Abstract
Objective
This pilot study aimed to assess the feasibility and effectiveness of an auricular acupressure intervention on sleep quality, mood state, and quality of life (QOL) among parents of children with cancer.
Methods
Thirty-five parents were assigned to three-weeks intervention in an active auricular acupressure group (AAG) or a sham auricular acupressure group (SAG). Feasibility was assessed by adherence to the acupressure protocol. Outcomes were measured using the Pittsburgh Sleep Quality Index for sleep quality, the Profile of Mood States for mood, and the QOL short form for QOL. The data were analyzed using generalized estimating equations to identify changes over time within and between the groups.
Results
Adherence to the protocol was 78%. There were no differences between the groups in overall sleep quality or mood state, but QOL in the Physical Component Summary was better in the AAG at time 1. Parents in the AAG exhibited significantly higher levels of vigor compared to those in the SAG group. Statistically significant differences were observed in the Physical Functioning and General Health subscales, with the AAG showing better outcomes than the SAG group at time 1 and time 2, respectively.
Conclusions
Likely due to the small sample size, the AAG and SAG did not differ in overall sleep quality, mood state, or QOL, but there were significant subscale differences that support intervention effectiveness. A fully powered large-scale trial is needed to determine whether this intervention would be effective for parents of children with cancer. Reducing symptom distress and improving QOL in these parents are essential, and interventions to achieve this goal must be tested.
Trial registration
ClinicalTrials.gov NCT05654155.
Keywords: Parents, Sleep quality, Quality of life, Mood, Auricular acupressure
Introduction
While the survival rate for children with cancer has dramatically improved over the past five decades, from 58.0% to 83.0%, the overall incidence rate continues to rise by approximately 0.8% per year among children and adolescents.1 Parents, who are often the primary caregivers, face increased stress due to the responsibility of managing their child's symptoms and medical treatments. Caring for a child with cancer can substantially increase parenting stress.2 Parents face an increased life burden related to fears about their children's potential death and concerns over the symptoms their children experience.3 Consequently, parents of children with cancer commonly experience sleep disturbances,4,5 mood disorders,3,6 and a diminished quality of life (QOL) compared to population norms.2,7
Sleep quality is essential for maintaining both physical and mental health. Studies have indicated that parents of children with chronic conditions, particularly cancer, report significantly poorer sleep quality and efficiency compared to parents of healthy children,8 with prevalence rates of sleep disturbance ranging between 37% and 48%.4,9 Mood disturbances, such as depression and anxiety, are also prevalent in parents of children with cancer.6 In a meta-analysis, van Warmerdam et al., (2019) highlighted substantial mental health challenges, revealing anxiety prevalence rates between 5.0% and 65.0% and depression rates from 7.0% to 91.0%. Furthermore, compared to parents of children without cancer, studies have shown that those with a child battling these disease exhibit markedly higher rates of anxiety and depression10 as well as poor QOL.2,7 Such disturbances in sleep and moods can adversely impact parents’ QOL and health, highlighting the need for targeted interventions in clinical settings.
Auricular acupressure, a therapy rooted in traditional Chinese medicine (TCM), is based on the theory that specific points on the ear correspond to different organs and systems in the body. By stimulating these points, it is believed that energy flow (Qi) in the body can be regulated, which may help restore balance and promote health.11,12 This non-invasive technique has been increasingly adopted in Western medicine and has shown promise in managing sleep disturbances,13, 14, 15 mood distress,16 and QOL17 in various clinical settings. However, despite its potential, the application of auricular acupressure specifically for parents of children with cancer remains underexplored. Therefore, this study aims to (1) assess the feasibility of administering an auricular acupressure intervention to parents of children with cancer and (2) evaluate the effectiveness of the auricular acupressure intervention on sleep quality, mood state, and QOL in parents of children with cancer. Effectiveness will be measured using well-established instruments, including the Pittsburgh Sleep Quality Index, the Profile of Mood States, and the QOL-short-form, to capture changes in these outcomes before and after the intervention in the active auricular acupressure Group (AAG). The data collected will be analyzed to determine the impact of the intervention in the AAG compared to the sham auricular acupressure group (SAG). It is hypothesized that parents in the AAG will experience significant improvements in sleep quality, mood state, and QOL over time compared to those in the SAG.
Methods
Study design and participants
This was a feasibility pilot study conducted using a randomized controlled design (Registration No. NCT05654155 on December 8, 2022) in which participants were randomly assigned to either an active auricular acupressure group (AAG) or a sham auricular acupressure group (SAG). Data were collected at baseline (time 0), 1 week (time 1), 2 weeks (time 2) and 3 weeks (time 3) after the end of the intervention, which was three weeks long. The study used a sham acupressure group as the control to closely replicate the intervention conditions without providing the therapeutic effects of actual auricular acupressure. This approach was designed to isolate the specific effects of the acupressure technique by controlling for placebo effects, which are often significant in interventions involving personal contact and ritual. Additionally, baseline data (time 0) on sleep quality, mood state, and QOL were collected from all participants before any auricular acupressure was administered. This comprehensive baseline assessment allowed for a more accurate evaluation of the intervention's true impact on the parents.
To be included in the study, participants needed to be a parent of a child (under 18 years) who was newly diagnosed with cancer (less than 3 months) and who was receiving treatment with chemotherapy. Parents were excluded if they were (1) receiving any medication or treatment for insomnia, (2) had received any acupuncture or acupressure in the past 3 months, or (3) had ever been diagnosed with other chronic illness (such as cancer, heart disease, or asthma) at the time of data collection. The exclusion of parents with chronic illnesses was intended to increase the homogeneity of the sample, as such conditions could potentially affect sleep and mood. To minimize selection bias, random sampling methods were employed. The inclusion criteria were designed to capture a wide range of demographic and socioeconomic backgrounds, ensuring that the sample was representative of the general population of parents caring for children with cancer.
