Abstract
Background
In Yemen, effective early detection and a comprehensive grasp of breast cancer symptoms and risk factors are vital in preventing its potentially deadly spread. However, challenges arise in combating breast cancer in Yemen due to the lack of patient registries, national strategies, and structured cancer treatment plans.
Objective
This research sought to evaluate the awareness levels of breast cancer and the perceived obstacles to breast cancer screening among adult Yemeni women.
Methods
A community-based cross-sectional questionnaire study was conducted from September 2023 to January 2024 from two teaching and largest hospitals in the capital municipality, Sana’a, Yemen, where 533 women (≥ 18 years old) were conveniently selected in this study. Data were analyzed using SPSS software (version 23).. The Chi-square test was used to test associations. The factors associated with breast cancer awareness and barriers to breast cancer screening were analyzed separately, using multivariable logistic regression.
Results
The study revealed that 88.6% of women were familiar with breast cancer, and 61.9% being knowledgeable about screening methods such as clinical breast examination (CBE) or mammography. The primary hindrance to screening (84.1%, n = 53) was the absence of symptoms or pain. The second most common reason for not undergoing screening was a lack of understanding about breast cancer and its treatment (61.9%, n = 39).
Conclusion
To enhance breast cancer screening rates among Yemeni women consistently, targeted educational programs emphasizing the benefits of early detection and dispelling misconceptions and barriers related to the disease are essential.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12672-024-01419-w.
Keywords: Awareness, Breast cancer, Breast cancer screening, Perceived Barriers, Yemeni Women
Introduction
Breast cancer (BCa) is the primary cancer among women globally, with a notable increase in developing countries where it is often identified at advanced stages [1, 2]. This multifactorial disease is influenced by a range of factors including population demographics, lifestyle choices, genetics, and environmental elements. Moreover, delayed detection, inadequate healthcare access, and suboptimal diagnostic and treatment resources are also significant contributors to the rising prevalence of breast cancer [3, 4]. Timely detection plays a crucial role in preventing cancer progression and ultimately saving lives. Regular mammogram screenings have proven effective in reducing mortality rates. However, across various demographic groups, adherence to screening falls short of ideal expectations. In many vulnerable communities, access to breast cancer-screening initiatives remains limited [4].
In Yemen, breast cancer stands out as the most prevalent cancer among women, accounting for 30.8% of cases and 17.4% of all cancers [5]. Recent World Health Organization data from 2020 revealed 2,894 new breast cancer cases in Yemen [6, 7]. This disease ranks as the leading cause of female mortality in the country. Notably, breast cancer awareness in Yemen is notably deficient, with limited information available from studies primarily conducted in key areas like Al-Mukalla and Sana'a. These studies indicate that only a small fraction, ranging from 11% to 17.4% of Yemeni women, engage in breast self-examinations, with merely 1.6% undergoing mammogram screenings [7]. Insufficient breast cancer awareness in women hampers their engagement in screening programs, thereby impeding early detection and treatment outcomes [8].This limitation leads to delayed identification of patients until the disease has advanced, potentially rendering curative treatments ineffective [9].
Additionally, breast cancer can have a substantial impact on quality of life and the cost-effectiveness of healthcare services [10]. In Yemen, despite efforts to tackle breast cancer through early detection, prevention, treatment, and palliative care initiatives, the challenges arise from the absence of cancer patient registries, national cancer care strategies, and comprehensive treatment plans. Moreover, the lack of systematic cancer monitoring in the country exacerbates the limitations of its resource-constrained healthcare system, leading to many women not being able to identify symptoms or appreciate the significance of early detection. Therefore, enhancing patient awareness through research on self-examination can lead to early diagnosis, treatment, and improved survival rates. Identifying barriers to successful management is crucial for healthcare professionals and policymakers in the Ministry of Health to develop strategies to reduce breast cancer prevalence. Notably, breast cancer has a higher morbidity and mortality rate globally [10, 11]. This study, therefore, aims to bridge the scientific gap by assessing breast cancer awareness levels and recognizing obstacles preventing Yemeni women from accessing screening services.
Materials and methods
Study setting and participants
This study employed a community-based cross-sectional design. Data collection occurred from September 2023 to January 2024, spanning three months, via a group of six female university graduates who were trained to conduct the interviews and distribute questionnaires to the participants.The participants were 533 women recruited from the two largest teaching hospitals in Capital Sana'a City, Yemen: University of Science and Technology Hospital (USTH) and Al-Gumhori Hospital. To gather insights on breast cancer awareness and screening barriers, participants completed a structured interview questionnaire.
The questionnaire assessed their knowledge of breast cancer, potential obstacles to undergoing screening, and other relevant information. The instrument was adapted from a previously published study by Islam et al. [14]. All study participants volunteered to participate and were free to withdraw their participation at any point. No names were identified on the questionnaires, and the responders were involved in the study with verbal consent.
Sample size calculation
We utilized the simplified sampling formula from OpenEpi version 3 to determine the sample size, which indicated that we need 430 participants. However, to increase our confidence level, we decided to slightly exceed the required sample size and set our target at 533 participants. Our target population comprised women who visited USTH and Al-Gumhori Hospital in Sana'a city. The sample size calculation was determined using a 5% margin of error and a 95% confidence level. OpenEpi version 3 software was employed for this computation.
