ABSTRACT
Impaired thermoregulatory function is a clinical feature of many health conditions that affect triathletes using wheelchairs and consequently, individual athlete performances may fluctuate according to environmental temperature. We aimed to determine the effect of 1) water temperature on wheelchair triathlon swim time and 2) air temperature on handcycle and wheelchair run (push) time. Published race records from 2017 to 2023 (n = 49 events) were extracted from the World Triathlon website. Bayesian negative binomial regression was used to separately model the nonlinear relationships between water temperature and swim time, and air temperature and handcycle and push time. Age, sex, sport class, whether wetsuits were worn (swim model), and swim time (handcycle and push model) were included as fixed effects. Over the observed water temperature range of 15.7–30.5°C, male swim time (mm:ss) improved from 14:13 (95% credible interval [CrI] = 12:27, 16:09) to 12:35 (95% CrI = 11:00, 14:19). Female swim time improved from 15:33 (95% CrI = 13:24, 17:55) to 12:46 (95% CrI = 11:03, 14:38). It was unclear whether handcycle and push time slowed over the observed air temperature range of 14–33°C. Warmer water temperatures, up to 30.5°C, were associated with faster swim times. It was unclear whether combined handcycle and push time slowed with increases in air temperature, up to 33°C. The integration of information on athlete impairment type and severity with performance data is needed to better understand the extent to which individual athlete performances fluctuate across environmental conditions.
KEYWORDS: Athletic performances, heat stress disorder, para-athletes, sports for persons with disabilities, temperature
Introduction
Impaired thermoregulatory function is a clinical feature of many health conditions that affect triathletes who use wheelchairs, including spinal cord injury [1] and multiple sclerosis [2]. Yet, the impact of environmental heat on endurance exercise performance in Para athlete populations has received little scientific attention [3]. The only available study, a recent investigation by Alkemade et al. [4], compared time-to-exhaustion in the heat (31.9°C and 72% relative humidity [rh]) between elite Para (cycling and wheelchair tennis) and able-bodied athletes [4]. The study found that in hot-humid conditions, Para athletes experienced similar performance decrements to able-bodied athletes.
A study of Para triathletes competing in the 2017 World Cup (water 27°C; air 33°C; 41% rh) and 2018 World Series (water 25°C; air 33°C; 35% rh) reported that the core temperature of triathletes using wheelchairs increased by an average of 1.4°C (~0.018°C/min) from pre- to post-race [5]. While the magnitude of the core temperature change was likely confounded by athletes’ heat adaptation status, the study shows that triathletes using wheelchairs experience significant levels of thermal strain. For context, in able-bodied triathletes, the rate of change in core temperature over an Olympic distance event (air 19.3°C; 55% rh) has been reported to be 0.019°C per minute [6].
World Triathlon implements a heat policy where the swim segment is canceled when water temperatures exceed 32°C (section 17.11j in [7]), and events are rescheduled or canceled when wet bulb globe temperature (WBGT) exceeds 32.2°C (section 10.3 in [7]). The policy, however, was designed to protect athlete health [8], not declines in performance, which could still be significant even within these temperature limits [9,10]. With global temperatures set to increase, triathletes who use wheelchairs will be increasingly required to perform in challenging environments [11]. To best prepare athletes, studies on how the performances of triathletes using wheelchairs fluctuate with environmental temperature are needed.
Using World Triathlon data, we aimed to determine the effect of 1) water temperature on swim time, and 2) air temperature on combined handcycle and run (herein push) time, in triathletes who use wheelchairs. We hypothesized that 1) swim time would improve in warmer water, reach a plateau, and subsequently slow in hotter temperatures, and 2) handcycle and push time would slow in a nonlinear fashion with increases in air temperature.
Materials and methods
Study overview
Race data from World Championship Series, World Championships, World Para Cup, World Para Series events between 2017 and 2023, and the Tokyo Paralympics were retrieved from the World Triathlon website (https://triathlon.org/paratriathlon/results), on May 29 2023. Race results included performance times and, in most instances, water and air temperature. We retrieved data from 2017 onwards, as this period coincides with the current classification system [12]. Data were de-identified by removing athlete names. Ethical approval for the study was not required because race records are made publicly available.
Wheelchair triathlon
Wheelchair triathlon is a multidisciplinary endurance sport that typically consists of a 750 m swim, a 20 km recumbent handcycle, and a 5 km run (push) in a racing chair, each separated by a brief transition. The swim is commenced in-water. Athletes are allowed to wear wetsuit bottoms, irrespective of the water temperature. Athletes may have one handler to support them during the two transition periods. Under the current classification system there are two sport classes, Wheelchair Triathlon Class 1 and Class 2 (section 17.2b in [7]). Class 1 athletes have more severe impairments than Class 2 athletes. Both sport classes compete in the same medal event. Male Class 1 athletes receive a time advantage of 03:00 min and female Class 1 athletes receive an advantage of 03:38 min (section 17.5i in [7]). On the elite circuit, Para triathletes compete in annual events scheduled in any season across different continents.
