Abstract
Objective
To conduct a comprehensive review of the literature on childhood risk factors and their associations with adulthood subclinical and clinical cardiovascular disease (CVD).
Study design
A systematic search was performed using the MEDLINE, EMBASE, PsycINFO, CINAHL, and Web of Science databases to identify English-language articles published through June 2018. Articles were included if they were longitudinal studies in community-based populations, the primary exposure occurred during childhood, and the primary outcome was either a measure of subclinical CVD or a clinical CVD event occurring in adulthood. Two independent reviewers screened determined whether eligibility criteria were met.
Results
There were 210 articles that met the predefined criteria. The greatest number of publications examined associations of clinical risk factors, including childhood adiposity, blood pressure, and cholesterol, with the development of adult CVD. Few studies examined childhood lifestyle factors including diet quality, physical activity, and tobacco exposure. Domains of risk beyond “traditional” cardiovascular risk factors, such as childhood psychosocial adversity, seemed to have strong published associations with the development of CVD.
Conclusions
Although the evidence was fairly consistent in direction and magnitude for exposures such as childhood adiposity, hypertension, and hyperlipidemia, significant gaps remain in the understanding of how childhood health and behaviors translate to the risk of adulthood CVD, particularly in lesser studied exposures like glycemic indicators, physical activity, diet quality, very early life course exposure, and population subgroups.
Cardiovascular disease (CVD) is the leading cause of death in the US: more than 1 million adults experience coronary events and more than 800 000 adults experience strokes each year.1 Although childhood clinical CVD is rare, CVD events that occur in adulthood, including myocardial infarction and stroke, are the products of the lifelong atherosclerotic process that begins in youth.2 Thus, the prevention and management of childhood risk factors and preservation of cardiovascular health across the lifespan are pediatric care priorities.3
Recognizing the early origins of CVD risk, research studies have begun to address the complex processes of risk development across the life course.4,5 Identifying childhood risk factors that are most strongly linked to the development of adult CVD can provide scientific evidence for childhood intervention, whereas identifying risk factors for which long-term data are sparse may guide future investigation.
Our objectives were to provide a comprehensive review of the existing literature on associations of childhood risk factors with adulthood subclinical and clinical CVD and identify evidence of emerging disparities in CVD risk as individuals age from childhood into adulthood, including age, sex, and race/ethnicity. The literature search and review was based on known adult risk factors for CVD, potential risk factors as stated in pediatric guidelines, and developmental factors arising at birth that may significantly impact the risk of adult CVD.3,6
Methods
A literature search was conducted using the MEDLINE, EMBASE, PsycINFO, CINAHL, and Web of Science databases to identify English-language articles published through June 2018. A research librarian assisted in planning the search and created correct search strings for the electronic databases. A full list of the search terms appears in Table I (available at www.jpeds.com). We did not search for unpublished articles nor did we review reference lists of included articles to identify additional studies. After deduplication, the search returned 8652 titles and abstracts.
Table I.
Review search terms
| Concepts | Terms |
|---|---|
|
| |
| Population at the time of exposure | fetal environment, birth, childhood through age 20 years Terms: child*, adolescen*, infan*, puberty, youth |
| Childhood exposure | Terms: metabolic syndrome, MetS, blood pressure, BP, hypertens*, cholesterol, lipid, hypercholesterolemia, dyslipidemia, hyperlipidemia, triglycerides, statin, glucose, glycemic, diabet*, insulin, adiposity, obes*, weight, waist circumference, BMI, body mass index, body composition, body size, diet*, nutri*, food*, intake, beverage*, physical activit*, exercise, fitness, sedentary, acceleromet*, smok*, cigar*, tobacco, secondhand, cotinine, preterm, birthweight, gestation*, breastfeed*, advers*, adverse childhood experiences, emotional distress, socioeconomic*, parental death, in utero |
| Population at the time of outcome | adulthood age 20 years and older Terms: adult*, middle age, older age |
Articles were included if they met the following a priori criteria: (1) longitudinal study design; (2) exposure occurred/characteristic emerged during childhood (infancy through age 20 years); (3) outcome ascertained in adulthood (ages ≥20 years); (4) the primary outcome was either a measure of subclinical CVD or a clinical CVD event; and (5) the study population was community based, not a clinically defined population (eg, patients with congenital heart disease). Descriptions of the included clinical and subclinical CVD outcomes and their common measurement methods are outlined in Table II. Articles that included multiple subtypes of CVD (eg, coronary heart disease [CHD] and stroke) in the outcome without estimating the association for each subtype of CVD separately were classified as having a CVD mixed definition outcome and were included in this review. Studies that only included as the main outcome CVD risk factors, such as hypertension or diabetes, were not included in this review.
Table II.
Description of adulthood clinical and subclinical CVD outcomes included in the literature review
| Characteristics | Description | Common clinical presentation |
|---|---|---|
|
| ||
| Types of clinical CVD | ||
| CHD also known as ischemic heart disease, coronary artery disease | Reduced blood flow to the heart due to narrowing or obstruction of the coronary arteries (atherothrombosis) | Myocardial infarction, angina, sudden cardiac death |
| Stroke | Reduced blood flow to the brain due to a blockage or rupture of the arteries supplying the brain | Ischemic stroke, hemorrhagic stroke, transient ischemic attack |
| Heart failure | Inability of the heart to supply body’s circulatory needs, commonly due to heart muscle pump dysfunction or inadequate relaxation | Congestive heart failure - syndrome manifested by shortness of breath, decreased exertional tolerance, and/or peripheral edema |
| Measurement methods | ||
| Arterial stiffness | Reduced elasticity of the large arteries | Pulse wave velocity - speed that systolic BP wave travels through the vascular system body. Distensibility and compliance - measures of volume and pressure in an artery during heart muscle contraction |
| Arterial wall thickness | Thickening of the large arterial walls, tracks the presence and progression of atherosclerosis | cIMT, the thickness of innermost 2 layers of the wall of the artery, where atherosclerosis develops |
| Arterial calcification | Build-up of calcium in the large arteries, marker of atherosclerosis | Coronary artery calcium scan determines the area and density of calcium deposits, which correlates with overall coronary plaque burden |
| Endothelial dysfunction | Ability of the small arteries to dilate and constrict properly | Flow mediated dilation - measures the ability of the artery to dilate as blood flow increases after ischemia |
| LV structure and function | Enlarged mass and thickness of the walls of the left ventricle (hypertrophy) and reduced volume of blood pumped from the left ventricle (ejection fraction) are subclinical signs of heart failure | Echocardiography - produces images of the left ventricle to measure: LV mass, LV hypertrophy, Relative wall thickness, LV ejection fraction |
Titles and abstracts were reviewed to assess for the defined eligibility criteria. After review, full-text was retrieved for 884 articles. Two independent reviewers screened all full-text articles to ensure all eligibility criteria were met. Inter-rater agreement of this screening was high (Cohen K = 0.89). A third reviewer resolved discrepancies for the 34 articles that were left unresolved by the initial review. Ultimately, 210 articles were included in the review (Figure 1; available at www.jpeds.com).
Figure 1.
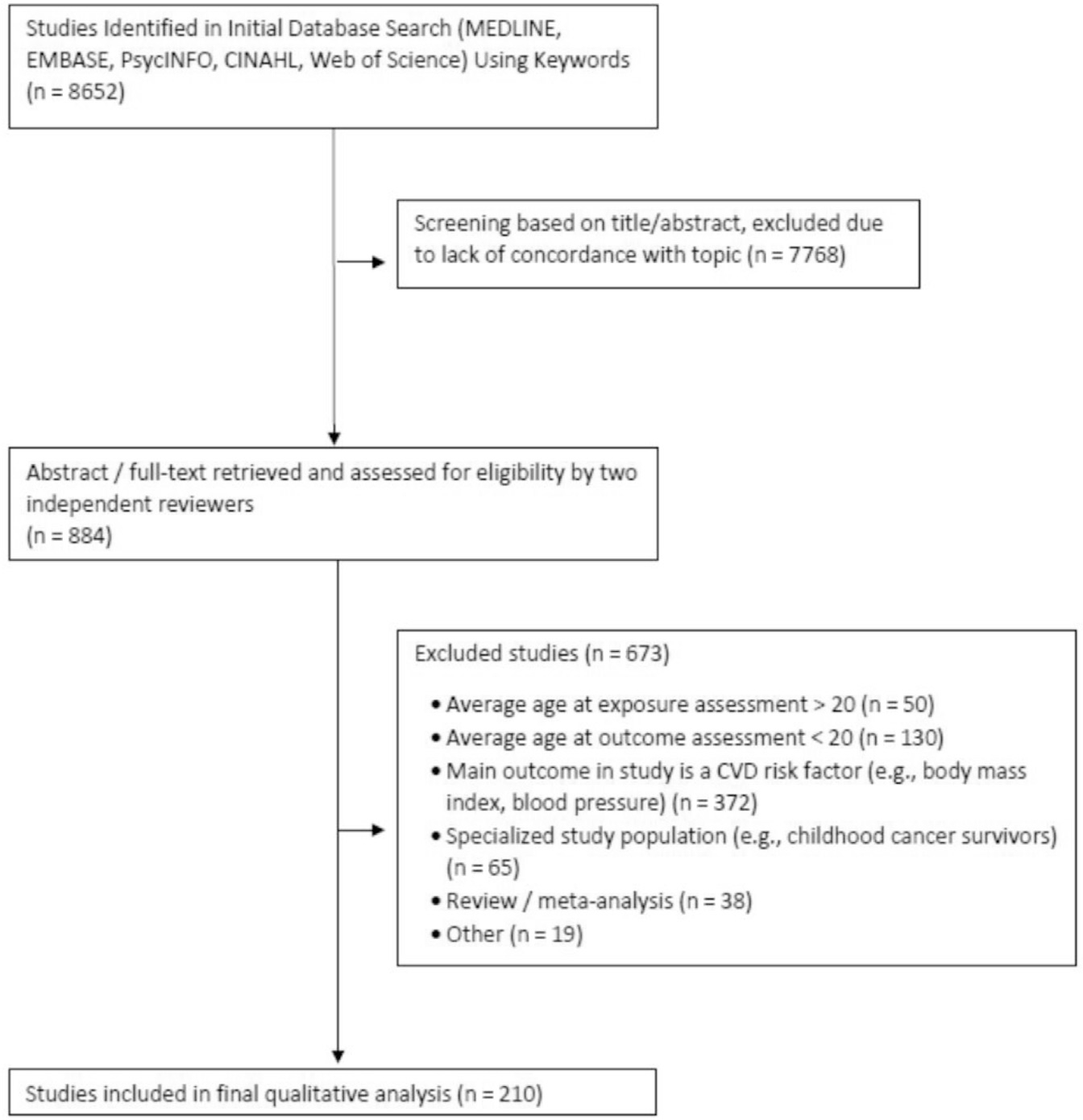
The CONSORT diagram illustrates the review search and extraction process, from the initial database search to the studies included in the final qualitative analysis.
Results
A listing of all articles included in this review is available in Table III (available at www.jpeds.com). This table includes the basic study characteristics of study cohort, sample size, exposure, outcome, and main finding; a listing of any subgroup analyses by age, sex, and race/ethnicity that were reported in the article; and 3 study quality indicators, namely, self-reported or objective exposure and outcome measurements, and type of outcome analysis. Figure 2 is the corresponding heat map by childhood risk factor and adulthood outcome, color coded by number of publications.
Table III.
Listing of all articles described and cited in the main text
| References | Year | Study cohort | Sample size | Exposure(s) measured in childhood | Type of exposure measurement (objective vs self-reported) | Outcome(s) measured in adulthood | Type of outcome measurement (objective vs self-reported) | Type of outcome analysis | Main finding(s) | Population subgroup analyses |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group | Sex | Race/ ethnicity | ||||||||||
|
| ||||||||||||
| Ceponiene et al7 | 2015 | Kaunas Cardiovascular Risk Cohort study | 380 | BP, adiposity | Objective | cIMT arterial stiffness | Objective | Continuous outcome | Higher BP and BMI associated with thicker cIMT in women only higher BP and BMI null association with PWV, both sexes | X | ||
| Yan et al8 | 2017 | Beijing Blood Pressure Cohort | 1252 | BP adiposity | Objective | cIMT arterial stiffness | Objective | Categorical outcome | Higher SBP and BMI associated with thicker cIMT, both sexes higher SBP associated with greater PWV, both sexes BMI null association with PWV, both sexes | X | ||
| Ferreiraet al9 | 2004 | Amsterdam Growth and Health Longitudinal Study | 159 | Adiposity | Objective | cIMT arterial stiffness | Objective | Categorical outcome | Higher BMI associated with thicker cIMT BMI null association with PWV no differences by sex |
X | ||
| Huynh et al10 | 2013 | Childhood Determinants of Adult Health (CDAH) | 2328 | Adiposity | Objective | cIMT arterial stiffness | Objective | Continuous outcome | Higher BMI associated with thicker cIMT BMI null association with PWV no differences by sex |
X | ||
| Ferreira et al11 | 2012 | Amsterdam Growth and Health Longitudinal Study | 373 | BP adiposity | Objective | Arterial stiffness | Objective | Continuous outcome | Highest tertile arterial stiffness had greater mean SBP, and greater mean BMI | |||
| Juonala et al12 | 2005 | The Cardiovascular Risk in Young Finns Study | 2255 | BP adiposity multiple risk factors | Objective | Arterial stiffness | Objective | Continuous outcome | Higher SBP and skinfold thickness associated with reduced arterial compliance greater number of risk factors associated with reduced arterial compliance | |||
| Vianna et al13 | 2014 | Pelotas (Brazil) Birth Cohort Study | 3701 | Breastfeeding, birthweight, adiposity | Self-reported | Arterial stiffness | Objective | Continuous outcome | Null association between breastfeeding or birthweight and PWV higher relative weight gain associated with greater arterial stiffness | |||
| Su et al14 | 2014 | YOung TAiwanese Cohort (YOTA) Study | 789 | Adiposity | Objective | cIMT | Objective | Categorical outcome | Childhood overweight and obesity associated with high cIMT | |||
| Hao et al15 | 2018 | Georgia Stress and Heart study | 626 | Adiposity | Objective LV | cIMT structure and function | Objective | Continuous outcome | Higher BMI groups associated with thicker cIMT and greater LV mass index | |||
| Raitakari et al16 | 2003 | The Cardiovascular Risk in Young Finns Study | 2229 | Lipids BP adiposity tobacco exposure multiple risk factors | Objective | cIMT | Objective | Continuous outcome | Greater LDL-C, SBP, BMI, smoking, and number of risk factors present was associated with thicker cIMT in men and women, when stratified by age groups 39 years and 12–18 years, only significant in 1218 years | X | X | |
| Oren et al17 | 2003 | Atherosclerosis Risk in Young Adults (ARYA) | 750 | Adiposity | Objective | cIMT | Objective | Continuous outcome | A 1-SD increase in BMI associated with thicker cIMT | |||
| Juonala et al18 | 2011 | Combined cohort of Bogalusa Heart Study, Muscatine Heart Study, Childhood Determinants of Adult Health, and Cardiovascular Risk in Young Finns Study | 6328 | Adiposity | Objective | cIMT | Objective | Event rate | Overweight/obese associated with thicker cIMT as compared with normal weight no differences by sex | X | ||
| Li et al19 | 2003 | Bogalusa Heart Study | 486 | Adiposity BP lipids | Objective | cIMT | Objective | Categorical outcome | Higher LDL-C and BMI associated with high cIMT; null association for SBP, HDL-C, triglycerides | |||
| Koskinen et al20 | 2018 | combined cohort of Bogalusa Heart Study, the Insulin Study, Childhood Determinants of Adult Health, and Cardiovascular Risk in Young Finns Study | 2893 | Adiposity BP lipids | Objective | cIMT | Objective | Event rate | Prehypertension, hypertension, overweight, obesity, borderline high LDL- cholesterol , high LDL-cholesterol and borderline low HDL-cholesterol associated with thicker cIMT; triglycerides not associated with cIMT | |||
| Juonala et al21 | 2010 | Combined cohort of Bogalusa Heart Study, Muscatine Heart Study, Childhood Determinants of Adult Health, and Cardiovascular Risk in Young Finns Study | 4380 | Adiposity BP lipids multiple risk factors | Objective | cIMT | Objective | Categorical outcome | Higher BMI, SBP associated with thicker cIMT; higher total cholesterol and number of risk factors only associated with thicker cIMT in exposure age 9–18; no association for triglycerides no sex differences | X | X | |
| Juonala et al22 | 2010 | Cardiovascular Risk in Young Finns Study | 1809 | Adiposity lipids physical activity diet multiple risk factors | Objective | cIMT | Objective | Continuous outcome | Low HDL-C, obesity, low physical activity, infrequent fruit consumption, and number of risk factors associated with thicker cIMT; no association for LDL-C or triglycerides no sex differences | X | ||
| Juonala et al23 | 2006 | Cardiovascular Risk in Young Finns Study | 2260 | Adiposity | Objective | cIMT | Objective | Continuous outcome | Overweight/obese associated with thicker cIMT as compared with normal weight | |||
| Freedman et al24 | 2004 | Bogalusa Heart Study | 513 | Adiposity | Objective | cIMT | Objective | Continuous outcome | Higher BMI associated with thicker cIMT, more strongly associated among women than men, and among White subjects than Blacks, and among ages 15–18 years at exposure as compared with younger ages | X | X | X |
| Koskinen et al25 | 2014 | Cardiovascular Risk in Young Finns Study | 1617 | Adiposity MetS | Objective | cIMT | Objective | Event rate | Overweight/obese and MetS associated with thicker cIMT | |||
| Menezes et al26 | 2016 | Bogalusa Heart Study | 3264 | Adiposity | Objective | cIMT | Objective | Continuous outcome | Higher BMI associated with thicker cIMT no sex differences | |||
| Davis et al27 | 2001 | Muscatine Heart Study | 725 | Adiposity Lipids | Objective | cIMT | Objective | Categorical outcome | Higher BMI associated with thicker cIMT in women only higher LDL associated with thicker cIMT in both men and women | X | ||
| Johnson et al28 | 2014 | MRC National Survey of Health and Development Study | 1273 | Adiposity | Objective | cIMT | Objective | Categorical outcome | Higher BMI associated with thicker cIMT in males only, and only at exposure ages 4 and 20 | X | X | |
| Charakida et al29 | 2014 | MRC National Survey of Health and Development Study | 1273 | Adiposity | Objective | cIMT | Objective | Continuous outcome | Overweight/obese not associated with thicker cIMT | |||
| Sabo et al30 | 2014 | Fels Longitudinal Study | 697 | Adiposity BP | Objective | LV structure and function | Objective | Continuous outcome | Higher BMI associated with greater LV mass in both men and women, but not associated with wall thickness BP not associated with LV mass or thickness |
X | ||
| Yang et al31 | 2017 | Childhood Determinants of Adult Health | 8498 | Adiposity | Objective | LV structure and function | Objective | Continuous outcome | Higher BMI associated with worse cardias function | |||
| Hardy et al32 | 2016 | MRC National Survey of Health and Development Study | 1617 | Birth weight adiposity | Objective | LV structure and function | Objective | Continuous outcome | Birthweight not associated with LV mass no sex differences higher BMI associated with higher LV mass | X | ||
| Li et al33 | 2004 | Bogalusa Heart Study | 467 | Adiposity | Objective | LV structure and function | Objective | Continuous outcome | Higher BMI associated with greater LV mass, stronger association in Blacks as compared with Whites | X | ||
| Tapp et al34 | 2014 | Childhood Determinants of Adult Health | 181 | Adiposity | Objective | LV structure and function | Objective | Continuous outcome | Higher BMI associated with greater LV mass no sex differences | X | ||
| Lai et al35 | 2014 | Bogalusa Heart Study | 1061 | Adiposity BP | Objective | LV structure and function | Objective | Continuous outcome | Higher SBP and BMI associated with greater LV mass | |||
