Abstract
Introduction
Partial anomalous pulmonary venous connection (PAPVC) is a potential cause of right-sided heart failure. Notably, a risk of sudden circulatory failure exists during lung surgery. Only a few reports of PAPVC complicated by lung cancer requiring lobectomy exist. Here, we report a case of left lower lung lobectomy complicated by an anomalous connection of the left upper pulmonary vein requiring revascularization.
Case presentation
A 66-year-old man was found with an abnormal mass shadow in the left lower lung field on chest radiography. Bronchoscopy revealed lung adenocarcinoma. Preoperative contrast-enhanced computed tomography showed that the left upper pulmonary vein did not perfuse the left atrium but was connected to the left brachiocephalic vein. Preoperative transthoracic echocardiography revealed right atrial and ventricular enlargement. The clinical diagnosis was stage IB (T2aN0M0). We decided to perform a left lower lobectomy and correct the PAPVC to maintain oxygenation after the lobectomy. The PAPVC was ligated, and the stump of the left upper pulmonary vein was anastomosed to the left atrial appendage without cardiopulmonary bypass. Postoperative contrast-enhanced computed tomography revealed intact reconstructed vessels. Postoperative transthoracic echocardiography showed no right ventricular overload. The patient’s postoperative clinical course following the surgical procedure was uneventful. Furthermore, the patient was followed up without any complications.
Conclusions
This rare case of successful surgical correction can inform clinicians of similar cases.
Keywords: Lung cancer, Partial anomalous pulmonary venous connection, Revascularization
Introduction
