Abstract
Background
Utilising ultrasound technology has resulted in higher success and lower complication rates during regional anaesthesia (RA) procedures. Proper training is necessary to accurately identify structures, optimise images, and improve hand–eye coordination. Simulation training using immersive virtual environments and simulation models has enabled this competency training to be conducted safely before performing on patients. We conducted a study to compare the simulator performance and users’ feedback on a Blue Phantom Regional Anaesthesia Ultrasound Training Block and NeedleTrainer™.
Methods
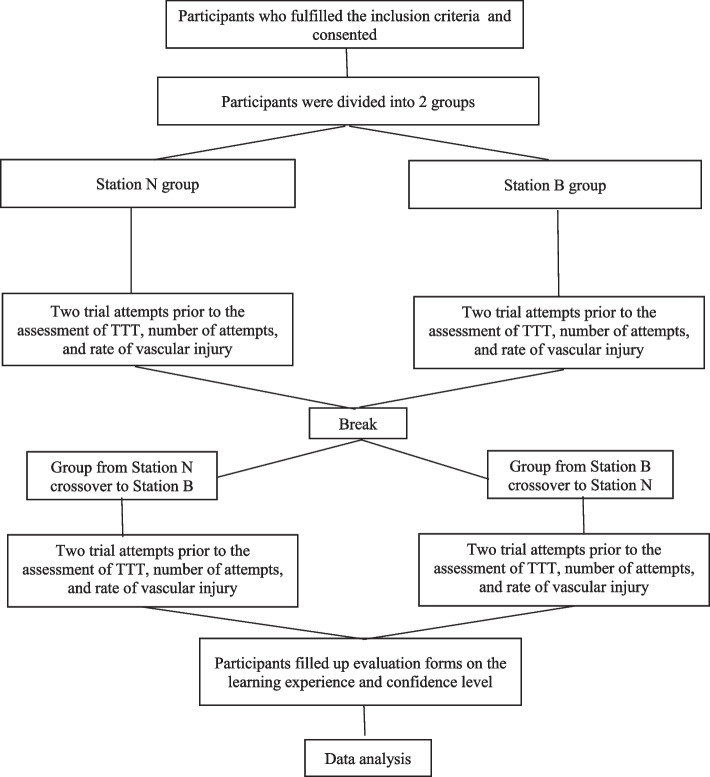
Forty-seven participants were recruited via convenient sampling during a RA workshop for novice practitioners. They were divided into the N or B group and then crossover to experience using both Blue Phantom and NeedleTrainer model. Time-to-reach-target, first-pass success rate, and complication rate were assessed, while the learning and confidence scores were rated using six-item and three-item questionnaires, respectively, via a 5-point Likert scale.
Results
Blue Phantom model has a longer time-to-target as compared to the NeedleTrainer model (16 ± 8 vs 8 ± 3 s, p < 0.001), higher first- pass success rate (100% vs 80.9%), and lower complication rate (0% vs 19.1%). Higher overall learning satisfaction scores (28 ± 4 vs 25 ± 4, p = 0.003) and confidence scores after training (13 ± 2 vs 12 ± 2, p < 0.001) were recorded for the Blue Phantom model.
Conclusions
We postulated that the artificial intelligence structure recognition software enables NeedleTrainer users to attain shorter time-to-target. That being said, Blue Phantom provides better operator learning satisfaction, improved confidence, higher success and lower complication rates among novice RA practitioners, possibly due to greater tactile feedback during the simulated training.
Keywords: Ultrasound simulator, Blue phantom, NeedleTrainer, Regional anaesthesia
Introduction
Since the assimilation of ultrasound into the anaesthetic practice, there has been a resurgence and rapid advances in regional anaesthesia. Regional anaesthesia is beneficial, especially in avoiding the risk of general anaesthesia in critically ill patients, reducing opioid usage, and is a vital component in multimodal analgesic strategy. However, the practice of regional anaesthesia, especially under ultrasound guidance, has a different learning curve than general anaesthesia. In ultrasound-guided regional anaesthesia, precise needle handling and hand-eye coordination are essential. The real-time visualization required for nerve blocks demands that practitioners maintain a steady trajectory and adjust the needle accurately [1]. The Department of Health United Kingdom recommended that healthcare professionals should first learn skills in a simulation environment and using other technologies [2]. This simulation environment helps trainees in regional anaesthesia to bridge their knowledge translation into clinical practice and minimise unintentional injury to actual patients. However, a conventional simulation environment may be costly to set up [3]. As such, various methods have been proposed, including the integration of augmented reality technology software into the available medical equipment [4].
