Abstract
Diabetes is a prevalent metabolic condition with substantial health and economic impacts. Therefore, effective and accessible indicators are essential for early detection and prevention. This study investigates the link between the waist-to-calf circumference ratio (WCR) and diabetes risk in a large cohort from the Longevity Check-Up (Lookup) 8+ Study. The present investigation is a retrospective cross-sectional study. Diabetes was defined either as self-reported diagnosis, or fasting plasma glucose equal to or greater than 126 mg/dL, or random plasma glucose equal to or greater than 200 mg/dL. The WCR was calculated by dividing waist circumference by calf circumference. A total population of 8900 participants (mean age 57.1 ± 14.8 years, 55% women) was included in the study. The prevalence of diabetes was 9.4%. Mean WCR displayed a significant trend (p for trend < 0.001), and the analysis of covariance (ANCOVA) revealed significant differences among the normal, pre-diabetes, diabetes groups. Unadjusted logistic regression showed a positive association between higher WCR and diabetes, which remained significant in the adjusted models. Receiver operating characteristic curve analysis indicated that WCR had a higher area under the curve compared to waist circumference alone, with cut-off values of 2.35 for men and 2.12 for women providing high sensitivity (91% for men, 92% for women) and specificity (74% for men, 75% for women). Our study introduces WCR as a novel, simple, and cost-effective anthropometric measure for identifying individuals at risk of diabetes, suitable for clinical use, especially in resource-limited settings.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-79329-8.
Keywords: Body composition, Metabolic syndrome, Obesity, Lifestyle, Cardiovascular risk, Waist circumference, Muscle mass, Anthropometric measures
Subject terms: Diabetes, Disease prevention
Introduction
Diabetes has emerged as a significant global health challenge1. Because the prevalence of diabetes continues to rise, there is a growing need to identify effective and accessible indicators that can aid in the early detection and prevention of this condition2,3.
Both diabetes and metabolic syndrome are complex conditions that involve a combination of factors, including insulin resistance, obesity, and abnormal lipid profiles4–7. Among them, central obesity is a well-established risk factor for both diabetes and metabolic syndrome, since visceral fat is metabolically active and contributes to insulin resistance and inflammation, two key components of those conditions8,9. For the above reason, anthropometric measurements which offer insights into body composition and distribution of fat and muscle have gained attention as potential markers of diabetes risk and cardiometabolic complications10–14. The waist-to-calf circumference ratio (WCR) has emerged as a potential indicator of these conditions due to its ability to capture different aspects of body composition15,16. The WCR is calculated as the ratio between waist circumference (WC) and calf circumference (CC). The WC has been shown to be a reliable and valid indicator of abdominal fat mass17, while the CC represents a proxy for total lean mass18,19. Therefore, WCR expresses the relationship between abdominal adiposity and body muscle mass20. A higher WCR could indicate a greater proportion of abdominal fat relative to muscle mass, potentially signifying an increased risk for insulin resistance and related metabolic disturbances21.
Despite growing evidence on the relationship between WCR and different health outcomes, the association between the WCR and diabetes has been relatively underexplored. To address this gap, the present study aimed to better understand the potential correlation between WCR and diabetes risk in a large cohort of community-dwelling adults of all ages enrolled in the Longevity Check-Up (Lookup) 8+.
Materials and methods
The present investigation is a retrospective cross-sectional study using data from the Lookup 8+ project (previously Longevity Check-up 7+). Lookup8+ is an ongoing initiative endorsed by the Department of Geriatrics of the Università Cattolica del Sacro Cuore and the Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS (Rome, Italy). The primary aim of Lookup 8+ is to foster the adoption of healthier lifestyles within the general population. The Lookup 8+ protocol obtained ethical approval from the Ethics Committee of Università Cattolica del Sacro Cuore (protocol #: A.1220/CE/2011) and is comprehensively documented elsewhere22. All participants provided written informed consent prior to enrollment. The manuscript was prepared according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) reporting guidelines for observational studies23.
Study sample
Between June 1st, 2015, and September 30th, 2023, a total of 17,934 individuals were recruited in public places and events. To provide a thorough geographical depiction of mainland Italy and its principal islands, cities of different sizes were selected. In major cities such as Rome, Naples, Catania, Genoa, Bologna and Milan, multiple initiatives were conducted to ensure a comprehensive representation of the sociodemographic traits of the population in different areas. To be considered for inclusion in Lookup 8+, candidates had to meet the minimum age requirement of 18 years and provide informed written consent. Exclusion criteria encompassed self-reported pregnancy, inability to perform physical performance tests, refusal of capillary blood testing to measure total cholesterol and glycemia, and inability/unwillingness to provide written informed consent. For the current investigation, the analysis focused on participants who completed a comprehensive anthropometric evaluation, which included measurements of both waist and calf circumferences.
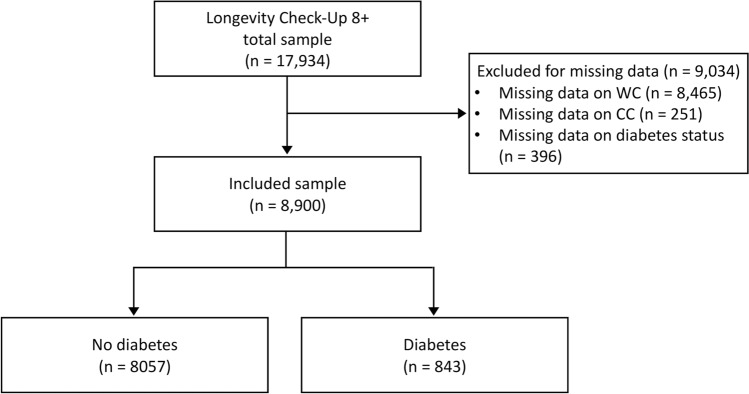
Following the exclusion of participants with missing data in the variables of interest, namely WC (n = 8465), CC (n = 251), and diabetes status (n = 396), the final analyzed cohort comprised 8900 participants (Fig. 1). In certain cases, participants had missing data in more than one area, which explains why the total number of persons with unavailable data outnumbers the number of removed participants.
Fig. 1.
Flowchart of the study sample selection. CC calf circumference, WC waist circumference.
Data collection
Participants underwent comprehensive evaluations, encompassing a brief questionnaire, objective measurements of cardiovascular health indicators, and measurement of anthropometric variables. The assessment of cardiovascular health metrics included the administration of a lifestyle habits questionnaire and a brief evaluation that included blood pressure measurement and point-of-care tests for total cholesterol and blood glucose20.
