Abstract
Acquired vulvar lymphangioma (AVL) is a rare but important condition that requires prompt diagnosis and appropriate management to alleviate symptoms and prevent complications. AVL can erupt locally as isolated or clustered lesions which range from translucent, fluid-filled vesicles to smooth, flesh-colored papules or nodules that exude serous or crystalline liquid spontaneously or after trauma. Clinically, it can also be asymptomatic. However, symptoms are commonly accompanied by vulvar itching, burning, soreness, or unpleasant discharge. Here, we report a case series of five Vietnamese patients with AV L with diverse clinical features.
Key words: acquired vulvar lymphangioma, diverse manifestations
Introduction
Vulvar lymphangiomas are relatively rare benign malformations composed of dilated lymphatic vessels.1 Only a few cases have been described in the literature. We report a case series of five adult female patients who presented with fluid-filled vulvar lesions (Figures 1, 2). Histopathological examination confirmed the diagnosis of acquired vulvar lymphangioma (AVL).
Case Reports
Table 1 summarizes the clinical characteristics of the patients. Their ages ranged from 47 to 78 years (mean age: 61 years). Two patients had a history of cancer treatment, one with lymphadenectomy, and the other with radiotherapy. All biopsy specimens showed identical histopathological findings (Figure 3). Blood vessels and lymphatic vessels were concentrated in the superficial dermis, interspersed with chronic inflammatory cells and fibrous tissue (Figure 3A). Thin-walled lymphatic cavities were dissected through collagen bundles in the dermis, with endothelial cells containing eosinophils, lymphocytes, and red blood cells (Figure 3B). No inflammation was observed in the dermis. No morphological characteristics suggestive of human papillomavirus (HPV) infection or dysplasia were observed.
Discussion
AV L is a rare but important condition that requires prompt diagnosis and appropriate management to alleviate symptoms and prevent complications. AV L can erupt locally as isolated or clustered lesions. Lesions can range from translucent, fluid-filled vesicles to smooth, flesh-colored papules or nodules that exude serous or crystalline liquid spontaneously or after trauma. Clinically, it can also be asymptomatic. However, symptoms are commonly accompanied by vulvar itching, burning, soreness, or unpleasant discharge.1–3 In addition, Gupta et al. reported that AV L can be an adverse outcome of hidradenitis suppurativa (HS).4 This finding highlights the importance of identifying comorbidities in patients with HS-related symptoms. Additionally, the emotional discomfort caused by this condition cannot be ignored; it can lead to aesthetic and psychosexual disorders in women who experience it.
Figure 1.
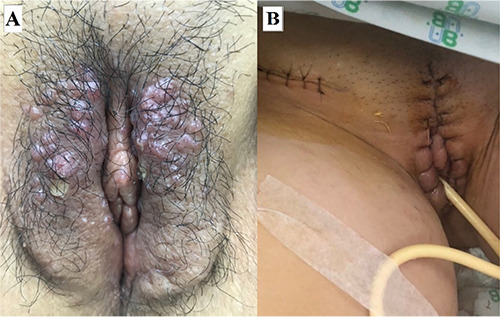
Case 1. (A) before treatment, clear fluid-filled vesicles on the vulva, (B) after treatment.
Figure 2.

Case 2: clusters of vesicles resembling frogspawn. Case 3: plane wart-like papules and vesicles. Case 4: papules and fluid-filled vesicles. Case 5: papules and pus-filled vesicles.
Figure 3.
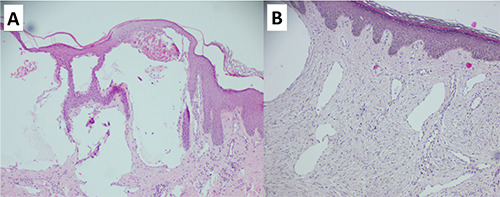
(A) Blood vessels and lymphatic vessels of various sizes, concentrated in the superficial dermis, alternating with chronic inflammatory cells, accompanied by fibrous tissue proliferation. (B) Thin-walled lymphatic vessels dissect through the dermis collagen bundles, with a layer of endothelial cells containing eosinophils mixed with lymphocytes and red blood cells.