Data and variables
Published separately for males and females, race records included a unique identifier for each athlete, a unique identifier for each race, the event location and year, swim, cycle, and run segment times, transition 1 and transition 2 time, and total race time. The athlete's year of birth was extracted from the World Triathlon website and used to calculate age. Race results are published with program notes, which generally include water and air temperature, and segment distances. Segment distance was used to calculate the average speed of the swim, cycle, and run for each athlete.
Air temperature was not defined; however, it was assumed to be dry bulb temperature, given that race conditions are monitored with a WBGT device (section 10.3 in [7]). Wet bulb globe temperature was not reported in the program notes, and no other information on the environmental conditions (e.g. relative humidity) was provided.
Data analysis
Our primary interest was to investigate 1) the effect of water temperature on swim time and 2) the effect of air temperature on handcycle and push time.
Negative binomial regression was used to separately model swim time (in seconds) and combined handcycle and push time (in seconds). The relationship between water temperature and swim time was modeled using a natural cubic smoothing spline (knots at 22°C and 26°C), because we expected average swim times to improve as water temperature warms, plateaus, and subsequently slows in hotter temperatures. The location of the knots was chosen based on exploratory plots. The model included sex (levels: male, female), age (mean centered), sport class (levels: 1, 2), and wetsuit (levels: allowed, mandatory, not allowed) as fixed effects. A random intercept was included for each unique race, to account for differences in water conditions (e.g. currents) and race tactics [13]. The inclusion of year as a fixed effect could be used to account for policy and/or technology changes. However, there were no significant policy or technology changes between 2017 and 2023, so we opted to exclude year from the model, particularly because it was perfectly correlated with changes in age, which would have complicated the modeling approach [14].
Air temperature was included as a second-order polynomial (quadratic) term in the handcycle and push time model, because we expected handcycle and push time to slow in a nonlinear fashion with increases in air temperature. The model included sex (levels: male, female), age (mean centered), and sport class (levels: 1, 2), swim time (group [sex] mean centered [15]) and swim time by sex as fixed effects. Swim time was included to account for prior race performance, which could affect handcycle and run time. A random intercept was included for each unique race to account for differences in course geography and race tactics [13]. Year was not included for the reasons described above.
We considered the potential influence of event calendar on performance times, by including month as a random effect variable. Accounting for month had no impact on the substantive conclusions of the analysis (Supplement 1). Consequently, month was not included in the models to avoid overfitting [16].
Models were implemented in a Bayesian framework using Stan [17] with the brms interface [18]. A uniform prior distribution was used for the regression coefficients; a half t-distribution (df = 3, mean = 0, SD = 2.5) prior for the standard deviation of the random effects; and a Gamma (shape = 0.01, scale = 0.01) prior for the shape parameter. Posterior estimates were generated using Markov chain Monte Carlo methods (4 chains 10,000 iterations, 50% burnin, no thinning). Posterior estimates of interest were as follows: 1) the mean and 66% and 95% credible interval (CrI) of regression coefficients, β; 2) the probability that β was greater or less than zero, given by Pr β > 0 or Pr β < 0, depending on whether the mean effect was positive or negative; and 3) the estimated marginal mean (and 95% CrI) effect of water temperature of swim time, and air temperature on handcycle and push time. Posterior predictive checks were performed to assess the suitability of all models.
The number of events and athletes, proportion of females, and athlete age were summarized descriptively. Data cleaning, wrangling, and visualization were done using packages from the tidyverse [19]. Missing data were assumed to be missing at random [20]. Missing x-variable values (except for missing wetsuit data) were imputed using random forests [21], a nonlinear modeling technique that makes no assumptions about interactions in the data [22]. Missing wetsuit data were conditionally imputed based on the random forest imputed water temperature value, as follows: <18°C “mandatory,” 18°C to 24.5°C “allowed,” or >24.5°C “not allowed” (section 17.11f and 17.11h in [7]). The data and R code are available at https://doi.org/10.5281/zenodo.10774736.
Results
Data cleaning
A total of 639 records from 52 events between 2017 and 2023 were initially extracted. Three events (33 records from 6 races) were removed because the race was modified to a duathlon due to poor water conditions. Events from the following were included: Paratriathlon World Cup (n = 17), World Paratriathlon Series (n = 10), World Triathlon Para Cup (n = 9), World Triathlon Para Series (n = 7), World Triathlon Grand Final (n = 3), World Triathlon Championship Finals (n = 1), World Triathlon Para Championships (n = 1), and Paralympics (n = 1). Seven athletes did not start a race, 10 did not finish and 13 were disqualified. One data point was removed because it exceeded the maximum race limit of 2 h (see 17.5c in [7]), leaving 575 race records for analysis.
