Abstract
A 60-year-old woman was admitted to the hospital with “repeated loss of consciousness for 20 years.” An electrocardiogram performed revealed sinus rhythm, and echocardiography, head/chest CTs, and a laboratory examination yielded no significant abnormalities. Besides, there were no positive results from the head-up tilt test. The subsequent decrease in heart rate and blood pressure following the ingestion of chili pepper indicated a potential case of vasovagal syncope(VVS) with cardioinhibition. Following cardioneuroablation, there was an observed increase in heart rate compared to pre-procedure levels. Furthermore, no recurrence of similar symptoms was reported during the one-year follow-up period.
Keywords: Cardioneuroablation, Vasovagal syncope, chili pepper stimulation, VVS
Introduction
Vasovagal syncope (VVS) is the predominant subtype of reflex syncope and represents the most prevalent etiology of syncope across all age demographics.1 Preceding the onset of VVS are discernible triggers such as prolonged standing, alterations in body position, pharmacological agents, alcohol consumption, and emotional fluctuations.2 The hallmark features of VVS include a transient loss of consciousness secondary to systemic hypotension and diminished cerebral perfusion, often accompanied by manifestations such as diaphoresis, emesis, pallor, and other associated symptoms. We report a case of syncope diagnosed as VVS by chili pepper consumption and successfully treated by cardioneuroablation.
Case Presentation
The patient was a 60-year-old woman who had been experiencing repeated loss of consciousness for over 20 years. Before the onset, there were obvious causes such as eating irritating food, defecation and fatigue. Electrocardiograms, holter electrocardiograms, and head-up tilt test were all normal for the patient in the hospital. She has no history of cardiovascular diseases.
Upon admission, the patient presented with a heart rate of 55 beats/min and a blood pressure of 140/90mmHg. Physical and laboratory tests revealed no obvious abnormalities, and the electrocardiogram showed sinus bradycardia. Echocardiography indicated mild aortic valve insufficiency, with the rest of the heart structure and function appearing normal. A lung CT scan revealed a few micronodules in both lungs, while a craniocerebral CT scan showed no significant abnormalities.
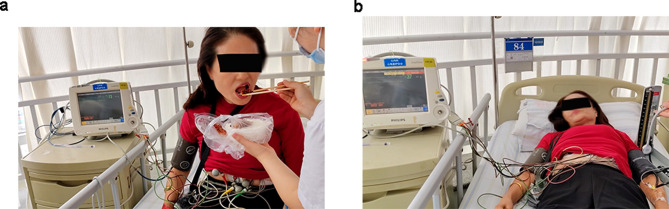
Given the patient’s history of syncope episodes occurring after the consumption of spicy foods such as hot peppers, it was hypothesized that the syncope might be related to this. Despite several upright tilt tests yielding no positive findings, with informed consent, a “chili pepper stimulation” experiment was conducted on the patient. During the experiment, it was observed that the patient’s blood pressure before consuming the pepper was 125/83mmHg, and the heart rate was 73 beats per minute. After consuming the pepper for 5 minutes, the patient experienced nausea and dizziness, followed by a gradual drop in heart rate to 37 beats/min and a drop in blood pressure to 56/37 mmHg, along with cold limbs and foggy consciousness (Figure 1). The patient was promptly administered atropine, dopamine, and continuous fluid rehydration, leading to a gradual recovery of blood pressure to 150/80mmHg and a heart rate of 90 beats/min. Based on the patient’s history and attack characteristics, the initial diagnosis was VVS.
Figure 1.
(a) The patient’s blood pressure was 125/83mmHg and heart rate was 73 beats/min before chili pepper stimulation. (b) After taking pepper, the heart rate reduced to 37 beats/min, and the blood pressure reduced to 56/37mmHg.