Smoking status was categorized into three groups: current smoker (individuals who have smoked at least 100 cigarettes in their lifetime and currently smoke), never smoked (individuals who have never smoked or have smoked less than 100 cigarettes in their lifetime), and former smoker (individuals who have smoked at least 100 cigarettes in their lifetime but stopped within 28 days of the interview). For the analysis, smoking status was classified as either present or never/former smoker. Body weight was measured using an analog medical scale, while body height was determined through a standard stadiometer. The body mass index (BMI) was derived by dividing weight (in kilograms) by the square of height (in meters). The operational definition of a healthy diet was established as a daily intake of at least three servings (~ 400 g) of fruits and/or vegetables20. The daily consumption of fruits and vegetables was determined using reference tables provided by the Italian Society of Nutrition (SINU) specifically designed for the Italian population24. Fruit and vegetable servings were used as a proxy for the quality of the dietary pattern, providing an indirect measure of overall diet quality in the analyses25,26. Regular engagement in physical activity or exercise was defined as participating in activities for a minimum of 30 min, at least twice a week, over the preceding year. Respondents were asked “Within the past year, have you partaken in physical activity or exercise for a minimum of 30 min, at least twice a week? If your answer is affirmative, please include details about the specific activity”. The assessed activities comprised: (a) low intensity walking for physical exertion, (b) running, cycling, or swimming, and (c) resistance training with or without stretching exercises. Participants were categorized into different groups based on their responses: (a) inactive (not participating in at least 30 min of physical activity or exercise twice a week), (b) light walkers, (c) engaged in running, cycling, or swimming, (d) engaged in strength training with or without stretching, and (e) engaged in light walking along with any other form of physical exercise. The categorization was selected to recognize the distinction between physical activity, such as walking, and physical exercise in terms of their composition and level of exertion27,28. For the analysis, participants were categorized as physically active or inactive. The measurement of total cholesterol was conducted using disposable strips and a reflectometric system, with a portable instrument (MultiCare-In, Biomedical Systems International srl, Florence, Italy)29. Blood pressure was measured with an electronic sphygmomanometer according to recommendations from European guidelines30. Blood glucose was tested from capillary blood samples using disposable strips based on an amperometric system using a MultiCare-In portable device29. Based on the current guidelines by the American Diabetes Association, individuals who self-reported diabetes, had a fasting blood glucose level of 126 mg/dL or greater, or had a random blood glucose equal to or greater than 200 mg/dL, were classified as having diabetes31. To further evaluate the variation of WCR across the diabetes spectrum, individuals with a fasting blood glucose level between 100 and 125 mg/dL or a random blood glucose level between 140 and 199 mg/dL were classified as having pre-diabetes31.
Waist and calf circumference assessment
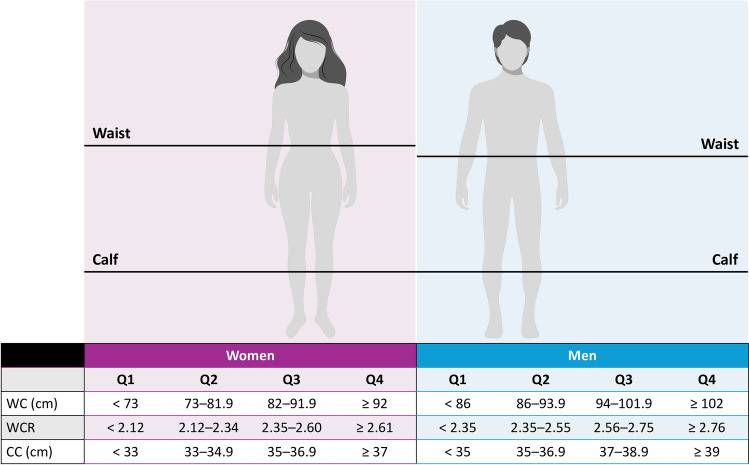
Anthropometric measurements were assessed using a non-stretchable pliable plastic tape. To measure WC, participants were asked to stand with their feet aligned closely together. WC was measured at the point of narrowest space between the ribs and hips at the end of a normal expiration. The measuring tape was placed with a comfortable tightness, ensuring it did not apply force on the skin32. The measurement of CC was conducted with participants in a sitting position, with knees and ankles at right angles and feet resting on the floor. The measurements were obtained at the point of greatest circumference on the right calf, perpendicular to its length, without applying pressure to the underlying skin layers. If the calf was covered by clothes, participants were requested to remove them. The measurements were approximated to the closest 0.1 cm33. The WCR was then calculated by dividing WC by CC. Quartiles for WC, CC, and WCR were calculated separately for men and women, as shown in Fig. 2.
Fig. 2.
Quartiles of cut-off values for waist circumference, calf circumference and waist-to-calf circumference ratio according to sex. CC calf circumference, WC waist circumference, WCR waist-to-calf circumference ratio.
Statistical analyses
The characteristics of the study participants were summarized using descriptive statistics, according to the diagnosis of diabetes. Continuous variables were presented as mean values ± standard deviation, while categorical variables were displayed as absolute numbers and percentages. The statistical significance of differences in means and proportions was evaluated using t-tests and chi-squared tests, respectively. Adjusted and unadjusted odds ratios (ORs) for the association between WCR quartiles and diabetes, along with their 95% confidence intervals (CIs), were computed by logistic regression models. Variables possibly linked to diabetes were incorporated into the models. The final analyses were thus fine-tuned through successive adjustments: initially for age (Model 1); subsequently for age, healthy diet, and physical activity (Model 2); and finally, for age, healthy diet, physical activity, BMI, blood pressure, and blood cholesterol (Model 3). To assess the predictive ability of WCR (independent variable) toward increased risk of diabetes (dependent variable), receiver operating characteristic (ROC) curves were constructed. The resulting area under the curve (AUC) was reported, and the sensitivity and specificity at the respective WCR thresholds were calculated. To compare the mean values of WCR between individuals with diabetes, pre-diabetes, and no diabetes, an analysis of covariance (ANCOVA) was conducted. For all tests, statistical significance was set as p < 0.05. All statistical analyses were conducted using the SPSS software (version 11.0, SPSS Inc., Chicago, IL).