There are various ultrasound simulation models, such as the Blue Phantom model, gelatine-based model, agar-based model, tofu-based model, silicon-based models, animal tissue, cadavers and the use of immersive technology [5]. The Blue Phantom model is a commercially available tissue simulator that offers realistic and quality ultrasound images [6]. It also has the highest fidelity among trainees compared to the gelatine-based and tofu-based models [7]. The Blue Phantom also endured repeated needle attempts without significant integrity degradation compared to the animal tissue [8]. However, the most critical disadvantage of the Blue Phantom is the relatively higher cost and the lower visual and tactile response compared to animal tissue [7, 8].
NeedleTrainer™ is a new ultrasound simulation adjunct solution that utilises augmented reality (AR) technology on real subjects. As such, it offers real-time and dynamic ultrasound images for flexible teaching without incurring patient complications [9]. It can be used safely to overlay the needle image to plan its trajectory safely and estimate the appropriate needle length needed for actual patients. More importantly, it can be used repeatedly without deteriorating image quality compared to other ultrasound simulator models. Although it offers a paramount visual experience, NeedleTrainer lacks the tactile experience practitioners need when performing regional anaesthesia. Despite this limitation, it is a helpful educational tool for novice practitioners in regional anaesthesia before training on actual patients. It helps to train hand–eye coordination of the ultrasound beam and needle trajectory, which is an essential skill in ultrasound-guided regional anaesthesia.
Immersive technology, which encompasses AR and virtual reality (VR) in anaesthesia training and practice, is rapidly gaining momentum [10, 11]. As they are still in the infancy stage, there needs to be more validation and feedback from trainees regarding their use in medical education. The Kirkpatrick Model has four levels for evaluating the training model: reaction, learning, behaviour, and results. However, as each level progresses, the difficulty in assessing and the cost involved in evaluation also increases. Levels 1 and 2 of the evaluation (reaction and learning) are usually done after the training [12]. Level 3, which evaluates behaviour, requires long-term observation and peer reviews, adding time and supervision costs. Level 4 is the most resource-intensive, needing extensive data collection and control over external factors to confirm that outcomes are due to training, often requiring multi-centre, long-term studies [12]. In this study we aimed to evaluate level 1 and 2 to first establish evidence of user satisfaction and learning gains, as these are critical prerequisites to justify further investment into real-world impact evaluations.
The Anatomy and Ultrasonography in Regional Anaesthesia (AURA) Workshop is an educational workshop organised to cater for the training of novice regional anaesthesia practitioners [13]. As AURA caters to the increased training demand nationwide, we need to evaluate our education model's learning experience and cost-effectiveness. This helps to determine a simulation model that provides a safe, sustainable and optimal learning environment for our trainees. Given the scarcity of literature evaluating the various ultrasound simulator models, our study aimed to compare the new NeedleTrainer with the existing Blue Phantom ultrasound tissue simulation model among novice regional anaesthesia practitioners regarding its training experience and user’s feedback.
Methods
Study design and population
This crossover study was approved by the Research Ethics Committee of Faculty of Medicine, UKM (JEP-2023-072). We define a novice as a practitioner with limited experience or formal training in performing ultrasound-guided nerve blocks, who lacks proficiency in advanced skills such as needle visualization, ultrasound-specific hand-eye coordination, and real-time interpretation of anatomical structures. This group includes individuals who perform regional anesthesia no more than once every two weeks. The study employed convenience sampling, recruiting participants who met this novice definition and provided consent. Those who had hand deformities or severe tremors were excluded.
Study location and duration
The study took place during the AURA workshop which was conducted within the premise of Hospital Canselor Tuanku Muhriz (HCTM), Kuala Lumpur, Malaysia. This workshop included lecture sessions on the first day, followed by simulation stations on the second day, during which the study was conducted.
Study protocol
All anaesthesiology trainees fulfilling the inclusion criteria and attending AURA were conveniently divided into two groups during the simulation session on the second day of the workshop. These two groups were assigned to two stations, Station N and Station B. Trainees in Station N began their training with the NeedleTrainer simulation, while those in Station B used an ultrasound tissue simulator. The NeedleTrainer was connected to a Vscan Air™ ultrasound machine by GE Healthcare, and, to ensure consistency, the same ultrasound device was used for all participants in both stations.
Each trainee had two trial attempts to become familiar with the procedure and the ability to identify structures before the assessment. An attempt was considered complete when the needle was inserted into the simulated skin and then taken out completely. During the evaluation, the time to target (TTT) was defined as the duration (in seconds) taken from needle insertion to reaching the intended site of the simulated nerve, with at least 50% needle visibility, including the needle tip on the ultrasound image. Additionally, the number of attempts and the rate of vascular puncture were documented, with vascular puncture was considered when the needle image overlayed on the simulated vessel on the ultrasound image. The NeedleTrainer provided real-time visual guidance with a bar indicator on the side of the monitor to display needle visibility. In contrast, needle visibility for the Blue Phantom model was assessed manually by a single investigator, who confirmed that at least 50% of the needle shaft was visible.
