Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic had substantially disrupted maternal health care provision and utilisation in Bangladesh. However, the extent of geographical disparities in service utilisation and how the health system withstood these challenges have not been studied. This study explores the divisional disparities in trends and disruptions in maternal health service utilisation caused by the COVID-19 pandemic.
Methods
Data was extracted from the District Health Information Software of Bangladesh from January 2017 to December 2021. We assessed the trend of first antenatal care visit, institutional delivery and number of caesarean sections over these years. We explored both the yearly and monthly trends to see the variations in the number of utilisations. Segmented regression with Poisson distribution was used to assess changes in service utilisation during the COVID-19 period. We reported incidence rate ratio (IRR) of service utilisation with a 95% confidence interval (CI) in different divisions during COVID-19 (2020–2021) compared to the reference period (2017–2019).
Results
Initially, a notable decline in maternal health care utilisation was observed in 2020 compared to the pre-pandemic period of 2017–2019. Divisional disparities were observed in this trend. Overall, compared to the pre-pandemic period, we observed around 30% decline in all three selected indicators of maternal health care. The lowest value was observed in Chattogram in 2020 (IRR = 0.66; 95% CI = 0.55–0.79) and Rajshahi in 2021 (IRR = 0.71; 95% CI = 0.60–0.82). For institutional delivery, Barishal division had the lowest IRR (0.64; 95% CI = 0.60–0.68) in 2020 and, in 2021 Rajshahi had the lowest IRR (0.71; 95% CI = 0.60–0.82). For caesarean section, the lowest value was observed in Barishal division (IRR = 0.48; 95% CI = 0.44–0.53) in 2020 and in Mymensingh (IRR = 0.37; 95% CI = 0.32–0.43) in 2021. By 2021, the three maternal health care utilisation indicators demonstrated recovery.
Conclusions
The effect of the pandemic, including lockdown, on the selected maternal service utilisation was observed in Bangladesh though there were substantial geographic disparities. These disruptions slightly recovered after the initial shock. These results will support the government in preparing the national and regional health systems for future epidemics in Bangladesh.
Coronavirus disease 2019 (COVID-19) had a profound impact on people’s lives globally [1]. Around 700 000 000 cases were identified and 7 000 000 deaths were recorded directly attributed to COVID-19 [2]. Like other countries, Bangladesh also experienced devastating impacts of the pandemic with around 29 000 officially reported deaths [2]. However, these numbers are likely underreported because of the lack of a strong surveillance system to detect all COVID-19-related cases and deaths. [3]. The World Health Organization (WHO) reported 141 000 people died as a result of COVID-19 in Bangladesh between 2020 and 2021 which is much higher than the official records [4]. Globally, the pandemic and lockdown that were imposed as control measures have been reported to have disrupted essential health services [5].
The government of Bangladesh announced a nationwide lockdown to prevent the disease spread from 23 March to 30 May 2020 [6]. This lockdown-imposed restrictions on the international and local travel, commercial activities, activities under educational institutes and social gatherings. Social distancing and limited travel restrictions continued to prevent further circulation of the disease. During the second wave (after the last week of March 2021) of COVID-19 in Bangladesh, the government announced another national lockdown with international travel restrictions in April 2021 [7,8].
Although restrictions were imposed on travels and social gatherings to maintain the social distancing, people were allowed to access all essential health services during lockdown periods. Yet during the pandemic period, 11% of pregnant women received antenatal care visit (ANC) in their third trimester, while 22% received it in pre-pandemic period [9]. Among other reasons, service disruption occurred due to the shortage of physician and nurses, since they were busy with COVID-19 efforts [10,11]. Besides on COVID-19-specific planning and reactions, multiple efforts have been initiated to increase the availability and readiness for essential maternal and neonatal health services such as guideline development, organised virtual meetings, recruitment of physicians and nurses [9,12,13].
Despite these efforts on the national level, the impact of COVID-19 on health care utilisation on divisional level has not been extensively investigated or documented in Bangladesh. Although the lockdown was nationwide, the response to health care systems may have been different in terms of accessing care as the case detection in different division varied widely [14]. A cross-sectional household survey conducted in a rural subdistrict reported the indirect effects of the early phase of the COVID-19 pandemic on the coverage of essential maternal health services [9]. This study reported that the effect of the early phase of the pandemic including lockdown on the selected maternal and child health service coverage was null in the study area. This needs further investigation at the subnational level to assess the impact of COVID-19 on the service use. The majority of the studies reported changes on a national level. Evidence on division level is still unavailable in Bangladesh. Also, most of the available evidence showed impact during the first wave of COVID-19. It is also important to document utilisation of routine health care services under different waves of the pandemic in Bangladesh.
National Health Management Information System (HMIS) of Bangladesh gives us a good opportunity to explore the trend and pattern of utilisation of health care at the public facilities over time [15,16]. Bangladesh health management information system adopted the District Health Information Software, version 2 (DHIS2) to capture updated health service utilisation data in 2009. Our study aims to explore the indirect effects of COVID-19 on maternal health indicators using routine health information data by different geographical divisions in Bangladesh. This study will support a responsive health system approach at the division level to prepare for the future epidemics in Bangladesh.
METHODS
Study settings
This study used information of the public facilities of Bangladesh extracted from DHIS2. The People’s Republic of Bangladesh is a country in South Asia with GDP per capita of 2688 USD (in 2022), and a land area of 147 547 km2 [17,18]. The country has around 165 million population and is one of the most densely populated countries in the world (1119 people per square kilometre) [19]. Administratively, the country is divided into eight divisions (Figure 1). We have included the divisional information in this study. The divisions are Barishal, Chattogram, Dhaka, Khulna, Rajshahi, Rangpur, Mymensingh and Sylhet.
Figure 1.
