Abstract
Background
Conservative surgery for adenomyosis has been shown to be effective. However, risk factors for postoperative recurrence have yet to be clarified. In this study, we aimed to determine the recurrence rate after conservative surgery for adenomyosis and identify the risk factors for recurrence.
Methods
This retrospective study was conducted in a tertiary hospital. Patients who underwent conservative surgery for adenomyosis between January 2013 and April 2023 were identified. Eligible patients were assigned to either the recurrent or non-recurrent group. Continuous and categorical variables were compared between the two groups using the Mann–Whitney U test or chi-squared test. Risk factors for recurrence were identified by Cox proportional risk analysis.
Results
Data for 133 eligible patients who underwent conservative surgery for adenomyosis were analyzed. The mean follow-up duration was 52 months. The recurrence rate after conservative surgery was 39.1% (52/133). Cox proportional risk analysis identified adenomyosis involving the posterior uterine wall (hazard ratio [HR] 6.505, P = 0.018), two or more adenomyotic lesions (HR 6.310, P = 0.030), laparotomy (HR 2.490, P = 0.029), and concomitant endometriosis (HR 2.313, P = 0.036) to be risk factors for recurrence after conservative surgery. Postoperative combined progestogen therapy (HR 0.126, P < 0.001) or treatment with a gonadotropin-releasing hormone agonist (GnRHa) (HR 0.237, P = 0.004) prevented recurrence of adenomyosis.
Conclusion
Adenomyosis continues to have a relatively high long-term recurrence rate after conservative surgery. Patients with adenomyosis involving the posterior wall of the uterus, those with two or more adenomyotic lesions, and those with concomitant endometriosis are at high risk for recurrence after conservative surgery. Postoperative progestogen or GnRHa therapy may reduce the risk of recurrence of adenomyosis. Considering the retrospective nature of this study and its small sample size, larger prospective studies are needed to confirm its findings.
Keywords: Adenomyosis, Conservative surgery, Recurrent, Progestogen, Gonadotropin-releasing hormone agonist
Background
Adenomyosis is a common benign uterine disease characterized by the abnormal presence of endometrial tissue within the myometrium [1]. Most patients with adenomyosis present with dysmenorrhea, abnormal uterine bleeding, and dyspareunia, which have a serious impact on their quality of life [2, 3]. As with endometriosis, adenomyosis has no typical findings on physical examination or laboratory investigations. Therefore, diagnosis of adenomyosis is based mostly on clinical suspicion and imaging methods, such as ultrasonography or magnetic resonance imaging of the pelvis [4]. Systematic reviews and meta-analyses have shown the sensitivity of transvaginal ultrasound for the diagnosis of adenomyosis [5]. With the widespread use of gynaecological ultrasound and the delayed age of female conception, more and more young women are being found to have adenomyosis [6]. In the past, hysterectomy was performed as radical treatment for adenomyosis [7, 8]. However, an increasing number of young patients are opting for fertility-preserving treatment, namely, medical therapy or conservative surgery [9].
The efficacy of medical therapy for adenomyosis is often time-limited in that symptoms can return promptly after medication is discontinued [10]. When medical therapy fails, conservative surgical treatment is required. Conservative surgery included adenomyomectomy or cytoreductive surgery/partial adenomyomectomy (laparotomy or laparoscopy) [11]. Studies have demonstrated that conservative surgical treatment is effective in relieving adenomyosis symptoms such as dysmenorrhea and bleeding, and for reducing uterine volume, but long-term postoperative management remains to be defined [12, 13]. Even though conservative surgery is effective for adenomyosis, recurrence rates of 22%–72% have been reported [14–17]. There is still no accepted definition of recurrence of adenomyosis. However, several criteria, including a visual analog scale (VAS) score of > 3, a Mansfield-Voda-Jorgensen (MVJ) score of ≥ 5, and a suspected recurrent adenomyotic lesion detected by follow-up transvaginal ultrasound and measuring ≥ 2 cm have been proposed [14, 18]. Combined postoperative use of gonadotropin-releasing hormone agonists (GnRHa) or progestogens has been reported to reduce recurrence rates, but efficacy also varies [15, 18, 19]. Therefore, it is important to be able to identify patients at high risk of postoperative recurrence during follow-up and intervene in a timely manner.
Despite the wide range of reported recurrence rates and the variable efficacy of medical therapy after conservative surgery, there have been few studies on risk factors for postoperative recurrence of adenomyosis. Sun et al. found that older age at the time of surgery (≥ 40 years) protected against recurrence but that concomitant ovarian endometriosis was a risk factor for recurrent adenomyosis [20]. Wang et al. observed that adenomyosis in the anterior uterine wall and in the fundus of the uterus was associated with a lower risk of recurrence but could not clarify the significance of foci in the posterior uterine wall [14]. Therefore, in this study, we retrospectively investigated the recurrence rate after conservative surgery for adenomyosis, the efficacy of surgery combined with hormonal therapy, and the risk factors associated with postoperative recurrence.
