ABSTRACT
Numerous vascular anomalies of the hepatic artery have been reported. Protection of the hepatic arterial supply is important during gastrectomy. We herein report a case in which an anatomical variant of the hepatic artery was discovered in a patient undergoing laparoscopic distal gastrectomy with D1+ lymph node dissection for early gastric cancer. A 50-year-old man was referred to our hospital because of epigastric pain and hematemesis, and he was diagnosed with early gastric cancer after hemostasis of a bleeding ulcer. Computed tomography showed an anatomical variation of the right hepatic artery, which branched from the gastroduodenal artery. Moreover, the right gastric artery branched from the right hepatic artery. Our preoperative understanding of this unusual branch of the hepatic artery enabled safe laparoscopic surgery with adequate lymph node dissection. No postoperative complications occurred. This vascular anomaly has not been previously reported in patients undergoing gastrectomy.
Keywords: gastric cancer, gastroduodenal artery, right hepatic artery
In recent years, several clinical trials have shown that laparoscopic distal gastrectomy is not inferior to open distal gastrectomy with respect to short-term outcomes.1, 2 Therefore, the application of minimally invasive surgery for gastrectomy has been expanding, and more delicate techniques are required. If the presence of vascular anomalies is not understood, inadequate lymph node dissection or unexpected complications may occur.
In this case report, we describe a rare vascular anatomical anomaly in which the right hepatic artery (RHA) branched from the gastroduodenal artery (GDA) and the right gastric artery (RGA) branched from the RHA in a patient undergoing gastrectomy for gastric cancer. The Michels classification is widely used for anatomical variants of the hepatic artery; however, it was difficult to apply in our case, and the estimated incidence of vascular anomalies is only 0.1–2.5%.3,4,5 The correlation between the hepatic artery and gastric artery is an important factor in gastrectomy. An abnormal hepatic vascular anomaly, not only in gastrectomy but also in hepatobiliary and pancreatic surgery, increases the risk of injury to the hepatic arterial supply and thus unexpected bleeding or ischemia.
PATIENT REPORT
A 50-year-old man was referred to our hospital because of epigastric pain and hematemesis. The patient had atrial fibrillation but no other medical, family, or psychosocial history. Upper gastrointestinal endoscopy revealed type 0-IIc early gastric cancer at the lesser curvature of the lower portion of the stomach after hemostasis of a bleeding ulcer. Examination of biopsy specimens revealed signet ring cell carcinoma. Neither regional lymph node metastasis nor distant metastasis was detected by abdominal computed tomography (CT). Therefore, the patient was diagnosed with stage I gastric cancer (8th UICC-TNM classification). CT showed an anatomical variation of the RHA, which branched from the GDA; additionally, the RGA branched from the root of the RHA. The left hepatic artery (LHA) branched from the common hepatic artery (CHA) (Fig. 1).
Fig. 1.
Preoperative three-dimensional computed tomography angiography. The RHA branched from the GDA. CHA, common hepatic artery; GDA, gastroduodenal artery; RGA, right gastric artery; RGEA, right gastroepiploic artery; LGA, left gastric artery; LHA, left hepatic artery; RHA, right hepatic artery; SPA, splenic artery.
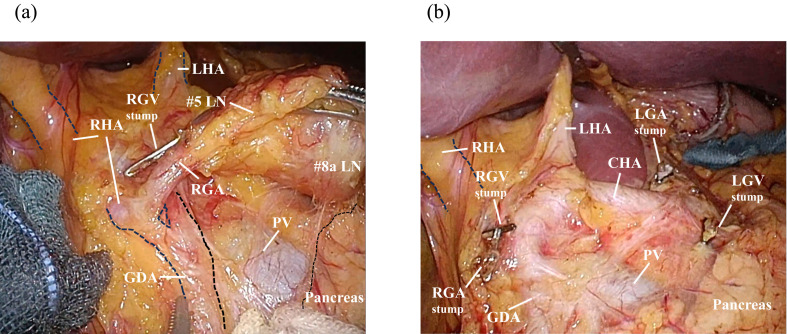
We performed laparoscopic distal gastrectomy with regional lymph node dissection, and the operation was completed with no serious difficulties except for the performance of supra-pancreatic lymph node dissection and separation of the RGA. As shown by preoperative imaging, intraoperative examination revealed that the RHA branched from the GDA and the RGA branched from the RHA. We easily identified each artery during dissection of adipose tissues containing the supra-pyloric lymph nodes (#5) and the supra-pancreatic lymph nodes (#8a) (Fig. 2a). The CHA was located on the cranial side, in contrast to the classical pattern, and the GDA was situated at the anterior aspect of the portal vein (Fig. 2b). Reconstruction was performed via the Roux-en-Y method. The operative time was short and intraoperative blood loss was minimal despite the anatomical variation. The patient developed no postoperative complications and was discharged on postoperative day 9. Histologic examination of the resected specimen demonstrated signet ring cell carcinoma invading the mucosa with no regional lymph node metastasis.
Fig. 2.
Perioperative findings. (a) The RHA branched from the GDA. (b) Lymph node dissection around the supra-pancreatic region was performed. LGA, LGV, RGA and RGV were dissected during the lymph node dissection. CHA, common hepatic artery; GDA, gastroduodenal artery; LGA, left gastric artery; LGV, left gastric vein; LHA, left hepatic artery; RGA, right gastric artery; RGV, right gastric vein; RHA, right hepatic artery; PV, portal vein.
