitization Inventory. The correlations are assessed using box-whisker plots for the categorical variables in a) to c), or as linear regression plots for the continuous variables in d) to f), where the blue shaded area refers to the 95% CI. *p < 0.05, **p < 0.01.
Table III.
Hierarchical linear regression to identify factors independently associated with hip pain scores.
| Factor | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B | β | B | β | B | β | |
| Age | 0.005 | 0.041 | 0.000 | 0.004 | -0.001 | -0.010 |
| Sex (ref: male) | 1.005* | 0.489* | 0.688‡ | 0.335‡ | 0.163 | 0.079 |
| BMI | -0.019 | -0.045 | -0.025 | -0.059 | -0.002 | -0.005 |
| Intensity of physical labour (ref: none) | ||||||
| Light | -0.353 | -0.149 | -0.125 | -0.053 | -0.223 | -0.094 |
| Moderate | -0.461 | -0.227 | -0.143 | -0.070 | -0.222 | -0.109 |
| Heavy | -0.412 | -0.185 | -0.198 | -0.087 | -0.364 | -0.164 |
| Smoking (ref: never) | ||||||
| Former | 0.443 | 0.213 | 0.481 | 0.231 | -0.057 | -0.027 |
| Current | 0.135 | 0.066 | 0.142 | 0.070 | -0.188 | -0.092 |
| Drinking (ref: never) | ||||||
| Former | -0.227 | -0.080 | -0.669 | -0.235 | -0.537 | -0.188 |
| Occasionally | -0.041 | -0.016 | -0.113 | -0.043 | 0.023 | 0.009 |
| Regularly | 0.033 | 0.013 | -0.402 | -0.153 | -0.511 | -0.195 |
| Comorbidities (ref: none) | ||||||
| One | -0.152 | -0.075 | -0.150 | -0.074 | -0.251 | -0.125 |
| Two or more | 0.389 | 0.172 | 0.073 | 0.032 | -0.207 | -0.092 |
| Aetiology of osteonecrosis (ref: alcohol) | ||||||
| Steroid | -0.720 | -0.333 | -0.453 | -0.209 | ||
| Traumatic | -0.535 | -0.229 | -0.615 | -0.264 | ||
| Other | -0.658 | -0.244 | -0.442 | -0.164 | ||
| Duration of osteonecrosis | 0.031‡ | 0.394‡ | 0.002 | 0.025 | ||
| Femoral head involvement (ref: unilateral) | ||||||
| Bilateral | 0.194 | 0.091 | 0.021 | 0.010 | ||
| ARCO stage (ref: I) | ||||||
| II | 0.386 | 0.167 | 0.394 | 0.171 | ||
| IIIa | 1.063‡ | 0.457‡ | 0.843‡ | 0.362‡ | ||
| IIIb | 1.136‡ | 0.4774‡ | 0.844‡ | 0.352‡ | ||
| IV | 0.966 | 0.371 | 0.644 | 0.247 | ||
| Bone marrow oedema (ref: no) | ||||||
| Yes | 0.587‡ | 0.267‡ | 0.325† | 0.148† | ||
| Joint effusion grade (ref: 1) | ||||||
| 2 | -0.149 | -0.069 | 0.182 | 0.087 | ||
| 3 | 0.560† | 0.278† | 0.370† | 0.1837† | ||
| Pain Catastrophizing Scale score | 0.031‡ | 0.393‡ | ||||
| Generalized Anxiety Disorder-7 score | 0.080† | 0.298† | ||||
| Patient Health Questionnaire-9 score | 0.052 | 0.165 | ||||
| Central Sensitization Inventory score | 0.020† | 0.276† | ||||
| Multiple R2 | 0.135 | 0.509 | 0.731 | |||
| Adjusted R2 | 0.087 | 0.455 | 0.697 | |||
p < 0.001, t-test.
p < 0.05, t-test.
p < 0.01, t-test.
