Abstract
Introduction
The purpose of this study was to elucidate differences and similarities in revision rates amongst studies and national registers featuring total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA). Thereby comparability and reproducibility between study and register findings should be created.
Materials and Methods
Clinical studies published between 2004 and September 2023 involving TKA or UKA were reviewed for total arthroplasty numbers, revision rates and demographic data. Findings were calculated as “revisions per 100 component years (CY)” and divided according to the nationality of the center. National arthroplasty registers were searched for numbers of arthroplasties and revisions alongside with demographic data. Revision rates in registers were compared to one another and comparison to revision rates from collected studies was drawn.
Results
After evaluation, 98 studies and seven registers met our inclusion criteria and were included in this study. Cumulative percent revision rate in studies was 3.35% after a mean follow-up of 5.7 years, corresponding to 0.71 revisions per 100 CY for TKA and 7.67% after a mean follow-up of 4.9 years, corresponding to 1.3 revisions per 100 CY for UKA. Registers showed mean overall revision rates of 5.63% for TKA and 11.04% for UKA.
Conclusions
A positive correlation of revision rates of TKA and UKA in studies and registers was found, with overall revision rates of UKA comparted to TKA being 2.29 times higher in clinical studies and 1.96 times higher in registers. Revision rates in registers were 1.56 times higher than presented in clinical studies.
Keywords: Unicompartmental knee arthroplasty, Total knee arthroplasty, Arthroplasty register, Revision rate, Systematic review
Introduction
Total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA) provide effective, rapid, and economical methods in restoring physiological articular function, reducing pain, and improving the quality of life in patients with severe osteoarthritis (OA) [1–3]. The prevalence of OA is steadily increasing as the obesity epidemic and aging of the population is gaining traction [2, 4]. If the OA is limited to one compartment, UKA enables the treatment of exclusively the medial or lateral compartment, while TKA is commonly used in knees, where the affected area is greater than one compartment [5, 6]. Unicompartmental knee arthroplasties show less mortality, morbidity and blood loss due to less resection of tissue, while restoring the normal kinematics of the joint by maintaining the function of the cruciate ligaments, resulting in superior functional outcome in comparison to TKA [5, 7]. Besides, patients receiving UKA being younger and more active, the recovery period and duration of hospitalization is shorter and major complications were registered less frequently, which results in lower cost in respect to TKA [5, 7].
Revision surgery of knee arthroplasty is scarse, but has severe consequences for the quality of life of the patient [5, 8, 9]. Most common reasons for revision surgery are infection, aseptic loosening, periprosthetic fracture, instability, pain, arthrofibrosis, polyethylene wear, patella failure or implant failure [8, 10, 11]. Higher revision rates in UKA compared to TKA is not linked to the younger age of patients receiving UKA or poorer outcome, but lower threshold considering revision surgery, which will typically result in a TKA [5, 12, 13]. Furthermore surgeons who perform less UKA tend to have higher revision rates [5, 7]. While clinical studies present a small part of the patient population, national registers include all surgeries performed in a country. To provide further assessment of revision rates of TKA and UKA and compare clinical results amongst countries, it is vital to draw comparisons between clinical studies and national registers and among one another [14, 15].
The aim of this meta-analysis was to evaluate, whether revision rates of TKA and UKA reported in clinical studies and national arthroplasty registers show potential correlation amongst different regions. Our hypothesis was, that regions presenting higher revision rates for TKA and UKA in registries, also show relatively high revision rates in studies.
Methods
Search strategy
A systematic research concerning revision rates of UKA and TKA was performed consulting Embase, PubMed and the Cochrane Controlled Trials Registry using the search terms: “(“unicompartmental knee arthroplasty” OR “total knee arthroplasty”) AND (“revision rates” OR “survival rates”)” [16, 17]. After titles and abstracts were reviewed by hand, we analyzed full text studies and noted relevant information in September 2023. References of included studies were screened for articles who could provide further case numbers and were excluded by our search term. Upon request, the complete results including our absolute research algorithm will be available. The PRISMA guideline (Preferred Reporting Items for Systematic Reviews and Meta-analyses) was used to ensure the highest quality of results [18].
Inclusion/exclusion
Inclusion criteria were clinical studies covering TKA and UKA with publication dates between 01.01.2004 and 11.09.2023. The follow-up time had to exceed 12 months and revision rates and reasons for revision had to be mentioned or could be calculated from the provided data. Revision surgery was defined as the removal, addition, or replacement of at least one component of the implanted prothesis or reoperation due to linked complications. Furthermore, information regarding geographical location of the medical center, component design, fixation type, mean age and sex had to be stated. Only papers published in peer-reviewed journals published in English or German language were examined. Comparing multiple studies treating the same cohort, the trial with the longest follow-up-period was included. Cadaveric studies, reviews, meta-analyses, imaging studies and case reports, along with trails showing less than a 12-month follow-up period were excluded. Studies reporting on data from private registers were included.
Quality assessment
All national arthroplasty registers and studies were searched by the author and co-author (S.O. and L.R.) independently to prevent bias. The Levels of Evidence according to the Oxford Centre for Evidence-Based Medicine were assessed when provided [19].
Data extraction
Every study that fulfilled the inclusion criteria was independently reviewed in full-text by the authors (S.O. and L.R.). The following data was noted: name of the article, PMID, DOI, authors, year of publication, country of publication, total UKA and TKA, distribution of sex, mean age, mean follow-up, number of revisions UKA/TKA and reasons for revision. Further calculations were made using this information. The process was supervised by the senior author who resolved any disagreements on consensus discussions between authors. Missing absolute revision numbers were calculated when possible.
Acquirement of clinical studies
Our search algorithm revealed 547 articles, of which 347 articles were excluded after a screening of title and abstract and application of inclusion and exclusion criteria. A total of 200 studies were evaluated as a whole. Finally, 98 articles met our inclusion and exclusion criteria and were used for assessment (Fig. 1).
Fig. 1.
Search process and acquirement of clinical studies and national registers
Clinical studies on revision rates of total knee arthroplasty
There were 461,387 total knee arthroplasties from 72 articles, covering a total of 2,695,243.4 observed CY. Studies included in our review were published from 2005 to 2023 (Table 1).
Table 1.