Missing data
From 575 race records, missing data were as follows: air temperature 17%, water temperature 14.6%, wet suit information 12.9%, swim time 3.7%, push time 1.7%, handcycle time 1.6%, and sport class 0.2%. Supplement 2 shows the combinations of missing data.
Paratriathlete demographics
There were 79 unique triathletes (n = 25 females) in the dataset (Figure 1a). Figure 1b shows the proportion of female athletes between 2017 and 2023. The mean age of male athletes remained similar across the study period, at about 37 y (Figure 1c). The mean age of female athletes was 29.5 y in 2017, increasing by 5.7 y in 2023 (Figure 1c).
Figure 1.
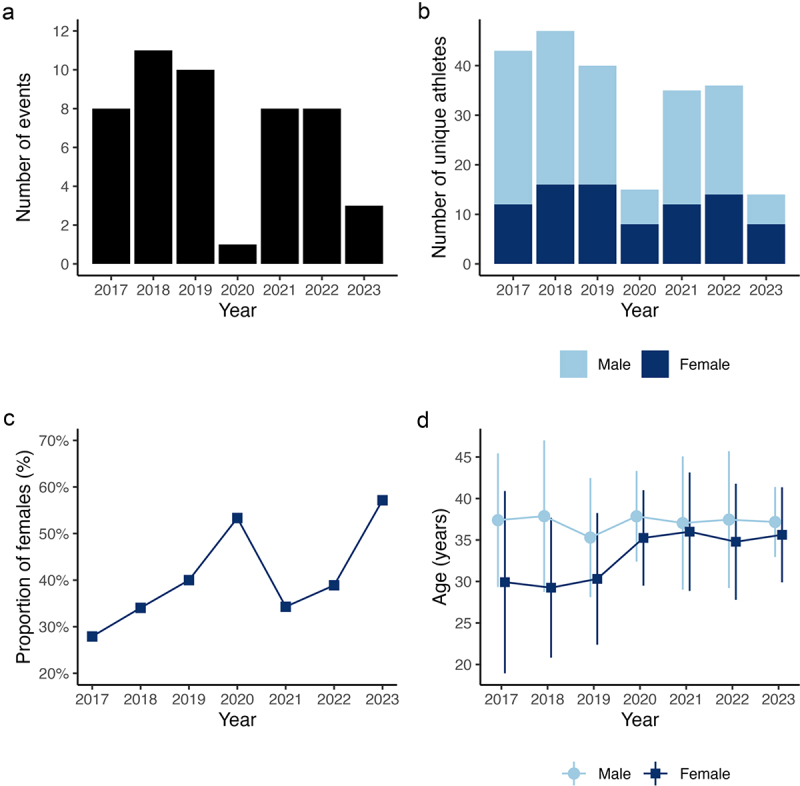
The number of wheelchair triathlon events (panel a), the number of unique male and female competitors (panel b), the proportion of female triathletes (panel c), and the age (mean with standard deviation) of male and female triathletes (panel d) between 2017 and 2023.
Overall and race segment times
Table 1 provides a summary of segment and race performance time and speed for male and female athletes.
Table 1.
Mean and standard deviation segment and overall race time and speed.
| Male Athletes | Female Athletes | |||
|---|---|---|---|---|
| Segment | Time (min) | Speed (km·h−1) | Time (min) | Speed (km·h−1) |
| Swim | 13.6 (2.9) | 3.4 (0.5) | 14.6 (2.3) | 3.2 (0.5) |
| Handcycle | 39.0 (6.3) | 32.0 (4.4) | 44.9 (6.9) | 27.7 (3.6) |
| Run (push) | 14.7 (3.0) | 21.1 (3.0) | 16.5 (2.6) | 18.7 (2.6) |
| Alla | 71.1 (9.9) | NC | 80.4 (9.0) | NC |
NC = Not computed. a All includes transition 1 and transition 2 times.
Water and air temperature
Figure 2a shows the relationship between water and air temperature. Water temperature ranged from 15.7°C to 30.5°C. Air temperature ranged from 14°C to 33°C. Figure 2b provides a summary of event locations, with missing temperature data indicated.
Figure 2.