ARCO, Association Research Circulation Osseous classification.
The final regression model explained 69.7% of the observed variance in pain scores, comprising 37% due to clinical and radiological characteristics, 24% due to psychological and neurophysiological characteristics, and 8.7% due to demographic characteristics.
Discussion
Using hierarchical multifactor linear regression, we provide what appear to be the first insights into the aetiology of pain associated with ONFH. Our analysis suggests that radiologically determined ARCO stage III, presence of bone marrow oedema, and grade 3 joint effusion contribute independently to self-reported hip pain intensity, as do scores on three psychosocial and neurophysiological questionnaires related to anxiety, pain catastrophizing, and central sensitization.
Demographic characteristics of the patient, primarily female sex, appear to contribute minimally to self-reported hip pain. Models 1 and 2 in our stepwise regression identified female sex as significantly associated with stronger pain, which is consistent with observations linking female sex with more severe pain in several conditions involving chronic pain.28,29 This sex bias may reflect genetic, physiological, hormonal, and psychosocial factors.29 However, sex was no longer significantly related to pain score in the final model, after controlling for confounding variables. Moreover, no other demographic variable significantly influenced perceived pain. A relatively small contribution of demographic factors to pain has also been reported for individuals with osteoarthritis.14,30 These considerations suggest that efforts to mitigate or even prevent ONFH-related pain may not differentiate patients according to demographic characteristics.
Our study found that clinical and radiological factors contribute substantially to pain in ONFH, whereas they contribute much less to pain in osteoarthritis.14,30 Bone marrow oedema, which occurs in many patients with ONFH and may arise from intramedullary venous stasis7 or through subchondral fracture of the femoral head, is strongly associated with ONFH progression and pain intensity.7-9,30,31 Nearly all patients with ONFH show hip joint effusion, as we observed in the present study, and our study provides the first evidence linking severe effusion to greater pain. Both bone marrow oedema and hip joint effusion worsen as ONFH progresses, peaking in ARCO stage III.7,9 This may explain why our patients in ARCO stage III reported the most severe pain. These findings highlight the usefulness of MRI for exploring the causes of pain in ONFH.
Substantial proportions of patients with ONFH show anxiety, depression, and pain catastrophizing,7,32 and our analysis suggests that when anxiety and pain catastrophizing are stronger, so too is perceived hip pain. Analogously, stronger symptoms of anxiety, depression, and pain catastrophizing have been linked to worse pain and lower quality of life in individuals with other musculoskeletal disorders.6,14,16,30 Detecting anxiety in patients with chronic pain can be challenging because few of them present obvious psychological symptoms.33 These considerations highlight the importance of psychological assessment of ONFH patients who report pain, especially when radiology fails to identify obvious causes of the pain. Future work should evaluate the ability of psychological interventions, such as antipsychotic drugs,34 cognitive behavioral therapy,35 and relaxation training,36 for alleviating pain associated with ONFH.
Central sensitization is a neurophysiological mechanism associated with enhanced sensitivity and pain responses, which mainly manifest as widespread hyperalgesia and allodynia caused by the augmentation of pain signalling in the spinal cord and brain.37 Traditional understanding of musculoskeletal-related pain has recently been challenged in light of evidence supporting a key role of central sensitization.38,39 Substantial evidence has linked central sensitization to chronic pain in various musculoskeletal disorders,18,37,40 but whether it occurs in ONFH is unclear. Our analysis suggests that it may also contribute heavily to pain in this disorder, which should be verified and explored further in future work, preferably involving specialized equipment such as a pressure algometer.
Current evidence has highlighted the notable connection between inflammation and the pathogenesis as well as progression of ONFH.41,42 Bone marrow oedema, severe joint effusion, and central sensitization have been associated with persistent inflammation in individuals with ONFH or other musculoskeletal disorders.43-45 Therefore, although we did not directly assess inflammation in our patients, our results imply that it may also contribute to ONFH-related pain. This finding underscores the significance of future investigations into pain-related inflammatory biomarkers, such as interleukin-1, interleukin-6, and Substance P, and the exploration of their correlation with the clinical presentation of pain in osteonecrosis.