| Yan et al36 | 2017 | Beijing Blood Pressure Cohort | 1256 | Adiposity BP | Objective | LV structure and function | Objective | Categorical outcome | Higher SBP and BMI associated with LV hypertrophy | |||
| Zhang et al37 | 2017 | Bogalusa Heart Study | 710 | Adiposity | Objective | LV structure and function | Objective | Categorical outcome | Higher BMI associated with greater LV mass | |||
| Sivanandam et al38 | 2006 | Fifth- to eighth-grade students in the Minneapolis and St. Paul, Minnesota, public schools with top 15% BP | 132 | Adiposity | Objective | LV structure and function | Objective | Continuous outcome | Higher BMI associated with greater LV mass | |||
| Toprak et al39 | 2008 | Bogalusa Heart Study | 824 | Adiposity BP | Objective | LV structure and function | Objective | Categorical outcome | Higher BMI and DBP associated with LV hypertrophy, association stronger in Blacks as compared with Whites | X | ||
| Mahoney et al40 | 1996 | Muscatine Heart Study | 384 | Adiposity BP lipids | Objective | Coronary artery calcification | Objective | Categorical outcome | Higher BMI and SBP, and lower HDL-C associated with presence of coronary artery calcification no sex differences | X | ||
| Berenson et al41 | 2016 | Bogalusa Heart Study | 5991 | Adiposity BP | Objective | Clinical CVD: CHD | Objective | Categorical outcome | Higher BMI and BP associated with greater CHD death | |||
| Lawlor et al42 | 2006 | Combined cohort of the Boyd- Orr, Christ’s Hospital, Glasgow Alumni studies | 14 561 | Adiposity | Objective | Clinical CVD: CHD clinical CVD: stroke | Objective | Time to event | Higher BMI associated with greater rate of CHD death no association with rate of stroke death no sex differences | X | ||
| Andersen et al43 | 2010 | Danish and Finnish individuals born 1924–1976 | 216 771 | Birth weight adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Low birthweight and higher BMI associated with higher risk of CHD | |||
| Falkstedt et al44 | 2007 | Swedish military conscription between 1949 and 1951 | 49 321 | Adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Higher BMI associated with greater risk of CHD and stroke study sample includes men only | X | ||
| Eriksson et al45 | 1999 | Men who were born at the Helsinki University Central Hospital, 1924–1933 | 3641 | Birth weight adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Lower birthweight, higher BMI, and faster change in BMI across childhood associated with greater risk of CHD death study sample includes men only | X | ||
| Baker et al46 | 2007 | Copenhagen schoolchildren born from 1930 to 1976 | 289 044 | Adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Higher BMI associated with greater CHD risk; stronger associations for women vs men and those who had high BMI at age 13 vs age 7 years | X | X | |
| Crump et al47 | 2017 | Swedish military conscripts, 1969–1997 | 1 547 407 | Adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Overweight or obese associated with increased risk of CHD study sample includes men only | X | ||
| Must et al48 | 2012 | Third Harvard Growth Study | 1877 | Adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Overweight associated with increased risk of CHD, among men only | X | ||
| Osler et al49 | 2009 | Men born in Copenhagen, Denmark in 1953 | 9143 | Birth weight adiposity | Objective | Clinical CVD: CHD | Objective | Time to event | Low birthweight and higher BMI associated with higher risk of CHD study sample includes men only | X | ||
| Lawlor et al50 | 2005 | Aberdeen Children of the 1950’s Study | 11 106 | Adiposity | Objective | Clinical CVD: CHD clinical CVD: stroke | Objective | Time to event | Higher BMI not associated with CHD obesity associated with increased risk of stroke no sex differences | X | ||
| Park et al51 | 2013 | Three British birth cohorts, born in 1946,1958 and 1970 | 11 447 | Adiposity | Objective | Clinical CVD: CHD | Self-reported | Categorical outcome | Overweight not associated with risk of CHD | |||
| Gjaerde et al52 | 2017 | Copenhagen schoolchildren born from 1930–1987 | 307 677 | Adiposity | Objective | Clinical CVD: stroke | Objective | Time to event | Higher BMI and faster weight gain during childhood associated with risk of stroke no sex differences | X | ||
| Ohlsson et al53 | 2017 | Men born in Gothenburg, Sweden from 1945–1961 | 37 669 | Adiposity | Objective | Clinical CVD: stroke | Objective | Time to event | Faster weight gain in childhood associated with increased risk of stroke study sample includes men only | X | ||
| Crump et al54 | 2016 | Swedish military conscripts, 1969–1997 | 1 547 294 | Adiposity | Objective | Clinical CVD: stroke | Objective | Time to event | Overweight or obese associated with increased risk of stroke study sample contains men only | X | ||
| Hogstrom et al55 | 2015 | Swedish military conscription between 1969–1986 | 811 579 | Adiposity diabetes | Objective | Clinical CVD: stroke | Objective | Time to event | Higher BMI and type 2 diabetes associated with increased risk of stroke study sample contains men only | X | ||
| Crump et al56 | 2017 | Military conscripts in Sweden during 1969–1997 | 1 330 610 | Adiposity | Objective | Clinical CVD: heart failure | Objective | Time to event | Higher BMI associated with higher risk of heart failure study sample contains men only | X | ||
| Rosengren et al57 | 2017 | Military conscripts in Sweden during 1968–2005 | 1 610 437 | Adiposity | Objective | Clinical CVD: heart failure | Objective | Time to event | Higher BMI associated with higher risk of heart failure study sample contains men only | X | ||
| Twig et al58 | 2017 | military conscripts in ISRAEL during 1967–2010 | 2 294 139 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Higher BMI associated with higher risk of CVD no sex differences | X | ||
| Bjorge et al59 | 2008 | National tuberculosis screening in Norway, 1963–1975 | 226 678 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Obesity associated with greater risk of CVD death no sex differences | X | ||
| Twig et al60 | 2016 | Military conscripts in Israel during 1967–2010 | 2 298 130 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Higher BMI associated with higher risk of CVD death | |||
| Batty G et al61 | 2016 | 1947 Scottish Mental Survey | 3839 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Higher weight at age 11 years was associated greater CVD mortality | |||
| Gunnell et al62 | 1998 | Boyd Orr cohort | 2399 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Obesity associated with greater risk of CVD death stronger association in exposure age >8 years than younger than 8 years | X | ||
| Imai et al63 | 2014 | Icelanders born between 1921 and 1935 and living in Reykjavik | 1924 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Faster BMI velocity associated with greater risk of CVD mortality no sex differences | X | ||
| Zheng et al64 | 2017 | Combined cohort of the Nurses’ Health Study and the Health Professionals Follow-up Study | 122 498 | Adiposity | Self-reported | Clinical CVD: mixed definition | Self-reported | Time to event | Those who had higher BMI in childhood had greater risk of CVD, stronger associations for women as compared with men | X | ||
| Must et al65 | 1992 | Third Harvard Growth Study | 508 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Higher BMI associated with greater CVD mortality risk, among men only | X | ||
| Morrison et al66 | 2012 | Princeton Lipid Research Clinics Follow-Up Study | 770 | Adiposity | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | High BMI associated with higher CVD risk | |||
| Furer et al67 | 2018 | Military conscripts in Israel during 1967–2010 | 2 294 139 | Adiposity | Objective | Clinical CVD: mixed definition | Objective | Time to event | Higher BMI associated with higher CVD mortality no sex differences | X | ||
| Bhuiyan et al68 | 2010 | Bogalusa Heart Study | 538 | Birth weight | Objective | Arterial stiffness | Objective | Continuous outcome | Low birthweight associated with reduced arterial compliance | X | X | |
| Rich-Edwards et al69 | 1997 | Nurses’ Health Study | 70 297 | Birth weight | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low birth weight associated with increased risk of nonfatal CVD study sample included women only | X | ||
| Lawani et al70 | 2014 | Atherosclerosis Risk in Communities | 10 132 | Birth weight | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low birth weight associated with higher risk of atrial fibrillation | |||
| Larsson et al71 | 2015 | Swedish Inpatient Register cohort | 53 005 | Birth weight | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Both low birth weight and high birth weight associated with increased risk of atrial fibrillation, among men only | X | ||
| Baker J et al72 | 2008 | Danish schoolchildren born from 1936–1979 | 216 464 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Time to event | Both low and high birth weight associated with increased CVD mortality no sex differences | X | ||
| Lawlor et al73 | 2004 | British women’s heart and health study | 1394 | Birth weight | Self-reported | Clinical CVD: CHD | Self-reported | Categorical outcome | Low birth weight was associated with greater CHD risk study sample included women only | X | ||
| Lawlor et al74 | 2005 | Aberdeen Children of the 1950’s Study | 10 803 | Birth weight | Objective | Clinical CVD: CHD | Objective | Time to event | Low birth weight was associated with greater CHD risk | |||
| Oberg et al75 | 2011 | Population-based cohort of like- sexed twinswith known zygosity born in Sweden from 1926 to 1958 | 23 689 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Categorical outcome | Birth weight was found to be inversely associated with risk of CVD within dizygotic but not monozygotic twin pairs | |||
| Syddall et al76 | 2005 | Hertfordshire Cohort Study | 37 615 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Time to event | Each SD lower birth weight associated with increased risk of CVD mortality no sex differences | X | ||
| Frankel et al77 | 1996 | Caerphilly Heart Disease Study | 1258 | Birth weight | Self-reported | Clinical CVD: CHD | Self-reported | Categorical outcome | Low birth weight associated with higher risk of CHD when adult BMI is also elevated study sample includes men only | X | ||
| Rajaleid et al78 | 2008 | Uppsala Birth Cohort | 11 822 | Birth weight | Objective | Clinical CVD: CHD | Objective | Time to event | Low birth weight associated with higher risk of CHD mortality, only present in higher social class men | X | ||
| Eriksson et al79 | 2001 | Helsinki Birth Cohort | 4630 | Birth weight | Objective | Clinical CVD: CHD | Objective | Time to event | Lower birthweight associated with higher risk of CHD study sample includes men only | X | ||
| Osmond et al80 | 1993 | Hertfordshire Cohort Study | 4630 | Birth weight | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | Low birthweight associated with higher risk of CVD no sex differences | X | ||
| Johnson et al81 | 2011 | Panel Study of Income Dynamics | 4387 | Birth weight SES | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | Low birth weight and childhood poverty associated with higher risk of CVD | |||
| Forsen et al82 | 1999 | Women born in Helsinki University Central Hospital during 1924–33 | 3447 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Time to event | Both low birth weight associated with increased risk of CHD study sample includes only women | X | ||
| Osmond et al83 | 2007 | Helsinki Birth Cohort | 12 439 | Birth weight adiposity | Objective | Clinical CVD: stroke | Objective | Time to event | Low birth weight and slow growth in first 2 years after birth associated with increased risk of stroke no sex differences | X | ||
| Koupilova et al84 | 1999 | Uppsala Birth Cohort | 1334 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Time to event | Low birth weight associated with higher CVD mortality study sample includes only men | X | ||
| Rich-Edwards et al85 | 2005 | Nurses’ Health Study | 66 111 | Birth weight | Self-reported | Clinical CVD: CHD clinical CVD: stroke | Objective | Time to event | Low birth weight associated with higher risk of CHD, but no association with stroke study sample includes onlywomen | X | ||
| Arnold et al86 | 2016 | Prospective cohort in a remote Indigenous Australian community | 852 | Birth weight | Objective | Clinical CVD: mixed definition | Objective | Time to event | Low birth weight associated with higher risk of CVD, stronger association for women as compared with men | X | ||
| Zoller et al87 | 2015 | National cohort study of individuals who were live- born in Sweden in 1973 through 1992 | 1 984 858 | Birth weight | Objective | Clinical CVD: CHD | Objective | Time to event | Low birth weight associated with higher risk of CHD | |||
| Leon et al88 | 1998 | Uppsala Birth Cohort | 14 611 | Birth weight | Objective | Clinical CVD: CHD | Objective | Time to event | Low birth weight associated with higher risk of CHD, among men only | X | ||
| Smith et al89 | 2016 | The Women’s Health Initiative | 63 815 | Birth weight | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low birth weight was associated with increased risk of CVD, associations less strong for Hispanic and African American women study sample includes onlywomen | X | X | |
| Hypponen et al90 | 2001 | Uppsala Birth Cohort | 14 611 | Birth weight | Objective | Clinical CVD: stroke | Objective | Time to event | Low birth weight was associated with increased risk of stroke | |||
| Forsen et al91 | 2004 | Helsinki Birth Cohort | 2345 | Weight gain | Objective | Clinical CVD: CHD | Objective | Time to event | Lower weight gain in infancy associated with increased risk of CHD study sample included men only | X | ||
| Forsen et al92 | 2004 | Helsinki Birth Cohort | 4130 | Weight gain | Objective | Clinical CVD: CHD | Objective | Time to event | Lower weight gain in infancy associated with increased risk of CHD study sample included women only | X | ||
| Leunissen et al93 | 2012 | PROgramming factors for GRowth And Metabolism (PROGRAM) study | 323 | Weight gain | Self-reported | cIMT | Objective | Continuous outcome | Faster weight gain in childhood associated with thicker cIMT | |||
| Terzis et al94 | 2012 | Cohort from Athens, Greece recruited in 1983 | 106 | Weight gain | Self-reported | cIMT | Objective | Continuous outcome | Faster weight gain in childhood associated with thicker cIMT | |||
| Chu et al95 | 2017 | Hanzhong adolescent hypertension cohort | 4623 | BP | Objective | Arterial stiffness | Objective | Continuous outcome | Higher SBP associated with greater arterial stiffness | |||
| Xi et al96 | 2017 | Bogalusa Heart Study | 1225 | BP | Objective | cIMT arterial stiffness LV structure and function | Objective | Time to event | Pediatric hypertension associated with high cIMT, greater arterial stiffness, and LV hypertrophy | |||
| Liang et al97 | 2014 | Beijing Blood Pressure Cohort | 1259 | BP | Objective | cIMT arterial stiffness LV structure and function | Objective | Categorical outcome | Pediatric hypertension associated with high cIMT, greater arterial stiffness, and LV hypertrophy | |||
| Li et al98 | 2004 | Bogalusa Heart Study | 835 | BP | Objective | Arterial stiffness | Objective | Categorical outcome | Higher SBP associated with greater arterial stiffness | |||
| Aatola et al99 | 2017 | Cardiovascular Risk in Young Finns Study | 1540 | BP | Objective | arterial stiffness | Objective | Event rate | High BP not associated with arterial stiffness, unless adult BP levels were also high; no sex differences | X | ||
| Aatola et al100 | 2013 | Cardiovascular Risk in Young Finns Study | 1241 | BP | Objective | Arterial stiffness | Objective | Categorical outcome | High BP associated with greater arterial stiffness | |||
| Vos et al101 | 2003 | Atherosclerosis Risk in Young Adults (ARYA) | 750 | BP | Objective | cIMT | Objective | Continuous outcome | Higher BP associated with thicker cIMT | |||
| Hao et al102 | 2017 | Georgia Stress and Heart study | 551 | BP | Objective | cIMT LV structure and function | Objective | Continuous outcome | Higher BP associated with thicker cIMT and greater LV mass no sex differences | X | ||
| Juhola et al103 | 2013 | International Childhood Cardiovascular Cohort Consortium | 4210 | BP | Objective | cIMT | Objective | Event rate | High BP associated with thicker cIMT | |||
| Hartiala et al104 | 2012 | Young Finns | 589 | BP lipids | Objective | Higher SBP and LDL- C associated with coronary artery calcification | Objective | Categorical outcome | Higher SBP associated with presence of coronary artery calcification | |||
| Magnussen et al105 | 2014 | prospective cohort of 181 individuals | 181 | BP lipids | Objective | LV structure and function | Objective | Continuous outcome | Higher triglycerides and higher DBP associated with greater LV mass | |||
| Sundstrom et al106 | 2011 | Swedish military conscription between 1969–1995 | 1207329 | BP | Objective | Clinical CVD: mixed definition | Objective | Time to event | BP associated with increased CVD study sample includes men only | X | ||
| Silventoinen et al107 | 2008 | Swedish military conscription between 1969 and 1994 | 1 145 758 | BP | Objective | clinical CVD: mixed definition | Objective | Time to event | BP associated with increased CVD across levels of BMI, strongest in obese study sample includes men only | X | ||
| Leiba et al108 | 2016 | Israeli military conscription between 1967–2010 | 2 298 130 | BP | Objective | Clinical CVD: mixed definition | Objective | Time to event | Pediatric hypertension associated with increased risk of CVD mortality | |||
| Erlingsdottir et al109 | 2010 | Children admitted to Landspitali University Hospital in Iceland for elective surgical procedures between 19501967 | 126 | BP | Objective | Clinical CVD: CHD | Self-reported | Categorical outcome | Pediatric hypertension associated with increased risk of CHD | |||