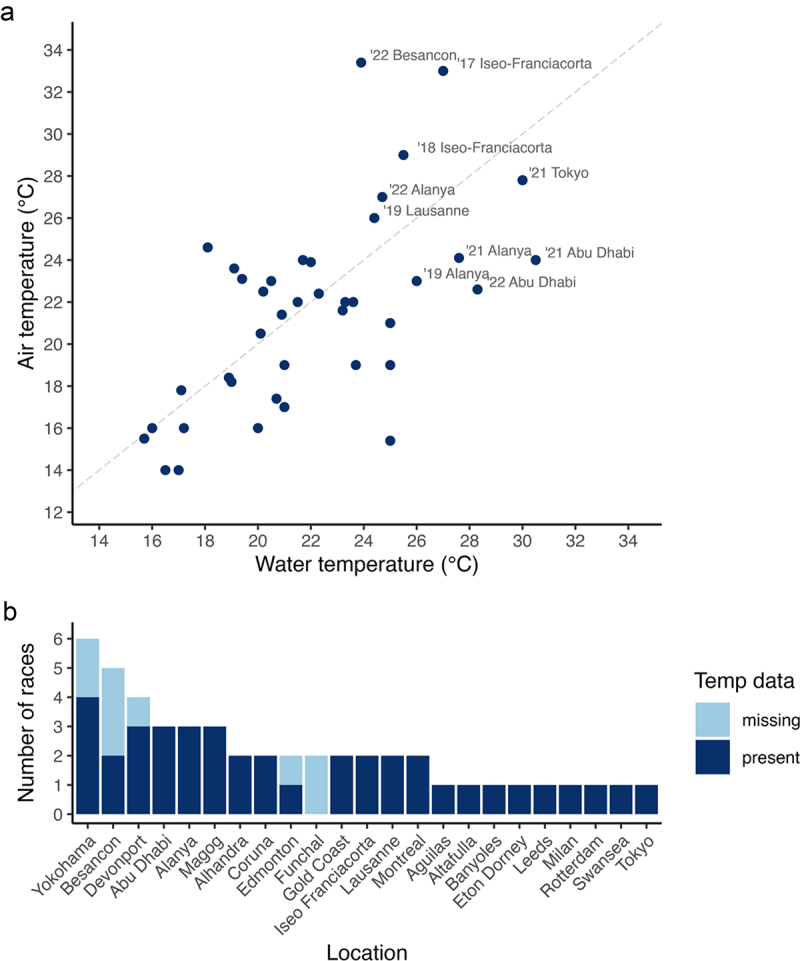
Water and air temperature from elite wheelchair triathlon events between 2017 and 2023 (panel a) and a summary of races (n = 49) according to location (panel b). In panel A, the dashed line represents the line of identity (r value of 1). Panel a location labels are provided for relatively hotter temperatures. Temp, temperature.
Water temperature and swim time
There was evidence that swim times decreased with increases in water temperature (Figure 3a and Figure 4a). There was a 95.8% chance that spline component 2 was less than zero (Pr β < 0 = .958), and a 97% chance that that spline component 3 was less than zero (Pr β < 0 = .97), see Figure 3a. Over the observed water temperature range of 15.7°C to 30.5°C, swim time (mm:ss) improved for men by 01:38 min, from 14:13 min (95% CrI = 12:27, 16:09) to 12:35 min (95% CrI = 11:00, 14:19), and improved for women by 02:47 min, from 15:33 min (95% CrI = 13:24, 17:55) to 12:46 (95% CrI = 11:03, 14:38). These changes represent a 11.5% change for men and a 17.9% change for women. A plot of individual athlete data is shown in Supplement 3 panel A.
Figure 3.
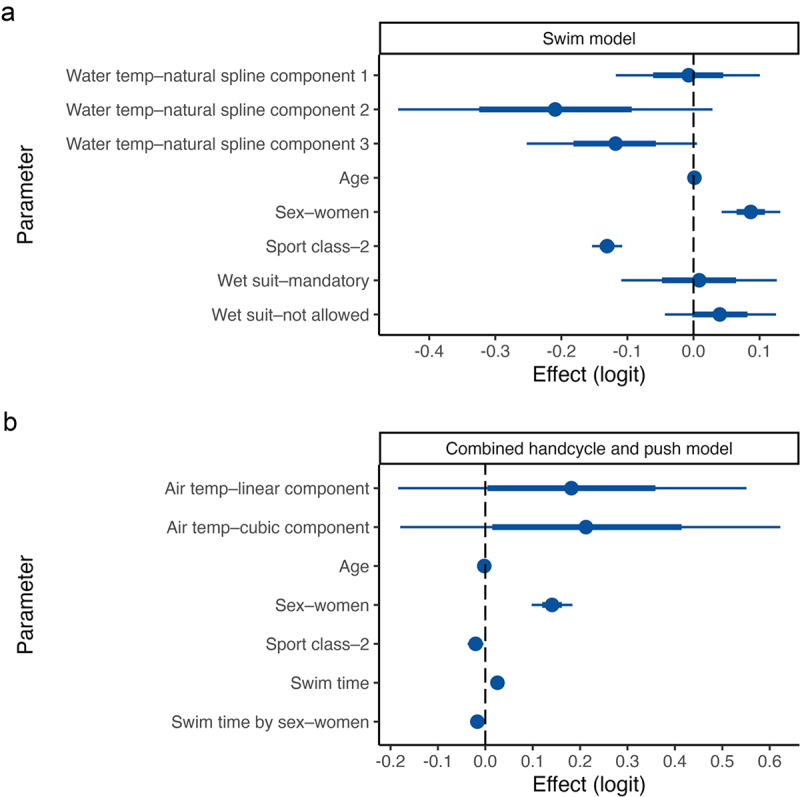
Posterior parameter estimates (logit scale) from the models of swim time (panel a), and handcycle and push time (panel b). The mean (circle) is shown with 66% (inner thick line) and 95% (outer thin line) credible intervals. Temp, temperature.