Methods
Study design and population
This retrospective study was conducted between January 2013 and April 2023 and was approved by the Ethics Committee of Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University (Ethical approvement: SYSKY-2024–475-01). The enrollment criteria included: 1) Age between 15–49 years; 2) Conservative surgery for adenomyosis, including adenomyectomy or cytoreductive surgery/partial adenomyectomy (laparotomy or laparoscopy); 3) Postoperative histopathological confirmation of adenomyosis; 4) Conservative surgery only or postoperative treatment with GnRHa alone for more than three courses or in combination with progestogens therapy. Progestogens including levonorgestrel releasing intrauterine system (LNG-IUS) or dienogest. Exclusion criteria included: 1) Hormone therapy was used three months prior to surgery; 2) With endometrial polyps or multiple smooth fibroids; 3) With coagulation disorders, gynaecological oncological diseases. 4) Transvaginal ultrasound was not performed at postoperative 1, 12, 24, and 36 months. 5) Failure to follow up.
Surgical procedure
All surgeries were performed under general anaesthesia by the same surgical team at Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University. During laparoscopic surgery, the patient is placed in the 30-degree Trendelenburg position, and diluted posterior pituitary hormone is injected into the myometrium via the abdomen to achieve hemostasis. A unipolar longitudinal incision is made on the surface of the uterus through the serosa and part of the myometrium to expose the thickened adenomyoma lesion. The lesion is removed with monopolar and scissors. If the endometrium is not penetrated during the procedure, the base of the lesion is closed with continuous sutures; if the uterine cavity is penetrated, the myometrium is closed with interrupted sutures in layers and the serosa is closed using “baseball” sutures. Laparotomy is performed with the patient in the lying position. A transverse incision is made in the lower abdomen, and the adenomyotic lesions are removed in a manner similar to that described above for laparoscopy, with saline washing of the pelvic cavity and placement of a pelvic drain at the end of the operation. Postoperative management options include GnRHa therapy for 3–6 months, combined progestogen therapy ((LNG-IUS or dienogest), or no therapy according to the patient's needs.
Data collection
Information on patient age, body mass index (BMI), menstrual history, fertility history, and major preoperative symptoms, including dysmenorrhea, pelvic pain and heavy menstrual bleeding (HMB), and infertility was collected from the Sun Yat-Sen Memorial Hospital data center. Data on the preoperative carbohydrate antigen 125 (CA125) level, preoperative uterine volume, preoperative VAS score, intraoperative bleeding, surgical approach, lesion size and location, and the postoperative therapies were also collected.
Dysmenorrhoea was assessed using VAS (0, no pain; 1–3, mild pain; 4–6, moderate pain; 7–10, severe pain). Menstrual bleeding was measured according to the MVJ score. An MVJ score ≥ 5 was classified as HMB. Uterine volume was calculated using the formula: volume = 0.52 × D1 × D2 × D3, where D1, D2, and D3 represent, respectively, the longitudinal, anteroposterior, and transverse dimensions of the uterus [18].
Patients were instructed to return at 1 month postoperatively for review of their surgical pathology results and to undergo transvaginal ultrasound to confirm complete resection of the lesion(s). Information regarding relief of symptoms and findings on transvaginal ultrasound was collected from all patients at 12, 24, and 36 months postoperatively via the data platform and telephone follow-up. Postoperative management and time to recurrence of adenomyosis were recorded. Symptom relief was defined as a decrease in VAS or normalization of menstrual blood flow. Recurrence was categorized as symptomatic or ultrasonographic. Symptomatic recurrence was defined as a postoperative VAS score > 3 or a postoperative MVJ score ≥ 5 [14, 18]. Ultrasonographic recurrence was defined as the presence of at least two ultrasound features of adenomyosis and a lesion size of ≥ 2 cm [14, 21]. In patients with concomitant endometriosis, recurrence was confirmed only if the patient had a suspicious adenomyotic lesion measuring ≥ 2 cm. The main points of observation were the recurrence rate and risk factors for recurrence after conservative surgery for adenomyosis.
Statistical analysis
Continuous variables were compared between groups using the Mann–Whitney U test or Kruskal–Wallis test and categorical variables using Pearson’s chi-squared test. Survival was defined as the interval between conservative surgery and recurrence of adenomyosis. We evaluated the probability of survival using the Kaplan–Meier method, with the horizontal axis of the curve representing survival time and the vertical axis representing the probability of patients without recurrence. A multifactorial Cox proportional risk model was used to identify independent risk factors for postoperative recurrence. All statistical analyses were performed using IBM SPSS Statistics for Windows version 26 (IBM Corp., Armonk, NY, USA). A P-value < 0.05 was considered statistically significant.
