Abstract
OBJECTIVES:
We sought to describe the indications for vasoactive medication administration, hemodynamic treatment targets, and specific agents used by various international emergency medical service (EMS) providers.
DESIGN AND SETTING:
In March 2022, we sent an online survey comprising of 20 questions to Medical Directors of EMSs across Australia, the Asia Pacific region, and North America.
PATIENTS:
A total of 108 EMS directors were emailed an invitation to participate.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Twenty-five EMS medical directors responded. Local site guidelines for vasoactive agent administration were available to 77.3% of providers. Epinephrine was commonly used as first-line vasoactive agent in 52% of questionnaire respondents, followed by norepinephrine (22%), dopamine (18%), and metaraminol (4%). Epinephrine was the most commonly used vasoactive agent across all forms of shock, with a higher proportion of utilization in cases of cardiogenic shock (58%) and patients suffering shock following cardiac arrest (56%).
CONCLUSIONS:
International EMS vasoactive use in the management of shock is heterogeneous. Future randomized controlled trials should aim to elucidate optimal prehospital treatment strategies for shock, including the initiation, choice of agent, and monitoring of vasoactive medication.
Keywords: emergency medical services, prehospital shock, shock, survey, vasoactive medication
KEY POINTS
Question: In a survey of international emergency medical service (EMS) providers, what are the hemodynamic treatment targets and specific agents used for management of prehospital shock?
Finding: International EMS vasoactive use in the management of shock is heterogeneous. Local site guidelines for vasoactive agent administration were available to 77.3% of providers. Epinephrine was commonly used as first-line vasoactive agent in 52% of questionnaire respondents. There was heterogeneity in utilization of vasoactive medications for different shock classifications.
Meaning: Randomized control data is required to develop systemic guidelines for management of prehospital shock.
Shock is a clinical syndrome that is characterized by cellular and tissue hypoxia due to either inadequate oxygen delivery, increased oxygen demand, or a combination of these processes (1). Patients present on a spectrum of illness severity, ranging from occult hypoperfusion (with preserved blood pressure) to fulminant circulatory collapse (1). In addition to treating the underlying pathology, prompt hemodynamic support is essential to augment cardiac output and improve systemic perfusion in order to restore cellular metabolism and limit the development of end-organ injury and dysfunction (2). The use of vasoactive medications to increase systemic vascular resistance and augment cardiac output constitute an essential element of the supportive care of this patient cohort. Despite the routine use of these agents in both the in-hospital and prehospital setting, there is a lack of data defining the current prescribing practices of emergency medical services (EMSs), limiting the development of standardized management guidelines (3). Through this study, we surveyed EMS medical directors with the aim of describing the indications for vasoactive medication administration, hemodynamic treatment targets, and specific agents used by various international EMS providers.
METHODS
In March 2022, we conducted an online survey of Medical Directors of EMSs across the Asia Pacific region and North America. Participation in the survey was voluntary and the study was approved by Alfred Health’s Human Research Ethics Committee (HREC 737/21; Project title: Current emergency medical service vasoactive use for the management of shock; approval date February 15, 2022). The survey was implemented with the National Statement on Ethical Conduct in Human Research 2023 (Australia) and with the Declaration of Helsinki.
A total of 108 EMS directors were emailed an invitation to participate, and the survey link was disseminated to via the Council of Ambulance Authorities Clinical Forum and the EMS Eagles Global Alliance. The survey was completed on the Qualtrics survey platform (Qualtrics, Provo, UT. https://www.qualtrics.com) and included a total of 20 questions addressing institutional protocols for prehospital care. The survey featured both multiple-choice and open-ended questions (Supplementary Data, http://links.lww.com/CCX/B431). Questions were derived from the findings of previous work (4, 5) and on consensus from experts in resuscitation from the Australian Resuscitation Outcomes Consortium. Before distribution, the questionnaire was piloted at hospitals associated with the study investigators; however, the pilot results were excluded from the final analysis to ensure data integrity and consistency. All responses from the final survey were included in the analysis, with no exclusions.