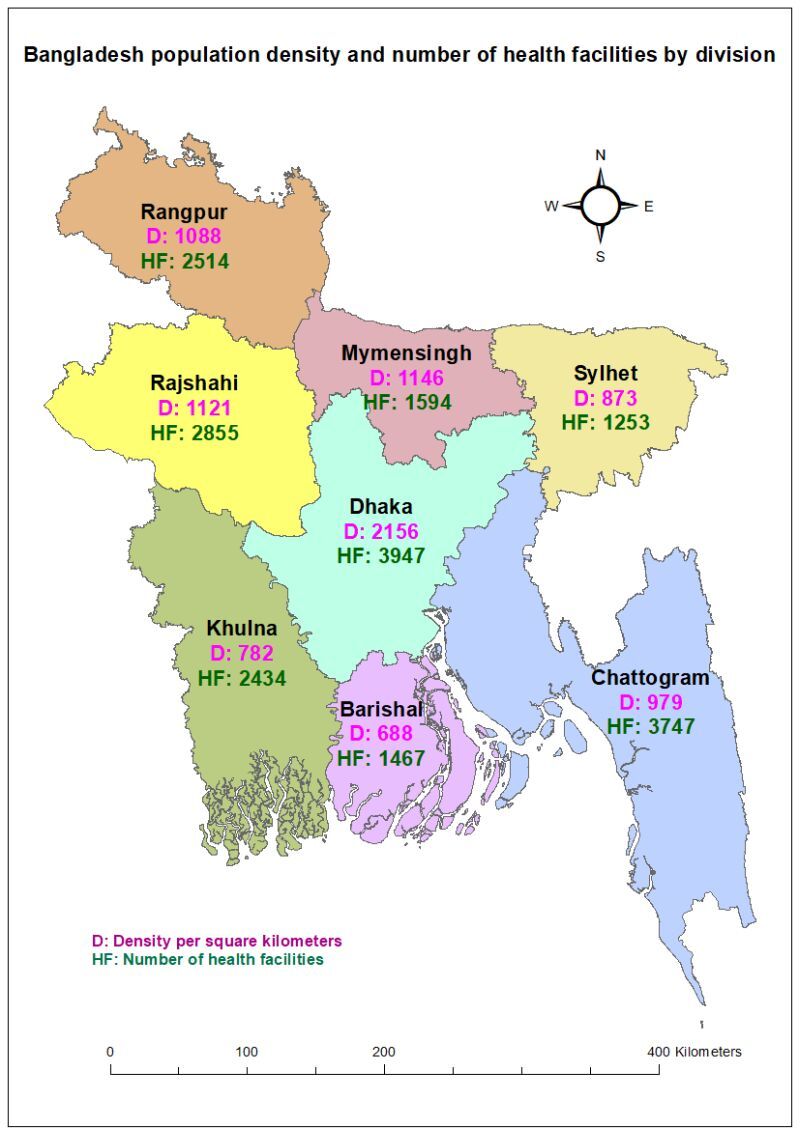
Population density and number of health facilities by division.
The health service in Bangladesh is governed by the Ministry of Health and Family Welfare [20]. District Health Information Software, version 2 (DHIS2) operates under the health services division governed by the Ministry of Health and Family Welfare [21].
Data sources
The data on monthly counts of service utilisation from January 2017 to December 2021 on division level was extracted from DHIS2 Bangladesh. It provides data on health-related indicators for routine monitoring and evaluation at the facilities. The data covers mostly public facilities because most of the private facilities do not report maternal health care service utilisation [16,22,23]. Data was collected on a monthly basis from all public facilities in all eight divisions in Bangladesh, namely Dhaka, Chattogram, Barishal, Khulna, Rajshahi, Rangpur, Mymensingh and Sylhet.
Outcome variables
The main outcome variables are number of pregnant women who had at least one ANC visit, number of institutional deliveries and number of women delivering through caesarean section. These variables are mostly used for monitoring the maternal health care utilisation.
Assessment and adjustment for incomplete reporting
We verified the completeness of the reporting for our selected indicators using supplementary data from DHIS2. Our adjustment method was based on assumptions about the levels of service outputs (pregnancy care and deliveries) at times when data was not reported, in comparison to periods with complete reports.
We employed the following formula to adjust for incomplete reporting:
N (adjusted) = N (reported) + N (reported) × (1 / (c) - 1) × k
where N represents the number of service outputs, c is the reporting completeness, and k is an adjustment factor. The adjustment factor k takes on values representing the assumed level of services in non-reporting time points, ranging from 0 (indicating no services) to 1.0 (indicating the same rate of services as reporting period). The values of k are as follows:
k = 0; no services during non-reported time point
k = 0.25; some services, but much lower than reporting time point
k = 0.5; half the rate compared to reporting time point
k = 0.75; nearly as much as reporting time point
k = 1.0; same rate of services as reporting time point.
The choice of the adjustment factor (k) requires consultation with experts with knowledge of the country’s health system. We have used the k = 0.75 as per the expert suggestion of Bangladesh, where it is assumed that we have some variation of service provision between the reporting and non-reporting facilities. Additional information on DHIS2 data quality is provided in Appendix S1 in the Online Supplementary Document.
Statistical analysis
We analysed the yearly trend to ascertain the increase or decrease in health care utilisation during the COVID-19 period. Next, we assessed the monthly trends to understand which time periods were mostly affected by COVID-19. We used segmented Poisson regression to quantify the size of any disruption in the trends in the monthly utilisation numbers. We have assessed the normality of the outcome variables and they were not normal which is an assumption for linear regression. Therefore, we fitted the Poisson regression which is widely accepted in such analyses for interrupted time series. The incidence rate ratios (IRR) are reported for explaining the impact of COVID-19 (2020, 2021) on our selected outcome variables compared to pre-COVID time (2017–2019). We have checked autocorrelation using Durbin Watson statistic [24]. We have also assessed our data for seasonality using Dickey-Fuller unit-root test and controlled for seasonality in the model [25]. Additional details on seasonality adjustment are provided in Appendix S2 in the Online Supplementary Document.
We have selected segmented Poisson regression with following justifications. Hospital service utilisation data, such as the number of visits or procedures, are count data. Poisson regression is specifically designed for modelling count data, making it a suitable choice. Segmented Poisson regression can model rates that change over time, which is essential for capturing the dynamic impact of COVID-19 as the situation evolves. It allows for the analysis of interruptions and interventions, such as lockdowns or policy changes, which have significant effects on service utilisation patterns. This method offers flexibility in modelling and understanding trends and patterns before, during, and after the COVID-19 pandemic periods.
We have quantified the rate of change by month during the pandemic period compared to pre-pandemic along with number of deaths per month. We reported the findings on divisional level. We used Stata version 15 (Texas, USA, 2015) for the quantitative analysis [26].
RESULTS
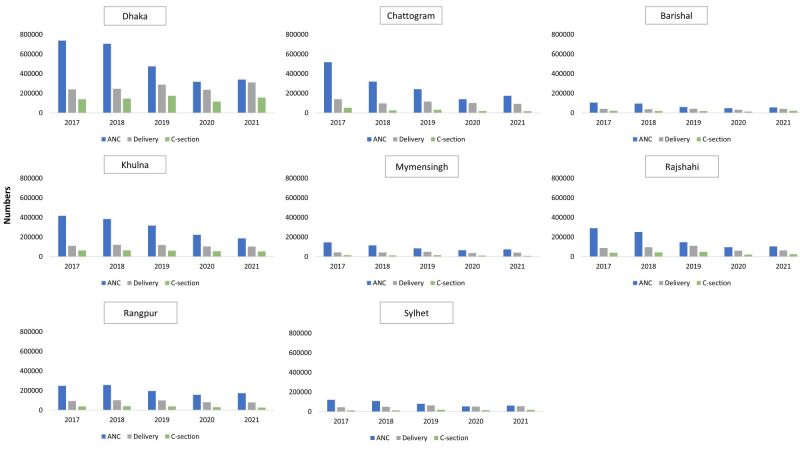
We present the annual changes in the number of ANC first visit, institutional delivery and caesarean section over the five-year period from 2017 to 2021 on divisional level (Figure 2).