| Juonala et al110 | 2008 | Cardiovascular Risk in Young Finns Study | 2265 | lipids Multiple risk factors | Objective | cIMT) | Objective | Continuous outcome | Type IIb dyslipidemia associated with thicker cIMT higher number of risk factors associated with thicker cIMT | |||
| Li et al111 | 2007 | Bogalusa Heart Study | 868 | Lipids | Objective | cIMT | Objective | Continuous outcome | Differences by race and sex in the association of lipids and thicker cIMT: White men, LDL-C and triglycerides significant; White women, LDL-C significant ; Black women, LDL-C significant; Black men, no significant association for any lipid levels | X | X | |
| Magnussen et al112 | 2009 | Combined cohort of Bogalusa Heart Study, Childhood Determinants of Adult Health, and Cardiovascular Risk in Young Finns Study | 1711 | Lipids | Objective | cIMT | Objective | Categorical outcome | Dyslipidemia associated with thicker cIMT | |||
| Frontini et al113 | 2008 | Bogalusa Heart Study | 437 | lipids | Objective | cIMT | Objective | Categorical outcome | Higher LDL-C associated with high cIMT; no association for HDL-C and triglycerides | |||
| Morrison et al114 | 2012 | Princeton Lipid Research Clinics Follow-Up Study | 909 | Lipids | Objective | clinical CVD: mixed definition | Self-reported | Categorical outcome | High triglycerides associated with increased risk of CVD | |||
| Morrison et al115 | 2009 | Princeton Lipid Research Clinics Follow-Up Study | 808 | Lipids | Objective | Clinical CVD: mixed definition | Self-reported | Time to event | High triglycerides associated with increased risk of CVD | |||
| Yajnik et al116 | 2015 | Pune Children’s Study | 357 | Glycemic indicators | Objective | cIMT | Objective | Continuous outcome | Higher fasting glucose associated with thicker cIMT | |||
| McCarron et al117 | 2001 | Glasgow Alumni study | 8354 | Tobacco exposure | Objective | Clinical CVD: mixed definition | Objective | Time to event | All categories of smoking exposure associated with higher risk CVD, with significant linear trend for amount of smoking study sample included men only | X | ||
| Whitley et al118 | 2012 | Harvard Alumni Health Study | 28 236 | Tobacco exposure | Objective | Clinical CVD: mixed definition | Objective | Time to event | Smoking associated with higher risk of CVD mortality study sample included men only | X | ||
| Choi et al119 | 2017 | National Health Interview Survey linked to the National Death Index | 90 278 | Tobacco exposure | Self-reported | Clinical CVD: mixed definition | Objective | Categorical outcome | Current and former smokers who started smoking at or before age 16 had higher risk of CVD | X | ||
| Geerts et al120 | 2008 | Atherosclerosis Risk in Young Adults (ARYA) | 732 | Tobacco exposure | Self-reported | cIMT | Objective | Continuous outcome | In utero parental smoking exposure associated with thicker cIMT | |||
| Gall et al121 | 2014 | Cardiovascular Risk in Young Finns Study | 1375 | Tobacco exposure | Self-reported | cIMT | Objective | Continuous outcome | Greater exposure to parental smoking was associated with thicker cIMT | |||
| West et al122 | 2015 | Cardiovascular Risk in Young Finns Study | 2448 | Tobacco exposure | Self-reported | coronary artery calcification | Objective | Event rate | Greater exposure to parental smoking was associated with higher risk of presence of coronary artery calcification | |||
| Palve et al123 | 2014 | Cardiovascular Risk in Young Finns Study | 2416 | Physical activity | Objective | Arterial stiffness | Objective | Continuous outcome | Greater physical activity associated with lower arterial stiffness, among men only | X | ||
| van de Laar et al124 | 2011 | Amsterdam Growth and Health Longitudinal Study | 373 | Physical activity | Objective | Arterial stiffness | Objective | Continuous outcome | Vigorous activity associated with lower arterial stiffness, no associations for light/ moderate activity | |||
| van de Laar et al125 | 2010 | Amsterdam Growth and Health Longitudinal Study | 373 | Physical activity | Objective | Arterial stiffness | Objective | Continuous outcome | Vigorous activity associated with lower arterial stiffness | |||
| Ried-Larsen et al126 | 2015 | European Youth Heart Study, Danish participants only | 277 | Physical activity | Objective | Arterial stiffness | Objective | Continuous outcome | Higher physical activity levels associated with lower arterial stiffness | |||
| Drca et al127 | 2014 | Population-based cohort of Swedish men | 44 410 | Physical activity | Objective | clinical CVD: mixed definition | Objective | Time to event | No association between physical activity and atrial fibrillation study sample included men only | X | ||
| Aatola et al128 | 2010 | Cardiovascular Risk in Young Finns Study | 1622 | Diet | Objective | Arterial stiffness | Objective | Continuous outcome | Higher fruit and vegetable intake associated with lower arterial stiffness | |||
| van de Laar et al129 | 2012 | Amsterdam Growth and Health Longitudinal Study | 373 | Diet | Self-reported | Arterial stiffness | Objective | Continuous outcome | Lower intake of fiber associated with lower arterial stiffness | |||
| van de Laar et al130 | 2013 | Amsterdam Growth and Health Longitudinal Study | 373 | Diet | Self-reported | Arterial stiffness | Objective | Continuous outcome | Greater adherence to the Mediterranean diet pattern associated with lower arterial stiffness | |||
| McCourt et al131 | 2014 | Northern Ireland Young Hearts Project | 487 | Diet | Self-reported | Arterial stiffness | Objective | Continuous outcome | No association between adherence to Mediterranean diet pattern and arterial stiffness | |||
| Kaikkonen et al132 | 2013 | Cardiovascular Risk in Young Finns Study | 823 | Diet | Self-reported | cIMT | Objective | Continuous outcome | Saturated, monounsaturated, and polyunsaturated fat consumption associated with thicker cIMT, but omega-3 fatty acid consumption associated with less thick cIMT, among women only | X | ||
| Mikkila et al133 | 2009 | Cardiovascular Risk in Young Finns Study | 785 | Diet | Self-reported | cIMT | Objective | Continuous outcome | Traditional Finnish dietary pattern (characterized by intake of rye, potatoes, butter, milk, sausages, and coffee) was associated with thicker cIMT, among men only | X | ||
| van der Pols et al134 | 2009 | Boyd Orr cohort | 4374 | Diet | Self-reported | clinical CVD: mixed definition | Objective | Time to event | Diet high in calcium associated with lower risk of stroke mortality, no association with CHD mortality | |||
| Ness et al135 | 2005 | Boyd Orr cohort | 1234 | Diet | Self-reported | clinical CVD: stroke | Objective | Time to event | Higher intake of vegetables and lower intake of fish associated with lower risk of stroke death | |||
| Jarvisalo et al136 | 2009 | Cardiovascular Risk in Young Finns Study | 3596 | Breastfeeding | Self-reported | Endothelial function cIMT | Objective | Continuous outcome | Breastfeeding in infancy associated with higher endothelial function, among men only breastfeeding in infancy not associated with cIMT | X | ||
| Martin et al137 | 2005 | Boyd Orr cohort | 362 | Breastfeeding | Self-reported | cIMT | Objective | Continuous outcome | Breastfeeding in infancy associated with less thick cIMT | |||
| Rich-Edwards et al138 | 2004 | Nurses’ Health Study | 87252 | Breastfeeding | Self-reported | Clinical CVD: CHD clinical CVD: stroke | Objective | Time to event | Breastfeeding in infancy not associated with CHD or stroke | |||
| Martin et al139 | 2004 | Boyd Orr cohort | 3555 | Breastfeeding | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Breastfeeding in infancy not associated with CVD mortality | |||
| Fall et al140 | 1992 | Hertfordshire Cohort Study | 5718 | Breastfeeding | Self-reported | Clinical CVD: CHD | Objective | Event rate | Breastfeeding in infancy associated with CHD, but only among those who had weaned before 1 year study sample included men only | X | ||
| Kivimaki et al141 | 2005 | Cardiovascular Risk in Young Finns Study | 2290 | SES | Self-reported | cIMT | Objective | Continuous outcome | No association between SES and cIMT | |||
| Kivimaki et al142 | 2006 | Cardiovascular Risk in Young Finns Study | 1922 | SES | Self-reported | cIMT endothelial function | Objective | Continuous outcome | No association between SES and cIMT No association between SES and flow-mediated dilation No sex differences |
X | ||
| Laitinen et al143 | 2017 | Cardiovascular Risk in Young Finns Study | 1871 | SES | Self-reported | LV structure and function | Objective | Continuous outcome | Low family SES was associated with higher LV mass | |||
| Smith et al144 | 1998 | cohort of men aged 35–64 who were recruited from workplaces in the west of Scotland between 1970 and 1973 | 5766 | SES | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Father’s occupation status associated with risk of CHD and stroke mortality | |||
| Kittleson et al145 | 2006 | John Hopkins Precursors Study | 1131 | SES | Self-reported | Clinical CVD: CHD | Objective | Time to event | Low parental SES associated with increased incidence of CHD | |||
| Lynch et al146 | 1994 | Kuopio Ischaemic Heart Disease Risk Factor Study | 2636 | SES | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low parental SES associated with increased incidence of CVD only if adult SES also low Study sample included men only |
X | ||
| Gliksman et al147 | 1995 | Nurses’ Health Study | 117 006 | SES | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low childhood SES associated with higher risk of CVD Study sample included women only | X | ||
| Heshmati et al148 | 2017 | Uppsala Birth Cohort | 10 593 | SES | Self-reported | Clinical CVD: stroke | Objective | Time to event | Social mobility was associated with risk of stroke, among women only | X | ||
| Lawlor et al149 | 2006 | Aberdeen Children of the 1950’s Study | 12 150 | SES | Self-reported | clinical CVD: mixed definition | Objective | Time to event | Father’s occupation status associated with risk of CHD and stroke mortality | |||
| Melchior et al150 | 2006 | GAZEL Cohort Study | 20 570 | SES | Self-reported | clinical CVD: mixed definition | Objective | Time to event | Low SES only associated with higher risk of CVD if adult SES was also low | |||
| Kamphuis et al151 | 2012 | GLOBE study | 11 701 | SES | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Lowest group of childhood SES associated with higher risk of CVD mortality | |||
| Osler et al152 | 2003 | Project Metropoli | 11 376 | SES | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Low SES in early life was associated with higher CVD mortality risk | |||
| Anderson et al153 | 2018 | Avon Longitudinal Study of Parents and Children | 4957 | Psychosocial adversity | Self-reported | cIMT arterial stiffness |
Objective | Continuous | Cumulative psychosocial adversity in childhood not associated with cIMT or arterial stiffness; Study sample included women only |
X | ||
| Rotar et al154 | 2015 | survivors of the Leningrad siege with age-sex matched individuals | 356 | psychosocial adversity | Self-reported | LV structure and function | Objective | Continuous outcome | Exposure to famine not associated with LV mass | |||
| Thurston et al155 | 2014 | Study ofWomen’s Health Across the Nation | 1369 | Psychosocial adversity | Self-reported | cIMT | Objective | Continuous outcome | A history of childhood sexual abuse, but not childhood physical abuse was associated with thicker cIMT Study sample included women only |
X | ||
| Loucks et al156 | 2014 | Coronary Artery Risk Development in Young Adults (CARDIA) Study | 2659 | Psychosocial adversity | Self-reported | cIMT | Objective | Continuous outcome | Adverse childhood family psychosocial environment associated with thicker cIMT in White men and women, but not in Black men or White | X | X | |
| Cruickshank et al157 | 2016 | The Determinants of Adolescent, Now Young Adult, Social Wellbeing, and Health Longitudinal Study | 666 | Psychosocial adversity | Self-reported | Arterial stiffness | Objective | Continuous outcome | Greater perceived racism associated with greater arterial stiffness | |||
| Juonala et al158 | 2016 | Cardiovascular Risk in Young Finns Study | 311 | Psychosocial adversity | Self-reported | Coronary artery calcification | Objective | Categorical outcome | Favorable childhood psychosocial environment associated with lower likelihood of the presence of coronary artery calcification | |||
| Head et al159 | 2008 | individuals born in Guernsey Island 1923–1937, later occupied by Germans during WWII | 873 | Psychosocial adversity | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Exposure to war-related occupation associated with higher risk of CVD | |||
| Korkeila et al160 | 2010 | Health and Social Support Study | 23 916 | Psychosocial adversity | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Greater number of adversities associated with greater risk of CVD, among women only | X | ||
| Halonen et al161 | 2015 | Finnish Public Sector Study | 37 699 | Psychosocial adversity | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Higher childhood adversity only associated with greater CVD risk if adult neighborhood disadvantage was also low | |||
| Morton et al162 | 2014 | National Survey of Midlife Development in the United States | 3032 | Psychosocial adversity | Self-reported | Clinical CVD: CHD | Self-reported | Categorical outcome | Higher levels of childhood misfortune associated with greater risk of CHD | |||
| Woo et al163 | 2010 | elderly individuals in Hong Kong attending health check | 3732 | Psychosocial adversity | Self-reported | Clinical CVD: CHD | Self-reported | Categorical outcome | Exposure to famine associated with greater risk of CHD | |||
| Dong et al164 | 2004 | Kaiser Permanente’s Health Appraisal Center | 17 337 | Psychosocial adversity | Self-reported | Clinical CVD: CHD | Self-reported | Categorical outcome | Number of childhood adverse childhood experiences associated with greater risk of CHD | |||
| Hollingshaus et al165 | 2015 | Utah Population Database | 663 729 | Psychosocial adversity | Self-reported | Clinical CVD: mixed definition | Objective | Time to event | Early-life parental death was associated with a higher risk of CVD mortality No sex differences | X | ||
| Robertson et al166 | 2017 | Swedish military conscription between 1968–2005 | 1 784 450 | Psychosocial adversity | Self-reported | Clinical CVD: heart failure | Objective | Time to event | Low stress resilience associated with higher risk of heart failure Study sample included men only |
X | ||
| Garad et al167 | 2017 | National Population Health Survey | 4048 | Psychosocial adversity | Self-reported | clinical CVD: mixed definition | Self-reported | Categorical outcome | Greater number of adversities associated with greater risk of CVD, among women only | X | ||
| Bergh et al168 | 2014 | Swedish military conscription | 237 879 | Psychosocial adversity | Self-reported | Clinical CVD: stroke | Objective | Time to event | Lower stress resiliency group associated with greater risk of stroke Study sample included men only |
X | ||
| Shi et al169 | 2018 | China Health and Retirement Longitudinal Study | 5772 | Psychosocial adversity | Self-reported | Clinical CVD: mixed definition | Self-reported | Categorical outcome | Exposure to famine in childhood associated with lower risk of CVD | |||
| Magnussen et al170 | 2012 | Combined cohort of Bogalusa Heart Study and Cardiovascular Risk in Young Finns Study | 1757 | MetS | Objective | cIMT | Objective | Event rate | Persistent MetS associated with greater risk of high cIMT | |||
| Koskinen et al171 | 2017 | Combined cohort of Bogalusa Heart Study, Cardiovascular Risk in Young Finns Study, Minnesota Insulin Study, and Princeton Lipid Research Clinics Follow-Up Study | 5803 | MetS | Objective | cIMT | Objective | Categorical outcome | MetS associated with greater risk of high cIMT, among exposure age groups 1118 years only No sex differences | X | X | |
| Magnussen et al172 | 2016 | Cardiovascular Risk in Young Finns Study | 1453 | MetS | Objective | cIMT | Objective | Categorical outcome | MetS associated with greater risk of high cIMT | |||
| Magnussen et al173 | 2010 | Combined cohort of Bogalusa Heart Study and Cardiovascular Risk in Young Finns Study | 1781 | MetS | Objective | cIMT | Objective | Event rate | MetS associated with greater risk of high cIMT, but BMI only has the same predictive capacity | |||
| Koivistoinen et al174 | 2011 | Cardiovascular Risk in Young Finns Study | 945 | MetS | Objective | Arterial stiffness | Objective | Continuous outcome | MetS associated with greater arterial stiffness | |||
| DeBoer et al175 | 2016 | Princeton Lipid Research Clinics Follow-Up Study | 711 | MetS | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | MetS associated with greater risk of CVD | |||
| Morrison et al176 | 2007 | Princeton Lipid Research Clinics Follow-Up Study | 771 | MetS | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | MetS associated with greater risk of CVD | |||
| DeBoer et al177 | 2015 | Princeton Lipid Research Clinics Follow-Up Study | 341 | MetS | Objective | Clinical CVD: mixed definition | Self-reported | Categorical outcome | MetS associated with greater risk of CVD | |||
| Laitinen et al178 | 2012 | Cardiovascular Risk in Young Finns Study | 856 | Number of risk factors | Objective | cIMT | Objective | Categorical outcome | Greater number risk factors associated with greater risk for high cIMT | |||
| Laitinen et al179 | 2015 | Cardiovascular Risk in Young Finns Study | 370 | Number of risk factors | Objective | Coronary artery calcification | Objective | Event rate | Lower number of risk factors associated with decreased risk of presence of coronary artery calcification No sex differences | X | ||
DBP, diastolic BP; SBP, systolic BP; PWV, pulse wave velocity.
Figure 2.