A partial anomalous pulmonary venous connection (PAPVC) is a congenital vessel anomaly. One or more pulmonary veins connect directly to the right atrium or indirectly flow through the systemic vein [1]. However, only a few reports of PAPVC complicated by lung cancer requiring lobectomy exist. The PAPVC is ligated if it is located in the pulmonary lobe designated for resection. However, determining whether revascularization should be performed if the lesion is located in a preserved lobe is necessary. Here, we report a case of left lower lung lobectomy complicated by an anomalous connection of the left upper pulmonary vein (LUPV) that required revascularization.
Case presentation
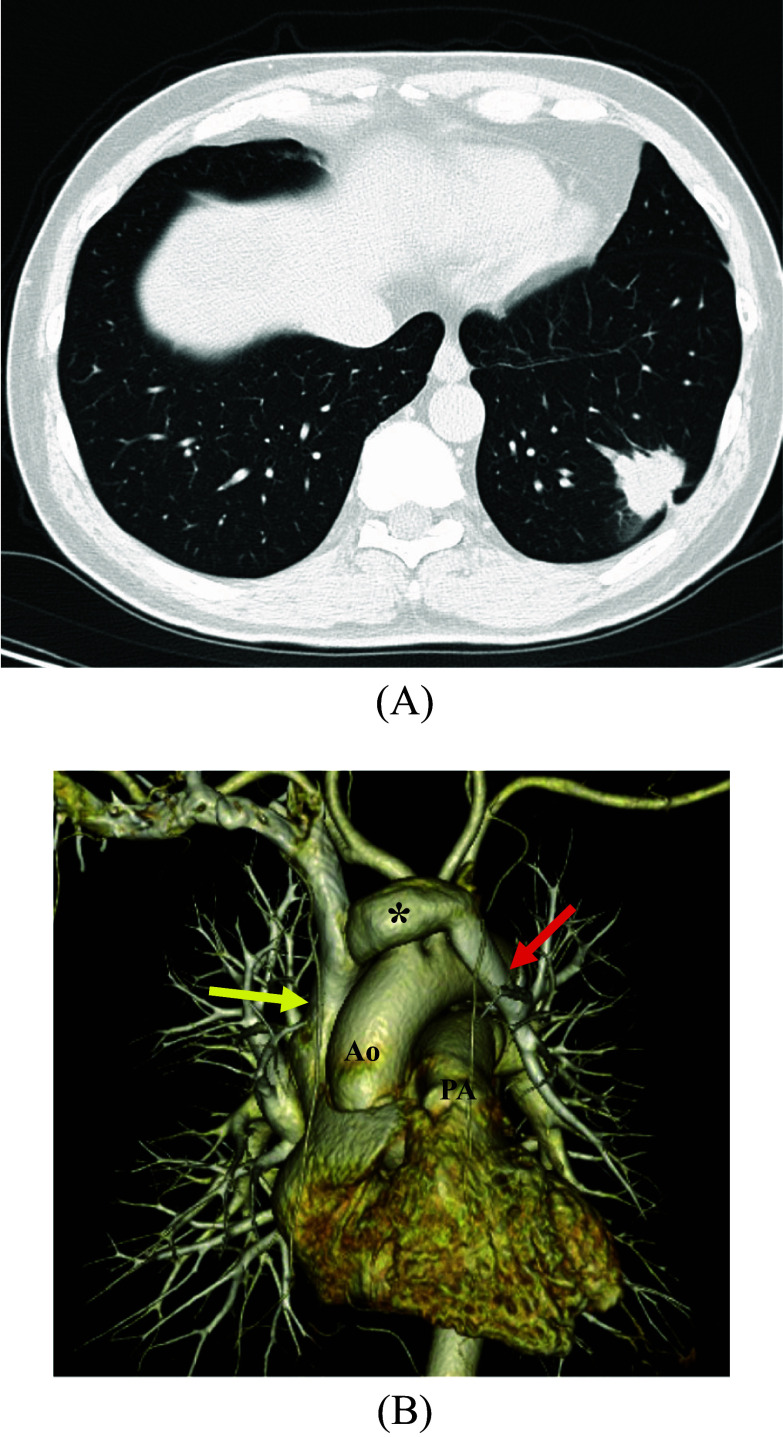
A 66-year-old man was found with an abnormal mass shadow in the left lower lung field on chest radiography. Bronchoscopy confirmed lung adenocarcinoma. Subsequently, the patient was referred to our hospital for surgical treatment. He was asymptomatic. On physical examination, the patient’s percutaneous oxygen saturation was 98% in room air, and his respiratory rate was 16/min. Pulmonary function tests showed the forced expiratory volume percent in 1 s was 70.57%, and the percent vital capacity was 101.1%. Preoperative contrast-enhanced computed tomography (CECT) revealed an ~ 39 mm mass in the left lower lobe (Fig. 1A). The LUPV did not perfuse the left atrium but was connected to the left brachiocephalic vein (Fig. 1B). Preoperative transthoracic echocardiography showed a left ventricular ejection fraction of 65.3%. No asynergies or atrial septal defects were found. The right atrium and ventricle were enlarged, and the clinical diagnosis was stage IB (T2aN0M0). We decided to perform a left lower lobectomy and correct the PAPVC to maintain oxygenation after the lobectomy.
Fig. 1.