Figure 2.
Yearly trend of maternal health indicators, number of first Antenatal Care contact, number of institutional delivery and number of caesarean sections from DHIS2 by divisions in Bangladesh. DHIS2 – District Health Information Software, version 2.
ANC first visit
There was a decline in ANC first visit from 2017 to 2019 in all divisions, with a dip in 2020 followed by a rebound in 2021. In all regions, the number of ANC services was highest in 2017, followed by a gradual decrease in subsequent years. Dhaka, despite having the highest absolute numbers of ANC services each year, saw a dramatic drop from around 0.74 million in 2017 to 0.32 million in 2020, indicating Dhaka was heavily impacted by the pandemic. In contrast, regions like Rangpur experienced less dramatic declines. For instance, Rangpur's ANC services dropped from 0.25 million in 2017 to 0.16 million in 2020 and slightly increased to 0.17 million in 2021, indicating a relatively more stable trend compared to Dhaka. In 2021, all the divisions experienced a substantial rebound but it is comparatively lower than the previous years of 2017–2019.
Institutional delivery
The graphs suggest a steady upward trend in the number of institutional deliveries from 2017 to 2019 in all divisions, with the exception in Chattogram. During the 2017–2019 period, Chattogram experienced a decline in 2018 compared to 2017, followed by an increase in 2019. The number of institutional deliveries in Chattogram in 2019 remained lower than the level observed in 2017. In 2021, the divisions experienced a substantial rebound except Chattogram, Khulna and Rangpur.
Caesarean section
A gradual increase in the number of caesarean section deliveries was observed from 2017 to 2019 in all divisions, except for Chattogram, which showed a decrease, and Barishal, where a decline was recorded in 2018 followed by consistency in 2019. In 2021, Dhaka, Barishal, Rajshahi and Sylhet showed a rebound in the trend from 2020 to 2021. While Chattogram, Khulna, Mymensingh and Rangpur reflected a drop in the numbers during 2021 as compared to 2020.
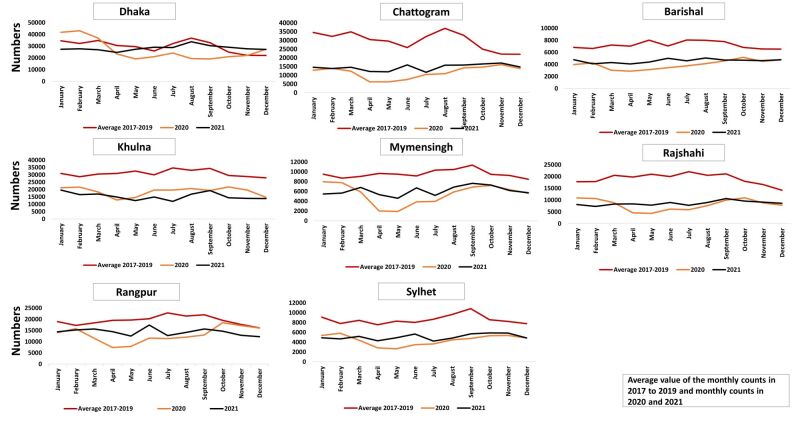
Monthly change: ANC first visit
In the year 2020 in all divisions, there was a noticeable drop in ANC visits in April, followed by a gradual increase in subsequent months. The highest decline in April 2020 was observed in Mymensingh. The number of ANC visits in 2021 was higher than in 2020 but never reached the levels observed in 2017–2019 in all divisions, except Dhaka, suggesting that the disruption in the utilisation of ANC services has not recovered in most divisions by the end of 2021 (Figure 3).
Figure 3.
Monthly trend of first antenatal care visit using DHIS2 data set from 2017 to 2021. DHIS2 – District Health Information Software, version 2.
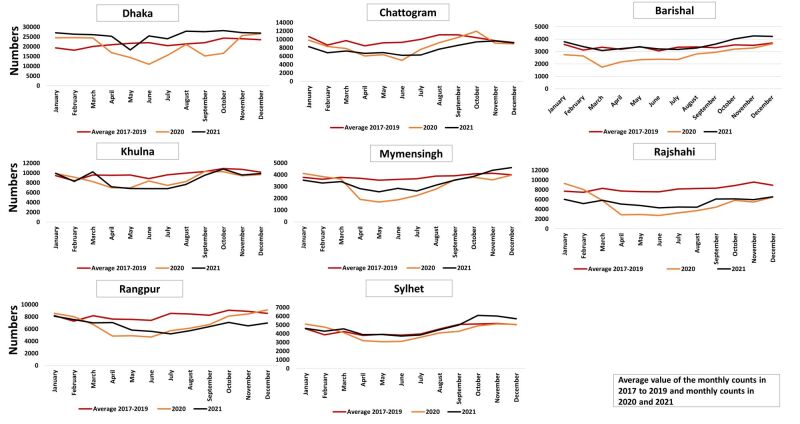
Monthly change: institutional delivery
In the year 2020, there was a noticeable drop in April and rise in August (Figure 4). The highest decline observed in Dhaka in April 2020. In contrast, the year 2021 exhibited a significant rebound in the values. Also, the values for year 2021 were aligned with the values of average of 2017–2019 with a slight variation in all divisions. The utilisation of delivery services recovered by the end of 2021 in all division except Rangpur and Rajshahi.
Figure 4.
Monthly trend of institutional delivery using DHIS2 data set from 2017 to 2021. DHIS2 – District Health Information Software, version 2.
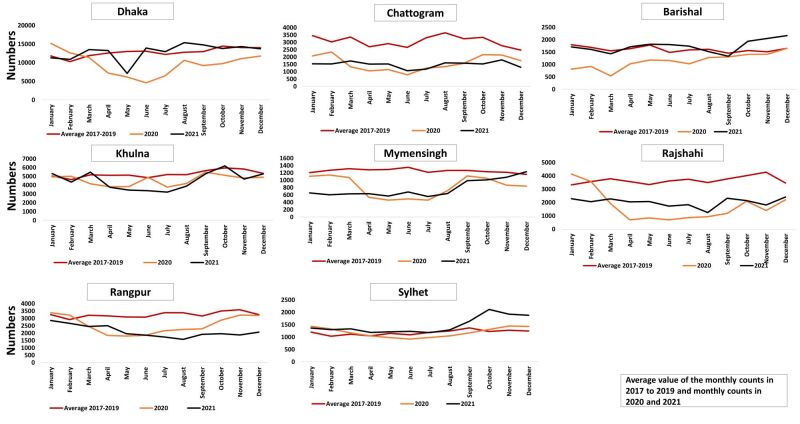
Monthly change: caesarean section
The average values of caesarean section during the years 2017–2019 remained relatively stable in all divisions with slight monthly fluctuations (Figure 5). In the year 2020, there was a noticeable drop in April and simultaneous rise in August. The year 2021 exhibited a visible rebound in the values. The values for year 2021 were aligned with the values of average of 2017–2019 with a slight variation in all divisions. There was a drop-in caesarean section but it recovered in 2021 in Dhaka, Barishal, Khulna and Sylhet.