Exclusion and inclusion criteria
Women aged 18 and above who visited USTH and Al-Gumhori Hospital in Sanaa city were eligible to participate in this study. Exclusion criteria encompassed those females aged less than 18 years. Nationalities other than Yemen, women working in the medical field, and women who participated in the pilot study were excluded.
Study instrument
A structured questionnaire was designed from previously published study that adapted validated questions [14]. For better understanding, the questionnaire was translated from English to Arabic and then back translated into English by several people proficient in both language. The questionnaire was divided into three sections, each section clearly labeled to indicate its content. The first section focused on sociodemographic variables, the second section had 9 close-ended questions (yes/no answer) and 3 open-ended questions about awareness of breast screening, and the third section is also composed of 13 close-ended questions (yes/no and I don't know the answer) about awareness of barriers to breast screening. The total number of questions was 42. The questionnaire was distributed to 9 experts from multiple fields, including clinical pharmacy, community medicine, pharmacy practice, internal medicine, and oncologist for content validation. The experts were asked to assess the relevance and representation of the items within their respective domains. Ten women assessed the clarity and comprehension of the questions in each domain. Then, the questionnaire was piloted-tested on 33 women. Then, a reliability statistic was conducted by Cronbach’s Alpha that equaled 0.7. Feedback from pilot study participants and face validation helped to improve data collection for the main study.
Data collection
At the beginning of the study, all participants were provided with a detailed verbal overview of the research goals, subject matter, time requirements, as well as assurances of confidentiality and anonymity. Following this, informed consent was acquired from each participant before the interviews commenced. To accommodate our population with limited literacy, data collection was carried out through structured interviews led by qualified clinical pharmacist graduates. Data gathering took place through in-person interviews, specifically at USTH and Al-Gumhori Hospital in Sanaa City, Yemen.
Ethical considerations
Our study protocol received ethics approval from the Research Ethics Committee of the Faculty of Pharmacy, University of Science and Technology, ( Ref. No. (1445/009). All methods were carried out in accordance with the declaration of Helsinki, and all its amendments and revisions.
Statistical analysis
Data were analyzed using SPSS software (version 23). Categorical variables were described using frequency distribution and percentages. Continuous variables were expressed by means and standard deviations. The chi-square test was used for the analysis of categorical variables. The correlation was analyzed using Pearson’s correlation coefficient. Univariable and multivariable logistic regression was applied to identify significant predictors of breast self-examination and clinical breast examination practice. An odds ratio (OR) and 95% confidence interval (CI) were used to analyze the degree to which dependent and independent variables are associated. Moreover, the perceived barrier toward screening among the women was displayed descriptively. A P-value of < 0.05 was considered statistically significant.
Results
Societal demographics
Of the 533 participants, the mean age was 30.53 (± 11.5) years and 89.7% lived in urban areas. 57.6% were married, and 47.8% were homemakers. Almost three-quarters (75.2%) of the participants had secondary education, and 9.2% had no education. 10.9% of the individuals were classified as obese, while 13.7% fell into the category of being underweight. Additionally, it was found that 51.2% of the female participants did not have any children. while 24.6% had 3 children or more. The distribution of monthly family income categories (Less than 50,000 R.Y, 50,000–100,000 R.Y, and more than 100,000 RY) was 24.2%, 34.1%, and 41.7%, respectively. 98.1% of the women's medical history revealed no past cases of breast cancer, 88.9% had no familial history of breast cancer among their relatives, 78.2% had no history of chronic disease, and 73.9% had not smoked cigarettes or shisha. More details of demographic factors can be seen in (Table 1).
Table 1.
The sociodemographic profile of the study participants (n = 533)
| Characteristics | N (%) | |
|---|---|---|
| Age | 18–31 | 350 (65.7) |
| 32–47 | 131 (24.6) | |
| 48–63 | 52 (9.8) | |
| BMI | Normal | 258 (48.4) |
| Underweight | 73 (13.7) | |
| Overweight | 144 (27.0) | |
| Obese | 58 (10.9) | |
| Marital condition | Married, widow and divorced | 307 (57.6) |
| Single | 226 (42.4) | |
| Number of offspring | Childless | 273 (51.2) |
| Only child | 78 (14.6) | |
| Two children | 51 (9.6) | |
| Three children or more | 131 (24.6) | |
| Monthly income of the family | Less than 50,000 R. Y | 129 (24.2) |
| 50,000–100,000 R. Y | 182 (34.1) | |
| More than 100,000 RY | 222 (41.7) | |
| Level of education | Secondary and above | 401 (75.2) |
| Primary | 83 (15.6) | |
| No education | 49 (9.2) | |
| Occupation | Housewife | 255 (47.8) |
| Student | 174 (32.6) | |
| Employed | 104 (19.5) | |
| Place of domicile | Urban | 478 (89.7) |
| Rural | 55 (10.3) | |
| Breast cancer medical history | Yes | 10 (1.9) |
| No | 523 (98.1) | |
| Family breast cancer case history | Yes | 59 (11.1) |
| No | 474 (88.9) | |
| History of chronic disease | Yes | 116 (21.8) |
| No | 417 (78.2) | |
| Smoke cigarettes or shisha | Yes | 139 (26.1) |
| No | 394 (73.9) | |
| Total | 533 (100) | |
The level of general awareness regarding breast cancer and breast screening methods.