Preoperative contrast-enhanced computed tomography. A Mass with a specula was observed in the left lower lobe. Its border was irregular, and its diameter was ~ 39 mm. B Left upper pulmonary vein (red arrow: LUPV) drained into the superior vena cava (yellow arrow) via the left brachiocephalic vein (asterisk) (Ao aorta, PA pulmonary artery)
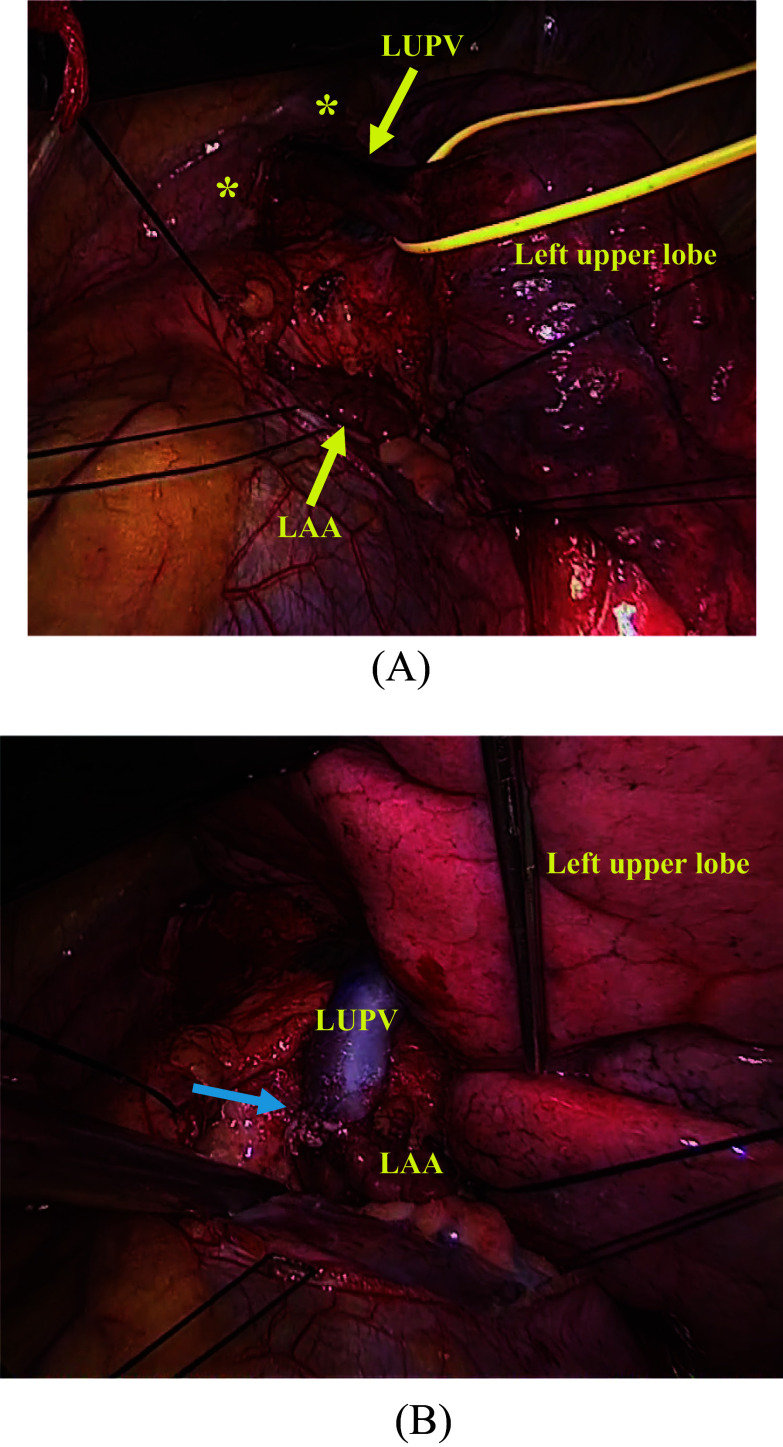
First, the patient underwent video-assisted left lower lobectomy with lymphadenectomy through left posterolateral thoracotomy in the fifth intercostal space under one-lung ventilation. Subsequently, the abnormal LUPV was corrected. Intraoperatively, the LUPV drained into the left brachiocephalic vein and was not connected to the left atrium. The LUPV was peeled to the confluence of the brachiocephalic vein to ensure it was sufficiently long. In the same view, the left side pericardium was incised, and the left atrium appeared. We confirmed that the LUPV could be anastomosed to the left atrial appendage and was not kinked during lung inflation. After 80 units/kg of heparin was injected, the junction between the LUPV and the left brachiocephalic vein was ligated using a Powered ECHELON FLEX (ETHICON, NJ, USA). The left atrium appendage was partially clamped. Subsequently, the LUPV stump was anastomosed to the left atrial appendage using a 6-0 PROLENE (ETHICON, NJ, USA) without cardiopulmonary bypass (Fig. 2). Postoperatively, we initiated anticoagulation with warfarin and aspirin to prevent thrombosis at the anastomotic site.