After the first session, all trainees had a short tea break before moving to the other station (with participants shifting from Station N to Station B, and vice versa). The trainees then repeated the similar process previously at their new stations. Following each participant's completion of both stations, they received a 6-item questionnaire to self-evaluate their learning experience and a 3-item questionnaire to self-assess their confidence level in regional anaesthesia using both models, via a 5-point Likert scale. This method utilises both levels 1 and 2 of the Kirkpatrick training evaluation model [12]. The study flow chart is shown in Fig. 1.
Fig. 1.
Study flow chart
Statistical test
All calculations and statistical analyses were performed by using Statistical Package for the Social Sciences (SPSS) version 29. Descriptive statistics were used for demographic data and Likert scale questions. Descriptive statistics included measurements of frequencies (n) and percentages (%) were presented using tables. For the purpose of homogeneity tests, the Likert scale scores for each questionnaire item were totalled up according to the respective sections. Higher scores indicate more positive responses and vice versa.
Non-parametric statistical tests were used to analyse the data in this study. A Kruskal-Wallis test for independent samples was conducted to assess the relationship between TTT, overall learning satisfaction scores and overall confidence scores with polynomial demographic data. Meanwhile, Mann-Whitney test was used to compare those variables with dichotomous demographic data. In these analyses, TTT, trainees' total learning satisfaction scores and trainees’ total confidence score served as the dependent variables, while demographic categories were used as the independent, or grouping, variable. For cases where the relationship was found to be statistically significant following the Kruskal-Wallis test, post-hoc analyses with the Dunn-test were carried out to identify the distinct groups that differed from one another. Additionally, to address the issue of multiple comparisons and reduce the Type I error rate, p-values were adjusted using the Bonferroni correction method.
In addition, Wilcoxon signed rank test was used to compare the TTT between NeedleTrainer and Blue Phantom models, while McNemar’s test was used to compare first-pass success rate and complication rate between the two simulation models. A p-value of less than 0.05 was considered to be statistically significant. The data obtained from this study can only represent the population of participants who attended AURA 2023.
Results
Forty-seven participants of novice anaesthesia practitioners from around Malaysia attending the AURA 2023 workshop were recruited into this study through convenient sampling and their demographic criteria are presented in Table 1. The majority of the respondents were female (57.4%), aged between 31-35 (59.6%) and currently a medical officer (57.4%). Of these, 59.6% of them had less than 5 years of anaesthetic experience and the majority of them perform regional anaesthesia once a month (34.0%).
Table 1.
Demographic characteristics of study sample
| Demographic characteristics | Frequency (n = 47) | |
|---|---|---|
| Gender | Male | 20 (42.6) |
| Female | 27 (57.4) | |
| Age | ≤ 30 | 10 (21.3) |
| 31–35 | 28 (59.6) | |
| ≥ 36 | 9 (19.1) | |
| Designation | Specialist | 8 (17.0) |
| Masters Trainee | 12 (25.5) | |
| Medical Officer | 27 (57.4) | |
| Experience in Anaesthesia (Years) | < 5 | 28 (59.6) |
| 5–10 | 16 (34.0) | |
| > 10 | 3 (6.4) | |
| Frequency of performing regional anaesthesia | Once a week | 12 (25.5) |
| Once a month | 16 (34.0) | |
| Once a year | 7 (14.9) | |
| Never | 12 (25.5) | |
Values are expressed in frequency (percentage)
As shown in Table 2, the Blue Phantom model exhibits a considerably higher median Time-to-Target (TTT) in relative to the NeedleTrainer model, with values of 16 s (interquartile range: 8–23 s) versus 8 s (interquartile range: 5–9 s) respectively, a significant difference exhibited by a p-value of less than 0.001. Furthermore, there is a markedly greater first-attempt success rate observed within the Blue Phantom model (100%) in comparison to the NeedleTrainer model (80.9%) (p-value 0.004), coupled with a substantially low rate of complications (0% versus 19.1%, p-value = 0.004)).
Table 2.
Time-to-target (TTT), success rate and complication rate between Blue Phantom and NeedleTrainer
| Variable | Blue Phantom | NeedleTrainer | p-Value |
|---|---|---|---|
| TTT (seconds) | 16 [8-23] | 8 [5-9] | < 0.001a |
| First pass success rate (frequency) | 47 (100%) | 38 (80.9%) | 0.004b |
| Complication rate (frequency) | 0 (0.0%) | 9 (19.1%) | 0.004b |
Values are expressed as median [interquartile range] and frequency (percentage)
aWilcoxon signed rank test, bMcNemar’s test
The self-assessed evaluation forms consisted of a 6-item questionnaire on self-evaluation of the trainees’ learning experience and a 3-item questionnaire on self-assessment of their confidence level in performing simulated RA using both models. The responses to each Likert scale questions is exhibited in the following Table 3. Comparative analysis reveals that participants attribute significant superior learning experience to the Blue Phantom model over the NeedleTrainer model in areas such as the optimisation of ultrasound beam for needle localization, improvement of hand–eye coordination, the usefulness and recommendation for future training purposes. Nevertheless, there is a consensus between the groups on the high level of learning outcome attained regarding identifying critical structures on ultrasound imagery and independent practice through the utilization of both models.