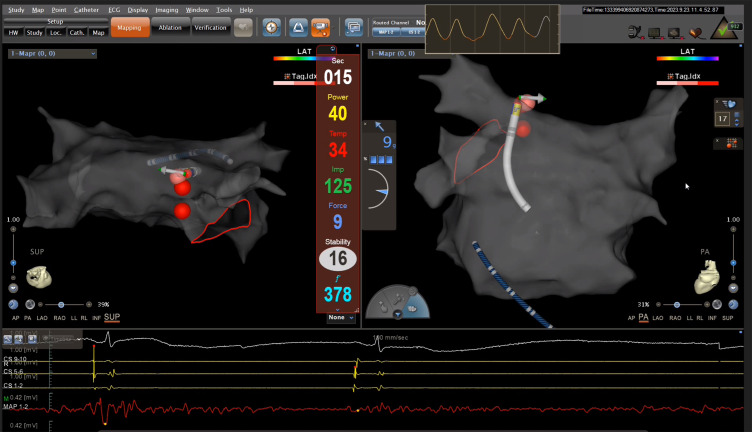
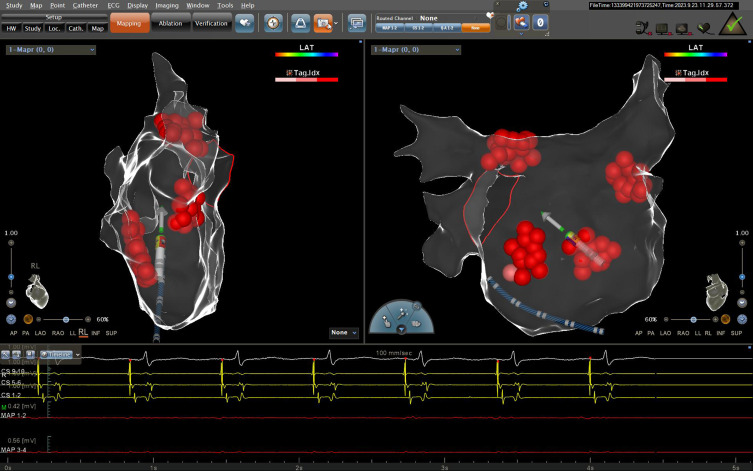
Despite unsuccessful medical interventions, the patient’s quality of life had been significantly impacted by recurrent syncope episodes. Consequently, a decision was made to proceed with the ablation of the cardioneuroablation. A cardiac electrophysiological study was performed before surgery. As a result, the sinoatrial conduction time, sinus node recovery time, and effective refractory period of the atrioventricular node were all normal for the patient. During ablation, we observed a decrease in heart rate and sinus arrest due to the vagus response caused by radiofrequency energy delivery to the left upper ganglion plexus (Figure 2). Following ventricular pacing protection, there was a notable increase in sinus heart rate subsequent to anatomic ablation at specific locations, including the left superior GP (LSGP; located in the superolateral area around the root of the left superior pulmonary vein), left inferior GP (LIGP; located in the inferoposterior area around the root of the left inferior pulmonary vein), right inferior GP (RIGP; located in the inferoposterior area around the root of the right inferior pulmonary vein), right anterior GP (RAGP; located in the superior-anterior area around the root of the right superior pulmonary vein) (Figure 3). Pepper stimulation did not induce arrhythmia after surgery, and head-up tilt testing did not reveal any abnormality. Subsequent to a one-year follow-up, the patient remained asymptomatic.
Figure 2.
Stimulation of cardiac ganglia during ablation induces cardiac arrest.
Figure 3.
Distribution of cardioneuroablation targets.
Discussion
This study presents a novel case of VVS triggered by the ingestion of chili pepper. Furthermore, the patient underwent cardioneuroablation, resulting in successful recovery post-surgery. Subsequent one-year follow-up assessments revealed the absence of syncope or prodromal symptoms in the patient.
The autonomic nervous system (ANS) ‘s influence on the cardiovascular system is crucial for maintaining physiological function. The ANS influences the heart through sympathetic nerves and the vagus nerve, which connect to cardiac neuronal ganglia.3,4 VVS is one of the most common types of syncope, which is a subtype of neurally-mediated reflex syncope. Classical VVS is characterized by bradycardia and/or decreased peripheral vascular resistance due to abnormal autonomic reflexes, which can manifest as vasodepressor, cardioinhibitory, or mixed type. Our patient exhibited common symptoms, including nausea, vomiting, dizziness, and a decrease in heart rate followed by a reduction in blood pressure five minutes after ingesting pepper, a phenomenon not previously documented in literature. Potential mechanisms for capsicum-induced syncope include sinus bradycardia, hypotension, and vasovagal syncope resulting from vagal hypertonia.5 The patient had previously undergone an head-up tilt test with negative results, making this case the first reported instance of VVS induced by cayenne pepper ingestion according to the literature search.