Fig. 2.
Intraoperative findings. A Left brachiocephalic vein was noted behind the pleura (asterisk). The left upper pulmonary vein (LUPV) connected to the left brachiocephalic vein. No pulmonary veins were entering the left atrium except for the left lower pulmonary vein. We marked the antero-wall of the LUPV to prevent kinking. B LUPV was anastomosed to the left atrial appendage. The blue arrow indicates the anastomotic site
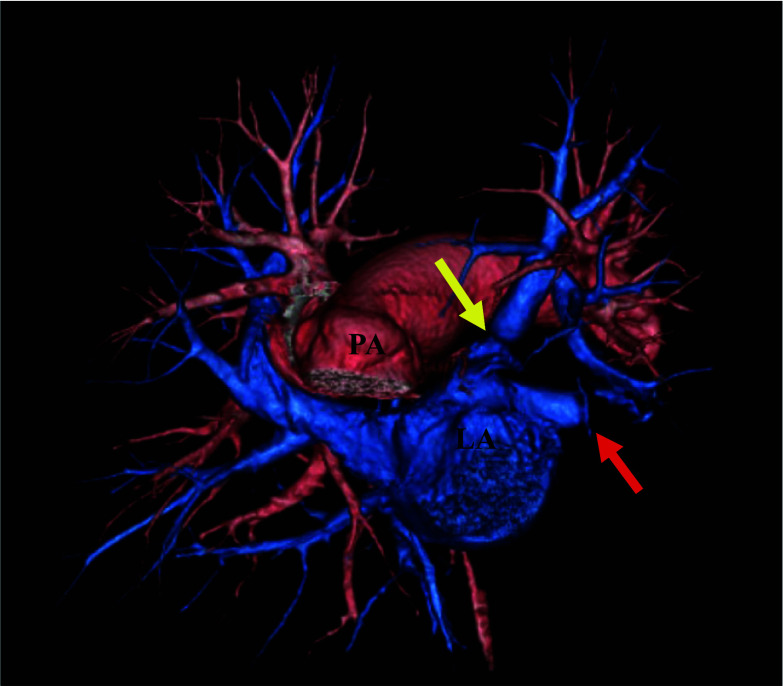
Postoperative CECT revealed intact reconstructed vessels (Fig. 3). Postoperative transthoracic echocardiography revealed no right ventricular overload.
Fig. 3.
Postoperative contrast-enhanced computed tomography. The anastomotic area was intact and patent (yellow arrow). The red arrow indicates the stump of the left lower pulmonary vein
The clinical course following the surgical procedure was uneventful, and the patient was discharged 8 days postoperatively. Additionally, the patient was followed up without any complications.
Discussion
PAPVC is a rare congenital vascular anomaly; its frequency is estimated at 0.4–0.7% in postmortem examinations [2]. Notably, PAPVCs are usually detected in the right lung, with only 10% of anomalies occurring in the left lung [2]. Furthermore, 80% of PAPVC cases are complicated by atrial septal defects [3]. PAPVCs without atrial septal defects are relatively rare, as in our case. Specifically, one or more pulmonary veins failed to connect to the left atrium, resulting in a left-to-right shunt. The more the left-to-right shunt increases, the more severe the symptoms [4]. However, PAPVC may remain undiagnosed until adulthood because only a few clinical symptoms typically manifest [2]. Importantly, PAPVC is found in 0.1% of the adults examined using computed tomography [5]. Many reports have shown that older patients with PAPVC have an increased right ventricular strain and symptoms of right heart failure [2].
In the present case, we decided to perform a left lower lobectomy for radical resection. PAPVC was diagnosed incidentally during preoperative examinations.
A pulmonary-to-systemic flow ratio (Qp/Qs) of greater than 1.5 is one of the surgical indications of PAPVC [6]. However, the surgical indications for PAPVC have not yet been defined.
