Abstract
Background
Frontline clinics - primary care clinics that predominantly serve low-income and socially disadvantaged communities - are facing increasing impacts from climate-related extreme events. This study evaluated staff perspectives at frontline clinics on the health risks of climate change, the impacts of extreme events on their clinics and patients, and their motivators to improve climate resiliency.
Methods
A national, cross-sectional survey was conducted of staff working at frontline clinics including administrators, case workers, and providers across the United States. Survey questions assessed clinic and respondent attributes, knowledge of health risks of climate change, preferences for climate change educational and operational resources, and clinic and patient climate impacts and resilience. The survey was distributed electronically to a convenience sample of primary care clinics and to the National Association of Community Health Centers (NACHC) and National Association of Free and Charitable Clinics (NAFC) listservs. Data was collected from September to November of 2021. Respondents were current staff who consented to the survey. Responses were collected via Qualtrics, and the statistical analysis was completed using Stata.
Results
A total of 430 surveys were completed representing clinics in 43 states. Most (82.0%) respondents reported human activities were causing climate change. Over half (52.8%) of respondents reported an operational disruption to their clinic from extreme events in the past 3 years, and another 54.4% had plans in place to address risks from extreme events. The most useful resources identified to improve operational resilience were checklists and planning guidance. Over half (52.0%) of respondents reported they were motivated to use these resources to improve clinic preparedness. Most (84.4%) providers and case workers reported that climate change impacted patient health, however only 36.2% discussed health risks with patients, with barriers including more pressing topics and time available. Another 55.7% of respondents reported they were motivated to learn ways to help patients prepare for extreme events.
Conclusions
Climate-related extreme events were reported to impact patient health and disrupt frontline clinic operations. Overcoming gaps in knowledge about climate change impacts on health and providing climate educational resources can engender motivation to improve clinic and patient resilience to climate change.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-024-02622-y.
Keywords: Clinic resilience, Primary health, Climate change, Extreme weather, Educational resources, Healthcare delivery
Background
Climate change is contributing to a greater intensity of extreme events, including heat, hurricanes, floods, droughts, and wildfires [1]. All of these events have direct and indirect impacts on health, contributing to excess morbidity and mortality [1, 2]. Climate change impacts everyone’s health, however certain populations – such as low-wealth individuals, those with chronic medical conditions, and racial and ethnic minorities – are disproportionately affected [3–5]. Moreover, climate change related extreme events are contributing to disruptions in healthcare access and delivery, magnifying existing health inequities [4–7]. Improving the climate resilience of health care – and in particular, frontline clinics, that provide care for communities most at-risk – has become increasingly urgent as climate hazards intensify. To that end, this study aims to identify frontline clinic staff knowledge on climate and human health, the impacts and resilience of their clinics and their patients to extreme events, and motivators to improve clinic and patient climate resilience.
Health care resilience to climate change is often considered in the context of cascading impacts to operations, such as providing continuity of care through supply chain shortages, power outages, or facility damage. Many organizations have released climate resilient healthcare guidance, from the World Health Organization’s Operational Frameworks [8, 9] to the United States (U.S.) Department of Health and Human Services’ Sustainable and Climate-Resilient Health Care Facilities Toolkit and Compendium [10, 11], and Health Care Without Harm’s Report on Strategies and Case Studies [12]. These tools provide essential administrative support and guidance but lack the individual perspectives of the staff who work in the healthcare facilities, and often focus on hospitals rather than primary care clinics, where the most at-risk populations frequently receive their care.
This survey elucidated perspectives of staff working at frontline clinics; here, we refer to frontline clinics as primary care clinics that predominantly serve low-income and socially disadvantaged communities, including Federally Qualified Health Centers (FQHCs), Free and Charitable Clinics (FCCs), and community-based primary care health clinics. Frontline clinics form an essential component of healthcare, providing safety net care to those who otherwise may have limited access to health care, regardless of their ability to pay [13–16]. FQHCs and FCCs together care for more than 35 million people annually in the United States [17, 18]. While approximately 59% of patients receiving care at FQHCs are publicly insured [17], FCCs often do not take federal insurance, and therefore are not included under Center for Medicare and Medicaid Services (CMS) regulations for emergency preparedness planning [19]. These clinics form the frontlines of health care, serving the populations most at risk from climate change.
Given frontline clinics facilitate access to health care for at-risk communities, the resilience of these clinics in the face of climate change is essential to providing consistent, affordable, and accessible health care. Not just in the United States, but globally, primary care clinics form the frontlines of climate resilience by ensuring access to health care for at-risk communities [20–22]. Frontline workers often refer to those who provide direct services to consumers, and comprise a multitude of professions, from police officers to janitors and maintenance workers [23]. Within health care, frontline workers often refers to those directly caring for patients – doctors and nurses as well as nursing assistants and home health aides [23]. We refer here to frontline clinics as the primary care clinics that directly care for those communities most at-risk. However, we evaluated all staff working at the clinics – not just the providers and case workers directly interacting with patients, but also the administrators and managers who play different yet critical roles in the functioning of these clinics. The entire staff who work in frontline clinics have rarely been included in research to understand their views on climate change, the health impacts of climate change on the patients they serve, and how to best prepare their clinics for extreme events.
Previous studies have evaluated the knowledge and attitudes of medical providers, typically focusing on whether humans were causing climate change and whether climate change affects health [24–28]. Predictors of physician communication and engagement about climate change are also beginning to be investigated; physician knowledge of effects of climate on health and personal beliefs have been associated with communicating about climate change with patients and with policy engagement [27–29]. Studies have also underscored the need to better understand what healthcare systems can do to improve their resilience to climate change [24, 27, 28]. However, we still do not fully understand what motivates the full range of staff working in frontline clinics to communicate climate risks with patients or what motivates them to improve clinic climate resilience.
Here, we report results from a national survey of all staff working at frontline clinics to address this research gap. The survey evaluated staff knowledge and attitudes on climate change and health risks, the impacts and resilience of extreme events on their patients and clinics, how best to communicate climate risks, and motivation to use climate resilience resources.