Table 1.
Clinical characteristics.
| Case | Age at presentation (years) | Predisposing conditions | Clinical presentation | Treatment | Follow-up (months) |
|---|---|---|---|---|---|
| 1 | 57 | None | Clear fluid-filled vesicles | Bilateral superficial vulvectomy | 6, no recurrence. |
| 2 | 59 | Cervical carcinoma, Cervicectomy g | Genital warts like, reyish-pink papules resembling frogspawn. | Observation | Until present |
| 3 | 65 | None | Plane warts like papules and vesicles | Observation | Until present |
| 4 | 47 | Intra-articular synovial sarcoma in the hip joint 25-ray radiotherapy itch | Painful, discomfort,, papules and fluid-filled vesicles y | Observation | Until present |
| 5 | 78 | Cervical carcinoma, 25-ray radiotherapyand | Painful, itchy papules pus-filled vesicles | Observation | Until present |
Given its rarity, AV L diagnosis can be challenging. However, early identification plays a crucial role in the optimal management of this condition. Multidisciplinary management involving gynaecologists, dermatologists, radiologists, and pathologists is necessary due to the complex nature of the condition.
This entity can be confused with conditions such as genital and plane warts. However, there are key distinctions between these conditions that can help distinguish them. Genital warts are small, flesh-colored, vascularized papules in the genital area that are caused by the HPV. The lesions are usually painless and do not secrete fluid, but they can cause itching and bleeding during intercourse. In contrast, plane warts, which are also caused by viral infection, typically appear as small, flat, flesh-colored, or pink bumps on the skin surface. They can occur anywhere on the body, including the vulva, and are usually painless.
There is currently no established treatment protocol for AVL. Treatment options range from observational to invasive procedures, such as electrocoagulation, CO2 laser therapy, sclerotherapy, and surgical excision, depending on the patient’s condition. Surgical intervention is an effective treatment option in most cases of AVL. However, several factors must be considered during surgical planning, including lesion size, extent, and location, as well as careful consideration given to preserving functional anatomy while achieving adequate removal margins.
AVL can also have a significant psychological impact on women. It can affect their self-esteem, body image, and sexual function. Women with vulvar lymphangioma may also experience anxiety, depression, and other emotional difficulties coping with their condition and its impact on their lives. Families of women with AVL may also be affected as they provide emotional support and assist with care tasks. They may also experience stress and anxiety when dealing with the challenges of living with their family members. It is important that women with AVL and their families receive appropriate medical and psychological support to manage the physical and emotional impact of their condition and maintain their quality of life.
Acknowledgments
The authors thank the STIs Clinic of Ho Chi Minh City Hospital of Dermato-Venereology for collecting the data.
Availability of data and materials
All data used to support the findings of this study are included within the article. Further enquiries can be directed to the corresponding author.
References
- 1.Griffiths CEM, Barker J, Bleiker TO, et al. Rook’s textbook of dermatology, 4, Volume 2016:105:34–42 [Google Scholar]
- 2.Mahajan RS, Marfatia YS, Shah AR, et al. Lymphangioma circumscriptum of the vulva- A case series. J Clin Diagn Res. 2021;15:WR01–WR4. [Google Scholar]
- 3.Marchitelli CE, Sluga MC, Domenech MM, et al. Report of 4 cases of vulvar lymphangioma: An update. Obstet Gynecol Int J. 2018;9:129–32. [Google Scholar]
- 4.Joseph P, Gupta N, Behl L, et al. Acquired lymphangioma circumscriptum of the vulva in a middle aged woman with chronic hidradenitis suppurativa – A case report. IP J Diagn Pathol Oncol. 2023;8:46–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used to support the findings of this study are included within the article. Further enquiries can be directed to the corresponding author.