This study was a single-blind randomized clinical trial. Participants were randomly assigned to either an active AAG or SAG using a sealed envelope. To ensure the randomness of the participant assignment, the researcher prepared an equal number of envelopes labeled “AAG” and “SAG”. Each envelope contained a card indicating the group assignment. To maintain the integrity of the randomization process, the envelopes were thoroughly shuffled and numbered consecutively before distribution. Participants were sequentially enrolled and assigned to groups based on the numbers of these sealed envelopes. The sample size was estimated using G∗Power (version 3.1.9.2). Repeated measures MANOVA (within factors) was selected as the statistical test, with the following parameters: (1) two groups with four measurements, (2) type-α error set at 0.05, (3) power set at 0.80, and (4) a small effect size of 0.25, based on Cohen's guidelines,18 and (5) correlation among repeated measures set at 0.5. The calculated total sample size required for each group was 14 participants. Twenty percent more subjects were added to the sample size to avoid the loss to follow-up of participants; therefore, at least 34 participants were expected to comprise the sample size for this study. As this study was a pilot investigation, the primary goals were to assess the feasibility of the intervention and to collect preliminary data on its effectiveness. Given the exploratory nature of pilot studies, a smaller sample size with fewer than 30 participants per group is considered acceptable and appropriate.19
Intervention: auricular acupressure program
The AAG participants received auricular acupressure three times a day for five days every week for three weeks. Using Dr. Huang's ear reflex theory, our AAG intervention included six acupoints (i.e. shenmen, subcortex, heart, kidney, anxious, and neurasthenia points) that have been demonstrated to be effective in improving sleep and emotional stability.11,12 The shenmen point is known for its sedative properties, which are beneficial for managing insomnia and stabilizing mood. In auricular medicine, both the heart and kidney points are recognized as “blood-activating points,” which are instrumental in energizing and invigorating the body's functions while also calming the spirit. The subcortex point is believed to soothe the nervous system and enhance neuroendocrine function, as well as improve sleep quality and mood stability. Additionally, the anxious and neurasthenia points help alleviate nervous exhaustion and boost mental energy, thereby enhancing the overall QOL, improving sleep quality, and stabilizing mood.11,12 In contrast, the participants in the SAG received the same protocol of auricular acupressure as the AAG, but six other acupoints were used near the treated acupoints: sacroiliac, neck, stomach, wrist, tonsil, and tongue. These points were selected specifically because they lack the functions associated with altering blood circulation or calming the spirit and thus were not expected to impact the participants' sleep and mood states.11,12 The intervention was conducted by a researcher who had completed an auricular acupressure training course taught by Dr. Huang,11 a medical doctor and certified auricular therapist.
Both acupressure interventions began by cleaning the earlobe using 75.0% alcohol. Then, a small piece of adhesive tape with vaccaria seeds, which provided pressure at specific points was taped onto each selected auricular acupoint on a participant's ear. To enhance the efficacy of stimulating the selected auricular acupoint, each piece of adhesive tape was equipped with two vaccaria seeds, following the recommendation of Dr. Huang, who was the President of the Auricular Medicine International Research & Training Center in Florida.11 Next, the researcher demonstrated the acupoints press technique to the participants. The participants were asked to press one acupoint slightly to more firmly for 1 minute until they felt discomfort or tingling, and then to move to the next acupoint until all six acupoints were completed. The ear seed tapes were kept in place for 5 days and then removed by the participant for 2 days. After the 2-day rest period, the participant returned to the researcher to have the ear tapes replaced. Unilateral auricular points were used for the intervention and the treatment was changed to the other ear every week until the 3-week intervention was completed. To minimize biases in the study, all auricular acupressure interventions, for both the AAG and SAG, were administered by the same researcher. To control for potential biases arising from the researcher not being blinded to the intervention, both groups received identical instructions on the acupressure technique, ensuring that the only variable was the location of the acupoints.
Measures
Demographic and child-related data
Demographic data for both parents and children were collected using a standardized questionnaire to ensure consistency and accuracy across all participants. The demographic data for the parents included variables such as age, education level, socioeconomic status, and religious affiliation, while the child-related data encompassed age, gender, and type of cancer. The collection of these data was crucial for understanding the context in which parents were experiencing sleep disturbances, mood changes, and QOL issues. Additionally, by including these data, we aimed to explore the potential discrepancies between the parents in the AAG and the SAG that could influence the study outcomes.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a widely validated multidimensional measure that assesses individuals' sleep quality across seven factors: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. The PSQI differentiates “poor” from “good” sleep over the past month. A global sum score of 5 or more indicates a poor sleeper. This measure was selected for the study due to its strong reliability (Cronbach's α of 0.83 and test–retest correlation coefficient of 0.85) and validity across diverse populations, making it particularly suitable for evaluating the sleep quality of parents under stress, such as those caring for children with cancer.20 Given that the data collection in this study occurred at baseline and weekly after the intervention, the PSQI instructions were modified to reflect sleep quality over the past week instead of the past month.
Profile of Mood State-Brief Form (POMS-BF)
The 30-item POMS-BF, a shorter version of the original POMS,21 was developed to investigate individuals' mood status. Participants responded to each item on a Likert-type scale ranging from 0 (not at all) to 4 (extremely), with higher scores indicating greater intensity of the respective mood states. The POMS-BF was chosen for its comprehensive assessment of mood status through six factors: tension, depression, anger, vigor, fatigue, and confusion. The POMS-BF has been used in a variety of populations in past studies and has been translated into Chinese, and its reliability and validity have been reported as sound.22,23 Chen et al. (2002) found that the Chinese version of the POMS-BF had excellent reliability, with Cronbach's α ranging from 0.98 to 0.99, and confirmed its construct validity through factor analysis.23
Quality of Life Short-Form 36 (QOL-SF)
The QOL-SF was utilized to measure the QOL of parents of children with cancer because of its comprehensive coverage of both the physical and mental health aspects. The QOL-SF is a health survey with 36 items, originally developed to measure the generic health and well-being of the general population.24 A total of eight domains comprise the QOL-SF, including Physical Functioning (PF), Role Limitation to Physical Problem (RP), Body Pain (BP), General Health (GH), Vitality (VT), Social Functioning (SF), Role Limitation to Emotion Problem (RE), and Mental Health (MH). The participants responded to each item on a Likert-type scale ranging from 1 to 3–6, depending on the item. Scores were calculated using Quality Metric PRO CoRE software to ensure the reliability and accuracy of the results. First, the raw scores of the QOL-SF were transformed to scores ranging from 0 (worst health state) to 100 (best health state), following the guidelines provided in the QOL-SF User's Manual.25 This transformation is standard practice for normalizing scores and making them comparable across different studies. Then, each domain of the QOL-SF score was further transformed into T scores using the standard score formulas to allow the results of this study to be meaningfully compared with other studies.