Methods
Survey methodology
A cross-sectional observational survey was conducted in collaboration between Harvard T.H. Chan School of Public Health’s Center for Climate, Health, and the Global Environment (C-CHANGE) and Americares, a 501(c)3 relief and development nonprofit organization that improves health for people affected by poverty or disaster.
Survey design
The overarching goal of the survey was to inform future development of resources for frontline clinic staff by the partner organizations to improve clinic resilience and communication of climate-related risks with patients. To this end, the survey was conceived to elicit, among all staff at frontline clinics, their knowledge on climate and human health, the impacts and resilience of their clinics to extreme events, and their motivators to improve clinic resilience. An additional subset of questions for only patient-facing staff asked about patient climate impacts, resilience, and how to best communicate climate risks with patients.
Survey questions were drafted by three subject matter experts as part of a pilot study in 2021 and then iteratively refined through three cycles of review by a team of six staff from Harvard C-CHANGE and Americares with expertise in health systems, disaster response, climate change, and survey design for the current study.
Survey distribution
The survey was distributed via emails addressed to clinics rather than individuals, with the goal of reaching all staff rather than specific individuals or roles. A convenience sample of clinics was reached using snow-ball sampling. The survey email invitation was sent to the Americares, the National Association of Community Health Centers (NACHC) and the National Association of Free and Charitable Clinics (NAFC) clinic networks listservs, that in total represent over 3,500 clinics and 450,000 healthcare workers nationwide [17, 18]. The survey was administered electronically from September 15, 2021, to November 15, 2021. Responses were collected via a secured Qualtrics survey. Responses were reviewed for duplicates based upon unique Internet Protocol (IP) address.
Survey content
The survey questions were divided into three sections for all respondents. The first section asked about clinic and respondent demographic characteristics. The clinic demographic characteristics included: clinic location, clinic type, clinic staff size and if the clinic was part of a larger network. The respondent demographics included: years in practice, years at the clinic, and role at the clinic. The self-selected roles were: (1) administrator, (2) case worker, (3) provider, and (4) “other”. The administrator category included all types of self-selected administrators. The case worker category included case workers, social workers, and case managers. The provider category included physicians, physician assistants, nurse practitioners, registered nurses, licensed practical nurses, pharmacists, and physical and occupational therapists. The “other” category was self-selected, and respondent’s own job descriptions included: dental staff, pharmacy staff, medical assistants and clinic support staff, patient representatives, advocates and access coordinators, clinic and nurse managers, facility and operations managers, program evaluators, safety officers, risk managers, emergency managers, and volunteers.
The second section covered staff knowledge and attitudes on climate change and human health impacts. This included: if human activities are causing climate change, knowledge of climate impacts on health and medical conditions, and concern for impacts of extreme events on their jobs.
The final section asked questions about clinic resilience to climate change-associated extreme events and motivation to use resilience resources. This included: if and how extreme events disrupted clinical care, plans to address these disruptions, clinic’s greatest needs during extreme events, potential resources to improve clinic resilience, and motivation to use these resources.
An additional subset of questions was asked only to self-identified providers and case workers. These questions covered climate impacts and resilience of patients and communication of climate risks with patients. This included: if and how extreme events harmed patient health, patients’ needs during extreme events, confidence in plans to protect patients from extreme events, if and what climate risks were discussed with patients, and barriers to communication. Additionally, these questions included preferred climate and health subjects, tools to educate patients and staff, and motivation to use these tools and prepare patients for extreme events.
All but the first section (which included only categorical questions) included both nominal categorical questions with a range of 2–18 categories and ordinal Likert scale questions, which were coded 1–5. The survey instrument is available as Additional File 2: Survey Questionnaire.
Survey measures
Outcome variables: The three outcome variables were motivation of staff to use clinic resilience resources, motivation of providers and case workers to use resources to help patients prepare for extreme events, and if providers and case workers discuss climate change with patients. These outcomes were selected based upon the previously determined need to identify ways to improve clinic resilience, motivation to use resources, and communication about climate change with patients [24, 27, 28]. Motivation was dichotomized with reported categories of 1–3 (not at all, a little, and somewhat motivated) considered “not motivated” and categories 4–5 (fairly and very motivated) considered “motivated.” Discussion of climate change was a binary outcome variable.
Independent variables: Belief that humans are causing climate change was a binary variable. The other independent variables (knowledge of climate effects on health, concern for extreme weather impacting job, belief that climate impacts patient health and confidence in developing disease management plans) were interval Likert scale responses from 1 to 5. Years of experience was a categorical variable divided into 5 categories. The odds ratios presented represent changes based upon a 1-unit change in the Likert scale [30]. Independent variables were based on subject matter expertise and prior studies [27–29].
Statistical analysis
Descriptive statistics were used to describe health center and respondent attributes, their climate change perceptions, and resilience of clinics for all respondents. Additionally, descriptive statistics were used for the subset of questions asking providers and case workers to identify preferred resource types for communicating and educating about climate resilience for their clinics.
All responses were cleaned for missingness, and only complete responses were used in the predictive analysis. Logistic regression was performed to determine the odds of the identified outcomes based on independent variables. All analysis was performed using Stata version 18.0 (College Station, Texas) [31].
Results
Survey response information
A total of 495 respondents consented to complete the survey. Respondents who only completed the introductory clinic and respondent demographic questions (approximately 20% of the survey) were excluded from analysis, leaving 430 survey responses included in the analysis.
The respondents’ roles included Administrators (39.8%), Case Workers (3.9%), Providers (30.0%) and Other (26.3%). The respondents’ clinics were from 43 states, with the highest proportions in California, New York, and Florida; 418 unique zip codes were represented. States representing 3% or more of respondents are listed in Table 1; the Other State category includes all of the remaining states with the full list provided in Additional File 1: Appendix. Of the clinics, 59.8% were Federally Qualified Health Centers (FQHCs) or Community Health Centers (CHCs), and 45.8% were Free and Charitable Clinics (FCCs); respondents could choose more than one option. Respondent characteristics are summarized in Table 1.
Table 1.