The data analyses were descriptive, and categorical variables were expressed as frequencies and compared by chi-square or Fisher exact test. Statistical analysis was performed in Stata (SE 18; StataCorp, College Station, TX) with a p value of less than 0.05 considered statistically significant.
RESULTS
A total of 25 EMS providers responded to the survey corresponding to a response rate of 23%. Responders were predominantly representing North American EMS providers (80%). Baseline demographic data of EMS provider services are provided in Table 1. Local site guidelines for hemodynamic parameters prompting vasoactive agent administration were available to 17 responders (77.3%). Vasoactive medications were administered by 88% of EMS providers. Clinical parameters for medication administration were reported by 28% of providers, including abnormal mentation (20%) and cool peripheries (8%). The skill set of EMS providers, and their respective eligibility to administer vasoactive medications was diverse, with critical care paramedics working across 44% of EMS services.
TABLE 1.
Emergency Medical Service Survey Provider Characteristics
| EMS location region (n = 25) | Shock evaluation | ||
| Asia/Pacific North America |
5 (20.0%) 20 (80.0%) |
Does your service have guidelines relating to hemodynamic parameters at which vasoactive infusions should be commenced? (n = 22) | |
| Yes No |
17 (77.3%) 5 (22.7%) |
||
| How many EMS providers are employed by your service? (n = 25) | In addition to hypotension, which other parameters would prompt EMS providers to commence a vasoactive infusion based on your service’s guidelines? (n = 25) | ||
| 0–100 100–1000 1000–5000 > 5000 |
3 (12.0%) 7 (28.0%) 11 (44.0%) 4 (16.0%) |
Cool peripheries | 2 (8.0%) |
| Abnormal mentation | 5 (20.0%) | ||
| Anaphylaxis | 1 (4.0%) | ||
| Tachycardia | 3 (12.0%) | ||
| Stroke | 2 (8.0%) | ||
| Bradycardia | 1 (4.0%) | ||
| No additional parameters | 18 (72.0%) | ||
| Does you service employ critical care/intensive care paramedics? (n = 25) | |||
| Yes | 11 (44.0%) | ||
| No | 14 (56.0%) | ||
| Can your EMS providers administer vasoactive medication infusions? (n = 25) | Before initiating a vasoactive infusion is a trial of fluid administration required? (n = 22) | ||
| Yes No |
22 (88.0%) 3 (12.0%) |
Yes No |
13 (59.1%) 9 (40.9%) |
| Which EMS providers are accredited to administer these agents in your service? (n = 22) | |||
| Medical doctor | 11 (50.0%) | ||
| Critical care paramedics | 9 (40.9%) | ||
| Advanced life support paramedics | 16 (72.7%) | ||
| Basic life support paramedic | 1 (4.5%) | ||
EMS = emergency medical service.
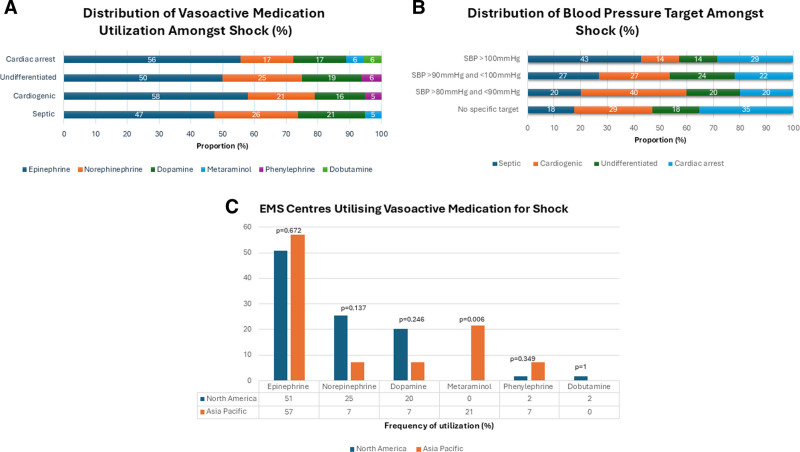
A fluid bolus challenge was recommended by 59% of providers before commencement of vasoactive medications. Use of vasoactive medications is summarized in Figure 1C. Cumulatively, epinephrine was the most used first-line vasoactive medication, administered in 52% of questionnaire respondents, followed by norepinephrine (22%), dopamine (18%), and metaraminol (4%). There was no statistically significant difference in rates of prescription in epinephrine (51% vs. 57%; p = 0.672), norepinephrine (25% vs. 7%; p = 0.137), and dopamine (20% vs. 7%; p = 0.246) among respondents of North America than the Asia Pacific. Metaraminol was solely prescribed among respondents in the Asia Pacific (21% vs. 0%; p < 0.05), while dobutamine was solely prescribed among respondents in North America (2% vs. 0%; p = 0.349). There was heterogeneity in the utilization of vasoactive medications for different shock classifications (Fig. 1A) and therapeutic systolic blood pressure targets across all forms of shock (Fig. 1B). Epinephrine appears to be most used vasoactive agent across all forms of shock, with a higher proportion of utilization in cases of cardiogenic shock (58%) and shock following cardiac arrest (56%). Use of phenylephrine is noted in cardiogenic (5%) and undifferentiated shock (6%).