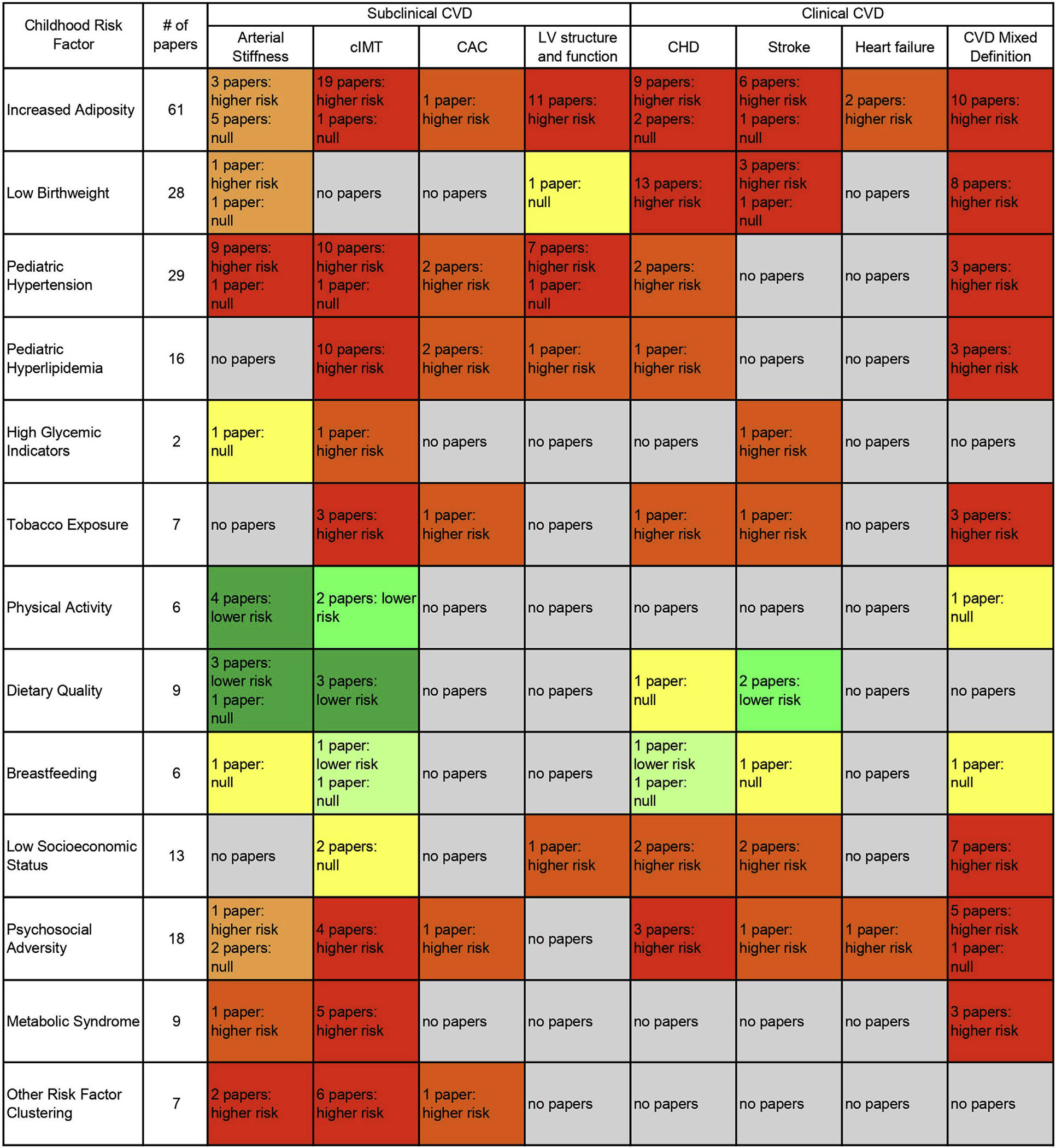
Heat map of identified articles examining childhood exposures and adulthood CVD. Each box lists the number of articles corresponding the exposure and CVD outcome pair. Yellow indicates that only null associations have been observed between the exposure and outcome. Colors deepen from light orange to red with an increasing number of articles indicating the exposure may be associated with higher CVD outcome risk. Colors deepen from light green to dark green with an increasing number of articles indicating the exposure may be associated with lower CVD outcome risk. Gray indicates that no articles examining the exposure and outcome pair were identified in this review. Articles that included multiple subtypes of CVD (eg, CHD and stroke) in the outcome without estimating the association for each subtype of CVD separately were classified as “CVD Mixed Definition”.
Adiposity
We identified 61 studies that examined the association between childhood adiposity and adulthood subclinical and clinical CVD. Almost all studies used body mass index (BMI) as the adiposity measure, but there was heterogeneity in whether BMI was analyzed continuously, categorically using percentile cut-points, or categorically using numeric cut-points.6
Subclinical CVD Outcomes.
Four articles found no significant association between childhood adiposity and adulthood arterial stiffness,7–10 but 2 other studies found associations between adiposity and increased arterial stiffness.11,12 One study found an association between adiposity at age 4 years and adulthood stiffness; however, this association was not found when examining adiposity at age 2 years.13
In 19 articles, childhood adiposity was associated with greater adult carotid intima-media thickness (cIMT).7–10,14–28 Sex differences in the association were examined in 11 of these articles, 7 articles found no difference between men and women, 3 articles found the association held among women only, and 1 article found the association held among men only.7–10,16,18,21,22,26–28 When examining the association by exposure age, there was a stronger association in adolescence (age ≥12 years) compared with earlier childhood.16,24 One article had a null finding, where overweight in early childhood (ages 2–11 years) was not associated with cIMT in older adulthood.29
The association between greater childhood adiposity and adverse adulthood left ventricular (LV) structure and function was significant across 11 articles.15,30–39 One study examined the association of BMI in adolescence and presence of adult coronary artery calcification, finding a positive association.40
Clinical CVD Outcomes.
Eleven articles examined associations between childhood adiposity and adult CHD finding higher risk of CHD with each SD increase in BMI (hazard ratio range per SD, 1.05–1.22).41–51 One article examined the associations by age group and found more robust associations at age 13 years as compared with age 7 years between childhood adiposity and a higher risk of adult CHD.46 Seven articles examined the associations between childhood adiposity and adulthood stroke; the hazard ratio range of higher risk of stroke with each SD increase in BMI was 1.15–1.29. Two articles found significant associations of increased adiposity with risk of adulthood heart failure.42,44,50,52–57 Last, there were 10 articles that used mixed-type definitions of CVD (eg, includes both CHD and stroke combined as a single outcome); the hazard ratio range of higher risk of CVD with each SD increase in BMI was 1.09–1.21 and the hazard ratio range of higher risk of CVD with childhood obesity was 2.3–3.9.58–67 One article stratified by childhood age group, finding stronger associations with CVD among children aged 8–14 years as compared with 2–8 years.62
Birthweight
Low birthweight is also a contributor to the pathogenesis of CVD. We found 28 articles examining associations of birthweight with adulthood subclinical and clinical CVD, all adjusted for gestational age. Three articles specifically examined subclinical CVD: 1 article found low birthweight (<2500 g) to be associated with greater arterial stiffness, and the other 2 found no association between low birthweight and either arterial stiffness or LV mass.13,32,68 The associations between lower birthweight and higher risk of clinical CVD were consistent across 25 studies and multiple CVD outcomes, including CHD, stroke, and CVD mortality; the hazard ratio range of higher risk of CVD with each SD decrease in birthweight was 1.11–1.43 and the hazard ratio range of higher risk of CVD with low birthweight was 2.2–3.6.43,45,49,69–90
Change in Adiposity Across Childhood
We identified 19 articles examining how change in adiposity across childhood may affect risk of adulthood CVD. Four studies examined the velocity of weight gain during early childhood, finding that lower levels of weight gain through age 2 years were associated with higher risk of CVD.79,83,91,92 However, after infancy, faster childhood weight gain was associated with a greater risk of CVD.45,52,53,63,79,93 Further, individuals who had low birthweight and then gained weight rapidly in childhood were at the greatest risk for adult CVD.45,79,93,94
Blood Pressure
We identified 29 articles examining childhood blood pressure (BP) and adult CVD outcomes, and these articles used a mix of continuous BP measurement and dichotomous elevated/not elevated BP classification. To determine elevated BP, studies applied the pediatric hypertension guidelines in effect at the time of analysis; thus, there is heterogeneity across publication date in how elevated BP is defined.
Subclinical CVD Outcomes.
Ten articles examined childhood BP and the association with adulthood arterial stiffness. Nine of these studies found that elevated BP was associated with greater arterial stiffness.7,8,11,12,95–100
The association between childhood BP and adult cIMT was measured in 11 articles. In 9 articles, there was an association between elevated BP and thicker cIMT.7,8,16,19–21,96,97,101–103 Five of these studies stratified the results by sex, but only 1 study found sex-specific differences with the association, present only among women.7 One study stratified by exposure age, and the association between BP and cIMT was only significant among adolescents aged 12–18 years.16 The association between childhood BP and adult coronary artery calcification was examined in 2 articles; both showed an association between elevated BP and the presence of coronary artery calcification.40,104
Eight articles examined associations between childhood BP and adulthood LV structure and function. Three articles found positive associations between BP and LV mass,35,102,105 but a fourth article found no association.30 The remaining 4 articles examined adulthood LV hypertrophy as the outcome; pediatric hypertension was associated with a higher risk of LV hypertrophy.36,39,96,97
Clinical CVD Outcomes.
Five articles examined childhood BP and adulthood CVD events.41,106–109 Elevated BP was associated with greater risk of CVD; the hazard ratio range of higher risk of CVD with each SD increase in BP was 1.05–1.18 and in the 1 study that examined higher risk of CVD with a dichotomous hypertension cut-off, the hazard ratio was 1.51. One study stratified risk of CVD by childhood BMI, finding significant associations between hypertension and CVD across BMI strata that were strongest among obese children.106
Lipids
We identified 16 articles using a heterogeneous mix of total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and/or triglycerides as the exposure of interest, with several articles comparing the performance of these lipid measures.
Subclinical CVD Outcomes.
Ten articles established consistent findings between pediatric hyperlipidemia and adult cIMT, but there were differences by type of lipids. LDL-C was measured in 8 articles, and higher LDL-C was consistently associated with thicker cIMT.16,19,20,27,110-113 There was consistently no association between triglyceride levels and cIMT across 7 studies.16,19–22,111,113 The findings on HDL-C were mixed: 3 studies found lower HDL-C associated with thicker cIMT, whereas 4 studies did not find any significant associations.16,19,20,22,111–113 One article examined total cholesterol, finding a positive association with thicker cIMT.21 In 2 articles that examined pediatric lipid levels and coronary artery calcification, the presence of coronary artery calcification was association with higher LDL-C in 1 article and lower HDL-C in the other article.40,104 One article examined childhood triglyceride levels and LV mass; the association between higher triglycerides and greater LV mass was significant.105
Two studies of childhood lipid levels and adult cIMT stratified their findings by age group, and in both, the associations held for adolescents but were not significant in early childhood.16,21 In another study, stratified by race and sex, the significant association between higher childhood LDL-C cholesterol and thicker adult cIMT was present for White men, White women, and Black women, but not for Black men.111 Several studies tested for sex differences in the association between pediatric lipid levels and adult cIMT, but none were found.16,21,22,27
Clinical CVD Outcomes.
Three articles examined childhood triglyceride levels and adulthood CVD, all showing significant associations between higher triglyceride levels and a higher incidence of CVD (hazard ratio range, 5.4–6.1).66,114,115 We found no articles examining other childhood lipid measures and adult CVD outcomes in the general population.
Glycemic Indicators
We found scant research connecting childhood glycemic indicators to adulthood CVD. One study examined fasting glucose and found associations with greater cIMT, but did not find any associations between fasting glucose and adult arterial stiffness.116 In another study, type 2 diabetes in adolescence was associated with a higher risk of stroke.55
Tobacco Exposure
Assessment of tobacco exposure includes both self-smoking in adolescence, that is, personal use of tobacco cigarettes, and secondary exposure to smoking in home- and community-based environments throughout childhood and adolescence.3 We identified 4 articles examining childhood self-smoking. Cigarette smoking was associated with thicker adulthood cIMT as well as CVD incidence.16,117,118 Another study, conducted only among current and former smokers, found a higher risk of developing CVD among those who initiated smoking before age 17 years as compared with those who started at age 17 years or after.119 Additionally, 3 articles examined exposure to parental smoking, finding significant associations with thicker adulthood cIMT and carotid atherosclerotic plaque.120–122 There was evidence of a dose response; the risk of thicker cIMT was higher if both parents reported smoking, and the risk of carotid plaque was lower if there was evidence of good “smoking hygiene” as demonstrated by reported parental smoking without concomitant detectable levels of serum cotinine in the child.120,122
Physical Activity
We identified 6 articles addressing childhood physical activity and risk of adulthood subclinical and clinical CVD. All but one of the studies relied on self-reported physical activity, and all studies used a continuous measure of physical activity.
Associations between childhood physical activity and adult arterial stiffness were mixed. In 1 study, greater childhood physical activity was associated with lower adulthood stiffness among men only,123 in 2 studies only vigorous physical activity was associated with lower stiffness (among both men and women), and in a fourth study both moderate and vigorous physical activity were associated with lower stiffness.124–126 In 2 studies, both moderate and vigorous physical activity during childhood were associated with lower adult cIMT.22,126 Finally, 1 study on adulthood atrial fibrillation among men did not find an association between physical activity at age 15 years and later incidence of atrial fibrillation.127
Diet
Nine articles evaluated various aspects of diet quality; 3 articles focused on overall diet quality and 6 articles focused on specific food groups, such as fruits and vegetables.
Subclinical CVD Outcomes.
Four studies focused on childhood diet and its potential impact on adult arterial stiffness. In 1 study, greater intake of fruits and vegetables was associated with less arterial stiffness, and in another study, greater intake of dietary fiber was associated with less arterial stiffness.128,129 Two studies examined the Mediterranean diet score finding an association with greater adherence to the Mediterranean diet and less arterial stiffness in 1 study and no association with arterial stiffness in the other study, respectively.130,131
Another 3 studies examined the association between childhood diet and adulthood cIMT as the outcome of interest. Greater fruit consumption was associated with thinner cIMT, as was consumption of omega-3 fatty acids.22,132 In contrast, greater consumption of saturated, monounsaturated, and polyunsaturated fat was associated with thicker adulthood cIMT.132 The third study found that adherence to a traditional Finnish diet was associated with a thicker cIMT among men only, most likely attributable to high consumption of fat and sodium.133
Clinical CVD Outcomes.
Two studies examined the association between childhood diet and adulthood CVD events. One study found an association between dairy/calcium consumption and lower risk of stroke, but found no association with CHD.134 The other study found that greater vegetable consumption was associated with lower risk of stroke, but greater fish consumption was associated with higher risk of stroke; importantly, this finding may be confounded by the dietary patterns of children during the Great Depression.135
Breastfeeding
Six articles examined associations between breastfeeding in infancy and adulthood CVD outcomes. Two studies examined breastfed infants and adult cIMT in those offspring; in 1 study, there was no association in younger adults (mean age of 31 years) and the other study found that breastfeeding in infancy was associated with thinner cIMT in older adults (mean age of 71 years).136,137 One article examining exposure to breastfeeding and adult arterial stiffness and 1 article examining breastfeeding and endothelial function showed no association.13,136 In 3 articles examining breastfeeding and adult CVD events, 1 study found no association with either CHD or stroke, 1 study found no association with CVD mortality, and the third study found a protective association between breastfeeding and CHD.138–140
Psychosocial Risk Factors
Socioeconomic Status.
We identified 13 articles examining childhood socioeconomic status (SES) with adult subclinical and clinical CVD. Most articles used the father’s occupation category as the socioeconomic measure, but childhood household income or parental educational attainment were also used to classify exposure. Two studies that examined SES and adult cIMT showed no association, as did the 1 study that examined SES and endothelial function.141,142 The 1 study examining SES and adult LV structure and function found an association between lower childhood SES and larger adulthood LV mass.143 In the 9 studies examining SES and clinical CVD outcomes, lower childhood SES was associated with higher incidence of clinical CVD (relative risk range, 1.3–1.8), including CHD, stroke, and CVD mortality.81,144–152 These associations were robust to multivariable adjustment of childhood and adulthood CVD risk factors, such as adiposity, hyperlipidemia, hypertension, smoking, and family history of CVD.
Psychosocial Adversity.
There were 18 articles examining childhood psychosocial adversity and adulthood CVD outcomes. There was little standardization across articles in the definition of adverse experiences; some studies measured a single adversity, such as exposure to famine or early life parental death, and other studies used scales with multiple adversities, such as an adverse childhood experiences scale or a life events scale. Almost all exposures were assessed retrospectively in adulthood.
Subclinical CVD Outcomes.
Associations between childhood psychosocial adversity and adulthood subclinical CVD were inconsistent or showed no association. There were 4 studies examining psychosocial adversity and cIMT; 2 studies found no association with cIMT, a third study found an association with cIMT for childhood sexual abuse only, and a fourth study found an association with cIMT among White individuals but not Black individuals.153–156 Three studies examined childhood psychosocial adversity and adulthood arterial stiffness; 2 studies found no association with arterial stiffness, but the third study found increased childhood exposure to racism was associated with greater arterial stiffness.153,154,157 There was no association observed in the 1 study that assessed the impact of childhood psychosocial adversity and adult LV mass.154 In the 1 study that examined coronary artery calcification, there was a significant association between greater childhood psychosocial adversity and adulthood presence of coronary artery calcification.158
Clinical CVD Outcomes.
There were 11 studies examining childhood psychosocial adversity and adulthood clinical CVD, finding significant positive associations with CHD, stroke, heart failure, and CVD mortality.159–169 The magnitude of the association varied by type of adversity exposure. The hazard ratio range of higher incidence of CVD associated with greater psychosocial adversity was 1.3–3.6, and each additional adversity conferred a 30%–70% higher risk of CVD.164 These associations were robust to adjustment for CVD risk factors as well as childhood SES.
Risk Factor Clustering
Metabolic Syndrome.
The metabolic syndrome (MetS) is defined as having at least 3 of the following risk factors: elevated BMI, elevated triglyceride levels, elevated BP, elevated fasting blood glucose, and lower HDL-C. We found 9 studies examined childhood MetS and adulthood CVD risk. Five studies reported that MetS was associated with greater cIMT.25,170–173 In 1 study, MetS was associated with greater arterial stiffness.174 In 3 studies, MetS was associated with greater CVD incidence.175–177 In the 1 study that examined the associations with adult cIMT by childhood age group, the association was only significant for adolescents aged 11–18 years.171
Other Risk Factor Combinations.
Seven additional studies examined traditional CVD risk factors, including lipids, BMI, BP, diabetes, smoking, diet, and physical activity in different childhood exposure combinations and examined their additive associations with adulthood subclinical CVD; all reported positive associations. Six studies found the number of CVD risk factors was associated with greater cIMT, 2 studies found the number of risk factors was associated with increased arterial stiffness, and 1 study demonstrated associations with presence of coronary artery calcification.12,16,21,22,110,178,179 Two studies that examined associations by age group found that the number of childhood risk factors and adulthood cIMT were only significant for ages 9–18 years.16,21
Other Risk Factors
The 36 remaining articles examined a heterogeneous mix of childhood exposures and the association with adulthood subclinical and clinical CVD. These articles fell into 2 broad categories: maternal and perinatal exposures, an emerging area of interest for cardiometabolic health, and other childhood characteristics and experiences.180–216 A full list of the articles is available in Table IV (available at www.jpeds.com).
Table IV.
