Abstract
Thirteen studies were included in the current systematic review and meta-analysis with 1131 participants. Both within- and between-group comparisons demonstrated reductions in depressive and PTSD symptoms with medium effect sizes post MBSR intervention. Additionally, MBSR demonstrated small effects in improving mindfulness in veterans at post-intervention. Maintenance of treatment effects were observed at follow-up for the three outcomes during within-group comparisons. Treatment effects were maintained at follow-up between-groups for depression and mindfulness, but not for PTSD symptoms. Furthermore, there were no significant differences between MBSR and cognitive behavioural therapy/person-centred group therapy intervention groups in the three outcomes.
Keywords: defence force, depression, MBSR, mental health, posttraumatic stress disorder (PTSD)
Introduction
Military service places individuals in extreme environments and exposes them to traumatic combat scenes and potentially debilitating injuries (Haagen et al., 2015; Inoue et al., 2023). The consequences of this accumulation of trauma can impact mental health long after service personnel have left the armed forces (van Hooff et al., 2019). As a result, veterans face a heightened risk of mental health disorders; posttraumatic stress disorder (PTSD) and depression are the most prevalent mental health conditions that veterans face (Inoue et al., 2023) and they form the central focus of the current study. PTSD refers to a psychological disorder that develops after witnessing or experiencing a traumatic event(s) or circumstance(s) and includes intrusion symptoms relating to the trauma, avoidance of reminders of the traumatic event, negative alterations in thinking and mood, and alterations in arousal and reactivity (American Psychiatric Association, 2023). Depression is a mental health condition that negatively affects people’s mood, thinking, and behaviour, often resulting in prolonged periods of low mood or a loss of interest or pleasure in activities (WHO, 2023). Approximately 50% of Australian Defence Force (ADF) veterans have been diagnosed with a mental disorder, including PTSD and depression, with the prevalence of PTSD symptoms in veterans (17.7%) twice as high as in the general population (8.7%) (van Hooff et al., 2019). In the UK, the prevalence of PTSD symptoms in veterans (9%) is more than twice as high as that of active defence members (4%) (Stevelink et al., 2018).
Treatments recommended for military-related PTSD include trauma-focused therapies such as prolonged exposure therapy, cognitive processing therapy, and trauma-focused cognitive behavioural therapy (Haagen et al., 2015; Meis et al., 2021; Watkins et al., 2018). However, these treatments present various challenges. Firstly, the high noncompletion or “dropout” rates, ranging from 25–48% pose a significant challenge when treating PTSD (Sciarrino et al., 2022; Steenkamp et al., 2020), and recent reviews suggested that noncompletion rates for PTSD treatment tend to be higher in veteran populations compared to civilians (Edwards-Stewart et al., 2021; Varker et al., 2021). A review by Edwards-Stewart et al. (2021) found that the therapy attrition rate of veterans participating in trauma-focused therapies (24.3%) is higher than that of veterans participating in non-trauma-focused therapies (16.1%). Secondly, clinically significant symptom improvement in trauma-focused therapies is found to be varied among military veterans (Steenkamp et al., 2020). For example, in a sample of 960 veterans, Murphy and Smith (2018) found that 27.5% of participants had poor treatment response and experienced higher rates of depression, anxiety, and anger after a trauma-focused cognitive behavioural therapy intervention. Moreover, the participants’ PTSD symptoms were maintained at a 12-month follow up. Thirdly, benefits from prolonged exposure and cognitive processing therapies are found to be minor; compared to non-trauma focused treatments (Steenkamp et al., 2020). For instance, in a random controlled trial (RCT) comparing the effectiveness of transcendental meditation to prolonged exposure for PTSD treatment for veterans, 61% of participants who were treated with transcendental meditation showed clinically significant improvement compared to 41% treated with prolonged exposure (Nidich et al., 2018). Given these challenges, there is a growing need for alternative therapeutic approaches for veterans dealing with mental health disorders (Hundt et al., 2020).
Mindfulness-based intervention (MBI) is one such promising alternative therapy. Mindfulness is defined as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (Kabat-Zinn, 2013: 145). Mindfulness can be cultivated through meditation, a state of detached observation and awareness of the present moment (Kabat-Zinn, 2003), aiming to increase awareness of thoughts and feelings of the present moment and attend to the thoughts and feelings without judgement (Kabat-Zinn, 2003, 2013; Li et al., 2023b, 2024a; Omidi et al., 2013; Schure et al., 2018). Meditation practices encourage emotional regulation by enabling an individual to respond rather than react to stressful situations (Bishop, 2002; Li et al., 2023a). Mindfulness-based stress intervention (MBSR) is one of the most widely studied MBIs. MBSR is a non-trauma focused treatment that is delivered through an eight-week standardised group program (Kabat-Zinn, 2003) and employs a mind-body connection and a relaxed non-judgemental state of mind to aid in reducing PTSD symptoms, arousal, and improve mood (Kim et al., 2013). A meta-analysis of randomised controlled trials (RCTs) in a general PTSD population, revealed a significant medium effect of MBSR on reducing PTSD symptoms (Hedges’ g = 0.46, p < 0.001) when compared to the treatment as usual (TAU; Liu et al., 2022). A meta-analysis of the effect of MBSR on the mental health of breast cancer survivors found a medium effect on reducing depression symptoms (Cohen’s d = 0.575, p < 0.0001) and a large effect on anxiety (Cohen’s d = 0.733, p < 0.0001) (Zainal et al., 2013). Within the veteran population, empirical evidence has shown reduction in symptoms of anxiety, depression, PTSD, and suicidal ideation among veterans after MBSR intervention (Felleman et al., 2016; Kearney et al., 2016; Marchand et al., 2021; Polusny et al., 2015; Serpa et al., 2014).
The promising effects of MBSR on mental health outcomes have led to a growing interest in exploring the underlying mechanisms that help understand the effects. Psychological factors such as self-reported mindfulness, decentering, acceptance, and emotional regulation have been identified as mechanisms of MBSR’s effects (Creswell, 2017). MBSR has been associated with higher levels of self-reported mindfulness, which in turn is associated with decreases in PTSD symptoms among veterans (Polusny et al., 2015). Decentering refers to a process of observing internal experiences from an objective and non-judging stance towards the self (Creswell, 2017; Kessel et al., 2016) and higher levels of decentering after MBSR intervention have been shown to be associated with lower levels of depressive symptoms (Kessel et al., 2016).
Neurobiologically, research suggests that mindfulness interventions may change the function and structure of the brain, which in turn results in improved mental health (Creswell, 2017). MBSR has been shown to increase ventrolateral prefrontal cortex activity, which was associated with reductions in anxiety symptoms (Hölzel et al., 2011). Furthermore Creswell et al. (2016) found that mindfulness meditation increased the resting state functional connectivity of brain networks (the Default Mode Network) and executive control (the Executive Control Network), resulting in improved mental health outcomes. Additionally, MBSR treatment was demonstrated to lead to changes in brain functions associated with a decrease in activation of fear, and stress responses in PTSD patients (Bremner et al., 2017).
The psychological and neurological mechanisms underlying the effect of MBSR on mental health outcomes reflect the paradigm of the mind-body relationship (Kabat-Zinn, 2013) that is informed by the embodied cognition framework. Embodied cognition proposes that the body’s interactions with the environment play a fundamental role in cognitive processing (Barsalou, 2008; Osypiuk et al., 2018). This theory takes a bottom-up approach whereby cognition and emotion are rooted in sensory perceptions and sensory-motor input from specific environments and situations (Borghi and Pecher, 2011; Hauke and Kritikos, 2016; Pietrzak et al., 2018). Consequently, knowledge becomes stored in neural patterns or “simulations” which link bodily states and the original experience with the environment, objects, or people (Barsalou, 1999; Borghi and Pecher, 2011). Therefore, when the same or similar situations to the original (namely, simulations) are present, the feedback loops established from these interactions are activated and influence mood states (Barsalou, 1999; Borghi and Pecher, 2011; Pietrzak et al., 2018).
For veterans suffering from PTSD, these simulations are conditions characterised by intrusive, distressing memories and flashbacks of a traumatic event (American Psychiatric Association [APA], 2013). Psychological and physiological distress is thus triggered by the exposure to internal or external simulations of the traumatic event (APA, 2013), which often leads to persistent avoidant behaviours, negative cognitions, and increasing depressive symptoms (APA, 2013; Felleman et al., 2016). These symptoms may lead to emotional dysregulation in everyday life. Emotional dysregulation is often accompanied by physiological reactions akin to a stress reaction, and the ability to accurately detect and evaluate these embodied signals are fundamental to emotional regulation. This evaluation is followed by developing appropriate regulation strategies that can mitigate and modify the emotional reactions to the stressful event (Price and Hooven, 2018). Interoceptive awareness, which refers to the awareness of bodily signals (Füstös et al., 2013), is essential for emotion regulation. Developing interoceptive skills through mindfulness meditation may aid in reducing PTSD and depressive symptoms by addressing maladaptive coping mechanisms such as thought suppression and emotional numbing (Felleman et al., 2016; Hauke and Kritikos, 2016).