Figure 1.
Emergency medical service (EMS) vasoactive agent use and systolic blood pressure (SBP) targets for shock. A, Distribution of vasoactive medication among different categories of shock. B, Blood pressure targets among shock categories. C, EMS center vasoactive medication utilization for shock.
DISCUSSION
To our knowledge, this is the first study describing the heterogeneity in clinical practice of vasoactive agent use among prehospital EMS providers in the Asia Pacific region and North America.
The heterogeneous choice of vasoactive agents by EMS providers stems from multiple possible rationales. First, despite multiple randomized controlled trials (RCTs), meta-analysis and consensus opinions, there remains equipoise with respect to the recommended first-line vasoactive agent in shock (6). Conducting RCTs in a shock population has historically been challenging and is often complicated by significant within trial heterogeneity, limiting the applicability of results to patients (1). Additionally, clinical assessment can be difficult in the prehospital setting, and compensatory mechanisms (such as vasoconstriction) can confound vital sign interpretation and affect the diagnosis and characterization of shock phenotype (7). This limits the relevance of trial findings to guidelines in prehospital care. The optimal therapeutic goals for different prehospital shock classifications are unknown, likely accounting for the diversity of blood pressure targets in our study. However, more data is becoming available to support blood pressure targets, which may provide further indications on target parameters for shock patients (8).
Epinephrine emerges as the most commonly used first-line vasoactive agent across all shock domains in the prehospital setting, likely due to its accessibility and familiarity among providers. Furthermore, its broad mechanism of action across alpha-1 and beta-1 adrenergic receptors produces robust inotropic and chronotropic effects, especially at lower doses (9). However, epinephrine use has been associated with side effects including ventricular arrhythmias, metabolic acidosis, and increased lactate level (1). Recent evidence also indicates increased rates of rearrest when epinephrine is compared with norepinephrine in out-of-hospital cardiac arrest survivors (10). In light of these considerations, it is imperative to conduct further research to evaluate the safety and efficacy of epinephrine compared with other vasoactive agents in prehospital shock management. The ongoing Paramedic Randomized Trial of Noradrenaline Versus Adrenaline in the Initial Management of Patients with Cardiogenic Shock (PANDA) trial (ACTRN12621000805875) aims to address this question among patients with suspected cardiogenic shock.
In view of the lack of evidence guiding prehospital vasoactive agent administration, we advocate for further research to address key knowledge gaps. Studies are needed to determine simplified and practical parameters for initiating fluid and vasoactive therapy in the prehospital setting. RCTs are required to evaluate optimal prehospital vasoactive agents in managing shock. Ultimately, incorporating these findings into prehospital EMS guidelines will help standardize and optimize shock management practices, thereby improving patient outcomes in emergency care settings.
The small study sample size and heterogeneous patient populations limits the generalizability of results and ability to make inferences on geographical disparities in care. The methodologies used to elicit online survey responses from EMS providers might introduce response bias, which limits external validity. Additionally, the multiple-choice format of the survey may have constrained participants’ responses, limiting the depth of insights gained from the data. There is also a lack of standardized criteria for classifying shock types, which could result in variability in EMS responders shock classification. Finally, the lack of robust evidence in prehospital shock management limits the generalizability of conclusions drawn from existing studies.
