Abstract
Background
Perinatal loss is a severe stressor that usually triggers distressing symptoms of acute grief. Moreover, acute grief can worsen with time and become a chronic debilitating state known as complicated grief. However, there is a lack of comprehensive reviews on this topic. This systematic review aims to synthesize the existing literature on complicated grief following the perinatal loss.
Methods
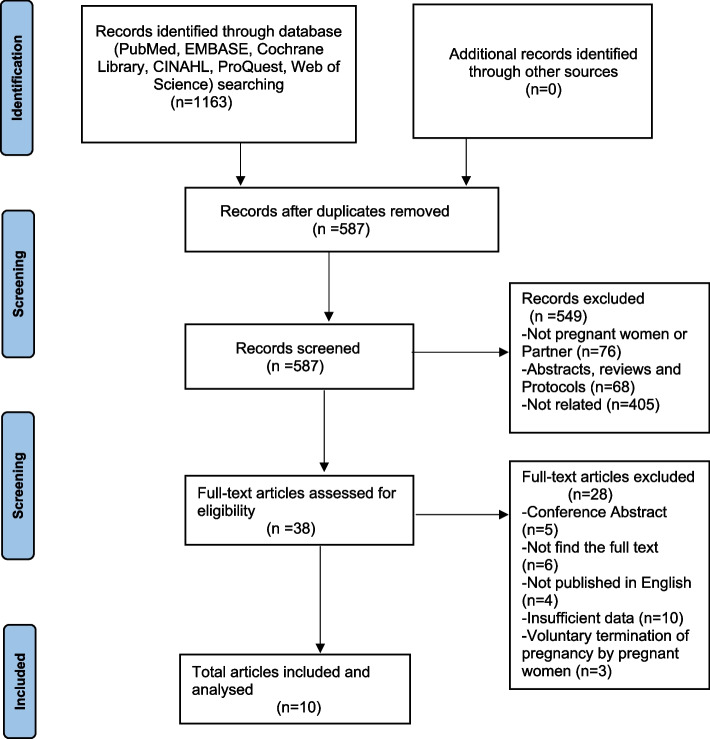
We systematically searched PubMed, Embase, Cochrane Library, CINAHL, ProQuest, and Web of Science to identify articles on complicated grief symptoms and influencing factors following perinatal loss. We performed a comprehensive, structured evaluation in full compliance with PRISMA guidelines.
Results
A systematic search produced 1163 results. Of these, 38 articles met the full-text screening criteria, and 10 pieces of literature met the inclusion criteria. Individuals may experience complicated grief following perinatal loss, manifesting in symptoms such as emotional reactions, physical responses, and social impairments. Furthermore, based on existing evidence, influencing factors include demographic characteristics, reproductive characteristics, marital relationships, social support, and coping strategies.
Conclusions
Complicated grief following perinatal loss is easily overlooked and has not been adequately studied. Further empirical research is needed to explore the symptoms and factors influencing this condition. A better understanding of complicated grief will help develop and optimize care strategies, informing future clinical practice and improving psychological support for individuals affected by perinatal loss.
Trial registration
PROSPERO registration number: CRD42023473510.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-06986-y.
Keywords: Perinatal loss, Complicated grief, Symptoms, Influencing factors, Systematic review
Introduction
Perinatal loss (PL) refers to pregnancy loss or neonatal death occurring between conception and 28 days after birth [1], including embryo damage, fetal death, miscarriage, stillbirth, neonatal death, etc. [2, 3]. It is estimated that nearly 7,000 stillbirths and 6,700 neonatal deaths occur daily worldwide, and 14%−20% of all pregnancies end in miscarriage [4, 5]. With medical advances, the incidence of perinatal loss has decreased in recent years, but 30% of women still experience perinatal loss [6].
The occurrence of perinatal loss is a devastating and traumatic event for parents, seriously affecting their physical and mental health [7]. Perinatal loss often occurs suddenly and unexpectedly. Compared with other bereavement events, in addition to immense grief, there are also many ambiguous and misunderstood situations. The pregnant woman may not know the exact time and cause of death, may be unable to disclose the details to others, and may have no specific person to mourn [8]. Additionally, there is a public misconception about perinatal loss, which is generally perceived by society as a ‘non-event’ or ‘just a miscarriage’, and the fetus as a ‘non-person’ [9]. Under the influence of many factors, perinatal loss tends to have a tremendous psychological impact on women and their family members, who may experience extreme sadness, irritability, shock, and emptiness [10]. Between 15–25% of parents experience symptoms such as anxiety [11], depression [12], or post-traumatic stress [13] following perinatal loss. When parents experience symptoms such as excessive worry, excessive self-blame, low mood, or excessive stress, they are identified after and caused by the loss, they are part of “complicated grief [14].” Complicated grief also increases the incidence of cardiovascular disease, diabetes, substance use, and suicide [8, 15, 16].