Data of clinical studies portraying total knee arthroplasty
| Authors | Year of publication | Country | Total TKA (n) | Mean Age (y) | Mean follow-up (y) | Revisions TKA (n) |
|---|---|---|---|---|---|---|
| Katchky et al.[20] | 2019 | Australia | 100 | 68 | 5.3 | 2 |
| Klasan et al.[21] | 2019 | Australia | 1288 | 76.6 | 7.8 | 13 |
| Hazratwala et al.[22] | 2023 | Australia | 165 | 65.1 | 2 | 3 |
| Victor et al.[23] | 2014 | Belgium | 245 | 68.1 | 11 | 11 |
| Beaupré et al.[24] | 2007 | Canada | 81 | 63.4 | 5 | 2 |
| MacDonald et al.[25] | 2008 | Canada | 5279 | 68.8 | 10.3 | 472 |
| Chaudhary et al.[26] | 2008 | Canada | 100 | 69.7 | 1.9 | 2 |
| Sando et al.[27] | 2015 | Canada | 414 | 68.9 | 12.3 | 11 |
| Rhee et al.[28] | 2018 | Canada | 17,243 | 67.1 | 1 | 241 |
| Demcoe et al.[29] | 2019 | Canada | 2815 | 64.7 | 3.2 | 63 |
| Khoshbin et al.[30] | 2019 | Canada | 450 | 67.8 | 7.4 | 14 |
| Teeter et al.[31] | 2019 | Canada | 50 | 69.2 | 2 | 4 |
| Garceau et al.[32] | 2020 | Canada | 390 | 64.6 | 4 | 43 |
| Shen et al.[33] | 2009 | China | 68 | 61 | 5.9 | 1 |
| Luo et al.[34] | 2022 | China | 200 | 68.8 | 5 | 3 |
| Wang et al.[35] | 2022 | China | 120 | 65.9 | 8.6 | 1 |
| Gaillard et al.[36] | 2016 | France | 4189 | 70.4 | 3.3 | 87 |
| Putman et al.[37] | 2018 | France | 263 | 61 | 9.3 | 18 |
| Erivan et al.[38] | 2019 | France | 202 | 70.8 | 15 | 14 |
| Schnurr et al.[39] | 2012 | Germany | 1121 | 68 | 2.9 | 32 |
| Hotfiel et al.[40] | 2017 | Germany | 72 | 62 | 10.3 | 3 |
| Fuchs et al.[41] | 2018 | Germany | 79 | 59 | 5.8 | 9 |
| Iosifidis et al.[42] | 2014 | Greece | 100 | 70 | 9.5 | 3 |
| Bouras et al.[43] | 2017 | Greece | 206 | 67.8 | 13.2 | 17 |
| Innocenti et al.[44] | 2014 | Italy | 87 | 58.8 | 11.3 | 2 |
| Rossi et al.[45] | 2020 | Italy | 72 | 66 | 10 | 3 |
| Giustra et al.[46] | 2023 | Italy | 128 | 71.5 | 12.5 | 4 |
| Nakamura et al.[47] | 2014 | Japan | 505 | 68.8 | 12.4 | 20 |
| Ueyama et al.[48] | 2020 | Japan | 257 | 76,2 | 10.1 | 10 |
| Schepers et al.[49] | 2012 | South Africa | 154 | 67.5 | 5 | 3 |
| Bae et al.[50] | 2012 | South Korea | 3014 | 63.4 | 10.2 | 156 |
| Lee et al.[51] | 2013 | South Korea | 106 | 67 | 5.1 | 4 |
| Kim et al.[52] | 2014 | South Korea | 888 | 66.5 | 12.2 | 11 |
| Kim et al.[53] | 2016 | South Korea | 1190 | 53.3 | 12.6 | 42 |
| Yang et al.[54] | 2017 | South Korea | 113 | 66.9 | 10.1 | 5 |
| Kim et al.[55] | 2017 | South Korea | 364 | 65,6 | 11 | 5 |
| Park et al.[56] | 2018 | South Korea | 334 | 70.3 | 10 | 10 |
| Oh et al.[57] | 2018 | South Korea | 496 | 66.4 | 9.3 | 10 |
| Kim et al.[58] | 2021 | South Korea | 190 | 65 | 20.3 | 5 |
| Kim et al.[59] | 2021 | South Korea | 268 | 69.1 | 11.1 | 14 |
| Baek et al.[60] | 2021 | South Korea | 585 | 67.5 | 11.2 | 16 |
| Baek et al.[61] | 2022 | South Korea | 171 | 60.3 | 12.5 | 12 |
| Lee et al.[62] | 2023 | South Korea | 855 | 71.5 | 11.9 | 30 |
| Munzinger et al.[63] | 2010 | Switzerland | 411 | 67 | 5.1 | 12 |
| Nouta et al.[64] | 2012 | The Netherlands | 104 | 67 | 11 | 3 |
| Kievit et al.[65] | 2013 | The Netherlands | 807 | 67 | 3.6 | 27 |
| Willems et al.[66] | 2020 | The Netherlands | 408 | 68.4 | 5 | 18 |
| van Ooij et al.[67] | 2022 | The Netherlands | 1271 | 65.5 | 20.5 | 128 |
| Clayton et al.[68] | 2006 | UK | 212 | 67 | 5.1 | 6 |
| Keenan et al.[69] | 2019 | UK | 249 | 66.7 | 10 | 14 |
| Clark et al.[70] | 2021 | UK | 127 | 65.2 | 5 | 3 |
| Brown et al.[71] | 2021 | UK | 2172 | 68 | 5 | 62 |
| Farhan-Alanie et al.[72] | 2023 | UK | 199 | 65.1 | 10 | 11 |
| Boettner et al.[73] | 2016 | USA | 181 | 67 | 3.3 | 5 |
| Chan et al.[74] | 2017 | USA CA | 30 | 59.1 | 5.1 | 3 |
| Varshneya et al.[75] | 2022 | USA CA | 333,054 | 62.7 | 5 | 4108 |
| Odland et al.[76] | 2011 | USA IA | 67 | 48.5 | 12.4 | 11 |
| Meding et al.[77] | 2010 | USA Indiana | 619 | 70.4 | 11.9 | 8 |
| Faris et al.[78] | 2015 | USA Indiana | 10,843 | 69.2 | 8.1 | 44 |
| Martin et al.[79] | 2016 | USA Minnesota | 28,667 | 68 | 10.1 | 1570 |
| Houdek et al.[80] | 2017 | USA Minnesota | 11,653 | 71 | 8 | 724 |
| Kremers et al.[81] | 2014 | USA MN | 16,584 | 68.8 | 9.4 | 1180 |
| Meftah et al.[82] | 2012 | USA NY | 138 | 69.2 | 10 | 3 |
| Deshmukh et al.[83] | 2016 | USA NY | 486 | 64.9 | 3.5 | 10 |
| Moussa et al.[84] | 2017 | USA NY | 439 | 71.3 | 2 | 11 |
| Dayan et al.[85] | 2020 | USA NY | 404 | 65 | 6.2 | 21 |
| Singh et al.[86] | 2023 | USA NY | 133 | 61.5 | 2.4 | 6 |
| Siljander et al.[87] | 2023 | USA NY | 282 | 65.7 | 5 | 4 |
| Yacovelli et al.[88] | 2021 | USA PA | 5970 | 66.4 | 3.6 | 26 |
| Bertin[89] | 2005 | USA UT | 251 | 69.2 | 5.9 | 3 |
| Peters et al.[90] | 2014 | USA UT | 468 | 62 | 3.5 | 28 |
| Pelt et al.[91] | 2019 | USA UT | 141 | 64 | 3 | 19 |
Clinical studies on revision rates of unicompartmental knee arthroplasty
We included twenty-six studies with 28,679 unicompartmental knee arthroplasties from 2009 to 2023 in our review, revealing 140,064.6 CY (Table 2).
Table 2.
Data of clinical studies portraying unicompartmental knee arthroplasty
| Authors | Year of publication | Country | Total UKA | Mean age (y) | Mean follow-up (y) | Revisions UKA (n) |
|---|---|---|---|---|---|---|
| Clark et al.[92] | 2010 | Australia | 398 | 63.5 | 3.6 | 15 |
| de Grave et al.[93] | 2018 | Belgium | 460 | 66 | 5.5 | 11 |
| Burnett et al.[94] | 2014 | Canada | 467 | 69.3 | 6.1 | 38 |
| Xu et al.[95] | 2017 | China | 64 | 59 | 7.2 | 6 |
| Knifsund et al.[96] | 2017 | Finland | 294 | 67 | 8.7 | 53 |
| Lustig et al.[97] | 2009 | France | 172 | 72.2 | 5.2 | 11 |
| Chatellard et al.[98] | 2013 | France | 559 | 69.5 | 5.2 | 14 |
| Sébilo et al.[99] | 2013 | France | 944 | 70 | 5.2 | 17 |
| Batailler et al.[100] | 2019 | France | 160 | 68.5 | 1.8 | 11 |
| Mergenthaler et al.[101] | 2021 | France | 391 | 66.9 | 26.3 | 29 |
| Heyse et al.[102] | 2011 | Germany | 163 | 67.5 | 4.6 | 15 |
| Heyse et al.[103] | 2012 | Germany | 223 | 53.7 | 10.8 | 15 |
| Maritan et al.[104] | 2023 | Italy | 95 | 61.2 | 7.8 | 5 |
| Woo et al.[105] | 2022 | Singapore | 242 | 61 | 10 | 15 |
| Song et al.[106] | 2016 | South Korea | 68 | 64 | 9 | 3 |
| Song et al.[107] | 2019 | South Korea | 50 | 60.8 | 12 | 11 |
| Lee et al.[108] | 2022 | South Korea | 21,194 | 60.41 | 4 | 1390 |
| Sever et al.[109] | 2019 | Turkey | 133 | 65.5 | 10.5 | 21 |
| Forster-Horváth et al.[110] | 2016 | UK | 236 | 68.2 | 7.3 | 20 |
| Chowdhry et al.[111] | 2017 | UK | 265 | 51.7 | 7.7 | 6 |
| Kennedy et al.[112] | 2018 | UK | 1,000 | 66.6 | 10 | 52 |
| Saenz et al.[113] | 2010 | USA | 144 | 72 | 3 | 16 |
| Edmiston et al.[114] | 2018 | USA IL | 65 | 61.3 | 6.9 | 4 |
| Kazarian et al.[115] | 2020 | USA Missouri | 253 | 62.9 | 3.7 | 36 |
| Berend et al.[116] | 2012 | USA OH | 132 | 68 | 3.3 | 1 |
| Hamilton et al.[117] | 2010 | USA Virginia | 507 | 66 | 3.3 | 26 |
Registers
National arthroplasty registers were accessed through the international registry network NORE (Network of Orthopedic Registries of Europe), which is a standing committee of EFORT (European Federation of National Associations of Orthopedics and Traumatology) [118]. Every register was included in their most recent presented edition. Registers had to provide data on total arthroplasty numbers (UKA and TKA), total revision numbers, sex, mean age, fixation, observed time period and covered country. Only registers who documented at least 90% of executed arthroplasties. Reports covering regional arthroplasty numbers or with insufficient data were excluded. Of 31 screened registers, a total of seven were included (Fig. 1). National arthroplasty registers from New Zealand, Sweden, Slovakia, Portugal, and Switzerland, covering different timeframes within 2003 to 2022, met the inclusion criteria and are represented in Table 3.
Table 3.