Although research has suggested that MBSR is efficacious for improving veteran mental health, reviews that provide a clear and comprehensive overview of available literature in this field are limited. The search in Cochrane, PROSPERO and eight databases (CINAHL, Emcare, MEDLINE, PsychInfo, PTSDPubs, PubMed, ProQuest Military Database, and SCOPUS) located one systematic review and meta-analysis of the effectiveness of mindfulness-based interventions (MBIs) on military veterans (Goldberg et al., 2020). Goldberg et al.’s (2020) study found that MBIs have a large effect on depression and a medium effect on PTSD at post-treatment. However, there are several limitations in Goldberg et al.’s study. Firstly, the study amalgamated MBSR and Mindfulness Based Cognitive Therapy (MBCT) interventions in the analysis and interpretation, which may obscure the distinct impact of each intervention. Despite the similarities shared by MBSR and MBCT, they represent distinct interventions with distinct foci (Fisher et al., 2023). When multiple MBIs are included in a single systematic review and meta-analysis, the effectiveness of each individual MBI may be masked (Ni et al., 2020). Therefore, evaluating MBSR and MBCT separately is crucial to discern the individual efficacy. Secondly, the employed data analysis methods of Goldberg et al. may have introduced methodological challenges. In Goldberg et al.’s study, the between-group effect was computed by subtracting the within-group effect for the control conditions and comparing that of the MBI conditions. The authors state that this analytic method took account of the potential between-group differences at baseline. However, as argued by Twisk et al. (2018), the between-group differences at baseline can be statistically adjusted, with recommendation to compare the mean scores at post-/follow-up timepoints between intervention and control groups while adjusting for baseline values. Moreover, as pointed out by Bland and Altman (2011), the analytic method of using separate paired tests against baseline and interpreting only one being significant (e.g., the intervention group) as indicating a difference between the intervention and control groups could be “conceptually wrong, statistically invalid, and consequently highly misleading” (p. 6; see Bland and Altman (2011) for more details). Bland and Altman advised that between-group difference should be performed by comparing the differences between the intervention and control groups directly after adjusting the baseline values. Lastly, Goldberg et al.’s study did not investigate the differences between MBIs and other established therapies such as cognitive behavioural therapy (CBT). Evaluating MBIs in relation to alternative therapies is essential for comprehensively understanding their efficacy and positioning in the spectrum of available treatment options. In conclusion, while Goldberg et al.'s (2020) study demonstrated promising results regarding the efficacy of MBIs on depression and PTSD among military veterans, careful consideration of the aforementioned limitations is essential for a nuanced interpretation of the findings and guiding future research in this domain.
The current study aims to address the research gaps in Goldberg et al.’s study by: 1) focusing on the effectiveness of MBSR on depression, PTSD, and mindfulness among military veterans; 2) directly comparing the differences between the treatment and control groups at post-intervention and follow-up timepoints with an adjustment of the baseline values; and 3) comparing the effectiveness of MBSR against other therapies if available. We will also analyse the within-group changes in the single-arm trials and MBSR intervention groups in the RCTs by comparing post-intervention and follow-up against baseline. Although within-group comparison has its limitations and is not generally used as confirmation of the efficacy of an intervention (Evans, 2010), it provides valuable information on how outcomes change in the same group of people after receiving the intervention (MBSR in this case). The following research questions (RQs) are proposed:
RQ1: Are there significant within-group changes in depression, PTSD, and mindfulness, comparing both post-intervention and follow-up against pre-intervention?
RQ2: Are there significant between-group differences in depression, PTSD, and mindfulness between the MBSR intervention and the control groups at post-intervention and follow-up?
RQ3: Are there significant between-group differences in depression and PTSD between MBSR and other therapies at post-intervention and follow-up?
Method
Guidelines by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were followed in the current systematic review and meta-analysis. The current systematic review was registered in PROSPERO (Registration number: CRD42022314834).
Inclusion and exclusion criteria
Inclusion criteria included clinical trial studies (including single-arm uncontrolled trials and RCTs) published in peer-reviewed journals and registered trials focusing on PTSD and depression in veterans, and mindfulness-based stress reduction (MBSR). The most common mental health conditions veterans may encounter (e.g., anxiety, alcohol/drug misuse and dependence, suicide) were also included because these mental health conditions are often comorbid with PTSD and depression. Exclusion criteria for primary screening included articles without the search terms in the title or abstract, not peer-reviewed, not published in English, review papers, book chapters, thesis submissions, case studies, editorials and letters to the editor, and articles without full-text.
Search strategy
JN conducted the data search in nine electronic databases between 18th July and 6th August 2021 (CINAHL, Emcare, MEDLINE, PsychInfo, PTSDPubs, PubMed, ProQuest Military Database, Cochrane register, and SCOPUS), for articles published from inception to August 2021. WL repeated the search to confirm the accuracy of the search. The search protocol was performed again on the 20th of December 2022, 7th of October 2023, and 6th of October 2024 to include new articles published since the original search, resulting in additional 281 titles and abstracts for screening and two new articles published in 2022 were included in the full-text methodological quality assessment. Table 1 presents the search strategy in the format of the Cochrane’s PICO search tool (Higgins et al., 2022).
Table 1.
PICO search strategy.
| PICO | Search strategy |
|---|---|
| Participation | MeSH term search: veterans, veterans health, veterans health services, hospitals veterans |
| Keyword search: former military personnel, former service men, former service women | |
| Intervention | MeSH term search: mindfulness, mindfulness-based stress reduction, MBSR, mindfulness-based interventions, meditation, relaxation therapy |
| Comparison | N/A |
| Outcome | MeSH term search: Mental Health, mental disorders, quality of life |
| Keyword search: mental health OR quality of life OR mental illness OR mental disorder* OR mental ill health OR suicid* OR substance abuse OR alcohol* OR drug* OR psychos?s OR depress* OR anxiet* OR nervous* OR social anxiet* OR emotional regulat* OR psychological distress OR emotional distress OR trauma OR post-trauma OR PTSD OR affective disorder* OR mood disorder* |
Study selection
Eligible studies were examined by the title and abstract screening, followed by the full-text methodological quality evaluation. The first two authors independently evaluated titles and abstracts of the retrieved articles coded ‘yes’, ‘no’, or maybe’ on blinded excel spreadsheets to determine eligibility (Astridge et al., 2023; Fisher et al., 2023; Li et al., 2024b). The studies marked as a unanimous ‘yes’ were included for further full-text methodological quality assessment. The studies marked unanimously with ‘no’ were excluded. The studies assessed as ‘maybe’ or those in disagreement, were discussed to reach an agreement to include or exclude from the current review (Fisher et al., 2023; Li et al., 2021b).
The full-text methodological quality assessment was performed by all three authors independently to assess the quality of the included studies, using the Mixed Methods Appraisal Tool (MMAT) Version 2018 (Hong et al., 2019). Quality of the studies were determined using the inter-rater agreement measure of Fleiss’ kappa (k): k < 0.20, 0.40, 0.60 and 0.80 suggesting poor, fair, moderate, substantial, and perfect agreements, respectively (Fleiss, 1971). Articles with k lower than 0.40 were discussed to reach an agreement for inclusion or exclusion in the review (Astridge et al., 2023; Fisher et al., 2023; Leow et al., 2024). All included articles had ks above 0.40.
Data extraction
A standard form was used to extract data, which included first author, publishing year, citation, country of the study, sample size, analytic methods, sample population demographics, measures of outcomes and findings (Fisher et al., 2023; Li et al., 2021b). The authors assessed the extracted data by coding the evidence for findings in each article as ‘unequivocal’, ‘credible’ or ‘unsupported’. An evaluation agreement index = ((Nunequivocal + Ncredible)/Nreviewers) for every article was estimated (Astridge et al., 2023; Fisher et al., 2023; Wigg et al., 2024). After the post-rating discussion amongst the authors, all included articles had an agreement index of 1, reaching unanimous agreements.
Data synthesis
Data synthesis was conducted employing a meta-analysis using the Comprehensive Meta-Analysis (CMA) V3 software (Borenstein et al., 2013). All included studies reported data on several outcome variables, which were based on the same participants. Therefore, the multiple outcomes model was employed to compute the effect sizes of the outcomes, which took correlations between different outcomes in the same study into account (Borenstein et al., 2021). The pooled effect size of an outcome across included studies was estimated using the random effects model.