Figure 5.
Monthly trend of caesarean section using DHIS2 data set from 2017 to 2021. DHIS2 – District Health Information Software, version 2.
Segmented regression: ANC first visit
The likelihoods of ANC first visit in these divisions during 2020 and 2021 were lower compared to the reference period 2017–2019 (Table 1). The number of ANC first visits was significantly less frequent during 2020–2021. The lowest value was observed in the Chattogram in 2020 (IRR = 0.66; 95% CI = 0.55–0.79) and Rajshahi in 2021 (IRR = 0.71; 95% CI = 0.60–0.82).
Table 1.
Results from segmented regression on first antenatal care visit interrupted time series presented in incidence rate ratio with 95% confidence interval
| Site | 2020 |
2021 |
||
|---|---|---|---|---|
|
|
IRR (CI)
|
P-value
|
IRR (CI)
|
P-value
|
| Bangladesh |
0.84 (0.72–0.99) |
0.042 |
0.82 (0.75–0.89) |
<0.001 |
| Dhaka |
1.04 (0.85–1.28) |
0.704 |
0.72 (0.62–0.84) |
<0.001 |
| Chattogram |
0.66 (0.55–0.79) |
<0.001 |
0.90 (0.83–0.98) |
0.019 |
| Barishal |
0.73 (0.71–0.75) |
<0.001 |
0.98 (0.85–1.15) |
0.840 |
| Khulna |
0.82 (0.76–0.89) |
<0.001 |
0.73 (0.68–0.79) |
<0.001 |
| Mymensingh |
0.99 (0.98–1.02) |
0.993 |
0.99 (0.94–1.06) |
0.992 |
| Rajshahi |
0.67 (0.54–0.83) |
<0.001 |
0.71 (0.60–0.82) |
<0.001 |
| Rangpur |
0.70 (0.69–0.71) |
<0.001 |
1.03 (0.92–1.15) |
0.634 |
| Sylhet | 0.77 (0.66–0.91) | 0.002 | 0.84 (0.77–0.92) | <0.001 |
CI – confidence interval, IRR – incidence rate ratio
Segmented regression: institutional delivery
Overall, Bangladesh observed 20% decline in 2020 and 13% decline in 2021 in the number of institutional deliveries compared to pre-COVID period (Table 2). Barishal observed the highest decline in 2020 (IRR = 0.64; 95% confidence interval (CI) = 0.60–0.68) and Rajshahi in 2021 (IRR = 0.53; 95% CI = 0.50–0.57).
Table 2.
Results from segmented regression on institutional delivery interrupted time series presented in incidence rate ratio with 95% confidence interval
| Site | 2020 |
2021 |
||
|---|---|---|---|---|
|
|
IRR (CI)
|
P-value
|
IRR (CI)
|
P-value
|
| Bangladesh |
0.80 (0.72–0.89) |
<0.001 |
0.87 (0.83–0.91) |
<0.001 |
| Dhaka |
0.79 (0.67–0.93) |
0.004 |
1.04 (1.02–1.07) |
0.001 |
| Chattogram |
1.00 (0.89–1.13) |
0.945 |
0.88 (0.76–1.01) |
0.073 |
| Barishal |
0.64 (0.60–0.68) |
<0.001 |
0.96 (0.90–1.02) |
0.165 |
| Khulna |
0.76 (0.70–0.82) |
<0.001 |
0.83 (0.77–0.89) |
<0.001 |
| Mymensingh |
0.73 (0.64–0.83) |
<0.001 |
0.68 (0.62–0.75) |
<0.001 |
| Rajshahi |
0.66 (0.55–0.81) |
<0.001 |
0.53 (0.50–0.57) |
<0.001 |
| Rangpur |
0.70 (0.59–0.82) |
<0.001 |
0.88 (0.83–0.93) |
<0.001 |
| Sylhet | 0.76 (0.70–0.83) | <0.001 | 0.74 (0.69–0.79) | <0.001 |
CI – confidence interval, IRR – incidence rate ratio
Segmented regression: caesarean section
The likelihood of taking caesarean section in these divisions during 2020–2021 was lower compared to the reference period 2017–2019, 30% decline observed in 2020 and 25% in 2021 (Table 3). The lowest value was observed in the Barishal division (IRR = 0.48; 95% CI = 0.44–0.53) in 2020. In 2021 highest decline observed in Mymensingh (IRR = 0.37; 95% CI = 0.32–0.43).
Table 3.
Results from segmented regression on caesarean section interrupted time series presented in incidence rate ratio with 95% confidence interval
| Site | 2020 |
2021 |
||
|---|---|---|---|---|
|
|
IRR (CI)
|
P-value
|
IRR (CI)
|
P-value
|
| Bangladesh |
0.70 (0.59–0.82) |
<0.001 |
0.75 (0.72–0.79) |
<0.001 |
| Dhaka |
0.74 (0.63–0.87) |
<0.001 |
0.76 (0.74–0.79) |
<0.001 |
| Chattogram |
0.90 (0.70–1.17) |
0.448 |
0.90 (0.72–1.12) |
0.349 |
| Barishal |
0.48 (0.44–0.53) |
<0.001 |
0.99 (0.89–1.01) |
0.929 |
| Khulna |
0.79 (0.75–0.84) |
<0.001 |
0.77 (0.69–0.86) |
<0.001 |
| Mymensingh |
0.70 (0.59–0.82) |
<0.001 |
0.37 (0.32–0.43) |
<0.001 |
| Rajshahi |
0.64 (0.48–0.85) |
0.002 |
0.48 (0.45–0.52) |
<0.001 |
| Rangpur |
0.77 (0.68–0.88) |
<0.001 |
0.83 (0.78–0.89) |
<0.001 |
| Sylhet | 0.74 (0.63–0.85) | <0.001 | 0.72 (0.63–0.81) | <0.001 |
CI – confidence interval, IRR – incidence rate ratio
DISCUSSION
Our study investigated the divisional disparities of the indirect impact of COVID-19 on key indicators of maternal health in Bangladesh using routine health information data. Our findings suggest during the first lockdown in 2020, all three maternal health indicators declined. We also observed decline in utilisation in 2021 compared to pre-COVID years, but the highest decline was observed during 2020. The number of women delivering through caesarean section declined around one-third during COVID-19, which the most among all three indicators. We observed lower incidence rate for ANC first visit in Chattogram and Rajshahi division; institutional delivery in Barishal and Rajshahi division and caesarean section in Barishal and Mymensingh divisions after the onset of COVID-19 in Bangladesh.