For missing values among continuous variables, we adopted the method of simple substitution using mean values. In order to minimize the effects of confounders such as preoperative hormonal medication and multiple uterine smooth muscle tumors on our findings, patients with these features were excluded at the study design stage.
Results
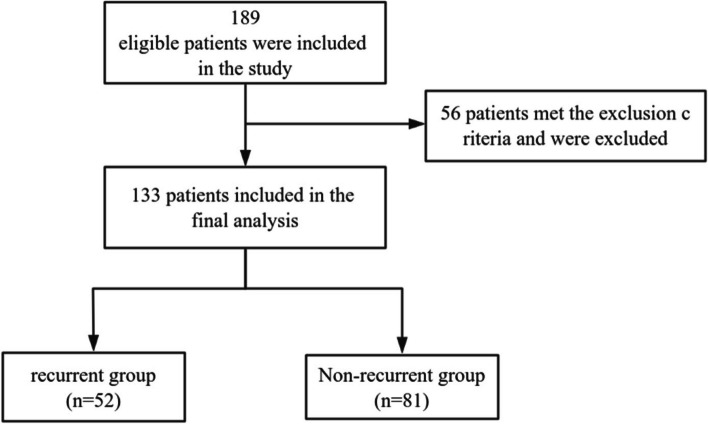
A total of 189 patients who underwent conservative surgery for adenomyosis during the study period were enrolled in the study. After 56 exclusions, 133 eligible patients were included in the analysis. There were 52 patients in the group with recurrence and 82 in the group without recurrence (Fig. 1). Transvaginal ultrasound at 1 month postoperatively confirmed that none of the 133 patients had residual lesions.
Fig. 1.
Flow chart of group allocation
The patient demographics and clinical characteristics are shown in Table 1. There was no significant between-group difference in age, body mass index, preoperative CA125 level, preoperative uterine volume or maximum lesion diameter. The mean number of abortions was significantly greater in the group with recurrence than in the group without recurrence (1.4 vs 0.8, P = 0.005). HMB was significantly more common in the group with recurrence (23.1% vs 7.4%, P = 0.010).
Table 1.
Demographic and clinical characteristics of the 2 groupsa
| Characteristics | All (n = 133) | Recurrent group (n = 52) | Non-recurrent group (n = 81) | P |
|---|---|---|---|---|
| Age, y | 36.0 ± 4.5 | 36.0 ± 4.7 | 36.0 ± 4.3 | 0.886 |
| BMI | 22.2 ± 3.2 | 22.4 ± 3.0 | 22.2 ± 3.4 | 0.985 |
| Menstrual and obstetrical histories | ||||
| Age of menartcha, y | 13.2 ± 1.1 | 13.4 ± 1.1 | 13.2 ± 1.2 | 0.470 |
| Period length, d | 6.3 ± 1.9 | 6.4 ± 1.4 | 6.2 ± 2.2 | 0.162 |
| Menstrual cycle, d | 29.8 ± 8.3 | 29.7 ± 5.4 | 29.9 ± 9.6 | 0.805 |
| Gestation | 1.8 ± 1.6 | 2.2 ± 1.7 | 1.5 ± 1.4 | 0.257 |
| Parity | 0.7 ± 0.8 | 0.8 ± 0.9 | 0.7 ± 0.8 | 0.904 |
| Abortion | 1.0 ± 1.2 | 1.4 ± 1.4 | 0.8 ± 1.0 | 0.005 |
| Preoperative CA125, U/ml | 116.0 ± 149.1 | 119.1 ± 128.8 | 113.7 ± 162.9 | 0.929 |
| Preoperative Uterine volume, cm3 | 143.6 ± 82.3 | 165.0 ± 79.5 | 129.5 ± 81.7 | 0.880 |
| Preoperative VAS score | 4.0 ± 3.0 | 4.1 ± 2.8 | 3.9 ± 3.2 | 0.045 |
| Main symptom | ||||
| Dysmenorrhea/Pelvic pain | 89(66.9%) | 33(63.5%) | 56(69.1%) | 0.497 |
| HMB | 18(13.5%) | 12(23.1%) | 6(7.4%) | 0.010 |
| Infertility or recurrent abortion | 8(6.0%) | 1(1.9%) | 7(8.6%) | 0.112 |
| Asymptomatic | 18(13.5%) | 6(11.5%) | 12(14.8%) | 0.590 |
| Types of adenomyosis | ||||
| Focal | 56(42.1%) | 24(46.2%) | 32(39.5%) | 0.449 |
| Diffuse | 77(57.9%) | 28(53.8%) | 49(60.5%) | |
| Location of the lesions | ||||
| Anterior | 15(11.3%) | 5(9.6%) | 10(12.3%) | 0.296 |
| Posterior | 63(47.4%) | 27(51.9%) | 36(44.4%) | |
| Fundus | 16(12.0%) | 3(5.8%) | 13(16.0%) | |
| Two or more lesions | 39(29.3%) | 17(32.7%) | 22(27.2%) | |
| Maximum diameter of lesion, cm | 4.7 ± 2.1 | 5.5 ± 2.2 | 4.2 ± 1.8 | 0.299 |
| Concomitant endometriosis | ||||
| Yes | 55(41.4%) | 21(40.4%) | 34(42.0%) | 0.856 |
| No | 78(58.6%) | 31(59.6%) | 47(58.0%) | |
Abbreviations: BMI body mass index (calculated as weight in kilograms divided by the square of height in meters), HMB heavy menstrual bleeding
aData are presented as mean ± standard deviation or as number (percentage)
The surgical and postoperative follow-up data are shown in Table 2. There was no significant between-group difference in the amount of intraoperative bleeding, follow-up time, or choice of postoperative therapies. Laparotomy was significantly more common in the group with recurrence than in the group without recurrence (71.2% vs 49.4%, P = 0.013). The recurrence rate after conservative surgery was 39.1% (52/133). In view of the small number of patients with pelvic pain, we evaluated dysmenorrhea and pelvic pain together. After surgery, dysmenorrhea/pelvic pain was relieved in 58.4% of cases (52/89) and HMB in 50.0% (9/18).