The eight domains of the QOL-SF can be summarized into two measures: Physical Component Score (PCS) and Mental Component Score (MCS). The higher the score in each domain of the QOL-SF, the better the QOL the parents perceived. The reliability and validity of the QOL-SF have been well established by empirical research.25
Feasibility assessment
The feasibility of the auricular acupressure intervention was assessed through the following key metrics: recruitment rate, retention rate, and adherence rate. The recruitment rate was determined by the proportion of eligible participants who agreed to join the study. The retention rate was calculated as the proportion of completed data collection points out of all possible data collection points. The adherence rate was measured by monitoring the consistency with which participants followed the prescribed acupressure protocol, specifically, the number of days the auricular seeds were kept in place as instructed.
Procedures
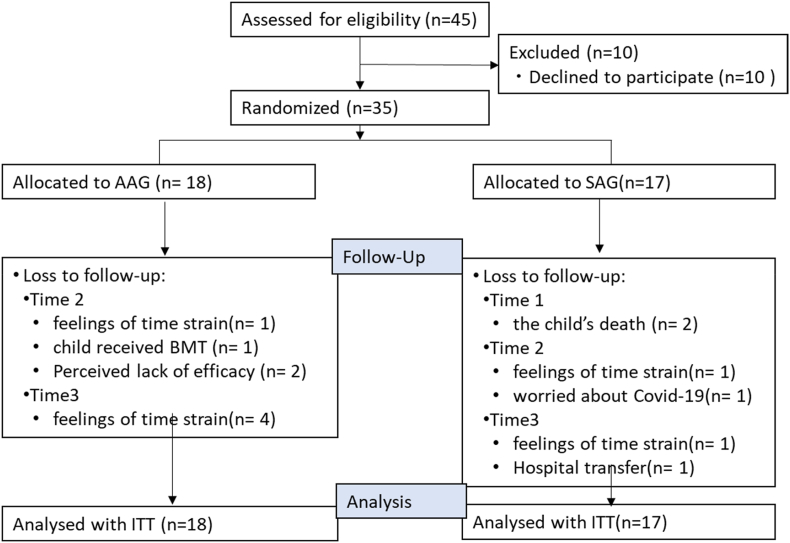
The participants were then randomly assigned to one of two groups: AAG or SAG. Before implementing the auricular acupressure program, all participants completed baseline (time 0) data collection. The participants then received appropriate treatment for the arm of the study to which they were assigned. Outcome data were collected weekly following five consecutive days of auricular acupressure during the three-week intervention. A trained data collector, who was not involved in administering the acupressure, conducted the data collection for the study. Fig. 1 shows the flow chart of the study.
Fig. 1.
Flow chart of this study. AAG, auricular acupressure group; SAG, sham auricular acupressure group; ITT, intention to treat analysis.
Data analysis
An intention to treat analysis (ITT) was performed, meaning that data from all participants, including those who dropped out of the study, were analyzed according to the group to which they were originally assigned. This approach helps preserve the randomization process and reduces the bias associated with non-completion. To assess the effectiveness of the auricular acupressure intervention over time, generalized estimating equations (GEE) were utilized for data analysis using SPSS statistical software, version 28.0 (IBM SPSS, Armonk, NY: IBM Corp). Descriptive were employed to analyze longitudinal continuous measurements. The GEE model included the effects of the group (AAG or SAG), time (measured across four time points), and their interaction (group ∗ time). Additionally, baseline scores for each specific outcome were included as covariates in the model to control for initial differences, thereby reducing selection bias and improving the precision of the estimates. GEE was chosen for its robustness to missing data, as it can include subjects in the analysis using all available data points, even when some time points are missing.26 Additionally, the data were assessed for normality and were deemed appropriate for GEE analysis. Model effects were tested with the Wald χ2 test at a significance level of P < 0.05. Post hoc tests were performed using Fisher's test of least significant difference (LSD). Other secondary analyses included descriptive statistics for baseline characteristics, Chi-square tests for categorical variables, and t-tests for continuous variables. These tests were used to explore potential baseline differences between the groups and to provide a comprehensive understanding of the data.
Ethical considerations
A hospital institutional review board at Chang Gung Memorial Hospital approved the study to ensure that ethical regulations and standards were met before it was conducted. The data collection procedure strictly followed the regulations for protecting subject confidentiality established by the hospital had established. A trained data collector approached eligible participants from a medical center in northern Taiwan. After the participants received verbal and written explanations about the study design and were asked whether they were willing to participate, they signed a consent form if they agreed to participate.
Results
Characteristics of participants
We recruited a total of 35 parents of children with cancer for this study; 18 were assigned to the AAG and 17 to the SAG (Table 1). The AAG included 16 mothers and 2 fathers, with a mean age of 35.67 ± 5.57 years. In this group, most had at least a high school education (44.4%, n = 8) and over 66% reported low socioeconomic levels. About 61.1% of the parents had religious beliefs. In the SAG, comprised of 14 mothers and 3 fathers, the mean age was 37.06 ± 6.91 years. Most had a high school education (52.9%, n = 9), and about 64.7% reported a low socioeconomic level. Almost 58.8% of the parents reported that they had no religious beliefs. There were no significant differences in any demographic data for parents between the AAG and the SAG.
Table 1.