This study has limitations. First, our results should be interpreted carefully in light of the fact that our modelling did not take into account all potentially important variables. This may help to explain why our final model was able to explain only 70% of the observed variance in self-reported hip pain. Future work should explore the potential contributions of additional patient- and disease-related factors, such as genetics, pain-related inflammatory factors, illness perception, and peripheral sensitization, to gain a more thorough understanding of pain in ONFH patients. Second, we excluded patients with a history of surgery for ONFH and those taking certain medications that could affect pain perception, such as analgesics, anxiolytics, and antidepressants. These exclusions raise the question of whether our results can be generalized to these patient populations. This limitation highlights the need for future research that is more deeply rooted in real-world clinical settings in order to understand the pain aetiology in a broader spectrum of osteonecrosis patients. Third, given the cross-sectional design of this study, we are unable to track the temporal changes in pain intensity over time. This limitation necessitates future longitudinal studies to capture the dynamic nature of pain in ONFH patients. Fourth, when assessing pain scores in patients with bilateral ONFH, we only focused on the hip experiencing more severe pain, neglecting the impact of pain in the contralateral hip. The pain in the contralateral hip may influence the precision of patients’ pain perception in the reported hip, potentially introducing a degree of bias into our findings. As such, it is important to develop a comprehensive pain scoring system that incorporates both hips for this specific patient population in future studies. Lastly, being a regional core hospital, it is likely that we see a higher proportion of patients with more severe osteonecrosis compared to primary care facilities. This scenario may introduce a patient selection bias into our study. Future multicentre studies are needed to address this potential source of bias.
In conclusion, our study provides the first insights into the aetiology of pain in ONFH, suggesting that multidimensional characteristics may jointly contribute. Of these characteristics, ARCO stage III, bone marrow oedema, grade 3 joint effusion, and greater pain catastrophizing, anxiety, and central sensitization are independently associated with greater pain severity, so targeting these characteristics may have the potential to alleviate ONFH-related pain. These findings highlight the need to comprehensively identify possible contributors to pain and guide the personalization of pain management accordingly, and support the use of MRI and psychological and pain sensitization assessment to identify potential causes of the pain.
Author contributions
C. Yue: Conceptualization, Funding acquisition, Project administration, Writing – review & editing
Z. Xue: Data curation, Formal analysis, Methodology
Y. Cheng: Data curation, Formal analysis, Investigation, Methodology
C. Sun: Investigation, Visualization, Writing – original draft
Y. Liu: Investigation, Project administration, Visualization
B. Xu: Supervision, Validation, Writing – original draft
J. Guo: Methodology, Project administration, Resources, Software
Funding statement
The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: this work is supported by the Project of Science and Technology of the Henan Province (202102310179); Heluo Talent Support Projects (2023HLTJ08); and Zhejiang Provincial Natural Science Foundation (LQ22H060003).
ICMJE COI statement
All authors report that this work is supported by the Project of Science and Technology of the Henan Province (202102310179); Heluo Talent Support Projects (2023HLTJ08); and Zhejiang Provincial Natural Science Foundation (LQ22H060003).
Data sharing
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.
Acknowledgements
We thank Xingyu Xiong PhD from West China hospital of Sichuan University for methodology support, and A. Chapin Rodríguez PhD for English language editing.
Ethical review statement
The study was approved by the hospital's Ethics Committee (2023ZXKT0004-01), and all participants provided written informed consent for their anonymized medical data to be collected, analyzed, and published for research purposes.
Open access funding
The authors report that they received open access funding for their manuscript from the Project of Science and Technology of the Henan province (202102310179).
Supplementary material
Detailed data on bone marrow edema and joint effusion grade distribution across Association Research Circulation Osseous classification stages.