Figure 4.
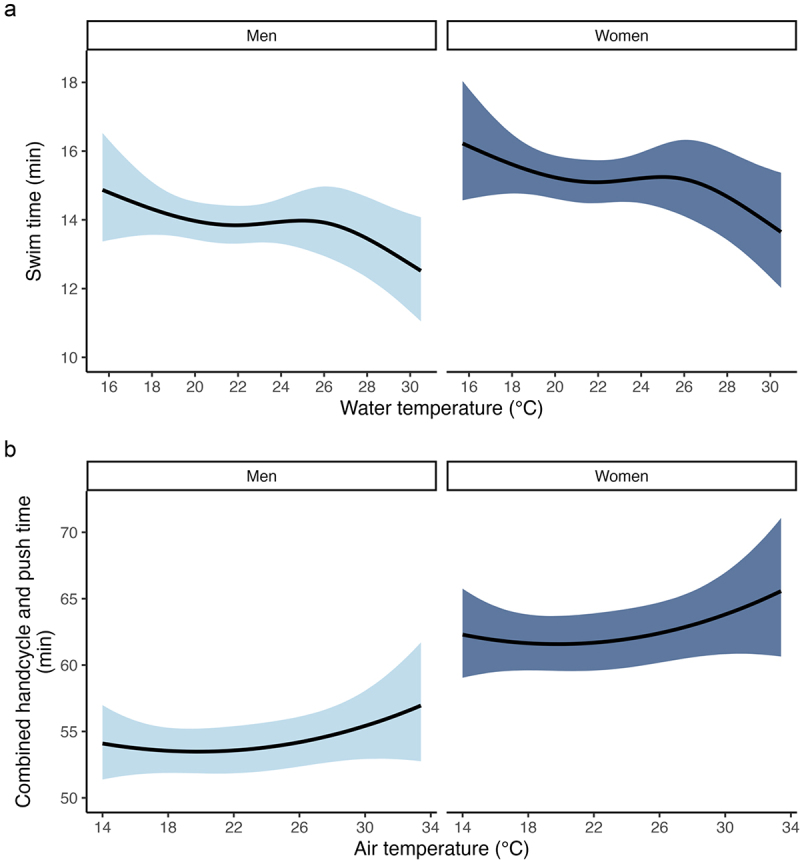
The relationship between water temperature and swim time (panel a) and air temperature and handcycle and push time (panel b). The solid black line indicates the marginal mean, and the ribbon indicates the 95% credible interval.
There were also effects of sex (Pr β > 0 = 1), age (Pr β > 0 = .971), and sport class (Pr β < 0 = 1) on swim time (Figure 3a). Females swam 01:15 min (95% CrI = 00:35, 01:50) slower than males. For each 1-year increase in age, the swim time increased (slowed) by 0.49 s (95% CrI = 0.48, 0.50). Class 2 athletes swam 01:42 min (95% CrI = 01:28, 02:08) faster than Class 1 athletes. It was unclear whether there was a wetsuit effect on swim time – the posterior probability that βmandatory and βnot allowed were greater than zero was 55.8% and 82% (Figure 3a).
Air temperature and combined handcycle and push time
It was unclear whether handcycle and push time increased (slowed) with increases in air temperature (Figures 3b and 4b). There was a 83.6% chance that the linear component was greater than zero (Pr β > 0 = .836), and an 84.8% chance that the cubic component was greater than zero (Pr β > 0 = .848; Figure 3b). A plot of individual athlete data is shown in Supplement 3 panel B.