Characteristic of the sample of parents and their children who have cancer (N = 35).
| Variable | AAG (n = 18) |
SAG (n = 17) |
Significant | ||
|---|---|---|---|---|---|
| n (%) | Mean ± SD | n (%) | Mean ± SD | ||
| Parents | |||||
| Age (year)a | 35.67 ± 5.77 | 37.06 ± 6.91 | 0.521 | ||
| Educationb | 0.597 | ||||
| High school | 8 (44.4) | 9 (52.9) | |||
| Undergraduate | 7 (38.9) | 7 (41.2) | |||
| Graduate | 3 (16.7) | 1 (5.9) | |||
| Socioeconomic statusb | 0.903 | ||||
| Medium to high | 6 (33.3) | 6 (35.3) | |||
| Low to lowest | 12 (66.7) | 11 (64.7) | |||
| Religiousb | 0.238 | ||||
| No | 7 (38.9) | 10 (58.8) | |||
| Yes | 11 (61.1) | 7 (41.2) | |||
| Children | |||||
| Age (year)a | 5.05 ± 3.39 | 6.32 ± 5.90 | 0.447 | ||
| Sexb | 0.625 | ||||
| Boy | 11 (61.1) | 9 (52.9) | |||
| Girl | 7 (38.9) | 8 (47.1) | |||
| Diseaseb | 0.833 | ||||
| ALL-SR | 6 (33.3) | 6 (35.3) | |||
| ALL-HR & VHR | 9 (50.0) | 7 (41.2) | |||
| Solid tumor | 3 (16.7) | 4 (23.5) | |||
AAG, active auricular acupressure group; SAG, sham acupressure group; SD, standard deviation; ALL-SR, acute lymphoblastic leukemia-standard risk; ALL-HR, acute lymphoblastic leukemia-high risk; ALL-VHR, acute lymphoblastic leukemia-very high risk.
Continuous variable reported mean and standard deviation (SD).
Categorical data reported n and percentage (%).
Among the children, there were 7 girls and 11 boys represented in the AAG. The mean age of the patients was 5.05 ± 3.39 years. The most common disease diagnosis was acute lymphoblastic leukemia (83.3%). In the SAG, there were 8 girls and 9 boys with cancer represented. The mean age of the patients was 6.32 ± 5.90 years. Acute lymphoblastic leukemia was the most common diagnosis (76.5%). There were no differences in any demographic data for children whose parents were assigned to the AAG and the SAG.
The feasibility of the auricular acupressure intervention in parents of children with cancer
A total of 45 parents were approached to participate in the study, and 35 (77.8%) agreed to join. Each participant completed baseline and three follow-up data collections during this 3-week auricular acupressure program. In total, 140 data collection points were scheduled (35 parents at 4 time points). During the treatment phase, two parents withdrew at time 1 following the loss of their child. Six other parents discontinued the program for different reasons: their children received a bone marrow transplant (BMT, n = 1), the parents' feelings of time strain (n = 2), or the parents’ worries about Covid-19 (n = 1). In addition, two parents who thought the intervention was ineffective dropped out at time 2. At time 3 (final data collection point), six parents dropped out because their child was transferred to a different hospital (n = 1) or due to their experience of time strain (n = 5). Thus, in total, we collected data for 116 of the 140 possible data collection points. The retention rate for this study was 82.9% (Fig. 1).
During the intervention period, parents in both the AAG and the SAG were asked to keep the auricular seeds taped on their ears for 3 weeks, 5 days each week. Thus, the possible total number of days the seeds should have been taped on the ears of these 35 parents was 525. This possible number was determined by multiplying 35 (parents) times 15 days (3 weeks, 5 days a week). Although some of the parents complained that they felt tingling while they pressed the acupoint seeds, all parents who participated in and completed the auricular acupressure program kept the seeds tape on their ears continually for 3 weeks. Therefore, the actual total number of days that the tapes were on the parents’ ears was 410 or 78.1% of the possible days. This suggests that the intervention was feasible and acceptable to the parents of children with cancer.
The effects of articular acupressure on sleep, mood state, and quality of life among parents of children with cancer
The effects of auricular acupressure on overall sleep, mood state, and QOL among parents of children with cancer are presented in Table 2. The results indicate no statistically significant differences between the AAG and the SAG in sleep quality, mood state, or total QOL after the treatments were completed. However, parents in the AAG showed a better QOL in the Physical Component Summary (PCS) of the QOL-SF than parents in the SAG at time 1.
Table 2.
The effects of auricular acupressure on sleep, mood state, and QOL among parents of children with cancer (N = 35).
| Variable | PSQI |
POMS |
PCS (QOL) |
MCS (QOL) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exp(B) | 95% CI | P | B | SE | P | B | SE | P | B | SE | P | |
| Intercept | 4.67 | 1.34–16.24 | 0.015 | 27.94 | 5.65 | < 0.001 | 54.18 | 1.37 | 0.000 | 36.31 | 2.46 | 0.000 |
| Group | ||||||||||||
| Experimental | 0.75 | 0.14–3.98 | 0.736 | −11.05 | 6.65 | 0.096 | 1.04 | 1.88 | 0.579 | 2.74 | 3.08 | 0.374 |
| Time | ||||||||||||
| Time 1 | 0.47 | 0.12–1.87 | 0.281 | −3.07 | 5.54 | 0.580 | −2.95∗ | 1.31 | 0.025 | 2.13 | 1.54 | 0.166 |
| Time 2 | 1.15 | 0.20–6.43 | 0.877 | −2.87 | 5.21 | 0.582 | −2.31 | 1.94 | 0.233 | 2.39 | 1.79 | 0.183 |
| Time 3 | 0.41 | 0.12–1.44 | 0.164 | −6.42 | 4.90 | 0.190 | −2.68 | 2.14 | 0.211 | 3.21∗ | 1.50 | 0.032 |
| Time∗group | ||||||||||||
| AAG∗Time 1 | 1.59 | 0.29–8.86 | 0.594 | 4.29 | 6.82 | 0.529 | 4.52∗∗ | 1.72 | 0.008 | −2.26 | 2.40 | 0.347 |
| AAG∗Time 2 | 0.34 | 0.05–2.35 | 0.275 | −0.34 | 6.64 | 0.960 | 2.55 | 2.36 | 0.280 | 0.06 | 2.40 | 0.981 |
| AAG∗Time 3 | 1.28 | 0.29–5.60 | 0.742 | 6.01 | 6.68 | 0.368 | 3.08 | 2.51 | 0.219 | −0.81 | 2.05 | 0.694 |
∗P < 0.05, ∗∗P < 0.01.