Additional articles identified, not described in main text
| References | Year | Study population | Exposure | Outcome | Main findings |
|---|---|---|---|---|---|
|
| |||||
| Tatsukawa et al180 | 2008 | 1559 Japanese men and women atomic bomb survivors | Amount of radiation exposure in utero | CVD: mixed definition | Greater dose of radiation associated with greater risk of CVD |
| Roseboom et al181 | 2000 | 736 men and women born during Dutch famine in 1943–1947 | Exposure to famine in utero | CVD: CHD | Exposure to famine in early gestation associated with higher risk of CHD |
| Ekamper et al182 | 2015 | 41 096 male military conscripts born in the Netherlands between 1944 and 1947 | Exposure to famine in utero | CVD: mixed definition | No increase in CVD mortality associated with prenatal famine exposure |
| Painter et al183 | 2007 | Dutch Famine Birth Cohort, 2414 men and women born in Amsterdam in 1943–1947 | Exposure to famine in utero | Arterial stiffness | Exposure to famine in utero was not associated with arterial stiffness in adulthood |
| van Abeelen et al184 | 2012 | Dutch Famine Birth Cohort, 2414 men and women born in Amsterdam in 1943–1947 | Exposure to famine in utero | CVD: mixed definition | Women exposed to famine in early gestation had a high risk of CVD mortality, no association among men |
| Rerkasem et al185 | 2012 | 565 twenty-year-olds whose mothers, while pregnant, participated in a nutritional study during 1989–1990 in Chiang Mai, Thailand | Maternal protein intake during pregnancy | cIMT | Lower maternal protein intake during pregnancy was associated with thicker cIMT in adulthood |
| Eriksson et al183 | 2014 | Helsinki Birth Cohort, 13 345 men and women born in Helsinki, Finland during 1934–1944 | Maternal BMI during pregnancy | CVD: mixed definition | Higher maternal BMI associated with increased risk of CVD in adulthood |
| Kajantie et al187 | 2009 | Helsinki Birth Cohort, 6410 men and women born in Helsinki, Finland during 1934–1944 | Exposure to preeclampsia or gestational hypertension in utero | CVD: stroke only | Exposure to preeclampsia or gestational hypertension in utero associated with increased risk of stroke in adulthood |
| Bjarnegard et al188 | 2013 | 37 young adults born at term with IUGR and controls in Malmo, Sweden | IUGR | LV structure and function | IUGR associated with small LV diameter |
| Skilton et al189 | 2011 | Cardiovascular Risk in Young Finns Study | Impaired fetal growth | cIMT and endothelial function | Impaired fetal growth was associated with impaired endothelial function and thicker cIMT in adulthood |
| Fan et al190 | 2010 | 2033 men and women born in Beijing, China between 1921 and 1954 | Fetal growth retardation | CVD: CHD only | Fetal growth retardation associated with increased risk of CHD in adulthood |
| Ueda et al191 | 2014 | 1 306 943 infants born in Sweden between 1983 and 1995 | Preterm birth | CVD: mixed definition | No association between preterm birth and CVD, except among for those born very preterm - higher incidence of stroke |
| Kajantie et al192 | 2015 | Helsinki Birth Cohort, 19 015 men and women born in Helsinki, Finland during 1934–1944 | Preterm birth | CVD: CHD and stroke | No increased risk of CHD or stroke in people born preterm, except for women born early preterm (<34 weeks) |
| Lewandowski et al193 | 2013 | 234 men and women 20 to 39 years of age who underwent cardiovascular magnetic resonance in Oxford, UK | Preterm birth | LV structure and function | Preterm birth associated with increased LV mass in adulthood |
| Risnes et al194 | 2009 | 31 307 Norwegian men and women born between 1934 and 1959 | Placenta-to-birth-weight ratio | CVD: mixed definition | Higher placenta-to-birth-weight ratio associated with increased risk of CVD mortality |
| Barker et al196 | 2010 | Helsinki Birth Cohort, 13 345 men and women born in Helsinki, Finland during 1934–1944 | Placental surface area | CVD: heart failure | Small placental surface area (<225 cm2) was associated with increased risk of heart failure in adulthood |
| Risnes et al195 | 2009 | 46 311 births in Trondheim, Norway, from 1920 to 1959 | Head circumference at birth | CVD: CHD/MI | Small head size at birth associated with increased risk of CHD death |
| Gunnell et al198 | 1998 | Boyd-Orr Cohort, 2547 children living in England and Scotland in 1937–1939 | Age and sex specific z scores for height, leg length, and trunk length | CHD | Shorter leg length associated with higher risk of CHD in both men and women, only for 8 and under |
| Silventoinen et al199 | 2012 | 232 063 children born in 19301976 who attended school in Copenhagen, Denmark | Growth in height from 7 to 13 years of age | CVD: CHD/MI | Height was inversely related to risk of CHD, but rapid growth in height was also associated with increased CHD risk |
| Whitley et al200 | 2012 | Boyd-Orr Cohort, 1043 children living in England and Scotland in 1937–1939 | Childhood stature: height, shoulder breadth, leg, trunk and foot length | CVD: mixed definition | Childhood stature associated with CVD morbidity and mortality in adulthood |
| Batty et al201 | 2007 | Hertfordshire Cohort, 4351 children in UK | Diarrhea in early childhood (age 05 years) | CHD | No evidence that diarrhea in early life associated with increased risk of CHD in older adults |
| Mueller et al202 | 2012 | Singapore Chinese Health Study, 34 022 women | Age at menarche | CVD: mixed definition | Higher age at menarche associated with lower risk of CHD among nonsmokers, but no association for smokers or stroke |
| Canoy et al203 | 2015 | Million Women Study, 1 217 840 women based in UK | Age at menarche | CVD: mixed definition | U-shaped association, early and late ages at menarche associated with increased CVD risk |
| Wang et al204 | 2016 | CHARLS: 2013 China Health and Retirement Longitudinal Study -nationally representative of Chinese residents aged ≥45, 10 000 men and women | Self-reported health in childhood (retrospective assessment) | CHD | Poor childhood health associated with higher risk of CHD |
| Juonala et al205 | 2006 | Cardiovascular Risk in Young Finns Study, 1617 children | C-reactive protein levels | cIMT | Childhood C-reactive protein did not predict adult cIMT |
| Du et al206 | 2018 | Bogalusa Heart Study, 1052 men and women | Serum adiponectin levels and BMI | cIMT | Association between higher BMI and thicker cIMT only present in those with childhood adiponectin levels below the median |
| Saarikoski et al207 | 2017 | Cardiovascular Risk in Young Finns Study | Serum adiponectin levels | cIMT | Lower adiponectin levels associated thicker cIMT in adulthood |
| Batty et al208 | 2005 | 6910 men born in 1953 in Copenhagen, Denmark | Childhood intelligence test scores, as measured by the Swedish Harnqvist intelligence test | CVD: mixed definition | Low intelligence associated with increased risk of CHD by not stroke |
| Keltikangas-Jarvinen et al209 | 2006 | Cardiovascular Risk in Young Finns Study, 708 children | Hyperactivity in childhood | cIMT | Hyperactivity predicted cIMT |
| Dedman et al210 | 2001 | Boyd-Orr Cohort, 4301 children living in England and Scotland in 1937–1939 | Housing conditions included crowding, water supply, toilet facilities, adequacy of ventilation, and cleanliness | CHD | Poorer housing conditions in childhood were associated with increased CHD mortality, independent from SES |
| Howard et al211 | 2013 | Reasons for Geographic and Racial Differences in Stroke study, 24 544 stroke-free men and women enrolled 2003–2007 | Residence in stroke belt during childhood | CVD: stroke only | Residence in the stroke belt important during adolescence, effect stronger in Blacks vs Whites |
| Aberg et al212 | 2015 | 1 166 035 Swedish male military conscripts registered in 1968–2005 | Aerobic fitness and muscle strength | CVD: stroke only | Low fitness and low muscle strength associated with increased risk of stroke |
| Ferreira et al213 | 2002 | Amsterdam Growth and Health Longitudinal Study, 154 men and women in the extended cardiorespiratory follow-up | Aerobic fitness | cIMT and arterial stiffness | Increased aerobic fitness associated with thinner cIMT and less arterial stiffness |
| Ferreira et al214 | 2003 | Amsterdam Growth and Health Longitudinal Study, 154 men and women in the extended cardiorespiratory follow-up | Changes in VO2max from adolescence to age 36 | cIMT and arterial stiffness | Increases in VO2max from adolescence to age 36 were associated with less arterial stiffness, but no association with cIMT |
| Lindgren et al215 | 2017 | 1 226 623 Swedish male military conscripts registered in 1969–2005 | Cardiorespiratory fitness | Heart failure | Greater fitness associated with lower risk of hospitalization for heart failure |
| Hogstrom et al216 | 2014 | 743 498 Swedish male military conscripts registered in 1969–1984 | Aerobic fitness | CVD: CHD/MI | Low aerobic fitness associated with increased risk of myocardial infarction |
IUGR, intrauterine growth restriction; MI, myocardial infarction.
Discussion
In this review of 210 articles examining childhood exposures and the development of subclinical and clinical CVD among adults, robust evidence linked increased pediatric adiposity with subclinical and clinical CVD; robust evidence linked pediatric hypertension, hyperlipidemia, and risk factor clustering with subclinical CVD, but limited evidence to date linked these factors with adult clinical CVD. Robust evidence linked low birthweight, worse SES, and psychosocial adversity with clinical CVD, but limited evidence was available for subclinical CVD. Breastfeeding, poor glycemic control, tobacco exposure, less physical activity, and worse diet quality during childhood all had limited numbers of studies across heterogeneous populations, and more research is necessary to determine whether those factors are consistently associated with subclinical and clinical CVD among adults. One promising new study to address some of the existing gaps in the research is the International Childhood Cardiovascular Cohort Consortium Outcomes Study (i3C Outcomes), in which detailed biological, physical, and socioeconomic measures collected in childhood are being harmonized across 7 existing longitudinal cohorts, and connected with self-reported incident CVD endpoints, medical records to adjudicate these endpoints, and national death records to explore CVD-related mortality.217 We found no consistent evidence for major sex differences in risk of subclinical or clinical CVD for childhood risk factors. Most studies that examined sex differences found similar associations for men and women with null interaction terms. In contrast, few studies examined potential differences by race and/or ethnicity; most cohorts had samples that were homogenous in race/ethnicity, and therefore did not permit analyses of this nature. Furthermore, the majority of cohorts were based in the US or Europe, with majority White populations. Few studies in this review were from cohorts based in Africa, Latin America, or Asia. New recruitment of diverse cohorts is needed to adequately understand any complex racial/ethnic differences in the associations between childhood risk factors and adulthood CVD, and special consideration should be given to global cohorts that have been underrepresented in previous research.
The majority of systematic reviews and meta-analyses linking childhood exposures and adult outcomes have focused on the development of risk factors in adulthood, such as hypertension or dyslipidemia. However, several have examined subsets of this comprehensive review. A systematic review published in 2014 relating either early life BP, BMI, and/or glycemic control to future cardiac structure and/or function found all 3 risk factors to be associated with worse future diastolic function.218 The age of exposure criteria differed, in that articles with young adults over age 20 years were included, but nevertheless, conclusions were similar to those we observed for childhood BMI and BP and LV structure and function. In another systematic review of childhood socioeconomic circumstances and CVD risk in adulthood published in 2006, the authors concluded that childhood SES was a robust predictor of adulthood CVD risk, as we have concluded in this review.219
There are multiple life course models (Figure 3) that may reflect contributory pathways from childhood exposure to adulthood CVD. Articles that have more robust associations with CVD as the exposure is measured in adolescence as compared with early childhood or in adulthood as compared with childhood may support a chain-of-risk life course model. This finding demonstrates that childhood risk factors may increase the likelihood of having adulthood risk factors, but the adulthood risk factor status primarily affects the outcome, which represents an encouraging pediatric model because childhood risk status may be modifiable, with favorable long-term consequences.5
Figure 3.
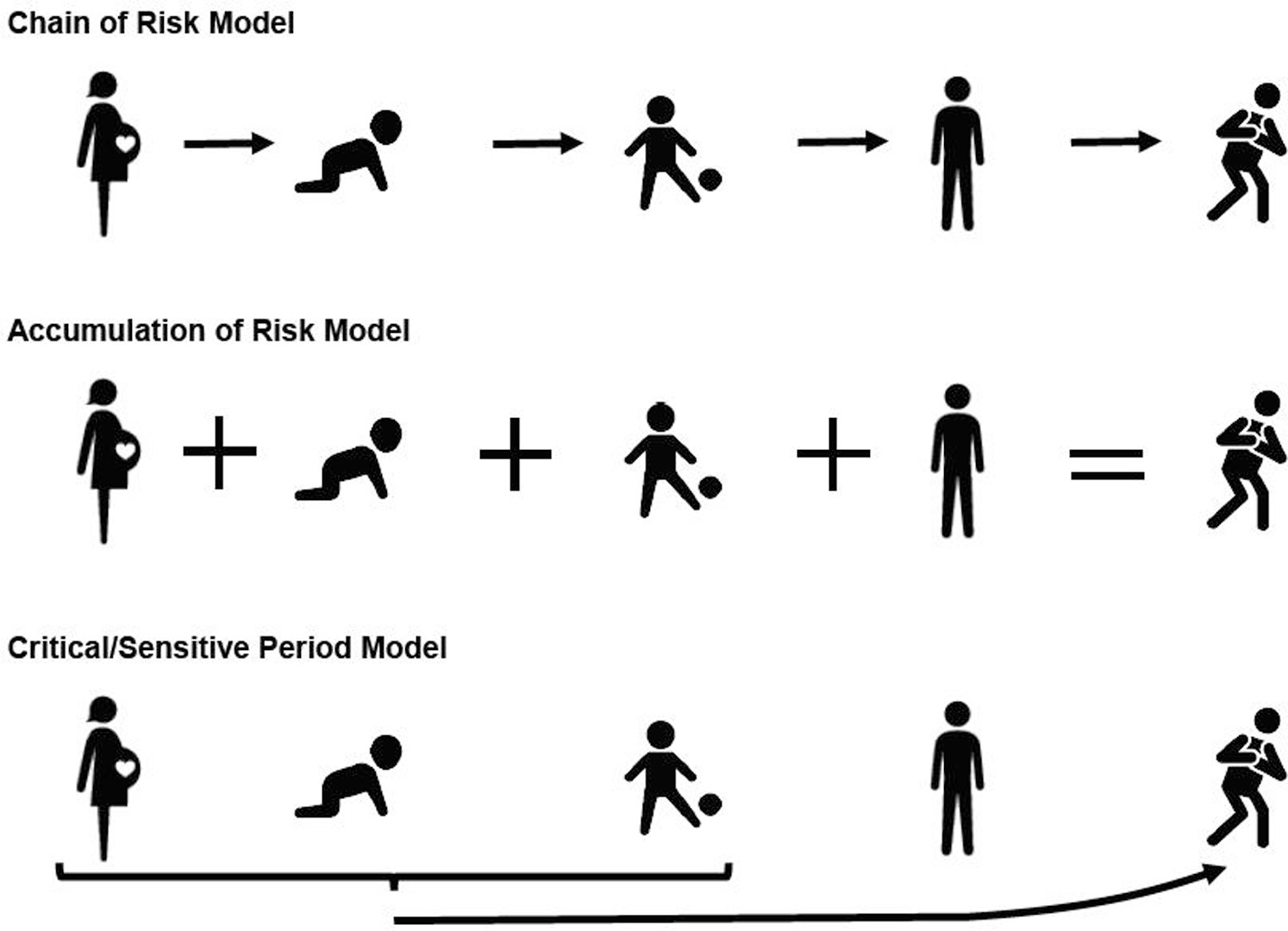
Life course models for CVD development. The 3 hypothesized life course models for the development of CVD: chain of risk, where childhood risk is entirely mediated through adulthood risk; accumulation of risk, where risk factors present at each life stage further increase adulthood risk; and the critical/sensitive period, where exposure at a certain point in the life course confers more risk as compared with other life course stages.
Articles that find the highest risk of adulthood CVD among those with persistent exposures in childhood and adulthood may represent an accumulation-of-risk model, whereby exposures at each point in the life course further increase likelihood of CVD development. Furthermore, in a sensitive period model, exposure at a certain point in the life course confers increased risk that is less harmful at a different time point. Both the accumulation-of-risk and sensitive periods models highlight the necessity of prevention in early childhood and the prenatal period, to decrease the likelihood of having the exposure and thus developing CVD in adulthood. Several complexities of longitudinal research emerged in this literature review.4 A prospective cohort with decades of follow-up requires a substantial investment of resources; consequently, a limited number of unique cohorts exist. There were multiple articles using the same cohort data, perhaps oversaturating findings that are specific to the sample population. Childhood exposures were frequently assessed retrospectively, leading to broad measures that are subject to recall bias. Other cohorts used medical and other administrative records to collect childhood exposures and/or adult CVD events. The increased use of electronic medical records may be a novel method to facilitate research on childhood exposures, but some risk factors are not routinely collected in clinical encounters, such as lifestyle behaviors.
Although many of the cohorts followed participants for decades, often the adulthood exposure assessments were conducted around ages 30–40 years. Although population-level subclinical atherosclerotic differences may be present by those ages, CVD events are rare. The studies that did use a prospective cohort design were, therefore, mostly examining “premature” CVD. It is likely that findings would shift with additional years of data collection and thus continued resources to encourage follow-up of these cohorts is necessary to capture the natural history of CVD. Further, few articles directly accounted for differential loss to follow-up in which healthier individuals are more likely to continue participating in the study and less likely to have a severe competing risk (such as non-CVD-related death), resulting in survivor bias toward the null.
Incomplete adjustment for confounding was major source of threat to internal validity. Retrospective studies often had only a few questions about childhood, limiting the adjustment for contextual factors that could influence the outcome and the exposure. For example, studies on birthweight and adulthood CVD often lacked data on maternal health, which could include family history of CVD risk. Prospective studies tended to have a greater range of childhood risk factors measured, but often lacked behavioral and lifestyle factors that could inform clinical risk factors in childhood, continuing into adulthood. External validity to contemporary prevention settings was limited by exposures that have had significant secular change over the course of follow-up. For example, dietary patterns and tobacco exposure—particularly secondhand tobacco exposure in children—have shifted over time. Findings must, therefore, be placed into context before applying them to preventive strategies.
Last, there are limitations in how the literature review was conducted and the results reported. This review was intended to broadly cover childhood exposure to known CVD risk factors and the relationship to adulthood subclinical and clinical CVD. We created search terms based on the extant knowledge of major CVD risk factors, and studies focused on emerging areas of research, such as the prenatal environment or neurodevelopment health, may not be not be fully captured in our systematic search. Further, with the known publication bias in the biomedical literature whereby articles with statistically significant findings are more likely to be submitted and accepted, analyses with null findings are likely underrepresented within our study and may bias our results toward significant findings. Given the breadth of the topic, we were unable to give detailed assessment of the quality of each of the included studies, and there may be differences in methodology, for example, sample size, sampling frame, adjustment for potential confounders, potential for measurement error, that impact the relative strength of the evidence. If the findings of a study were counter to the other included studies for a similar exposure and outcome, we did attempt to provide additional details to understand the divergent findings. Finally, the heterogeneous nature of the exposure measurements, outcome ascertainment, duration of follow-up, and background environment of the studies, as well as the potential for oversaturation from specific study cohorts precluded reliable quantification of associations through meta-analysis.