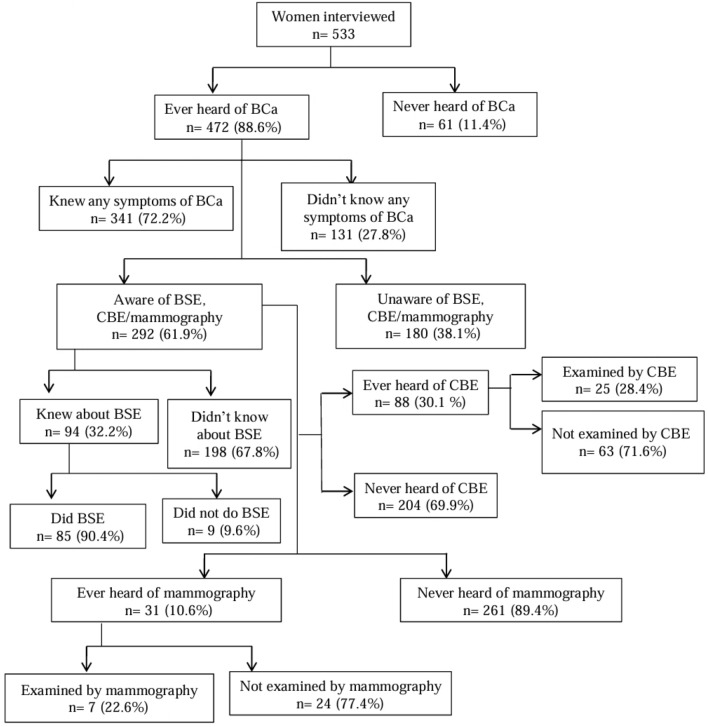
Most participants (88.6%) were familiar with breast cancer (BCa), as shown in Fig. 1. Among the 472 women who had heard of BC, 72.2% were aware of the symptoms. Of those who had ever heard of BCa (61.9%; n = 292), 32.2% were knowledgeable about breast self –examination (BSE), and 90.4% performed it. 30.1% (n = 88) had heard of CBE, and 28.4% (n = 25) had undergone it. Furthermore, 10.6% (n = 31) had heard of mammography, but only 7 women (22.6%) had a mammogram. Women residing in rural areas were significantly associated with lower awareness of BCa (OR, 0.207; 95% CI 0.084–0.331), as were those with only primary (OR, 0.418; 95%CI 0.011–0.825) or no education (OR, 0.315; 95%CI 0.152–0.478). Additionally, women aged 32–47 years (OR, 0.108; 95%CI 0.029–0.187) and 48–63 years (OR, 0.306; 95%CI 0.060–0.552) were less likely to be aware of BCa compared to women aged 18–31 years. Overweight or obese women were associated with more awareness of BCa (OR, 1.471; 95%CI 0.664–3.260) and (OR, 1.766; 95%CI 0.527–5.917) than those women with an average body mass index (BMI). However, women with one child, two or three children or more were associated with less awareness of BCa (OR, 0.478; 95%CI 0.176–0.780), (OR, 0.257; 95%CI 0.042–0.471), and (OR, 0.146; 95%CI 0.074–0.217), respectively, compared to women with no children. Single women (OR, 0.301; 95%CI 0.176–0.425) were also less likely to be aware of BCa than married women. Women with a monthly income of less than 50,000 R.Y and 50,000–100,000 R.Y (OR, 0.236; 95%CI 0.156–0.315) and (OR, 0.148; 95%CI 0.066–0.230) were less aware compared to women with a monthly income of more than 100,000 RY. Employed women (OR, 0.183; 95%CI 0.033–0.333) were associated with less BCa awareness than housewives. Furthermore, women with no history of breast cancer (OR, 997; 95%CI 0.892–1.102) or breast cancer in their family (OR, 0.807; 95%CI 0.585–1.028) were associated with less awareness of BCa. Similarly, women with no previous history of chronic diseases (OR, 0.895; 95%CI 0.648–1.142) or who did not smoke cigarettes or shisha (OR, 0.865; 95%CI 0.620–1.110) were associated with less awareness of BCa compared to those who had a history of chronic disease or smoked cigarettes or shisha. (Table 2).
Fig. 1.
Illustrates the knowledge and practices of breast cancer and breast cancer screening among the study population
Table 2.