Table 2.
Surgical approach and postoperative management modalities and symptom reliefa
| Characteristics | All (n = 133) | Recurrent group (n = 52) | Non-recurrent group (n = 81) | P |
|---|---|---|---|---|
| Approaches of surgery | ||||
| Laparotomy | 77(57.9%) | 37(71.2%) | 40(49.4%) | 0.013 |
| Laparoscopy | 56(42.1%) | 15(28.8%) | 41(50.6%) | |
| Intraoperative bleeding, ml | 117.9 ± 250.8 | 152.3 ± 347.4 | 95.8 ± 159.9 | 0.114 |
| Follow-up time | 52.4 ± 42.1 | 62.7 ± 39.1 | 45.9 ± 42.9 | 0.478 |
| Postoperative therapies | ||||
| Surgery-only | 46(34.6%) | 23(44.2%) | 23(28.4%) | 0.061 |
| GnRHa | 50(37.6%) | 18(34.6%) | 32(39.5%) | 0.570 |
| Progestogens | 37(27.8%) | 11(21.2%) | 26(32.1%) | 0.169 |
| Dysmenorrhea/Pelvic pain relief |
All (n = 89) |
Recurrent group (n = 44) | Non-recurrent group (n = 45) | P |
| Yes | 52(58.4%) | 7(15.9%) | 45(100%) | N/A |
| No | 37(41.6%) | 37(84.1%) | 0 | |
| HMB relief | All (n = 18) | Recurrent group(n = 10) | Non-recurrent group(n = 8) | P |
| Yes | 9(50.0%) | 1(10.0%) | 8(100%) | N/A |
| No | 9(50.0%) | 9(90.0%) | 0 | |
Abbreviations: GnRHa gonadotropin-releasing hormone agonist
N/A Not applicable
aData are presented as mean ± standard deviation or as number (percentage)
Our Cox proportional risk model included six variables, namely, abortions, preoperative VAS score, location of lesions, concomitant endometriosis, approaches of surgery, and postoperative therapies (Table 3). Abortions, preoperative VAS score, and approaches of surgery were included in the Cox proportional risk model because of their significant p-values in the univariate analysis, whereas location of the lesions, concomitant endometriosis, and postoperative therapies were included in view of previous reports in the literature or in clinical experience that they may be associated with recurrence after conservative surgery for adenomyosis [14, 18]. Cox proportional risks analysis showed that lesions in the posterior uterine wall (hazard ratio [HR] 6.505, P = 0.018), two or more adenomyotic lesions (HR 6.310, P = 0.030), laparotomy (HR 2.490, P = 0.029), concomitant endometriosis (HR 2.313, P = 0.036), abortions (HR 1.578, P = 0.001), and the VAS score (HR 1.181, P = 0.036) were risk factors for recurrence after conservative surgery for adenomyosis (Table 3). Postoperative combined progestogen therapy (HR 0.126, P < 0.001) or GnRHa (HR 0.237, P = 0.004) prevented recurrence of adenomyosis after surgery. Kaplan–Meier curves for patients with adenomyosis who received treatment after conservative surgery are shown in Fig. 2.
Table 3.