The within-group comparisons included data of the single-arm uncontrolled trials and the intervention group in RCTs. The mean within-group differences were computed by the means at post-intervention/follow-up deducting the baseline means. For between-group effect analysis, the group differences were computed using the mean scores of an outcome variable at post-intervention and follow-up of the MBSR intervention groups deducting those of the control group after adjusting the baseline values (Fisher et al., 2023).
For studies reporting multiple estimates of effect sizes for an outcome (e.g., multiple effect sizes of subscales for PTSD/mindfulness in the same study), the overall effect size was used in the main meta-analysis to estimate the overall effect size across studies. A two-level meta-analysis was conducted when the overall effect size was not available (Astridge et al., 2023; Fisher et al., 2023; Freedman et al., 2024). Firstly, using the fixed effect model, the multiple effect sizes within each study for an outcome was computed to yield a pooled effect size for the outcome within the study. Secondly, using the random effects model, the pooled effect size obtained from the first step was entered to the main meta-analysis (Hedges, 2019).
Hedges’ g was used to report the effect size that was identified as being small, medium, or large as per g = 0.20, 0.50, and 0.80, respectively (Cohen, 1988). A default correlation of r = 0.50 was used for within-group effects for studies that did not report correlations of the outcome variable between pre-intervention and post-intervention/follow-up (Fisher et al., 2023; White et al., 2019). For the study reporting the standard error (SE) of a mean (Arefnasab et al., 2016), the standard deviation (SD) was obtained from the SE by multiplying by the square root of the sample size (SD = SE × √N; Higgins and Green, 2011).
Heterogeneity was evaluated with I2 statistics where low, moderate, and high heterogeneity being represented by I2 = 25, 50, and 75 and over (Borenstein et al., 2019). To investigate publication bias, Egger’s regression test was conducted. Publication bias was identified when p values were significant (Borenstein et al., 2019).
Assessing risk of bias in included studies
An assessment of the risk of bias for each included study was conducted employing the Prediction Model Study Risk of Bias Assessment Tool (PROBAST; Wolff et al., 2019). The overall risks of biases for all included articles were rated as low by the first two authors. Publication bias test was also performed to evaluate if studies with nonsignificant results were withheld from publication.
Results
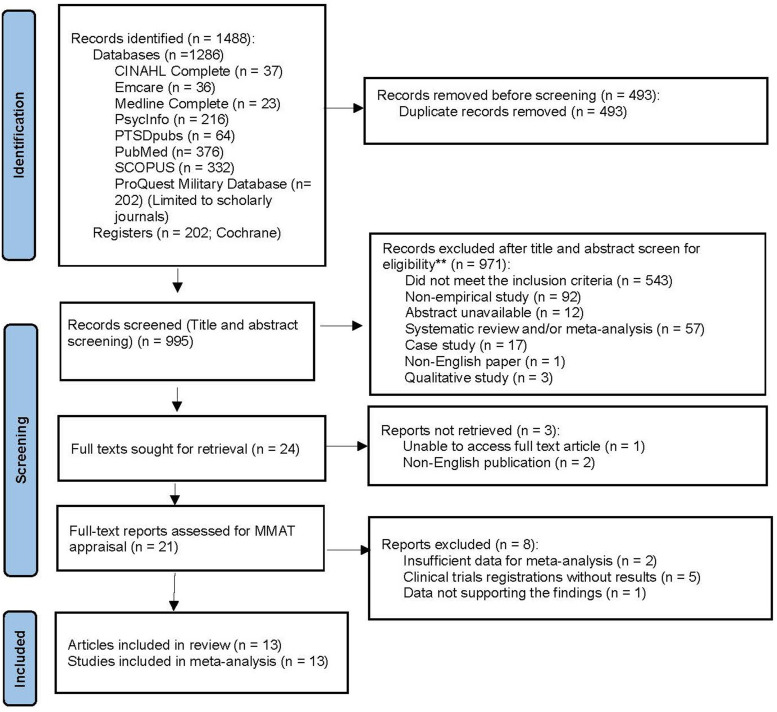
The PRISMA diagram in Figure 1 shows studies that were included and excluded in the current study. After removing the duplicates, 995 titles were identified in the literature search. Title and abstract screening excluded 971 titles; 24 studies were sought for retrieval for full text screening. The full texts of eight studies were not available. Emails were sent to the corresponding authors of the eight studies to request the full text. Seven full texts were received, including two non-English articles and five clinical trial registrations. The author of one paper did not respond to our request. As a result, three studies were excluded (including the two non-English articles and one full-text unavailable), which left 21 studies for full text analysis. Among the 21 studies, five clinical trial registrations without results were excluded. Two studies did not provide sufficient data for meta-analysis. The authors of these two studies were contacted requesting missing data for meta-analysis, but there was no response. These two studies were thus removed. One study (Saban et al., 2022) was excluded for the following reasons: the authors claimed no significant group differences at baseline in PTSD and depression between MBSR and control groups, however the current research team found significant differences (PTSD: p = 0.048, depression: p = 0.042). Additionally, the authors claimed participants in the MBSR group reported lowered perceived stress, loneliness, and symptoms of PTSD compared to those in the actively control group, however, the data presented contradicted this. The final number of the included study was 13.
Figure 1.
PRISMA flow chart of results of systematic review and meta-analysis.
Characteristics of included studies
Of the 13 studies included in this meta-analysis, the majority were conducted in the USA (n = 11), followed by Iran (n = 2) with a total of 1131 participants. Eight studies were randomised controlled trials (RCTs) and five were single-arm uncontrolled trials. Participants were predominantly male (80.9%) with an average age of 50.2 years. Most studies (n = 11) followed the standardised MBSR protocol (e.g., 2.5 h per week for 8 weeks) with (n = 7) or without (n = 4) the full-day retreat, while two studies shortened MBSR. Summaries of characteristics and findings of the included studies are presented in Table 2 and Table S1, respectively.
Table 2.
Characteristics of included studies.
| First author | Country | Research design | Demographic information | Psychiatric history | Scales | MBSR protocol |
|---|---|---|---|---|---|---|
| Arch et al. (2013) | USA | Randomised controlled trial (RCT) MBSR vs cognitive behavioural therapy (CBT) with 3 timepoints: Pre- and post-intervention, and 3-month follow up |
N = 105 Age: M = 45.9 (SD = 13.68) Sex: 83% male, 17% female |
Panic disorder: 30.39% Generalised anxiety disorder (GAD): 37.25% Seasonal affective disorder (SAD): 15.69% PTSD: 14.71% Obsessive-compulsive disorder (OCD): 4.90% |
Beck Depression Inventory (BDI) | 10 weekly × 1.5 h modified MBSR sessions with the full-day retreat |
| Arefnasab et al. (2016) | Iran | RCT MBSR vs Waiting list with 2 timepoints: Pre- and post-intervention |
N = 40 Age: M = 50.2 (SD = 5.25) Sex: 100% male |
Mental health conditions unreported | General Health Questionnaire (GHQ) | 8 weekly × 2.5 h MBSR sessions without the full-day retreat |
| Bremner et al. (2017) | USA | RCT MBSR vs present-centred group therapy (PCGT) with 3 timepoints: Pre- and post-intervention, and 6-month follow up |
N = 26 Age: M = 34.0 (SD = 7) Sex: 100% male |
Combat-related PTSD | Clinician-administered PTSD Scale (CAPS); Five Facet Mindfulness Questionnaire (FFMQ) | 8 weekly × 2.5 h MBSR sessions without the full-day retreat |
| Davis et al. (2019) | USA | RCT MBSR vs PCGT with 5 timepoints: Pre-, during- (week 3 and week 6) and post-intervention, and 7-week follow up |
N = 214 Age: M = 51.7 (SD = 10.9) Sex: 80% male, 20% female |
PTSD | CAPS; Patient Health Questionnaire-9 (PHQ-9); FFMQ | 8 weekly × 1.5 h modified MBSR sessions with the full-day retreat |