In conclusion, an examination of childhood risk factors and their associations with adulthood subclinical and clinical CVD reveals a large and varied body of evidence in which some areas of consistency can be discerned. As robust evidence emerges demonstrating that risk of CVD-related morbidity and mortality have origins in childhood, pediatric clinicians can continue to be encouraged to address major risk factors in their practice, understanding that they may alter life-long health trajectories and improve outcomes across decades for their patients. Likewise, the public health implications of intervening on childhood risks factors such as obesity or pediatric hypertension can amount huge improvements in the population-level incidence of CVD, as well as improvements in the long-term sequalae of chronic disease: years of potential life lost, disability adjusted life years, and overall spending on healthcare.
Nevertheless, major gaps remain in the research and in understanding how childhood health behaviors translate to risk of CVD later in life. This review is intended to update the current data to guide future research not only towards to addressing gaps, but also toward developing novel risk factor trajectories, cardiovascular health growth curves, and a priori exploration of maternal and intergenerational risk transmission. It may also point the way to future interventional studies designed to decrease the long-term incidence of subclinical and clinical CVD.
Acknowledgments
Supported by the American Heart Association (17SFRN33700101 [to N.B.]). The funder/sponsor did not participate in the work. The authors declare no conflicts of interest.
Glossary
- BP
Blood pressure
- BMI
Body mass index
- CVD
Cardiovascular disease
- cIMT
Carotid intima-media thickness
- CHD
Coronary heart disease
- HDL-C
High-density lipoprotein cholesterol
- LDL-C
Low-density lipoprotein cholesterol
- LV
Left ventricular
- MetS
Metabolic syndrome
- SES
Socioeconomic status
Data Statement
Data sharing statement available at www.jpeds.com.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 2019;139:e56–528. [DOI] [PubMed] [Google Scholar]
- 2.McGill HC Jr, McMahan CA, Herderick EE, Malcom GT, Tracy RE, Strong JP. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr 2000;72:1307s–15s. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011;128:S213–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hardy R, Lawlor DA, Kuh D. A life course approach to cardiovascular aging. Future Cardiol 2015;11:101–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health 2003;57:778–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grossman DC, Bibbins-Domingo K, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 2017;317:2417–26. [DOI] [PubMed] [Google Scholar]
- 7.Ceponiene I, Klumbiene J, Tamuleviciute-Prasciene E, Motiejunaite J, Sakyte E, Ceponis J, et al. Associations between risk factors in childhood (12–13 years) and adulthood (48–49 years) and subclinical atherosclerosis: the Kaunas Cardiovascular Risk Cohort Study. BMC Cardiovasc Disord 2015;15:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan Y, Hou D, Liu J, Zhao X, Cheng H, Xi B, et al. Childhood body mass index and blood pressure in prediction of subclinical vascular damage in adulthood: Beijing blood pressure cohort. J Hypertens 2017;35:47–54. [DOI] [PubMed] [Google Scholar]
- 9.Ferreira I, Twisk JW, van Mechelen W, Kemper HC, Seidell JC, Stehouwer CD. Current and adolescent body fatness and fat distribution: relationships with carotid intima-media thickness and large artery stiffness at the age of 36 years. J Hypertens 2004;22:145–55. [DOI] [PubMed] [Google Scholar]
- 10.Huynh Q, Blizzard L, Sharman J, Magnussen C, Schmidt M, Dwyer T, et al. Relative contributions of adiposity in childhood and adulthood to vascular health of young adults. Atherosclerosis 2013;228:259–64. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira I, van de Laar RJ, Prins MH, Twisk JW, Stehouwer CD. Carotid stiffness in young adults: a life-course analysis of its early determinants: the Amsterdam Growth and Health Longitudinal Study. Hypertension 2012;59:54–61. [DOI] [PubMed] [Google Scholar]
- 12.Juonala M, Jarvisalo MJ, Maki-Torkko N, Kahonen M, Viikari JS, Raitakari OT. Risk factors identified in childhood and decreased carotid artery elasticity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 2005;112:1486–93. [DOI] [PubMed] [Google Scholar]
- 13.Vianna CA, Horta BL, Gigante DP, de Barros FC. Pulse wave velocity at early adulthood: breastfeeding and nutrition during pregnancy and childhood. PLoS One 2016;11:e0152501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Su TC, Liao CC, Chien KL, Hsu SH, Sung FC. An overweight or obese status in childhood predicts subclinical atherosclerosis and prehypertension/hypertension in young adults. J Atheroscler Thromb 2014;21:1170–82. [DOI] [PubMed] [Google Scholar]
- 15.Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Body mass index trajectories in childhood is predictive of cardiovascular risk: results from the 23-year longitudinal Georgia Stress and Heart study. Int J Obes (Lond) 2018;42:923–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raitakari OT, Juonala M, Kahonen M, Taittonen L, Laitinen T, Maki-Torkko N, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 2003;290:2277–83. [DOI] [PubMed] [Google Scholar]
- 17.Oren A, Vos LE, Uiterwaal CS, Gorissen WH, Grobbee DE, Bots ML. Change in body mass index from adolescence to young adulthood and increased carotid intima-media thickness at 28 years of age: the Atherosclerosis Risk in Young Adults study. Int J Obes Relat Metab Disord 2003;27:1383–90. [DOI] [PubMed] [Google Scholar]
- 18.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876–85. [DOI] [PubMed] [Google Scholar]
- 19.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA 2003;290:2271–6. [DOI] [PubMed] [Google Scholar]
- 20.Koskinen J, Juonala M, Dwyer T, Venn A, Thomson R, Bazzano L, et al. Impact of lipid measurements in youth in addition to conventional clinic-based risk factors on predicting preclinical atherosclerosis in adulthood: International Childhood Cardiovascular Cohort Consortium. Circulation 2018;137:1246–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation 2010;122:2514–20. [DOI] [PubMed] [Google Scholar]
- 22.Juonala M, Viikari JS, Kahonen M, Taittonen L, Laitinen T, Hutri-Kahonen N, et al. Life-time risk factors and progression of carotid atherosclerosis in young adults: the Cardiovascular Risk in Young Finns study. Eur Heart J 2010;31:1745–51. [DOI] [PubMed] [Google Scholar]
- 23.Juonala M, Raitakari M, Viikari JSA, Raitakari OT. Obesity in youth is not an independent predictor of carotid IMT in adulthood. The Cardiovascular Risk in Young Finns Study. Atherosclerosis 2006;185:388–93. [DOI] [PubMed] [Google Scholar]
- 24.Freedman DS, Dietz WH, Tang R, Mensah GA, Bond MG, Urbina EM, et al. The relation of obesity throughout life to carotid intima-media thickness in adulthood: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 2004;28:159–66. [DOI] [PubMed] [Google Scholar]
- 25.Koskinen J, Magnussen CG, Sabin MA, Kahonen M, Hutri-Kahonen N, Laitinen T, et al. Youth overweight and metabolic disturbances in predicting carotid intima-media thickness, type 2 diabetes, and metabolic syndrome in adulthood: the Cardiovascular Risk in Young Finns study. Diabetes Care 2014;37:1870–7. [DOI] [PubMed] [Google Scholar]
- 26.Menezes AMB, da Silva CTB, Wehrmeister FC, Oliveira PD,Oliveira IO, Goncalves H, et al. Adiposity during adolescence and carotid intima-media thickness in adulthood: results from the 1993 Pelotas Birth Cohort. Atherosclerosis 2016;255:25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation 2001;104:2815–9. [DOI] [PubMed] [Google Scholar]
- 28.Johnson W, Kuh D, Tikhonoff V, Charakida M, Woodside J, Whincup P, et al. Body mass index and height from infancy to adulthood and carotid intima-media thickness at 60 to 64 years in the 1946 British Birth Cohort Study. Arterioscler Thromb Vasc Biol 2014;34:654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Charakida M, Khan T, Johnson W, Finer N, Woodside J, Whincup PH, et al. Lifelong patterns of BMI and cardiovascular phenotype in individuals aged 60–64 years in the 1946 British birth cohort study: an epidemiological study. Lancet Diabetes Endocrinol 2014;2:648–54. [DOI] [PubMed] [Google Scholar]
- 30.Sabo RT, Yen MS, Daniels S, Sun SS. Associations between childhood body size, composition, blood pressure and adult cardiac structure: the Fels Longitudinal Study. PLoS One 2014;9:e106333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang H, Huynh QL, Venn AJ, Dwyer T, Marwick TH. Associations of childhood and adult obesity with left ventricular structure and function. Int J Obes (Lond) 2017;41:560–8. [DOI] [PubMed] [Google Scholar]
- 32.Hardy R, Ghosh AK, Deanfield J, Kuh D, Hughes AD. Birthweight, childhood growth and left ventricular structure at age 60–64 years in a British birth cohort study. Int J Epidemiol 2016;45:1091–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. Childhood adiposity as a predictor of cardiac mass in adulthood: the Bogalusa Heart Study. Circulation 2004;110:3488–92. [DOI] [PubMed] [Google Scholar]
- 34.Tapp RJ, Venn A, Huynh QL, Raitakari OT, Ukoumunne OC, Dwyer T, et al. Impact of adiposity on cardiac structure in adult life: the Childhood Determinants of Adult Health (CDAH) study. BMC Cardiovasc Disord 2014;14:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lai CC, Sun D, Cen R, Wang J, Li S, Fernandez-Alonso C, et al. Impact of long-term burden of excessive adiposity and elevated blood pressure from childhood on adulthood left ventricular remodeling patterns: the Bogalusa Heart Study. J Am Coll Cardiol 2014;64:1580–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yan Y, Liu J, Wang L, Hou D, Zhao X, Cheng H, et al. Independent influences of excessive body weight and elevated blood pressure from childhood on left ventricular geometric remodeling in adulthood. Int J Cardiol 2017;243:492–6. [DOI] [PubMed] [Google Scholar]
- 37.Zhang H, Zhang T, Li S, Guo Y, Shen W, Fernandez C, et al. Long-term excessive body weight and adult left ventricular hypertrophy are linked through later-life body size and blood pressure: The Bogalusa Heart Study. Circ Res 2017;120:1614–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sivanandam S, Sinaiko AR, Jacobs DR Jr, Steffen L, Moran A, Steinberger J. Relation of increase in adiposity to increase in left ventricular mass from childhood to young adulthood. Am J Cardiol 2006;98:411–5. [DOI] [PubMed] [Google Scholar]
- 39.Toprak A, Wang H, Chen W, Paul T, Srinivasan S, Berenson G. Relation of childhood risk factors to left ventricular hypertrophy (eccentric or concentric) in relatively young adulthood (from the Bogalusa Heart Study). Am J Cardiol 2008;101:1621–5. [DOI] [PubMed] [Google Scholar]
- 40.Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J Am Coll Cardiol 1996;27:277–84. [DOI] [PubMed] [Google Scholar]
- 41.Berenson GS, Srinivasan SR, Xu JH, Chen W. Adiposity and cardiovascular risk factor variables in childhood are associated with premature death from coronary heart disease in adults: the Bogalusa Heart Study. Am J Med Sci 2016;352:448–54. [DOI] [PubMed] [Google Scholar]
- 42.Lawlor DA, Martin RM, Gunnell D, Galobardes B, Ebrahim S, Sandhu J, et al. Association of body mass index measured in childhood, adolescence, and young adulthood with risk of ischemic heart disease and stroke: findings from 3 historical cohort studies. Am J Clin Nutr 2006;83:767–73. [DOI] [PubMed] [Google Scholar]
- 43.Andersen LG, Angquist L, Eriksson JG, Forsen T, Gamborg M, Osmond C, et al. Birth weight, childhood body mass index and risk of coronary heart disease in adults: combined historical cohort studies. PLoS One 2010;5:e14126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Falkstedt D, Hemmingsson T, Rasmussen F, Lundberg I. Body mass index in late adolescence and its association with coronary heart disease and stroke in middle age among Swedish men. Int J Obes (Lond) 2007;31:777–83. [DOI] [PubMed] [Google Scholar]
- 45.Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ 1999;318:427–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357:2329–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crump C, Sundquist J, Winkleby MA, Sundquist K. Interactive effects of obesity and physical fitness on risk of ischemic heart disease. Int J Obes (Lond) 2017;41:255–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Must A, Phillips SM, Naumova EN. Occurrence and timing of childhood overweight and mortality: findings from the third Harvard Growth Study. J Pediatr 2012;160:743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Osler M, Lund R, Kriegbaum M, Andersen AM. The influence of birth weight and body mass in early adulthood on early coronary heart disease risk among Danish men born in 1953. Eur J Epidemiol 2009;24:57–61. [DOI] [PubMed] [Google Scholar]
- 50.Lawlor DA, Leon DA. Association of body mass index and obesity measured in early childhood with risk of coronary heart disease and stroke in middle age: findings from the Aberdeen Children of the 1950s prospective cohort study. Circulation 2005;111:1891–6. [DOI] [PubMed] [Google Scholar]
- 51.Park MH, Sovio U, Viner RM, Hardy RJ, Kinra S. Overweight in childhood, adolescence and adulthood and cardiovascular risk in later life: pooled analysis of three British birth cohorts. PLoS One 2013;8:e70684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gjaerde LK, Gamborg M, Angquist L, Truelsen TC, Sorensen TIA, Baker JL. Association of childhood body mass index and change in body mass index with first adult ischemic stroke. JAMA Neurol 2017;74:1312–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ohlsson C, Bygdell M, Sonden A, Jern C, Rosengren A, Kindblom JM. BMI increase through puberty and adolescence is associated with risk of adult stroke. Neurology 2017;89:363–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crump C, Sundquist J, Winkleby MA, Sundquist K. Interactive effects of physical fitness and body mass index on risk of stroke: a national cohort study. Int J Stroke 2016;11:683–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hogstrom G, Nordstrom A, Eriksson M, Nordstrom P. Risk factors assessed in adolescence and the later risk of stroke in men: a 33-year follow-up study. Cerebrovasc Dis 2015;39:63–71. [DOI] [PubMed] [Google Scholar]
- 56.Crump C, Sundquist J, Winkleby MA, Sundquist K. Aerobic fitness, muscular strength and obesity in relation to risk of heart failure. Heart 2017;103:1780–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rosengren A, Aberg M, Robertson J, Waern M, Schaufelberger M, Kuhn G, et al. Body weight in adolescence and long-term risk of early heart failure in adulthood among men in Sweden. Eur Heart J 2017;38:1926–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Twig G, Ben-Ami Shor D, Furer A, Levine H, Derazne E, Goldberger N, et al. Adolescent body mass index and cardiovascular disease-specific mortality by midlife. J Clin Endocrinol Metab 2017;102:3011–20. [DOI] [PubMed] [Google Scholar]
- 59.Bjorge T, Engeland A, Tverdal A, Smith GD. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents. Am J Epidemiol 2008;168:30–7. [DOI] [PubMed] [Google Scholar]
- 60.Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374:2430–40. [DOI] [PubMed] [Google Scholar]
- 61.Batty GD, Calvin CM, Brett CE, Cukic I, Deary IJ. Childhood body weight in relation to cause-specific mortality: 67 year follow-up of participants in the 1947 Scottish Mental Survey. Medicine (Baltimore) 2016;95:e2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 1998;67:1111–8. [DOI] [PubMed] [Google Scholar]
- 63.Imai CM, Gunnarsdottir I, Gudnason V, Aspelund T, Birgisdottir BE, Thorsdottir I, et al. Faster increase in body mass index between ages 8 and 13 is associated with risk factors for cardiovascular morbidity and mortality. Nutr Metab Cardiovasc Dis 2014;24:730–6. [DOI] [PubMed] [Google Scholar]
- 64.Zheng Y, Song M, Manson JE, Giovannucci EL, Hu FB. Group-based trajectory of body shape from ages 5 to 55 years and cardiometabolic disease risk in 2 US cohorts. Am J Epidemiol 2017;186:1246–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. a follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med 1992;327:1350–5. [DOI] [PubMed] [Google Scholar]
- 66.Morrison JA, Glueck CJ, Woo JG, Wang P. Risk factors for cardiovascular disease and type 2 diabetes retained from childhood to adulthood predict adult outcomes: the Princeton LRC Follow-up Study. Int J Pediatr Endocrinol 2012;2012:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Furer A, Afek A, Orr O, Gershovitz L, Rabbi ML, Derazne E, et al. Sex-specific associations between adolescent categories of BMI with cardiovascular and non-cardiovascular mortality in midlife. Cardiovasc Diabetol 2018;17:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bhuiyan AR, Chen W, Srinivasan SR, Azevedo MJ, Berenson GS. Relationship of low birth weight to pulsatile arterial function in asymptomatic younger adults: the Bogalusa Heart Study. Am J Hypertens 2010;23:168–73. [DOI] [PubMed] [Google Scholar]
- 69.Rich-Edwards JW, Stampfer MJ, Manson JE, Rosner B, Hankinson SE, Colditz GA, et al. Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. BMJ 1997;315:396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lawani SO, Demerath EW, Lopez FL, Soliman EZ, Huxley RR,Rose KM, et al. Birth weight and the risk of atrial fibrillation in whites and African Americans: the Atherosclerosis Risk In Communities (ARIC) study. BMC Cardiovasc Disord 2014;14:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Larsson SC, Drca N, Jensen-Urstad M, Wolk A. Incidence of atrial fibrillation in relation to birth weight and preterm birth. Int J Cardiol 2015;178:149–52. [DOI] [PubMed] [Google Scholar]
- 72.Baker JL, Olsen LW, Sorensen TI. Weight at birth and all-cause mortality in adulthood. Epidemiology 2008;19:197–203. [DOI] [PubMed] [Google Scholar]