Relationship between sociodemographic characteristic and awareness of breast cancer (n = 472)
| Variables | Ever heard of BCa | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| OR (CI) | P value | OR (CI) | P value | |
| Age (in years) | ||||
| 18–31 | 1.0 | 1.0 | ||
| 32–47 | 2.290 (0.893–5.875) | 0.085 | 0.108 (0.029–0.187) | 0.007 |
| 48–63 | 0.556 (0.181–1.714) | 0.307 | 0.306 (0.060–0.552) | 0.015 |
| ± BMI (kg/m2) | ||||
| Normal weight | 1.0 | 1.0 | ||
| Underweight | 0.926 (0.359–2.387) | 0.873 | 0.188 (0.051–0.326) | 0.007 |
| Overweight | 0.311 (0.024–0.598) | 0.342 | 1.471 (0.664–3.260) | 0.034 |
| Obese | 0.497 (0.150–0.844) | 0.357 | 1.766 (0.527–5.917) | 0.005 |
| Marital condition | ||||
| Married (Widow and Divorced) | 1.0 | 1.0 | ||
| Single | 0.328(0.083–1.296) | 0.112 | 0.301 (0.176–0.425) | 0.000 |
| Number of offspring | ||||
| Childless | 1.0 | 1.0 | ||
| Only child | 0.686 (0.163–2.894) | 0.608 | 0.478 (0.176–0.780) | 0.002 |
| Two children | 0.293(0.071–1.211) | 0.090 | 0.257 (0.042–0.471) | 0.019 |
| Three children or more | 0.555 (0.144–2.134) | 0.391 | 0.146 (0.074–0.217) | 0.000 |
| Monthly income of the family | ||||
| More than 100,000 RY | 1.0 | 1.0 | ||
| Less than 50,000 RY | 0.333 (0.149–0.743) | < 0.007 | 0.236 (0.156–0.315) | 0.000 |
| 50,000–100,000 RY | 0.680(0.294–1.576) | 0.369 | 0.148 (0.066–0.230) | 0.000 |
| Level of education | ||||
| Secondary and above | 1.0 | 1.0 | ||
| Primary | 0.104 (0.038–0.288) | < 0.000 | 0.418 (0.011–0.825) | 0.044 |
| No education | 0.247 (0.103–0.592) | < 0.002 | 0.315 (0.152–0.478) | 0.000 |
| Housewife | 1.0 | 1.0 | ||
| Student | 1.395 (0.501–3.886) | 0.524 | 0.129 (0.103–0.361) | 0.275 |
| Employed | 2.166 (0.635–7.389) | 0.217 | 0.183(0.033–0.333) | 0.017 |
| Place of domicile | ||||
| Urban | 1.0 | 1.0 | ||
| Rural | 0.411 (0.188–0.895) | < 0.025 | 0.207 (0.084–0.331) | 0.001 |
| Breast cancer medical history | ||||
| Yes | 1.0 | 1.0 | ||
| No | 1.947 (0.397–9. (541 | 0.411 | 0.997 (0.892–1.102) | 0.000 |
| Family breast cancer case history | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.119 (0.016–0.877) | 0.037 | 0.807 (0.585–1.028) | 0.000 |
| History of chronic disease | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.924 (0.471–1. (812 | 0.817 | 0.895 (0.648–1.142) | 0.000 |
| Smoke cigarettes or shisha | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.817 (0.433–1.541) | 0.532 | 0.865 (0.620–1.110) | 0.000 |
OR odds ratio, CI confidence interval, p value significant at < 0.05
Barriers affecting breast cancer screening
The reasons given by women who were aware of CBE or mammography for not getting screened included the absence of symptoms or pain (84.2%), insufficient knowledge about breast cancer and its treatment options (62.0%), and not knowing screening was needed (54.1%). Among the barriers that hinder Yemeni women from breast screening werefamily did not allow them to go for screening and the absence of specialty centers, both of which were reported with the least frequency at6.5% and 7.9% respectively (Table 3).
Table 3.
Respondents’ Awareness about barriers to breast screening (n = 292)
| No | Barriers | Frequency (%) |
|---|---|---|
| 1 | I did not experience any symptoms or pain | 246 (84.2) |
| 2 | Insufficient knowledge regarding breast cancer and its treatment | 181(62.0) |
| 3 | I was unaware of the necessity for screening | 158 (54.1) |
| 4 | The fear of the diagnostic test and its outcome was present | 121(41.4) |
| 5 | The process of undressing for the diagnosis felt embarrassing and uncomfortable | 111(38.0) |
| 6 | Expensive (accommodation, treatment, medicine) | 93(31.8) |
| 7 | I had insufficient time available for screening | 93 (31.8) |
| 8 | I had no knowledge of the correct place to go | 79 (27.0) |
| 9 | Lack of communication with health care providers | 65 (22.3) |
| 10 | Health care service centres was too far | 65 (22.3) |
| 11 | There are no expected benefits from the screening | 56 (19.2) |
| 12 | Poor read communication and transportation | 56 (19.2) |
| 13 | No accompany to go for screening | 42 (13.4) |
| 14 | Religious reason | 28 (9.6) |
| 15 | No speciality centres for screening | 23 (7.9) |
| 16 | My family did not allow me to go | 19 (6.5) |
Various factors were found to be associated with clinical breast examination (CBE) among women
Through multivariable analysis. The findings revealed several trends. Firstly, women with no education were less likely to undergo CBE (OR, 0.419; 95%CI 0.164–1.836; p = 0.020). Additionally, women aged 32–47 years (OR, 0.339; 95%CI 0.115–0.563; p = 0.004) and 48–63 years (OR, 0.667; 95%CI 0.057–1.276; p = 0.032) were less likely to undergo CBE compared to women aged 18–31 years. Furthermore, women with two children (OR, 0.551; 95%CI 0.030–1.072; p = 0.039) were less likely to undergo CBE than women without children. Single women (OR, 0.095; 95%CI 0.067–0.504; p = 0.000) were also less likely to undergo CBE compared to married women. Additionally, women with a monthly income less than 50,000 R.Y and 50,000–100,000 R.Y (OR, 0.422; 95%CI 0.050–0.793; p = 0.027) and (OR, 0.917; 95%CI 0.172–1.662; p = 0.017) respectively were less likely to undergo CBE compared to women with a monthly income more than 100,000 RY. Moreover, women residing in rural areas (OR, 0.207; 95%CI 0.084–0.331; p = 0.001) were less likely to undergo CBE compared to women living in urban areas. Women with no history of breast cancer (OR, 0.312; 95%CI 0.076–0.549; p = 0.010) were less likely to undergo CBE compared to women with a history of breast cancer. Similarly, women with no history of breast cancer in their family (OR, 0.730; 95%CI 0.123–1.338; p = 0.010) were less likely to undergo CBE compared to women with a history of breast cancer in their family. Additionally, women with no history of chronic disease (OR, 0.857; 95%CI 0.003–1.711; p = 0.049) were less likely to undergo CBE than women with a chronic disease history. Lastly, women who did not smoke cigarettes or shisha (OR, 0.340; 95%CI 0.060–0.620; p = 0.018) were less likely to undergo CBE compared to women who did smoke cigarettes or shisha. (Table 4).