Multivariate Cox regression analysis of risk factors associated with recurrence at follow-up
| Predictors | b value | HR value | HR 95.0%CI | P |
|---|---|---|---|---|
| Abortions | 0.456 | 1.578 | 1.208–2.062 | 0.001 |
| Preoperative VAS score | 0.166 | 1.181 | 1.029–1.355 | 0.036 |
| Location of the lesions | ||||
| Anterior | 0a | |||
| Posterior | 1.872 | 6.505 | 1.388–30.481 | 0.018 |
| Fundus | 0.938 | 2.555 | 0.367–17.772 | 0.343 |
| Two or more lesions | 1.842 | 6.310 | 1.194–33.348 | 0.030 |
| Concomitant endometriosis | ||||
| No | 0a | |||
| Yes | 0.838 | 2.313 | 1.058–5.055 | 0.036 |
| Approaches of surgery | ||||
| Laparoscopy | 0a | |||
| Laparotomy | 0.912 | 2.490 | 1.100–5.639 | 0.029 |
| Postoperative therapies | ||||
| Surgery-only | 0a | |||
| GnRHa | −1.440 | 0.237 | 0.090–0.625 | 0.004 |
| Progestogens | −2.075 | 0.126 | 0.040–0.394 | < 0.001 |
Abbreviations: GnRHa gonadotropin-releasing hormone agonist
aControl group
Fig. 2.
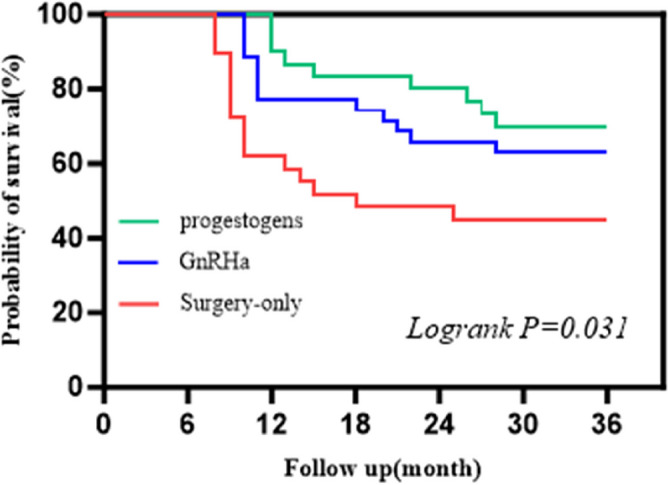
Kaplan–Meier estimates of survival in patients on three postoperative hormone therapies
Pregnancy was attempted by 69 of the 133 patients postoperatively, with a final pregnancy rate of 26.1% (18/69) and 16 successful deliveries. Three patients opted for hysterectomy after recurrence.
Discussion
Conservative surgery is an option for patients with adenomyosis who wish to preserve their fertility. Conservative surgery has been proved to be effective and seems to be more sustainable than hysterectomy with fewer surgical consumables and a smaller carbon footprint [13, 22]. However, postoperative recurrence rates of 22%–72% have been reported [14–17]. In our study, the recurrence rate after conservative surgery for adenomyosis was 39.1% (52/133). The wide variation in postoperative recurrence rates may reflect differences in surgical teams and duration of follow-up. Early identification of the risk of recurrence and timely intervention are important in order to improve the surgical outcome and reduce the rate of postoperative recurrence. However, there have been few studies on risk factors for recurrence after surgery for adenomyosis.
Patients with adenomyotic lesions in the anterior uterine wall or the fundus of the uterus are at low risk of recurrence after conservative surgery, but the significance of lesions located in the posterior wall has not been clarified [14]. Our findings demonstrated that foci in the posterior wall is a risk factor for recurrence of adenomyosis after conservative surgery (HR 6.505, P = 0.018). Focal adenomyosis located in the outer myometrium (FAOM) is associated with deep posterior infiltrative lesions involving the bowel [23]. The presence of FAOM is also significantly associated with the severity of deep infiltrating endometriosis (DIE) [24]. Shi et al. investigated the effect of lesion localization on clinical features in 158 patients who underwent conservative surgery for adenomyosis and found that lesions in the posterior wall of the uterus were associated with HMB [25]. The susceptibility of adenomyotic lesions located in the posterior wall to recurrence after surgery may be related to involvement of the bowel, more severe deep infiltrative lesions in the posterior region, and more rapid onset of symptomatic recurrence. Therefore, it may be appropriate to intervene after conservative surgery in patients with adenomyosis whose lesions are located in the posterior wall. Furthermore, clinicians should keep in mind the possibility of comorbid endometriosis and DIE during follow-up.