Demographic characteristics of respondents and clinics
| Characteristics of respondents | n (%) | Characteristics of clinics | n (%) |
|---|---|---|---|
| Respondent role | Clinic location | ||
| Administrators | 171 (39.8) | California | 98 (23.4) |
| Case Workers | 17 (3.9) | New York | 63 (15.1) |
| Providers | 129 (30.0) | Florida | 59 (14.1) |
| Other | 113 (26.3) | North Carolina | 33 (7.9) |
| Years in practice | Massachusetts | 27 (6.5) | |
| Less than 5 | 76 (17.7) | Texas | 13 (3.1) |
| 5–10 | 78 (18.1) | Other State | 125 (29.9) |
| 10–15 | 74 (17.2) | Clinic type | |
| Greater than 15 | 202 (47.0) | FQHC/CHC | 257 (59.8) |
| Years at clinic | FCC | 197 (45.8) | |
| Less than 5 | 171 (39.8) | Clinic Staff Size (mean +/- SD) | 65.8 +/- 35.1 |
| 5–10 | 121 (28.1) | Part of larger clinic network | |
| 10–15 | 62 (14.4) | Yes | 233 (54.2) |
| Greater than 15 | 76 (17.7) | No | 197 (45.8) |
Legend Response total (n) and percentage (%). For clinic staff size, all clinics with over 100 staff were counted as 100. FQHC refers to Federally Qualified Health Centers, CHC to Community Health Centers and FCC to Free and Charitable Clinics
Climate change and health knowledge and perceptions
Most (82.0%) respondents reported they believe that human activities are causing climate change, with similar responses across roles at clinics. Only 21.3% of respondents reported they knew “a good deal” or “a lot” about climate change effects on health, with one quarter (24.8%) reporting knowing “nothing at all” or “hardly anything.” Respondents identified specific medical conditions connected to climate change including chronic respiratory illnesses (92.2%), heat stroke (72.8%), skin cancer (62.2%), anxiety disorders (61.9%), and hay fever (51.3%). The full response list is available in Additional File 1: Appendix.
Approximately one quarter (25.4%) of respondents reported moderate or extreme concern about the effects of extreme weather on their ability to perform their job, a little less than a quarter (22.0%) reported they were somewhat concerned, and a little over half (52.6%) reported they were not at all or only slightly concerned.
Clinic climate resilience
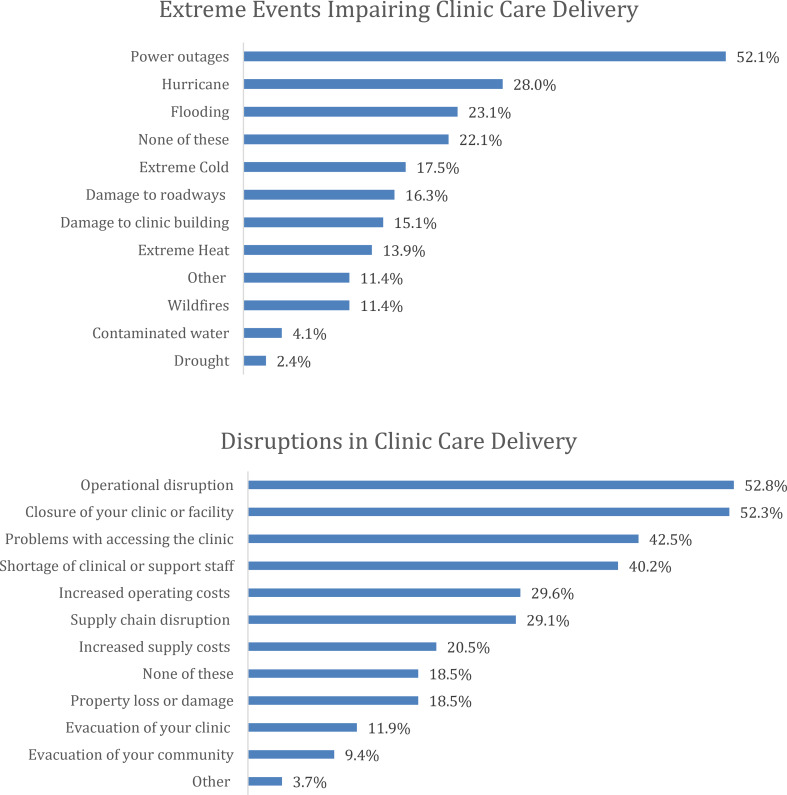
In the past three years, respondents reported their clinics experienced extreme events that caused disruptions in care. This question asked about both care delivery disruptions directly from extreme events (i.e., hurricanes and floods) as well as secondarily from cascading events (i.e., power outages and road damage). Clinics reported experiencing events including power failures (52.1%), hurricanes (28.0%), and floods (23.1%). An additional question elucidated just the cascading impacts of the extreme events on clinic operations. Participants reported disruptions from the extreme events including operational disruptions such as power outages (52.8%), closures of clinics (52.3%), problems with access to the clinic (42.5%), and staff shortages (40.2%); full results in Fig. 1.
Fig. 1.
Types of extreme events reported by respondents to impair clinic care delivery (including both direct impacts from extreme events and cascading impacts) and reported disruptions in clinic care delivery after extreme events. Legend Respondents could select multiple events and disruptions, total percentages presented, events occurred over the past 3 years
Respondents also noted that extreme weather contributed to loss or spoilage of vaccines (15.8%), medications (11.8%), and shortages of personal protective equipment (18.5%).
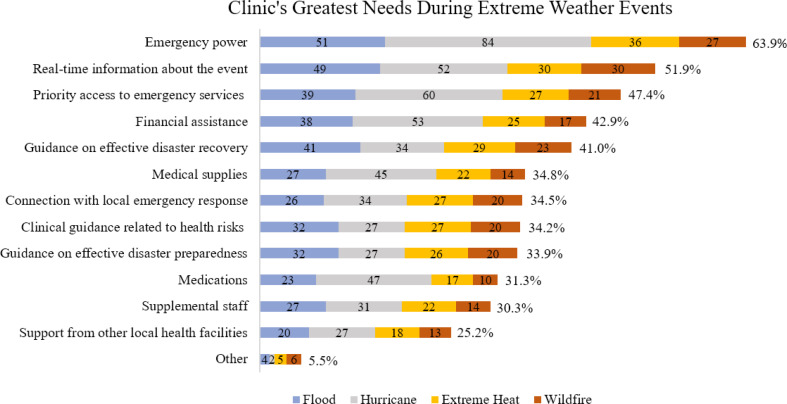
Just over half (54.4%) of respondents reported they have plans in place to address risks to healthcare access and delivery during extreme weather. Over half (57.4%) of respondents identifying that they work at a FQHC or CHC, and nearly half (49.6%) of respondents identifying that they work at a FCC, reported having plans in place for healthcare access and delivery during extreme events, although many were unsure (24.5% and 32.4%, respectively). The greatest need of clinics before, during, and after extreme weather events identified by respondents was emergency power, with additional clinic needs reported during these events including real-time information related to the impacts of the event, access to emergency services and financial assistance; full results in Fig. 2.