Results
Mean age of the 8900 participants was 57.1 ± 14.8 years (range: 18–98), with 4882 (55%) women. The prevalence of diabetes was 9.4% (843/8900) and was significantly higher in men than in women. The main characteristics of participants stratified by the diagnosis of diabetes are presented in Table 1. Individuals diagnosed with diabetes had lower levels of physical activity and were less likely to adhere to a healthy diet compared with those without diabetes. Furthermore, participants living with diabetes had higher BMI, systolic and diastolic blood pressure, and serum glucose levels. Conversely, blood cholesterol concentrations were higher among participants without diabetes. Notably, individuals with diabetes had significantly greater WC than those without diabetes, whereas CC did not differ significantly between groups. WCR values were higher among participants with diabetes than in those without diabetes. Further analyses were conducted to compare the mean WCR among subjects with diabetes, pre-diabetes, and no diabetes. The results showed significant differences in the mean values of WCR across the groups, with an average WCR of 2.4 ± 0.33 in individuals without diabetes, 2.6 ± 0.33 in individuals with pre-diabetes, and 2.7 ± 0.33 in diabetic individuals. The statistical analysis indicated a significant trend (p for trend < 0.001). An ANCOVA was conducted to examine the differences in WCR levels among individuals with normal glycemic status, pre-diabetes and diabetes, while controlling for age, sex, healthy diet, and physical activity (Supplementary Table 1). The results indicate a significant difference in WCR among the three groups [F(2, 8750) = 71.468, p < 0.001]. Age, sex, diet, and physical activity were also significant covariates. The adjusted means for WCR were 2.4 ± 0.33, 2.6 ± 0.33, and 2.8 ± 0.35, for normal glycemic status, pre-diabetes and diabetes, respectively. These findings suggest a progressive increase in WCR with worsening glycemic status.
Table 1.
Characteristics of study population according to the diagnosis of diabetes.
| Characteristics | Total sample (n = 8900) |
Diabetes (n = 843) |
No diabetes (n = 8,057) |
p |
|---|---|---|---|---|
| Age (years) | 57.1 ± 14.8 | 65.8 ± 13.1 | 56.2 ± 14.7 | < 0.001 |
| < 65 years | 6024 (68) | 356 (42) | 5668 (68) | |
| ≥ 65 years | 2876 (32) | 487 (58) | 2389 (32) | |
| Sex | < 0.001 | |||
| Men | 4018 (45) | 465 (55) | 3553 (44) | |
| Women | 4882 (55) | 378 (45) | 4504 (56) | |
| Active smoking | 1765 (20) | 169 (20) | 1596 (20) | 0.44 |
| Healthy diet | 5505 (62) | 547 (65) | 4958 (61) | 0.02 |
| Physically active | 5216 (59) | 405 (47) | 4811 (60) | < 0.001 |
| BMI (kg/m2) | 24.8 ± 4.0 | 26.7 ± 4.8 | 24.6 ± 3.9 | < 0.001 |
| Blood cholesterol (mg/dL) | 194.9 ± 36.2 | 187.6 ± 37.1 | 195.7 ± 36.0 | < 0.001 |
| Blood glucose (mg/dL) | 105.4 ± 23.7 | 150.4 ± 40.7 | 100.7 ± 14.8 | < 0.001 |
| Systolic blood pressure (mmHg) | 124.9 ± 16.2 | 129.9 ± 16.6 | 124.3 ± 16.1 | < 0.001 |
| Diastolic blood pressure (mmHg) | 76.1 ± 9.9 | 76.9 ± 9.8 | 75.9 ± 9.9 | 0.01 |
| Waist circumference (cm) | 88.3 ± 13.5 | 96.6 ± 14.5 | 87.5 ± 13.1 | < 0.001 |
| Calf circumference (cm) | 35.9 ± 3.5 | 36.1 ± 3.9 | 35.9 ± 3.4 | 0.07 |
| Waist-to-calf circumference ratio | 2.5 ± 0.3 | 2.7 ± 0.3 | 2.4 ± 0.3 | < 0.001 |
Data are reported as absolute value (percentage) for age group, sex, smoking status, healthy diet, and physical activity. All other variables are shown, means ± standard deviation. Healthy diet: consumption of at least three portions (≥ 400 g) of fruit and/or vegetables per day. Physically active: physical exercise at least twice a week. BMI body mass index. Measured values are reported for systolic blood pressure, diastolic blood pressure, blood cholesterol and blood glucose.
Figure 3 depicts the prevalence of diabetes among male and female participants, stratified by quartiles of WC and CC. The highest prevalence of diabetes was observed among individuals in the higher WC quartile and lower CC quartiles. Conversely, the lower prevalence of diabetes was found among participants in the lower WC quartiles and higher CC quartiles. This pattern was consistent in both men and women.
Fig. 3.
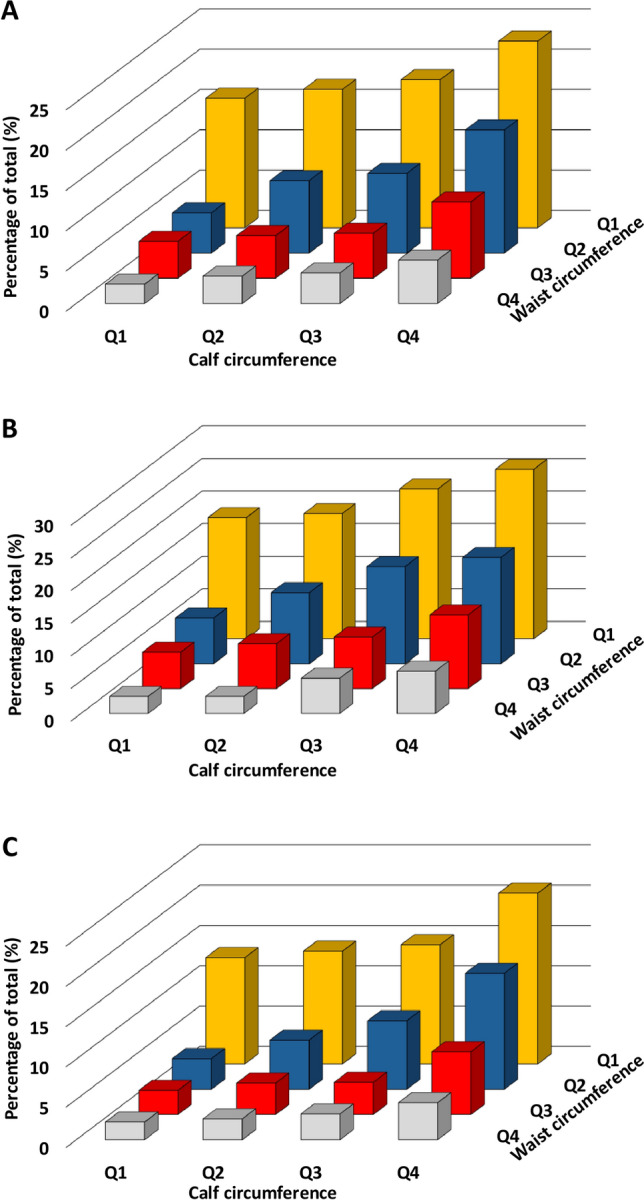
Diabetes prevalence across waist circumference (WC) and calf circumference (CC) quartiles in the total sample (A), men (B), and women (C). The X-axis shows the quartiles of WC (progressing from Q1, the lowest, to Q4, the highest) alongside quartiles of CC (from Q1 to Q4 in increasing order). Each bar represents the percentage of individuals with diabetes within each specific combination of WC and CC quartiles. The direction of progression in diabetes rate can be observed for both WC and CC across the quartiles.