In our study, recurrence was more likely in patients with two or more adenomyotic lesions (HR 6.310, P = 0.030) or those who underwent laparotomy (HR 2.490, P = 0.029). Adenomyosis is characterised by the invasion of endometrial tissue into the myometrium, which blurs the boundary between the lesion and normal tissue [26]. The area of complete removal of the adenomyotic lesion remains inaccurate because of the lack of clear boundaries, and removal of the lesion is always accompanied by resection of the uterine myometrium, which is destructive to the uterine wall [11]. Therefore, when performing conservative surgery for adenomyosis, it is important to remove as many lesions as possible and try to preserve as much normal uterine tissue as possible. Unlike with previously reported indocyanine green infrared imaging [27], our procedure is performed under white light, which does not exclude the possibility of tiny residual lesions. There is no exact criterion for choosing between laparoscopy and laparotomy. The decision is usually based on a combination of the patient's specific circumstances, personal wishes, and the surgeon’s clinical experience. Previous literature reviews have found no significant difference in the efficacy of the various types of conservative surgery performed for adenomyosis [13]. Laparotomy seems to be more favorable than laparoscopy for severe diffuse adenomyosis [15]. Focal adenomyosis lesions smaller than 5 cm may be treatable laparoscopically [28]. However, the surgical approach for adenomyosis remains controversial, and more supportive evidence is needed.
Patients with adenomyosis and concomitant endometriosis are at higher risk of recurrence [20, 29]. Women with endometriosis often have concomitant adenomyosis and vice versa [30, 31]. Higher pain scores after laparoscopy have been reported in patients with adenomyosis combined with DIE [32]. Zhu et al. and Landi et al. found that patients with adenomyosis combined with endometriosis had a significantly higher rate of clinical recurrence after surgery than patients with adenomyosis or endometriosis alone [15, 33]. Patients with adenomyosis and concomitant endometriosis are recommended to receive hormone suppression therapy after conservative surgery and to be followed closely for dysmenorrhea and changes in severity of pain.
We also found an association between the number of abortions and the risk of adenomyosis recurrence after conservative surgery (HR 1.578, P = 0.001). The pathogenesis of adenomyosis is associated with damage to the endometrium, and perioperative interventions may reduce the risk of adenomyosis when uterine dilatation and curettage are performed [4, 34]. However, the mechanisms via which the number of abotions influence the risk of recurrence in patients with adenomyosis remain unclear and should be explored in the future.
Application of hormone therapy after conservative surgery for adenomyosis or in the perioperative period may reduce the risk of recurrence [16, 18, 35]. In our study, postoperative combined progestogen therapy (HR 0.126, P < 0.001) or GnRHa (HR 0.237, P = 0.004) protected against adenomyosis. Combined hormone therapy may reduce the risk of postoperative recurrence in patients with two or more adenomyotic lesions or lesions located in the posterior wall.
This study had some limitations. First, it had a retrospective design, and patients' preoperative pain scores and number of abortions were self-reported. Therefore, the possibility of recall bias during follow-up cannot be excluded. Second, there is no exact criterion for selection of a conservative surgical modality for adenomyosis, which introduces the possibility of selection bias. Third, the study was performed at a single center and had a small sample size, which limits the generalizability of our findings. However, this meant that patients received similar treatment. Prospective studies in larger sample sizes are needed to confirm our results.
Conclusions
This study identified a high long-term recurrence rate after conservative surgery for adenomyosis. Patients with adenomyosis involving the posterior wall of the uterus, those with two or more adenomyotic lesions, and those with concomitant endometriosis are at high risk for recurrence after conservative surgery. Combined hormonal therapy postoperatively may reduce the risk of recurrence. However, considering the retrospective design of this study and its small sample size, prospective studies in larger samples are needed to confirm its findings.
Acknowledgements
We are grateful to all the patients who participated in this study. Thanks to M.S. Dehua Liao for his valuable comments.
Abbreviations
- GnRHa
Gonadotropin-releasing hormone agonist
- LNG-IUS
Levonorgestrel releasing intrauterine system
- BMI
Body mass index
- HMB
Heavy menstrual bleeding
- CA125
Carbohydrate antigen 125
- MVJ
Mansfield-Voda-Jorgensen
- VAS
Visual analogue scale
- DIE
Deep infiltrating endometriosis
Authors’ contributions
KJL and GZZ were responsible for the interpretation of data and manuscript drafting; YCW and MQX contributed to conception and study design; XZZ was mainly in charge of the data analysis; BRL took part in the acquisition of data. All authors read and approved the final manuscript.
Funding
This study was supported by funds from the National Natural Science Foundation of China (81901457, 82171670, 81802552).
Data availability
Data and related materials supporting the findings of this study are available upon request from the corresponding author.
Declarations
Ethics approval and consent to participate
This study was approved by the Review Committee of Sun Yat-sen Memorial Hospital of Sun Yat-sen University, Guangzhou City, Guangdong Province, China (Ethical approval number: SYSKY-2024–475-01). We confirm that all methods were performed in accordance with relevant guidelines and regulations. Although this was a retrospective study, it did not involve human experimentation. An informed consent waiver was obtained for our study from the Institutional Review Board of Sun Yat-sen Memorial Hospital, Sun Yat-sen University.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Keji Lu and Guangzheng Zhong contributed equally to this work and should be considered co-first authors.