- 73.Lawlor DA, Davey Smith G, Ebrahim S. Birth weight is inversely associated with coronary heart disease in post-menopausal women: findings from the British women’s heart and health study. J Epidemiol Community Health 2004;58:120–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lawlor DA, Ronalds G, Clark H, Smith GD, Leon DA. Birth weight is inversely associated with incident coronary heart disease and stroke among individuals born in the 1950s: findings from the Aberdeen Children of the 1950s prospective cohort study. Circulation 2005;112:1414–8. [DOI] [PubMed] [Google Scholar]
- 75.Oberg S, Cnattingius S, Sandin S, Lichtenstein P, Iliadou AN. Birth weight predicts risk of cardiovascular disease within dizygotic but not monozygotic twin pairs: a large population-based co-twin-control study. Circulation 2011;123:2792–8. [DOI] [PubMed] [Google Scholar]
- 76.Syddall HE, Sayer AA, Simmonds SJ, Osmond C, Cox V, Dennison EM, et al. Birth weight, infant weight gain, and cause-specific mortality: the Hertfordshire Cohort Study. Am J Epidemiol 2005;161:1074–80. [DOI] [PubMed] [Google Scholar]
- 77.Frankel S, Elwood P, Sweetnam P, Yarnell J, Smith GD. Birthweight, body-mass index in middle age, and incident coronary heart disease. Lancet 1996;348:1478–80. [DOI] [PubMed] [Google Scholar]
- 78.Rajaleid K, Manor O, Koupil I. Does the strength of the association between foetal growth rate and ischaemic heart disease mortality differ by social circumstances in early or later life? J Epidemiol Community Health 2008;62:e6. [DOI] [PubMed] [Google Scholar]
- 79.Eriksson JG, Forsen T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ 2001;322:949–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Osmond C, Barker DJ, Winter PD, Fall CH, Simmonds SJ. Early growth and death from cardiovascular disease in women. BMJ 1993;307:1519–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Johnson RC, Schoeni RF. Early-life origins of adult disease: national longitudinal population-based study of the United States. Am J Public Health 2011;101:2317–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Forsen T, Eriksson JG, Tuomilehto J, Osmond C, Barker DJ. Growth in utero and during childhood among women who develop coronary heart disease: longitudinal study. BMJ 1999;319:1403–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Osmond C, Kajantie E, Forsen TJ, Eriksson JG, Barker DJ. Infant growth and stroke in adult life: the Helsinki birth cohort study. Stroke 2007;38:264–70. [DOI] [PubMed] [Google Scholar]
- 84.Koupilova I, Leon DA, McKeigue PM, Lithell HO. Is the effect of low birth weight on cardiovascular mortality mediated through high blood pressure? J Hypertens 1999;17:19–25. [DOI] [PubMed] [Google Scholar]
- 85.Rich-Edwards JW, Kleinman K, Michels KB, Stampfer MJ, Manson JE, Rexrode KM, et al. Longitudinal study of birth weight and adult body mass index in predicting risk of coronary heart disease and stroke in women. BMJ 2005;330:1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Arnold L, Hoy W, Wang Z. Low birthweight increases risk for cardiovascular disease hospitalisations in a remote Indigenous Australian community–a prospective cohort study. Aust N Z J Public Health 2016;40(Suppl 1):S102–6. [DOI] [PubMed] [Google Scholar]
- 87.Zoller B, Sundquist J, Sundquist K, Crump C. Perinatal risk factors for premature ischaemic heart disease in a Swedish national cohort. BMJ Open 2015;5:e007308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Leon DA, Lithell HO, Vagero D, Koupilova I, Mohsen R, Berglund L, et al. Reduced fetal growth rate and increased risk of death from ischaemic heart disease: cohort study of 15 000 Swedish men and women born 1915–29. BMJ 1998;317:241–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Smith CJ, Ryckman KK, Barnabei VM, Howard BV, Isasi CR, Sarto GE, et al. The impact of birth weight on cardiovascular disease risk in the Women’s Health Initiative. Nutr Metab Cardiovasc Dis 2016;26:239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hypponen E, Leon DA, Kenward MG, Lithell H. Prenatal growth and risk of occlusive and haemorrhagic stroke in Swedish men and women born 1915–29: historical cohort study. BMJ 2001;323:1033–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Forsen TJ, Eriksson JG, Osmond C, Barker DJ. The infant growth of boys who later develop coronary heart disease. Ann Med 2004;36:389–92. [DOI] [PubMed] [Google Scholar]
- 92.Forsen T, Osmond C, Eriksson JG, Barker DJ. Growth of girls who later develop coronary heart disease. Heart 2004;90:20–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega AC. Effect of birth size and catch-up growth on adult blood pressure and carotid intima-media thickness. Horm Res Paediatr 2012;77:394–401. [DOI] [PubMed] [Google Scholar]
- 94.Terzis ID, Papamichail C, Psaltopoulou T, Georgiopoulos GA, Lipsou N, Chatzidou S, et al. Long-term BMI changes since adolescence and markers of early and advanced subclinical atherosclerosis. Obesity (Silver Spring) 2012;20:414–20. [DOI] [PubMed] [Google Scholar]
- 95.Chu C, Dai Y, Mu J, Yang R, Wang M, Yang J, et al. Associations of risk factors in childhood with arterial stiffness 26 years later: the Hanzhong adolescent hypertension cohort. J Hypertens 2017;35:S10–5. [DOI] [PubMed] [Google Scholar]
- 96.Xi B, Zhang T, Li S, Harville E, Bazzano L, He J, et al. Can pediatric hypertension criteria be simplified? A prediction analysis of subclinical cardiovascular outcomes from the Bogalusa Heart Study. Hypertension 2017;69:691–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liang Y, Hou D, Shan X, Zhao X, Hu Y, Jiang B, et al. Cardiovascular remodeling relates to elevated childhood blood pressure: Beijing Blood Pressure Cohort Study. Int J Cardiol 2014;177:836–9. [DOI] [PubMed] [Google Scholar]
- 98.Li S, Chen W, Srinivasan SR, Berenson GS. Childhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa Heart Study. Hypertension 2004;43:541–6. [DOI] [PubMed] [Google Scholar]
- 99.Aatola H, Koivistoinen T, Tuominen H, Juonala M, Lehtimaki T, Viikari JSA, et al. Influence of child and adult elevated blood pressure on adult arterial stiffness: the Cardiovascular Risk in Young Finns Study. Hypertension 2017;70:531–6. [DOI] [PubMed] [Google Scholar]
- 100.Aatola H, Magnussen CG, Koivistoinen T, Hutri-Kahonen N, Juonala M, Viikari JS, et al. Simplified definitions of elevated pediatric blood pressure and high adult arterial stiffness. Pediatrics 2013;132:e70–6. [DOI] [PubMed] [Google Scholar]
- 101.Vos LE, Oren A, Uiterwaal C, Gorissen WH, Grobbee DE, Bots ML. Adolescent blood pressure and blood pressure tracking into young adulthood are related to subclinical atherosclerosis: the Atherosclerosis Risk in Young Adults (ARYA) study. Am J Hypertens 2003;16:549–55. [DOI] [PubMed] [Google Scholar]
- 102.Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Blood pressure trajectories from childhood to young adulthood associated with cardiovascular risk: results from the 23-year Longitudinal Georgia Stress and Heart Study. Hypertension 2017;69:435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation 2013;128:217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hartiala O, Magnussen CG, Kajander S, Knuuti J, Ukkonen H,Saraste A, et al. Adolescence risk factors are predictive of coronary artery calcification at middle age: the Cardiovascular Risk in Young Finns study. J Am Coll Cardiol 2012;60:1364–70. [DOI] [PubMed] [Google Scholar]
- 105.Magnussen CG, Dwyer T, Venn A. Family history of premature coronary heart disease, child cardio-metabolic risk factors and left ventricular mass. Cardiol Young 2014;24:938–40. [DOI] [PubMed] [Google Scholar]
- 106.Silventoinen K, Magnusson PK, Neovius M, Sundstrom J, Batty GD, Tynelius P, et al. Does obesity modify the effect of blood pressure on the risk of cardiovascular disease? A population-based cohort study of more than one million Swedish men. Circulation 2008;118:1637–42. [DOI] [PubMed] [Google Scholar]
- 107.Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ 2011;342:d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Leiba A, Twig G, Levine H, Goldberger N, Afek A, Shamiss A, et al. Hypertension in late adolescence and cardiovascular mortality in midlife: a cohort study of 2.3 million 16- to 19-year-old examinees. Pediatr Nephrol 2016;31:485–92. [DOI] [PubMed] [Google Scholar]
- 109.Erlingsdottir A, Indridason OS, Thorvaldsson O, Edvardsson VO. Blood pressure in children and target-organ damage later in life. Pediatr Nephrol 2010;25:323–8. [DOI] [PubMed] [Google Scholar]
- 110.Juonala M, Viikari JS, Ronnemaa T, Marniemi J, Jula A, Loo BM, et al. Associations of dyslipidemias from childhood to adulthood with carotid intima-media thickness, elasticity, and brachial flow-mediated dilatation in adulthood: the Cardiovascular Risk in Young Finns Study. Arterioscler Thromb Vasc Biol 2008;28:1012–7. [DOI] [PubMed] [Google Scholar]
- 111.Li S, Chen W, Srinivasan SR, Tang R, Bond MG, Berenson GS. Race (black-white) and gender divergences in the relationship of childhood cardiovascular risk factors to carotid artery intima-media thickness in adulthood: the Bogalusa Heart Study. Atherosclerosis 2007;194:421–5. [DOI] [PubMed] [Google Scholar]
- 112.Magnussen CG, Venn A, Thomson R, Juonala M, Srinivasan SR, Viikari JS, et al. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the Cardiovascular Risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol 2009;53:860–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Frontini MG, Srinivasan SR, Xu J, Tang R, Bond MG, Berenson GS. Usefulness of childhood non-high density lipoprotein cholesterol levels versus other lipoprotein measures in predicting adult subclinical atherosclerosis: the Bogalusa Heart Study. Pediatrics 2008;121:924–9. [DOI] [PubMed] [Google Scholar]
- 114.Morrison JA, Glueck CJ, Wang P. Childhood risk factors predict cardiovascular disease, impaired fasting glucose plus type 2 diabetes mellitus, and high blood pressure 26 years later at a mean age of 38 years: the Princeton-lipid research clinics follow-up study. Metabolism 2012;61:531–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Morrison JA, Glueck CJ, Horn PS, Yeramaneni S, Wang P. Pediatric triglycerides predict cardiovascular disease events in the fourth to fifth decade of life. Metabolism 2009;58:1277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yajnik CS, Katre PA, Joshi SM, Kumaran K, Bhat DS, Lubree HG, et al. Higher glucose, insulin and insulin resistance (HOMA-IR) in childhood predict adverse cardiovascular risk in early adulthood: the Pune Children’s Study. Diabetologia 2015;58:1626–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McCarron P, Smith GD, Okasha M, McEwen J. Smoking in adolescence and young adulthood and mortality in later life: prospective observational study. J Epidemiol Community Health 2001;55:334–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Whitley E, Lee IM, Sesso HD, Batty GD. Association of cigarette smoking from adolescence to middle-age with later total and cardiovascular disease mortality: the Harvard Alumni Health Study. J Am Coll Cardiol 2012;60:1839–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Choi SH, Stommel M. Impact of age at smoking initiation on smoking-related morbidity and all-cause mortality. Am J Prev Med 2017;53:33–41. [DOI] [PubMed] [Google Scholar]
- 120.Geerts CC, Bots ML, Grobbee DE, Uiterwaal CS. Parental smoking and vascular damage in young adult offspring: is early life exposure critical? The atherosclerosis risk in young adults study. Arterioscler Thromb Vasc Biol 2008;28:2296–302. [DOI] [PubMed] [Google Scholar]
- 121.Gall S, Huynh QL, Magnussen CG, Juonala M, Viikari JS, Kahonen M, et al. Exposure to parental smoking in childhood or adolescence is associated with increased carotid intima-media thickness in young adults: evidence fromtheCardiovascularRiskinYoungFinnsstudyandtheChildhoodDeterminants of Adult Health Study. Eur Heart J 2014;35:2484–91. [DOI] [PubMed] [Google Scholar]
- 122.West HW, Juonala M, Gall SL, Kahonen M, Laitinen T, Taittonen L, et al. Exposure to parental smoking in childhood is associated with increased risk of carotid atherosclerotic plaque in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 2015;131:1239–46. [DOI] [PubMed] [Google Scholar]
- 123.Palve KS, Pahkala K, Magnussen CG, Koivistoinen T, Juonala M, Kahonen M, et al. Association of physical activity in childhood and early adulthood with carotid artery elasticity 21 years later: the cardiovascular risk in Young Finns Study. J Am Heart Assoc 2014;3:e000594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.van de Laar RJ, Ferreira I, van Mechelen W, Prins MH, Twisk JW, Stehouwer CD. Habitual physical activity and peripheral arterial compliance in young adults: the Amsterdam growth and health longitudinal study. Am J Hypertens 2011;24:200–8. [DOI] [PubMed] [Google Scholar]
- 125.van de Laar RJ, Ferreira I, van Mechelen W, Prins MH, Twisk JW, Stehouwer CD. Lifetime vigorous but not light-to-moderate habitual physical activity impacts favorably on carotid stiffness in young adults: the Amsterdam Growth and Health Longitudinal Study. Hypertension 2010;55:33–9. [DOI] [PubMed] [Google Scholar]
- 126.Ried-Larsen M, Grontved A, Kristensen PL, Froberg K, Andersen LB. Moderate-and-vigorous physical activity from adolescence to adulthood and subclinical atherosclerosis in adulthood: prospective observations from the European Youth Heart Study. Br J Sports Med 2015;49:107–12. [DOI] [PubMed] [Google Scholar]
- 127.Drca N, Wolk A, Jensen-Urstad M, Larsson SC. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men. Heart 2014;100:1037–42. [DOI] [PubMed] [Google Scholar]
- 128.Aatola H, Koivistoinen T, Hutri-Kahonen N, Juonala M, Mikkila V, Lehtimaki T, et al. Lifetime fruit and vegetable consumption and arterial pulse wave velocity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 2010;122:2521–8. [DOI] [PubMed] [Google Scholar]
- 129.van de Laar RJ, Stehouwer CD, van Bussel BC, te Velde SJ, Prins MH, Twisk JW, et al. Lower lifetime dietary fiber intake is associated with carotid artery stiffness: the Amsterdam Growth and Health Longitudinal Study. Am J Clin Nutr 2012;96:14–23. [DOI] [PubMed] [Google Scholar]
- 130.van de Laar RJ, Stehouwer CD, van Bussel BC, Prins MH, Twisk JW, Ferreira I. Adherence to a Mediterranean dietary pattern in early life is associated with lower arterial stiffness in adulthood: the Amsterdam Growth and Health Longitudinal Study. J Intern Med 2013;273:79–93. [DOI] [PubMed] [Google Scholar]
- 131.McCourt HJ, Draffin CR, Woodside JV, Cardwell CR, Young IS, Hunter SJ, et al. Dietary patterns and cardiovascular risk factors in adolescents and young adults: the Northern Ireland Young Hearts Project. Br J Nutr 2014;112:1685–98. [DOI] [PubMed] [Google Scholar]
- 132.Kaikkonen JE, Jula A, Mikkila V, Juonala M, Viikari JS, Moilanen T, et al. Childhood serum fatty acid quality is associated with adult carotid artery intima media thickness in women but not in men. J Nutr 2013;143:682–9. [DOI] [PubMed] [Google Scholar]
- 133.Mikkila V, Rasanen L, Laaksonen MM, Juonala M, Viikari J, Pietinen P, et al. Long-term dietary patterns and carotid artery intima media thickness: the Cardiovascular Risk in Young Finns Study. Br J Nutr 2009;102:1507–12. [DOI] [PubMed] [Google Scholar]
- 134.van der Pols JC, Gunnell D, Williams GM, Holly JM, Bain C, Martin RM. Childhood dairy and calcium intake and cardiovascular mortality in adulthood: 65-year follow-up of the Boyd Orr cohort. Heart 2009;95:1600–6. [DOI] [PubMed] [Google Scholar]
- 135.Ness AR, Maynard M, Frankel S, Smith GD, Frobisher C, Leary SD, et al. Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart 2005;91:894–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jarvisalo MJ, Hutri-Kahonen N, Juonala M, Mikkila V, Rasanen L, Lehtimaki T, et al. Breast feeding in infancy and arterial endothelial function later in life. The Cardiovascular Risk in Young Finns Study. Eur J Clin Nutr 2009;63:640–5. [DOI] [PubMed] [Google Scholar]
- 137.Martin RM, Ebrahim S, Griffin M, Davey Smith G, Nicolaides AN, Georgiou N, et al. Breastfeeding and atherosclerosis: intima-media thickness and plaques at 65-year follow-up of the Boyd Orr cohort. Arterioscler Thromb Vasc Biol 2005;25:1482–8. [DOI] [PubMed] [Google Scholar]
- 138.Rich-Edwards JW, Stampfer MJ, Manson JE, Rosner B, Hu FB, Michels KB, et al. Breastfeeding during infancy and the risk of cardiovascular disease in adulthood. Epidemiology 2004;15:550–6. [DOI] [PubMed] [Google Scholar]
- 139.Martin RM, Davey SmithG, Mangtani P, Tilling K, Frankel S, Gunnell D. Breastfeeding and cardiovascular mortality: the Boyd Orr cohort and a systematic review with meta-analysis. Eur Heart J 2004;25:778–86. [DOI] [PubMed] [Google Scholar]
- 140.Fall CH, Barker DJ, Osmond C, Winter PD, Clark PM, Hales CN. Relation of infant feeding to adult serum cholesterol concentration and death from ischaemic heart disease. BMJ 1992;304:801–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kivimaki M, Lawlor DA, Juonala M, Smith GD, Elovainio M, Keltikan-gas-Jarvinen L, et al. Lifecourse socioeconomic position, C-reactive protein, and carotid intima-media thickness in young adults: the cardiovascular risk in Young Finns Study. Arterioscler Thromb Vasc Biol 2005;25:2197–202. [DOI] [PubMed] [Google Scholar]
- 142.Kivimaki M, Smith GD, Juonala M, Ferrie JE, Keltikangas-Jarvinen L, Elovainio M, et al. Socioeconomic position in childhood and adult cardiovascular risk factors, vascular structure, and function: Cardiovascular Risk in Young Finns study. Heart 2006;92:474–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Laitinen TT, Puolakka E, Ruohonen S, Magnussen CG, Smith KJ, Viikari JSA, et al. Association of socioeconomic status in childhood with left ventricular structure and diastolic function in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA Pediatr 2017;171:781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Smith GD, Hart C, Blane D, Hole D. Adverse socioeconomic conditions in childhood and cause specific adult mortality: prospective observational study. BMJ 1998;316:1631–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kittleson MM, Meoni LA, Wang NY, Chu AY, Ford DE, Klag MJ. Association of childhood socioeconomic status with subsequent coronary heart disease in physicians. Arch Intern Med 2006;166:2356–61. [DOI] [PubMed] [Google Scholar]
- 146.Lynch JW, Kaplan GA, Cohen RD, Kauhanen J, Wilson TW, Smith NL, et al. Childhood and adult socioeconomic status as predictors of mortality in Finland. Lancet 1994;343:524–7. [DOI] [PubMed] [Google Scholar]