Fig. 2.
Clinics reported greatest needs during all extreme weather events. Legend Respondents could choose more than one event; percentages for all types of events combined (% at right of bar graph) are presented, as well as disaggregated into response counts for each extreme event type (#s overlying bar sections; total responses varied by event type). “Priority access to emergency services” refers to priority restoration of critical utilities (i.e., restoration of electricity)
Clinic resources to improve resilience
Respondents identified checklists (60.2%), planning guidance (56.0%), plan or policy templates (54.0%), brief information sheets (51.0%), direct training of staff (50.2%), discussion-based exercise scenarios (36.6%), short videos (32.1%) and train-the-trainer guidance (31.3%) as resources that would be useful to improve clinic operational resilience.
Approximately half (52.2%) of respondents reported they would be fairly or very motivated to use resources to improve climate change clinical preparedness.
Patient climate impacts and resilience
A subset of survey questions was asked solely to providers and case workers who directly interact with patients (N = 141). In the past three years, respondents stated that extreme heat (63.4%), power outages (45.0%), and extreme cold (32.8%), among other events, had harmed their patients’ health (Additional File 1: Appendix). Respondents stated their patients’ needs during extreme events included shelter (80.5%), food (60.3%), transportation assistance (58.0%), medications (56.3%), financial assistance (50.0%), medical supplies (39.7%) and real time information (36.2%). Needs disaggregated by extreme event type are outlined in Additional File 1: Appendix.
Of all providers and case workers, approximately one quarter (25.5%) reported they were at least fairly confident in their ability to develop disease management plans to protect their patients from extreme weather, another third (29.8%) reported they were somewhat confident, and 44.7% reported they were not confident in developing disease management plans to protect patients.
Communicating climate health risks with patients
Most providers and case workers (84.4%) reported that they believe that climate change affects patient health, with 5.7% stating it does not. About one-third (36.2%) reported discussing health risks of climate change with patients. The most discussed risks were extreme heat (78.4%), worsening allergy seasons (66.7%), and air pollution (60.8%); full risks in Additional File 1: Appendix. The greatest barriers identified to patient communication included more pressing topics (81.3%), time available in the clinical encounters (67.9%), and knowledge about climate change and health (61.2%). Fewer respondents reported the barriers of controversy/politicization of climate change (33.6%), not part of the clinical encounter (26.9%), not part of my responsibility (23.9%), perception of peers (18.7%), and personal/professional risk (17.9%).
Respondents stated they were most interested in the climate and health subjects of air quality (70.7%), health care access (63.9%), health equity (59.4%), mental health (59.4%) and heat exposure (58.6%); full list is available in Additional File 1: Appendix. Preferred patient educational tools included brief information sheets, pamphlets and ready to use social media content. Preferred clinic staff educational tools also included brief information sheets as well as short informational videos and online learning modules (Table 2).
Table 2.
Climate and health educational tools reported by providers and case workers to be of interest for patients and clinical staff
| Patient tools | N | % | Clinical staff tools | N | % |
|---|---|---|---|---|---|
| Brief information sheets | 107 | 81.1% | Brief information sheets | 88 | 66.7% |
| Pamphlets | 63 | 47.7% | Short informational videos | 64 | 48.5% |
| Ready to use social media content | 51 | 38.6% | Online learning modules | 63 | 47.7% |
| Short videos | 50 | 37.9% | Electronic record checklists or templates | 60 | 45.4% |
| Group session guides | 21 | 15.9% | Written checklists | 59 | 44.7% |
| Other | 8 | 6.1% | Clinical encounter discussion prompts | 52 | 39.4% |
| In-person workshops | 36 | 27.3% | |||
| Other | 5 | 3.8% |
Legend Respondents could select multiple educational tools
Over half (55.7%) of respondents reported that they were extremely or very motivated to learn ways to help patients prepare for extreme weather, 47.3% reported they were extremely or very motivated to learn about climate change and health, and another 41.0% reported they were extremely or very motivated to help their patients learn more about climate change and health.
For emergency communication with patients during extreme weather events, respondents reported the most often used techniques were phone calls and secure text messaging; the same techniques were reported as the most effective ways of communicating in an emergency. The full list is available in Additional File 1: Appendix.
Predictors of motivation to use clinic resilience resources and to discuss climate change
Respondents who reported that they believed humans are causing climate change had 4.39 times greater odds of reporting motivation to use clinic resilience resources than those who did not report the belief that humans are causing climate change. Conversely, reporting the belief that humans are not causing climate change reduced the odds by 77% of reported motivation to use clinic resilience resources. For each interval increase in reported concern about the impacts of extreme weather on their work, staff had nearly twice the odds (1.96) of reporting motivation to use clinic resilience resources. Staff had 1.55 times the odds of reporting motivation to use clinic resilience resources with each interval increase in reported knowledge about the effects of climate change on health. Years of experience was not a significant predictor of reported motivation to use resources (Table 3).
Table 3.