Table 2 shows the results of unadjusted and adjusted logistic regression models. In the unadjusted analysis, a significant positive association between higher WCR and the likelihood of diabetes was observed in both men (OR 5.41; 95% CI 3.85–7.58) and women (OR 6.85; 95% CI: 4.72–9.95). The association remained statistically significant after adjusting for potential confounding factors such as age, healthy diet, physical activity, BMI, blood pressure, and cholesterol level. In the fully adjusted model, participants in higher quartiles of WCR had greater risk of having diabetes compared with those in lower quartiles (OR 1.78; 95% CI 1.16–2.73 for men and OR 3.37; 95% CI 2.09–5.44 for women).
Table 2.
Crude and adjusted odds ratio of diabetes and 95% confidence intervals in the study population.
| Unadjusted | Model 1 | Model 2 | Model 3 | |
|---|---|---|---|---|
| Odds ratio (95% confidence interval) | ||||
| Men | ||||
| WCR quartiles | ||||
| Q1 | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Q2 | 1.92 (1.32–2.78) | 1.34 (0.91–1.96) | 1.27 (0.89–1.86) | 1.21 (0.79–1.83) |
| Q3 | 2.78 (1.94–3.98) | 1.59 (1.09–2.32) | 1.49 (1.02–2.18) | 1.35 (0.89–2.05) |
| Q4 | 5.41 (3.85–7.58) | 2.60 (1.80–3.75) | 2.33 (1.60–3.39) | 1.78 (1.16–2.73) |
| Age | 1.04 (1.03–1.05) | 1.04 (1.03–1.05) | 1.03 (1.02–1.04) | |
| Healthy diet | 1.08 (0.88–1.34) | 1.02 (0.81–1.28) | ||
| Physical activity | 0.75 (0.60–0.92) | 0.84 (0.67–1.06) | ||
| BMI (kg/m2) | 1.06 (1.03–1.10) | |||
| Systolic blood pressure (mmHg) | 1.01 (1.00–1.01) | |||
| Diastolic blood pressure (mmHg) | 0.98 (0.97–1.02) | |||
| Cholesterol (mg/dL) | 0.99 (0.99–0.99) | |||
| Women | ||||
| WCR quartiles | ||||
| Q1 | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Q2 | 1.53 (0.98–2.38) | 1.24 (0.79–1.94) | 1.26 (0.80–1.99) | 1.28 (0.78–2.11) |
| Q3 | 2.83 (1.89–4.22) | 1.96 (1.29–2.97) | 1.96 (1.28–2.99) | 1.91 (1.20–3.05) |
| Q4 | 6.85 (4.72–9.95) | 3.92 (2.62–5.88) | 3.81 (2.52–5.76) | 3.37 (2.09–5.44) |
| Age | 1.03 (1.02–1.04) | 1.03 (1.02–1.04) | 1.03 (1.02–1.04) | |
| Healthy diet | 0.98 (0.77–1.25) | 0.92 (0.71–1.18) | ||
| Physical activity | 0.80 (0.64–0.99) | 0.83 (0.65–1.05) | ||
| BMI (kg/m2) | 1.04 (1.01–1.07) | |||
| Systolic blood pressure (mmHg) | 1.00 (0.99–1.01) | |||
| Diastolic blood pressure (mmHg) | 1.00 (0.98–1.01) | |||
| Cholesterol (mg/dL) | 0.99 (0.99–0.99) | |||
WCR waist-to-calf ratio.
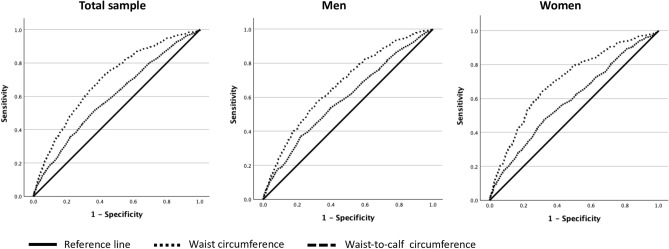
ROC curve analysis was conducted to assess the predictive capacity of WCR. The results demonstrated that AUCs were greater for WCR compared to WC alone (Fig. 4). In men, a WCR cut-off value of 2.35 had 91% and 74% sensitivity and specificity, respectively. In women, a WCR cut-off value of 2.12 had 92% and 75% sensitivity and specificity, respectively.
Fig. 4.
Receiver operating characteristic curve analysis for predicting diabetes according to waist circumference and waist-to-calf circumference ratio. Areas under the curve: total sample, WC = 0.59, WCR = 0.70; men, WC = 0.59; WCR = 0.67; women, WC = 0.59; WCR = 0.70.
Discussion
The aim of the present study was to examine the association between WCR and diabetes in a large sample of community-dwelling individuals of varying age groups. Our findings revealed that participants with greater WC and smaller CC had a significantly higher prevalence of diabetes. Conversely, those with smaller WC and greater CC exhibited a lower prevalence of diabetes. Logistic regression models showed a significant association between a higher WCR and increased odds of diabetes in both men and women, which remained statistically significant after adjusting for multiple potential confounders. ROC curve analysis demonstrated that WCR was a better predictor of diabetes than WC alone, with cut-off values of 2.35 in men and 2.12 in women providing high sensitivity and specificity. These findings contribute to the growing body of evidence on the association between body composition evaluated using anthropometric measures and metabolic disorders. To the best of our knowledge, this is the first study to demonstrate an association between high WCR values and diabetes.
Abdominal fat is recognized as a causal factor for cardiometabolic disorders, whereas muscle mass has a protective effect15. Additionally, muscle mass plays a crucial role in glucose metabolism and overall metabolic health. Indeed, sarcopenia has been linked to insulin resistance and an increased risk of metabolic syndrome and cardiovascular complications14,34,35. Simultaneously assessing WC and CC may provide more precise information about individual phenotypes than WC or CC alone. Individuals with high abdominal adiposity and low muscle mass have a heightened susceptibility to developing metabolic and cardiovascular diseases compared with those with contrasting phenotypes or elevated abdominal fat mass alone. Indeed, the simultaneous presence of obesity and sarcopenia has been associated with increased prevalence of metabolic alterations36, as well as cardiometabolic complications, including increased risk of cardiovascular events, diabetes, and diabetic nephropathy than isolated sarcopenia or obesity37. Ramirez-Velez et al.38 demonstrated that muscle-to-fat ratio is a reliable predictor of cardiometabolic complications since early adulthood. Moreover, a greater WCR was linked to an increased risk of cardiovascular and non-cardiovascular mortality39. Hence, appraising the relationship between adiposity and skeletal muscle mass may be crucial in evaluating cardiovascular risk.