Bangladesh's experience with maternal service utilisation during COVID-19 mirrors some aspects seen in other low- and middle-income countries but also presents unique challenges. Consistent with our findings, Wangmo and colleagues using national health information system of Bangladesh (DHIS2) found substantial reductions in the essential health services including maternal health services utilisation from April 2020 to May 2020 [27]. These services include the number of outpatient appointments, inpatient admissions, first ANC visits and institutional normal vaginal deliveries, as well as the percentage of children fully immunised by the Expanded Programme on Immunisation, assessed for each month and level of health facility. Other studies in Asia and Africa including countries such as Uganda, Pakistan, India, Kenya, Zambia, Demographic Republic of the Congo, Haiti, Liberia and South Africa have also found declines in maternal service utilisation during the first of months of the pandemic [15,28–31]. Most public health facilities in Bangladesh were over-crowded and reported to have low coverage and quality of services, poor hygiene and sanitation practises during pandemic [32,33]. During COVID-19 pandemic, care seekers faced many challenges. There were socio cultural reasons for this decline in the service utilisation during COVID-19. The plausible reason for decrease in selected maternal health services in Bangladesh could be a switched focus towards pandemic, decline in economy, the execution of area-wise lockdown, travel restrictions, shortened visiting hour by government in the public facilities, lack of medical equipment such as personal protective equipment for health workers [34–36]. Due to COVID-19 pandemic, most of the health workers’ duty was redesigned to serve the emergency response which led to human resource scarcity in the public facilities [36]. Concerns for safety issues and fear of having COVID-19 infection in both the patients and health workers contributed to the decline in the utilisation of selected maternal health services [37]. Fear of contracting the virus led many pregnant women to avoid hospital visits, resulting in reduced access to essential maternal health services [15]. In Bangladesh, other factors included the unavailability of transport during the pandemic [38]. However, Bangladesh implemented innovative solutions like midwife-led telemedicine services to address some of these gaps. This contrasts with countries such as Nigeria and South Africa, where similar declines occurred but without widespread telemedicine initiatives [15].
Our observation of declining utilisation in 2021 compared to pre-COVID years with highest decline during 2020 is similar to the study of Angeles and colleagues [28]. Reductions in ANC first visit and institutional deliveries during first month of pandemic with a gradual and incomplete recovery by August 2020 have been shown on national level in Bangladesh [28]. Service utilisation increased gradually when the lockdown was lifted, but did not entirely bounce back to pre-pandemic levels [39]. Limitation on public transit and scarcity of transportation was being existed from March 2020–2021 in Bangladesh that could be a feasible cause of reduced maternal health service utilisation [38]. However, significant increase in trends were noticed by Ebola post-outbreak in Liberia which took almost one year to regain than the pre-outbreak level [40]. Recent study using routine monitoring data in Pakistan found a drop of 57% in caesarean section rate and 37% in institutional delivery during January–May 2020 and an increase in June–September 2020 with another decline in October–December 2020 [37]. Another study in the Demographic Republic of the Congo reported decreased ANC first visit after the pandemic started but institutional delivery remained unaffected. Antenatal care service utilisation recovered when the lockdown was lifted, but the trend in rates of maternal health services (ANC first visit and institutional delivery) did not rise over time as compared to the trend of expected pre-COVID-19 situation [39]. The COVID-19 pandemic resulted in serious disruption in ANC and institutional delivery services for one month in Cameroon, Demographic Republic of the Congo, Liberia, Malawi, Mali, Nigeria, Sierra Leone and Somalia with a different size and time frame [41]. Research in South Africa highlighted a disproportionate impact of COVID-19 pandemic on ANC first visit and caesarean section in public facilities in different divisions from April 2020 to June 2021 [31]. Another study in Bangladesh noticed a gradual but not parallel increase in service utilisation during 2021 which supports our findings [27]. This may be due to a flexible lockdown which expected to simultaneously trade off both public health and economic restart, possibly to improve future life and to reopen the economy before the successful development of vaccines. This was put in place following the second wave of COVID-19 pandemic [42].
Our observation highlighted divisional disparities in the selected maternal health services utilisation during and post-pandemic situation. Lower incidence rate was observed for ANC first visit in Chattogram and Rajshahi division; institutional delivery in Barishal and Rajshahi division and caesarean section in Barishal and Mymensingh divisions in Bangladesh. Studies have shown that women in Rajshahi division were less likely to have ANC visits during the pre-pandemic years compared to other divisions in Bangladesh [43,44]. In 2016, Sarker and colleagues, shared their field level experience in three districts of Rajshahi division and assumed that the socio-cultural factors are linked to delayed ANC services in the study areas [45]. Around 32% of the health workers were repurposed for the COVID-19 emergency response in Mymensingh division [27]. This may have generated a gap of human resource which may have caused lower maternal health services utilisation during 2020–2021 in Mymensingh [27].
A major drawback of DHIS2 in Bangladesh is its inability to include data from private health facilities. This omission leads to incomplete health information, which can impede effective health planning and policy-making. Our data showed a declining trend of number of first ANC visit which is contradictory from the survey data [46]. One of the potential reasons for this could be the transition from public to private facilities for seeking ANC. As DHIS2 lacks private health facility data, we observed a decline in the overall ANC trend.
We also acknowledge the data quality may have been an issue while using and interpreting DHIS2 data, especially in the case of ANC information in this analysis. A low resource setting with technical infrastructure, lack of skilled health worker, insufficient software development and data security issues may have created challenges in maintaining the electronic data system in Bangladesh [47]. Lack of training on data management regarding HMIS dashboard, insufficient supervision from district health manager and higher authorities, absence of feedback on the quality of monthly reports influenced the data quality [48,49]. Gaps in data availability, under-reporting, incompleteness and inconsistency of the reports were also evident in the DHIS2 data in Nigeria [50,51]. Inadequate human resource, lack of standard operating procedure contributed to poor data reporting [48]. Follow up patients are preferably enrolled as new patients by health care providers that raises data quality issue of inaccurate number of service utilisation [16]. In some instances, data from peripheral level health facilities takes an average of three months to reach the central office. Patient load also affected the online registration and data entry process. Lack of human resource, slow internet connectivity, frequent changes in DHIS2 versions, maintaining both manual registry and electronic database were identified as barriers to maintain quality routine data in DHIS2 in Bangladesh [16]. Checking quality and providing feedback on a regular basis from higher authority helps to reduce data errors in DHIS2 [16].