Predictors of reported motivation to use clinic and patient resilience resources and discuss climate change
| All staff | Providers & case workers | ||
|---|---|---|---|
| Motivation to use clinic resilience resources | Discussion of climate change with patients | Motivation to use patient resources to help prepare | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Belief that humans are causing climate change | 4.39 (1.56, 12.36)* | 0.38 (0.80, 1.76) | 1.71 (0.37, 7.98) |
| Knowledge of climate effects on health | 1.55 (1.21, 1.99)** | 1.03 (0.68, 1.59) | 1.14 (0.76, 1.72) |
| Years of experience doing current job | 1.02 (0.85, 1.22) | 1.11 (0.81, 1.53) | 1.07 (0.80, 1.44) |
| Concern that extreme weather is affecting job | 1.96 (1.60, 2.39)*** | 0.89 (0.67, 1.18) | 1.06 (0.81, 1.39) |
| Belief that climate change affects patient health | 1.67 (1.02, 2.75)* | 1.85 (1.19, 2.87)** | |
| Confidence in developing disease management plans | 1.30 (0.96, 1.78) | 1.10 (0.82, 1.47) | |
Legend Unadjusted Odds Ratios (OR) with 95% Confidence Intervals (CI). Results presented of questions asked to all staff (N = 365) and questions asked only to providers & case workers (N = 121). Starred results are statistically significant; * represents α < 0.05, ** represents α < 0.01, and *** represents α < 0.001
Direct patient care staff (providers and case workers) reported they were more likely to discuss climate change with patients (OR 1.67) and reported they were more motivated to use resilience resources to help patients prepare for extreme events (OR 1.85) for each interval increase of reported belief that climate change affects patient health. The additional variables of reported belief that humans are causing climate change, knowledge of climate effects on health, years of experience, concern that extreme weather is affecting job, and confidence in developing management plans were not significant predictors in this analysis; sample size was smaller of providers and case workers compared to all staff (Table 3).
Discussion
This study reveals novel perspectives on climate change and health impacts and clinic and patient climate resilience from a geographically diverse sample of staff at frontline clinics who serve populations particularly vulnerable to a changing climate. Respondents overwhelmingly reported the belief that humans are causing climate change, although less than a quarter reported they were confident of the health effects associated with climate change, which is consistent with prior studies [24–28]. Respiratory disease and heat stroke were most commonly reported to be connected to climate change, which is supported by prior evidence, even if these may not constitute the majority of disease burden in the United States from climate change [2, 32, 33].
Despite approximately half of respondents reporting they were not concerned about the effects of extreme events on their jobs, an equivalent number reported these same events disrupted care delivery. The disconnect between reported level of concern and reported disruptions may indicate a cognitive dissonance regarding abstract compared to directly observed features of climate change [34]. In addition, this disconnect may signify a gap in knowledge about direct impacts of extreme events compared to their cascading impacts such as power failures and road closures that have significantly impaired care delivery [35, 36]. The underlying reason for these disconnects is not fully elucidated in this study and warrants further investigation.
Climate change-related extreme events were reported to disrupt clinical operations, impede access to care, and prompt clinic shutdowns. The greatest need reported during extreme events was emergency power, with over half of respondents stating prior power outages had interrupted care. Across the United States, extreme events are increasingly contributing to power outages that harm health and disrupt clinical care [5, 7, 37]. Given the need for emergency power reported across extreme events, and the potential disruptions without power, it is imperative to prioritize both funding for clinics to obtain back-up power systems as well as developing guidelines for emergency power across all frontline clinics.
Although there are federal regulations for healthcare facilities receiving Medicare and Medicaid funds requiring back-up power for critical services such as operating rooms and critical care units, these regulations often do not apply to primary care services offered at frontline clinics, or for facilities not receiving federal funding [38]. The prospect of more frequent and persistent interruptions to care delivery at frontline clinics [37, 39] – clinics that often provide safety net care for those most at-risk to climate extremes – underscores the need to ensure federal policies cover all frontline clinics, and that there is operational and financial support to enact these policies. This survey was conducted prior to the passage of the Inflation Reduction Act, representing an essential step in federal support for climate resilience, particularly for healthcare organizations serving the most at-risk populations [40, 41]. Frontline clinics form an integral component of the greater healthcare ecosystem and have identified the resources needed to improve resilience to extreme events, the foremost being back-up power; we now need to ensure they have the fundamental and ongoing support to initiate these improvements for climate resilience.
The Emergency Preparedness Rule from Centers for Medicare and Medicaid Services (CMS) established in 2016 requires all providers accepting CMS payments to follow “national emergency preparedness requirements to ensure adequate planning for both natural and man-made disasters [19].” Despite the reported interruptions in clinical care from extreme events and the CMS requirement for disaster planning, only 54.4% of respondents reported they have plans in place to address care interruptions from extreme events. Compliance with the requirement for disaster planning depends on receipt of CMS payments, and 45.8% of clinic respondents were from free and charitable clinics (FCCs) that may provide care without CMS reimbursement. Current policy leaves out an essential component of the healthcare ecosystem, FCCs, which may benefit from guidelines, but only with concurrent financial and operational support to enact these emergency preparedness measures. Although more clinics that identified as Federally Qualified Health Centers reported having plans in place for extreme events than FCCs (57.4% v. 49.6%), both may benefit from increased awareness, support, and development of these preparedness plans. Healthcare professionals are increasingly calling for improved healthcare resilience to extreme events; this study delineates what clinics need and the ongoing gaps in preparedness that can be incorporated into improved climate resilience guidance [36, 42, 43].
Despite the increased need for healthcare resilience to climate change – as indicated by reported health disruptions during extreme events in this study and others [4, 6, 44, 45] – few studies have evaluated how to improve frontline clinic resilience at a staff level. Results from this survey suggest that staff at frontline clinics prefer succinct, algorithmic materials such as checklists and plans as well as direct training of staff to improve clinic resilience. Not surprisingly, concurrence with the scientific consensus that humans are causing climate change, as well as knowledge of health effects from climate change, were associated with greater motivation to use resiliency resources. This supports the need for education on climate change and health for all staff at frontline clinics to improve their utilization of climate resilience resources.
Provider and case worker perspectives on climate & health
Providers and case workers tended to believe that climate change impacts patient health (84.4%), and those that did were more likely to discuss climate change with their patients and be motivated to prepare them for extreme events. However, many identified barriers that limited their ability to discuss climate change with patients, including other pressing issues, limited time, and lack of knowledge. These results are similar to prior studies, also identifying time and knowledge as barriers to engagement in clinical settings [24]. These barriers may provide insight for future interventions, such as by providing patient education in pamphlets or through automated electronic medical record messaging that do not take time away from the clinical encounter or other issues. Engaging allied health professionals who may have more time with patients, such as community health workers, health educators, or patient navigators may also help overcome these reported barriers. For instance, allied health professionals have effectively used targeted interventions to facilitate access to care and address social determinants of health, skills that can also be used to address climate impacts on health [46, 47].