Table 3.
Participants' self-evaluation of learning experience and confidence level following simulated training using Blue Phantom and NeedleTrainer models
| Variable | Blue Phantom | NeedleTrainer | p-Valuea |
|---|---|---|---|
| Learning experience | |||
| Identifying critical structure | 4 [4, 5] | 5 [4, 5] | 0.180 |
| Optimizing needle location | 5 [4, 5] | 4 [3–5] | < 0.001 |
| Hand–eye coordination improvement | 5 [4, 5] | 4 [3–5] | < 0.001 |
| Usefulness for future workshop | 5 [5–5] | 5 [4, 5] | 0.001 |
| Practice independently | 4 [3–5] | 4 [3–5] | 0.150 |
| Recommended for training | 5 [4, 5] | 5 [4, 5] | 0.015 |
| Overall score | 28 [24–30] | 25 [21–29] | 0.003 |
| Confidence level | |||
| Identifying critical structure | 4 [4, 5] | 4 [4, 5] | 0.290 |
| Optimizing needle location | 5 [4, 5] | 4 [3–5] | < 0.001 |
| Hand–eye coordination improvement | 4 [4, 5] | 4 [3, 4] | < 0.001 |
| Overall score | 13 [12–15] | 12 [10–13] | < 0.001 |
| Preference | 26 (55.3%) | 7 (14.9%) | NA |
Values are expressed as median [interquartile range] and frequency (percentage)
aWilcoxon signed rank test
The self-evaluation on confidence level data suggests that the Blue Phantom model yields a marginally higher confidence level in optimization of ultrasound techniques for needle localization and in hand–eye coordination. Both Blue Phantom model and NeedleTrainer model were given high scores in confidence level to identify critical structure using ultrasound imagery. In summary, from Table 3 we can see that among the Blue Phantom group, there were higher recorded scores in terms of learning satisfaction (28 ± 4 vs 25 ± 4, p = 0.003) and post-training confidence scores (13 ± 2 vs 12 ± 2, p < 0.001). Preference for the Blue Phantom training model was indicated by 26 out of 47 participants, as opposed to the NeedleTrainer model, which was favoured by a mere 7 participants.
Evaluations of homogeneity were performed across dependent variables in relation to each category of demographic data (Tables 4, 5 and 6). Participants aged 30 and younger demonstrated a statistically longer Time-to-Target (TTT) for both Blue Phantom and NeedleTrainer models and manifested a lower overall confidence score for the NeedleTrainer model relative to those aged 36 and above. We found that female participants have significantly higher learning satisfaction scores (28.0 ±2.0 vs 25.0 ±3.0, p=0.005) and confidence scores after training (15.0 ±3.0 vs 12.5±1.5, p=0.015) for the Blue Phantom model compared to male participants. Additionally, medical officers within the cohort showed a significantly lower overall confidence score for the NeedleTrainer model when compared to Masters-level trainees.
Table 4.
Sub-analysis of TTT achieved among participants in Blue Phantom and NeedleTrainer group
| Blue Phantom | NeedleTrainer | |||||
|---|---|---|---|---|---|---|
| TTT (sec) | p- Value | Post-hoc p-valuec | TTT (sec) | p- Value | Post-hoc p-valuec | |
| Gender | 0.425a | NA | 0.820a | NA | ||
| Male | 14 [8–21] | 8 [6–9] | ||||
| Female | 16 [8–26] | 7 [5–12] | ||||
| Age | 0.018b | ≤ 30—≥ 36 (0.016) | 0.028b | ≤ 30—≥ 36 (0.038) | ||
| ≤ 30 | 23[18–29] | 10 [7–22] | ||||
| 31–35 | 15 [8–24] | 7 [5–9] | ||||
| ≥ 36 | 11 [8–15] | 6 [4–10] | ||||
| Designation | 0.056b | NA | 0.225b | NA | ||
| Specialist | 13 [8–19] | 6 [4–7] | ||||
| Masters Trainee | 9 [8–16] | 8 [5–11] | ||||
| Medical Officer | 21 [12–26] | 8 [6–12] | ||||
| Anaesthetic experience | 0.051b | NA | 0.756b | NA | ||
| < 5 | 19 [12–24] | 8 [6–11] | ||||
| 5–10 | 12 [8–21] | 7 [5–9] | ||||
| > 10 | 8 [8–11] | 7 [4–12] | ||||
| Frequency of performing RA | 0.128b | NA | 0.262b | NA | ||
| Once a week | 11 [7–14] | 6 [5–8] | ||||
| Once a month | 17 [8–26] | 8 [5–12] | ||||
| Once a year | 23 [8–38] | 8 [6–36] | ||||
| Never | 18 [14–21] | 7 [6–9] | ||||
aMann–Whitney Test, b Independent Kruskal Wallis Test, c post-hoc significance values adjusted by the Bonferroni correction for multiple tests
Table 5.