| Felleman et al. (2016) | USA | Single-arm uncontrol trial (SAUT) with 3 timepoints: Pre- and post-intervention, and 4-month follow up |
N = 116 Age: M = 52.3 (SD = 11.46) Sex: 88% male, 12% female |
PTSD | PTSD Checklist Civilian Version (PCL-C); PHQ-9 | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
| Harding et al. (2018) | USA | SAUT with 3 timepoints: Pre- and post-intervention, and 4-month follow up |
N = 55 Age: M = 52.6 (SD = 11.68) Sex: 85.5% male, 14.5% female |
PTSD with comorbid IBS | PCL-C; PHQ-9; FFMQ | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
| Kearney et al. (2012) | USA | SAUT with 3 timepoints: Pre- and post-intervention, and 4-month follow up |
N = 92 Age: M = 51.0 (SD = 10.6) Sex: 76% male, 24% female |
Depression: 58.7% Bipolar disorders: 7.6% General anxiety: 17.4% PTSD: 34.8% |
PCL-C; PHQ-9; FFMQ | 8 weekly × 2.5h MBSR sessions with the full-day retreat |
| Kearney et al. (2013) | USA | RCT MBSR vs treatment as usual (TAU) with 3 timepoints: Pre- and post-intervention, and 4-month follow up |
N = 47 Age: M = 52.0 (SD = 13.4) Sex: 78% male, 22% female |
PTSD | PCL-C; PHQ-9 | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
| Kearney et al. (2016) | USA | RCT MBSR vs treatment as usual (TAU) with 3 timepoints: Pre and post-intervention, and 6-month follow up |
N = 55 Age: M = 51.3 (SD = 6.8) Sex: 85.5% male, 14.5% female |
Depression: 50% Anxiety: 19.2% PTSD: 29.8% |
PCL-C; PHQ-9; FFMQ | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
| Kluepfel et al. (2013) | USA | SAUT with 2 timepoints: Pre- and post-intervention |
N = 30 Age: M = 60.0 (SD = 11.45) Sex: 84% male, 16% female |
PTSD: 82.1% Depression: 39.2% Bipolar disorder: 10.7% Personality Disorder: 14.2% Other anxiety disorder: 10.7% |
BDI; Mindfulness Attention Awareness Scale (MAAS) | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
| Omidi et al. (2013) | Iran | RCT MBSR vs TAU with 2 timepoints: Pre and post-intervention |
N = 62 Age: M = 35.5 (SD unreported) Sex: 100% male |
PTSD | Inventory of Mood States (IMS) | 8 weekly × 2.5 h MBSR sessions without the full-day retreat |
| Serpa et al. (2014) | USA | SAUT with 2 timepoints: Pre- and post-intervention |
N = 79 Age: M = 60.0 (SD = 7) Sex: 89% male, 11% female |
Mental health conditions unreported | PHQ-9; FFMQ | 8 weekly × 2.5 h MBSR sessions without the full-day retreat |
| Shapira et al. (2022) | USA | RCT MBSR vs PCTG with 3 timepoints: pre-, post- and 4-month follow up |
N = 210 Age: M = 55.0 (SD = 12) Sex: 84% male, 16% female |
PTSD | PHQ-9, FFMQ | 8 weekly × 2.5 h MBSR sessions with the full-day retreat |
Test of RQ1
Within-group effects comparing post-intervention against pre-intervention
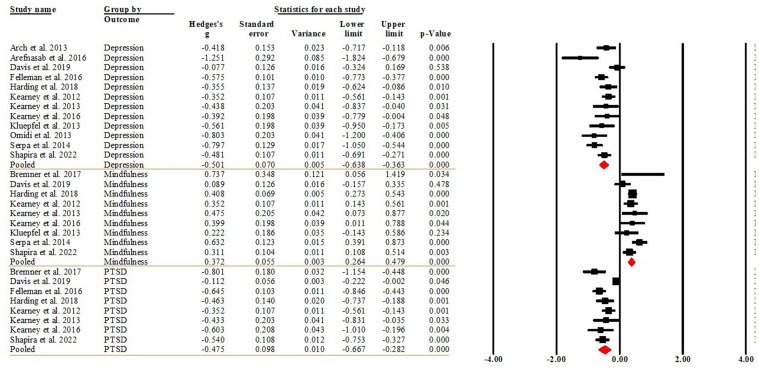
Of the 13 studies, 12 reported within-group differences in depression (Arch et al., 2013; Arefnasab et al., 2016; Davis et al., 2019; Felleman et al., 2016; Harding et al., 2018; Kearney et al., 2012, 2013, 2016; Kluepfel et al., 2013; Omidi et al., 2013; Serpa et al., 2014; Shapira et al., 2022), 8 reported within group differences for PTSD comparing the post-intervention against the baseline (pre-intervention) (Bremner et al., 2017; Davis et al., 2019; Felleman et al., 2016; Harding et al., 2018; Kearney et al., 2012, 2013, 2016; Shapira et al., 2022), and 9 reported within-group differences for mindfulness (Bremner et al., 2017; Davis et al., 2019; Harding et al., 2018; Kearney et al., 2012, 2013, 2016; Kluepfel et al., 2013; Serpa et al., 2014; Shapira et al., 2022). The pooled effect sizes indicated that MBSR had medium effect sizes on depression (Hedge’s g = −0.501, 95%CI [−0.638, −0.363], p < 0.001) and PTSD (Hedge’s g = −0.475, 95%CI [−0.667, −0.282], p < 0.001), and a small effect size on mindfulness (Hedge’s g = 0.372, 95%CI [0.264, 0.479], p < 0.001).That said, MBSR significantly reduced depression and PTSD by about 0.501 and 0.474 standard deviations (SDs), respectively; and significantly increased mindfulness by 0.372 SDs. Figure 2 displays the forest plot of the analysis. The I2 = 62.815 (p = 0.002) for depression and I2 = 81.525 (p < 0.001) for PTSD indicated that heterogeneity was moderate and substantial, respectively. The I2 = 34.577 (p = 0.141) for mindfulness indicated that heterogeneity was low. The Egger’s regression test (intercept = −2.227, t = 1.357, df = 27; p = 0.186) suggested publication bias was not detected.
Figure 2.
Forest plot of the within-group effects comparing post-intervention against pre-intervention.
Meta-regression was performed to determine which factors contributed to the heterogeneity. The moderators of sample size (Q = 0.22, df = 1, p = 0.619), publishing year (Q = 0.30, df = 1, p = 0.586) and MBSR protocol (Q = 0.98, df = 2, p = 0.613) were not accountable for the substantial heterogeneity. The moderators of measure (Q = 93.38, df = 8, p < 0.001) and country (Q = 5.84, df = 1, p = 0.016), were found to be responsible for the heterogeneity.
Within-group effects comparing follow-up against pre-intervention
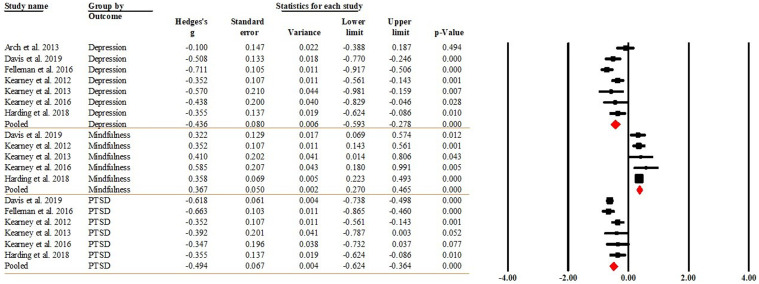
Seven studies reported within-group differences in depression (Arch et al., 2013; Davis et al., 2019; Felleman et al., 2016; Harding et al., 2018; Kearney et al., 2012, 2013, 2016), six reported within-group differences for PTSD (Davis et al., 2019; Felleman et al., 2016; Harding et al., 2018; Kearney et al., 2012, 2013, 2016), and five reported within-group differences for mindfulness (Davis et al., 2019; Harding et al., 2018; Kearney et al., 2012, 2013, 2016) at follow-up against the pre-intervention timepoints. The pooled effect sizes indicated that MBSR had small effect sizes on depression (Hedge’s g = −0.436, 95%CI [−0.593, −0.278], p < 0.001), PTSD (Hedge’s g = −0.494, 95%CI [−0.624, −0.364], p < 0.001), and mindfulness (Hedge’s g = 0.367, 95% CI [0.270, 0.465], p < 0.001). That is, MBSR significantly reduced depression and PTSD by about 0.436 and 0.494 SDs, respectively; and increased mindfulness by 0.367 SDs. Figure 3 displays the forest plot of the analysis. The I2 = 56.338 (p = 0.033) for depression, I2 = 47.246 (p = 0.091) for PTSD, and I2 = zero (p = 0.858) for mindfulness indicated that heterogeneity was moderate, low and trivial, respectively. The Egger’s regression test (intercept = 0.801, t = 0.325, df = 16, p = 0.749) suggested publication bias was not detected.
Figure 3.
Forest plot of the within-group effects comparing follow-up against pre-intervention.
Meta-regression was performed to determine which factors contributed to the heterogeneity. The moderators of sample size (Q = 0.53, df = 1, p = 0.468), publishing year (Q = 0.11, df = 1, p = 0.744) and MBSR protocol (Q = 0.01, df = 1, p = 0.914) were not predictors for the heterogeneity. The moderator of measure (Q = 16.42, df = 5, p = 0.006) was accountable for the significant heterogeneity.