Healthcare providers, medical journals, and public health associations are increasingly recognizing the need to engage in climate and health education and advocacy [24, 28, 36, 48, 49]. Consistent with this increasing engagement, providers in this study expressed motivation to learn more about climate change and help prepare their patients. Brief information sheets, pamphlets, and videos or online modules were among the educational modalities most of interest to respondents – and represent potential ways to improve knowledge and preparedness for climate impacts.
Limitations
There are several limitations to this study. First, this was a convenience sample of clinics with certain regions over-represented across the United States (including the West and Northeast); responses may not be representative of other regions. For instance, 38.5% of respondent clinics were from California and New York, and although these are two of the most populous states, they are also predominantly liberal states, and opinions on climate change vary by political leanings of states [50, 51]. This over-representation could lead to a potential response bias, particularly for questions concerning climate change knowledge and attitudes. This is partially limited as the next most respondents were from Florida and North Carolina, more conservative states with views on climate change in line with national average, and respondents represented a total of 43 states [50, 51].
An analysis of rural compared to urban community health centers was not performed as the rurality of clinic location was not asked and may warrant further investigation. This study was completed by staff at frontline clinics (predominantly FQHCs and FCCs), and therefore may not be generalizable to other outpatient clinic settings or populations. Although all staff were invited to participate in the survey and many distinct roles were represented in the responses, approximately 70% were providers and administrators, potentially leading to a response bias in favor of those roles.
In addition, we are unable to know the total number of individuals who received the survey given the snowballing sampling methodology, and as a result, the overall response rate. Given this non-random sampling method, the results may not be generalizable to the entire population. Response bias may have occurred as those completing the survey may have been most interested in climate change resilience a priori. Notably, 18% of respondents did not agree with the scientific consensus that human activities are driving climate change which suggests a diversity of respondents.
This survey was administered during the COVID-19 pandemic, in the fall of 2021; given the significant impact of the pandemic on frontline clinic care delivery [52, 53], this may result in bias of the results towards other priorities (i.e. COVID-19), and may have reduced the overall response rate. A minority of respondents only filled out the initial demographic characteristics but did not respond to the rest of the substantive questions (hence the threshold of 20% of responses completed for inclusion into the study analysis). This survey was administered electronically via email to clinics; the electronic administration may limit the reliability of the responses [54]. Additionally, results are now over two years old, leading to potential secular threat.
The statistical analysis did not include confounders or effect modification for the associations evaluated, partly due to limitations on the survey length and types of questions asked; this represents an area for future study. Limitations of the predictive analysis include the smaller sample size for providers and case workers, and therefore although some variables were not significantly predictive, it may be due to inadequate sample size and conclusions should not be drawn based on this study alone.
Despite these limitations, this study is the first to our knowledge to assess the views of all types of frontline clinic staff, including administrators, case workers, and providers, with a focus on clinic resilience and resources, providing valuable insight from a critical component of the healthcare system.
Conclusions
Frontline clinics care for communities particularly sensitive to climate risks [55], making them an integral facet of climate resilience and health protection. In this study, extreme events have already disrupted clinic operations, and frontline clinics identified emergency power as their greatest need for preparedness. Improving identified gaps in preparedness planning may also improve clinic climate resilience. Staff at frontline clinics were motivated to learn about climate and health and to prepare their patients and clinics for the present and growing threat of climate-related extreme events.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- C-CHANGE
Center for Climate, Health, and the Global Environment
- CMS
Centers for Medicare and Medicaid Services
- FQHCs
Federally Qualified Health Centers
- FCCs
Free and Charitable Clinics
- NACHC
National Association of Community Health Centers
- NAFC
National Association of Free and Charitable Clinics
- U.S.
United States
Author contributions
TW: Developed the methodology and conducted the formal analysis, lead the writing of the original draft and review and editing. TM: Contributed to conceptualization of the survey and methodology for survey deployment and analysis and contributed to writing review & editing. MF: Contributed to survey conceptualization and development and deployment and writing review and editing. KS: Contributed to survey conceptualization and development and deployment and writing review and editing. CH: Contributed to survey analysis and writing review and editing. NMT: Major contributor in writing and editing. CD: Contributed to survey analysis methodology and was a major contributor to writing and editing and provided resource support and supervision. AB: Lead conceptualization of the survey and deployment. Contributed to development of survey analysis and major contributor to writing and editing the manuscript as well as provided resource support and supervision. All authors read and approved the final manuscript to be published.
Funding
This work was made possible in part by a grant from Biogen. The funder had no role in the conceptualization, design, data analysis, or interpretation of the results of the study or in the decision to publish or in writing or approval of the manuscript.
Data availability
Data is provided within the manuscript and supplementary files. We have made the survey questionnaire publicly available in the appendix with this manuscript. The datasets generated and analyzed for this study are not publicly available, given we analyzed a specific population and sharing of the data could potentially lead to disclosure of identities. However, data may be available for the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study that involves human subjects was approved by the Harvard T.H. Chan School of Public Health Institutional Review Board Protocol # IRB21-0726. Informed consent was obtained from all subjects prior to completing the electronic survey. A brief introduction to the survey detailing the purpose of the survey, the voluntary nature, confidentiality, and potential risks and benefits per guidelines of informed consent was provided electronically and participants consented electronically prior to completing the survey. The introduction process for electronic informed consent was approved by the above Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.IPCC. Summary for policymakers. In: Masson -Delmotte V, Zhai P, Pirani A, Connors SL, Péan C, Berger S, et al. editors. Climate Change 2021: the Physical Science Basis Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2021. pp. 3–32. [Google Scholar]
- 2.Cissé G, McLeman R, Adams H, Aldunce P, Bowen K, Campbell-Lendrum D et al. Health, Wellbeing, and the Changing Structure of Communities [Internet]. Pörtner HO, Roberts D, Fischlin A, Howden M, Méndez C, Pereira JJ, editors. Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2022. p. In Press. https://www.ipcc.ch/working-group/wg2/
- 3.EPA. Climate Change and Social Vulnerability in the United States: a focus on six impacts. U.S. Environmental Protection Agency; 2021. Report No.: EPA 430-R-21-003.