Data of national registers regarding total knee arthroplasty and unicompartmental knee arthroplasty
| Registry | Country | Total UKA | Revisions UKA | Mean Age UKA (y) | Total TKA | Revisions TKA | Mean age TKA (y) |
|---|---|---|---|---|---|---|---|
| Portuguese Arthroplasty Register May 2010[119] | Portugal | 67 | 4,018 | 291 | 68.4 | ||
| Swiss National Hip & Knee Joint Registry Report 2022[120] | Switzerland | 15,364 | 64.5 | 91,129 | 12,309 | 69.5 | |
| New Zealand Orthopaedic Association Registry [121] | New Zealand | 16,891 | 1,474 | 66.1 | 143,501 | 5,224 | 68.3 |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER – ANNUAL REPORT 2020 – PART I [122] | Sweden | 7,690 | 1,562 | 127,060 | 4,691 | ||
| Australian Orthopaedic Association National Joint Replacement Registry[123] | Australia | 70,925 | 4,813 | 65.4 | 886,536 | 26,004 | 68.4 |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER – ANNUAL REPORT 2020 – PART II[122] | Sweden | 1,820 | 152 | 14,967 | 687 | ||
| Slovak Arthroplasty Register[124] | Slovakia | 10,772 | 411 |
Outcome measures
The main aim of this review was to compare TKA and UKA revision rates amongst national registers and studies. To counterbalance different follow-up times and to make studies and registers more comparable, we calculated the revision rate and “revisions per 100 observed component years (CY)” [14, 15, 125, 126] when possible. This enables comparison of study data without the influence of follow-up times and cohort size.
Component years are calculated by mean follow-up time (in years) multiplied by the number of primary arthroplasties at the mean follow-up time. Therefore, longer mean follow-up times and larger numbers of primary arthroplasties have higher statistical power than studies with smaller groups and shorter follow-up.
In order to determine the revisions per 100 observed component years, the total number of revisions is firstly divided by the CY. Secondly, this quotient is multiplied by 100. Using this method, revision rates are made more quantifiable amongst studies and registers [14, 15, 125, 126].
Additionally, we compared revision rates in registers and mean revisions per 100 observed CY in TKA and UKA in studies, calculating the relative difference between revision rates of TKA and UKA. Correlation of revision rates and mean revisions per 100 observed CY in TKA and UKA were explored through linear regression computation.
Statistical analysis was executed using Microsoft Excel and IBM SPSS Statistics 21 (SPSS Inc., Chicago, IL).
Results
Clinical studies on survival rate of TKA
Seventy-one clinical studies published from July 2005 to September 2023 have met our inclusion criteria. In total 461,387 total knee arthroplasties and 9499 revisions were registered. Patient age was 64.2 on average. The mean follow-up time was 5.7 years revealing in 2,695,243.4 component years recorded. This exposes an average of 0.71 revisions per 100 component years and a mean revision rate of 3.35% amongst studies with a mean follow up of 5.7 years. Typical reasons for revisions were infection, stiffness, instability, trauma and septic or aseptic loosening. Full results are shown in Table 4.
Table 4.
Results of calculations regarding total knee arthroplasty in clinical studies
| Country | Total TKA | Revisions TKA (n) | Revision rate | Mean follow-up | Observed component years TKA (CY) (n) | Rev/CY x 100 (TKA) | Mean age (y) |
|---|---|---|---|---|---|---|---|
| China | 388 | 5 | 1.28865979 | 6.2556701 | 2427.2 | 0.21557271 | 66.5360825 |
| Italy | 287 | 9 | 3.1358885 | 11.5090592 | 3303.1 | 0.29003492 | 66.2703833 |
| South Korea | 8574 | 320 | 3.73221367 | 11.1874831 | 95921.48 | 0.33905449 | 64.1784784 |
| Japan | 762 | 30 | 3.93700787 | 11.6209974 | 8855.2 | 0.35238344 | 71.285958 |
| South Africa | 154 | 3 | 1.94805195 | 5 | 770 | 0.38961039 | 67.461039 |
| Belgium | 245 | 11 | 4.48979592 | 11 | 2695 | 0.40816327 | 68.1012245 |
| UK | 2959 | 96 | 3.2443393 | 5.76716233 | 17065.0333 | 0.45146634 | 67.5048665 |
| Greece | 306 | 20 | 6.53594771 | 11.9908497 | 3669.2 | 0.47048668 | 68.5189542 |
| Australia | 1553 | 18 | 1.15904701 | 7.04007298 | 10933.2333 | 0.47183476 | 74.821217 |
| Switzerland | 411 | 12 | 2.91970803 | 5.09338462 | 2093.38108 | 0.57323533 | 67 |
| France | 4654 | 119 | 2.55694027 | 4.14518908 | 19291.71 | 0.6099024 | 69.8861624 |
| The Netherlands | 2590 | 176 | 6.7953668 | 12.4312355 | 32196.9 | 0.51284711 | 66.4790734 |
| Total | 461387 | 9499 | 3.35178146 | 5.6914844 | 2695243.37 | 0.712708 | 64.1634087 |
| USA | 410410 | 7784 | 1.89663995 | 5.68569207 | 2333464.88 | 0.91112994 | 63.7858367 |
| Germany | 1272 | 44 | 3.4591195 | 3.46041667 | 4401.65 | 1.12781742 | 67.1014151 |
| Canada | 26822 | 852 | 3.17799568 | 3.41080612 | 91484.6417 | 1.32466046 | 67.1870032 |
Register data on TKA
The assessment of international register datasets resulted in seven registers originating from six countries, as shown in Table 5. Throughout 1,277,983 primary TKA and 49,617 revisions were listed. This concluded a pooled revision rate of 5.63% amongst register covering timeframes within 2003 to 2022. Sweden showcases itself with two datasets. The first one is covering the years 2009–2018 and the second one the year 2019.
Table 5.
Results of calculations featuring total knee arthroplasty in national registers
| Registry | Country | Total TKA | Revisions TKA | Proportion (Revisions TKA/total TKA) % |
|---|---|---|---|---|
| Australian Orthopaedic Association National Joint Replacement Registry | Australia | 886536 | 26004 | 2.93321422 |
| New Zealand Orthopaedic Association Registry | New Zealand | 143501 | 5224 | 3.64039275 |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER–ANNUAL REPORT 2020–PART I | Sweden | 127060 | 4691 | 3.69195656 |
| Slovakisches Arthroplasty Register | Slovakei | 10772 | 411 | 3.81544746 |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER – ANNUAL REPORT 2020–PART II | Sweden | 14967 | 687 | 4.59009822 |
| Total | 1277983 | 49617 | 5.63153491 | |
| Portuguese Arthroplasty Register May 2010 | Portugal | 4018 | 291 | 7.24240916 |
| Swiss National Hip & Knee Joint Registry Report 2022 | Switzerland | 91129 | 12309 | 13.507226 |
Clinical studies on survival rate of UKA
There were twenty-six studies covering unicompartmental knee arthroplasty from February 2009 to November 2022 that matched our inclusion criteria. Overall, 28,679 unicompartmental knee arthroplasties and 1841 revisions in patients with a mean age of 61.89 years were recorded and results were portrayed in Table 6. With a mean follow-up of 4.9 years, 140,064.6 component years were traced. Out of 100 observed component years, 1.3 revisions were registered, along with a mean revision rate of 7.67% and a mean follow up of 4.9 years. Infection, instability, bearing dislocation, malpositioning, loosening, osteoarthritis, wear pain and trauma were characteristic reasons for revision.
Table 6.
Results of calculations illustrating unicompartmental knee arthroplasty in clinical studies
| Country | Total UKA | Revisions UKA (n) | Revision rate | Mean follow-up | Observed component years UKA (CY) (n) | Rev/CY x 100 (UKA) | Mean age (y) |
|---|---|---|---|---|---|---|---|
| Belgium | 460 | 11 | 2.39130435 | 5.5 | 2530 | 0.43478261 | 66 |
| Singspore | 242 | 15 | 6.19834711 | 10 | 2420 | 0.61983471 | 61.0198473 |
| UK | 1501 | 78 | 5.19653564 | 9.17707972 | 13774.7967 | 0.65652002 | 64.220986 |
| Italy | 95 | 5 | 5.26315789 | 7.75763158 | 736.975 | 0.67844907 | 61.1715789 |
| Australia | 398 | 15 | 3.76884422 | 3.58333333 | 1426.16667 | 1.05177048 | 63.5 |
| France | 2226 | 82 | 3.68373765 | 8.63485924 | 19221.1967 | 1.22115831 | 69.3912848 |
| China | 64 | 6 | 9.375 | 7.2 | 460.8 | 1.30208333 | 59 |
| Total | 28679 | 1841 | 7.67147048 | 4.88387431 | 140064.631 | 1.30486561 | 61.8928046 |
| Germany | 386 | 30 | 7.77202073 | 8.18186528 | 3158.2 | 1.3116768 | 59.5274611 |
| South Korea | 21312 | 1404 | 6.58783784 | 4.01889255 | 85650.638 | 1.32323175 | 60.4223696 |
| Canada | 467 | 38 | 8.13704497 | 6.08333333 | 2840.91667 | 1.33759643 | 69.3 |
| Turkey | 133 | 21 | 15.7894737 | 10.5 | 1396.5 | 1.5037594 | 65.5 |
| USA | 1101 | 83 | 7.53860127 | 3.5 | 3890.64167 | 2.05154726 | 66.0346957 |
| Finland | 294 | 53 | 18.0272109 | 8.7 | 2557.8 | 2.07209321 | 67 |
Register data on UKA
Data concerning UKA was illustrated in four registers, two originating from Sweden (2009–2018 and 2019). Throughout 97,326 unicompartmental knee arthroplasties and 8001 revision surgeries were recorded. This is resulting in a pooled revision rate of 11.04% amongst registers covering periods within 2003–2022 (Table 7).