- 147.Gliksman MD, Kawachi I, Hunter D, Colditz GA, Manson JE, Stampfer MJ, et al. Childhood socioeconomic status and risk of cardiovascular disease in middle aged US women: a prospective study. J Epidemiol Community Health 1995;49:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Heshmati A, Chaparro MP, Goodman A, Koupil I. Early life characteristics, social mobility during childhood and risk of stroke in later life: findings from a Swedish cohort. Scand J Public Health 2017;45:419–27. [DOI] [PubMed] [Google Scholar]
- 149.Lawlor DA, Ronalds G, Macintyre S, Clark H, Leon DA. Family socioeconomic position at birth and future cardiovascular disease risk: findings from the Aberdeen Children of the 1950s cohort study. Am J Public Health 2006;96:1271–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Melchior M, Berkman LF, Kawachi I, Krieger N, Zins M, Bonenfant S, et al. Lifelong socioeconomic trajectory and premature mortality (35–65 years) in France: findings from the GAZEL Cohort Study. J Epidemiol Community Health 2006;60:937–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kamphuis CB, Turrell G, Giskes K, Mackenbach JP, van Lenthe FJ. Socioeconomic inequalities in cardiovascular mortality and the role of childhood socioeconomic conditions and adulthood risk factors: a prospective cohort study with 17-years of follow up. BMC Public Health 2012;12:1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Osler M, Andersen AM, Due P, Lund R, Damsgaard MT, Holstein BE. Socioeconomic position in early life, birth weight, childhood cognitive function, and adult mortality. A longitudinal study of Danish men born in 1953. J Epidemiol Community Health 2003;57:681–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Anderson EL, Fraser A, Caleyachetty R, Hardy R, Lawlor DA, Howe LD. Associations of adversity in childhood and risk factors for cardiovascular disease in mid-adulthood. Child Abuse Negl 2018;76:138–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rotar O, Moguchaia E, Boyarinova M, Kolesova E, Khromova N, Freylikhman O, et al. Seventy years after the siege of Leningrad: does early life famine still affect cardiovascular risk and aging? J Hypertens 2015;33:1772–9. [DOI] [PubMed] [Google Scholar]
- 155.Thurston RC, Chang Y, Derby CA, Bromberger JT, Harlow SD, Janssen I, et al. Abuse and subclinical cardiovascular disease among midlife women: the study of women’s health across the nation. Stroke 2014;45:2246–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Loucks EB, Taylor SE, Polak JF, Wilhelm A, Kalra P, Matthews KA. Childhood family psychosocial environment and carotid intima media thickness: the CARDIA study. Soc Sci Med 2014;104:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Cruickshank JK, Silva MJ, Molaodi OR, Enayat ZE, Cassidy A, Karamanos A, et al. Ethnic differences in and childhood influences on early adult pulse wave velocity: the determinants of adolescent, now young adult, social wellbeing, and health longitudinal study. Hypertension 2016;67:1133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Juonala M, Pulkki-Raback L, Elovainio M, Hakulinen C, Magnussen CG, Sabin MA, et al. Childhood psychosocial factors and coronary artery calcification in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA Pediatr 2016;170:466–72. [DOI] [PubMed] [Google Scholar]
- 159.Head RF, Gilthorpe MS, Byrom A, Ellison GT. Cardiovascular disease in a cohort exposed to the 1940–45 Channel Islands occupation. BMC Public Health 2008;8:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Korkeila J, Vahtera J, Korkeila K, Kivimaki M, Sumanen M, Koskenvuo K, et al. Childhood adversities as predictors of incident coronary heart disease and cerebrovascular disease. Heart 2010;96:298–303. [DOI] [PubMed] [Google Scholar]
- 161.Halonen JI, Stenholm S, Pentti J, Kawachi I, Subramanian SV, Kivimaki M, et al. Childhood psychosocial adversity and adult neighborhood disadvantage as predictors of cardiovascular disease: a cohort study. Circulation 2015;132:371–9. [DOI] [PubMed] [Google Scholar]
- 162.Morton PM, Mustillo SA, Ferraro KF. Does childhood misfortune raise the risk of acute myocardial infarction in adulthood? Soc Sci Med 2014;104:133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Woo J, Leung JC, Wong SY. Impact of childhood experience of famine on late life health. J Nutr Health Aging 2010;14:91–5. [DOI] [PubMed] [Google Scholar]
- 164.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation 2004;110:1761–6. [DOI] [PubMed] [Google Scholar]
- 165.Hollingshaus MS, Smith KR. Life and death in the family: early parental death, parental remarriage, and offspring suicide risk in adulthood. Soc Sci Med 2015;131:181–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Robertson J, Schioler L, Toren K, Soderberg M, Love J, Waern M, et al. Mental disorders and stress resilience in adolescence and long-term risk of early heart failure among Swedish men. Int J Cardiol 2017;243:326–31. [DOI] [PubMed] [Google Scholar]
- 167.Garad Y, Maximova K, MacKinnon N, McGrath JJ, Kozyrskyj AL, Colman I. Sex-specific differences in the association between childhood adversity and cardiovascular disease in adulthood: evidence from a national cohort study. Can J Cardiol 2017;33:1013–9. [DOI] [PubMed] [Google Scholar]
- 168.Bergh C, Udumyan R, Fall K, Nilsagard Y, Appelros P, Montgomery S. Stress resilience in male adolescents and subsequent stroke risk: cohort study. J Neurol Neurosurg Psychiatry 2014;85:1331–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Shi Z, Nicholls SJ, Taylor AW, Magliano DJ, Appleton S, Zimmet P. Early life exposure to Chinese famine modifies the association between hypertension and cardiovascular disease. J Hypertens 2018;36:54–60. [DOI] [PubMed] [Google Scholar]
- 170.Magnussen CG, Koskinen J, Juonala M, Chen W, Srinivasan SR, Sabin MA, et al. A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa heart and Cardiovascular Risk in Young Finns Studies. J Am Coll Cardiol 2012;60:1631–9. [DOI] [PubMed] [Google Scholar]
- 171.Koskinen J, Magnussen CG, Sinaiko A, Woo J, Urbina E, Jacobs DR Jr, et al. Childhood age and associations between childhood metabolic syndrome and adult risk for metabolic syndrome, Type 2 Diabetes mellitus and carotid intima media thickness: the International Childhood Cardiovascular Cohort Consortium. J Am Heart Assoc 2017;6:e005632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Magnussen CG, Cheriyan S, Sabin MA, Juonala M, Koskinen J, Thomson R, et al. Continuous and dichotomous metabolic syndrome definitions in youth predict adult type 2 Diabetes and carotid artery intima media thickness: the Cardiovascular Risk in Young Finns Study. J Pediatr 2016;171:97–103.e1–3. [DOI] [PubMed] [Google Scholar]
- 173.Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 2010;122:1604–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Koivistoinen T, Hutri-Kahonen N, Juonala M, Aatola H, Koobi T, Lehtimaki T, et al. Metabolic syndrome in childhood and increased arterial stiffness in adulthood: the Cardiovascular Risk In Young Finns Study. Ann Med 2011;43:312–9. [DOI] [PubMed] [Google Scholar]
- 175.DeBoer MD, Gurka MJ, Morrison JA, Woo JG. Inter-relationships between the severity of metabolic syndrome, insulin and adiponectin and their relationship to future type 2 diabetes and cardiovascular disease. Int J Obes (Lond) 2016;40:1353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics 2007;120:340–5. [DOI] [PubMed] [Google Scholar]
- 177.DeBoer MD, Gurka MJ, Woo JG, Morrison JA. Severity of metabolic syndrome as a predictor of cardiovascular disease between childhood and adulthood: the Princeton Lipid Research Cohort Study. J Am Coll Cardiol 2015;66:755–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Laitinen TT, Pahkala K, Magnussen CG, Viikari JS, Oikonen M, Taittonen L, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 2012;125:1971–8. [DOI] [PubMed] [Google Scholar]
- 179.Laitinen TT, Pahkala K, Magnussen CG, Oikonen M, Viikari JS, Sabin MA, et al. Lifetime measures of ideal cardiovascular health and their association with subclinical atherosclerosis: the Cardiovascular Risk in Young Finns Study. Int J Cardiol 2015;185:186–91. [DOI] [PubMed] [Google Scholar]
- 180.Tatsukawa Y, Nakashima E, Yamada M, Funamoto S, Hida A, Akahoshi M, et al. Cardiovascular disease risk among atomic bomb survivors exposed in utero, 1978–2003. Radiat Res 2008;170:269–74. [DOI] [PubMed] [Google Scholar]
- 181.Roseboom TJ, van der Meulen JH, Osmond C, Barker DJ, Ravelli AC, Schroeder-Tanka JM, et al. Coronary heart disease after prenatal exposure to the Dutch famine, 1944–45. Heart 2000;84:595–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Ekamper P, van Poppel F, Stein AD, Bijwaard GE, Lumey LH. Prenatal famine exposure and adult mortality from cancer, cardiovascular disease, and other causes through age 63 years. Am J Epidemiol 2015;181:271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Painter RC, de Rooij SR, Bossuyt PM, de Groot E, Stok WJ, Osmond C, et al. Maternal nutrition during gestation and carotid arterial compliance in the adult offspring: the Dutch famine birth cohort. J Hypertens 2007;25:533–40. [DOI] [PubMed] [Google Scholar]
- 184.van Abeelen AF, Veenendaal MV, Painter RC, de Rooij SR, Dijkgraaf MG, Bossuyt PM, et al. Survival effects of prenatal famine exposure. Am J Clin Nutr 2012;95:179–83. [DOI] [PubMed] [Google Scholar]
- 185.Rerkasem K, Wongthanee A, Rerkasem A, Chiowanich P, Sritara P, Pruenglampoo S, et al. Intrauterine nutrition and carotid intimal media thickness in young Thai adults. Asia Pac J Clin Nutr 2012;21:247–52. [PubMed] [Google Scholar]
- 186.Eriksson JG, Sandboge S, Salonen MK, Kajantie E, Osmond C. Long-term consequences of maternal overweight in pregnancy on offspring later health: findings from the Helsinki Birth Cohort Study. Ann Med 2014;46:434–8. [DOI] [PubMed] [Google Scholar]
- 187.Kajantie E, Eriksson JG, Osmond C, Thornburg K, Barker DJ. Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki birth cohort study. Stroke 2009;40:1176–80. [DOI] [PubMed] [Google Scholar]
- 188.Bjarnegard N, Morsing E, Cinthio M, Lanne T, Brodszki J. Cardiovascular function in adulthood following intrauterine growth restriction with abnormal fetal blood flow. Ultrasound Obstet Gynecol 2013;41:177–84. [DOI] [PubMed] [Google Scholar]
- 189.Skilton MR, Viikari JS, Juonala M, Laitinen T, Lehtimaki T, Taittonen L, et al. Fetal growth and preterm birth influence cardiovascular risk factors and arterial health in young adults: the Cardiovascular Risk in Young Finns Study. Arterioscler Thromb Vasc Biol 2011;31:2975–81. [DOI] [PubMed] [Google Scholar]
- 190.Fan Z, Zhang ZX, Li Y, Wang Z, Xu T, Gong X, et al. Relationship between birth size and coronary heart disease in China. Ann Med 2010;42:596–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ueda P, Cnattingius S, Stephansson O, Ingelsson E, Ludvigsson JF, Bonamy AK. Cerebrovascular and ischemic heart disease in young adults born preterm: a population-based Swedish cohort study. Eur J Epidemiol 2014;29:253–60. [DOI] [PubMed] [Google Scholar]
- 192.Kajantie E, Osmond C, Eriksson JG. Coronary heart disease and stroke in adults born preterm - the Helsinki Birth Cohort Study. Paediatr Perinat Epidemiol 2015;29:515–9. [DOI] [PubMed] [Google Scholar]
- 193.Lewandowski AJ, Augustine D, Lamata P, Davis EF, Lazdam M, Francis J, et al. Preterm heart in adult life: cardiovascular magnetic resonance reveals distinct differences in left ventricular mass, geometry, and function. Circulation 2013;127:197–206. [DOI] [PubMed] [Google Scholar]
- 194.Risnes KR, Romundstad PR, Nilsen TI, Eskild A, Vatten LJ. Placental weight relative to birth weight and long-term cardiovascular mortality: findings from a cohort of 31,307 men and women. Am J Epidemiol 2009;170:622–31. [DOI] [PubMed] [Google Scholar]
- 195.Risnes KR, Nilsen TI, Romundstad PR, Vatten LJ. Head size at birth and long-term mortality from coronary heart disease. Int J Epidemiol 2009;38:955–62. [DOI] [PubMed] [Google Scholar]
- 196.Barker DJ, Gelow J, Thornburg K, Osmond C, Kajantie E, Eriksson JG. The early origins of chronic heart failure: impaired placental growth and initiation of insulin resistance in childhood. Eur J Heart Fail 2010;12:819–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Palinski W Effect of maternal cardiovascular conditions and risk factors on offspring cardiovascular disease. Circulation 2014;129:2066–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Gunnell DJ, Davey Smith G, Frankel S, Nanchahal K, Braddon FE, Pemberton J, et al. Childhood leg length and adult mortality: follow up of the Carnegie (Boyd Orr) Survey of Diet and Health in Pre-war Britain. J Epidemiol Community Health 1998;52:142–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Silventoinen K, Baker JL, Sorensen TI. Growth in height in childhood and risk of coronary heart disease in adult men and women. PLoS One 2012;7:e30476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Whitley E, Martin RM, Davey Smith G, Holly JM, Gunnell D. The association of childhood height, leg length and other measures of skeletal growth with adult cardiovascular disease: the Boyd-Orr cohort. J Epidemiol Community Health 2012;66:18–23. [DOI] [PubMed] [Google Scholar]
- 201.Batty GD, Smith GD, Fall CH, Sayer AA, Dennison E, Cooper C, et al. Association of diarrhoea in childhood with blood pressure and coronary heart disease in older age: analyses of two UK cohort studies. Int J Epidemiol 2007;36:1349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Mueller NT, Odegaard AO, Gross MD, Koh WP, Yuan JM, Pereira MA. Age at menarche and cardiovascular disease mortality in Singaporean Chinese women: the Singapore Chinese Health Study. Ann Epidemiol 2012;22:717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Canoy D, Beral V, Balkwill A, Wright FL, Kroll ME, Reeves GK, et al. Age at menarche and risks of coronary heart and other vascular diseases in a large UK cohort. Circulation 2015;131:237–44. [DOI] [PubMed] [Google Scholar]
- 204.Wang Q, Shen JJ. Childhood health status and adulthood cardiovascular disease morbidity in rural China: are they related? Int J Environ Res Public Health 2016;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Juonala M, Viikari JS, Ronnemaa T, Taittonen L, Marniemi J, Raitakari OT. Childhood C-reactive protein in predicting CRP and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. Arterioscler Thromb Vasc Biol 2006;26:1883–8. [DOI] [PubMed] [Google Scholar]
- 206.Du Y, Zhang T, Sun D, Li C, Bazzano L, Qi L, et al. Effect of serum adiponectin levels on the association between childhood body mass index and adulthood carotid intima-media thickness. Am J Cardiol 2018;121:579–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Saarikoski LA, Juonala M, Huupponen R, Viikari JS, Lehtimaki T, Jokinen E, et al. Low serum adiponectin levels in childhood and adolescence predict increased intima-media thickness in adulthood. The Cardiovascular Risk in Young Finns Study. Ann Med 2017;49:42–50. [DOI] [PubMed] [Google Scholar]
- 208.Batty GD, Mortensen EL, Nybo Andersen AM, Osler M. Childhood intelligence in relation to adult coronary heart disease and stroke risk: evidence from a Danish birth cohort study. Paediatr Perinat Epidemiol 2005;19:452–9. [DOI] [PubMed] [Google Scholar]
- 209.Keltikangas-Jarvinen L, Pulkki-Raback L, Puttonen S, Viikari J, Raitakari OT. Childhood hyperactivity as a predictor of carotid artery intima media thickness over a period of 21 years: the Cardiovascular Risk in Young Finns Study. Psychosom Med 2006;68:509–16. [DOI] [PubMed] [Google Scholar]
- 210.Dedman DJ, Gunnell D, Davey Smith G, Frankel S. Childhood housing conditions and later mortality in the Boyd Orr cohort. J Epidemiol Community Health 2001;55:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Howard VJ, McClure LA, Glymour MM, Cunningham SA, Kleindorfer DO, Crowe M, et al. Effect of duration and age at exposure to the Stroke Belt on incident stroke in adulthood. Neurology 2013;80:1655–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Aberg ND, Kuhn HG, Nyberg J, Waern M, Friberg P, Svensson J, et al. Influence of cardiovascular fitness and muscle strength in early adulthood on long-term risk of stroke in Swedish Men. Stroke 2015;46:1769–76. [DOI] [PubMed] [Google Scholar]
- 213.Ferreira I, Twisk JW, Van Mechelen W, Kemper HC, Stehouwer CD. Current and adolescent levels of cardiopulmonary fitness are related to large artery properties at age 36: the Amsterdam Growth and Health Longitudinal Study. Eur J Clin Invest 2002;32:723–31. [DOI] [PubMed] [Google Scholar]
- 214.Ferreira I, Twisk JW, Stehouwer CD, van Mechelen W, Kemper HC. Longitudinal changes in .VO2max: associations with carotid IMT and arterial stiffness. Med Sci Sports Exerc 2003;35:1670–8. [DOI] [PubMed] [Google Scholar]
- 215.Lindgren M, Aberg M, Schaufelberger M, Aberg D, Schioler L, Toren K, et al. Cardiorespiratory fitness and muscle strength in late adolescence and long-term risk of early heart failure in Swedish men. Eur J Prev Cardiol 2017;24:876–84. [DOI] [PubMed] [Google Scholar]
- 216.Hogstrom G, Nordstrom A, Nordstrom P. High aerobic fitness in late adolescence is associated with a reduced risk of myocardial infarction later in life: a nationwide cohort study in men. Eur Heart J 2014;35:3133–40. [DOI] [PubMed] [Google Scholar]
- 217.Sinaiko AR, Jacobs DR Jr, Woo JG, Bazzano L, Burns T, Hu T, et al. The International Childhood Cardiovascular Cohort (i3C) consortium outcomes study of childhood cardiovascular risk factors and adult cardiovascular morbidity and mortality: design and recruitment. Contemp Clin Trials 2018;69:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ghosh AK, Francis DP, Chaturvedi N, Kuh D, Mayet J, Hughes AD, et al. Cardiovascular risk factors from early life predict future adult cardiac structural and functional abnormalities: a systematic review of the published literature. J Cardiol Ther 2014;2:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Galobardes B, Smith GD, Lynch JW. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Ann Epidemiol 2006;16:91–104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing statement available at www.jpeds.com.