Sensitivity analysis
Two sensitivity analyses were performed to examine whether the results were robust to the decisions made in the process of including the modified MBSR in the meta-analysis. Two studies utilising modified MBSR (Arch et al., 2013; Davis et al., 2019) in the within-group analysis (comparing post-intervention and follow-up against pre-intervention) were removed. The results showed that the significance and direction of the effects on all outcomes did not change (Tables S2 and S3).
Test of RQ2
Effects between MBSR and control groups at post-intervention
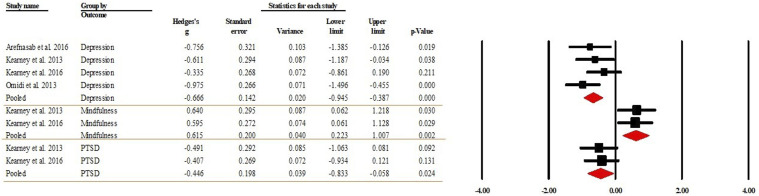
Of the 13 included studies, four, two and two studies reported between-group differences between the MBSR and control (TAU or waiting list [WL]) groups at the post-intervention timepoint in depression (Arefnasab et al., 2016; Kearney et al., 2013, 2016; Omidi et al., 2013), PTSD (2019; Kearney et al., 2013; Kearney et al., 2016), and mindfulness (Kearney et al., 2013, 2016), respectively. The pooled effect sizes indicated that MBSR had medium effect sizes on depression (Hedge’s g = −0.666, 95% CI [−0.945, −0.387], p < 0.001), PTSD (Hedge’s g = −0.446, 95% CI [−0.833, −0.058], p = 0.024), and mindfulness (Hedge’s g = 0.615, 95% CI [0.223, 1.007], p = 0.002). That said, depression and PTSD significantly decreased by 0.446 and 0.615 SDs, respectively, in the MBSR compared to control/TAU groups; and mindfulness significantly increased by 0.615 SDs in the MBSR group. Figure 4 presents the forest plot of the analysis. The I2 was zero for all three outcomes with p = 0.393 for depression, p = 0.911 for PTSD and p = 0.831 for mindfulness, indicating that heterogeneity was trivial. Meta-regression thus was not performed for moderator analysis. The Egger’s regression test (intercept = −1.228, t = 0.093, df = 6; p = 0.929) suggested publication bias was not detected.
Figure 4.
Forest plot of the effects between MBSR and control groups at post-intervention.
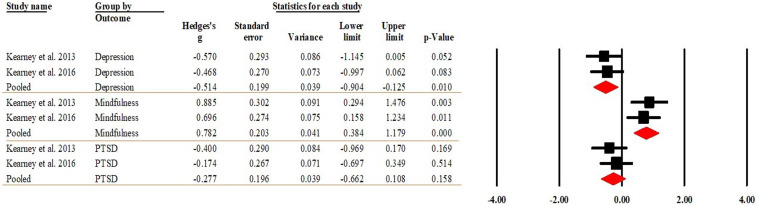
Effects between MBSR and control groups at follow-up
Two studies each (Kearney et al., 2013, 2016) reported the differences between the MBSR and control (TAU and WL) groups at follow-up in depression and PTSD. Two studies (Kearney et al., 2013, 2016) reported mindfulness. The pooled effect sizes indicated that MBSR had a medium effect size on depression (Hedge’s g = −0.514, 95% CI [−0.904, −0.125], p = 0.010) and mindfulness (Hedge’s g = 0.782, 95% CI [0.384, 1.179], p < 0.001). The pooled effect size showed that MBSR had no effect on PTSD (Hedge’s g = −0.277, 95% CI [−0.662, 0.108], p = 0.158). That said, depression significantly decreased by 0.514 SDs in the MBSR compared to control/TAU groups; and mindfulness significantly increased by 0.782 SDs in the MBSR group. Figure 5 displays the forest plot of the analysis. The heterogeneity indicator I2 was zero for all three outcomes, with p being 0.798 for depression, 0.568 for PTSD and 0.642 for mindfulness, suggesting that heterogeneity was trivial. The Egger’s regression test (intercept = 9.500, t = 0.444, df = 4, p = 0.680) suggested publication bias was not detected. Due to the small number of studies, sensitivity analysis was not performed.
Figure 5.
Forest plot of the effects between MBSR and control groups at follow-up.
Test of RQ3
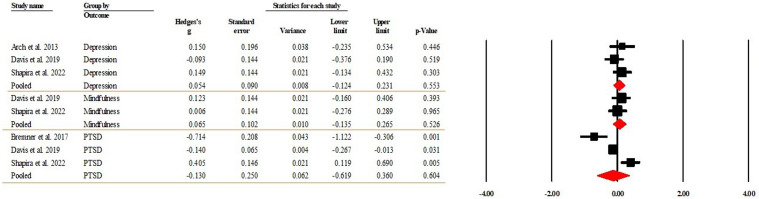
Effects between MBSR and other therapies at post-intervention
Among the included studies, there was one RCT compared MBSR with CBT (Arch et al., 2013) and three compared MBSR to present-centred group therapy (PCGT) (Bremner et al., 2017; Davis et al., 2019; Shapira et al., 2022). Three studies each reported the between-group differences at the post-intervention timepoint in depression (Arch et al., 2013; Davis et al., 2019) and PTSD (Bremner et al., 2017; Davis et al., 2019). Two studies reported mindfulness (Davis et al., 2019; Shapira et al., 2022). The pooled effect sizes indicated that depression (Hedge’s g = 0.054, 95% CI [−0.124, 0.231], p = 0.553), PTSD (Hedge’s g = −0.130, 95% CI [−0.619, 0.360], p = 0.604), and mindfulness (Hedge’s g = 0.065, 95% CI [−0.135, 0.265], p = 0.526) were at similar levels between the MBSR and CBT/PCGT groups. Figure 6 present the forest plot of the analysis. The I2 = zero for both depression (p = 0.426) and mindfulness (p = 0.566) indicated that heterogeneity was trivial. The I2 = 90.521 (p < 0.001) for PTSD indicated that heterogeneity was high. Due to the low number of studies included in the analysis, mete-regression for moderator analysis was not performed. The Egger’s regression test (intercept = 1.081, t = 0.573 df = 6; p = 0.587) suggested publication bias was not detected.
Figure 6.
Forest plot of the effects between MBSR and CBT/PCGT groups at post-intervention.
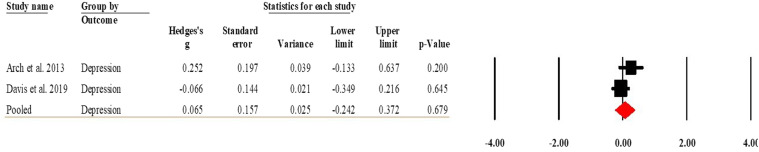
Effects between MBSR and CBT/PCGT groups at follow-up
One study reported the differences at the follow-up timepoint in depression comparing MBSR to CBT (Arch et al., 2013) and one compared MBSR to PCGT (Davis et al., 2019). The pooled effect sizes indicated that the levels of depression were similar in the MBSR and CBT/PCGT groups (Hedge’s g = 0.065, 95% CI [−0.242, 0.372], p = 0.679). Figure 7 present the forest plot of the analysis. The I2 = 41.427 (p = 0.191) for depression indicated that heterogeneity was low. Due to the low number of studies included in the analysis, publication bias and sensitivity analyses were not performed.
Figure 7.
Forest plot of the effects between MBSR and CBT/PCGT groups at follow-up.
Discussion
To the authors’ knowledge, this is the first systematic review and meta-analysis to identify the effectiveness of MBSR in reducing depression and PTSD symptoms and improving mindfulness in military veterans. A total of 13 studies with 1131 participants were included in the systematic review and meta-analysis.
Our findings from both within- and between-group comparisons suggest that MBSR demonstrated small to medium effects in reducing depressive and PTSD symptoms and improving mindfulness in veterans at post-intervention. These effects endured and remained consistent in the within-group comparison at follow-up (Range: 2-6 months; Mean = 3.8 months). However, when comparing MBSR to control groups at follow-up, the effects on depression and mindfulness persisted, but not on PTSD. Our findings are consistent with the findings in Goldberg et al.’s (2020) systematic review on the efficacy of MBIs for military veterans, which also found that MBIs are superior to the control group on measures of depression and PTSD at post-treatment. The authors additionally found that at follow-up (mean length = 3.19 months), MBIs continued to outperform the control group on reducing depression, but not PTSD.