Grief occurs in all forms of loss, and ‘normal grief’ is a universal response to feelings of loss and is considered a physiological and instinctive response [17]. Although grief can be very painful, some people gradually regulate their emotions over time and adapt to the world in which the loss has occurred [18]. Yet, for many people, grief does not ease but remains intense and disabling, extending beyond the expected duration and course of the grieving process [19, 20]. In current research, we use complicated grief (CG) to refer to this ongoing grief response, which is also often known as prolonged grief (PG) or traumatic grief (TG), with CG being the most widely used term in the literature. It is more devastating and pervasive than 'normal grief,' and is characterized by persistent searching for and remembrance of the deceased, as well as intense and distressing emotions [21, 22]. CG describes a prolonged state of grief with a twelve-month duration criterion to ensure that ‘normal grief’ reactions in the acute post-bereavement state are not confused with complicated grief [23, 24], suggesting that the individual is unable to accept and release the death psychologically, and to integrate the death into life [25]. Currently, there is no consensus on the symptoms and influencing factors of CG, but it is a common and clinically significant disorder that represents a pathological grieving process [12, 26]. It is therefore not surprising that there is debate about CG in the medical and psychological literature, including its diagnostic classification and disease nomenclature. It is referred to as prolonged grief disorder (PGD) in the International Classification of Disorders (11th Edition) (ICD-11) [27], whereas the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5) called it persistent complex bereavement disorder (PCBD) [28].
Perinatal loss can be one of the most devastating events parents experience and may have serious long-term consequences for their mental health [29]. Kersting and Wagner [30] found that 25–30% of parents experience CG following perinatal loss. It is characterized by persistent, distressing, and debilitating symptoms, leading to physical, psychosocial, emotional, and cognitive changes. Lundorff et al. [31] identified CG as a bereavement-specific syndrome that requires targeted treatment. Currently, the understanding of complicated grief following perinatal loss remains uncertain and insufficient. Some studies have focused only on the symptoms and factors contributing to 'normal grief' without exploring those associated with complicated grief. Overall, according to the findings, a significant proportion of parents with perinatal loss have experienced CG [16, 25]. However, the symptoms of CG following perinatal loss and its influencing factors remain unclear. Through searches in relevant systematic review databases, we have not found any published or ongoing systematic reviews on this topic. To fill this gap, we conducted a systematic review of the relevant evidence in this field, aiming to comprehensively synthesize the symptoms of CG following perinatal loss and explore the influencing factors contributing to its development. This study can provide a theoretical foundation for preventing CG following perinatal loss, reduce the incidence of CG among parents after perinatal loss, and ultimately enhance their psychosocial outcomes.
The purpose of this study was to conduct a systematic review of the existing literature on CG following perinatal loss. Specifically, there were two research questions: 1) What are the symptoms of CG following perinatal loss? 2) What are the factors influencing CG following perinatal loss?
Methods
Preregistration
This study was preregistered in PROSPERO’s international registry of systematic reviews under registration number CRD42023473510. We complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis PRISMA guidelines [32].
Search strategy
We conducted literature searches in PubMed, EMBASE, Cochrane Library, CINAHL, ProQuest, and Web of Science databases between 17 October and 12 November 2023. The search time frame in electronic databases was limited within the period from database inception through 12 November, 2023, for published articles. A combination of keywords was used for searching, and relevant studies were traced and supplemented by consulting the reference list to ensure a complete search rate. The keywords searched were: perinatal loss OR fetal death OR perinatal death OR miscarriage OR stillbirth OR embryo damage OR neonatal death AND prolonged grief OR complicated grief OR traumatic grief OR delayed grief OR dysfunctional grief OR abnormal grief OR chronic grief OR distorted grief OR morbid grief OR maladaptive grief OR persistent complex bereavement-related disorder. Two researchers (X.Z and Y.C) performed the literature search independently. For detailed search strategies for each database, please see Supplementary File 1.
Inclusion and exclusion criteria
After the preliminary database search, two researchers (X.Z and Y.C) reviewed and screened the literature in two steps: 1) removing duplicate literature by reading the title and abstract and 2) reading the full text. Each potential literature was labeled as “included,” “excluded,” or “unclear,” and the presence of an “unclear” paper was judged and evaluated by a third researcher (T.Y.Z) and finally resolved through research group discussion. When full text was unavailable, we contacted the original authors to obtain it. Studies were selected according to the inclusion and exclusion criteria.
The inclusion criteria in this review include 1) original studies, peer-reviewed and formally published; 2) parents over 18 years of age who experienced perinatal loss (miscarriage, fetal death, stillbirth, neonatal death, etc.); 3) studies focusing on complicated grief in parents with perinatal loss. Exclusion criteria included: 1) study subjects with severe psychiatric disorders or comorbidities; 2) literature with missing data and duplicate publications; 3) books, conference abstracts, reviews, news, or research protocols; 4) studies published in languages other than English.