Sub-analysis of learning satisfaction among participants in Blue Phantom and NeedleTrainer group
| Blue Phantom | NeedleTrainer | |||
|---|---|---|---|---|
| Learning satisfaction | p-Value | Learning satisfaction | p-Value | |
| Gender | 0.005a | 0.863a | ||
| Male | 25.0 [23.25–28.0] | 24.5 [21.5–28.5] | ||
| Female | 28.0 [26.0–30.0] | 26.0 [21.0–29.0] | ||
| Age | 0.160b | 0.080b | ||
| ≤ 30 | 27.5 [23.0–28.0] | 24.5 [18.75–27.25] | ||
| 31–35 | 26.5 [24.25–29.75] | 24.5 [21.0–28.75] | ||
| ≥ 36 | 30.0 [26.0–30.0] | 29.0 [24.5–30.0] | ||
| Designation | 0.555b |
0.033b (Post-hoc not significant c) |
||
| Specialist | 28.0 [24.5–30.0] | 27.5 [24.5–30.0] | ||
| Masters Trainee | 28.0 [26.0–30.0] | 27 [21.25–30.0] | ||
| Medical Officer | 27.0 [24.0–29.0] | 24 [20- 27] | ||
| Anaesthetic experience | 0.619b | 0.779b | ||
| < 5 | 27.5[24.0–29.0] | 25.0[21.0–28.0] | ||
| 5–10 | 28.0[25.25–30.0] | 25.0[21.25–29.75] | ||
| > 10 | 26.0[20.0–30.0] | 26.0 [23.0–30.0] | ||
| Frequency of performing RA | 0.795b | 0.485b | ||
| Once a week | 27.5 [26.0–29.75] | 26.5[21.25–29.75] | ||
| Once a month | 27 [23.25–30.0] | 24.5[21–27.75] | ||
| Once a year | 28.0 [23.0–30.0] | 24.0 [17.0–28.0] | ||
| Never | 27.5 [24.0–30.0] | 26.0 [23.25–28.75] | ||
aMann–Whitney Test, b Independent Kruskal Wallis Test, c post-hoc significance values adjusted by the Bonferroni correction for multiple tests
Table 6.
Sub-analysis of confidence scores among participants in Blue Phantom and NeedleTrainer group
| Blue Phantom | NeedleTrainer | |||
|---|---|---|---|---|
| Confidence | p-Value | Confidence | p-Value | |
| Gender | 0.015a | 0.377a | ||
| Male | 12.5 [11.25–14.0] | 11.5 [9.0–13.75] | ||
| Female | 15.0 [12.0–15.0] | 12.0 [10.0–13.0] | ||
| Age | 0.613b |
0.017b (≤ 30—≥ 36 (0.017) c) |
||
| ≤ 30 | 13.0[12.0–15.0] | 10.5 [9.0–13.0] | ||
| 31–35 | 13.0[12.0–15.0] | 12.0 [10.0–13.0] | ||
| ≥ 36 | 15.0 [12.0–15.0] | 14.0 [12.0–15.0] | ||
| Designation | 0.741b |
0.010b (Medical Officer-Masters Trainee (0.031)c) |
||
| Specialist | 13.0 [12.0–15.0] | 13.0 [12.0–15.0] | ||
| Masters Trainee | 13.5 [12.25–15.0] | 13.0 [12.25–15.0] | ||
| Medical Officer | 13.0 [12.0–15.0] | 11.0 [9.0–12.0] | ||
| Anaesthetic experience | 0.757b | 0.164b | ||
| < 5 | 13.0[12.0–14.75] | 12.0[10.0–13.0] | ||
| 5–10 | 14.5[12.0–15.0] | 12.5[10.25–13.75] | ||
| > 10 | 15.0[9.0–15.0] | 15.0[12.0–15.0] | ||
| Frequency of performing RA | 0.841b | 0.090b | ||
| Once a week | 13.0 [12.0–15.0] | 13.0 [12.0–14.75] | ||
| Once a month | 13.0 [12.0–15.0] | 11.5 [10.0–12.0] | ||
| Once a year | 13.0[10.0–15.0] | 9.0[8.0–13.0] | ||
| Never | 13.5 [12.0–15.0] | 12.5 [10.25–14.75] | ||
aMann–Whitney Test, b Independent Kruskal Wallis Test, c post-hoc significance values adjusted by the Bonferroni correction for multiple tests
Discussions
Both Blue Phantom and NeedleTrainer ultrasound simulators are advanced tools used for RA training without the risk of harming real patients. The Blue Phantom model is designed with patented materials that closely match the feel of human tissue when being inserted with a needle. It can also replicate the acoustic characteristics of human tissue, allowing users to experience ultrasound imaging as they would during scanning of real patients. The simulated skin can endure at least 1000 needle sticks without compromising its integrity [6, 7]. In comparison, the new NeedleTrainer enables operators to scan real human volunteer body and practice inserting a blunt retractile needle towards a chosen target. Although this simulator lacks the tactile feedback of real-life needle insertion, the holographic needle image allows operators to learn the necessary movements for precise needle placement in human [9, 14].