Various interventions have been proposed for the management of VVS, including health education, lifestyle modifications, tilt training, drug therapy, and permanent pacemaker implantation for patients with cardioinhibition.6 However, the efficacy of these interventions remains suboptimal, particularly among young patients. Recent research suggests that GP catheter ablation may be a promising and safe alternative for the treatment of VVS, particularly in individuals with predominantly cardioinhibition.7 This method involves endocardial ablation of vagus nerve endings on the atrial wall, supplemented by radiofrequency application in the primary epicardial cardiac ganglion region.7–9 In this instance, the patient initially exhibited a reduction in heart rate followed by a decrease in blood pressure in cardioinhibitory VVS. Over the course of the last two decades, the patient’s medical history indicated poor response to multiple drug therapies such as Shensong Yangxin capsules, beta blockers and traditional Chinese medicine and conservative treatments. Subsequently, GP ablation was performed as an alternative to pacemaker implantation, resulting in a favorable prognosis upon follow-up. This case highlights the potential efficacy of cardioneuroablation in managing vasovagal syncope with cardioinhibition. However, the fact that no complete atropine trial was performed and that cardioneuroablation was performed without control of extracardiac vagal nerve stimulation (ECVS) was the limitations in this case.
Funding Statement
This work was funded by the National Natural Science Foundation of China (No.82160072, No.82360085), the Natural Science Foundation of Hubei Province (No.2023AFD073) and the Science and Technology Support Project of Enshi Prefecture Science and Technology Bureau (No. D20230075, D20230079).
Ethical Approval and Patient Consent
The details of the case report were approved by the ethics committee of the Central Hospital of Enshi Tujia and Miao Autonomous Prefecture. Written consent was obtained from the patient for the publication of the case details and related images. Publication of case details is exempt from institutional approval.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Li L, Po S, Yao Y. Cardioneuroablation for treating vasovagal syncope: current status and future directions. Arrhythm Electrophysiol Rev. 2023;12:e18. PMID: 37457436; PMCID: PMC10345939. doi: 10.15420/aer.2023.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armani Prata A, Katsuyama E, Scardini P, et al. Cardioneuroablation in patients with vasovagal syncope: an updated systematic review and meta-analysis. Heart Rhythm. 2024;25:S1547–5271(24)03079–0. PMID: 39067734. doi: 10.1016/j.hrthm.2024.07.103 [DOI] [PubMed] [Google Scholar]
- 3.Amir B, Lanciano SB, Rubinshtein R, Nussinovitch U. Autonomic responses in young females with typical vasovagal syncope. Intern Emerg Med. 2024;19:1345–1351. PMID: 38700783. doi: 10.1007/s11739-024-03622-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: relationship to vasovagal syncope and theBezold-Jarisch reflex. Br J Anaesth. 2001;86(6):859–868. doi: 10.1093/bja/86.6.859 [DOI] [PubMed] [Google Scholar]
- 5.Alboni P, Alboni M. Typical vasovagal syncope as a “defense mechanism” for the heart by contrasting sympathetic overactivity. Clin Auton Res. 2017;27(4):253–261. PMID: 28669087. doi: 10.1007/s10286-017-0446-2 [DOI] [PubMed] [Google Scholar]
- 6.Sutton R, de Jong JSY, Stewart JM, Fedorowski A, de Lange FJ. Pacing in vasovagal syncope: physiology, pacemaker sensors, and recent clinical trials-Precise patient selection and measurable benefit. Heart Rhythm. 2020;17(5 Pt A):821–828. PMID: 32036025; PMCID: PMC7196018. doi: 10.1016/j.hrthm.2020.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pachon JC, Pachon EI, Pachon JC, et al. “Cardioneuroablation”--new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace. 2005;7(1):1–13. PMID: 15670960. doi: 10.1016/j.eupc.2004.10.003 [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Luo D, Liu S, et al. Selective ablation of atrial ganglionated plexus attenuates vasovagal reflex in a canine model. Pacing Clin Electrophysiol. 2019;42(1):13–19. PMID: 30426527. doi: 10.1111/pace.13547 [DOI] [PubMed] [Google Scholar]
- 9.Aksu T, Brignole M, Calo L, et al. Cardioneuroablation for the treatment of reflex syncope and functional bradyarrhythmias: a scientific statement of the European Heart Rhythm Association (EHRA) of the ESC, the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS) and the Latin American Heart Rhythm Society (LAHRS). Europace. 2024;26(8):euae206. PMID: 39082698; PMCID: PMC11350289. doi: 10.1093/europace/euae206 [DOI] [PMC free article] [PubMed] [Google Scholar]