Table 7.
Results of calculations depicting unicompartmental knee arthroplasty in national registers
| Registry | Country | Total UKA | Revisions UKA | Proportion (Revisions UKA/total UKA) % |
|---|---|---|---|---|
| Australian Orthopaedic Association National Joint Replacement Registry | Australia | 70925 | 4813 | 6.78604159 |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER–ANNUAL REPORT 2020–PART II | Sweden | 1820 | 152 | 8.35164835 |
| New Zealand Orthopaedic Association Registry | New Zealand | 16891 | 1474 | 8.72654076 |
| Total | 97326 | 8001 | 11.0440811 | |
| THE SWEDISH KNEE ARTHROPLASTY REGISTER–ANNUAL REPORT 2020–PART I | Sweden | 7690 | 1562 | 20.3120936 |
TKA and UKA revision rates in studies
Sufficient study data on revision rates for TKA and UKA were documented for ten nations. When looking at TKA, we recorded 2,580,987.9 observed component years, with a mean revision rate of 6.15 revisions per 100 CY at a mean age of 67.5 years. With 133,690 observed component years UKA showed a mean revision rate of 1.14 revisions per 100 CY at a mean patient age of 63.9. As a result, there were on average 2.29 times higher revision rates and 1.85 times more revisions per 100 CY in the UKA cohorts than in the TKA cohorts, with similar divergence between countries.
A positive correlation of pooled revision rates of TKA with UKA in studies was found. Considering a broad array of data was used, with varying numbers of studies depicting region specific revision rates, a coefficient of determination of R2 = 0.2405 is indicating linear correlation (Fig. 2).
Fig. 2.

Chart of linear regression of revision rate/component years × 100 of total knee arthroplasty and unicompartmental knee arthroplasty in clinical studies by countries
TKA and UKA revision rates in registers
There were solely four registers reporting on TKA and UKA at the same time, with Sweden being represented twice (2009–2018 and 2019). While the mean revision rate for TKA was at 3.71%, the mean revision rate for UKA was at 8.73%, being 2.38 times as high and showing similar variation amongst countries.
Only four registers reporting on three countries provided data for both, TKA and UKA, resulting in a low coefficient of determination of R2 = 0.0043. Nevertheless, considering the large number of cases featured in arthroplasty registers, a positive correlation of TKA and UKA revision rates could be found (Fig. 3).
Fig. 3.
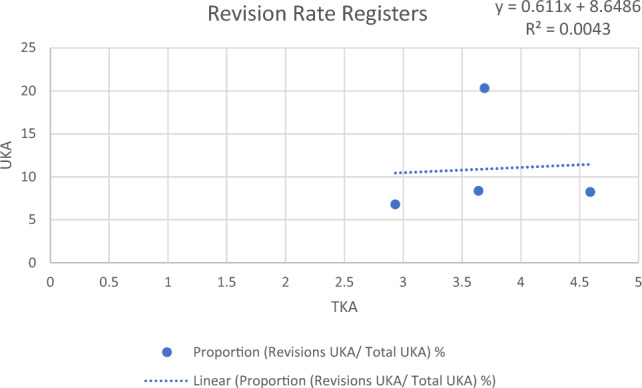
Chart of linear regression of revision rates of total knee arthroplasty and unicompartmental knee arthroplasty in national arthroplasty registers
Discussion
The most important finding of this study was a positive correlation of revision rates of TKA and UKA in different regions in registers and studies, affirming our hypothesis. Studies dealing with UKA revealed 2.29 times higher revision rates in comparison to TKA. Register data continue this trend by presenting 1.96 times higher revision rates for UKA than for TKA.
Mean revision rates in registers (5.63% TKA, 11.04% UKA) were about 1.56 times as high as pooled revision rates described in studies (TKA: 3.35% and 0.71/100CY; UKA: 7.67% and 1.3/100CY UKA). On that note a certain degree of comparability is given. This correlation could be registered in a few countries represented in studies and registers such as TKA in Switzerland, where revision rate in registers was 5.63% and studies showed 2.92% (0.57 rev/100CY). Same relation was observed in revision numbers of UKA in Australia (registers 6.79% vs. studies 3.77% & 1.05 rev/100CY). However, revision rates of TKA in Australia showed divergent behaviour (registers 13.51% vs. studies 1.16% & 0.57 rev/100CY).
Registers represent the national average values, while studies record smaller cohorts limited to one or more defined centers. High volume centers and surgeons, who specialise in these procedures show significantly lower revision rates than low volume surgeons and centers [127]. With higher volume surgeons and centers publishing more papers, lower revision rates as described in studies appear comprehensible.
Apart from center and surgeon volume, surgeon experience and more recent investigations also had great influence on the reported revision rate. The Swedish Arthroplasty Register Part II covering solely the year 2019 is showing values near the pooled revision rate for TKA and UKA, while Part I of the Swedish Arthroplasty Register dealing with the years 2009–2018 is reporting much higher revision rates for UKA.
Higher revision rates for UKA don’t necessarily depict bad function or worse outcomes than TKA. Orthopaedic surgeons experiencing some sort of complications after UKA implantation tend to show lower threshold for revision of aseptic UKA than TKA. The reason for this is suspected in TKA being the revision for UKA and surgeons having more experience in the implantation of TKA in respect to UKA [128–130]. Revision of UKA through TKA show satisfying results, although is accompanied by greater bone loss, more augments and thicker polyethylene components, while providing similar revision rates, complications and hospital stay than primary TKA [131]. UKA being revised using another UKA is rarely performed. Finally, revision threshold for UKA is significantly lower than for TKA [129].
Study patients receiving TKA show a mean age of 64.2 years and an average of 5.7 years of follow up. Participants in papers representing UKA display lower age (61.9 years) with shorter follow-up time (4.9 years). Registers show a similar trend for mean patient age, with UKA patients being younger.
Some limitations need to be noted. This analysis includes a great amount of study and register data, whereby a vast array of cases is covered. Unfortunately, many data sets are incomplete, preventing inclusion in studies of any kind to some extent. This is resulting in studies and national register that cannot be included in studies because of a lack of information, showing that quality of meta-analysis is dependent on the quality of data presented. Additional limitation was poor accessibility, indistinct display of information and foreign language of registers, lowering reproducibility and impeding analysis. Furthermore, since no patient-reported outcome measures were listed, no quality of clinical outcome of UKA or TKA can be demonstrated.
In order to provide comparability and reproducibility, more nations should conduct accessible arthroplasty registers supplying sufficient data in English language. In succession, future studies on revision rates could be compared to international registry data, making it easier to elaborate differences and promoting research on knee arthroplasty.
Conclusion
A positive correlation of revision rates of TKA and UKA in studies and registers was found. Revision rates of UKA comparted to TKA were 2.29 times higher in clinical studies and 1.96 times higher in registers. Revision rates in registers were about 1.56 times higher than presented in clinical studies.
Funding
Open access funding provided by Medical University of Graz.