- 4.Raker EJ, Arcaya MC, Lowe SR, Zacher M, Rhodes J, Waters MC. Mitigating Health disparities after Natural disasters: lessons from the RISK project. Health Aff Proj Hope. 2020;39(12):2128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flores NM, McBrien H, Do V, Kiang MV, Schlegelmilch J, Casey JA. The 2021 Texas Power Crisis: distribution, duration, and disparities. J Expo Sci Environ Epidemiol. 2023;33(1):21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kishore N, Marqués D, Mahmud A, Kiang MV, Rodriguez I, Fuller A, et al. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med. 2018;379(2):162–70. [DOI] [PubMed] [Google Scholar]
- 7.Casey JA, Fukurai M, Hernández D, Balsari S, Kiang MV. Power Outages and Community Health: a Narrative Review. Curr Environ Health Rep. 2020;7(4):371–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Operational framework for building climate resilient health systems [Internet]. World Health Organization. 2015. https://apps.who.int/iris/bitstream/handle/10665/189951/9789241565073_eng.pdf?sequence=1
- 9.WHO. Operational framework for building climate resilient and low carbon health systems [Internet]. Geneva: World Health Organization. 2023. https://www.who.int/publications/i/item/9789240081888
- 10.DHHS. Sustainable and Climate Resilient Health Care Facilities Toolkit [Internet]. USA. 2024 Apr. https://toolkit.climate.gov/topics/human-health/building-climate-resilience-health-sector
- 11.Department of Health and Human Services. Compendium of Federal Resources for Health Sector Emissions Reduction and Resilience [Internet]. USA. 2023 [cited 2023 Jun 21]. https://www.hhs.gov/climate-change-health-equity-environmental-justice/climate-change-health-equity/actions/health-care-sector-pledge/federal-resources/index.html
- 12.Gibbons E et al. Climate Resilience for Health Care and Communities: Strategies and Case Studies [Internet]. Health Care Without Harm; 2022 Jan. https://noharm-uscanada.org/climate-resilience-for-health-care-and-communities
- 13.Center for Medicare and Medicaid Services. Federally Qualified Health Center [Internet]. Center for Medicare and Medicaid Services. 2019. https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents/FQHC-Text-Only-Factsheet.pdf
- 14.NAFC, About. NAFC | National Association of Free & Charitable Clinics [Internet]. 2021 [cited 2024 Apr 3]. https://nafcclinics.org/about-us/
- 15.HealthCare.gov [Internet]. [cited 2024 Aug 15]. Federally Qualified Health Center (FQHC) - Glossary. https://www.healthcare.gov/glossary/federally-qualified-health-center-fqhc
- 16.What is a Health. Center? | Bureau of Primary Health Care [Internet]. [cited 2024 Aug 15]. https://bphc.hrsa.gov/about-health-center-program/what-health-center
- 17.NACHC. America’s Health Centers: By The Numbers [Internet]. NACHC. 2023 [cited 2024 Jun 24]. https://www.nachc.org/resource/americas-health-centers-by-the-numbers/
- 18.NAFC. National Association of Free and Charitable Clinics Data Report. 2024 [Internet]. 2024 [cited 2024 Jun 24]. cclinics.org/wp-content/uploads/2024/03/NAFC-Data-Report-2024.pdf
- 19.CMS.gov. Emergency Preparedness Rule [Internet]. 2023 [cited 2023 Aug 17]. https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertemergprep/emergency-prep-rule
- 20.Lokotola CL. Towards a climate-resilient primary health care service. South Afr Fam Pract off J South Afr Acad Fam Pract Care. 2023;65(1):e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kadandale S, Marten R, Dalglish S, Rajan D, Hipgrave D. Primary health care and the climate crisis. Bull World Health Organ. 2020;98:818–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blashki G, McMichael T, Karoly DJ. Climate change and primary health care. Aust Fam Physician. 2007;36(12):986–9. [PubMed] [Google Scholar]
- 23.Blau FD, Koebe J, Meyerhofer PA. Who are the essential and frontline workers? Bus Econ Clevel Ohio. 2021;56(3):168–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kotcher J, Maibach E, Miller J, Campbell E, Alqodmani L, Maiero M, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health. 2021;5(5):e316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheffield PE, Durante KT, Rahona E, Zarcadoolas C. Emerging roles of health care providers to mitigate climate change impacts: a perspective from East Harlem, New York. Health Hum Rights. 2014;16(1):113–21. [PMC free article] [PubMed]
- 26.Dupraz J, Burnand B. Role of Health Professionals Regarding the Impact of Climate Change on Health—An Exploratory Review. Int J Environ Res Public Health [Internet]. 2021;18(6). https://www.mdpi.com/1660-4601/18/6/3222 [DOI] [PMC free article] [PubMed]
- 27.André H, Gonzalez Holguera J, Depoux A, Pasquier J, Haller DM, Rodondi PY et al. Talking about Climate Change and Environmental Degradation with patients in primary care: a cross-sectional survey on knowledge, potential domains of action and points of View of General practitioners. Int J Environ Res Public Health. 2022;19(8). [DOI] [PMC free article] [PubMed]
- 28.Lee HR, Pagano I, Borth A, Campbell E, Hubbert B, Kotcher J et al. Health professional’s willingness to advocate for strengthening global commitments to the Paris climate agreement: findings from a multi-nation survey. J Clim Change Health. 2021; Vol 2. [DOI] [PMC free article] [PubMed]
- 29.Völker M, Hunchangsith P. Drivers of Physicians’ Engagement in addressing eco-health problems. EcoHealth. 2018;15(4):853–63. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan GM, Artino ARJ. Analyzing and interpreting data from likert-type scales. J Grad Med Educ. 2013;5(4):541–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.StataCorp, Stata. Release 18. College Station. TX: StataCorp LLC; 2023. [Google Scholar]
- 32.Campbell S, Remenyi TA, White CJ, Johnston FH. Heatwave and health impact research: a global review. Volume 53. Health & Place; 2018. pp. 210–8. [DOI] [PubMed]