Data extraction and quality assessment
Two researchers (X.Z and Y.C) reviewed the selected papers and extracted the key information of the research into Excel files after discussion in the research group. The selected papers were then reviewed to identify the findings related to the two research questions. The relevant information was extracted into the Excel file under the following research title.
the symptoms of CG following perinatal loss
the influencing factors of CG following perinatal loss
For quality review purposes, two researchers (X.Z and Y.C) were assessed separately using the Critical Assessment Skills Programme (CASP) standards (https://casp-uk.net/). Each paper was reviewed and categorized as obvious or not obvious by the CASP criteria, and a third researcher (T.Y.Z) was asked if there was any disagreement. Papers were not excluded from this review, but the weighting of the body of literature was moderated.
Results
Literature search
According to the search strategy, 1163 articles were retrieved from six databases. After excluding studies that did not meet the inclusion criteria, 10 studies were finally included in the systematic review. The specific PRISMA flowchart is shown in Fig. 1.
Fig. 1.
PRISMA flow diagram of the studies screening process
Characteristics of included studies
The characteristics of the included studies are shown in Table 1. Studies were published between 2007 and 2023. A total of 10 articles from different countries were included in this systematic review: Australia (n = 2), USA (n = 2), Germany (n = 2), Spain (n = 1), France (n = 1), Brazil and Canada (n = 1), Denmark (n = 1). The sample was recruited primarily through perinatal loss support associations, hospitals, social media, letters, or snowball sampling. The number of participants in each study ranged from 10 to 831, with 2374 participants included in this review. Six of the studies specifically focused on mothers after perinatal loss [33–38], one on fathers [39], and three included both mothers and fathers [40–42].
Table 1.
Data extraction for included studies
| First author, year, country | Title | Methodology | Demographic characteristics | Symptoms | Influencing factors |
|---|---|---|---|---|---|
| Azeez et al., 2022, Australian [39] | Overwhelming and unjust: A qualitative study of fathers’ experiences of grief following neonatal death | Qualitative research design was used, and thematic analysis was adopted for data analysis | Participants for this study were ten Australian men and had experienced a neonatal death at least six months earlier. The aged range was 31–42 years (M = 35 years, SD = 3.46) | Highly emotional, grief on identity, physical symptoms (sleep disturbances, nightmares, stabbing pain, or general bodily pain), anger, sense of injustice | Gender role socialization, personality and culture, models of coping |
|
Buskmiller et al., 2023, USA [33] |
Validation of a Brief Measure for Complicated Grief Specific to Reproductive Loss | Cross-sectional study, The Brief Grief Questionnaire (BGQ) was used to describe grief after perinatal loss | 140 women, the aged range was 31.2–39.0 years (M = 35 years) | Emotional response, trauma symptoms, anxiety, depression | Reminder symptoms, the use of psychiatric medications, Suboptimal timing of the next pregnancy |
| Cassidy et al., 2023, Spain [40] | The Disenfranchisement of Perinatal Grief: How Silence, Silencing and Self-Censorship Complicate Bereavement (a Mixed Methods Study) | Based on an ethnographic and mixed-methods research design | Three heterosexual couples and seven women in heterosexual relationships | Undermining support, meaning-making and continuing bonds | The passing of time, competing discourses of loss, the biometrics of pregnancy, gendered ideas of reproduction and feeling rules, asymmetries in social power; social spheres, socio-materialities and performance/ritual, and structural aspects of social and familial organization |
| Grauerholz et al., 2021, United States [34] | Uncovering Prolonged Grief Reactions Subsequent to a Reproductive Loss: Implications for the Primary Care Provider | Qualitative research design was used, and summative content analysis was adopted for data analysis | 164 recent website blogs from female participants who self-reported having experienced a miscarriage or abortion in their lifetime | Ambiguity of the loss, lack of acknowledgment, and support from loved ones, maladaptive occupational adjustment, impact of multiple pregnancy losses | Subsequent relationship problems, substance misuse, depression, suicidal ideation, and PTSD |
| Kokou-Kpolou et al., 2018, France [35] |
Persistent depressive and grief symptoms for up to 10 years following perinatal loss: Involvement of negative cognitions |
Adopting a cross-sectional quantitative methodology | Sample included 98 bereaved mothers, all of French nationality. Their mean age was 33.89 years (range = 20–49 years, Mdn = 33) | Depressive symptoms, painful, prolonged and debilitating symptoms | Cause of the death, negative cognitions about the world, cognitions and type of death |
| Paris et al., 2016, Brazil and Canada [36] |
Factors associated with the grief after stillbirth: a comparative study between Brazilian and Canadian women |