Blood from the PAPVC was perfused into the left brachiocephalic vein. Therefore, after lobectomy, we speculated that the hemodynamics would be similar to those found in left pneumonectomy due to blood flow from the PAPVC. We considered that the Qp/Qs increased and oxygenation decreased because the left-to-right shunt flow increased postoperatively.
Furthermore, we presumed that the patient had right heart overload because the preoperative transthoracic echocardiography showed right ventricular dilatation. ElBardissi et al. reported a patient who died of right heart failure due to uncorrected PAPVC after a lung cancer procedure [7]. Moreover, right-sided heart overload can cause right-sided heart failure in the long term. Therefore, we decided to correct the PAPVC.
However, the operative procedure has not yet been established. Five cases of reconstructive PAPVC were associated with lung resection (Table 1) [8–12]. If the PAPVC was located in the same lung lobe to be resected, we identified an abnormal vessel and ligated it. Otherwise, careful measures should be taken. PAPVC on the right side necessitates intra-atrial flow diversion with cardiopulmonary bypass, employing techniques such as the Warden procedure or the double-decker method [3, 12]. In contrast, the left PAPVC could be reconstructed without cardiopulmonary bypass. In the present case, the PAPVC was anastomosed to the left atrial appendage for anatomical reasons. Takei et al. anastomosed an anomalous vein to the stump of a pulmonary vein connected to a resected lobe [8].
Table 1.
Reconstructive cases of partial anomalous pulmonary vein connection associated with lung resection
| Year | Author | Age | Gender | Tumor location | Resection | PAPVC source | PAPVC drain | Anastomotic site |
|---|---|---|---|---|---|---|---|---|
| 2002 | Takei et al. | 58 | Female | LLL | Lobectomy | LUPV | LBCV | LLPV |
| 2005 | Sakurai et al. | 48 | Male | LUL | Pneumonectomy | RUPV | SVC | Intra-atrial flow diversion |
| 2006 | Smith et al. | 45 | Female | LLL | Lobectomy | LUPV | LBCV | LAA |
| 2017 | Kawagoe et al. | 74 | Female | LLL | Lobectomy | LUPV | LBCV | LLPV |
| 2020 | Fukumoto et al. | 66 | Female | LUL | Lobectomy | RUPV | SVC | Double-decker method |
| 2024 | Present case | 66 | Male | LLL | Lobectomy | LUPV | LBCV | LAA |
LUL left upper lobe, LLL left lower lobe, LUPV left upper pulmonary vein, LLPV left lower pulmonary vein, RUPV right upper pulmonary vein, LBCV left brachiocephalic vein, SVC superior vena cava, LAA left atrial appendage
Postoperatively, anticoagulation therapy was initiated to prevent thrombogenesis at the anastomotic site. The target prothrombin time-international normalized ratio was set at 2.0. Transthoracic echocardiography performed in the second postoperative month revealed no right ventricular overload. Therefore, warfarin was discontinued because the reconstructed vessel was not obstructed, and aspirin was continued.
The patient’s postoperative course was uneventful. This rare case of successful surgical treatment of PAPVC with lung cancer in different lobes can guide clinicians in managing similar cases.
Conclusions
PAPVC is a potential cause of right-sided heart failure. In particular, a risk of sudden circulatory failure exists during lung surgery. Therefore, the indications for surgical correction must be carefully determined. This rare case of successful surgical correction of PAPVC with lobectomy can inform clinicians in managing similar cases.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Abbreviations
- CECT
Contrast-enhanced computed tomography
- LUPV
Left upper pulmonary vein
- PAPVC
Partial anomalous pulmonary venous connection
- Qp/Qs
Pulmonary-to-systemic flow ratio
Author contributions
KN contributed to the acquisition of the clinical data and prepared the manuscript for this case report. JT performed the operations and perioperative management and contributed to the drafting and revision of the manuscript. TF supervised decision-making, implemented the treatment plan for the patient, and prepared the manuscript. All the authors have read and approved the final version of the manuscript.