Policy and programme implications
There are many initiatives taken by government, private (Non-Governmental Organizations (NGOs) and International Non-Governmental Organizations (INGOs)) organisations during COVID-19 [34,52,53]. The Government of Bangladesh initiated several schemes, interventions, policies to continued uninterrupted health services across the country, but the care seeking did not adequately improve after COVID-19 in the immediate next year according to the data on public facilities of Bangladesh. In order to act in timely manner Bangladesh, need to have early strategic planning for combating evolving challenges during pandemic. Appropriate response plans and management are crucial for the sustainability of the nation. An elaborate national plan with focus on divisional differences may help government in effective planning and resource optimisation. Special focus should be given to Chattogram, Rajshahi, Barishal, and Mymensingh for future resource planning.
Strengths and limitations
This study has several strengths that further contribute to the potential of data in DHIS2 for local, real-time monitoring of selected maternal health services. The inclusion of the large sample size of DHIS2 data from different divisions in Bangladesh allowed for conclusions to be drawn across regions. The unique data allowed for exploration of both yearly and monthly trends using interrupted time series data approach to understand seasonal patterns and time periods, and to see the variation in the number of maternal health services utilisation which were mostly disrupted by COVID-19 period.
There are limitations in estimating the coverage of maternal health services through the DHIS2 in Bangladesh. First, we observed a wide-spread absence of population data, decreased quality and completeness of data collection during the COVID-19 pandemic. A significant reason for incomplete data in the national routine health information system in Bangladesh could be uncovered data of private facilities under the DHIS2 network [16]. Therefore, the true impact on the coverage of maternal health services might be less than what was originally observed based on DHIS2 utilisation data in the early phase of the pandemic.
Second, there were gaps, delays in the documentation and reporting of routine services and lack of control in DHIS2 electronic version in the initial phase of the pandemic, particularly during the lockdown period. The quantitative analysis of the changes in the level of service utilisation is prone to bias from several issues of HMIS data. Third, absence of data on maternal and neonatal health services from Directorate General of Family Planning and private facilities in the DHIS2 dashboard contributes to a gap in generalisability regarding disparities in geographical and periodic findings [16,22,54]. Moreover, the lack of varied independent variables and qualitative data limits a thorough understanding of service recipient characteristics. Third, the established formula for adjusting the incomplete reporting does not contain the validity parameter of the estimate. Therefore, it was difficult for us to ascertain how the choices of adjustment factors affected the validity of the results. Fourthly, we have used the facility-based data and could not explore the socio-cultural context. More detailed analysis on how socio-cultural factors influence maternal health service utilisation in Bangladesh could strengthen our analysis. Lastly, we did not identify adequate evidence to explain the regional disparities in maternal service utilisation during COVID-19. We discussed the disparities, but further research endeavours will be required to better explain the reasons behind these differences.
CONCLUSIONS
Our analysis sheds light on disruptions in selected maternal health services following COVID-19 and afterward in Bangladesh. Regional differences in maternal health service utilisation during and after COVID-19 were apparent, particularly in Chattogram, Rajshahi, Barishal, and Mymensingh, where the effects were most pronounced. This will inform the policy makers for timely response during future pandemics considering divisional disparities. The analytical approach used in this paper could also be utilised as a form of surveillance to detect service interruptions beyond the pandemic in Bangladesh.
Additional material
Acknowledgments
Ethics statement: This study constitutes a secondary analysis of routine healthcare data; therefore, ethical certification was not required.
Data availability: The data set used in this study is available according to the existing data policy of International Centre for Diarrhoeal Disease Research.
Footnotes
Funding: This study was supported by a grant of the Bill & Melinda Gates Foundation to the Countdown to 2030 for Women’s, Children’s and Adolescents’ Health, through US Fund for UNICEF (Grant Number INV-001299).
Authorship contributions: Aniqa Tasnim Hossain, as the first author, developed the manuscript with the support from Nadia Akseer and Ema Akter. Agbessi Amouzou and Shams El Arifeen, as senior authors, provided guidance and feedback to Aniqa Tasnim Hossain at every stage of developing the paper. Ema Akter, Md. Alamgir Hossain and KM Tanvir conducted the analyses with support from Aniqa Tasnim Hossain. Ridwana Maher Manna, Tasnu Ara and Bibek Ahamed extracted the data from DHIS2 system. Ahmed Ehsanur Rahman and Abu Bakkar Siddique supported in conceptualisation and developing the draft. Md Hafizur Rahman, Abu Sayeed, M Sabbir Haider, Sabrina Jabeen, Shafiqul Ameen, Mohammad Sohel Shomik, Anisuddin Ahmed, Luis Huicho, Alicia Matijasevich and Abdoulaye Maiga reviewed and edited the final draft of the paper. All authors read and approved the final manuscript.
Disclosure of interest: The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests.
REFERENCES
- 1.World Health Organization. Impact of COVID-19 on people’s livelihoods, their health and our food systems. Joint statement by ILO, FAO, IFAD and WHO. 2020. Available: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems. Accessed: 1 February 2024.
- 2.Worldometer. Covid-19 coronavirus pandemic: Worldometer. 2023. Available: https://www.worldometers.info/coronavirus/country/bangladesh/. Accessed: 1 February 2024.
- 3.Uddin M, Ashrafi SAA, Azad AK, Chowdhury A, Chowdhury HR, Riley ID, et al. Improving coverage of civil registration and vital statistics, Bangladesh. Bull World Health Organ. 2019;97:637. 10.2471/BLT.18.219162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dhaka Tribune. WHO estimates Covid-19 death toll in Bangladesh 5 times higher than official figures 2022. Available: https://www.dhakatribune.com/bangladesh/health/269673/who-estimates-covid-19-death-toll-in-bangladesh-5. Accessed: 1 April 2024.
- 5.World Health Organization. Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November–December 2021: interim report, 7 February 2022. Geneva: World Health Organization; 2022. [Google Scholar]
- 6.Shammi M, Bodrud-Doza M, Islam ARMT, Rahman MM.Strategic assessment of COVID-19 pandemic in Bangladesh: comparative lockdown scenario analysis, public perception, and management for sustainability. Environ Dev Sustain. 2021;23:6148–91. 10.1007/s10668-020-00867-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bari R, Sultana F.Second Wave of COVID-19 in Bangladesh: An integrated and coordinated set of actions is crucial to tackle current upsurge of cases and deaths. Front Public Health. 2021;9:699918. 10.3389/fpubh.2021.699918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institute of Population Research and Training (NIPORT), Ministry of Health and Family Welfare. (MoH&FW). Bangladesh Health Facility Survey 2017, Final Report. 2020. Contract No.: 25 October, 2021.