© 2024 Yue et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Chen Yue, Email: Orthopedics.Yue@outlook.com.
Zhang Xue, Email: 835068143@qq.com.
Yan Cheng, Email: hnzgyancheng@163.com.
Chaojun Sun, Email: 13526432023@163.com.
Youwen Liu, Email: liuyouwen543@sina.com.
Bin Xu, Email: spotxu@163.com.
Jiayi Guo, Email: DoctorGuoJY@outlook.com.
Data Availability
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.
References
- 1. Zhao D, Zhang F, Wang B, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version) J Orthop Translat. 2020;21:100–110. doi: 10.1016/j.jot.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR. Nontraumatic osteonecrosis of the femoral head: where do we stand today? A ten-year update. J Bone Joint Surg Am. 2015;97-A(19):1604–1627. doi: 10.2106/JBJS.O.00071. [DOI] [PubMed] [Google Scholar]
- 3. Microsurgery Department of the Orthopedics Branch of the Chinese Medical Doctor Association. Group from the Osteonecrosis and Bone Defect Branch of the Chinese Association of Reparative and Reconstructive Surgery. Microsurgery and Reconstructive Surgery Group of the Orthopedics Branch of the Chinese Medical Association Chinese guideline for the diagnosis and treatment of osteonecrosis of the femoral head in adults. Orthop Surg. 2017;9(1):3–12. doi: 10.1111/os.12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bergman J, Nordström A, Nordström P. Epidemiology of osteonecrosis among older adults in Sweden. Osteoporos Int. 2019;30(5):965–973. doi: 10.1007/s00198-018-04826-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Snowden GT, Clement ND, Zhang S, Xue Q, Simpson A. Orthopaedic long COVID - the unknown unknowns: are we facing a pandemic of avascular necrosis following COVID-19? Bone Joint Res. 2022;11(1):10–11. doi: 10.1302/2046-3758.111.BJR-2021-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wood TJ, Thornley P, Petruccelli D, Kabali C, Winemaker M, de Beer J. Preoperative predictors of pain catastrophizing, anxiety, and depression in patients undergoing total joint arthroplasty. J Arthroplasty. 2016;31(12):2750–2756. doi: 10.1016/j.arth.2016.05.056. [DOI] [PubMed] [Google Scholar]
- 7. Huang GS, Chan WP, Chang YC, Chang CY, Chen CY, Yu JS. MR imaging of bone marrow edema and joint effusion in patients with osteonecrosis of the femoral head: relationship to pain. AJR Am J Roentgenol. 2003;181(2):545–549. doi: 10.2214/ajr.181.2.1810545. [DOI] [PubMed] [Google Scholar]
- 8. Hatanaka H, Motomura G, Ikemura S, et al. Differences in magnetic resonance findings between symptomatic and asymptomatic pre-collapse osteonecrosis of the femoral head. Eur J Radiol. 2019;112:1–6. doi: 10.1016/j.ejrad.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 9. Kim YM, Oh HC, Kim HJ. The pattern of bone marrow oedema on MRI in osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000;82-B(6):837–841. doi: 10.1302/0301-620x.82b6.10740. [DOI] [PubMed] [Google Scholar]
- 10. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–2097. doi: 10.1016/S0140-6736(21)00393-7. [DOI] [PubMed] [Google Scholar]
- 12. Allegri M, Clark MR, De Andrés J, Jensen TS. Acute and chronic pain: where we are and where we have to go. Minerva Anestesiol. 2012;78(2):222–235. [PubMed] [Google Scholar]