Data availability
Additional data is available on request.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A et al (2018) Knee replacement. Lancet Lond Engl 392:1672–1682. 10.1016/S0140-6736(18)32344-4 [DOI] [PubMed] [Google Scholar]
- 2.Gademan MGJ, Hofstede SN, Vliet Vlieland TP, Nelissen RGH, van de Marang MPJ (2016) Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskelet Disord 17:463. 10.1186/s12891-016-1325-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Streck LE, Hanreich C, Cororaton AD, Boettner CS, Boettner F (2023) Does high activity after total and unicompartmental knee arthroplasty increase the risk for aseptic revision? Arch Orthop Trauma Surg 143:5843–5848. 10.1007/s00402-023-04794-1 [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Jordan JM (2010) Epidemiology of osteoarthritis. Clin Geriatr Med 26:355–369. 10.1016/j.cger.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray DW, Parkinson RW (2018) Usage of unicompartmental knee arthroplasty. Bone Jt J 100:432–435. 10.1302/0301-620X.100B4.BJJ-2017-0716.R1 [DOI] [PubMed] [Google Scholar]
- 6.D’Ambrosi R, Ursino C, Mariani I, Ursino N, Formica M, Chen AF (2023) Clinical outcomes, complications, and survivorship for unicompartmental knee arthroplasty versus total knee arthroplasty in patients aged 80 years and older with isolated medial knee osteoarthritis: a matched cohort analysis. Arch Orthop Trauma Surg 143:6371–6379. 10.1007/s00402-023-04916-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liddle AD, Pandit H, Judge A, Murray DW (2015) Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Jt J 97:1506–1511. 10.1302/0301-620X.97B11.35551 [DOI] [PubMed] [Google Scholar]
- 8.Postler A, Lützner C, Beyer F, Tille E, Lützner J (2018) Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 19:55. 10.1186/s12891-018-1977-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gehrke T, Alijanipour P, Parvizi J (2015) The management of an infected total knee arthroplasty. Bone Jt J 97:20–29. 10.1302/0301-620X.97B10.36475 [DOI] [PubMed] [Google Scholar]
- 10.Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA (2017) Current Epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 32:2663–2668. 10.1016/j.arth.2017.03.066 [DOI] [PubMed] [Google Scholar]
- 11.Tarazi JM, Chen Z, Scuderi GR, Mont MA (2021) The epidemiology of revision total knee arthroplasty. J Knee Surg 34:1396–1401. 10.1055/s-0041-1735282 [DOI] [PubMed] [Google Scholar]
- 12.Salman LA, Abudalou A, Khatkar H, Ahmed G, Dakin SG, Kendrick B et al (2023) Impact of age on unicompartmental knee arthroplasty outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 31:986–997. 10.1007/s00167-022-07132-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee J, Tay ML, Frampton CM, Young SW (2024) Clinical and functional outcomes of TKA after HTO or UKA: a New Zealand joint registry study. Arch Orthop Trauma Surg. 10.1007/s00402-024-05302-9 [DOI] [PubMed] [Google Scholar]
- 14.Hauer G, Vielgut I, Amerstorfer F, Maurer-Ertl W, Leithner A, Sadoghi P (2018) Survival rate of short-stem hip prostheses: a comparative analysis of clinical studies and national arthroplasty registers. J Arthroplasty 33:1800–1805. 10.1016/j.arth.2018.01.017 [DOI] [PubMed] [Google Scholar]
- 15.Hauer G, Heri A, Klim S, Puchwein P, Leithner A, Sadoghi P (2020) Survival rate and application number of total hip arthroplasty in patients with femoral neck fracture: an analysis of clinical studies and national arthroplasty registers. J Arthroplasty 35:1014–1022. 10.1016/j.arth.2019.11.033 [DOI] [PubMed] [Google Scholar]
- 16.Altman DG (2001) Systematic reviews of evaluations of prognostic variables. BMJ 323:224–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D et al (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134:663–694. 10.7326/0003-4819-134-8-200104170-00012 [DOI] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 2021:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.OCEBM Levels of Evidence n.d. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed Aug 15 2024
- 20.Katchky AM, Jones CW, Walter WL, Shimmin AJ (2019) Medial ball and socket total knee arthroplasty: five-year clinical results. Bone Jt J 101:59–65. 10.1302/0301-620X.101B1.BJJ-2018-0434.R1 [DOI] [PubMed] [Google Scholar]
- 21.Klasan A, Putnis SE, Yeo WW, Fritsch BA, Coolican MR, Parker DA (2019) Advanced age is not a barrier to total knee arthroplasty: a detailed analysis of outcomes and complications in an elderly cohort compared with average age total knee arthroplasty patients. J Arthroplasty 34:1938–1945. 10.1016/j.arth.2019.05.007 [DOI] [PubMed] [Google Scholar]
- 22.Hazratwala K, Gouk C, Wilkinson MPR, O’Callaghan WB (2023) Navigated functional alignment total knee arthroplasty achieves reliable, reproducible and accurate results with high patient satisfaction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 31:3861–3870. 10.1007/s00167-023-07327-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Victor J, Ghijselings S, Tajdar F, Van Damme G, Deprez P, Arnout N et al (2014) Total knee arthroplasty at 15–17 years: does implant design affect outcome? Int Orthop 38:235–241. 10.1007/s00264-013-2231-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beaupré LA, Al-Yamani M, Huckell JR, Johnston DWC (2007) Hydroxyapatite-coated tibial implants compared with cemented tibial fixation in primary total knee arthroplasty. A randomized trial of outcomes at five years. J Bone Joint Surg Am 89:2204–2211. 10.2106/JBJS.F.01431 [DOI] [PubMed] [Google Scholar]
- 25.MacDonald SJ, Charron KD, Bourne RB, Naudie DD, McCalden RW, Rorabeck CH (2008) The John insall award: gender-specific total knee replacement: prospectively collected clinical outcomes. Clin Orthop 466:2612–2616. 10.1007/s11999-008-0430-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaudhary R, Beaupré LA, Johnston DWC (2008) Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am 90:2579–2586. 10.2106/JBJS.G.00995 [DOI] [PubMed] [Google Scholar]
- 27.Sando T, McCalden RW, Bourne RB, MacDonald SJ, Somerville LE (2015) Ten-year results comparing posterior cruciate-retaining versus posterior cruciate-substituting total knee arthroplasty. J Arthroplasty 30:210–215. 10.1016/j.arth.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 28.Rhee C, Lethbridge L, Richardson G, Dunbar M (2018) Risk factors for infection, revision, death, blood transfusion and longer hospital stay 3 months and 1 year after primary total hip or knee arthroplasty. Can J Surg J Can Chir 61:165–176. 10.1503/cjs.007117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Demcoe AR, Bohm ER, Hedden DR, Burnell CD, Turgeon TR (2019) Does oxidized zirconium make a difference? Midterm cohort survivorship of symmetric posterior condyle posterior-stabilized total knee arthroplasty. Can J Surg J Can Chir 62:118–122. 10.1503/cjs.007518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khoshbin A, Stavrakis A, Sharma A, Woo P, Atrey A, Lee Y-YL et al (2019) Patient-reported outcome measures of total knee arthroplasties for post-traumatic arthritis versus osteoarthritis: a short-term (5- to 10-year) retrospective matched cohort study. J Arthroplasty 34:872-876.e1. 10.1016/j.arth.2019.01.022 [DOI] [PubMed] [Google Scholar]
- 31.Teeter MG, Marsh JD, Howard JL, Yuan X, Vasarhelyi EM, McCalden RW et al (2019) A randomized controlled trial investigating the value of patient-specific instrumentation for total knee arthroplasty in the Canadian healthcare system. Bone Jt J 101:565–572. 10.1302/0301-620X.101B5.BJJ-2018-1323.R1 [DOI] [PubMed] [Google Scholar]
- 32.Garceau SP, Warschawski YS, Tang A, Sanders EB, Schwarzkopf RM, Backstein DJ (2020) The effect of polyethylene liner thickness on patient outcomes and failure after primary total knee arthroplasty. J Arthroplasty 35:2072–2075. 10.1016/j.arth.2020.03.017 [DOI] [PubMed] [Google Scholar]
- 33.Shen B, Yang J, Zhou Z, Kang P, Wang L, Pei F (2009) Survivorship comparison of all-polyethylene and metal-backed tibial components in cruciate-substituting total knee arthroplasty–Chinese experience. Int Orthop 33:1243–1247. 10.1007/s00264-008-0634-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo Z, Zhou K, Wang H, Pei F, Zhou Z (2022) Comparison between mid-term results of total knee arthroplasty with single-radius versus multiple-radii posterior-stabilized prostheses. J Knee Surg 35:204–214. 10.1055/s-0040-1713897 [DOI] [PubMed] [Google Scholar]