There were also effects of sex (Pr β > 0 = 1), age (Pr β < 0 = 1), and sport class (Pr β < 0 = .992) on swim time (Pr β > 0 = 1), and sex by swim time (Pr β < 0 = 1) on handcycle and push time (Figure 3b). Handcycle and push time was 08:06 min (95% CrI = 05:30, 10:27) slower for females than males. For each 1-year increase in age, handcycle and push time decreased (improved) by 13.95 s (95% CrI = 13.93, 13.96). Class 2 athletes were 01:05 min (95% CrI = 00:14, 02:08) faster than Class 1 athletes.
Discussion
Our retrospective analysis of elite wheelchair triathlon competition data showed that warmer temperatures, up to 30.5°C, were associated with faster swim performances. It was unclear whether combined handcycle and push time slowed with increases in air temperature, up to 33°C. Athletes’ use of heat preparation strategies before races in warmer conditions, the presence of only mild heat stress, and/or convective cooling efficiencies may have contributed to the inconclusive result.
There was a marked difference in swim times between low (<18°C) and high (>26°C) water temperatures (Figure 4a). Faster performances in warmer water may be explained by an acute increase in physical function due to vasodilation and increases in muscle and tissue temperature. However, we could not find any evidence to support this statement. It is reasonable to assume that the warm-water benefit would be greatest for triathletes with health conditions where function is adversely affected by the cold, for example, cerebral palsy [23]. However, we found little evidence to suggest that sport class – in theory, a proxy of level of impairment – had a modifying effect on the relationship between water temperature and swim time (Supplement 4 panel A). In the interest of (not) overfitting the model [16], we did not include a temperature by sport class interaction.
As recommended [10,24], and based on previous studies [5,25], many athletes would have prepared for races in hot conditions by undertaking heat-based training. The use of heat preparation strategies along with more acute measures, such as pre-race ice-slurry ingestion, may have diminished the negative effect of heat on performance, leading to an unclear result [26,27]. The presence of only relatively mild heat stress could be another contributing factor. Water vapor pressure, a key component of environmental heat stress [28], was unknown. In active individuals, the risk of adverse heat effects begins to increase from WBGT 19–25.6°C [29]. These WBGTs could translate to a range of dry bulb temperature and relative humidity combinations. For example, assuming a solar load of 350 W/m2 and an airspeed of 5.5 m/s (20 km/h cycling with no wind), a WBGT of 24°C could translate to 24.5°C and 85%, or 35.4°C and 20%. Heat stress would be decreased in dry-warm conditions, due to the benefits of velocity-based (convective) cooling efficiencies during the handcycle and push segments [30,31]. Unfortunately, while World Triathlon uses a heat policy that relies on WBGT, these data were not reported in program notes.
There is a general lack of scientific literature concerning 1) the effect of heat on exercise and 2) the physiological risk of heat illness in the types of health conditions that affect triathletes using wheelchairs [3]. Evidence from indoor wheelchair rugby (air 18.4–20.9°C; 31–45% rh) indicates an inverse relationship between physical impairment and performance, such that athletes with severe physical impairments experience larger reductions in performance and greater thermal strain, due to their reduced heat loss capacity [32]. If the detrimental effect of heat on triathlon performance was associated with a level of impairment [32,33], it would stand to reason that Class 1 athletes (with the greatest impairments) may experience more pronounced heat-mediated declines in performance. However, we found little evidence to suggest that sport class had a modifying effect on the relationship between air temperature and performance (Supplement 4 panel B). We did not include an interaction between air temperature and sport class in our model, again to avoid overfitting [16].
Limitations
World Triathlon program notes included water and air temperature but not WBGT data. As WBGT considers air temperature, relative humidity, and solar radiant heat, the relationship between WBGT and handcycle and push time could be different to the relationship between air temperature and handcycle and push time. We did not have any information on athlete type and impairment, which could have a modifying effect on the relationship between water and air temperature and performance [34–36]. Triathletes using wheelchairs can wear wetsuit bottoms irrespective of the water temperature. This could explain why the effect of wetsuit on swim times was unclear.
Future directions
Future studies should integrate information on athlete impairment type and severity, with WBGT and performance data, to better understand how individual athlete performances fluctuate across environmental conditions. Such insights could be used to inform whether the time advantage received by Class 1 triathletes should vary as a function of the environmental conditions. While beyond the focus of the current study, we noted that the current World Triathlon heat policy used for Para athlete events is based on recommendations for non-disabled persons [8]. Future studies should explore whether a specific heat policy for Para triathletes is needed, tailored in a similar manner to the exertional heat stroke policy for Para athletes [37].