This was a cross-sectional, descriptive, exploratory study | 26 women that experienced a stillbirth registered in the Mortality Information System (SIM), living in the Maringá, and 18 women that attended the Centre d’Études et de Recherche en Intervention Familiale (CERIF) in Canada | Intense, prolonged, distressing, disabling suffering; high anxiety and postpartum depression | Sociodemographic characteristics (age, religion, formal educational, paid job); reproductive characteristics (previous pregnancy with live-born baby; absence of occurrence of previous loss; and unintended pregnancy); marital satisfaction |
| McSpedden et al., 2017, Australia [37] | The presence and predictors of complicated grief symptoms in perinatally bereaved mothers from a bereavement support organization | The method of cross-sectional survey and questionnaire was adopted | A total of 121 mothers completed the questionnaire, ranging in age from 23 to 52 | Intense distress; a range of cognitive, emotional, and behavioral symptoms; and functional impairment, all persisting for at least 6 months | The presence of living children, loss of time to occur |
| Kersting et al., 2013, Germany [41] | Brief Internet-Based Intervention Reduces Posttraumatic Stress and Prolonged Grief in Parents after the Loss of a Child during Pregnancy: A Randomized Controlled Trial | Participants were recruited through a website, which presented general information about the intervention and its treatment modules, and outlined the study procedure | 228 parents were identified as eligible, gave their informed consent, and were randomized using a true random number service | Traumatic stress, separation distress, intrusions thoughts, avoidance behavior, and hyperarousal | Self-confrontation, cognitive restructuring, social sharing |
| Kersting et al., 2007, Germany [38] | Complicated grief after traumatic loss: A 14-month follow up study | A longitudinal study design was used in the study | 62 women who had undergone termination of pregnancy (TOP) | Grief related intrusions, behavior to avoid grief-related emotional stress, difficulties/failures to adapt to the loss | Strength of religious faith, extent of belief in necessity of psychotherapeutically support, extent of fear that the child is not healthy, wish for a child, extent of social support, and life time mental health |
| Mork et al., 2023, Denmark [42] | Grief trajectories after loss in pregnancy and during the neonatal period | Used questionnaire data from the Danish longitudinal cohort | Parents bereaved in pregnancy from 14 weeks of gestation, during birth, or within the first months after birth, included 676 parents | Intense emotional pain, a profound longing for and preoccupation with the deceased to an impairing degree for a duration of at least six months | Type of loss, gender, previous losses in pregnancy, and any living children |
Symptoms of CG following perinatal loss
Given the different perspectives of scholars on CG, it is important to focus on the symptoms of CG following perinatal loss. In the literature included in this study, a range of symptoms of CG following perinatal loss have been identified. Firstly, the delayed onset and intensity of grief following perinatal loss are emphasized as a significant symptom [43, 44]. Parents may experience prolonged and profound grief that may persist for 5–10 years after perinatal loss [35, 45]. Another prominent symptom following perinatal loss is emotional reactivity, including intense feelings of sadness, guilt, anger, anxiety, and depression [33, 35–39, 42]. These emotional responses often intertwine to form a complex and profound psychological burden, making it difficult for parents to escape from distress and turmoil [46, 47]. Feelings of guilt may stem from a sense of responsibility for the perinatal loss [35], and anger may arise from perceived injustices [39]. At the same time, anxiety and depression may represent doubts about the future and one’s self [33].
CG following perinatal loss not only manifests itself as symptoms in terms of emotional reactivity but may also trigger a range of physical responses. Many parents live in unending pain after loss, and this pain is not only psychological but may also translate into physical discomfort and symptoms, with physical discomforts such as sleep disturbances and stabbing pain [35, 39, 41]. Nightmares are also one of the common physical symptoms of CG following perinatal loss [19]. Parents may experience frequent nightmares that may be related to their lost child or scenes associated with the loss [42]. These nightmares may exacerbate their pain and grief.
In addition, social impairments are among the symptoms of CG of perinatal loss, including difficulties in communicating with others, interpersonal relationship disturbances, and the emergence of avoidance behaviors [38, 40, 41]. Parents may feel misunderstood and isolated as society often lacks understanding of the grief following perinatal loss [41]. This situation can lead to a range of avoidant behaviors and a reluctance to interact with others, resulting in difficulties integrating into everyday life. If this maladaptive state persists over a long period, it can affect family and intimate relationships, leaving them alienated and disturbed in their interactions with others [34].
Influencing factors of CG following perinatal loss
In general, there was some overlap in the included literature in terms of the factors influencing the perinatal loss of CG. Some of the factors influencing CG were derived from qualitative studies (n = 3) [34, 36, 39], and only one paper used questionnaire data from a large longitudinal cohort [42], limiting the applicability of this evidence. The specific factors included in the review are shown in Table 1.