In this crossover study, the Blue Phantom model is found to have a longer TTT, higher first pass success rate and lower complication rate compared to the NeedleTrainer model. The high success and low complication rate can be attributed to the highly realistic tactile feedback and acoustic characteristics of the ultrasound imaging that closely match the feel of human tissue [6, 7]. However, the impressive success and complication rate could also potentially stem from an excessively clear needle visibility in the ultrasound imaging, which may not accurately reflect real-world clinical scenarios [7]. This heightened visibility could possibly explain the significantly higher learning satisfaction and confidence scores regarding ultrasound beam optimization for needle localization among participants in this study. Other than that, considering that the Blue Phantom model has existed for quite some time, participants might have prior skill acquisition in using the model compared to the novice NeedleTrainer.
On the other hand, the higher TTT of the Blue Phantom model may result from the resistance offered by the replicated tissue itself against the needle. A previous research with the same findings suggested that novice anaesthetic practitioners often take more time to reach their target using the Blue Phantom model as compared to other simulation models due to the relatively lower image quality to identify ultrasonographic artifacts [15]. This study also found that the median score for learning satisfaction in identifying critical structure from ultrasound imaging is one point lower for Blue Phantom compared to NeedleTrainer however the difference is not statistically significant.
As for the NeedleTrainer, participants of this research had lower TTT, lower first pass success rate and higher complication rate associated with this model. The lack of tactile resistant, the real-time scanning on a real subject and the incorporation of artificial intelligence structure recognition software in the NeedleTrainer can be the factors that contributed to the significant reduction in TTT compared to the Blue Phantom model. On the flip side, the NeedleTrainer models exhibit a lower first pass-success rate and a higher complication rate, which contradicts their intended benefits [9, 14]. Here we can see that while the NeedleTrainer simulator specializes in offering real subject ultrasound scanning experience to train in directing the needle towards the target while avoiding vascular puncture, the opposite might occur in especially those who are not familiar with the simulator. Since NeedleTrainer model is novice for RA training, adaptation by trainees with the simulator is needed in order to meet the learning objectives and fully potentiate the model’s capability [10, 11, 16]. The retractable needle of the NeedleTrainer is also a significant drawback because it results in the lack of tactile feedback from tissue resistance during needle insertion which possibly caused the trainees to advance the needle faster and overshot into inadvertent vascular or pleural puncture during the simulation [9, 14]. This might explain why there are significantly lower learning satisfaction and confidence scores regarding hand-eye coordination improvement for the NeedleTrainer compare to the Blue Phantom model in this study. Development of tactile skill is one of the objectives that need to be achieved by the simulator model in order to mimic real-life experience. Kumar et al. (2022) reinforce that high-fidelity simulation, including tactile feedback, aids in realistic practice and better skill transfer to clinical environments [16]. This is particularly crucial for needle-based procedures, where tactile cues are directly linked to procedural safety and accuracy [16]. The inability to replicate this variation of real-life experience would not just affect the learning experience and confidence scores of participants, but could also affect the transferability of skills from the simulated environment to actual clinical settings [17, 18].
Additionally, this study’s findings point that participants aged 30 and younger demonstrated a statistically longer TTT for both Blue Phantom and NeedleTrainer models. Although age does not directly proportionate to experience, we assume older participants have more experience and higher designation in the clinical field thus tend to possess higher clinical skills compared to younger participants . Previous studies found that performance scores using a simulated ultrasound-guided RA model, measured by the step-by-step metrics, are higher among experienced participants compared to novices [19, 20]. Other than that, this study revealed that female participants reported notably higher overall learning satisfaction and confidence scores for the Blue Phantom compared to male participants. At the same time, participants aged 30 years old and below and medical officers demonstrated significantly lower post-training confidence scores when using the NeedleTrainer, in contrast to those aged 36 years old and older and Masters trainees, respectively.