Another relevant finding of our study is the higher risk of diabetes in women compared to men, which may be attributed to a combination of several factors. Women often exhibit higher body fat percentages and distinct fat distribution patterns compared to males40. Hormonal differences, particularly the decrease in estrogen levels during menopause, can exacerbate visceral fat accumulation and increase diabetes risk40,41. Furthermore, gender-specific metabolic responses to fat accumulation and differences in lifestyle and behavioral factors may also play a role42,43. However, it is important to consider that these findings may be influenced by other unmeasured confounding factors such as socioeconomic status, genetic predisposition, and differences in access to healthcare and health-seeking behavior.
The association between the WCR and cardiometabolic complications is an area of growing research interest. Studies exploring the association between WCR and diabetes/metabolic syndrome have shown promising results. Both diabetes and metabolic syndrome are complex conditions that involve a combination of factors, including insulin resistance, obesity, and abnormal lipid profiles4. The WCR, which takes into account abdominal fat distribution and muscle mass, has emerged as a potential indicator of these conditions due to its ability to capture the relationships between different aspects of body composition. Wu et al.15 demonstrated that implementing both CC and WCR in the definition of metabolic syndrome was associated with higher risk of cardiovascular compared to the conventional criteria. The combination of metabolic syndrome with low CC showed the strongest association with inflammation15, which represents a significant factor contributing to cardiovascular risk44–46. In the same study, the coexistence of metabolic syndrome and elevated WCR was found to be associated with an augmented insulin resistance15. In patients with diabetes, a greater WCR was associated with carotid artery atherosclerosis16,47 and non-alcoholic fatty liver disease48. Finally, in older adults, WCR was positively associated with frailty49, as well as impaired cognition50,51, and decreased health-related quality of life52. Further investigations are needed to establish the exact nature of this relationship, considering factors like age, sex, ethnicity, and additional confounding variables.
Although this study presents intriguing findings, it is essential to acknowledge its potential limitations. First, the cross-sectional design precludes the establishment of causality between greater WCR and diabetes risk. Second, a substantial proportion of individuals were excluded from the study because of missing data in the variables of interest. Despite attempts to restrict the time of assessments to a manageable extent, persons were evaluated while participating in retail activities or attending social gatherings. Therefore, participants frequently opted to terminate the evaluation prior to the completion of data collection. However, the primary characteristics of persons with missing data were not different from those who were included in the study. Moreover, the large sample size helped minimize the influence of participant exclusion on the validity of results. Third, WC and CC serve as surrogate markers for abdominal fat mass and peripheral lean mass, respectively. However, WC and CC have demonstrated to be reliable predictors of body adiposity53 and muscle mass54,55. Additionally, we cannot ascertain whether the observed inverse association between diabetes and changes in WCR should be attributed to a protective effect of increased lean mass, reduced abdominal fat mass, or both. This underscores the need for further investigation utilizing longitudinal study designs and imaging techniques such as dual X-ray absorptiometry, computed tomography, or magnetic resonance imaging for a more accurate estimation of muscle mass and fat distribution. Fourth, information on specific medications or medical conditions was not available. The collection of a thorough medical history would have excessively increased the duration of assessments, rendering them unsuitable for the non-traditional settings in which the study was conducted. Further research is necessary to address this limitation and to appraise the impact of clinical characteristics on the correlation between WCR and diabetes. Fifth, the impact of fat or lean mass distribution on metabolic and diabetes diseases may vary across diverse populations. Our study was conducted exclusively in Italy and virtually included only Caucasians, limiting the generalizability of our findings to other ethnic groups. Sixth, the sample period encompasses a duration of eight years, including the occurrence of the COVID-19 pandemic. This event had the potential to impact lifestyle and health patterns, possibly leading to changes in the incidence of metabolic diseases and body composition56. Nevertheless, these variables do not impact the cross-sectional association between anthropometric parameters and diabetes risk, which remains the primary focus of our investigation; however, we acknowledge it as a possible limitation. Seventh, our study only included individuals living in the community; therefore, findings may not be generalizable to other settings. Eighth, no socioeconomic characteristics were collected in our investigation. Socioeconomic disparities are associated with increased cardiometabolic risks57. Additionally, the willingness of individuals to participate in health campaigns and screening activities is significantly influenced by socioeconomic vulnerability, income, and education58. To minimize obstacles to participation, all check-ups were provided free of charge during events that were open to the public and held in easily accessible places. Furthermore, as previously mentioned, our research was conducted in cities of varying sizes and within diverse areas within larger cities to guarantee a comprehensive representation of sociodemographic characteristics.
Conclusions
Findings from the present study indicate that WCR may be a valuable and practical anthropometric index for identifying individuals with diabetes. Its potential as an indicator of diabetes and metabolic syndrome risk lies in its ability to offer insights into both abdominal fat distribution and muscle mass. As research in this area progresses, an understanding of this relationship has the potential to enhance risk assessment and implement targeted interventions for these prevalent metabolic conditions. Healthcare professionals can utilize measurements of waist and calf circumferences to identify individuals at an elevated risk of these health complications, thereby enabling the implementation of tailored interventions to mitigate risks and promote metabolic health. Furthermore, readily accessible measurements empower individuals to make informed lifestyle choices, which contributes to their overall well-being and potentially to healthier and longer lives.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The article processing charge was funded by the Italian Ministry of Health (Ricerca Corrente 2024).
The Look-Up 8+ Study Group is composed as follows:
Steering Committee: Francesco Landi, Roberto Bernabei
Coordination: Emanuele Marzetti, Riccardo Calvani, Luca Mariotti
Writing Panel: Stefano Cacciatore, Hélio José Coelho-Junior, Francesca Ciciarello, Vincenzo Galluzzo, Anna Maria Martone, Anna Picca, Andrea Russo, Sara Salini, Matteo Tosato
Field investigators: Gabriele Abbatecola, Clara Agostino, Fiorella Ambrosio, Francesca Banella, Carolina Benvenuto, Damiano Biscotti, Vincenzo Brandi, Maria Modestina Bulla, Caterina Casciani, Lucio Catalano, Camilla Cocchi, Giuseppe Colloca, Federica Cucinotta, Manuela D’Angelo, Mariaelena D’Elia, Federica D’Ignazio, Daniele Elmi, Marta Finelli, Francesco Pio Fontanella, Domenico Fusco, Ilaria Gattari, Giordana Gava, Tommaso Giani, Giulia Giordano, Rossella Giordano, Francesca Giovanale, Simone Goracci, Silvia Ialungo, Rosangela Labriola, Elena Levati, Myriam Macaluso, Luca Marrella, Claudia Massaro, Rossella Montenero, Maria Vittoria Notari, Maria Paudice, Martina Persia, Flavia Pirone, Simona Pompei, Rosa Ragozzino, Carla Recupero, Antonella Risoli, Stefano Rizzo, Daria Romaniello, Giulia Rubini, Barbara Russo, Stefania Satriano, Giulia Savera, Elisabetta Serafini, Annalise Serra Melechì, Francesca Simeoni, Sofia Simoni, Chiara Taccone, Elena Tagliacozzi, Roberta Terranova, Salvatore Tupputi, Matteo Vaccarella, Emiliano Venditti, Chiara Zanchi, Maria Zuppardo.