Informed by the embodied cognition framework, the body-mind relationship paradigm suggests that the signals from the body concerning both internal and external stressors encountered during military service and in their everyday life can significantly impact cognitions, motivation, and mood states (Hauke and Kritikos, 2016; Osypiuk et al., 2018). This influence may contribute to the manifestation of symptoms associated with depression and PTSD. Through MBSR practice, which increases mindfulness and encourages participants to acknowledge challenging and complicated body and mind relationships without judgement and avoidance, veterans may be able to adopt a holistic approach. This approach assists them to develop strategies to regulate emotional and behavioural responses to the stressors (Schure et al., 2018). Consequently, with the increased levels of mindfulness veterans may obtain a better sense of control in stressful situations which may result in reduced physiological reactivity and symptoms of PTSD and depression (Chiesa et al., 2014; Priya and Kalra, 2018; Schure et al., 2018).
Several factors may contribute to the insignificant result in PTSD comparing MBSR and control groups at follow-up. Firstly, only two studies were included in the meta-analysis. Such a small volume of data may decrease statistical power to detect effect sizes. Secondly, the complexity of PTSD in veterans may contribute to the insignificant treatment gain at follow-up. This finding indicates that MBSR alone may not be a viable replacement for the recommended trauma-focused therapies for treating veteran PTSD (e.g., prolonged exposure therapy, cognitive processing therapy, and trauma-focused cognitive behavioural therapy). Instead, MBSR may serve as an important foundation treatment that enhances patients’ motivation, willingness, and ability to engage with the full-length trauma-focused treatments for better treatment outcomes (Possemato et al., 2016). MBSR as a stress reduction adjunct may reduce dropout and enhance ongoing engagement for veterans to complete trauma-focused therapies.
Our comparison between MBSR and CBT/PCGT indicates that there were no significant differences between MBSR and CBT/PCGT with regards to the outcomes of depression, PTSD and mindfulness, meaning that MBSR is as effective as CBT and PCGT. This finding is consistent with findings in recent reviews that compare the efficacy between MBSR and CBT in chronic pain (Khoo et al., 2019) and mental health outcomes of anxiety, depression and sleep quality (Li et al., 2021a). These two reviews found no significant differences between MBSR and CBT in terms of the treatment outcomes of chronic pain, anxiety, depression, and sleep quality. Our findings indicate that MBSR could be used as an alternative psychotherapy to CBT/PCGT for reducing veteran depressive and PTSD symptoms.
The findings of the sensitivity analysis indicate that removing studies using shortened MBSR did not alter the significance or direction of the effects on the outcomes. This finding is consistent with the finding in a recent meta-analysis that found that the efficacy of MBSR in diabetes patients was not moderated by the MBSR protocols (e.g., eight-week MBSR with/without full-day retreat and shortened MBSR) (Fisher et al., 2023). Future RCTs are warranted to evaluate the effect of low-dose MBSR on the mental health of veterans.
Results from the heterogeneity analyses indicate the heterogeneities in depression and PTSD in the pre-post within-group comparisons; and in PTSD between the MBSR and CBT/PCGT groups at post intervention were substantial. The meta-regression analyses show that scales and countries, where the studies were conducted, contributed to the heterogeneities. The high levels of heterogeneity suggest the effects of MBSR on the outcome variables are low in some veteran populations and high in others (Borenstein, 2019). Therefore, generalising results from the current study will be taken with caution.
There are several limitations worth noting within the current study. First, the limited number of RCTs (Arch et al., 2013; Arefnasab et al., 2013; Bremner et al., 2017; Davis et al., 2019; Felleman et al., 2016; Kearney et al., 2013, 2016; Omidi et al., 2013) in the meta-analysis is likely to reduce the statistical power for detecting differences between the MBSR and control groups. Second, the underrepresentation of females in the included studies (Arch et al., 2013; Arefnasab et al., 2013, 2016; Harding et al., 2018; Kearney et al., 2013, 2016) hinders a comprehensive understanding of MBSR’s effects in diverse populations. This is consistent with a previous review of MBIs with veteran populations where participants were 85% male across all studies (Marchand et al., 2021). Third, the geographical representation being restricted to the USA and Iran, limits the generalisability of the findings to all veteran populations.
Despite the limitations, the current study offers important clinical implications. The positive impact of MBSR on veterans’ mental health can enhance their engagement with other treatments, especially trauma-focussed ones. Treatment avoidance and attrition are well documented challenges within veteran populations, both through a treatment lens (Sciarrino et al., 2022; Steenkamp et al., 2020) and through the lens of PTSD psychopathology (APA, 2013). Mindfulness practice as a mild form of exposure therapy (Baer, 2003; Felleman et al., 2016; Kearney et al., 2012) opens veterans to confronting uncomfortable experiences (emotional, environmental, social) through increased acceptance, non-judgement, and heightened awareness of the present moment (Felleman et al., 2016; Hauke and Kritikos, 2016; Kabat-Zinn, 2003, 2013; Omidi et al., 2013; Schure et al., 2018). Consequently, the automatisation of avoidance behaviours triggered by trauma-based treatments could potentially be mitigated through the development of a ‘mindful mind’ (Kabat-Zinn, 2005). This mental state may provide new neural simulations (Barsalou, 1999; Borghi and Pecher, 2011) that support the cognitive system to interpret the treatment situations as safe (Balcetis and Cole, 2009; Tuerk et al., 2011).
Conclusion
Findings from this review and meta-analysis indicate MBSR is moderately effective in reducing depression and PTSD symptoms and improving mindfulness in military veterans. These results suggest that MBSR could be utilised as a non-trauma focused therapy for improving veterans’ mental health.
Supplemental Material
Supplemental Material for The effectiveness of mindfulness-based stress reduction (MBSR) on depression, PTSD, and mindfulness among military veterans: A systematic review and meta-analysis by Wendy Wen Li, Jaime Nannestad, Timothy Leow and Carolyn Heward in Health Psychology Open.
Author contributions: W.L. substantially contributed to study design, data collection and analysis, data interpretation, data-reanalysis for the revision and the writing of the manuscript. J.N. contributed to study design, data collection and analysis, data interpretation and the writing of the manuscript. T.L. and C.H. contributed to data analysis and critical review of the manuscript. All authors have reviewed and agreed to their individual contribution(s) before submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study received funding from the Tropical Australian Academic Health Centre (TAAHC; Reference number: MF0000821).
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Wendy Wen Li https://orcid.org/0000-0002-0056-6130
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Washington: American Psychiatric Publishing. DOI: 10.1176/appi.books.9780890425596 (accessed 18 February 2023). [DOI] [Google Scholar]
- American Psychiatric Association (2023) What is posttraumatic stress disorder (PTSD)? Available at: https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd (accessed 20 October 2023).