- 9.Mhajabin S, Hossain AT, Nusrat N, Jabeen S, Ameen S, Banik G, et al. Indirect effects of the early phase of the COVID-19 pandemic on the coverage of essential maternal and newborn health services in a rural subdistrict in Bangladesh: results from a cross-sectional household survey. BMJ Open. 2022;12:e056951. 10.1136/bmjopen-2021-056951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta N, Dhamija S, Patil J, Chaudhari B.Impact of COVID-19 pandemic on healthcare workers. Ind Psychiatry J. 2021;30:S282–S284. 10.4103/0972-6748.328830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hossain I. Covid-19: Health professional shortage remains a challenge in Bangladesh. Dhaka Tribune. 2020. Available: https://www.dhakatribune.com/bangladesh/health/230548/covid-19-health-professional-shortage-remains-a. Accessed: 1 April 2024.
- 12.Directorate General of Health Services of Bangladesh. National Guideline for providing essential Maternal, Newborn and Child Health Services in the context of COVID-19. 2020. Available: https://catalyzingrightscovid19.law.duke.edu/ihrc_measure/national-guideline-for-providing-essential-maternal-newborn-and-child-health-services-in-the-context-of-covid-19/. Accessed: 1 February 2024.
- 13.bdnews24.com. Bangladesh moves to recruit 2,000 doctors, 5,000 nurses amid virus outbreak. bdnews24com. 2020. Available: https://bdnews24.com/bangladesh/bangladesh-moves-to-recruit-2000-doctors-5000-nurses-amid-virus-outbreak. Accessed: A February 2024.
- 14.Bangladesh GoTPsRo. COVID-19 Dynamic Dashboard for Bangladesh 2024. Available: http://103.247.238.92/webportal/pages/covid19.php. Accessed: 1 April 2024.
- 15.Ahmed T, Rahman AE, Amole TG, Galadanci H, Matjila M, Soma-Pillay P, et al. The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: call for a contextualised pandemic response in LMICs. Int J Equity Health. 2021;20:77. 10.1186/s12939-021-01414-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Begum T, Khan SM, Adamou B, Ferdous J, Parvez MM, Islam MS, et al. Perceptions and experiences with district health information system software to collect and utilize health data in Bangladesh: a qualitative exploratory study. BMC Health Serv Res. 2020;20:456. 10.1186/s12913-020-05322-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nahar S, Costello A.The hidden cost of ‘free’ maternity care in Dhaka, Bangladesh. Health Policy Plan. 1998;13:417–22. 10.1093/heapol/13.4.417 [DOI] [PubMed] [Google Scholar]
- 18.Rahman M, Rob U, Noor FR, Bellows B.Out-of-Pocket Expenses for Maternity Care in Rural Bangladesh: A Public-Private Comparison. Int Q Community Health Educ. 2012–2013;33:143–57. 10.2190/IQ.33.2.d [DOI] [PubMed] [Google Scholar]
- 19.Bangladesh Bureau of Statistics; Statistics and Information Division of Ministry of Planning; Government of the People’s Republic of Bangladesh. Population and Housing Census 2022. Dhaka: Bangladesh Bureau of Statistics; 2022. Available: https://sid.portal.gov.bd/sites/default/files/files/sid.portal.gov.bd/publications/01ad1ffe_cfef_4811_af97_594b6c64d7c3/PHC_Preliminary_Report_(English)_August_2022.pdf. Accessed: 15 April 2024. [Google Scholar]
- 20.Directorate General of Health Services – Ministry of Health and Family Welfare – Government of Bangladesh. Health Bulletin 2017. Dhaka: Management Information System; 2018. Available: https://old.dghs.gov.bd/index.php/en/home/4364-health-bulletin-2017. Accessed: 15 April 2024. [Google Scholar]
- 21.Directorate General of Health Services (DGHS). DHIS - Interface for collection of nation-wide health data. Available: https://old.dghs.gov.bd/index.php/en/e-health/our-ehealth-eservices/84-english-root/ehealth-eservice/94-dhis-interface-for-collection-of-nation-wide-health-data. Accessed: 15 April 2024.
- 22.Management information System. Health Bulletin 2017 Dhaka: Director General of Health System2017. Available: http://www.dghs.gov.bd/index.php/en/home/4364-health-bulletin-2017. Accessed: 30 April 2024.
- 23.Kabir MH, Kibria M. HIS Mapping: An Inventory of Digital Tools in Use by the Ministry of Health and Family Welfare in Bangladesh. 2021. Available: https://www.data4impactproject.org/wp-content/uploads/2021/08/HIS-Mapping-in-Bangladesh_fs-21-525_FINAL.pdf. Accessed: 15 April 2024.
- 24.Champion R, Lenard C, Mills T.Demonstrating the Durbin-Watson statistic. Statistician. 1998;47:643–4. 10.1111/1467-9884.00161 [DOI] [Google Scholar]
- 25.Paparoditis E, Politis DN.The asymptotic size and power of the augmented Dickey–Fuller test for a unit root. Econom Rev. 2018;37:955–73. 10.1080/00927872.2016.1178887 [DOI] [Google Scholar]
- 26.Baum CF. An introduction to Stata programming. Texas: Stata Press College Station; 2009. [Google Scholar]
- 27.Wangmo S, Sarkar S, Islam T, Rahman MH, Landry M.Maintaining essential health services during the pandemic in Bangladesh: the role of primary health care supported by routine health information system. WHO South-East Asia J Public Health. 2021;10:93. 10.4103/2224-3151.309884 [DOI] [Google Scholar]
- 28.Angeles G, Silverstein H, Ahsan KZ, Kibria MG, Rakib NA, Escudero G, et al. Estimating the effects of COVID-19 on essential health services utilization in Uganda and Bangladesh using data from routine health information systems. Front Public Health. 2023;11:1129581. 10.3389/fpubh.2023.1129581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naqvi S, Naqvi F, Saleem S, Thorsten VR, Figueroa L, Mazariegos M, et al. Health care in pregnancy during the COVID-19 pandemic and pregnancy outcomes in six low-and-middle-income countries: Evidence from a prospective, observational registry of the Global Network for Women’s and Children’s Health. BJOG. 2022;129:1298–307. 10.1111/1471-0528.17175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aranda Z, Binde T, Tashman K, Tadikonda A, Mawindo B, Maweu D, et al. Disruptions in maternal health service use during the COVID-19 pandemic in 2020: experiences from 37 health facilities in low-income and middle-income countries. BMJ Glob Health. 2022;7:e007247. 10.1136/bmjgh-2021-007247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thsehla E, Balusik A, Boachie MK, Tombe-Mdewa W, Kabudula C, Du Toit J, et al. Indirect effects of COVID-19 on maternal and child health in South Africa. Glob Health Action. 2023;16:2153442. 10.1080/16549716.2022.2153442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hassan MZ, Monjur MR, Styczynski AR, Rahman M, Banu S.Protecting frontline healthcare workers should be the top priority in low-resource health systems: Bangladesh and COVID-19. Infect Control Hosp Epidemiol. 2021;42:121–2. 10.1017/ice.2020.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reza HM, Sultana F, Khan IO.Disruption of healthcare amid COVID-19 pandemic in Bangladesh. Open Public Health J. 2020;13:438–440. 10.2174/1874944502013010438 [DOI] [Google Scholar]