AAG, active auricular acupressure group; B, estimated parameter; SE, standard error; PSQI, The Pittsburgh Sleep Quality Index; POMS, Profile of Mood State; PCS, Physical Component Summary; MCS, Mental Component Summary; QOL, quality of life.
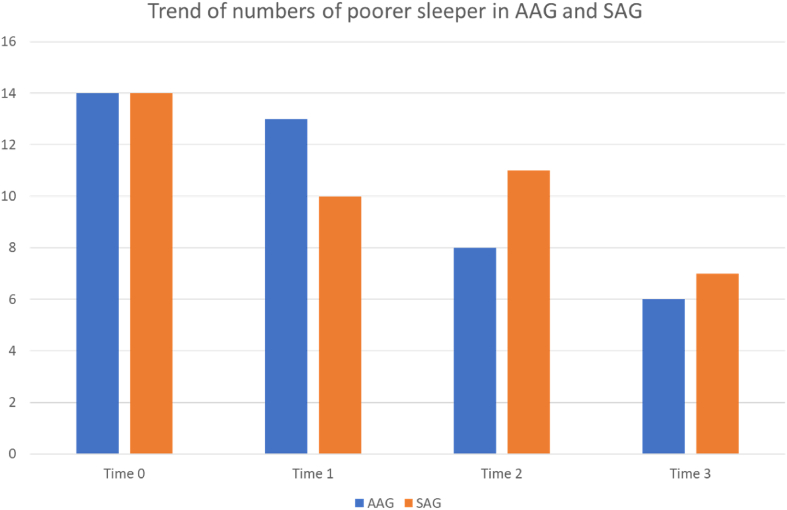
There were no differences in sleep quality between the groups, and the distribution of parents with poor sleep in both the AAG and the SAG is presented in Fig. 2. The total number of parents reporting poor sleep in both the AAG and the SAG gradually decreased over time. However, the reduction in sleep problems was more pronounced in the AAG, with fewer parents in this group reporting poor sleep at time points 2 and 3 compared to those in the SAG.
Fig. 2.
Trend of numbers of poorer sleeper in AAG and SAG across time among parents of children with cancer. AAG, active auricular acupressure group; SAG, sham acupressure group; Time 0, baseline data collection which is pre-intervention; Time 1, 1-week after intervention; Time 2, 2-week after intervention; Time 3, 3-week after intervention.
We further examined the effects of auricular acupressure on each domain of mood state (POMS-SF) among parents of children with cancer, as shown in Table 3. Parents in the AAG group exhibited significantly higher levels of “vigor” compared to those in the SAG group (χ2 = 7.72, P = 0.005). However, there were no statistically significant differences between the two groups in the other mood state domains.
Table 3.
The effects of auricular acupressure on mood state among parents of children with cancer (N = 35).
| Variable | Tension |
Depression |
Anger |
Vigor |
Fatigue |
Confusion |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | P | B | SE | P | B | SE | P | B | SE | P | B | SE | P | B | SE | P | |
| Intercept | 5.82 | 1.24 | < 0.001 | 4.59 | 1.23 | < 0.001 | 4.88 | 1.36 | < 0.001 | 2.59 | 0.77 | < 0.001 | 7.88 | 1.27 | < 0.001 | 7.35 | 0.80 | 0.000 |
| Group | ||||||||||||||||||
| AAG | −1.55 | 1.45 | 0.285 | −1.64 | 1.35 | 0.224 | −0.88 | 1.53 | 0.564 | 3.58∗∗ | 1.29 | 0.005 | −2.55 | 1.58 | 0.106 | −0.85 | 1.03 | 0.406 |
| Time | ||||||||||||||||||
| Time 1 | −0.72 | 1.31 | 0.583 | 0.58 | 1.35 | 0.669 | −0.25 | 1.42 | 0.861 | 0.93 | 0.68 | 0.170 | −1.35 | 1.18 | 0.252 | −0.27 | 0.71 | 0.703 |
| Time 2 | −0.64 | 1.31 | 0.623 | −0.33 | 1.19 | 0.782 | −0.04 | 1.40 | 0.978 | 1.68 | 1.24 | 0.175 | 0.11 | 1.12 | 0.921 | −0.08 | 0.84 | 0.928 |
| Time 3 | −1.45 | 1.12 | 0.195 | −0.97 | 1.12 | 0.386 | −0.77 | 1.23 | 0.534 | −0.33 | 0.70 | 0.641 | −2.34 | 1.24 | 0.058 | −0.92 | 0.71 | 0.195 |
| Time∗group | ||||||||||||||||||
| AAG∗T1 | 1.11 | 1.46 | 0.449 | −0.19 | 1.53 | 0.903 | 0.42 | 1.69 | 0.806 | −0.65 | 1.16 | 0.574 | 2.41 | 1.58 | 0.128 | −0.23 | 0.90 | 0.798 |
| AAG∗T2 | 0.00 | 1.53 | 0.998 | 0.23 | 1.50 | 0.879 | 0.26 | 1.74 | 0.883 | −0.10 | 1.61 | 0.952 | 0.11 | 1.53 | 0.940 | −0.85 | 0.99 | 0.391 |
| AAG∗T3 | 1.78 | 1.54 | 0.249 | 0.84 | 1.40 | 0.549 | 1.08 | 1.69 | 0.524 | 0.62 | 1.25 | 0.617 | 3.02 | 1.67 | 0.070 | −0.73 | 0.94 | 0.440 |
∗∗P <0.01.
AAG, active auricular acupressure group; B, estimated parameter; SE, standard error.
The effects of auricular acupressure on each domain of QOL in the parents of children with cancer are shown in Table 4. Parents in the AAG showed better PF in the QOL-SF compared to parents in the SAG at time 1. Additionally, parents in the AAG reported better GH at time 2 compared to those in the SAG.