Meiqing Xie and Yingchen Wu contributed as co-corresponding author for this work.
Contributor Information
Meiqing Xie, Email: xiemq@mail.sysu.edu.cn.
Yingchen Wu, Email: wuyingchen123@163.com.
References
- 1.Bulun SE, Yildiz S, Adli M, Chakravarti D, Parker JB, Milad M, et al. Endometriosis and adenomyosis: shared pathophysiology. Fertil Steril. 2023;119(5):746–50. [DOI] [PubMed] [Google Scholar]
- 2.Bulun SE, Yildiz S, Adli M, Wei JJ. Adenomyosis pathogenesis: insights from next-generation sequencing. Hum Reprod Update. 2021;27(6):1086–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moldassarina RS. Modern view on the diagnostics and treatment of adenomyosis. Arch Gynecol Obstet. 2023;308(1):171–81. [DOI] [PubMed] [Google Scholar]
- 4.Schrager S, Yogendran L, Marquez CM, Sadowski EA. Adenomyosis: diagnosis and management. Am Fam Physician. 2022;105(1):33–8. [PubMed] [Google Scholar]
- 5.Andres MP, Borrelli GM, Ribeiro J, Baracat EC, Abrao MS, Kho RM. Transvaginal ultrasound for the diagnosis of adenomyosis: systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25(2):257–64. [DOI] [PubMed] [Google Scholar]
- 6.Moawad G, Kheil MH, Ayoubi JM, Klebanoff JS, Rahman S, Sharara FI. Adenomyosis and infertility. J Assist Reprod Genet. 2022;39(5):1027–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharara FI, Kheil MH, Feki A, Rahman S, Klebanoff JS, Ayoubi JM, et al. Current and prospective treatment of adenomyosis. J Clin Med. 2021;10(15):3410. [DOI] [PMC free article] [PubMed]
- 8.Oliveira MAP, Crispi CP Jr, Brollo LC, Crispi CP, De Wilde RL. Surgery in adenomyosis. Arch Gynecol Obstet. 2018;297(3):581–9. [DOI] [PubMed] [Google Scholar]
- 9.Stratopoulou CA, Donnez J, Dolmans MM. Conservative management of uterine adenomyosis: medical vs. surgical approach. J Clin Med. 2021;10(21):4878. [DOI] [PMC free article] [PubMed]
- 10.Vannuccini S, Luisi S, Tosti C, Sorbi F, Petraglia F. Role of medical therapy in the management of uterine adenomyosis. Fertil Steril. 2018;109(3):398–405. [DOI] [PubMed] [Google Scholar]
- 11.Grimbizis GF, Mikos T, Tarlatzis B. Uterus-sparing operative treatment for adenomyosis. Fertil Steril. 2014;101(2):472–87. [DOI] [PubMed] [Google Scholar]
- 12.Younes G, Tulandi T. Conservative surgery for adenomyosis and results: a systematic review. J Minim Invasive Gynecol. 2018;25(2):265–76. [DOI] [PubMed] [Google Scholar]
- 13.Mikos T, Lioupis M, Anthoulakis C, Grimbizis GF. The outcome of fertility-sparing and nonfertility-sparing surgery for the treatment of adenomyosis. A systematic review and meta-analysis. J Minim Invasive Gynecol. 2020;27(2):309-31 e3. [DOI] [PubMed] [Google Scholar]
- 14.Wang W, Ma X, Zhang M, Wu Z, Xiang T, Wang S. Comparison of recurrence rate and risk factors in patients with focal adenomyosis with and without medical treatment after conservative surgery. Int J Gynaecol Obstet. 2023;161(2):594–600. [DOI] [PubMed] [Google Scholar]
- 15.Zhu L, Chen S, Che X, Xu P, Huang X, Zhang X. Comparisons of the efficacy and recurrence of adenomyomectomy for severe uterine diffuse adenomyosis via laparotomy versus laparoscopy: a long-term result in a single institution. J Pain Res. 2019;12:1917–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang PH, Liu WM, Fuh JL, Cheng MH, Chao HT. Comparison of surgery alone and combined surgical-medical treatment in the management of symptomatic uterine adenomyoma. Fertil Steril. 2009;92(3):876–85. [DOI] [PubMed] [Google Scholar]
- 17.Shi JH, Zhu SY, Li XY, Dai Y, Leng JH. The role of levonorgestrel-releasing intrauterine system for recurrence prevention after conservative surgery among patients with coexistent ovarian endometrioma and diffuse adenomyosis: A retrospective case control study with long-term follow up. J Gynecol Obstet Hum Reprod. 2023;52(5):102572. [DOI] [PubMed] [Google Scholar]