After reviewing the research findings, we have identified that sociodemographic factors, including age, religious beliefs, level of education, and work, can have a certain impact on the development of CG following perinatal loss [35–38]. Individuals aged between 20 and 34 years, who have no religious beliefs, have completed 12 years or less of formal education, and are unemployed, tend to be more vulnerable to experiencing complicated grief following perinatal loss [35, 36]. Additionally, reproductive-related characteristics, such as gestational age, manner of loss, unintended pregnancy, prior experiences of related loss, and timing of subsequent pregnancies, are closely associated with the occurrence of CG following perinatal loss. The presence of living children is an important risk factor [37]. If the presence of a living child may affect the formation of CG to some extent, parents can often put their emotions on the line and place their relational points on other children [36]. CG is also exacerbated by gestation periods greater than 28 weeks [36], which may be related to the attachment relationships formed by the fetus.
There may be risk factors for CG associated with the perinatal loss itself. For example, marital relationships, especially after loss, have been repeatedly proposed as risk factors for CG [36, 40]. The quality of the marital relationship after loss may significantly impact an individual’s risk of CG [36]. Mutual support and understanding between spouses may ease the burden of grief and loss, whereas conflict, estrangement, or lack of mutual understanding may increase the risk of CG [41].
The formation of CG following perinatal loss is related to social support and coping strategies. Individuals who experience perinatal loss and receive adequate social support, including emotional support, informational support, and tangible assistance, are generally better able to cope with their sadness and loss [39–41]. Social support can alleviate feelings of loneliness and helplessness, assisting individuals in developing positive coping mechanisms [41]. Furthermore, the coping strategies adopted by individuals facing perinatal loss are crucial in the formation of CG [48]. Adopting proactive coping strategies, such as seeking social support and engaging in supportive activities, can help alleviate grief and anxiety, promote emotional regulation, and facilitate recovery [38].
Discussion
As far as can be ascertained, this is the first systematic review of the literature on CG following perinatal loss that systematically examines the symptoms and influencing factors. Different researchers have studied the symptoms and influencing factors of CG following perinatal loss. However, these studies have yet to form a comprehensive and systematic conclusion. Therefore, this study was designed to summarize the literature on the symptoms and factors influencing CG following perinatal loss using a systematic review approach, with the aim of providing an evidence-based foundation for the development of effective prevention and care interventions, as well as a scientific basis for improving psychological support and care for individuals following perinatal loss in future clinical practice.
A pertinent finding of this review is that parents experiencing perinatal loss have a higher frequency of CG than parents experiencing other types of grief [31, 34]. CG symptoms often persist for a long time, with some lasting up to 10 years or even a lifetime; it is characterized by a high degree of invisibility and diverse symptomatology [35]. CG symptoms following perinatal loss are not only emotional, including intense sadness, guilt, anger, anxiety, and depression [49], but also affect physical well-being. These symptoms can cause physical discomfort, such as sleep disturbances, tingling, and nightmares [50]. CG may also impact social interactions, leading to disconnection from family and friends [51, 52]. These physical and psychological effects can significantly reduce a person’s quality of life, affecting work, family and social life [53].
Currently, CG symptoms related to post-perinatal loss are often overlooked or misdiagnosed. Therefore, healthcare workers should pay particular attention to possible CG symptoms and perform a comprehensive assessment when evaluating parents following perinatal loss.
This systematic review found that perinatal loss of CG results from multiple interacting factors, including demographic characteristics, reproductive characteristics, marital relationships, social support, and coping strategies [40, 41]. Although these influences can be difficult to resolve and alleviate, understanding them can help us recognize and respond to CG. Among the identified influencing factors, coping strategies and social support are very important [30, 39]; they can provide emotional support, information, and guidance while reducing feelings of isolation [38]. This review initially integrated the factors influencing CG in perinatal loss. However, it is important to highlight that most of the risk factors discussed in the literature are not empirically supported, but theoretical. Large-scale empirical studies are needed to further elucidate the factors influencing CG following perinatal loss. Despite the shortcomings, the factors identified in the studies are instructive for clinical practice.
Given the diversity of individuals and socio-cultural factors, some understanding exists, but the factors influencing CG following perinatal loss require further exploration. This will help identify high-risk individuals and provide a basis for personalized preventive and intervention measures.
A growing body of evidence supports the hypothesis that people with perinatal loss are at risk of experiencing CG [1, 31, 38]. Importantly, it is considered to be a clinically relevant disorder [54]. CG, which prevents a person from returning to pre-social functioning, has been linked to psychological disorders and an increased risk of death [55]. It is also listed in the DSM-5 as persistent complex bereavement disorder (PCBD) [56]. This systematic review is based on case reports and perspectives that highlight the importance of focusing on CG in individuals with perinatal loss. However, in a systematic search of six databases, only ten papers met the inclusion criteria. This shows that this is an under-researched area. In particular, no studies with Chinese samples met the criteria. Following perinatal loss, parents are at a vulnerable time, experiencing physical, psychological and life-related stress [57]. If a person has experienced a perinatal loss, coping can become even more challenging and difficult [58]. Timely and accurate identification of symptoms and factors influencing CG following perinatal loss is clinically important in preventing its continuation. It can enable more effective support and interventions to assist parents through this difficult period and facilitate their recovery. Thus, we need larger, longitudinal, empirical studies to deepen our knowledge of this condition and provide evidence on the best ways to clinically support people experiencing perinatal loss with CG symptoms.