- 13. Wouters RM, Vranceanu A-M, Slijper HP, et al. Patients with thumb-base osteoarthritis scheduled for surgery have more symptoms, worse psychological profile, and higher expectations than nonsurgical counterparts: a large cohort analysis. Clin Orthop Relat Res. 2019;477(12):2735–2746. doi: 10.1097/CORR.0000000000000897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hoogendam L, van der Oest MJW, Tsehaie J, et al. Psychological factors are more strongly associated with pain than radiographic severity in non-invasively treated first carpometacarpal osteoarthritis. Disabil Rehabil. 2021;43(13):1897–1902. doi: 10.1080/09638288.2019.1685602. [DOI] [PubMed] [Google Scholar]
- 15. Fu K, Metcalf B, Bennell KL, et al. The association between psychological factors and pain exacerbations in hip osteoarthritis. Rheumatol (Sunnyvale) 2021;60(3):1291–1299. doi: 10.1093/rheumatology/keaa494. [DOI] [PubMed] [Google Scholar]
- 16. Dahmani D, Taik FZ, Berrichi I, Fourtassi M, Abourazzak FE. Impact of central sensitization on pain, disability and psychological distress in patients with knee osteoarthritis and chronic low back pain. BMC Musculoskelet Disord. 2023;24(1):877. doi: 10.1186/s12891-023-07019-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hattori T, Shimo K, Niwa Y, Tokiwa Y, Matsubara T. Association of chronic pain with radiologic severity and central sensitization in hip osteoarthritis patients. J Pain Res. 2021;14:1153–1160. doi: 10.2147/JPR.S296273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sanzarello I, Merlini L, Rosa MA, et al. Central sensitization in chronic low back pain: a narrative review. J Back Musculoskelet Rehabil. 2016;29(4):625–633. doi: 10.3233/BMR-160685. [DOI] [PubMed] [Google Scholar]
- 19. Nijs J, Paul van Wilgen C, Van Oosterwijck J, van Ittersum M, Meeus M. How to explain central sensitization to patients with “unexplained” chronic musculoskeletal pain: practice guidelines. Man Ther. 2011;16(5):413–418. doi: 10.1016/j.math.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 20. Elm E von, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yoon BH, Mont MA, Koo KH, et al. The 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head. J Arthroplasty. 2020;35(4):933–940. doi: 10.1016/j.arth.2019.11.029. [DOI] [PubMed] [Google Scholar]
- 22. Mitchell DG, Rao V, Dalinka M, et al. MRI of joint fluid in the normal and ischemic hip. AJR Am J Roentgenol. 1986;146(6):1215–1218. doi: 10.2214/ajr.146.6.1215. [DOI] [PubMed] [Google Scholar]
- 23. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–532. doi: 10.1037//1040-3590.7.4.524. [DOI] [Google Scholar]
- 26. Mayer TG, Neblett R, Cohen H, et al. The development and psychometric validation of the central sensitization inventory. Pain Pract. 2012;12(4):276–285. doi: 10.1111/j.1533-2500.2011.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 28. Osborne NR, Davis KD. Sex and gender differences in pain. Int Rev Neurobiol. 2022;164:277–307. doi: 10.1016/bs.irn.2022.06.013. [DOI] [PubMed] [Google Scholar]
- 29. Pieretti S, Di Giannuario A, Di Giovannandrea R, et al. Gender differences in pain and its relief. Ann Ist Super Sanita. 2016;52(2):184–189. doi: 10.4415/ANN_16_02_09. [DOI] [PubMed] [Google Scholar]
- 30. Blackburn J, van der Oest MJW, Selles RW, et al. Which psychological variables are associated with pain and function before surgery for de quervain’s tenosynovitis? A cross-sectional study. Clin Orthop Relat Res. 2019;477(12):2750–2758. doi: 10.1097/CORR.0000000000000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meier R, Kraus TM, Schaeffeler C, et al. Bone marrow oedema on MR imaging indicates ARCO stage 3 disease in patients with AVN of the femoral head. Eur Radiol. 2014;24(9):2271–2278. doi: 10.1007/s00330-014-3216-8. [DOI] [PubMed] [Google Scholar]