- 35.Wang W, Xiang S, Wang Y, Lv C, Wang C, Zhang H (2022) Evaluation of double-high insert mid-term outcomes in cruciate-retaining medial-pivotal total knee arthroplasty—a propensity score-matched analysis with averaged 8-year follow-up. BMC Musculoskelet Disord 23:571. 10.1186/s12891-022-05484-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaillard R, Lustig S, Peltier A, Villa V, Servien E, Neyret P (2016) Total knee implant posterior stabilised by a third condyle: design evolution and post-operative complications. Orthop Traumatol Surg Res OTSR 102:1061–1068. 10.1016/j.otsr.2016.08.015 [DOI] [PubMed] [Google Scholar]
- 37.Putman S, Argenson J-N, Bonnevialle P, Ehlinger M, Vie P, Leclercq S et al (2018) Ten-year survival and complications of total knee arthroplasty for osteoarthritis secondary to trauma or surgery: a French multicentre study of 263 patients. Orthop Traumatol Surg Res OTSR 104:161–164. 10.1016/j.otsr.2017.11.019 [DOI] [PubMed] [Google Scholar]
- 38.Erivan R, Fadlallah E, Villatte G, Mulliez A, Descamps S, Boisgard S (2019) Fifteen-year survival of the Cedior™ total knee prosthesis. Eur J Orthop Surg Traumatol Orthop Traumatol 29:1709–1717. 10.1007/s00590-019-02491-7 [DOI] [PubMed] [Google Scholar]
- 39.Schnurr C, Güdden I, Eysel P, König DP (2012) Influence of computer navigation on TKA revision rates. Int Orthop 36:2255–2260. 10.1007/s00264-012-1606-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hotfiel T, Carl H-D, Eibenberger T, Gelse K, Weiß J, Jendrissek A et al (2017) Cementless femoral components in bicondylar hybrid knee arthroplasty in patients with rheumatoid arthritis: a 10-year survivorship analysis. J Orthop Surg Hong Kong 25:2309499017716252. 10.1177/2309499017716252 [DOI] [PubMed] [Google Scholar]
- 41.Fuchs M, Effenberger B, Märdian S, Berner A, Kirschbaum S, Pumberger M et al (2018) Mid-term survival of total knee arthroplasty in patients with posttraumatic osteoarthritis. Acta Chir Orthop Traumatol Cech 85:319–324 [PubMed] [Google Scholar]
- 42.Iosifidis M, Iliopoulos E, Neofytou D, Sakorafas N, Andreou D, Alvanos D et al (2014) The Rotaglide mobile-bearing total knee arthroplasty: no difference between cemented and hybrid implantation. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 22:1843–1848. 10.1007/s00167-013-2829-9 [DOI] [PubMed] [Google Scholar]
- 43.Bouras T, Bitas V, Fennema P, Korovessis P (2017) Good long-term results following cementless TKA with a titanium plasma coating. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 25:2801–2808. 10.1007/s00167-015-3769-3 [DOI] [PubMed] [Google Scholar]
- 44.Innocenti M, Matassi F, Carulli C, Nistri L, Civinini R (2014) Oxidized zirconium femoral component for TKA: a follow-up note of a previous report at a minimum of 10 years. Knee 21:858–861. 10.1016/j.knee.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 45.Rossi SMP, Perticarini L, Mosconi M, Ghiara M, Benazzo F (2020) Ten-year outcomes of a nitrided Ti-6Al-4V titanium alloy fixed-bearing total knee replacement with a highly crosslinked polyethylene-bearing in patients with metal allergy. Knee 27:1519–1524. 10.1016/j.knee.2020.08.007 [DOI] [PubMed] [Google Scholar]
- 46.Giustra F, Bistolfi A, Bosco F, Fresia N, Sabatini L, Berchialla P et al (2023) Highly cross-linked polyethylene versus conventional polyethylene in primary total knee arthroplasty: comparable clinical and radiological results at a 10-year follow-up. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 31:1082–1088. 10.1007/s00167-022-07226-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakamura S, Ito H, Kobayashi M, Nakamura K, Toyoji U, Komistek RD et al (2014) Are the long term results of a high-flex total knee replacement affected by the range of flexion? Int Orthop 38:761–766. 10.1007/s00264-013-2179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ueyama H, Kanemoto N, Minoda Y, Yamamoto N, Taniguchi Y, Nakamura H (2020) Long-term clinical outcomes of medial pivot total knee arthroplasty for Asian patients: a mean 10-year follow-up study. Knee 27:1778–1786. 10.1016/j.knee.2020.09.009 [DOI] [PubMed] [Google Scholar]
- 49.Schepers A, Cullingworth L, van der Jagt DR (2012) A prospective randomized clinical trial comparing tibial baseplate fixation with or without screws in total knee arthroplasty: a radiographic evaluation. J Arthroplasty 27:454–460. 10.1016/j.arth.2011.04.001 [DOI] [PubMed] [Google Scholar]
- 50.Bae DK, Song SJ, Park MJ, Eoh JH, Song JH, Park CH (2012) Twenty-year survival analysis in total knee arthroplasty by a single surgeon. J Arthroplasty 27:1297-1304.e1. 10.1016/j.arth.2011.10.027 [DOI] [PubMed] [Google Scholar]
- 51.Lee D-H, Lee D-K, Shin Y-S, Han S-B (2013) Mid-term outcomes of floating platform mobile-bearing total knee arthroplasty under navigational guidance with a minimum 4-year follow-up. J Arthroplasty 28:1801–1805. 10.1016/j.arth.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 52.Kim Y-H, Park J-W, Kim J-S, Kulkarni SS, Kim Y-H (2014) Long-term clinical outcomes and survivorship of press-fit condylar sigma fixed-bearing and mobile-bearing total knee prostheses in the same patients. J Bone Joint Surg Am 96:e168. 10.2106/JBJS.M.01130 [DOI] [PubMed] [Google Scholar]
- 53.Kim Y-H, Park J-W, Kim J-S (2016) A comparison of 5 models of total knee arthroplasty in young patients. J Arthroplasty 31:994–999. 10.1016/j.arth.2015.11.015 [DOI] [PubMed] [Google Scholar]
- 54.Yang HY, Seon JK, Shin YJ, Lim HA, Song EK (2017) Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg 9:169–176. 10.4055/cios.2017.9.2.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim Y-H, Park J-W, Kim J-S (2017) Clinical outcome of medial pivot compared with press-fit condylar sigma cruciate-retaining mobile-bearing total knee arthroplasty. J Arthroplasty 32:3016–3023. 10.1016/j.arth.2017.05.022 [DOI] [PubMed] [Google Scholar]
- 56.Park J-K, Seon J-K, Cho K-J, Lee N-H, Song E-K (2018) Is immediate postoperative mechanical axis associated with the revision rate of primary total knee arthroplasty? A 10-year follow-up study. Clin Orthop Surg 10:167–173. 10.4055/cios.2018.10.2.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oh S-M, Bin S-I, Kim J-Y, Cho H-I, Lee B-S, Kim J-M (2018) Does the preoperative varus deformity influence the survival of postoperative neutral-aligned TKAs? An analysis with a minimum 5-year follow-up. J Arthroplasty 33:3181–3185. 10.1016/j.arth.2018.06.001 [DOI] [PubMed] [Google Scholar]
- 58.Kim Y-H, Park J-W, Jang Y-S (2021) 20-year minimum outcomes and survival rate of high-flexion versus standard total knee arthroplasty. J Arthroplasty 36:560–565. 10.1016/j.arth.2020.07.084 [DOI] [PubMed] [Google Scholar]
- 59.Kim G-W, Jin QH, Lim J-H, Song E-K, Seon J-K (2021) No difference of survival between cruciate retaining and substitution designs in high flexion total knee arthroplasty. Sci Rep 11:6537. 10.1038/s41598-021-85892-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baek J-H, Lee SC, Choi K, Ahn HS, Nam CH (2021) Long-term survivorship of total knee arthroplasty with a single-radius, high-flexion posterior stabilized prosthesis. Knee 30:275–282. 10.1016/j.knee.2021.04.017 [DOI] [PubMed] [Google Scholar]
- 61.Baek J-H, Lee SC, Kim J-W, Ahn HS, Nam CH (2022) Inferior outcomes of primary total knee arthroplasty in patients with rheumatoid arthritis compared to patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 30:2786–2792. 10.1007/s00167-021-06675-9 [DOI] [PubMed] [Google Scholar]
- 62.Lee YM, Kim GW, Lee CY, Song E-K, Seon J-K (2023) No difference in clinical outcomes and survivorship for robotic, navigational, and conventional primary total knee arthroplasty with a minimum follow-up of 10 years. Clin Orthop Surg 15:82–91. 10.4055/cios21138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Munzinger UK, Maffiuletti NA, Guggi T, Bizzini M, Preiss S, Drobny T (2010) Five-year results of the Innex total knee arthroplasty system. Int Orthop 34:1159–1165. 10.1007/s00264-009-0887-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nouta K-A, Pijls BG, Nelissen RGHH (2012) All-polyethylene tibial components in TKA in rheumatoid arthritis: a 25-year follow-up study. Int Orthop 36:565–570. 10.1007/s00264-011-1341-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kievit AJ, Schafroth MU, Blankevoort L, Sierevelt IN, van Dijk CN, van Geenen RCI (2014) Early experience with the Vanguard complete total knee system: 2–7 years of follow-up and risk factors for revision. J Arthroplasty 29:348–354. 10.1016/j.arth.2013.05.018 [DOI] [PubMed] [Google Scholar]