This systematic review also has some limitations. First, it only included peer-reviewed studies, excluding grey literature and unpublished studies, which may have led to the omission of some relevant information. Second, the study only searched for English articles and did not include studies published in other languages, which may have resulted in an incomplete literature search. Finally, to ensure comprehensiveness, this review included some studies with lower levels of evidence.
Conclusion
To summarize, this systematic review found that CG is indeed common in parents with perinatal loss. We note several key clinical findings, for the symptoms of CG following perinatal loss are diverse, not only in terms of emotional reactions, but also in terms of a certain degree of negative impact on physical health, and even in terms of impediments to normal social interactions; moreover, in addition to the general influencing factors, social support and coping strategies play an important role in influencing the situation. Currently, it is encouraging that an increasing number of studies have focused on CG following perinatal loss. Therefore, larger scale empirical studies are necessary to explore and study this population in depth, and to provide effective interventions in a timely manner.
Supplementary Information
Acknowledgements
We would like to thank the National Natural Science Foundation of China for its support of this work.
Authors’ contributions
XZ, TYZ conceived this study. XZ, YC, MZZ, MMY, MLW, TYZ contributed to final study design and data analysis. XZ, YC, MLW, TYZ completed abstract and full text review and data extraction. XZ, MLW, TYZ produced the first manuscript draft. All authors have read and approved the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No. 71974061).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tieying Zeng, Email: 984451641@qq.com.
Meiliyang Wu, Email: 1006862631@qq.com.
References
- 1.Donegan G, Noonan M, Bradshaw C. Parents experiences of pregnancy following perinatal loss: an integrative review. Midwifery. 2023;121:103673. [DOI] [PubMed] [Google Scholar]
- 2.Charrois EM, Bright KS, Wajid A, Mughal MK, Hayden KA, Kingston D. Effectiveness of psychotherapeutic interventions on psychological distress in women who have experienced perinatal loss: a systematic review protocol. Syst Rev. 2020;9(1):125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sereshti M, Nahidi F, Simbar M, Ahmadi F, Bakhtiari M, Zayeri F. Mothers’ perception of quality of services from health centers after perinatal loss. Electron Physician. 2016;8(2):2006–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, Flenady V, Froen JF, Qureshi ZU, Calderwood C, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387(10018):587–603. [DOI] [PubMed] [Google Scholar]
- 5.Zhuang SM, Chen MY, Ma XM, Jiang JJ, Xiao GH, Zhao YA, Hou JW, Wang YH. The needs of women experiencing perinatal loss: a qualitative systematic review and meta-synthesis. Women Birth. 2023;36(5):409–20. [DOI] [PubMed] [Google Scholar]
- 6.Blackmore ER, Côté-Arsenault D, Tang W, Glover V, Evans J, Golding J, O’Connor TG. Previous prenatal loss as a predictor of perinatal depression and anxiety. Brit J Psychiat. 2011;198(5):373–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanhope KK, Temple JR, Bann C, Parker CB, Dudley D, Hogue CJR. Variation in self-identified most stressful life event by outcome of previous pregnancy in a population-based sample interviewed 6–36 months following delivery. Soc Sci Med. 2021;282:114138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frost J, Bradley H, Levitas R, Smith L, Garcia J. The loss of possibility: scientisation of death and the special case of early miscarriage. Sociol Health Ill. 2007;29(7):1003–22. [DOI] [PubMed] [Google Scholar]
- 9.Bardos J, Hercz D, Friedenthal J, Missmer SA, Williams Z. A national survey on public perceptions of miscarriage. Obstet Gynecol. 2015;125(6):1313–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirui KM, Lister ON. Lived experiences of mothers following a perinatal loss. Midwifery. 2021;99:103007. [DOI] [PubMed] [Google Scholar]
- 11.Lee L, McKenzie-McHarg K, Horsch A. The impact of miscarriage and stillbirth on maternal-fetal relationships: an integrative review. J Reprod Infant Psyc. 2017;35(1):32–52. [DOI] [PubMed] [Google Scholar]
- 12.Hunter A, Tussis L, MacBeth A. The presence of anxiety, depression and stress in women and their partners during pregnancies following perinatal loss: a meta-analysis. J Affect Disorders. 2017;223:153–64. [DOI] [PubMed] [Google Scholar]