The article processing charge was funded by the Italian Ministry of Health (Ricerca Corrente 2024). The Look-Up 8+ Study Group is composed as follows: Steering Committee: Francesco Landi, Roberto Bernabei Coordination: Emanuele Marzetti, Riccardo Calvani, Luca Mariotti Writing Panel: Stefano Cacciatore, Hélio José Coelho-Junior, Francesca Ciciarello, Vincenzo Galluzzo, Anna Maria Martone, Anna Picca, Andrea Russo, Sara Salini, Matteo Tosato Field investigators: Gabriele Abbatecola, Clara Agostino, Fiorella Ambrosio, Francesca Banella, Carolina Benvenuto, Damiano Biscotti, Vincenzo Brandi, Maria Modestina Bulla, Caterina Casciani, Lucio Catalano, Camilla Cocchi, Giuseppe Colloca, Federica Cucinotta, Manuela D’Angelo, Mariaelena D’Elia, Federica D’Ignazio, Daniele Elmi, Marta Finelli, Francesco Pio Fontanella, Domenico Fusco, Ilaria Gattari, Giordana Gava, Tommaso Giani, Giulia Giordano, Rossella Giordano, Francesca Giovanale, Simone Goracci, Silvia Ialungo, Rosangela Labriola, Elena Levati, Myriam Macaluso, Luca Marrella, Claudia Massaro, Rossella Montenero, Maria Vittoria Notari, Maria Paudice, Martina Persia, Flavia Pirone, Simona Pompei, Rosa Ragozzino, Carla Recupero, Antonella Risoli, Stefano Rizzo, Daria Romaniello, Giulia Rubini, Barbara Russo, Stefania Satriano, Giulia Savera, Elisabetta Serafini, Annalise Serra Melechì, Francesca Simeoni, Sofia Simoni, Chiara Taccone, Elena Tagliacozzi, Roberta Terranova, Salvatore Tupputi, Matteo Vaccarella, Emiliano Venditti, Chiara Zanchi, Maria Zuppardo.
Abbreviations
- ANCOVA
Analysis of covariance
- AUC
Area under the curve
- BMI
Body mass index
- CC
Calf circumference
- CI
Confidence interval
- OR
Odds ratio
- ROC
Receiver operating characteristic
- WC
Waist circumference
- WCR
Waist-to-calf circumference ratio
Author contributions
S.C., A.M.M., and F.L. conceptualized the study. R.C. and E.M. developed the methodology. M.T. and V.G. performed the validation. F.C., G.G., and C.M. conducted the investigation. S.C., A.M.M., and F.L. prepared the original draft of the manuscript. S.C., A.M.M., and F.L. prepared Figs. 1, 2, 3, 4. R.C. and E.M. reviewed and edited the manuscript. E.M. and F.L. acquired funding. F.L. supervised the project. All authors read, reviewed, and approved the final version of the manuscript.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of the research participants.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Università Cattolica del Sacro Cuore, Rome, Italy (protocol #A.1220/CE/2011).
Consent for publication
Informed consent was obtained from all subjects involved in the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Stefano Cacciatore and Anna Maria Martone.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Stefano Cacciatore, Email: stefano.cacciatore01@icatt.it.
Francesco Landi, Email: francesco.landi@policlinicogemelli.it.
The Lookup 8+ Study Group:
Francesco Landi, Roberto Bernabei, Emanuele Marzetti, Riccardo Calvani, Luca Mariotti, Stefano Cacciatore, Hélio José Coelho-Junior, Francesca Ciciarello, Vincenzo Galluzzo, Anna Maria Martone, Anna Picca, Andrea Russo, Sara Salini, Matteo Tosato, Gabriele Abbatecola, Clara Agostino, Fiorella Ambrosio, Francesca Banella, Carolina Benvenuto, Damiano Biscotti, Vincenzo Brandi, Maria Modestina Bulla, Caterina Casciani, Lucio Catalano, Camilla Cocchi, Giuseppe Colloca, Federica Cucinotta, Manuela D’Angelo, Mariaelena D’Elia, Federica D’Ignazio, Daniele Elmi, Marta Finelli, Francesco Pio Fontanella, Domenico Fusco, Ilaria Gattari, Giordana Gava, Tommaso Giani, Giulia Giordano, Rossella Giordano, Francesca Giovanale, Simone Goracci, Silvia Ialungo, Rosangela Labriola, Elena Levati, Myriam Macaluso, Luca Marrella, Claudia Massaro, Rossella Montenero, Maria Vittoria Notari, Maria Paudice, Martina Persia, Flavia Pirone, Simona Pompei, Rosa Ragozzino, Carla Recupero, Antonella Risoli, Stefano Rizzo, Daria Romaniello, Giulia Rubini, Barbara Russo, Stefania Satriano, Giulia Savera, Elisabetta Serafini, Annalise Serra Melechì, Francesca Simeoni, Sofia Simoni, Chiara Taccone, Elena Tagliacozzi, Roberta Terranova, Salvatore Tupputi, Matteo Vaccarella, Emiliano Venditti, Chiara Zanchi, and Maria Zuppardo
References
- 1.GBD 2021 Diabetes Collaborators Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet402(10397), 203–234. 10.1016/S0140-6736(23)01301-6 (2023). [DOI] [PMC free article] [PubMed]
- 2.Makam, A. N., Nguyen, O. K., Moore, B., Ma, Y. & Amarasingham, R. Identifying patients with diabetes and the earliest date of diagnosis in real time: an electronic health record case-finding algorithm. BMC Med. Inform. Decis. Mak.13(1), 81. 10.1186/1472-6947-13-81 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metsovitis, T. et al. Role of nutrition and healthy lifestyle, for individuals in primary prevention: recent data, gaps in evidence and future directions. Arch. Med. Sci.10.5114/aoms/187841 (2024). [Google Scholar]