The above data points out that trainees with different background might have different degrees of inclination towards different simulation models for the purpose of RA training. Both the phantom model and the AR system are complementary tools that can help novice RA practitioner to gain competency and confidence in their technical skills. As an emerging technology, AR has the potential to aid in the development of effective, clinically efficient RA skills that can be easily adopted in any practice [4, 10, 11, 21]. However, it’s clear that no single modality is sufficient on its own to train the diverse skills required for performing regional anaesthesia. For this reason, it is good to emphasize the need to make available tailored simulation programs to adapt to the specific learners’ needs according to their level of expertise and preferences [16, 18, 22]. Afterall, the purpose of simulated training is to aid in development of clinical competency regardless of the simulator’s degree of fidelity or sophistication.
In light of our data, novice RA practitioners in this study expressed a preference for the Blue Phantom model and recommended its use for future training. The high overall scores of learning satisfaction and confidence level of the model are likely to contribute to this preference. Nevertheless, when choosing a simulation model for the purpose of training, it is important to consider factors such as cost, accessibility, availability of expert instructors and skill transferability rate [8, 23, 24]. Therefore, further validation and feedback from trainees and trainers with larger sample sizes are required to determine the efficacy of using any simulation models for purpose of RA training. The benefit-cost ratio of different models as well as the clinical competency achieved by participants undergoing different training models should also be considered.
It is important to note that the study had a few limitations. This includes its small sample size which were recruited through convenience sampling. Moreover, participants were only given two practice trials before being assessed which may have been insufficient to facilitate adequate skill acquisition in using both simulation models and the study was not blinded. Furthermore, the study evaluated different target positions (supraclavicular block and brachial plexus block) and did not inquire about participants' prior experience of using the Blue Phantom model which both might affect the training experience.
Conclusions
The study highlights the potential of AR in RA training. We postulated that the real subject scanning experience and the incorporation of artificial intelligence structure recognition software enable NeedleTrainer users to attain shorter time-to-target. Putting it all together, Blue Phantom model provides better operator learning satisfaction, improved confidence, higher success and lower complication rates among novice RA practitioners, possibly due to greater tactile feedback during the simulated training. Having said that, both simulators serve to enhance the skills of healthcare professionals in ultrasound-guided procedures, ensuring safer and more effective patient care.
Acknowledgements
We would like to express out gratitude to Faculty of Medicine, Universiti Kebangsaan Malaysia for giving us the opportunity to conduct this study.
Authors’ contributions
MNM, CWK, IK, TKW, ALCC, MB, AS, AA, VVSM are responsible for the initial study conceptualization. SAS, CWK, IK, TKW, ALCC, MB, AS, AA, VVSM contributed in data acquisition, data analysis and original manuscript drafting. MNM critically review and edit the manuscript. MNM and AI supervised the research activity. All authors have read and agreed to publish the final version of the manuscript.
Funding
The research was funded by the Faculty of Medicine, Universiti Kebangsaan Malaysia (research code: FF-2023–050).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participte
This study is approved by the UKM Ethics Review Board (approval code: JEP-2023-072), on 13th February 2023.
Consent for publication
Informed consent were taken prior to respondents’ participation in this study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mohammad Nizam Mokhtar, Siti Aisyah Suhaini, Weng Ken Chan, Iskandar Khalid, Kok Wang Tan, Angelina Chia Chia Lim, Maryam Budiman, Afifah Samsudin, Asmah Azizeh, Vimal Varma Spor Madiman and Azarinah Izaham contributed equally.
References
- 1.Barrington MJ, Wong DM, Slater B, Ivanusic JJ, Ovens M. Ultrasound-Guided Regional Anesthesia: How Much Practice Do Novices Require Before Achieving Competency in Ultrasound Needle Visualization Using a Cadaver Model. Regional Anesth Pain Med. 2012;37:334. Available from: http://rapm.bmj.com/content/37/3/334.abstract. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health and Social Care. A framework for technology enhanced learning - GOV.UK. 2011 [cited 2024 Jan 27]. Available from: https://www.gov.uk/government/publications/a-framework-for-technology-enhanced-learning.
- 3.Al-Elq AH. Simulation-based medical teaching and learning. J Family Community Med. 2010;17:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Privorotskiy A, Garcia VA, Babbitt LE, Choi JE, Cata JP. Augmented reality in anesthesia, pain medicine and critical care: a narrative review. J Clin Monit Comput. 2022;36:33–9. [DOI] [PubMed] [Google Scholar]
- 5.Taylor A, McLeod GA. Simulation Models in Ultrasound-Guided Regional Anesthesia. 2018 [cited 2024 Jan 27]. Available from: https://www.asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2018/11/09/simulation-models-in-ultrasound-guided-regional-anesthesia.