CONCLUSIONS
The use of vasoactive agents in management of shock varies widely across EMS systems in the Asia Pacific region and North America. Management of prehospital shock presents significant challenges due to lack of robust evidence. There is an urgent need for well-designed trials to elucidate optimal treatment strategies, including the initiation, choice of agent, and monitoring of vasoactive agents in prehospital settings.
Supplementary Material
Footnotes
Drs. Bloom and Goel are co-first authors.
Dr. Stub is supported by the National Heart Foundation of Australia (NHFA) fellowship during the conduct of the study and receiving personal fees from Proctor for Abbott, Edwards, and Medtronic outside the submitted work and the National Health and Medical Research Council (NHMRC) investigator grant. Dr. Bloom is supported by a NHMRC and a NHFA Post-Graduate Scholarships. Dr. Goel is supported by a Monash University post-graduate scholarship. Dr. Kaye is supported by an NHMRC Investigator Grant. Dr. Nehme is supported by a NHFA fellowship. Dr. Cartledge is supported by a NHFA post-graduate fellowship. Dr. Chan reported receiving consultancy and research support from Abiomed and Johnson & Johnson. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Contributor Information
Jason E. Bloom, Email: jason.elliott.bloom@gmail.com.
David Anderson, Email: andersondavidjohn@gmail.com.
Susie Cartledge, Email: Susie.Cartledge@monash.edu.
Ziad Nehme, Email: ziad.nehme@ambulance.vic.gov.au.
Jocasta Ball, Email: jocasta.ball@monash.edu.
Amminadab Eliakundu, Email: lemmy.eliakundu@monash.edu.
William Chan, Email: william.chan@unimelb.edu.au.
Derek P. Chew, Email: derek.chew@monash.edu.
David M. Kaye, Email: david.kaye@baker.edu.au.
Dion Stub, Email: dionstub@gmail.com.
REFERENCES
- 1.Bloom JE, Chan W, Kaye DM, et al. : State of shock: Contemporary vasopressor and inotrope use in cardiogenic shock. J Am Heart Assoc. 2023; 12:e029787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thiele H, Ohman EM, Desch S, et al. : Management of cardiogenic shock. Eur Heart J 2015; 36:1223–1230 [DOI] [PubMed] [Google Scholar]
- 3.Holler JG, Bech CN, Henriksen DP, et al. : Nontraumatic hypotension and shock in the emergency department and the prehospital setting, prevalence, etiology, and mortality: A systematic review. PLoS One 2015; 10:e0119331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bray JE, Cartledge S, Finn J, et al. : The current temperature: A survey of post-resuscitation care across Australian and New Zealand intensive care units. Resusc Plus 2020; 1–2:100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheeren TWL, Bakker J, Kaufmann T, et al. : Current use of inotropes in circulatory shock. Ann Intensive Care 2021; 11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belletti A, Castro ML, Silvetti S, et al. : The effect of inotropes and vasopressors on mortality: A meta-analysis of randomized clinical trials. Br J Anaesth 2015; 115:656–675 [DOI] [PubMed] [Google Scholar]
- 7.Galvagno SMJ, Sikorski RA, Floccare DJ, et al. : Prehospital point of care testing for the early detection of shock and prediction of lifesaving interventions. Shock 2020; 54:710–716 [DOI] [PubMed] [Google Scholar]
- 8.Lamontagne F, Meade MO, Hébert PC, et al. ; Canadian Critical Care Trials Group. Higher versus lower blood pressure targets for vasopressor therapy in shock: A multicentre pilot randomized controlled trial. Intensive Care Med 2016; 42:542–550 [DOI] [PubMed] [Google Scholar]
- 9.Circulation: Vasopressors. 2008. Available at: https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.107.728840. Accessed April 5, 2024 [Google Scholar]
- 10.Wender ER, Counts CR, Van Dyke M, et al. : Prehospital administration of norepinephrine and epinephrine for shock after resuscitation from cardiac arrest. Prehosp Emerg Care 2024; 28:453–458 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.