Table 4.
Various factors were found to be associated with clinical breast examination (CBE) among women (n = 88)
| Variables | CBE | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| OR (CI) | P value | OR (CI) | P value | |
| Age (in years) | ||||
| 18–31 | 1.0 | 1.0 | ||
| 32–47 | 0.863 (0.148–5.044) | 0.870 | 0.339 (0.115–0.563) | 0.004 |
| 48–63 | 4.550 (0.339–16.030) | 0.125 | 0.667 (0.057–1.276) | 0.032 |
| Marital condition | ||||
| Married (Widow and Divorced) | 1.0 | 1.0 | ||
| Single | 0.328(0.083–1.296) | 0.112 | 0.095 (0.067–0.504) | 0.000 |
| Number of offspring | ||||
| Childless | 1.0 | 1.0 | ||
| Only child | 0.131 (0.009–1.967) | 0.141 | 1.000 (0.551–2.551) | 0.202 |
| Two children | 2.365(0.414–13.497) | 0.333 | 0.551 (0.030–1.072) | 0.039 |
| Three children or more | 0.387 (0.042–3.577) | 0.403 | 0.150 (0.047–0.346) | 0.133 |
| Monthly income of the family | ||||
| More than 100,000 RY | 1.0 | 1.0 | ||
| Less than 50,000 RY | 0.584 (0.151–2.262) | 0.436 | 0.422 (0.050–0.793) | 0.027 |
| 50,000–100,000 RY | 0.478(0.120–1.901) | 0.295 | 0.917 (0.172–1.662) | 0.017 |
| Level of education | ||||
| Secondary and above | 1.0 | 1.0 | ||
| Primary | 0.821 (0.752–0.951) | 0.643 | 0.509 (0.149–1.167) | 0.127 |
| No education | 0.962 (0.713–1.562) | 0.916 | 0.419 (0.164–1.836) | 0.020 |
| Place of domicile | ||||
| Urban | 1.0 | 1.0 | ||
| Rural | 0.287 (0.009–9.338 | 0.482 | 0.207 (0.084–0.331) | 0.001 |
| Breast cancer medical history | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.145 (0.011–1. (873 | 0.139 | 0.312 (0.076–0.549) | 0.010 |
| Family breast cancer case history | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.230 (0.070–0. (758 | 0.016 | 0.730 (0.123–1.338) | 0.019 |
| History of chronic disease | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.321 (0.104–0. (989 | 0.048 | 0.857 (0.003–1.711) | 0.049 |
| Smoke cigarettes or shisha | ||||
| Yes | 1.0 | 1.0 | ||
| No | 0.714 (0.229–2. (226 | 0.562 | 0.340 (0.060–0.620) | 0.018 |
OR odds ratio, CI confidence interval, p value: < 0.0
An association between barriers to breast cancer screening and the absence of screening participation
Table 5 demonstrates that women who were not allowed by their families to undergo breast screening had higher odds of not receiving screening (OR = 4.726, 95% CI 2.884–7.744). Additionally, the same finding for, women who had religious reasons (OR = 4.041, 95% CI 2.483–6.577), women who believed there was no accompanying person available for screening (OR = 3.686, 95% CI 2.273–5.978), and women who thought there were no specialty centers for screening (OR = 3.367, 95% CI 2.083–5.442).
Table 5.