Table 4.
The effects of auricular acupressure on quality of life among parents of children with cancer (N = 35).
| Variable | PF |
RP |
BP |
GH |
VT |
SF |
RE |
MH |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | |
| Intercept | 52.70 | 1.29 | 45.40 | 1.55 | 51.82 | 1.93 | 47.62 | 1.97 | 44.91 | 2.46 | 43.77 | 1.85 | 38.15 | 2.17 | 38.71 | 2.41 |
| Group | ||||||||||||||||
| Experimental | 1.01 | 1.53 | −0.72 | 2.50 | 4.22 | 2.46 | 2.21 | 3.05 | 2.41 | 3.05 | 1.31 | 2.85 | 2.35 | 3.06 | 2.86 | 2.98 |
| Time | ||||||||||||||||
| Time 1 | −2.08∗ | 0.96 | −1.09 | 1.81 | −0.72 | 1.41 | −3.14 | 1.69 | 0.71 | 1.99 | −1.51 | 1.26 | 2.26 | 1.34 | 1.18 | 1.92 |
| Time 2 | −2.33 | 2.06 | 0.59 | 2.50 | 0.64 | 2.34 | −4.42∗∗ | 1.35 | −0.74 | 1.84 | 0.39 | 1.82 | 2.93 | 2.35 | 0.58 | 2.37 |
| Time 3 | −1.70 | 1.98 | −2.23 | 2.28 | 1.23 | 2.50 | −3.52 | 2.24 | 1.06 | 1.80 | 1.45 | 1.90 | −0.55 | 2.09 | 3.49 | 1.96 |
| Time∗group | ||||||||||||||||
| AAG∗T1 | 2.72∗ | 1.12 | 3.09 | 2.85 | 1.98 | 2.09 | 3.69 | 2.36 | −0.38 | 2.81 | 3.18 | 2.43 | −1.09 | 2.73 | −2.48 | 2.55 |
| AAG∗T2 | 2.45 | 2.23 | 1.50 | 3.71 | 0.24 | 2.74 | 5.16∗ | 2.26 | 3.43 | 2.69 | 1.59 | 2.76 | 0.79 | 3.18 | 0.48 | 2.87 |
| AAG∗T3 | 1.42 | 2.15 | 4.37 | 3.32 | 0.41 | 2.86 | 4.72 | 3.10 | 0.44 | 2.97 | 0.48 | 2.89 | 4.11 | 2.85 | −1.73 | 2.52 |
∗P < 0.05, ∗∗P < 0.01.
AAG, active auricular acupressure group; B, estimated parameter; SE, standard error; PF, Physical Functioning; RP, Role Limitation to Physical Problem; BP, Body Pain; GH, General Health; VT, Vitality; SF, Social Functioning; RE, Role Limitation to Emotion Problem; MH, Mental Health.
Discussion
Previous studies have demonstrated the effectiveness of auricular acupressure interventions on sleep,27 mood,28 and QOL29 in various populations, such as cancer patients and students; however, research in pediatric oncology settings remains limited. This study contributes to the existing body of knowledge by providing evidence that auricular acupressure, a non-invasive and practical intervention, can benefit sleep quality, mood state, and QOL in the parents of children with cancer. Unlike other interventions such as exercise30 and relaxation techniques,31 which can be time-consuming and often require guidance from health care providers, auricular acupressure offers a more accessible and convenient option for parents. Once the seeded tapes were applied, the participants could easily continue the treatment independently at home. As our study results indicated an adherence rate of 78% to the protocol, this suggests that auricular acupressure is not only a safe procedure but also an effective self-care strategy for managing the psychological and physical burdens faced by parents of children with cancer. This finding aligns with and expands upon existing research,32 demonstrating the feasibility of auricular acupressure as an effective intervention for parents facing the stress of caring for a child with cancer.
The effects of auricular acupressure on sleep quality have shown mixed results in previous studies. While some researchers have identified auricular acupressure as an effective and safe intervention for improving sleep quality in cancer patients,13,33 others have found no significant association between the intervention and a reduction in sleep problems.34 In our study, we observed a trend toward a reduction in the number of parents reporting poor sleep in the AAG, but this trend did not reach statistical significance. The lack of significant findings may be attributed to the small sample size in this pilot study, which limited the statistical power to detect differences. Future research with a larger sample size is needed to more conclusively examine the efficacy of auricular acupressure on sleep quality in parents of children with cancer. By expanding the sample size, future studies could better assess the potential benefits and address the inconsistencies observed in previous research.
Previous research has indicated that auricular acupressure can positively affect mood states, such as reducing depression and anxiety.35 However, unlike some prior studies, our research did not find significant differences between the AAG and the SAG in the overall mood state or in the specific domains of mood, except for “vigor”. Our results are consistent with the findings of Lin et al. (2021), who demonstrated that auricular acupressure could alleviate cancer-related fatigue in lung cancer patients undergoing chemotherapy,36 helping individuals feel more energetic, lively, and enthusiastic. One possible explanation for the limited effects observed in our study could be the short duration of the intervention. An integrative review of acupressure interventions for older adults found that the duration of these interventions varied from 10 days to 1 year, with 4 weeks being common.35 In our study, we recruited parents of children who were newly diagnosed with cancer (less than 3 months) for a 3-week intervention. This period is particularly stressful for parents, as they face uncertainty about their child's disease and treatment while also dedicating significant time to caring for and supporting their children. We suggest that future studies consider extending the length of the intervention to at least 4–6 weeks and potentially conducting the intervention during the maintenance phase of the child's cancer treatment (at least 4–6 months after diagnosis) when parents may be more settled and have a better understanding of their child's treatment options.
Auricular acupressure therapy focuses on restoring the balance of a person's energy, known as Qi, which flows throughout the body and is essential for maintaining overall health.12 Auricular acupoints are believed to correspond to internal organs, and when these points are stimulated, it can help regulate energy imbalances, potentially leading to improved health.12 Improved health status often results in better QOL and indeed, auricular acupressure has been shown to improve QOL.28,29 Consistent with these findings, our study showed that parents in the AAG experienced better QOL in the PCS as well as in the PF and GH subscales at time 1 (1 week) and time 2 (2 weeks), respectively.