Funding
No external support was obtained for this manuscript, including funding for equipment and drugs.
Availability of data and materials
None.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient and his family for this publication.
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Healey JE Jr. An anatomic survey of anomalous pulmonary veins: their clinical significance. J Thorac Surg. 1952;23:433–44. 10.1016/S0096-5588(20)31117-X. [PubMed] [Google Scholar]
- 2.ElBardissi AW, Dearani JA, Suri RM, Danielson GK. Left-sided partial anomalous pulmonary venous connections. Ann Thorac Surg. 2008;85:1007–14. 10.1016/j.athoracsur.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 3.Said SM, Burkhart HM, Schaff HV, Cetta F, Phillips SD, Barnes RD, et al. Single-patch, 2-patch, and caval division techniques for repair of partial anomalous pulmonary venous connections: does it matter? J Thorac Cardiovasc Surg. 2012;143:896–903. 10.1016/j.jtcvs.2011.09.074. [DOI] [PubMed] [Google Scholar]
- 4.Kawasaki H, Oshiro Y, Taira N, Furugen T, Ichi T, Yohena T, et al. Partial anomalous pulmonary venous connection coexisting with lung cancer: a case report and review of relevant cases from the literature. Ann Thorac Cardiovasc Surg. 2017;23:31–5. 10.5761/atcs.cr.16-00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho M-L, Bhalla S, Bierhals A, Gutierrez F. MDCT of partial anomalous pulmonary venous return (PAPVR) in adults. J Thorac Imaging. 2009;24:89–95. 10.1097/RTI.0b013e318194c942. [DOI] [PubMed] [Google Scholar]
- 6.Singhal K, Newton AD, Corbett C, Predina JD. Management of partial anomalous pulmonary venous connections in patients requiring pulmonary resection: a case report and systematic review. J Thorac Dis. 2017;9:5434–9. 10.21037/jtd.2017.11.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Black MD, Shamji FM, Goldstein W, Sachs HJ. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg. 1992;53:689–91. 10.1016/0003-4975(92)90336-3. [DOI] [PubMed] [Google Scholar]
- 8.Takei H, Suzuki K, Asamura H, Kondo H, Tsuchiya R. Successful pulmonary resection of lung cancer in a patient with partial anomalous pulmonary venous connection: report of a case. Surg Today. 2002;32:899–901. 10.1007/s005950200176. [DOI] [PubMed] [Google Scholar]
- 9.Sakurai H, Kondo H, Sekiguchi A, Naruse Y, Makuuchi H, Suzuki K, et al. Left pneumonectomy for lung cancer after correction of contralateral partial anomalous pulmonary venous return. Ann Thorac Surg. 2005;79:1778–80. 10.1016/j.athoracsur.2003.10.092. [DOI] [PubMed] [Google Scholar]
- 10.Smith RL II, Zorn GL III, Peeler BB, Jones DR. Combined bronchial sleeve resection and repair of partial anomalous pulmonary venous return. J Thorac Cardiovasc Surg. 2006;132:982–3. 10.1016/j.jtcvs.2006.05.062. [DOI] [PubMed] [Google Scholar]
- 11.Kawagoe I, Hayashida M, Nozumi Y, Banno T, Hirayama S, Suzuki K, et al. A combination of a partial anomalous pulmonary venous connection (PAPVC) and a lung tumor requiring pulmonary resection. J Cardiothorac Vasc Anesth. 2017;31:274–8. 10.1053/j.jvca.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Fukumoto K, Goto M, Ichikawa Y, Kawasumi Y, Uchiyama M, Maekawa A, et al. Lobectomy with bronchoplasty and pulmonary arterial angioplasty for lung cancer after correction of contralateral partial anomalous pulmonary venous connection. Surg Case Rep. 2020;6:310. 10.1186/s40792-020-01083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.