An association was found between barriers to breast cancer screening and the absence of screening participation
| Variables | OR | 95% CI | P-value |
|---|---|---|---|
| I did not experience any symptoms or pain | 0.365 | 0.228, 0.586 | 0.000 |
| Insufficient knowledge regarding breast cancer and its treatment | 0.530 | 0.333, 0.843 | 0.010 |
| I was unaware of the necessity for screening | 1.553 | 0.979, 2.464 | 0.062 |
| The fear of the diagnostic test and its outcome was present | 1.429 | 0.902, 2.265 | 0.129 |
| The process of undressing for the diagnosis felt embarrassing and uncomfortable | 2.903 | 1.805, 4.668 | 0.000 |
| Expensive (accommodation, treatment, medicine) | 1.997 | 1.254, 3.182 | 0.004 |
| I had insufficient time available for screening | 2.509 | 1.567, 4.019 | 0.000 |
| I had no knowledge of the correct place to go | 1.597 | 1.006, 2.534 | 0.050 |
| Lack of communication with health care providers | 2.237 | 1.401, 3.573 | 0.001 |
| Health care service centres was too far | 2.819 | 1.754, 4.529 | 0.000 |
| There are no expected benefits from the screening | 2.903 | 1.805, 4.668 | 0.000 |
| Poor read communication and transportation | 1.997 | 1.254,3.182 | 0.004 |
| No accompany to go for screening | 3.686 | 2.273,5.978 | 0.000 |
| Religious reason | 4.041 | 2.483, 6.577 | 0.000 |
| No speciality centres for screening | 3.367 | 2.083, 5.442 | 0.000 |
| My family did not allow me to go | 4.726 | 2.884, 7.744 | 0.000 |
Discussion
This study has demonstrated that the plurality of the participants (88.6%) had heard about breast cancer and its symptoms, while (61.9%) had an intermediate level of awareness of breast screening. The results indicated that age between 18–31 years were more aware than other age. It's attributed to being generally more educated and demonstrating a greater interest in health-related issues than older women and more use of social media. Analogous findings were reported in studies conducted in Malaysia and Jordan, which demonstrated sufficient awareness among young women [13, 14], in contrast, another study done in Qatar [15] found that older women were more BCa aware. It may be due to the fact that they have regular contact with healthcare providers. Relative to women with normal BMI, the enhanced awareness observed amongst overweight and obese women may be explained by an association between higher BMI and higher socio-economic status, and they are more conscious of their health due to the potential risks associated with excess weight. This finding aligned with a study carried out in Pakistan [12]. In the current study, married women have more awareness of breast cancer compared to single women. Perhaps overweight women have more responsibilities and commitments to taking care of their families and children. This finding aligned with a study carried out in Malaysia [16]. In contrast to the current study, unmarried women have more awareness of breast cancer compared to married women in a study done in Bangladesh [17] It is contributed that unmarried women in the latter study were better educated and had high family income. In this study, women who had one child, two children and three children or more were less aware of BCa compared with women who had no child. This may be because they are occupied with childcare responsibilities and upbringing.
Our findings revealed a significant association between breast cancer (BCa) awareness and family monthly income. This suggests that access to financial resources likely plays a role in affording examinations and doctor visits. Similar observations were reported in a study conducted in India [18].
The study also found a statistically significant correlation between education level and BCa awareness. Women with higher education exhibited considerably greater awareness compared to those with less education. This aligns with research conducted in Bangladesh and Saudi Arabia [17, 19]. Interestingly, the results indicated that employment status might influence BCa awareness in Yemeni women. Contrary to expectations, employed participants demonstrated lower awareness than housewives. This could potentially be attributed to the demanding nature of their jobs leaving less time for self-education on breast cancer.Our finding regarding lower BCa awareness among employed women contrasts with research from Saudi Arabia [19]. This difference might be explained by the presence of education and awareness campaigns targeted towards employed women in their workplaces in Saudi Arabia. Furthermore, the study revealed lower BCa awareness among participants residing in rural areas. This can likely be attributed to factors such as lower literacy rates, limited access to mass media, socioeconomic challenges, and restricted decision-making power for women within households. This aligns with previous studies conducted in Bangladesh and Egypt [17, 20].
However, our study also found a positive association between BCa awareness and a personal or family history of the disease. This suggests that personal experiences and increased access to information about breast cancer likely play a role in raising awareness. The current study indicates that only a few numbers of participants were aware of CBE, and a low percentage of them had actually undergone the examination. This could be attributed to several factors, such as a shortage of available mammography equipment, limited technical support, absence of formal screening programs, low income, and insufficient educational initiatives. Consequently, breast cancer tends to be diagnosed at later stages in these cases. Similar findings have been reported in studies done in Bangladesh and Malaysia [17, 21]. Interestingly, another study done in Bangladesh [14] demonstrated a higher level of awareness about CBE. These variations observed across studies may be due to differences in the sampled population (such as university students versus the general population) and variations in sampling methods (convenience sampling versus random sampling). Furthermore, this study demonstrated that women who had two or more children were less probable to receive a clinical breast examination (CBE) compared to women who had no children. This finding may be attributed to the fact that women with multiple children are often older and may experience isolation that is more social. However, they may also have not more available time to visit healthcare providers, suggesting that other factors may be influencing their lower rates of CBE utilization. Interestingly, this finding aligns with a study conducted in Bangladesh [14].