- 32. Chen S-B, Hu H, Gao Y-S, He H-Y, Jin D-X, Zhang C-Q. Prevalence of clinical anxiety, clinical depression and associated risk factors in chinese young and middle-aged patients with osteonecrosis of the femoral head. PLoS One. 2015;10(3):e0120234. doi: 10.1371/journal.pone.0120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Barnett LA, Pritchard MG, Edwards JJ, et al. Relationship of anxiety with joint pain and its management: a population survey. Musculoskeletal Care. 2018;16(3):353–362. doi: 10.1002/msc.1243. [DOI] [PubMed] [Google Scholar]
- 34. Vela J, Dreyer L, Petersen KK, Arendt-Nielsen L, Duch KS, Kristensen S. Cannabidiol treatment in hand osteoarthritis and psoriatic arthritis: a randomized, double-blind, placebo-controlled trial. Pain. 2022;163(6):1206–1214. doi: 10.1097/j.pain.0000000000002466. [DOI] [PubMed] [Google Scholar]
- 35. Majeed MH, Ali AA, Sudak DM. Psychotherapeutic interventions for chronic pain: evidence, rationale, and advantages. Int J Psychiatry Med. 2019;54(2):140–149. doi: 10.1177/0091217418791447. [DOI] [PubMed] [Google Scholar]
- 36. Álvarez-Melcón AC, Valero-Alcaide R, Atín-Arratibel MA, Melcón-Álvarez A, Beneit-Montesinos JV. Effects of physical therapy and relaxation techniques on the parameters of pain in university students with tension-type headache: a randomised controlled clinical trial. Neurol Ed. 2018;33(4):233–243. doi: 10.1016/j.nrl.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 37. van Griensven H, Schmid A, Trendafilova T, Low M. Central sensitization in musculoskeletal pain: lost in translation? J Orthop Sports Phys Ther. 2020;50(11):592–596. doi: 10.2519/jospt.2020.0610. [DOI] [PubMed] [Google Scholar]
- 38. Lluch Girbés E, Meeus M, Baert I, Nijs J. Balancing “hands-on” with “hands-off” physical therapy interventions for the treatment of central sensitization pain in osteoarthritis. Man Ther. 2015;20(2):349–352. doi: 10.1016/j.math.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 39. López-Ruiz M, Losilla JM, Monfort J, et al. Central sensitization in knee osteoarthritis and fibromyalgia: beyond depression and anxiety. PLoS One. 2019;14(12):e0225836. doi: 10.1371/journal.pone.0225836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Steen Pettersen P, Neogi T, Magnusson K, et al. Associations between joint pathologies and central sensitization in persons with hand osteoarthritis: results from the Nor-Hand study. Rheumatology (Oxford) 2022;61(6):2316–2324. doi: 10.1093/rheumatology/keab708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ma M, Tan Z, Li W, Zhang H, Liu Y, Yue C. Osteoimmunology and osteonecrosis of the femoral head. Bone Joint Res. 2022;11(1):26–28. doi: 10.1302/2046-3758.111.BJR-2021-0467.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ma M, Tan Z, Li W, Zhang H, Liu Y, Yue C. Infographic: osteoimmunology mechanism of osteonecrosis of the femoral head. Bone Joint Res. 2022;11(1):29–31. doi: 10.1302/2046-3758.111.BJR-2021-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Molfetta L, Florian A, Saviola G, Frediani B. Bone marrow edema: pathogenetic features. Clin Ter. 2022;173(5):434–439. doi: 10.7417/CT.2022.2459. [DOI] [PubMed] [Google Scholar]
- 44. Tan Z, Wang Y, Chen Y, et al. The dynamic feature of macrophage M1/M2 imbalance facilitates the progression of non-traumatic osteonecrosis of the femoral head. Front Bioeng Biotechnol. 2022;10:912133. doi: 10.3389/fbioe.2022.912133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129(2):343–366. doi: 10.1097/ALN.0000000000002130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings for this study are available to other researchers from the corresponding author upon reasonable request.