- 13.Bhat A, Byatt N. Infertility and perinatal loss: when the bough breaks. Curr Psychiatry Rep. 2016;18(3):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koopmans L, Wilson T, Cacciatore J, Flenady V. Support for mothers, fathers and families after perinatal death. Cochrane Database Syst Rev. 2013;6:CD000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huberty JL, Matthews J, Leiferman J, Hermer J, Cacciatore J. When a baby dies: a systematic review of experimental interventions for women after stillbirth. Reprod Sci. 2017;24(7):967–75. [DOI] [PubMed] [Google Scholar]
- 16.Eisma MC, Stroebe MS. Emotion regulatory strategies in complicated grief: a systematic review. Behav Ther. 2021;52(1):234–49. [DOI] [PubMed] [Google Scholar]
- 17.De Stefano R, Muscatello MRA, Bruno A, Cedro C, Mento C, Zoccali RA, Pandolfo G. Complicated grief: a systematic review of the last 20 years. Int J Soc Psychiatr. 2021;67(5):492–9. [DOI] [PubMed] [Google Scholar]
- 18.Farris D. The other side of sadness: what the new science of bereavement tells us about life after loss. Libr J. 2009;134(13):97–97. [Google Scholar]
- 19.Kersting A, Brähler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131(1–3):339–43. [DOI] [PubMed] [Google Scholar]
- 20.Majd M, Chen MA, Chirinos DA, Brown RL, Leroy AS, Murdock KW, Wu-Chung EL, Thayer JF, Fagundes CP. Trajectories of depressive symptoms early in the course of bereavement: patterns, psychosocial factors and risk of prolonged grief. Stress Health. 2024;40(3):e3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroebe M, Schut H, van den Bout J, editors. Complicated grief: scientific foundations for health care professionals. 1st ed. London: Routledge; 2013.
- 22.Prigerson HG, Vanderwerker LC, Maciejewski PK. A case for inclusion of prolonged grief disorder in DSM-V. In: Handbook of bereavement research and practice: advances in theory and intervention. American Psychological Association 2008: Washington D.C; 2008. p. 165–186. [Google Scholar]
- 23.Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, Raphael B, Marwit SJ, Wortman C, Neimeyer RA, et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11. Plos Med. 2009;6(8):e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mauro C, Reynolds CF, Maercker A, Skritskaya N, Simon N, Zisook S, Lebowitz B, Cozza SJ, Shear MK. Prolonged grief disorder: clinical utility of ICD-11 diagnostic guidelines. Psychol Med. 2019;49(5):861–7. [DOI] [PubMed] [Google Scholar]
- 25.Dodd A, Guerin S, Delaney S, Dodd P. Complicated grief: knowledge, attitudes, skills and training of mental health professionals: a systematic review. Patient Educ Couns. 2017;100(8):1447–58. [DOI] [PubMed] [Google Scholar]
- 26.Armstrong DS, Hutti MH, Myers J. The influence of prior perinatal loss on parents’ psychological distress after the birth of a subsequent healthy infant (vol 38, pg 654, 2009). Jognn-J Obst Gyn Neo. 2016;45(5):E67–9. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD). https://www.who.int/standards/classifications/classification-of-diseases.
- 28.Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington: American Psychiatric Association; 2013. [Google Scholar]
- 29.Doherty ME, Scannell-Desch E. Posttraumatic growth in women who have experienced loss of a child. Mcn-Am J Matern-Chil. 2021;46(5):264–70. [DOI] [PubMed] [Google Scholar]
- 30.Kersting A, Wagner B. Complicated grief after perinatal loss. Dialogues Clin Neurosci. 2012;14(2):187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O’Connor M. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disorders. 2017;212:138–49. [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buskmiller C, Grauerholz KR, Bute J, Brann M, Fredenburg M, Refuerzo JS. Validation of a brief measure for complicated grief specific to reproductive loss. Cureus. 2023;15(4):e37884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grauerholz KR, Berry SN, Capuano RM, Early JM. Uncovering prolonged grief reactions subsequent to a reproductive loss: implications for the primary care provider. Front Psychol. 2021;12:673050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kokou-Kpolou K, Megalakaki O, Nieuviarts N. Persistent depressive and grief symptoms for up to 10 years following perinatal loss: involvement of negative cognitions. J Affect Disord. 2018;241:360–6. [DOI] [PubMed] [Google Scholar]
- 36.Paris GFMF, Pelloso SM. Factors associated with the grief after stillbirth: a comparative study between Brazilian and Canadian women. Rev Esc Enferm USP. 2016;50(4):546–53. [DOI] [PubMed] [Google Scholar]