- 4.Aschner, P. Metabolic syndrome as a risk factor for diabetes. Expert Rev. Cardiovasc. Ther.8(3), 407–412. 10.1586/erc.10.13 (2010). [DOI] [PubMed] [Google Scholar]
- 5.Dandona, P., Aljada, A., Chaudhuri, A., Mohanty, P. & Garg, R. Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation111(11), 1448–1454. 10.1161/01.CIR.0000158483.13093.9D (2005). [DOI] [PubMed] [Google Scholar]
- 6.Skoumas, I. et al. Lipoprotein(a), metabolic profile and new-onset type 2 diabetes in patients with familial combined hyperlipidemia: A 9 year follow-up study. J. Clin. Lipidol.17(4), 512–518. 10.1016/j.jacl.2023.05.103 (2023). [DOI] [PubMed] [Google Scholar]
- 7.Matsubayashi, Y. et al. Impact of metabolic syndrome and metabolic dysfunction-associated fatty liver disease on cardiovascular risk by the presence or absence of type 2 diabetes and according to sex. Cardiovasc. Diabetol.21(1), 90. 10.1186/s12933-022-01518-4 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Despres, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature444(7121), 881–887. 10.1038/nature05488 (2006). [DOI] [PubMed] [Google Scholar]
- 9.Tian, X. et al. Insulin resistance mediates obesity-related risk of cardiovascular disease: a prospective cohort study. Cardiovasc. Diabetol.21(1), 289. 10.1186/s12933-022-01729-9 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cacciatore, S. et al. Predictive values of relative fat mass and body mass index on cardiovascular health in community-dwelling older adults: Results from the Longevity Check-up (Lookup) 7. Maturitas185, 108011. 10.1016/j.maturitas.2024.108011 (2024). [DOI] [PubMed] [Google Scholar]
- 11.Lee, C. M. Y. et al. Comparison of relationships between four common anthropometric measures and incident diabetes. Diabetes Res. Clin. Pract.132, 36–44. 10.1016/j.diabres.2017.07.022 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khader, Y., Batieha, A., Jaddou, H., El-Khateeb, M. & Ajlouni, K. The performance of anthropometric measures to predict diabetes mellitus and hypertension among adults in Jordan. BMC Public Health19(1), 1416. 10.1186/s12889-019-7801-2 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu, C. Y., Chen, H. H., Chi, K. H. & Chen, P. C. Obesity indices and the risk of total and cardiovascular mortality among people with diabetes: a long-term follow-up study in Taiwan. Cardiovasc. Diabetol.22(1), 345. 10.1186/s12933-023-02072-3 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orsi, E. et al. Body mass index versus surrogate measures of central adiposity as independent predictors of mortality in type 2 diabetes. Cardiovasc. Diabetol.21(1), 266. 10.1186/s12933-022-01706-2 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu, C. J. et al. Does the additional component of calf circumference refine metabolic syndrome in correlating with cardiovascular risk?. J. Clin. Endocrinol. Metab.103(3), 1151–1160. 10.1210/jc.2017-02320 (2018). [DOI] [PubMed] [Google Scholar]
- 16.Kim, S. K. et al. Ratio of waist-to-calf circumference and carotid atherosclerosis in Korean patients with type 2 diabetes. Diabetes Care34(9), 2067–2071. 10.2337/dc11-0743 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ross, R. et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol.16(3), 177–189. 10.1038/s41574-019-0310-7 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li, X. et al. Calf circumference and all-cause mortality: a systematic review and meta-analysis based on trend estimation approaches. J. Nutr. Health Aging26(9), 826–838. 10.1007/s12603-022-1838-0 (2022). [DOI] [PubMed] [Google Scholar]
- 19.Landi, F. et al. Estimated appendicular skeletal muscle mass using calf circumference and mortality: Results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Exp. Gerontol.169, 111958. 10.1016/j.exger.2022.111958 (2022). [DOI] [PubMed] [Google Scholar]
- 20.Landi, F., Calvani, R., Tosato, M., Martone, A. M., Fusco, D., Sisto, A., Ortolani, E., Savera, G., Salini, S. & Marzetti, E. Age-related variations of muscle mass, strength, and physical performance in community-dwellers: results from the Milan EXPO Survey. J. Am. Med. Dir. Assoc.18(1), 88 e17–88 e24. 10.1016/j.jamda.2016.10.007 (2017). [DOI] [PubMed]
- 21.Verboven, K. et al. Abdominal subcutaneous and visceral adipocyte size, lipolysis and inflammation relate to insulin resistance in male obese humans. Sci. Rep.8(1), 4677. 10.1038/s41598-018-22962-x (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landi, F. et al. Cardiovascular health metrics, muscle mass and function among Italian community-dwellers: the Lookup 7+ project. Eur. J. Public Health28(4), 766–772. 10.1093/eurpub/cky034 (2018). [DOI] [PubMed] [Google Scholar]
- 23.von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol.61(4), 344–349. 10.1016/j.jclinepi.2007.11.008 (2008). [DOI] [PubMed] [Google Scholar]
- 24.Società Italiana di Nutrizione Umana (SINU). Available online: https://sinu.it/tabelle-larn-2014/ (Accesed on 8 May 2024).