- 66.Willems JH, Rassir R, Sierevelt IN, Nolte PA (2020) There is no difference in postoperative pain, function and complications in patients with chondrocalcinosis in the outcome of total knee arthroplasty for end-stage osteoarthritis. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 28:2970–2979. 10.1007/s00167-019-05725-7 [DOI] [PubMed] [Google Scholar]
- 67.van Ooij B, de Keijzer DR, Hoornenborg D, Sierevelt IN, Haverkamp D (2022) Lower revision rates for cemented fixation in a long-term survival analysis of three different LCS designs. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 30:2707–2713. 10.1007/s00167-021-06587-8 [DOI] [PubMed] [Google Scholar]
- 68.Clayton RAE, Amin AK, Gaston MS, Brenkel IJ (2006) Five-year results of the Sigma total knee arthroplasty. Knee 13:359–364. 10.1016/j.knee.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 69.Keenan O, Brenkel I, Walmsley P (2019) Ten-year results of the press fit condylar sigma cobalt-chrome total knee replacement. J Knee Surg 32:222–226. 10.1055/s-0038-1641138 [DOI] [PubMed] [Google Scholar]
- 70.Clark AN, Hounat A, O’Donnell S, May P, Doonan J, Rowe P et al (2021) Electromagnetic navigated versus conventional total knee arthroplasty-a five-year follow-up of a single-blind randomized control trial. J Arthroplasty 36:3451–3455. 10.1016/j.arth.2021.06.007 [DOI] [PubMed] [Google Scholar]
- 71.Brown M, Ramasubbu R, Jenkinson M, Doonan J, Blyth M, Jones B (2021) Significant differences in rates of aseptic loosening between two variations of a popular total knee arthroplasty design. Int Orthop 45:2859–2867. 10.1007/s00264-021-05151-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Farhan-Alanie OM, Altell T, O’Donnell S, May P, Doonan J, Rowe P et al (2023) No advantage with navigated versus conventional mechanically aligned total knee arthroplasty-10 year results of a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 31:751–759. 10.1007/s00167-022-07158-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boettner F, Renner L, Arana Narbarte D, Egidy C, Faschingbauer M (2016) Total knee arthroplasty for valgus osteoarthritis: the results of a standardized soft-tissue release technique. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:2525–2531. 10.1007/s00167-016-4054-9 [DOI] [PubMed] [Google Scholar]
- 74.Chan JY, Giori NJ (2017) Uncemented metal-backed tantalum patellar components in total knee arthroplasty have a high fracture rate at midterm follow-up. J Arthroplasty 32:2427–2430. 10.1016/j.arth.2017.02.062 [DOI] [PubMed] [Google Scholar]
- 75.Varshneya K, Hong CS, Tyagi V, Ruberte Thiele RA, Huddleston JI (2022) Imageless computer navigation reduces 5-year all-cause revision rates after primary total knee arthroplasty. J Arthroplasty 37:S211–S215. 10.1016/j.arth.2022.02.004 [DOI] [PubMed] [Google Scholar]
- 76.Odland AN, Callaghan JJ, Liu SS, Wells CW (2011) Wear and lysis is the problem in modular TKA in the young OA patient at 10 years. Clin Orthop 469:41–47. 10.1007/s11999-010-1429-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Meding JB, Wing JT, Ritter MA (2010) Total knee arthroplasty with 4.4 mm of tibial polyethylene an update. J Arthroplasty 25:772–774. 10.1016/j.arth.2009.05.026 [DOI] [PubMed] [Google Scholar]
- 78.Faris PM, Ritter MA, Davis KE, Priscu HM (2015) Ten-year outcome comparison of the anatomical graduated component and vanguard total knee arthroplasty systems. J Arthroplasty 30:1733–1735. 10.1016/j.arth.2015.04.042 [DOI] [PubMed] [Google Scholar]
- 79.Martin JR, Beahrs TR, Stuhlman CR, Trousdale RT (2016) Complex primary total knee arthroplasty: long-term outcomes. J Bone Joint Surg Am 98:1459–1470. 10.2106/JBJS.15.01173 [DOI] [PubMed] [Google Scholar]
- 80.Houdek MT, Watts CD, Wyles CC, Martin JR, Trousdale RT, Taunton MJ (2017) Metal or modularity: why do metal-backed tibias have inferior outcomes to all-polyethylene tibial components in patients with osteoarthritis. J Arthroplasty 32:836–842. 10.1016/j.arth.2016.09.036 [DOI] [PubMed] [Google Scholar]
- 81.Kremers HM, Sierra RJ, Schleck CD, Berry DJ, Cabanela ME, Hanssen AD et al (2014) Comparative survivorship of different tibial designs in primary total knee arthroplasty. J Bone Joint Surg Am 96:e121. 10.2106/JBJS.M.00820 [DOI] [PubMed] [Google Scholar]
- 82.Meftah M, Ranawat AS, Ranawat CS (2012) Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg Am 94:426–432. 10.2106/JBJS.K.00152 [DOI] [PubMed] [Google Scholar]
- 83.Deshmukh AJ, Rathod PA, Moses MJ, Snir N, Marwin SE, Dayan AJ (2016) Does a non-stemmed constrained condylar prosthesis predispose to early failure of primary total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3194–3199. 10.1007/s00167-014-3494-3 [DOI] [PubMed] [Google Scholar]
- 84.Moussa ME, Lee Y-Y, Patel AR, Westrich GH (2017) Clinical outcomes following the use of constrained condylar knees in primary total knee arthroplasty. J Arthroplasty 32:1869–1873. 10.1016/j.arth.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 85.Dayan I, Moses MJ, Rathod P, Deshmukh A, Marwin S, Dayan AJ (2020) No difference in failure rates or clinical outcomes between non-stemmed constrained condylar prostheses and posterior-stabilized prostheses for primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 28:2942–2947. 10.1007/s00167-019-05684-z [DOI] [PubMed] [Google Scholar]
- 86.Singh V, Yeroushalmi D, Christensen TH, Bieganowski T, Tang A, Schwarzkopf R (2023) Early outcomes of a novel bicruciate-retaining knee system: a 2-year minimum retrospective cohort study. Arch Orthop Trauma Surg 143:503–509. 10.1007/s00402-022-04351-2 [DOI] [PubMed] [Google Scholar]
- 87.Siljander BR, Chandi SK, Debbi EM, McLawhorn AS, Sculco PK, Chalmers BP (2023) A comparison of clinical outcomes after total knee arthroplasty in patients with preoperative nickel allergy receiving cobalt chromium or nickel-free implant. J Arthroplasty 38:S194–S198. 10.1016/j.arth.2023.04.048 [DOI] [PubMed] [Google Scholar]
- 88.Yacovelli S, Grau LC, Hozack WJ, Courtney PM (2021) Functional outcomes are comparable between posterior stabilized and cruciate-substituting total knee arthroplasty designs at short-term follow-up. J Arthroplasty 36:986–990. 10.1016/j.arth.2020.09.008 [DOI] [PubMed] [Google Scholar]
- 89.Bertin KC (2005) Cruciate-retaining total knee arthroplasty at 5–7 years followup. Clin Orthop. 10.1097/01.blo.0000160381.23052.34 [DOI] [PubMed] [Google Scholar]
- 90.Peters CL, Mulkey P, Erickson J, Anderson MB, Pelt CE (2014) Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop 472:175–180. 10.1007/s11999-013-3068-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pelt CE, Sandifer PA, Gililland JM, Anderson MB, Peters CL (2019) Mean three-year survivorship of a new bicruciate-retaining total knee arthroplasty: are revisions still higher than expected? J Arthroplasty 34:1957–1962. 10.1016/j.arth.2019.04.030 [DOI] [PubMed] [Google Scholar]
- 92.Clark M, Campbell DG, Kiss G, Dobson PJ, Lewis PL (2010) Reintervention after mobile-bearing Oxford unicompartmental knee arthroplasty. Clin Orthop 468:576–580. 10.1007/s11999-009-1089-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Winnock de Grave P, Barbier J, Luyckx T, Ryckaert A, Gunst P, van den Daelen L (2018) Outcomes of a fixed-bearing, medial, cemented unicondylar knee arthroplasty design: survival analysis and functional score of 460 cases. J Arthroplasty 33:2792–2799. 10.1016/j.arth.2018.04.031 [DOI] [PubMed] [Google Scholar]
- 94.Burnett RSJ, Nair R, Hall CA, Jacks DA, Pugh L, McAllister MM (2014) Results of the Oxford Phase 3 mobile bearing medial unicompartmental knee arthroplasty from an independent center: 467 knees at a mean 6-year follow-up: analysis of predictors of failure. J Arthroplasty 29:193–200. 10.1016/j.arth.2014.01.035 [DOI] [PubMed] [Google Scholar]
- 95.Xu T, Lao Y, Wang J, Liu F, Xiao L, Tong P (2017) Mid-term results of Oxford phase-3 medial unicompartmental knee arthroplasty for medial arthritis in Chinese patients. ANZ J Surg 87:287–290. 10.1111/ans.13764 [DOI] [PubMed] [Google Scholar]
- 96.Knifsund J, Hatakka J, Keemu H, Mäkelä K, Koivisto M, Niinimäki T (2017) Unicompartmental knee arthroplasties are performed on the patients with radiologically too mild osteoarthritis. Scand J Surg SJS Off Organ Finn Surg Soc Scand Surg Soc 106:338–341. 10.1177/1457496917701668 [DOI] [PubMed] [Google Scholar]