Several limitations of this study should be acknowledged. As a pilot study, the small sample size (35 parents) limited our ability to detect potential differences that may have been present. While the high homogeneity of our study population, with over 80% of children diagnosed with acute lymphoblastic leukemia (ALL), helped reduce variability and strengthen the internal consistency of our findings, it also represented a limitation by potentially limiting the generalizability of the results. The overall survival rate for ALL is approximately 90.0%, which is higher than that of other cancers such as acute myeloid leukemia (68.0%) and certain solid tumors, including brain tumors (74.0%) and osteosarcoma (68.0%).1 Since the disease and treatment status of a child can significantly impact parental QOL,37 it is important to consider including a more diverse range of cancer diagnoses in any large-scale trial of auricular acupressure in the future. Additionally, although we controlled for baseline scores for each specific outcome to minimize initial differences between the two groups and to reduce selection bias, the significant intercepts in each model suggest that baseline differences may still have influenced the results. This indicates the need for further refinement of the study design and statistical modeling in future research.
Conclusions
This pilot study demonstrated the feasibility of an auricular acupressure intervention for parents of children with cancer. While the small sample size limited the ability to detect significant differences in overall sleep quality and mood state between the groups, the intervention showed promising results in improving QOL in the PCS and specific subscales. These findings suggest that auricular acupressure may be a viable, non-invasive strategy to enhance the physical aspects of QOL for parents in highly stressful caregiving roles. In clinical practice, auricular acupressure could be considered a complementary therapy to support parents’ physical well-being, potentially easing the burden associated with caring for a child with cancer. However, further research with a larger sample size is necessary to fully determine the effectiveness of this therapy in improving sleep, mood, and overall QOL.
Ethics statement
The study was approved by the institutional review board of Chang Gung Memorial Hospital (IRB No. 201702205B0), and all participants provided written informed consent prior to participation.
Funding
This study was supported by grants from the Ministry of Science and Technology Taiwan (Grant Nos. 101-2314-B-255-002-MY2, 105-2314-B-255 -004) and the Chang Gung Medical Research Fund (Grant Nos. CMRPF1H0081, BMRPA63). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
CRediT authorship contribution statement
Chiang, Yi-Chien: Conceptualization, Methodology, Formal analysis, Investigation, Writing, Supervision, and Funding acquisition. Chen, Shih-Hsiang: Conceptualization, Methodology, and Writing; Moser, Debra K.: Writing Original Draft, Review, and Editing. Wen, Yu-Chuan: Conceptualization, Resources, and Investigation. Lin, Yu-Ting: Conceptualization, Resources, and Investigation. Hsiao, Ya-Chu: Conceptualization, Methodology, Formal analysis, and Writing. All authors had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Data availability statement
The data cannot be made publicly available as they include sensitive information that could potentially compromise the confidentiality of the research participants.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the authors used ChatGPT to check grammar. After using the tool, the authors reviewed and edited the content as necessary and take full responsibility for the final content of the publication.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank all the participants for their kind cooperation.
References
- 1.American Cancer Society Cancer Facts and Figures 2022. 2022. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2022.html
- 2.Morhun J.M., Racine N.M., Guilcher G.M.T., Tomfohr-Madsen L.M., Schulte F.S.M. Health-related quality of life and well-being in parents of infants and toddlers with cancer. Curr Oncol. 2020;27(2):e206–e215. doi: 10.3747/co.27.4937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Qadire M., Aloush S., Alkhalaileh M., Qandeel H., Al-Sabbah A. Burden among parents of children with cancer in Jordan: prevalence and predictors. Cancer Nurs. 2020;43(5):396–401. doi: 10.1097/NCC.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 4.Zupanec S., Jones H., Stremler R. Sleep habits and fatigue of children receiving maintenance chemotherapy for ALL and their parents. J Pediatr Oncol Nurs. 2010;27(4):217–228. doi: 10.1177/1043454209358890. [DOI] [PubMed] [Google Scholar]
- 5.Meltzer L.J., Sanchez-Ortuno M.J., Edinger J.D., Avis K.T. Sleep patterns, sleep instability, and health related quality of life in parents of ventilator-assisted children. J Clin Sleep Med. 2015;11(3):251–258. doi: 10.5664/jcsm.4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collins M.L.Z., Bregman J., Ford J.S., Shields C.L. Depression, anxiety, and stress in parents of patients with retinoblastoma. Am J Ophthalmol. 2019;207:130–143. doi: 10.1016/j.ajo.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Eche I.J., Aronowitz T., Shi L., McCabe M.A. Parental uncertainty: parents' perceptions of health-related quality of life in newly diagnosed children with cancer. Clin J Oncol Nurs. 2019;23(6):609–618. doi: 10.1188/19.CJON.609-618. [DOI] [PubMed] [Google Scholar]
- 8.Clement-Carbonell V., Portilla-Tamarit I., Rubio-Aparicio M., Madrid-Valero J.J. Sleep quality, mental and physical health: a differential relationship. Int J Environ Res Public Health. 2021;18(2):460. doi: 10.3390/ijerph18020460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rensen N., Steur L.M.H., Schepers S.A., et al. Concurrence of sleep problems and distress: prevalence and determinants in parents of children with cancer. Eur J Psychotraumatol. 2019;10(1) doi: 10.1080/20008198.2019.1639312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Warmerdam J., Zabih V., Kurdyak P., et al. Prevalence of anxiety, depression, and posttraumatic stress disorder in parents of children with cancer: a meta-analysis. Pediatr Blood Cancer. 2019;66(6) doi: 10.1002/pbc.27677. [DOI] [PubMed] [Google Scholar]