- Arch JJ, Ayers CR, Baker A, et al. (2013) Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behaviour Research and Therapy 51(4–5): 185–196. DOI: 10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Arefnasab Z, Ghanei M, Noorbala AA, et al. (2013) Effect of mindfulness-based stress reduction on quality of life (SF-36) and spirometry parameters, in chemically pulmonary injured veterans. Iranian Journal of Public Health 42(9): 1026–1033. [PMC free article] [PubMed] [Google Scholar]
- Arefnasab Z, Babamahmoodi A, Babamahmoodi F, et al. (2016) Mindfulness-based stress reduction (MBSR) and its effects on psychoimmunological factors of chemically pulmonary injured veterans. Iran Journal of Allergy, Asthma, and Immunology 15(6): 476–486. [PubMed] [Google Scholar]
- Astridge B, Li WW, McDermott B, et al. (2023) A systematic review and meta-analysis on adverse childhood experiences: prevalence in youth offenders and their effects on youth recidivism. Child Neglect and Abuse 140: 106055. DOI: 10.1016/j.chiabu.2023.106055. [DOI] [PubMed] [Google Scholar]
- Baer RA. (2003) Mindfulness training as a clinical intervention: a conceptual and empirical review. Clinical Psychology 10(2): 125–143. DOI: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- Balcetis E, Cole S. (2009) Body in mind: the role of embodied cognition in self-regulation. Social and Personality Psychology Compass 3(5): 759–774. DOI: 10.1111/j.1751-9004.2009.00197. [DOI] [Google Scholar]
- Barsalou LW. (1999) Perceptual symbol systems. Behavioral and Brain Sciences 22(4): 577–609. DOI: 10.1017/S0140525X99002149. [DOI] [PubMed] [Google Scholar]
- Barsalou LW. (2008) Grounded cognition. Annual Review of Psychology 59(1): 617–645. DOI: 10.1146/annurev.psych.59.103006.093639. [DOI] [PubMed] [Google Scholar]
- Bishop S. (2002) What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine 64(1): 71–83. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. (2011) Comparisons against baseline within randomised groups are often used and can be highly misleading. Trials 12: 264. DOI: 10.1186/1745-6215-12-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M. (2019) Common mistakes in meta-analysis and how to avoid them. Biostat, Inc. Available at: https://meta-analysis-books.com/pages/cmma/download/excerpt/Heterogeneity.pdf. [Google Scholar]
- Borenstein M, Hedges L, Higgins J, et al. (2013) Comprehensive Meta-Analysis Version 3. Englewood: Biostat. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. (2019) Comprehensive Meta Analysis. Available at: https://www.meta-analysis.com/downloads/Meta-Analysis_Manual_V3.pdf. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. (2021) Introduction to meta-analysis. 2nd ed. Wiley. [Google Scholar]
- Borghi AM, Pecher D. (2011) Introduction to the special topic embodied and grounded cognition. Frontier Psychology 2: 187. DOI: 10.3389/fpsyg.2011.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Mishra S, Campanella C, et al. (2017) A pilot study of the effects of mindfulness-based stress reduction on post-traumatic stress disorder symptoms and brain response to traumatic reminders of combat in Operation Enduring Freedom/Operation Iraqi Freedom combat veterans with post-traumatic stress disorder. Frontiers in Psychiatry 8(157): 1–15. DOI: 10.3389/fpsyt.2017.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A, Anselmi R, Serretti A. (2014) Psychological mechanisms of mindfulness-based interventions: what do we know? Holistic Nursing Practice 28(2): 124–148. DOI: 10.1097/HNP.0000000000000017. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical Power Analysis for the Behavioral Sciences. New York: Routledge. [Google Scholar]
- Creswell JD. (2017) Mindfulness interventions. Annual Review of Psychology 68(1): 491–516. DOI: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Taren AA, Lindsay EK, et al. (2016) Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biological Psychiatry 80(1): 53–61. DOI: 10.1016/j.biopsych.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Davis LL, Whetsell C, Hamner MB, et al. (2019) A multisite randomized controlled trial of mindfulness-based stress reduction in the treatment of posttraumatic stress disorder. Psychiatric Research and Clinical Practice 1(2): 39–48. DOI: 10.1176/appi.prcp.20180002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards-Stewart A, Smolenski DJ, Bush NE, et al. (2021) Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. Journal of Traumatic Stress 34(4): 808–818. DOI: 10.1002/jts.22653. [DOI] [PubMed] [Google Scholar]
- Evans SR. (2010) Clinical trial structures. Journal of Experimental Stroke and Translational Medicine 3(1): 8–18. DOI: 10.6030/1939-067x-3.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felleman BI, Stewart DG, Simpson TL, et al. (2016) Predictors of depression and PTSD treatment response among veterans participating in mindfulness-based stress reduction. Mindfulness 7(4): 886–895. DOI: 10.1007/s12671-016-0527-7. [DOI] [Google Scholar]
- Fisher V, Li WW, Malabu U. (2023) The effectiveness of mindfulness-based stress reduction (MBSR) on the mental health, HbA1C and mindfulness of diabetes patients: a systematic review and meta-analysis of randomised controlled trials. Applied Psychology: Health and Well-being 15: 1733–1749. DOI: 10.1111/aphw.12441. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. (1971) Measuring nominal scale agreement among many raters. Psychological Bulletin 76: 378–382. [Google Scholar]
- Freedman B, Li WW, Liang Z, et al. (2024) The prevalence of incivility in hospitals and the effects of incivility on patient safety culture and outcomes: a systematic review and meta-analysis. Journal of Advanced Nursing, Advance online publication. DOI: 10.1111/jan.16111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Füstös J, Gramann K, Herbert BM, et al. (2013) On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Social Cognitive and Affective Neuroscience 8(8): 911–917. DOI: 10.1093/scan/nss089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Riordan KM, Sun S, et al. (2020) Efficacy and acceptability of mindfulness-based interventions for military veterans: a systematic review and meta-analysis. Journal of Psychosomatic Research 138: 110232. DOI: 10.1016/j.jpsychores.2020.110232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haagen JFG, Smid GE, Knipscheer JW, et al. (2015) The efficacy of recommended treatments for veterans with PTSD: a metaregression analysis. Clinical Psychology Review 40: 184–194. DOI: 10.1016/j.cpr.2015.06.008. [DOI] [PubMed] [Google Scholar]
- Harding K, Simpson T, Kearney D. (2018) Reduced symptoms of post-traumatic stress disorder and irritable bowel syndrome following mindfulness-based stress reduction among veterans. The Journal of Alternative and Complementary Medicine 24(12): 1159–1165. DOI: 10.1089/acm.2018.0135. [DOI] [PubMed] [Google Scholar]
- Hauke G, Kritikos A. (2016) Embodiment in psychotherapy. In: Cooper H, Hedges L, Valentine JC. (eds) The Handbook of Research Synthesis and Meta-Analysis. New York: Russel Sage Foundation, 281–298. [Google Scholar]
- Hedges L. (2019) Stochastically dependent effect sizes. In: Cooper H, Hedges L and Valentine JC (eds) The handbook of research synthesis and meta-analysis. Russel Sage Foundation, 281–298. [Google Scholar]
- Higgins JPT, Green S. (2011) Obtaining standard deviations from standard errors and confidence intervals for group means. Available from: https://handbook-5-1.cochrane.org/chapter_7/7_7_3_2_obtaining_standard_deviations_from_standard_errors_and.htm (accessed on 15 January 2023).
- Higgins J, Thomas J, Chandler J, et al. (2022). Cochrane Handbook for Systematic Reviews of Interventions, Available from: https://www.training.cochrane.org/handbook (accessed on 10 January 2023). [Google Scholar]
- Hölzel BK, Carmody J, Vangel M, et al. (2011) Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research 191(1): 36–43. DOI: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong QN, Pluye P, Fabregues S, et al. (2019) Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. Journal of Clinical Epidemiology 111: 49–59. DOI: 10.1016/j.jclinepi.2019.03.008. [DOI] [PubMed] [Google Scholar]
- Hundt NE, Ecker AH, Thompson K, et al. (2020) “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychological Services 17(4): 414–421. DOI: 10.1037/ser0000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue C, Shawler E, Jordan CH, et al. (2023) Veteran and Military Mental Health Issues. St. Petersburg: StatPearls Publishing. [PubMed] [Google Scholar]
- Kabat-Zinn J. (2003) Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice 10(2): 144–156. DOI: 10.1093/clipsy.bpg016. [DOI] [Google Scholar]
- Kabat-Zinn J. (2013) Full Catastrophe Living: How to Cope with Stress, Pain and Illness Using Mindfulness. Boston: Little Brown. [Google Scholar]
- Kearney DJ, McDermott K, Malte C, et al. (2012) Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology 68(1): 101–116. DOI: 10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Malte C, et al. (2013) Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. Journal of Clinical Psychology 69(1): 14–27. DOI: 10.1002/jclp.21911. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, Simpson TL, Malte CA, et al. (2016) Mindfulness-based stress reduction in addition to usual care is associated with improvements in pain, fatigue, and cognitive failures among veterans with Gulf War Illness. The American Journal of Medicine 129(2): 204–214. DOI: 10.1016/j.amjmed.2015.09.015. [DOI] [PubMed] [Google Scholar]
- Kessel R, Gecht J, Forkmann T, et al. (2016) Exploring the relationship of decentering to health related concepts and cognitive and metacognitive processes in a student sample. BMC Psychology 4(1): 11–21. DOI: 10.1186/s40359-016-0115-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo E-L, Small R, Cheng W, et al. (2019) Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evidence Based Mental Health 22: 26–35. DOI: 10.1136/ebmental-2018-300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Schneider SM, Kravitz L, et al. (2013) Mind-body practices for posttraumatic stress disorder. Journal of Investigative Medicine 61(5): 827–834. DOI: 10.2310/JIM.0b013e3182906862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluepfel L, Ward T, Yehuda R, et al. (2013) The evaluation of mindfulness-based stress reduction for veterans with mental health conditions. Journal of Holistic Nursing 31(4): 248–255. DOI: 10.1177/0898010113495975. [DOI] [PubMed] [Google Scholar]