- 25.Landi, F. et al. Relationship between cardiovascular health metrics and physical performance in community-living people: Results from the Longevity check-up (Lookup) 7+ project. Sci. Rep.8(1), 16353. 10.1038/s41598-018-34746-4 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cacciatore, S., Gava, G., Calvani, R., Marzetti, E., Coelho-Junior, H. J., Picca, A., Esposito, I., Ciciarello, F., Salini, S., Russo, A. et al. Lower adherence to a Mediterranean diet is associated with high adiposity in community-dwelling older adults: results from the Longevity Check-Up (Lookup) 7+ Project. Nutrients15(23). 10.3390/nu15234892 (2023). [DOI] [PMC free article] [PubMed]
- 27.American College of Sports Medicine, Chodzko-Zajko, W. J., Proctor, D. N., Fiatarone Singh, M. A., Minson, C. T., Nigg, C. R., Salem, G. J. & Skinner, J. S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc.41(7), 1510–1530. 10.1249/MSS.0b013e3181a0c95c (2009). [DOI] [PubMed]
- 28.Coelho-Junior, H. J., Calvani, R., Picca, A., Tosato, M., Landi, F. & Marzetti, E. Engagement in aerobic exercise is associated with a reduced prevalence of sarcopenia and severe sarcopenia in Italian older adults. J. Pers. Med.13(4). 10.3390/jpm13040655 (2023). [DOI] [PMC free article] [PubMed]
- 29.Rapi, S., Bazzini, C., Tozzetti, C., Sbolci, V. & Modesti, P. A. Point-of-care testing of cholesterol and triglycerides for epidemiologic studies: evaluation of the multicare-in system. Transl. Res.153(2), 71–76. 10.1016/j.trsl.2008.11.010 (2009). [DOI] [PubMed] [Google Scholar]
- 30.Mancia, G. et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens.41(12), 1874–2071. 10.1097/HJH.0000000000003480 (2023). [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024. Diabetes Care47(Suppl 1), S20–S42. 10.2337/dc24-S002 (2024). [DOI] [PMC free article] [PubMed]
- 32.Ness-Abramof, R. & Apovian, C. M. Waist circumference measurement in clinical practice. Nutr. Clin. Pract.23(4), 397–404. 10.1177/0884533608321700 (2008). [DOI] [PubMed] [Google Scholar]
- 33.Martone, A. M. et al. A simple medical device development according to normative values of calf circumference across ages: results from the Italian Longevity Check-up 7+ (Lookup 7+) project. J. Cachexia Sarcopenia Muscle15(1), 36–44. 10.1002/jcsm.13286 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu, Z. J. & Zhu, C. F. Causal relationship between insulin resistance and sarcopenia. Diabetol. Metab. Syndr.15(1), 46. 10.1186/s13098-023-01022-z (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.da Silva Rosa, S. C., Nayak, N., Caymo, A. M. &, Gordon, J. W. Mechanisms of muscle insulin resistance and the cross-talk with liver and adipose tissue. Physiol. Rep.8(19), e14607. 10.14814/phy2.14607 (2020). [DOI] [PMC free article] [PubMed]
- 36.Lopez-Lopez, J. P. et al. The prediction of metabolic syndrome alterations is improved by combining waist circumference and handgrip strength measurements compared to either alone. Cardiovasc. Diabetol.20(1), 68. 10.1186/s12933-021-01256-z (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wannamethee, S. G. & Atkins, J. L. Sarcopenic obesity and cardiometabolic health and mortality in older adults: a growing health concern in an ageing population. Curr. Diabetes Rep.23(11), 307–314. 10.1007/s11892-023-01522-2 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramirez-Velez, R. et al. Muscle mass to visceral fat ratio is an important predictor of the metabolic syndrome in college students. Br. J. Nutr.121(3), 330–339. 10.1017/S0007114518003392 (2019). [DOI] [PubMed] [Google Scholar]
- 39.Dai, M. et al. Association of waist-calf circumference ratio, waist circumference, calf circumference, and body mass index with all-cause and cause-specific mortality in older adults: a cohort study. BMC Public Health23(1), 1777. 10.1186/s12889-023-16711-7 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Broni, E. K. et al. The diabetes-cardiovascular connection in women: understanding the known risks, outcomes, and implications for care. Curr. Diabetes Rep.22(1), 11–25. 10.1007/s11892-021-01444-x (2022). [DOI] [PubMed] [Google Scholar]
- 41.Thong, E. P., Codner, E., Laven, J. S. E. & Teede, H. Diabetes: a metabolic and reproductive disorder in women. Lancet Diabetes Endocrinol.8(2), 134–149. 10.1016/S2213-8587(19)30345-6 (2020). [DOI] [PubMed] [Google Scholar]
- 42.Kautzky-Willer, A., Harreiter, J. & Pacini, G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr. Rev.37(3), 278–316. 10.1210/er.2015-1137 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kautzky-Willer, A., Leutner, M. & Harreiter, J. Sex differences in type 2 diabetes. Diabetologia66(6), 986–1002. 10.1007/s00125-023-05891-x (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henein, M. Y., Vancheri, S., Longo, G. & Vancheri, F. The role of inflammation in cardiovascular disease. Int. J. Mol. Sci.23(21). 10.3390/ijms232112906 (2022). [DOI] [PMC free article] [PubMed]
- 45.Rolver, M. G., Emanuelsson, F., Nordestgaard, B. G. & Benn, M. Contributions of elevated CRP, hyperglycaemia, and type 2 diabetes to cardiovascular risk in the general population: observational and Mendelian randomization studies. Cardiovasc. Diabetol.23(1), 165. 10.1186/s12933-024-02207-0 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu, D. et al. Combined effect of adiposity and elevated inflammation on incident type 2 diabetes: a prospective cohort study. Cardiovasc. Diabetol.22(1), 351. 10.1186/s12933-023-02067-0 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rao, H. A., Harischandra, P. & Yadav, S. Correlation of waist to calf circumference ratio and carotid intima-media thickness in diabetes mellitus. Curr. Diabetes Rev.17(3), 387–393. 10.2174/1573399816999200729124903 (2021). [DOI] [PubMed] [Google Scholar]
- 48.Choe, E. Y. et al. Waist-to-calf circumstance ratio is an independent predictor of hepatic steatosis and fibrosis in patients with type 2 diabetes. J. Gastroenterol. Hepatol.33(5), 1082–1091. 10.1111/jgh.14011 (2018). [DOI] [PubMed] [Google Scholar]
- 49.Dai, M. et al. Is waist-calf circumference ratio associated with frailty in older adults? Findings from a cohort study. BMC Geriatr.23(1), 492. 10.1186/s12877-023-04182-9 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cao, X., Yang, B. & Zhou, J. Waist-to-calf circumstance ratio and cognitive function among Chinese older adults: Mediating roles of physical performance and social activity. Front. Aging Neurosci.15, 1166341. 10.3389/fnagi.2023.1166341 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu, M. et al. Association of waist-calf circumference ratio with incident cognitive impairment in older adults. Am. J. Clin. Nutr.115(4), 1005–1012. 10.1093/ajcn/nqac011 (2022). [DOI] [PubMed] [Google Scholar]
- 52.Yang, S. et al. Waist-calf circumference ratio is an independent risk factor of HRQoL in centenarians. Diabetes Metab. Syndr. Obes.13, 277–287. 10.2147/DMSO.S231435 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Flegal, K. M. et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am. J. Clin. Nutr.89(2), 500–508. 10.3945/ajcn.2008.26847 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gonzalez, M. C., Mehrnezhad, A., Razaviarab, N., Barbosa-Silva, T. G. & Heymsfield, S. B. Calf circumference: cutoff values from the NHANES 1999–2006. Am. J. Clin. Nutr.113(6), 1679–1687. 10.1093/ajcn/nqab029 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Asai, C. et al. Maximal calf circumference reflects calf muscle mass measured using magnetic resonance imaging. Arch. Gerontol. Geriatr.83, 175–178. 10.1016/j.archger.2019.04.012 (2019). [DOI] [PubMed] [Google Scholar]
- 56.Mamudu, H. M. et al. The prevalence of metabolic conditions before and during the COVID-19 pandemic and its association with health and sociodemographic factors. PLoS One18(2), e0279442. 10.1371/journal.pone.0279442 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Powell-Wiley, T. M. et al. Social determinants of cardiovascular disease. Circ. Res.130(5), 782–799. 10.1161/CIRCRESAHA.121.319811 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burioni, R., Contucci, P., Fedele, M., Vernia, C. & Vezzani, A. Enhancing participation to health screening campaigns by group interactions. Sci. Rep.5, 9904. 10.1038/srep09904 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of the research participants.