DISCUSSION
Three-dimensional (3D) CT angiography facilitates easy detection of vascular anomalies, and some reports have emphasized that it contributes to safer procedures for gastric cancer.6, 7 We routinely perform 3D CT angiography (SYNAPSE VINCENT; Fujifilm Corporation, Tokyo, Japan) before gastrectomy.
Hiatt et al. described various anatomical patterns of the hepatic artery using a modification of the Michels classification.8 However, they did not describe rare patterns, such as that in the present case. Kobayashi et al. reported variations in the branches of the hepatic artery as shown by abdominal angiographic images of 1200 patients, and the RHA originating from the GDA was seen in only 0.1% of 1200 cases.4 Choi et al. more recently reported RHA originated from the GDA in 2.5% of 4942 cases using CT.5 The superior mesenteric artery is the most common origin of branching of the RHA. Although a few papers have described finding an anomalous hepatic artery from the GDA during pancreaticoduodenectomy,9, 10 this may be the first case report of such a rare vascular anatomical anomaly in a patient undergoing laparoscopic distal gastrectomy with lymph node dissection. In pancreaticoduodenectomy, if the GDA is mistakenly dissected at the point where the LHA branches off, the RHA will be inadvertently dissected. Additionally, in gastrectomy, mistaking the LHA for the proper hepatic artery can lead to difficulty in identifying the RGA. The present case had another distinct feature possibly due to such vascular branching: upon dissecting the adipose tissues containing the supra-pancreatic lymph nodes (#8a), the portal vein was identified before the CHA. In any case, damage to the hepatic artery can lead to bleeding or ischemia of the liver or bile duct, potentially resulting in adverse outcomes. Therefore, when such vascular anomalies are present, surgery must be performed with extreme care.
Minimally invasive techniques such as laparoscopic or robot-assisted surgery have become increasingly popular in gastrectomy. These surgeries require more delicate procedures than those used in open surgery, making a preoperative understanding of vascular anomalies even more crucial.
Even considering just the hepatic artery, various vascular anomalies are listed in the Adachi classification and Michels classification.3, 11 With advancements in preoperative vascular imaging techniques such as 3D CT angiography, new and more detailed vascular anomalies may be reported in the future. We previously reported a rare case of gastric resection in which the GDA branched from the celiac artery with the left gastric artery, splenic artery, and CHA.7 However, if a thorough understanding of these anomalies is attained before surgery, minimally invasive procedures can be safely completed without significant complications or inadequate lymph node dissection. Additional cases of rare vascular anomalies should be accumulated to further define the key points to be aware of during surgery.
Acknowledgments
Acknowledgments: We thank Angela Morben, DVM, ELS, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Katai H,Mizusawa J,Katayama H,Morita S,Yamada T,Bando E,et al. Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol. 2020;5:142-51. 10.1016/S2468-1253(19)30332-2 [DOI] [PubMed] [Google Scholar]
- 2.Etoh T,Ohyama T,Sakuramoto S,Tsuji T,Lee SW,Yoshida K,et al. ; Japanese Laparoscopic Surgery Study Group (JLSSG). Five-Year Survival Outcomes of Laparoscopy-Assisted vs Open Distal Gastrectomy for Advanced Gastric Cancer. JAMA Surg. 2023;158:445-54. 10.1001/jamasurg.2023.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3..Michels NA. Blood supply and anatomy of the upper abdominal organs, with a descriptive atlas. (No Title). 1955.
- 4.Kobayashi S,Otsubo T,Koizumi S,Ariizumi S,Katagiri S,Watanabe T,et al. Anatomic variations of hepatic artery and new clinical classification based on abdominal angiographic images of 1200 cases. Hepatogastroenterology. 2014;61:2345-8. [PubMed] [Google Scholar]
- 5.Choi TW,Chung JW,Kim HC,Lee M,Choi JW,Jae HJ,et al. Anatomic Variations of the Hepatic Artery in 5625 Patients. Radiol Cardiothorac Imaging. 2021;3:e210007. 10.1148/ryct.2021210007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayashi H,Hirahara N,Matsubara T,Takao S,Okamura H,Nakamura K,et al. Duplicate left gastric artery identified during robot-assisted distal gastrectomy: a case report. Surg Case Rep. 2023;9:148. 10.1186/s40792-023-01698-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shimizu S,Matsunaga T,Sakano Y,Makinoya M,Shishido Y,Miyatani K,et al. A gastroduodenal artery that branched from the celiac artery in gastrectomy: A rare case of an anatomical variant. Asian J Endosc Surg. 2024;17:e13268. 10.1111/ases.13268 [DOI] [PubMed] [Google Scholar]
- 8.Hiatt JR,Gabbay J,Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994;220:50-2. 10.1097/00000658-199407000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adamthwaite JA,Pennington N,Menon KV. Anomalous hepatic arterial anatomy discovered during pancreaticoduodenectomy. Surg Radiol Anat. 2007;29:269-71. 10.1007/s00276-007-0189-1 [DOI] [PubMed] [Google Scholar]
- 10.Krishna PS,soori A,Kalayarasan R,Biju P. Replaced Segment 6 Artery From the Gastroduodenal Artery: A Challenging and Rare Anatomical Variation of Hepatic Artery in Pancreaticoduodenectomy. Cureus. 2023;15:e44605. 10.7759/cureus.44605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adachi B. Das arteriensystem der Japaner. Band. 1928. [Google Scholar]