- 33.Mirsaeidi M, Motahari H, Khamesi MT, Sharifi A, Campos M, Schraufnagel DE. Climate Change and respiratory infections. Annals Am Thorac Soc. 2016;13:1223–30. [DOI] [PubMed] [Google Scholar]
- 34.Bergquist M, Nilsson A, Schultz PW. Experiencing a Severe Weather Event Increases Concern About Climate Change. Front Psychol [Internet]. 2019;10. https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2019.00220 [DOI] [PMC free article] [PubMed]
- 35.Leal Filho W, Abeldaño Zuñiga RA, Sierra J, Dinis MAP, Corazza L, Nagy GJ, et al. An assessment of priorities in handling climate change impacts on infrastructures. Sci Rep. 2024;14(1):14147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sherman JD, MacNeill AJ, Biddinger PD, Ergun O, Salas RN, Eckelman MJ. Sustainable and Resilient Health Care in the Face of a changing climate. Annu Rev Public Health. 2023;44:255–77. [DOI] [PubMed] [Google Scholar]
- 37.Climate Central. Weather-related Power Outages Rising | Climate Central [Internet]. 2024 [cited 2024 Aug 26]. https://www.climatecentral.org/climate-matters/weather-related-power-outages-rising
- 38.Federal Emergency Management Agency and Assistant Secretary for Preparedness and Response. Healthcare Facilities and Power Outages Guidance for State, Local, Tribal, Territorial, and Private Sector Partners [Internet]. FEMA. 2019. https://www.fema.gov/sites/default/files/2020-07/healthcare-facilities-and-power-outages.pdf
- 39.Klinger C, Landeg O, Murray V. Power outages, extreme events and health: a systematic review of the literature from 2011–2012. PLoS Curr. 2014;6:ecurrentsdis04eb1dc5e73dd1377e05a10e9edde673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Health (OASH) O of the AS for. The Office of Climate Change and Health Equity (OCCHE) Quickfinder for Leveraging the Inflation Reduction Act for the Health Sector [Internet]. 2023 [cited 2024 Mar 1]. https://www.hhs.gov/climate-change-health-equity-environmental-justice/climate-change-health-equity/quickfinder-ira/index.html
- 41.US EPA O. Inflation Reduction Act Community Change Grants Program [Internet]. 2023 [cited 2024 Mar 3]. https://www.epa.gov/inflation-reduction-act/inflation-reduction-act-community-change-grants-program
- 42.Salas Renee N. The Growing Link Between Climate Change and Health. NEJM Catal [Internet]. [cited 2023 Aug 8];3(3). 10.1056/CAT.22.0052
- 43.Curtis S, Fair A, Wistow J, Val D, Oven K. Impact of extreme weather events and climate change for health and social care systems. Environ Health. 2017;16:23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamideh S, Sen P, Fischer E. Wildfire impacts on education and healthcare: paradise, California, after the Camp Fire. Nat Hazards. 2022;111(1):353–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bedi NS, Dresser C, Yadav A, Schroeder A, Balsari S. Wildfire Threat to Inpatient Health Care Facilities in California, 2022. Am J Public Health. 2023;113(5):555–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gkiouleka A, Aquino MRJ, Ojo-Aromokudu O, van Daalen KR, Kuhn IL, Turner-Moss E, et al. Allied health professionals: a promising ally in the work against health inequalities- A rapid review. Public Health Pract Oxf Engl. 2022;3:100269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis SF, Enderby P, Harrop D, Hindle L. Mapping the contribution of Allied Health professions to the wider public health workforce: a rapid review of evidence-based interventions. J Public Health Oxf Engl. 2017;39(1):177–83. [DOI] [PubMed] [Google Scholar]
- 48.Atwoli L, Baqui AH, Benfield T, Bosurgi R, Godlee F, Hancocks S, et al. Call for emergency action to Limit Global temperature increases, Restore Biodiversity, and protect Health. N Engl J Med. 2021;385(12):1134–7. [DOI] [PubMed] [Google Scholar]
- 49.US Call to Action on Climate, Health, and Equity. A Policy Action Agenda [Internet]. 2019 [cited 2023 Aug 16]. https://climatehealthaction.org/cta/climate-health-equity-policy/
- 50.NW, St 1615L. Suite 800Washington, Inquiries D 20036USA202 419 4300 | M 857 8562 | F 419 4372 | M. Religious Landscape Study [Internet]. Pew Research Center’s Religion & Public Life Project. 2024 [cited 2024 Jun 2]. https://www.pewresearch.org/religious-landscape-study/database/
- 51.Marlon J. Yale Climate Opinion Maps 2023 [Internet]. Yale Program on Climate Change Communication. 2023 [cited 2024 Jun 2]. https://climatecommunication.yale.edu/visualizations-data/ycom-us/
- 52.Simon J, Mohanty N, Masinter L, Hamilton A, Jain A. COVID-19: exploring the repercussions on federally qualified Health Center Service Delivery and Quality. J Health Care Poor Underserved. 2021;32(1):137–44. [DOI] [PubMed] [Google Scholar]
- 53.Cook N, McGrath BM, Navale SM, Koroukian SM, Templeton AR, Crocker LC, et al. Care Delivery in Community Health Centers before, during, and after the COVID-19 pandemic (2019–2022). J Am Board Fam Med JABFM. 2024;36(6):916–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Menon V, Muraleedharan A. Internet-based surveys: relevance, methodological considerations and troubleshooting strategies. Gen Psychiatry. 2020;33(5):e100264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bernstein AS, Stevens KL, Koh HK. Patient-centered Climate Action and Health Equity. JAMA. 2022;328(5):419–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is provided within the manuscript and supplementary files. We have made the survey questionnaire publicly available in the appendix with this manuscript. The datasets generated and analyzed for this study are not publicly available, given we analyzed a specific population and sharing of the data could potentially lead to disclosure of identities. However, data may be available for the corresponding author upon reasonable request.