Conclusion
Our analysis showed that in elite wheelchair triathlon events, warmer water temperatures were associated with faster swim performances. The effect of hotter air temperatures on handcycle and push time was inconclusive. There was little evidence to suggest that sport class had a modifying effect on the relationship between temperature and performance, in either the swim, or the handcycle and push. Athletes’ use of heat preparation strategies before races in warmer conditions, mild heat stress, and/or velocity-based (convective) cooling efficiencies may explain the inconclusive result. The integration of information on impairment type and severity, with WBGT and athlete performance data is needed to provide greater insight into how the performances of triathletes who use wheelchairs fluctuate across environmental conditions.
Supplementary Material
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data and R code are available at the doi:10.5281/zenodo.10774736.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/23328940.2024.2391170
List of Abbreviations
- CrI
Credible interval
- df
Degrees of freedom
- Pr
Probability
- rh
Relative humidity
- SD
Standard deviation
- WBGT
Wet bulb globe temperature
Author contributions (using CRediT)
David Borg: Conceptualization; data curation; formal analysis; methodology; visualization; and writing – original draft and editing. Alexander Gibson: Conceptualization; methodology; and writing – review and editing. Aaron Bach: Methodology and writing – review and editing. Emma Beckman: Methodology and writing – review and editing. Sean Tweedy: Methodology and writing – review and editing. Ian Stewart: Conceptualization; methodology; supervision; and writing – review and editing.
References
- [1].Wecht JM, La Fountaine MF, Handrakis JP, et al. Autonomic nervous system dysfunction following spinal cord injury: cardiovascular, cerebrovascular, and thermoregulatory effects. Curr Phys Med Rehabil Rep. 2015;3(3):197–205. doi: 10.1007/s40141-015-0093-2 [DOI] [Google Scholar]
- [2].Christogianni A, Bibb R, Davis SL, et al. Temperature sensitivity in multiple sclerosis: An overview of its impact on sensory and cognitive symptoms. Temperature. 2018;5(3):208–223. doi: 10.1080/23328940.2018.1475831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Price MJ. Preparation of Paralympic athletes; environmental concerns and heat acclimation. Front Physiol. 2016;6:6:415. doi: 10.3389/fphys.2015.00415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Alkemade P, de Korte JQ, Bongers CC, et al. Humid heat equally impairs maximal exercise performance in elite para-athletes and able-bodied athletes. Med Sci Sports Exerc. 2023;55(10):1835–1844. doi: 10.1249/MSS.0000000000003222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Stephenson BT, Hoekstra SP, Tolfrey K, et al. High thermoregulatory strain during competitive paratriathlon racing in the heat. Int J Sports Physiol Perform. 2020;15(2):231–237. doi: 10.1123/ijspp.2019-0116 [DOI] [PubMed] [Google Scholar]
- [6].Logan-Sprenger HM. Fluid balance and thermoregulatory responses of competitive triathletes. J Therm Biol. 2019;79:69–72. doi: 10.1016/j.jtherbio.2018.12.003 [DOI] [PubMed] [Google Scholar]
- [7].World Triathlon . Competition rules 2023. https://www.triathlon.org/uploads/docs/World-Triathlon_Competition-Rules_2023_20221122.pdf
- [8].Armstrong LE, Casa DJ, Millard-Stafford M, et al. American college of sports medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572. doi: 10.1249/MSS.0b013e31802fa199 [DOI] [PubMed] [Google Scholar]
- [9].Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25(S1):6–19. doi: 10.1111/sms.12467 [DOI] [PubMed] [Google Scholar]
- [10].Griggs KE, Stephenson BT, Price MJ, et al. Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature. 2020;7(1):37–57. doi: 10.1080/23328940.2019.1617030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lee JY, Kim H, Gasparrini A, et al. Predicted temperature-increase-induced global health burden and its regional variability. Environ Int. 2019;131:105027. doi: 10.1016/j.envint.2019.105027 [DOI] [PubMed] [Google Scholar]
- [12].Torres EA. ITU paratriathlon history. Triathlon Med. 2020;391–392. [Google Scholar]
- [13].Harrison XA, Donaldson L, Correa-Cano ME, et al. A brief introduction to mixed effects modelling and multi-model inference in ecology. PeerJ. 2018;6:e4794. doi: 10.7717/peerj.4794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bell A, Jones K. Explaining fixed effects: random effects modeling of time-series cross-sectional and panel data. Polit Sci Res Methods. 2015;3(1):133–153. doi: 10.1017/psrm.2014.7 [DOI] [Google Scholar]