- 6.CAE Healthcare - CAE Blue Phantom | CAE Healthcare. [cited 2024 Feb 12]. Available from: https://www.caehealthcare.com/solutions/brands/cae-blue-phantom.
- 7.Lahham S, Smith T, Baker J, Purdy A, Frumin E, Winners B, et al. Procedural simulation: medical student preference and value of three task trainers for ultrasound guided regional anesthesia. World J Emerg Med. 2017;8:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuel J, Kerr E, Young D, Watson M, Raj D. The use of joints of meat as phantoms for ultrasound-guided needling skills: a prospective blinded study. Ultrasound J. 2022;14(1):14. 10.1186/s13089-022-00263-9. [DOI] [PMC free article] [PubMed]
- 9.NeedleTrainer - Intelligent Ultrasound. [cited 2024 Jan 27]. Available from: https://www.intelligentultrasound.com/needletrainer/.
- 10.Alam F, Matava C. A new virtual world? The future of immersive environments in anesthesiology. Anesth Analg. 2022;135:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shevlin SP, Turbitt L, Burckett-St Laurent D, Macfarlane AJ, West S, Bowness JS. Augmented Reality in Ultrasound-Guided Regional Anaesthesia: An Exploratory Study on Models With Potential Implications for Training. Cureus. 2023;15(7):e42346. 10.7759/cureus.42346. [DOI] [PMC free article] [PubMed]
- 12.Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick’s four levels of training evaluation. ATD Press; 2016.
- 13.Khalid I, Chan WK. Anatomy & Ultrasonography for Regional Anaesthesia (AURA) 2023: An Anaesthesia Competency Training in Immersive Virtual Environment (ACTIVE). Berita Anestesiologi. 2023;35:12–4. [Google Scholar]
- 14.Evans A, Shevlin S, Turbitt L, Burkett-St Laurent D, Bowness J, Hunter L, et al. Pilot study to explore if an augmented reality NeedleTrainer device improves novice performance of a nerve block on a phantom. Br J Anaesth. 2022;129:e109–10. [Google Scholar]
- 15.Dang D. Abstract No. : ABS0260: Comparison of phantom cadaver based simulations with blue phantom model for teaching ultrasound guided regional anaesthesia: a randomised controlled trial. Indian J Anaesth. 2022;66:S59.
- 16.Kumar AH, Sultan E, Mariano ER, Udani AD. A modern roadmap for the use of simulation in regional anesthesiology training. Curr Opin Anaesthesiol. 2022;35:654–9. [DOI] [PubMed] [Google Scholar]
- 17.McGaffey M, Linden AZ, Sears W, Monteith G, Khosa DK, Blois SL. Teaching Accuracy Through Repeated Gamified Echography Training (TARGET): Assessment of an Ultrasound Skill Simulator in Teaching Ultrasound-Guided Needle Placement, a Prospective Observational Study. J Vet Med Educ. 2024;51(1):95-103. 10.3138/jvme-2022-0131. [DOI] [PubMed]
- 18.Kumar AH, Udani AD. Simulation in Regional Anesthesia. In: Mahoney B, Minehart R, Pian-Smith M, editors. Comprehensive Healthcare Simulation: Anesthesiology. Springer: Cham; 2019. p. 257–64. [Google Scholar]
- 19.Chuan A, Qian J, Bogdanovych A, Kumar A, McKendrick M, McLeod G. Design and validation of a virtual reality trainer for ultrasound-guided regional anaesthesia. Anaesthesia. 2023;78:739–46. [DOI] [PubMed] [Google Scholar]
- 20.Savage M, Spence A, Turbitt L. The educational impact of technology-enhanced learning in regional anaesthesia: a scoping review. Br J Anaesth. 2024;133(2):400–15. 10.1016/j.bja.2024.04.045. [DOI] [PubMed]
- 21.Ramlogan RR, Chuan A, Mariano ER. Contemporary training methods in regional anaesthesia: fundamentals and innovations. Anaesthesia. 2021;76:53–64. [DOI] [PubMed] [Google Scholar]
- 22.Walsh CD, Ma IWY, Eyre AJ, Dashti M, Stegeman J, Dias RD, et al. Implementing ultrasound-guided nerve blocks in the emergency department: A low-cost, low-fidelity training approach. AEM Educ Train. 2023;7(5):e10912. 10.1002/aet2.10912. [DOI] [PMC free article] [PubMed]
- 23.Kim TE, Tsui BCH. Simulation-based ultrasound-guided regional anesthesia curriculum for anesthesiology residents. Korean J Anesthesiol. 2018;72:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen XX, Trivedi V, Alsaflan AHA, Todd SC, Tricco AC, McCartney CJL, et al. Ultrasound-guided regional anesthesia simulation training: a systematic review. Reg Anesth Pain Med. 2017;42:741–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.