- 37.McSpedden M, Mullan B, Sharpe L, Breen LJ, Lobb EA. The presence and predictors of complicated grief symptoms in perinatally bereaved mothers from a bereavement support organization. Death Stud. 2017;41(2):112–7. [DOI] [PubMed] [Google Scholar]
- 38.Kersting A, Kroker K, Steinhard J, Ludorff K, Wesselmann U, Ohrmann P, Arolt V, Suslow T. Complicated grief after traumatic loss: a 14-month follow up study. Eur Arch Psychiatry Clin Neurosci. 2007;257(8):437–43. [DOI] [PubMed] [Google Scholar]
- 39.Azeez S, Obst KL, Due C, Oxlad M, Middleton P. Overwhelming and unjust: a qualitative study of fathers’ experiences of grief following neonatal death. Death Stud. 2022;46(6):1443–54. [DOI] [PubMed] [Google Scholar]
- 40.Cassidy PR. The disenfranchisement of perinatal grief: how silence, silencing and self censorship complicate bereavement (a mixed methods study). Omega (Westport). 2023;88(2):709–31. 10.1177/00302228211050500. [DOI] [PubMed] [Google Scholar]
- 41.Kersting ADR, Steinig J, Walter F, Kroker K, Baust K, Wagner B. Brief internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: a randomized controlled trial. Psychother Psychosom. 2013;82(6):372–81. [DOI] [PubMed] [Google Scholar]
- 42.Mork S, Hvidtjorn D, Moller S, Henriksen TB, O’Connor M, Bonanno GA. Grief trajectories after loss in pregnancy and during the neonatal period. J Psychiatr Res. 2023;168:293–9. [DOI] [PubMed] [Google Scholar]
- 43.Enez O. Complicated grief: epidemiology, clinical features, assessment, and diagnosis. Curr Approaches Psychiatry. 2018;10(3):269–79. [Google Scholar]
- 44.Berry SN, Winsor T, Huene L. A proposed framework for perinatal loss trauma informed care. J Neonat Nurs. 2023;29:916–21. 10.1016/j.jnn.2023.08.004. [Google Scholar]
- 45.Wakefield JC. Should prolonged grief be reclassified as a mental disorder in DSM-5? J Nerv Ment Dis. 2012;200(6):499–511. [DOI] [PubMed] [Google Scholar]
- 46.Dodd A, Guerin S, Delaney S, Dodd P. Psychiatrists’, psychologists’ and counselors’ attitudes regarding complicated grief. J Affect Disord. 2019;256:358–63. [DOI] [PubMed] [Google Scholar]
- 47.Kishimoto M, Yamaguchi A, Niimura M, Mizumoto M, Hikitsuchi T, Ogawa K, Ozawa N, Tachibana Y. Factors affecting the grieving process after perinatal loss. BMC Womens Health. 2021;21(1):313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jones K, Robb M, Murphy S, Davies A. New understandings of fathers’ experiences of grief and loss following stillbirth and neonatal death: a scoping review. Midwifery. 2019;79:102531. [DOI] [PubMed] [Google Scholar]
- 49.Mughal S, Azhar Y, Mahon MM, Siddiqui WJ. Grief Reaction and Prolonged Grief Disorder. 2023 Nov 14. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed]
- 50.Hilberdink CE, Ghainder K, Dubanchet A, Hinton D, Djelantik AAAMJ, Hall BJ, Bui E. Bereavement issues and prolonged grief disorder: a global perspective. Glob Ment Health (Camb). 2023;10:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Toedter LJLJ, Alhadeff JM. The perinatal grief scale: development and initial validation. Am J Orthopsychiatry. 1988;58(3):435–49. [DOI] [PubMed] [Google Scholar]
- 52.Hutti MH, Armstrong DS, Myers J. Evaluation of the perinatal grief intensity scale in the subsequent pregnancy after perinatal loss. J Obstet Gynecol Neonatal Nurs. 2013;42(6):697–706. [DOI] [PubMed] [Google Scholar]
- 53.Fernández-Sola C, Camacho-Avila M, Hernández-Padilla JM, Fernández-Medina IM, Jiménez-López FR, Hernández-Sánchez E, Conesa-Ferrer MB, Granero-Molina J. Impact of perinatal death on the social and family context of the parents. Int J Environ Res Public Health. 2020;17(10):3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Doering BK, Eisma MC. Treatment for complicated grief: state of the science and ways forward. Curr Opin Psychiatr. 2016;29(5):286–91. [DOI] [PubMed] [Google Scholar]
- 55.Fernández-Ordoñez E, González-Cano-Caballero M, Guerra-Marmolejo C, Fernández-Fernández E, García-Gámez M. Perinatal grief and post-traumatic stress disorder in pregnancy after perinatal loss: a longitudinal study protocol. Int J Environ Res Public Health. 2021;18(6):2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, Reynolds C, Lebowitz B, Sung S, Ghesquiere A, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Papapetrou CPK, Mourouzis I, Kouzoupis A. Pregnancy and the perinatal period: the impact of attachment theory. Psychiatriki. 2020;31(3):257–70. [DOI] [PubMed] [Google Scholar]
- 58.Ghesquiere A, Bagaajav A, Metzendorf M, Bookbinder M, Gardner DS. Hospice bereavement service delivery to family members and friends with bereavement-related mental health symptoms. Am J Hosp Palliat Care. 2019;36(5):370–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.