- Leow T, Li WW, Miller DJ, et al. (2024) Prevalence of university non-continuation and mental health conditions, and effect of mental health conditions on non-continuation: a systematic review and meta-analysis. Journal of Mental Health, Advance online publication. DOI: 10.1080/09638237.2024.2332812. [DOI] [PubMed] [Google Scholar]
- Li J, Cai Z, Li X, et al. (2021. a) Mindfulness-based therapy versus cognitive behavioral therapy for people with anxiety symptoms: a systematic review and meta-analysis of random controlled trials. Annals of Palliative Medicine 10(7): 7596–7612. DOI: 10.21037/apm-21-1212. [DOI] [PubMed] [Google Scholar]
- Li WW, Chhabra J, Singh S. (2021. b) Palliative care education and its effectiveness: a systematic review. Public Health 194: 96–108. DOI: 10.1016/j.puhe.2021.02.033. [DOI] [PubMed] [Google Scholar]
- Li WW, Miller D, Leow T, et al. (2023. a) The relationship between mindfulness and mental distress in Chinese people during the COVID-19 pandemic: moderating effects of infection severity of region and mediating effects of resilience and self-efficacy. Journal of Pacific Rim Psychology 17: 1–14. DOI: 10.1177/18344909231192765. [DOI] [Google Scholar]
- Li WW, Miller D, Shapiro S, et al. (2023. b) Editorial: mindfulness and mental health in the time of the COVID-19 pandemic. Frontiers in Psychology 14: 1209911. DOI: 10.3389/fpsyg.2023.1209911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li WW, McIntyre R, Reid C, et al. (2024. a) A Systematic review on the state of the art of culturally adapted mindfulness-based interventions for First Nations peoples: cultural adaptation, effectiveness, and feasibility. Mindfulness, Advance online publication. DOI: 10.1007/s12671-024-02440-4. [DOI] [Google Scholar]
- Li WW, Heward C, Merrick A, et al. (2024. b) Prevalence of experiencing public humiliation and its effects on victims’ mental health: a systematic review and meta-analysis. Journal of Pacific Rim Psychology 18: 1–17. DOI: 10.1177/18344909241252325. [DOI] [Google Scholar]
- Liu Q, Zhu J, Zhang W. (2022) The efficacy of mindfulness-based stress reduction intervention 3 for post-traumatic stress disorder (PTSD) symptoms in patients with PTSD: a meta-analysis of four randomized controlled trials. Stress and Health 38(4): 626–636. DOI: 10.1002/smi.3138. [DOI] [PubMed] [Google Scholar]
- Marchand WR, Sandoval K, Lackner R, et al. (2021) Mindfulness-based interventions for military veterans: a systematic review and analysis of the literature. Complementary Therapies in Clinical Practice 42: 101274–101284. DOI: 10.1016/j.ctcp.2020.101274. [DOI] [PubMed] [Google Scholar]
- Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. (2021) A theory of planned behavior scale for adherence to trauma-focused posttraumatic stress disorder treatments. Journal of Traumatic Stress 34(2): 440–453. DOI: 10.1002/jts.22620. [DOI] [PubMed] [Google Scholar]
- Murphy D, Smith KV. (2018) Treatment efficacy for veterans with posttraumatic stress disorder: latent class trajectories of treatment response and their predictors. Journal of Traumatic Stress 31(5): 753–763. DOI: 10.1002/jts.22333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Y, Ma L, Li J. (2020) Effects of mindfulness-based stress reduction and mindfulness-based cognitive therapy in people with diabetes: a systematic review and meta-analysis. Journal of Nursing Scholarship 52(4): 379–388. DOI: 10.1111/jnu.12560. [DOI] [PubMed] [Google Scholar]
- Nidich S, Mills PJ, Rainforth M, et al. (2018) Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial. The Lancet Psychiatry 5(12): 975–986. DOI: 10.1016/S2215-0366(18)30384-5. [DOI] [PubMed] [Google Scholar]
- Omidi A, Mohammadi A, Zargar F, et al. (2013) Efficacy of mindfulness-based stress reduction on mood States of veterans with post-traumatic stress disorder. Archives of Trauma Research 1(4): 151–154. DOI: 10.5812/atr.8226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypiuk K, Thompson E, Wayne PM. (2018) Can Tai Chi and Qigong postures shape our mood? Toward an embodied cognition framework for mind-body research. Frontiers in Human Neuroscience 12: 174–184. DOI: 10.3389/fnhum.2018.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak T, Lohr C, Jahn B, et al. (2018) Embodied cognition and the direct induction of affect as a compliment to cognitive behavioural therapy. Behavioral Sciences 8(29): 1–23. DOI: 10.3390/bs8030029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Thuras P, et al. (2015) Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. The Journal of the American Medical Association 314(5): 456–465. DOI: 10.1001/jama.2015.8361. [DOI] [PubMed] [Google Scholar]
- Possemato K, Bergen-Cico D, Treatman S, et al. (2016) A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. Journal of Clinical Psychology 72(3): 179–193. DOI: 10.1002/jclp.22241. [DOI] [PubMed] [Google Scholar]
- Price CJ, Hooven C. (2018) Interoceptive awareness skills for emotion regulation: theory and approach of mindful awareness in body-oriented therapy (MABT). Frontiers in Psychology 9(798): 1–20. DOI: 10.3389/fpsyg.2018.00798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priya G, Kalra S. (2018) Mind-body interactions and mindfulness meditation in diabetes. European Endocrinology 14(1): 35–41. DOI: 10.17925/ee.2018.14.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saban KL, Collins EG, Mathews HL, et al. (2022) Impact of a mindfulness-based stress reduction program on psychological well-being, cortisol, and inflammation in women veterans. Journal of General Internal Medicine 37: S751–761. DOI: 10.1007/s11606-022-07584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schure MB, Simpson TL, Martinez M, et al. (2018) Mindfulness-based processes of healing for veterans with post-traumatic stress disorder. Journal of Alternative and Complementary Medicine 24(11): 1063–1068. DOI: 10.1089/acm.2017.0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciarrino NA, Bartlett BA, Smith LJ, et al. (2022) Factors contributing to PTSD treatment dropout in veterans returning from the wars in Iraq and Afghanistan: a systematic review. Psychological Services 19(1): 183–200. DOI: 10.1037/ser0000519. [DOI] [PubMed] [Google Scholar]
- Serpa J, Taylor S, Tillisch K. (2014) Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Medical Care 52(5): 19–24. [DOI] [PubMed] [Google Scholar]
- Shapira I, Richman J, Pace TWW, et al. (2022) Biomarker response to mindfulness intervention in veterans diagnosed with post-traumatic stress disorder. Mindfulness 13(10): 2448–2460. DOI: 10.1007/s12671-022-01969-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Marmar CR. (2020) First-line psychotherapies for military-related PTSD. The Journal of the American Medical Association 323(7): 656–657. DOI: 10.1001/jama.2019.20825. [DOI] [PubMed] [Google Scholar]
- Stevelink SAM, Jones M, Hull L, et al. (2018) Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study. The British Journal of Psychiatry 213(6): 690–697. DOI: 10.1192/bjp.2018.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Grubaugh A, et al. (2011) Prolonged exposure therapy for combat-related posttraumatic stress disorder: an examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders 25(3): 397–403. DOI: 10.1016/j.janxdis.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk J, Bosman L, Hoekstra T, et al. (2018) Different ways to estimate treatment effects in randomised controlled trials. Contemporary Clinical Trials Communications 10: 80–85. DOI: 10.1016/j.conctc.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hooff M, Lawrence-Wood E, Sadler N, et al. (2019) Transition and Wellbeing Research Programme: Key Findings Report. Available at: https://www.dva.gov.au/sites/default/files/twrp_key_findings_report_web_acc_final.pdf (accessed on 8 January 2023). [Google Scholar]
- Varker T, Jones KA, Arjmand H-A, et al. (2021) Dropout from guideline-recommended psychological treatments for posttraumatic stress disorder: a systematic review and meta-analysis. Journal of Affective Disorders Reports 4(100093): 1–10. DOI: 10.1016/j.jadr.2021.100093. [DOI] [Google Scholar]
- Watkins LE, Sprang KR, Rothbaum BO. (2018) Treating PTSD: a review of evidence-based psychotherapy interventions. Frontiers in Behavioral Neuroscience 12(258): 1–19. DOI: 10.3389/fnbeh.2018.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White CA, Uttl B, Holder MD. (2019) Meta-analyses of positive psychology interventions: the effects are much smaller than previously reported. PLoS One 14(5): 1–48. DOI: 10.1371/journal.pone.0216588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2023) Depressive disorder (depression). Available at: https://www.who.int/news-room/fact-sheets/detail/depression (accessed 21 October 2023).
- Wigg L, Li WW, Leow T. (2024) A systematic review and meta-analysis on teaching by humiliation in medical training: its frequency and impact on the mental health outcomes of medical trainees. Medical Science Educator, Advance online publication. DOI: 10.1007/s40670-024-02213-7. [DOI] [Google Scholar]
- Wolff R, Moons KGM, Riley RD, et al. (2019) PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Annals of International Medicine 170: 51–58. DOI: 10.7326/M18-1376. [DOI] [PubMed] [Google Scholar]
- Zainal NZ, Booth S, Huppert FA. (2013) The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psycho-Oncology 22(7): 1457–1465. DOI: 10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The effectiveness of mindfulness-based stress reduction (MBSR) on depression, PTSD, and mindfulness among military veterans: A systematic review and meta-analysis by Wendy Wen Li, Jaime Nannestad, Timothy Leow and Carolyn Heward in Health Psychology Open.