- 18.Jiang J, Pan Y, Yu J, Zhang Y, Yang Y, Xu H, et al. Laparoscopic adenomyomectomy combined with levonorgestrel-releasing intrauterine system is effective for long-term management of adenomyosis. BMC Womens Health. 2024;24(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan IS, Hsu TF, Shih YC, Chang YH, Wang PH, Chen YJ. Maintenance dienogest therapy following adjuvant gonadotropin-releasing hormone agonist treatment after uterus-sparing surgery in adenomyosis: A retrospective cohort study. Int J Gynaecol Obstet. 2023;161(3):751–9. [DOI] [PubMed] [Google Scholar]
- 20.Sun F, Yu J, Pan Y, Huo X, Yang Y, Xu H. Risk factors for symptomatic recurrence after laparoscopic adenomyomectomy: a 3-year follow-up. J Minim Invasive Gynecol. 2023;30(7):555–61. [DOI] [PubMed] [Google Scholar]
- 21.Borghese G, Doglioli M, Orsini B, Raffone A, Neola D, Travaglino A, et al. Progression of adenomyosis: Rate and associated factors. Int J Gynaecol Obstet. 2024;167(1):214–22. [DOI] [PubMed] [Google Scholar]
- 22.National Institute for H, Care Research Global Health Research Unit on Global S. Reducing the environmental impact of surgery on a global scale: systematic review and co-prioritization with healthcare workers in 132 countries. Br J Surg. 2023;110(7):804–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chapron C, Tosti C, Marcellin L, Bourdon M, Lafay-Pillet MC, Millischer AE, et al. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum Reprod. 2017;32(7):1393–401. [DOI] [PubMed] [Google Scholar]
- 24.Marcellin L, Santulli P, Bourdon M, Maignien C, Campin L, Lafay-Pillet MC, et al. Focal adenomyosis of the outer myometrium and deep infiltrating endometriosis severity. Fertil Steril. 2020;114(4):818–27. [DOI] [PubMed] [Google Scholar]
- 25.Shi J, Wu Y, Li X, Gu Z, Zhang C, Yan H, et al. Effects of localization of uterine adenomyosis on clinical features and pregnancy outcome. Sci Rep. 2023;13(1):14714. [DOI] [PMC free article] [PubMed]
- 26.Harmsen MJ, Trommelen LM, de Leeuw RA, Tellum T, Juffermans LJM, Griffioen AW, et al. Uterine junctional zone and adenomyosis: comparison of MRI, transvaginal ultrasound and histology. Ultrasound Obstet Gynecol. 2023;62(1):42–60. [DOI] [PubMed] [Google Scholar]
- 27.Vizzielli G, Cosentino F, Raimondo D, Turco LC, Vargiu V, Iodice R, et al. Real three-dimensional approach vs two-dimensional camera with and without real-time near-infrared imaging with indocyanine green for detection of endometriosis: A case-control study. Acta Obstet Gynecol Scand. 2020;99(10):1330–8. [DOI] [PubMed] [Google Scholar]
- 28.Kwack JY, Im KS, Kwon YS. Conservative surgery of uterine adenomyosis via laparoscopic versus laparotomic approach in a single institution. J Obstet Gynaecol Res. 2018;44(7):1268–73. [DOI] [PubMed] [Google Scholar]
- 29.Yu W, Liu G, Liu C, Zhang Z. Recurrence‑associated factors of laparoscopic adenomyomectomy for severely symptomatic adenomyoma. Oncol Lett. 2018;16(3):3430–8. [DOI] [PMC free article] [PubMed]
- 30.Di Donato N, Montanari G, Benfenati A, Leonardi D, Bertoldo V, Monti G, et al. Prevalence of adenomyosis in women undergoing surgery for endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;181:289–93. [DOI] [PubMed] [Google Scholar]
- 31.Upson K, Missmer SA. Epidemiology of adenomyosis. Semin Reprod Med. 2020;38(2–03):89–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lazzeri L, Di Giovanni A, Exacoustos C, Tosti C, Pinzauti S, Malzoni M, et al. Preoperative and postoperative clinical and transvaginal ultrasound findings of adenomyosis in patients with deep infiltrating endometriosis. Reprod Sci. 2014;21(8):1027–33. [DOI] [PubMed] [Google Scholar]
- 33.Landi S, Mereu L, Pontrelli G, Stepniewska A, Romano L, Tateo S, et al. The influence of adenomyosis in patients laparoscopically treated for deep endometriosis. J Minim Invasive Gynecol. 2008;15(5):566–70. [DOI] [PubMed] [Google Scholar]
- 34.Guo SW. The pathogenesis of adenomyosis vis-a-vis endometriosis. J Clin Med. 2020;9(2):485. [DOI] [PMC free article] [PubMed]
- 35.Chao X, Song X, Wu H, You Y, Li L, Lang J. Adjuvant therapy in conservative surgery for adenomyosis. Int J Gynaecol Obstet. 2021;154(1):119–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and related materials supporting the findings of this study are available upon request from the corresponding author.