- 97.Lustig S, Paillot J-L, Servien E, Henry J, Ait Si Selmi T, Neyret P (2009) Cemented all polyethylene tibial insert unicompartimental knee arthroplasty: a long term follow-up study. Orthop Traumatol Surg Res OTSR 95:12–21. 10.1016/j.otsr.2008.04.001 [DOI] [PubMed] [Google Scholar]
- 98.Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J et al (2013) Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res OTSR 99:S219-225. 10.1016/j.otsr.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 99.Sébilo A, Casin C, Lebel B, Rouvillain J-L, Chapuis S, Bonnevialle P et al (2013) Clinical and technical factors influencing outcomes of unicompartmental knee arthroplasty: retrospective multicentre study of 944 knees. Orthop Traumatol Surg Res OTSR 99:S227-234. 10.1016/j.otsr.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 100.Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S (2019) Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 27:1232–1240. 10.1007/s00167-018-5081-5 [DOI] [PubMed] [Google Scholar]
- 101.Mergenthaler G, Batailler C, Lording T, Servien E, Lustig S (2021) Is robotic-assisted unicompartmental knee arthroplasty a safe procedure? A case control study. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 29:931–938. 10.1007/s00167-020-06051-z [DOI] [PubMed] [Google Scholar]
- 102.Heyse TJ, Efe T, Rumpf S, Schofer MD, Fuchs-Winkelmann S, Schmitt J et al (2011) Minimally invasive versus conventional unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 131:1287–1290. 10.1007/s00402-011-1274-9 [DOI] [PubMed] [Google Scholar]
- 103.Heyse TJ, Khefacha A, Peersman G, Cartier P (2012) Survivorship of UKA in the middle-aged. Knee 19:585–591. 10.1016/j.knee.2011.09.002 [DOI] [PubMed] [Google Scholar]
- 104.Maritan G, Franceschi G, Nardacchione R, Furlan E, Mariani I, Ursino N et al (2023) Similar survivorship at the 5-year follow-up comparing robotic-assisted and conventional lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 31:1063–1071. 10.1007/s00167-022-07218-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Woo BJ, Liow MHL, Lo NN, Yeo SJ, Chen JY (2022) No differences in 10-year clinical outcomes and quality of life between patients with different mediolateral femoral component positions in fixed-bearing medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 30:3176–3183. 10.1007/s00167-021-06620-w [DOI] [PubMed] [Google Scholar]
- 106.Song EK, Mohite N, Lee S-H, Na B-R, Seon J-K (2016) Comparison of outcome and survival after unicompartmental knee arthroplasty between navigation and conventional techniques with an average 9-year follow-up. J Arthroplasty 31:395–400. 10.1016/j.arth.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 107.Song SJ, Bae DK, Kim KI, Park CH (2019) Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 27:1310–1319. 10.1007/s00167-019-05390-w [DOI] [PubMed] [Google Scholar]
- 108.Lee S-H, Kim H-R, Seo H-Y, Seon J-K (2022) A comparative study of 21,194 UKAs and 49,270 HTOs for the risk of unanticipated events in mid-age patients from the national claims data in South Korea. BMC Musculoskelet Disord 23:127. 10.1186/s12891-022-05080-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sever GB, Cankuş C (2019) The long-term results of cemented Oxford unicompartmental knee arthroplasty: a single-center experience. Eklem Hast Ve Cerrahisi Jt Dis Relat Surg 30:233–240. 10.5606/ehc.2019.66429 [DOI] [PubMed] [Google Scholar]
- 110.Forster-Horváth C, Artz N, Hassaballa MA, Robinson JR, Porteous AJ, Murray JR et al (2016) Survivorship and clinical outcome of the minimally invasive Uniglide medial fixed bearing, all-polyethylene tibia, unicompartmental knee arthroplasty at a mean follow-up of 7.3years. Knee 23:981–986. 10.1016/j.knee.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 111.Chowdhry M, Khakha RS, Norris M, Kheiran A, Chauhan SK (2017) Improved survival of computer-assisted unicompartmental knee arthroplasty: 252 cases with a minimum follow-up of 5 years. J Arthroplasty 32:1132–1136. 10.1016/j.arth.2016.11.027 [DOI] [PubMed] [Google Scholar]
- 112.Kennedy JA, Matharu GS, Hamilton TW, Mellon SJ, Murray DW (2018) Age and outcomes of medial meniscal-bearing unicompartmental knee arthroplasty. J Arthroplasty 33:3153–3159. 10.1016/j.arth.2018.06.014 [DOI] [PubMed] [Google Scholar]
- 113.Saenz CL, McGrath MS, Marker DR, Seyler TM, Mont MA, Bonutti PM (2010) Early failure of a unicompartmental knee arthroplasty design with an all-polyethylene tibial component. Knee 17:53–56. 10.1016/j.knee.2009.05.007 [DOI] [PubMed] [Google Scholar]
- 114.Edmiston TA, Manista GC, Courtney PM, Sporer SM, Della Valle CJ, Levine BR (2018) Clinical outcomes and survivorship of lateral unicompartmental knee arthroplasty: does surgical approach matter? J Arthroplasty 33:362–365. 10.1016/j.arth.2017.09.009 [DOI] [PubMed] [Google Scholar]
- 115.Kazarian GS, Barrack TN, Okafor L, Barrack RL, Nunley RM, Lawrie CM (2020) High prevalence of radiographic outliers and revisions with unicompartmental knee arthroplasty. J Bone Joint Surg Am 102:1151–1159. 10.2106/JBJS.19.01277 [DOI] [PubMed] [Google Scholar]
- 116.Berend KR, Kolczun MC, George JW, Lombardi AV (2012) Lateral unicompartmental knee arthroplasty through a lateral parapatellar approach has high early survivorship. Clin Orthop 470:77–83. 10.1007/s11999-011-2005-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hamilton WG, Ammeen D, Engh CA, Engh GA (2010) Learning curve with minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 25:735–740. 10.1016/j.arth.2009.05.011 [DOI] [PubMed] [Google Scholar]
- 118.Arthroplasty Registries - NORE - EFORT n.d. https://nore.efort.org/arthroplasty-registries. Accessed 15 Aug 2024
- 119.R.P.A - Home n.d. http://www.rpa.spot.pt/?lang=en-GB. Accessed 26 January 2024
- 120.SIRIS Report Hip & Knee. SIRIS IMPLANT n.d. http://www.siris-implant.ch/de/Downloads&category=16. Accessed 26 Jan 2024
- 121.McKie J, Taylor J, Devane P, Young S, Coleman B, Debenham M, et al. Registry Management Committee n.d.
- 122.Annual reports - Svenska knäprotesregistret n.d. http://www.myknee.se/en/publications/annual-reports. Accessed 26 Jan 2024
- 123.Australian Orthopaedic Association National Joint Replacement Registry, Smith PN, Australian National University Medical School, Gill DRJ, Australian Orthopaedic Association National Joint Replacement Registry, McAuliffe MJ, et al. 2023 Hip, knee & shoulder arthroplasty: 2023 annual report. Australian Orthopaedic Association. 10.25310/YWQZ9375
- 124.Nečas L, Katina S. Slovakian arthroplasty register n.d. [PubMed]
- 125.Pabinger C, Lumenta DB, Cupak D, Berghold A, Boehler N, Labek G (2015) Quality of outcome data in knee arthroplasty. Acta Orthop 86:58–62. 10.3109/17453674.2014.961119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pabinger C, Berghold A, Boehler N, Labek G (2013) Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthritis Cartilage 21:263–268. 10.1016/j.joca.2012.11.014 [DOI] [PubMed] [Google Scholar]
- 127.Baker P, Jameson S, Critchley R, Reed M, Gregg P, Deehan D (2013) Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am 95:702–709. 10.2106/JBJS.L.00520 [DOI] [PubMed] [Google Scholar]
- 128.Di Martino A, Bordini B, Barile F, Ancarani C, Digennaro V, Faldini C (2021) Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: a registry study on 6453 prostheses. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 29:3323–3329. 10.1007/s00167-020-06184-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Johnson WB, Engh CA, Parks NL, Hamilton WG, Ho PH, Fricka KB (2020) A lower threshold for revision of aseptic unicompartmental vs total knee arthroplasty. Bone Jt J 102-B:91–95. 10.1302/0301-620X.102B6.BJJ-2019-1538.R1 [DOI] [PubMed] [Google Scholar]
- 130.Tay ML, Monk AP, Frampton CM, Hooper GJ, Young SW (2023) A comparison of clinical thresholds for revision following total and unicompartmental knee arthroplasty. Bone Jt J 105-B:269–276. 10.1302/0301-620X.105B3.BJJ-2022-0872.R2 [DOI] [PubMed] [Google Scholar]
- 131.Sun X, Su Z (2018) A meta-analysis of unicompartmental knee arthroplasty revised to total knee arthroplasty versus primary total knee arthroplasty. J Orthop Surg 13:158. 10.1186/s13018-018-0859-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Additional data is available on request.