- 34.Nguyen PH, Sununtnasuk C, Pant A, Tran Mai L, Kachwaha S, Ash D, et al. Provision and utilisation of health and nutrition services during COVID-19 pandemic in urban Bangladesh. Matern Child Nutr. 2021;17:e13218. 10.1111/mcn.13218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahmmed MM, Babu MA, Ferdosy J.Direct and indirect effects of COVID-19 on maternal and child health in Bangladesh. Journal of Statistics and Management Systems. 2021;24:175–92. 10.1080/09720510.2020.1833465 [DOI] [Google Scholar]
- 36.Al-Zaman MS.Healthcare crisis in Bangladesh during the COVID-19 pandemic. Am J Trop Med Hyg. 2020;103:1357. 10.4269/ajtmh.20-0826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emmanuel F, Ahmad A, Reza T, Shahzad K, Rehman FU, Malik M, et al. Indirect effects of COVID-19 pandemic on reproductive, maternal, newborn and child health services in Pakistan. East Mediterr Health J. 2022;28:258–65. 10.26719/emhj.22.011 [DOI] [PubMed] [Google Scholar]
- 38.Shaik ME, Hossain QS, Rony GFF.Impact of COVID-19 on public transportation and road safety in Bangladesh. SN Comput Sci. 2021;2:453. 10.1007/s42979-021-00849-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hategeka C, Carter SE, Chenge FM, Katanga EN, Lurton G, Mayaka SM-N, et al. Impact of the COVID-19 pandemic and response on the utilisation of health services in public facilities during the first wave in Kinshasa, the Democratic Republic of the Congo. BMJ Glob Health. 2021;6:e005955. 10.1136/bmjgh-2021-005955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wagenaar BH, Augusto O, Beste J, Toomay SJ, Wickett E, Dunbar N, et al. The 2014–2015 Ebola virus disease outbreak and primary healthcare delivery in Liberia: Time-series analyses for 2010–2016. PLoS Med. 2018;15:e1002508. 10.1371/journal.pmed.1002508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shapira G, Ahmed T, Drouard SHP, Amor Fernandez P, Kandpal E, Nzelu C, et al. Disruptions in maternal and child health service utilization during COVID-19: analysis from eight sub-Saharan African countries. Health Policy Plan. 2021;36:1140–51. 10.1093/heapol/czab064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Y-T, Yen Y-F, Yu S-H, Chia-Yu Su E.A flexible lockdown by integrating public health and economic reactivation to response the crisis of COVID-19: responses to comments by Alvaro J Idrovo on “An examination on the transmission of COVID-19 and the effect of response strategies: a comparative analysis”. Int J Environ Res Public Health. 2020;17:8068. 10.3390/ijerph17218068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Akter MB, Mahmud A, Karim MR.Determinants of Antenatal Care Visits in Bangladesh: A Quantile Regression Analysis. Health Serv Res Manag Epidemiol. 2023;10:23333928231168119. 10.1177/23333928231168119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhowmik KR, Das S, Islam MA.Modelling the number of antenatal care visits in Bangladesh to determine the risk factors for reduced antenatal care attendance. PLoS One. 2020;15:e0228215. 10.1371/journal.pone.0228215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sarker BK, Rahman M, Rahman T, Rahman T, Khalil JJ, Hasan M, et al. Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh. PLoS One. 2020;15:e0241185. 10.1371/journal.pone.0241185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Institute of Population Research and Training; Medical Education and Family Welfare Division; Ministry of Health and Family Welfare. Bangladesh Demographic and Health Survey 2022: Key Indicators Report. Dhaka: National Institute of Population Research and Training; 2023. [Google Scholar]
- 47.Billah SM, Haque R, Chowdhury AI, Siraj MS, Rahman QS, Hossain T, et al. Setting up a maternal and newborn registry applying electronic platform: an experience from the Bangladesh site of the global network for women’s and children’s health. Reprod Health. 2020;17:148. 10.1186/s12978-020-00993-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mboera LE, Rumisha SF, Mbata D, Mremi IR, Lyimo EP, Joachim C.Data utilisation and factors influencing the performance of the health management information system in Tanzania. BMC Health Serv Res. 2021;21:498. 10.1186/s12913-021-06559-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Odei-Lartey EO, Prah RKD, Anane EA, Danwonno H, Gyaase S, Oppong FB, et al. Utilization of the national cluster of district health information system for health service decision-making at the district, sub-district and community levels in selected districts of the Brong Ahafo region in Ghana. BMC Health Serv Res. 2020;20:514. 10.1186/s12913-020-05349-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bhattacharya AA, Umar N, Audu A, Felix H, Allen E, Schellenberg JR, et al. Quality of routine facility data for monitoring priority maternal and newborn indicators in DHIS2: a case study from Gombe state, Nigeria. PLoS One. 2019;14:e0211265. 10.1371/journal.pone.0211265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ohiri K, Ukoha NK, Nwangwu CW, Chima CC, Ogundeji YK, Rone A, et al. An assessment of data availability, quality, and use in malaria program decision making in Nigeria. Health Syst Reform. 2016;2:319–30. 10.1080/23288604.2016.1234864 [DOI] [PubMed] [Google Scholar]
- 52.Barua M, Saha A, Chowdhury S, Chowdhury S, Sajow SH, Sarker M.Implementation of a community-based referral project to improve access to emergency obstetric and newborn care in Rohingya population during COVID-19 pandemic in Bangladesh. BMJ Innov. 2022;8:247–254. 10.1136/bmjinnov-2021-000831 [DOI] [PubMed] [Google Scholar]
- 53.Palo SK, Dubey S, Negi S, Sahay MR, Patel K, Swain S, et al. Effective interventions to ensure MCH (Maternal and Child Health) services during pandemic related health emergencies (Zika, Ebola, and COVID-19): A systematic review. PLoS One. 2022;17:e0268106. 10.1371/journal.pone.0268106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahsan KZ, Tahsina T, Iqbal A, Ali NB, Chowdhury SK, Huda TM, et al. Production and use of estimates for monitoring progress in the health sector: the case of Bangladesh. Glob Health Action. 2017;10:1298890. 10.1080/16549716.2017.1298890 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.