- 11.Huang L.C. Auricular International Research & Training; Orlando, FL: 2005. Auricular Medicine: A Complete Manual of Auricular Diagnosis and Treatment. [Google Scholar]
- 12.Huang L.C., Huang W.S. Orlando FL: Auricular International Research & Training; 2007. Handbook of Auricular Treatment Prescriptions & Formulae. [Google Scholar]
- 13.Lu H.B., Ma R.C., Yin Y.Y., et al. Auricular acupressure for improving sleep quality in patients with lung cancer: a systematic review and meta-analysis. Holist Nurs Pract. 2022;36(4):E27–E37. doi: 10.1097/HNP.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y., Zhang J., Jin Y., Zhang Q. Auricular acupressure therapy for patients with cancer with sleep disturbance: a systematic review and meta-analysis. Evid Based Comple Alternat Med. 2021;2021 doi: 10.1155/2021/3996101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu D.J., Dong H.C., Tang T.N., Zhu S.F. Acupressure for insomnia: a protocol for systematic review and meta-analysis. Medicine (Baltim) 2018;97(45) doi: 10.1097/MD.0000000000013180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bang Y.Y., Park H. Effects of auricular acupressure on the quality of sleep and anxiety in patients undergoing cardiac surgery: a single-blind, randomized controlled trial. Appl Nurs Res. 2020;53 doi: 10.1016/j.apnr.2020.151269. [DOI] [PubMed] [Google Scholar]
- 17.Chou Y.H., Yeh M.L., Huang T.S., Hsu H. Acupoint stimulation improves pain and quality of life in head and neck cancer patients with chemoradiotherapy: a randomized controlled trial. Asia Pac J Oncol Nurs. 2022;9(1):61–68. doi: 10.1016/j.apjon.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen J. Lawrence Erlbaum Associates; New York, NY: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 19.Hertzog M.A. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–191. doi: 10.1002/nur.20247. [DOI] [PubMed] [Google Scholar]
- 20.Buysse D.J., Reynolds CF 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 21.Mcnair D.M., Lorr M., Droppleman L.F. Educational and Industrial Testing Services; San Diego, CA: 1971. Manual for the Profile of Mood States. [Google Scholar]
- 22.Shacham S. A shortened version of the profile of mood states. J Pers Assess. 1983;47(3):305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- 23.Chen K.M., Snyder M., Krichbaum K. Translation and equivalence: the profile of mood states short form in English and Chinese. Int J Nurs Stud. 2002;39(6):619–624. doi: 10.1016/s0020-7489(01)00068-2. [DOI] [PubMed] [Google Scholar]
- 24.Ware J.E., Jr., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Maruish M.E. Quality Metric Incorporated; Lincoln, RI: 2011. User's Manual for the SF-36v2 Health Survey. [Google Scholar]
- 26.Lin L., Jing X., Zhang Y., et al. Factors influencing compliance with auricular acupressure therapy in patients with cancer-related fatigue. Patient Prefer Adherence. 2020;14:1275–1281. doi: 10.2147/ppa.S261466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chueh K.H., Chang C.C., Yeh M.L. Effects of auricular acupressure on sleep quality, anxiety, and depressed mood in RN-BSN students with sleep disturbance. J Nurs Res. 2018;26(1):10–17. doi: 10.1097/jnr.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 28.Yin X.J., Wang F., Lin G.P., Gong X.L., Yao M.Y. Effects of auricular acupressure on depression in stroke patients: a single-blind randomized controlled trial. Complement Ther Clin Pract. 2022;48 doi: 10.1016/j.ctcp.2022.101596. [DOI] [PubMed] [Google Scholar]
- 29.Vallim E.T.A., Marques A., Coelho R., et al. Auricular acupressure in the quality of life of women with breast cancer: a randomized clinical trial. Rev Esc Enferm USP. 2019;53 doi: 10.1590/S1980-220X2018043603525. [DOI] [PubMed] [Google Scholar]
- 30.Halliday G.C., Miles G.C.P., Marsh J.A., Kotecha R.S., Alessandri A.J. Regular exercise improves the well-being of parents of children with cancer. Pediatr Blood Cancer. 2017;64(12) doi: 10.1002/pbc.26668. [DOI] [PubMed] [Google Scholar]
- 31.Pouraboli B., Poodineh Z., Jahani Y. The effect of relaxation techniques on anxiety, fatigue and sleep quality of parents of children with leukemia under chemotherapy in South East Iran. Asian Pac J Cancer Prev. 2019;20(10):2903–2908. doi: 10.31557/APJCP.2019.20.10.2903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu T.T., Pan H.W., Kuo H.C., et al. Concomitant benefits of an auricular acupressure intervention for women with cancer on family caregiver sleep quality. Cancer Nurs. 2021;44(5):E323–e330. doi: 10.1097/ncc.0000000000000842. [DOI] [PubMed] [Google Scholar]
- 33.Yoon H.G., Park H. The effect of auricular acupressure on sleep in breast cancer patients undergoing chemotherapy: a single-blind, randomized controlled trial. Appl Nurs Res. 2019;48:45–51. doi: 10.1016/j.apnr.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 34.Wan Q., Luo S., Wang X., et al. Association of acupuncture and auricular acupressure with the improvement of sleep disturbances in cancer survivors: a systematic review and meta-analysis. Front Oncol. 2022;12 doi: 10.3389/fonc.2022.856093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hmwe N.T.T., Browne G., Mollart L., Allanson V., Chan S.W. An integrative review of acupressure interventions for older people: a focus on sleep quality, depression, anxiety, and agitation. Int J Geriatr Psychiatry. 2019;34(3):381–396. doi: 10.1002/gps.5031. [DOI] [PubMed] [Google Scholar]
- 36.Lin L., Zhang Y., Qian H.Y., et al. Auricular acupressure for cancer-related fatigue during lung cancer chemotherapy: a randomised trial. BMJ Support Palliat Care. 2021;11(1):32–39. doi: 10.1136/bmjspcare-2019-001937. [DOI] [PubMed] [Google Scholar]
- 37.Litzelman K., Catrine K., Gangnon R., Witt W.P. Quality of life among parents of children with cancer or brain tumors: the impact of child characteristics and parental psychosocial factors. Qual Life Res. 2011;20(8):1261–1269. doi: 10.1007/s11136-011-9854-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data cannot be made publicly available as they include sensitive information that could potentially compromise the confidentiality of the research participants.