Additionally, our findings indicated that single women were less probable to receive a clinical breast examination (CBE) compared to married women. This observation may be attributed to cultural and religious beliefs, which can serve as significant barriers for Yemeni women when it comes to accessing and undergoing CBE. Cultural and religious factors can influence women's decisions regarding health-seeking behaviors, including CBE. In some societies, there may be a stigma associated with unmarried women undergoing certain medical examinations, which could contribute to their lower rates of CBE utilization. Moreover, cultural norms and religious beliefs may shape perceptions of modesty and privacy, making it more challenging for single women to feel comfortable undergoing CBE. This finding aligns with a study conducted in Bangladesh [14].
Moreover, our study found that women residing in rural areas were less likely to undergo clinical breast examination (CBE) compared to women living in urban areas. This disparity in CBE utilization may be attributed to several factors prevalent in rural settings. Firstly, low literacy rates and limited access to educational resources in rural areas can contribute to a lack of awareness and understanding about the importance of breast cancer screening, including CBE. Additionally, women in rural areas may have limited exposure to mass media campaigns or health promotion initiatives that could increase their knowledge about CBE. Secondly, poverty and socioeconomic factors prevalent in rural communities can pose significant barriers to accessing healthcare services, including CBE. Limited financial resources and the cost of transportation to healthcare facilities can prevent women from seeking regular screenings. Moreover, cultural and social factors play a role in CBE utilization among rural women. Women's position within households, feelings of shyness, personal modesty, and embarrassment during breast examinations can discourage them from undergoing CBE.
These findings align with studies conducted in Bangladesh and Pakistan [14, 22], respectively, further emphasizing the impact of rural residency on CBE uptake. Most importantly, barriers that hinder Yemeni women from early detection was that they had no symptoms (84.1%). This finding was consistent with study done in Bangladesh by [14]. The second most barrier in this study was lack of information about breast cancer and its treatment, while the less barriers were family not allowing to go, no screening center and religious reason were reported by 6.3%, 7.9% and 9.5% of women, respectively.
Limitations of study
This study is the first work in Yemen that has assessed the barriers to breast cancer self-examination and early diagnosis. However, there are still some limitations, which include not using randomization sampling and international standardized questionnaires. In addition, the sample size was not large enough, along with a few numbers of hospitals in which this survey was conducted. Thus, the findings may not be able to be generalized to the rest of women in Yemen. Moreover, selection biases are largely expected in this study due to the problem of cross-sectional study method that was used in our study.
Conclusion
In this study, a notable disparity was found between breast cancer awareness and screening behaviors. While participants were familiar with the disease and some symptoms, many lacked understanding of essential screening techniques such as clinical breast examinations and mammograms. Limited knowledge and absence of symptoms were key obstacles to screening. To enhance outcomes for Yemeni women, it is vital to implement educational programs that dispel misconceptions about breast cancer. Leveraging social media platforms presents a promising avenue to expand outreach and boost screening participation rates.
Supplementary Information
Acknowledgements
The authors want to thank the 6th year Pharma-D students at University of Science and Technology, female branch for helping us in collecting data.as well as the administration and medical staff of both hospitals for their effective help.
Transparency statement
Associate Professor. Dr. Faisal Ali, the corresponding author, affirms that this research paper provides a genuine, precise, original and clear description of the conducted study. It ensures that all significant elements of the study have been included and that any deviations from the original plan (and, if applicable, registration) have been adequately clarified.
Author contributions
Othman, G., and Ali, F., have contributed significantly across all aspects of the work, including conception, study design, execution, data acquisition, analysis, interpretation, editing, critically reviewing, and supervision. As a result, they share equal responsibility as the first author. The remaining authors, Maria Mudathira, Heba Almoliky, Maria Al-qahtania, Nora Alezzia, Nosibah Ameena, Doa’a Anwar Ibrahim a, Mohammed Mohammed Battaha, Mohamed Izham Mohamed Ibrahimd. have participated in drafting, data collection, reviewing and have given their final approval for publication. Each author has endorsed the choice of journal for submission and has agreed to assume full accountability for all aspects of the research.
Data availability
Data Availability Statement Data and any further information are available upon reasonable requested.
Declarations
Ethics approval and consent to participate
Our study protocol received ethics approval from the Research Ethics Committee of the Faculty of Pharmacy, University of Science and Technology, Ref: (1445/009). All study participants volunteered to participate and were free to withdraw their participation at any point. No names were identified on the questionnaires, and the responders were involved in the study with verbal consent.