- [15].Yanagida T. Misty: miscellaneous functions. R package version 0.4.12. 2023. https://CRAN.R-project.org/package=m
- [16].Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66(3):411–421. doi: 10.1097/00006842-200405000-00021 [DOI] [PubMed] [Google Scholar]
- [17].Stan Development Team . Rstan: the R interface to Stan. R package version 2.21.2. 2020. http://mc-stan.org
- [18].Bürkner PC. Brms: an R package for Bayesian multilevel models using Stan. J Stat Soft. 2017;29(1):80:1–28. doi: 10.18637/jss.v080.i01 [DOI] [Google Scholar]
- [19].Wickham H, Averick M, Bryan J, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43):1686. doi: 10.21105/joss.01686 [DOI] [Google Scholar]
- [20].Borg DN, Nguyen R, Tierney NJ. Missing data: current practice in football research and recommendations for improvement. Sci Med Footb. 2022;6(2):262–267. doi: 10.1080/24733938.2021.1922739 [DOI] [PubMed] [Google Scholar]
- [21].Van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Soft. 2011;45(3):1–67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- [22].Shah AD, Bartlett JW, Carpenter J, et al. Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol. 2014;179(6):764–774. doi: 10.1093/aje/kwt312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Li S, Shin H, Zhou P, et al. Different effects of cold stimulation on reflex and non-reflex components of poststroke spastic hypertonia. Front Neurol. 2017;8:169. doi: 10.3389/fneur.2017.00169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gibson OR, James CA, Mee JA, et al. Heat alleviation strategies for athletic performance: A review and practitioner guidelines. Temperature. 2020;7(1):3–36. doi: 10.1080/23328940.2019.1666624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Alkemade P, Daanen HAM, Janssen TWJ, et al. Heat preparedness and exertional heat illness in Paralympic athletes: A Tokyo 2020 survey. Temperature. 2023;10(2):264–275. doi: 10.1080/23328940.2022.2147364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Castle PC, Kularatne BP, Brewer J, et al. Partial heat acclimation of athletes with spinal cord lesion. Eur J Appl Physiol. 2013;113(1):109–115. doi: 10.1007/s00421-012-2417-6 [DOI] [PubMed] [Google Scholar]
- [27].Stephenson BT, Tolfrey K, Goosey-Tolfrey VL. Mixed active and passive, heart rate-controlled heat acclimation is effective for Paralympic and able-bodied triathletes. Front Physiol. 2019;10:1214. doi: 10.3389/fphys.2019.01214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. doi: 10.1016/j.autneu.2016.03.001 [DOI] [PubMed] [Google Scholar]
- [29].Roberts WO, Armstrong LE, Sawka MN, et al. ACSM expert consensus statement on exertional heat illness: recognition, management, and return to activity. Curr Sports Med Rep. 2021;20(9):470–484. doi: 10.1249/JSR.0000000000000878 [DOI] [PubMed] [Google Scholar]
- [30].Saunders AG, Dugas JP, Tucker R, et al. The effects of different air velocities on heat storage and body temperature in humans cycling in a hot, humid environment. Acta Physiol Scand. 2005;183(3):241–255. doi: 10.1111/j.1365-201X.2004.01400.x [DOI] [PubMed] [Google Scholar]
- [31].Zhang Y, Bishop PA. Risks of heat illness in athletes with spinal cord injury: current evidence and needs. Front Sports Act Living. 2020;1:68. doi: 10.3389/fspor.2019.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Griggs KE, Havenith G, Price M, et al. Thermoregulatory responses during competitive wheelchair rugby match play. Int J Sports Med. 2017;38(3):177–183. doi: 10.1055/s-0042-121263 [DOI] [PubMed] [Google Scholar]
- [33].Griggs KE, Leicht CA, Price MJ, et al. Thermoregulation during intermittent exercise in athletes with a spinal-cord injury. Int J Sports Physiol Perform. 2015;10(4):469–475. doi: 10.1123/ijspp.2014-0361 [DOI] [PubMed] [Google Scholar]
- [34].Petrofsky JS. Thermoregulatory stress during rest and exercise in heat in patients with a spinal cord injury. Europ J Appl Physiol. 1992;64(6):503–507. doi: 10.1007/BF00843758 [DOI] [PubMed] [Google Scholar]
- [35].Price MJ. Thermoregulation during exercise in individuals with spinal cord injuries. Sports Med. 2006;36(10):863–879. doi: 10.2165/00007256-200636100-00005 [DOI] [PubMed] [Google Scholar]
- [36].Trbovich M, Ortega C, Schroeder J, et al. Effect of a cooling vest on core temperature in athletes with and without spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20(1):70–80. doi: 10.1310/sci2001-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Hosokawa Y, Adami PE, Stephenson BT, et al. Prehospital management of exertional heat stroke at sports competitions for Paralympic athletes. Br J Sports Med. 2022;56(11):11:599–604. doi: 10.1136/bjsports-2021-104786 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and R code are available at the doi:10.5281/zenodo.10774736.