Consent to participate
Informed consent was obtained from all participants prior to the interview.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abdul Hadi M, Hassali MA, Shafie AA, Awaisu A. Knowledge and perception of breast cancer among women of Various ethnic groups in the state of Penang: a cross-sectional Survey. Med Princ Pract. 2010;19(1):61–7. 10.1159/000252837. [DOI] [PubMed] [Google Scholar]
- 2.Alam NE, Islam MS, Ullah H, Molla MT, Shifat SK, Akter S, Aktar S, Khatun MM, Ali MR, Sen TC, Chowdhury K, Pervin R, Mohiuddin AKM. Evaluation of knowledge, awareness and attitudes towards breast cancer risk factors and early detection among females in Bangladesh: a hospital based cross-sectional study. PLoS ONE. 2021;16(9): e0257271. 10.1371/journal.pone.0257271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Naggar RA, Al-Maktari LA, Alshaikhli H, Trafford J, Saleh B, Mossfer SI. Critical assessment of three decades of breast cancer research in Yemen: systematic review. Med Legal Update. 2021. 10.37506/mlu.v21i2.2812. [Google Scholar]
- 4.Al-Najar MS, Nsairat A, Nababteh B, Essam D, Tarawneh D, Alrabadi N, Alzoubi KH. Awareness about breast cancer among adult women in Jordan. SAGE Open. 2021. 10.1177/21582440211058716. [Google Scholar]
- 5.Bawazir A, Bashateh N, Jradi H, Bin Breik A. Breast cancer screening awareness and practices among women attending primary health care centers in the Ghail- Bawazir District of Yemen. Clin Breast Cancer. 2018. 10.1016/j.clbc.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Binhussien BF, Ghoraba M. Awareness of breast cancer screening and risk factors among Saudi females at family medicine department in security forces hospital, Riyadh. J Family Med Prim Care. 2018;7(6):1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biswas S, Syiemlieh J, Nongrum R, Sharma S, Siddiqi M. Impact of educational level and family income on breast cancer awareness among college-going girls in Shillong (Meghalaya), India. Asian Pac J Cancer Prev. 2020;21(1):3639–46. 10.31557/APJCP.2020.21.12.3639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donnelly TT, Khater AH, Al-Bader SB, Al Kuwari MG, Malik M, Al-Meer N, Singh R, Fung T. Factors that influence awareness of breast cancer screening among Arab women in Qatar: results from a cross sectional survey. Asian Pac J Cancer Prev. 2014;15(23):10157–64. 10.7314/apjcp.2014.15.23.10157. [DOI] [PubMed] [Google Scholar]
- 9.Esmail Hassan E, Seedhom AE, Mahfouz EM. Awareness about breast cancer and its screening among Rural Egyptian women, Minia District: a population-based study. Asian Pac J Cancer Prev. 2017;18(6):1623–8. 10.22034/APJCP.2017.18.6.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Francies FZ. Rodney Hull, Richard Khanyile, and Zodwa Dlamini Breast cancer in low-middle income countries: abnormality in splicing and lack of targeted treatment options. Am J Cancer Res. 2020;10(5):1568–91. [PMC free article] [PubMed] [Google Scholar]
- 11.GLOBOCAN: Estimated cancer incidence, mortality and prevalence worldwide; 2022. http://globocan.iarc.fr/Default.aspx Accessed 2–5–2024.
- 12.Huang J, Paul SFC, Veeleah L, Xiao C, Hanyue D, Yinzi J, Jinqiu Y, Xiang-qian L, Zhi-Jie Z, Martin CSW. Global incidence and mortality of breast cancer: a trend analysis. Aging. 2021;13(4):5748–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hussain I, Majeed A, Masood I, Ashraf W, Imran I, Saeed H, Ur Rehman A, Hashmi FK, Saleem F, Akbar M, Chaudhry MO, Ullah J, Rasool MF. A national survey to assess breast cancer awareness among the female university students of Pakistan. PLoS ONE. 2022;17(1): e0262030. 10.1371/journal.pone.0262030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR. Awareness of breast cancer and barriers to breast screening uptake in Bangladesh: a population based survey. Maturitas. 2016;84:68–74. 10.1016/j.maturitas.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Kirubakaran R, Chee Jia T, Mahamad Aris N. Awareness of breast cancer among surgical patients in a tertiary hospital in Malaysia. Asian Pac J Cancer Prev. 2017;18(1):115–20. 10.22034/APJCP.2017.18.1.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parsa P, Kandiah M. Predictors of adherence to clinical breast examination and mammography screening among Malaysian women. Asian Pac J Cancer Prev. 2010;11(3):681–8. [PubMed] [Google Scholar]
- 17.Qedair JT, Al Qurashi AA, Alfayea T, Mortada H, Alsudais A, Almuntashiri S, Hakami AY. Level and predictors of breast cancer awareness among Saudi women: a nationwide study. Womens Health. 2022;18:17455057221133836. 10.1177/17455057221133835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seely JM. Progress and remaining gaps in the early detection and treatment of breast cancer. Curr Oncol. 2023;30(3):3201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talib ZM, Amersi F, Harit AP, Saleh MN. Promoting breast cancer awareness and clinical breast examination in the LMIC: experiences from Tajikistan, Pakistan and Kenya. Cur Breast Cancer Rep. 2019;11:152–7. [Google Scholar]
- 20.Tukasiewicz S, Marcin C, Alicja F, Jacek B, Robert S, Andrzej S. Breast cancer—epidemiology, risk factors, classification, prognostic markers, and current treatment strategies—an updated review. Cancers. 2021;13(17):4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.http://apps.who.int/hpvcentre/statistics/dynamic/ico/country.2008;;pdf/BGD.df?CFID=4005139 & CFTOKEN=50211239 Accessed 28 5 2024.
- 22.Yusoff J, Ismail A, Manaf MRA, Ismail F, Abdullah N, Muhammad R, Suhaimi SNA, Zin RRM. Quality of life of women with breast cancer in a tertiary referral university hospital. Health Qual Life Outcomes. 2022;20(1):15. 10.1186/s12955-022-01921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data Availability Statement Data and any further information are available upon reasonable requested.